What is acute bronchitis
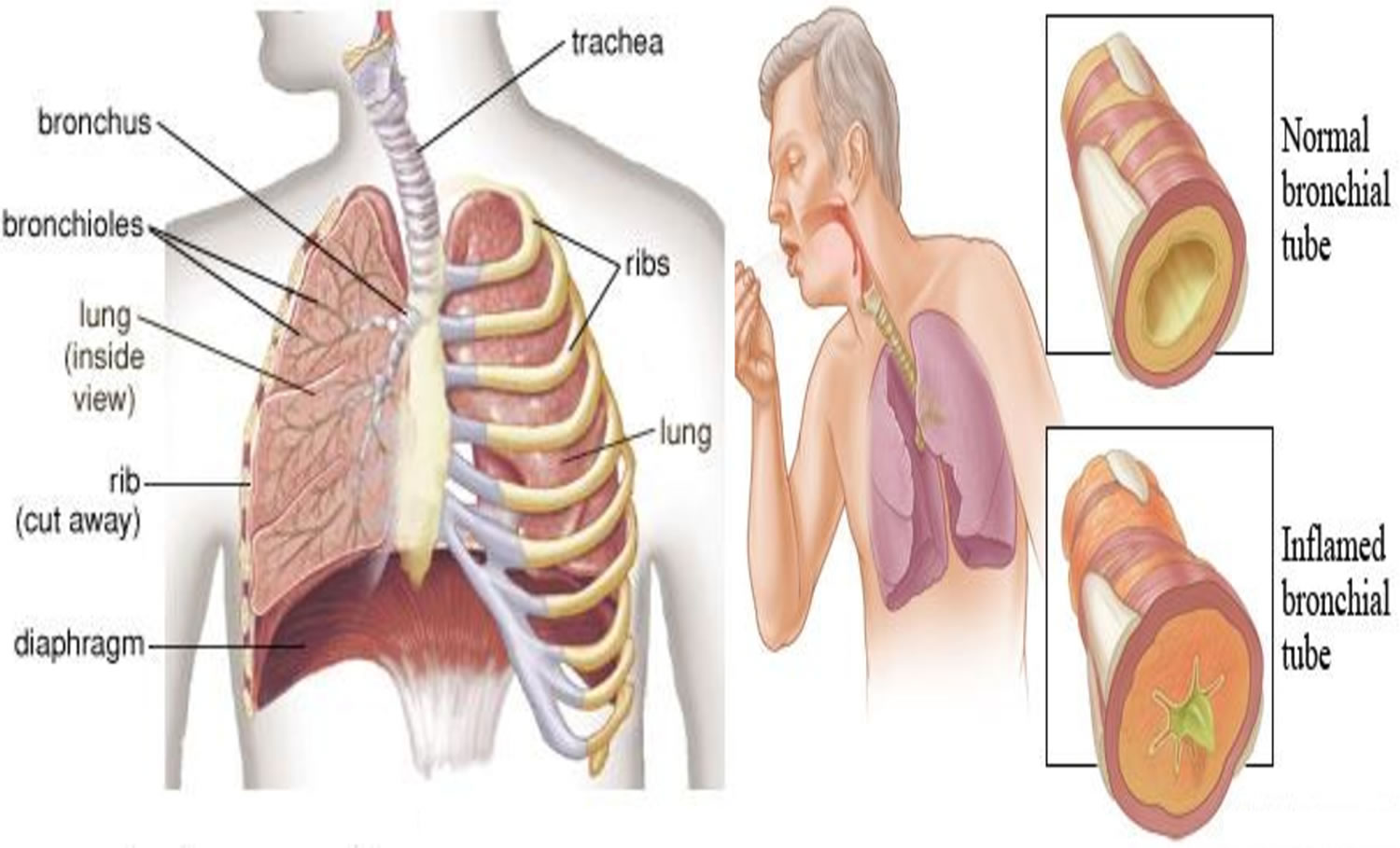
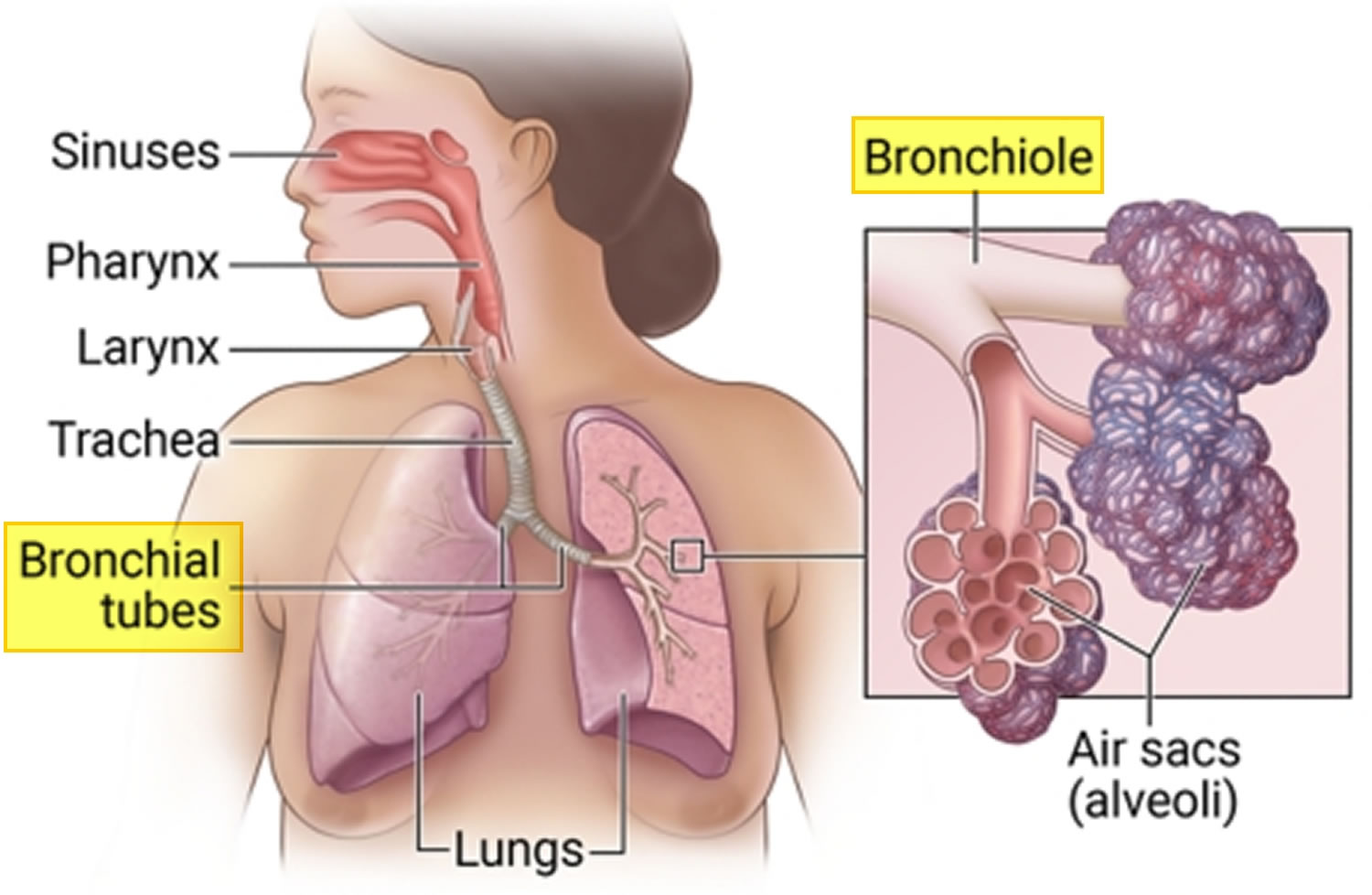
Bronchitis is a medical term for when the major airways that carry air to your lungs, your bronchi (bronchial tubes), become inflamed. Acute bronchitis usually happens because of a virus or breathing in something that irritates your lungs such as tobacco smoke, fumes, dust and air pollution. This irritation can cause severe coughing spells that bring up mucus, wheezing, chest pain, chest tightness, shortness of breath and a low fever. There are two main types of bronchitis: acute bronchitis and chronic bronchitis.
Acute bronchitis is a form of lower respiratory infection that affects the air tubes (bronchi) of your lungs. Acute bronchitis is a clinical diagnosis characterized by acute cough, with or without sputum production, and signs of lower respiratory tract infection in the absence of chronic lung disease, such as chronic obstructive pulmonary disease (COPD) or an identifiable cause, such as pneumonia or sinusitis 1. Acute bronchitis usually comes on suddenly and lasts for a week to 10 days. This is very different from chronic bronchitis, which is a more serious, life-long condition.
Most cases of acute bronchitis get better within several days. But your cough can last for two to three weeks after the infection is gone. This happens because your bronchial tubes take a while to heal.
The same viruses that cause colds and the flu (influenza) often cause acute bronchitis. These viruses spread through the air when people cough, or though physical contact (for example, on unwashed hands). Being exposed to tobacco smoke, air pollution, dusts, vapors, and fumes can also cause acute bronchitis. Less often, bacteria can also cause acute bronchitis.
Acute bronchitis usually gets better on its own without the need for medical treatment. Acute bronchitis treatments include rest, fluids, and aspirin (for adults) or acetaminophen (paracetamol) to treat fever. A humidifier or steam may also help. You may need inhaled medicine to open your airways if you are wheezing. Antibiotics won’t help if the cause is viral bronchitis. You may get antibiotics if the cause is acute bacterial bronchitis.
Figure 1. Bronchial tubes
Figure 2. Acute bronchitis
See a doctor if you have any of the following:
- Temperature of 100.4 °F (38 °C) or higher
- Cough with bloody mucus
- Shortness of breath or trouble breathing
- Symptoms that last more than 3 weeks
- Repeated episodes of bronchitis
This list is not all-inclusive. Please see a doctor for any symptom that is severe or concerning you.
Is acute bronchitis contagious?
Yes. Most of the time, acute bronchitis is caused by a virus, such as the flu (influenza) virus. However, many different viruses — all of which are very contagious — can cause acute bronchitis.
Viruses spread mainly from person to person by droplets produced when an ill person coughs, sneezes or talks and you inhale the droplets. Viruses may also spread through contact with an infected object. This happens when you touch something with the virus on it and then touch your mouth, eyes or nose.
To reduce your risk of catching viruses that can cause bronchitis:
- Avoid close contact with people who have the flu or another respiratory illness
- Wash your hands often or use an alcohol-based hand sanitizer
- Avoid touching your eyes, nose and mouth
- Get an annual flu shot
People who have chronic bronchitis or asthma sometimes develop acute bronchitis. In these cases, the acute bronchitis is most likely a complication of the existing condition. This type of bronchitis is not caused by an infectious virus, so it’s less likely to be contagious.
Acute bronchitis vs chronic bronchitis
Bronchitis is when the airways that carry air to your lungs, your bronchi or bronchial tubes, become inflamed. This irritation can cause severe coughing spells that bring up mucus, wheezing, chest pain, chest tightness, shortness of breath and a low fever. There are two main types of bronchitis: acute bronchitis and chronic bronchitis.
Acute bronchitis is a form of lower respiratory infection that affects the air tubes (bronchi) of the lungs. Acute bronchitis usually comes on suddenly and lasts for a week to 10 days. This is very different from chronic bronchitis, which is a more serious, life-long condition.
Unlike acute bronchitis, which usually develops from a respiratory infection such as a cold and goes away in a week or two, chronic bronchitis is a more serious condition that develops over time. Symptoms may get better or worse, but they will never completely go away. These extended periods of inflammation cause sticky mucus to build up in the airways, leading to long-term breathing difficulties.
Along with emphysema, chronic bronchitis is one of the lung diseases that comprise COPD (chronic obstructive pulmonary disease). There are a number of treatments available to help control symptoms and ease breathing problems in people with chronic bronchitis.
Chronic bronchitis key facts:
- Chronic bronchitis is included in the umbrella term COPD (chronic obstructive pulmonary disease). Your doctor may refer to your disease as either chronic bronchitis or COPD (chronic obstructive pulmonary disease).
- Cigarette smoking is a major cause of chronic bronchitis. Other factors that increase your risk of developing this disease include exposure to air pollution as well as dust or toxic gases in the workplace or environment. It may also occur more frequently in individuals who have a family history of bronchitis.
- To diagnose chronic bronchitis, your doctor will look for a productive cough (producing mucus) that lasts at least three months and happens multiple times over the course of at least two years. Tests used to diagnose chronic bronchitis include pulmonary function tests, chest X-rays or CT scans.
- Chronic bronchitis is not curable but there are a number of treatments that can help you manage your symptoms. These include bronchodilators that open your airways, steroids to reduce inflammation, oxygen therapy and pulmonary rehabilitation.
Acute bronchitis signs and symptoms
During the first few days of illness, acute bronchitis symptoms are similar to that of a common cold. Symptoms of acute bronchitis last less than 3 weeks.
The most common symptoms of acute bronchitis are:
- Runny, stuffy nose
- Low-grade fever
- Chest congestion or tightness
- Wheezing or a whistling sound while breathing
- Shortness of breath
- A cough that may produce clear, yellow or green mucus (sputum)
- Feeling run-down or tired (fatigue)
- Sore throat
- Mild headache
- Mild body aches
- Chills
Because the cough associated with acute bronchitis is so bothersome and slow to resolve, patients often seek treatment. The duration of acute bronchitis–related cough is typically two to three weeks, with a pooled estimate of 18 days in one systematic review 2. This corresponds to results of a prospective trial, which found that patients who had a cough for at least five days had a median of 18 days of coughing 3.
Besides the cough, other signs and symptoms of acute bronchitis include sputum production, dyspnea (shortness of breath), nasal congestion, headache, and fever 4, 5. The first few days of an acute bronchitis infection may be indistinguishable from the common cold. Patients may have substernal or chest wall pain when coughing. Fever is not a typical finding after the first few days, and presence of a fever greater than 100°F (37.8°C) should prompt consideration of influenza or pneumonia. Production of sputum, even purulent, is common and does not correlate with bacterial infection 6.
Acute bronchitis complications
- Secondary pneumonia. Pneumonia is an infection in one or both of your lungs. It causes the air sacs of your lungs to fill up with fluid or pus. Pneumonia can range from mild to severe, depending on the type of germ causing the infection, your age, and your overall health
- Respiratory distress
The risk of developing complications from acute bronchitis, such as pneumonia, is greater in some people. These include:
- Young children
- The elderly
- People who have asthma
- People who have other health issues (such as cancer or diabetes)
- People who haven’t gotten vaccines for flu, pneumonia, or whooping cough.
Acute bronchitis causes
Acute bronchitis is most often caused by a contagious virus 7, 5. Approximately 95% of acute bronchitis in healthy adults are caused by viruses. The most commonly identified viruses are respiratory syncytial virus (RSV), influenza virus A and B, parainfluenza, rhinovirus, enterovirus, coronavirus and human metapneumovirus 7. First, the virus affects your nose, sinuses, and throat. Then the infection travels to the lining of your bronchial tubes. As your body fights the virus, swelling occurs and mucus is produced.
You can catch a virus from breathing it in or by skin contact. You are at higher risk of catching the virus if you have close contact with someone who has a cold or acute bronchitis.
Lesser-known causes of acute bronchitis are:
- Bacteria or fungal infections.
- Exposure to irritants, such as smoke, dust, or fumes. You are at greater risk if your bronchial tubes already have damage.
- GERD (gastroesophageal reflux disease), which causes heartburn. You can get acute bronchitis when stomach acid gets into the bronchial tubes.
Bacteria are detected in 1% to 10% of cases of acute bronchitis 5. When the infection is bacterial, the isolated pathogens are usually the same as those responsible for community-acquired pneumonia, for example, Streptococcus pneumonia and Staphylococcus aureus 8. Atypical bacteria, such as Mycoplasma pneumoniae, Chlamydophila pneumoniae, and Bordetella pertussis, are rare causes of acute bronchitis. In a study of sputum samples of adults with acute cough for more than five days, Mycoplasma pneumoniae was isolated in less than 1% of cases and Chlamydophila pneumoniae was not identified 9.
Approximately 10% of patients presenting with a cough lasting at least two weeks have evidence of Bordetella pertussis infection (whooping cough) 10. During outbreaks, pertussis detection is more likely in children and those with prolonged coughs 10. Antibiotics can eradicate Bordetella pertussis from the nasopharynx. They do not seem to shorten the course of illness unless given in the first one to two weeks 11. Isolated outbreaks of pertussis occur throughout the United States, and increased testing of adults and children should be considered during these periods.
Acute bronchitis can sometimes be caused by allergens, irritants and fungi. Irritants include smoke inhalation, polluted air inhalation, dust, among others 12.
You are more vulnerable to developing acute bronchitis if:
- You have close contact with someone who has a cold or acute bronchitis
- You have not been immunized against the flu
- You are exposed to lung irritants like tobacco smoke, fumes, dust and air pollution
Acute bronchitis risk factors
Factors like a history of smoking, living in a polluted place, crowding, and a history of asthma, are all risk factors for acute bronchitis 13. In some people, acute bronchitis can be triggered by particular allergens like pollens, perfume, and vapors.
Acute bronchitis pathophysiology
Acute bronchitis is the result of acute inflammation of the bronchi (bronchial tubes) secondary to various triggers, most commonly viral infection, allergens, pollutants, etc 13. The infection usually starts in your nose or throat and travels to the bronchial tubes. When your body tries to fight the infection, it causes the bronchial tubes to swell. Inflammation of the bronchial wall leads to mucosal thickening, epithelial-cell desquamation, and denudation of the basement membrane 13. At times, a viral upper respiratory infection can progress to infection of the lower respiratory tract resulting in acute bronchitis 14. This causes you to cough. Sometimes it is a dry cough, but often you will cough up mucus (sputum). The swelling also narrows your airways, allowing less air to pass through, which can cause wheezing, chest tightness and shortness of breath. With time, the immune system can fight off the infection and your airways return to normal.
Acute bronchitis prevention
You can help prevent acute bronchitis by staying healthy and avoiding lung irritants that include smoking. To help protect your lungs, wear a mask over your mouth and nose when using lung irritants such as paint, paint remover or varnish. Wash your hands often with soap to kill any contagious viruses and receive a flu shot every year. Ask your doctor if you should get a pneumonia shot, especially if you’re 65 or older.
You can help prevent acute bronchitis by doing your best to stay healthy and keep others healthy, including:
- Washing your hands with soap often to kill any contagious viruses.
- Get recommended vaccines, such as the flu vaccine.
- Don’t smoke and avoid secondhand smoke. If you smoke, the best defense against acute bronchitis is to quit. Smoking damages your bronchial tubes and puts you at risk for infection. Smoking also slows down the healing process.
- Cover your mouth and nose when coughing or sneezing.
- Wear a mask over your nose and mouth when using lung irritants. These could include paint, paint remover, or varnish.
Acute bronchitis diagnosis
To diagnose acute bronchitis, your doctor will ask about your symptoms and do a physical examination including listening to your breathing and your chest with a stethoscope. You may also have other tests. Though they rarely order additional tests, if you have a fever, your physician may order a chest X-ray to rule out pneumonia.
Indications for chest X-ray in adult patients with symptoms of acute bronchitis 15:
- Dyspnea (shortness of breath), bloody sputum, or rusty sputum color
- Pulse (heart rate) > 100 beats per minute
- Respiratory rate > 24 breaths per minute
- Oral body temperature > 100°F (37.8°C)
- Focal consolidation, egophony, or fremitus on chest examination.
Acute bronchitis treatment
Most cases of acute bronchitis go away on their own because they are caused caused by a virus. The infection simply has to run its course over several weeks. Treatment options your doctor may suggest are:
- Resting and getting plenty of fluids
- Drinking lots of water, which helps loosen chest congestion
- A cough suppressant and/or pain reliever
- A humidifier or steam
Antibiotics are not effective for treating viral infections. Antibiotics have been shown to provide only minimal benefit, reducing the cough or illness by about half a day, and have adverse effects, including allergic reactions, nausea and vomiting, and Clostridium difficile infection 16. But if your doctor suspects that you have a bacterial infection, he or she may give you antibiotics.
If you have whooping cough (pertussis) or pneumonia, which can have similar symptoms to acute bronchitis, your doctor will most likely prescribe antibiotics.
All major guidelines on acute bronchitis, including those from the American College of Chest Physicians, recommend against using antibiotics for acute bronchitis unless the patient has a known pertussis infection 17, 1. The American Academy of Pediatrics recommends that antibiotics not be used for apparent viral respiratory illnesses, including sinusitis, pharyngitis, and bronchitis 18. Despite these recommendations, antibiotics are often prescribed for acute bronchitis 19.
Acute bronchitis home remedies
Home remedies focus on easing your symptoms.
Below are some ways you can feel better while your body fights off acute bronchitis:
- Get plenty of rest.
- Drink plenty of fluids, but avoid caffeine and alcohol.
- Use a clean humidifier or cool mist vaporizer.
- Use saline nasal spray or drops to relieve a stuffy nose.
- For young children, use a rubber suction bulb to clear mucus.
- Breathe in steam from a bowl of hot water or shower.
- Suck on lozenges. Do not give lozenges to children younger than 4 years of age.
- Use honey to relieve cough for adults and children at least 1 year of age or older. Honey can soothe coughs – either eaten on its own or stirred into a warm drink. Studies in children suggest that honey can soothe coughs associated with upper respiratory tract infections. But children under the age of one shouldn’t eat honey because they sometimes react sensitively to certain bacteria in it.
- Take over-the-counter (OTC) pain relievers to reduce inflammation, ease pain, and lower your fever. These could include acetaminophen (paracetamol) or ibuprofen. Never give aspirin to a child. It has been linked to Reye syndrome, which can affect the liver and brain.
Ask your doctor or pharmacist about over-the-counter (OTC) medicines that can help you feel better. Always use over-the-counter medicines as directed. Remember, over-the-counter (OTC) medicines may provide temporary relief of symptoms, but they will not cure your illness.
There are some over-the-counter cough medicines that help break up or loosen mucus. Look for the word “guaifenesin” on the label or ask your pharmacist for a suggestion.
Do not hold in a cough that brings up mucus. This type of cough helps clear mucus from your bronchial tubes. If you smoke, you should quit. It will help your bronchial tubes heal faster.
Some people who have acute bronchitis need inhaled medicine. You might need this if you are wheezing. It can help open your bronchial tubes and clear out mucus. You usually take it with an inhaler. An inhaler sprays medicine right into your bronchial tubes. Your doctor will decide if this treatment is right for you.
A randomized controlled trial showed that compared with placebo, there was no benefit from ibuprofen in decreasing severity or duration of cough in patients with acute bronchitis 20 Another randomized controlled trial comparing ibuprofen, acetaminophen (paracetamol) and steam inhalation found that those with a lower respiratory tract infection or age younger than 16 years had a modest reduction in symptom severity when taking ibuprofen over acetaminophen (paracetamol), although the ibuprofen group was more likely to seek care again for new or nonresolving symptoms 21.
Antihistamines are often used in combination with decongestants in the treatment of acute cough. Two trials of antihistamines alone showed no benefit compared with placebo in relieving cough symptoms. Combination decongestant/antihistamines are more likely to have adverse effects with no to modest improvement in cough symptom scores 22. In 2008, The U.S. Food and Drug Administration (FDA) warned against the use of over-the-counter cough medications containing antihistamines and antitussives in young children because of the high risk for harm and these medications are no longer labeled for use in children younger than four years. They are continuing to investigate the safety of these medications in children up to 11 years of age 23.
Over-the-counter medicine and children
Be careful when giving over-the-counter (OTC) medicines to children. Not all over-the-counter (OTC) medicines are recommended for children of certain ages.
Pain relievers:
- Children younger than 6 months: only give acetaminophen (paracetamol).
- Children 6 months or older: it is OK to give acetaminophen (paracetamol) or ibuprofen.
- NEVER give aspirin to children because it can cause Reye’s syndrome, a rare but very serious illness that harms the liver and brain.
Cough and cold medicines:
- Children younger than 4 years old: DO NOT use unless a doctor specifically tells you to. Use of over-the-counter cough and cold medicines in young children can result in serious and potentially life-threatening side effects.
- Children 4 years or older: discuss with your child’s doctor if over-the-counter cough and cold medicines are safe to give to your child for temporary symptom relief.
Be sure to ask your doctor or pharmacist about the right dosage of over-the-counter medicines for your child’s age and size. Also, tell your child’s doctor and pharmacist about all prescription and over-the-counter medicines they are taking.
Acute bronchitis cough medicine
Cough suppressants
Antitussives are medicines that suppress coughing, also known as cough suppressants, work by reducing the cough reflex and can be divided into central opioids and peripherally acting agents. Codeine is a centrally acting, weak opioid that suppresses cough. Two studies show no benefit from codeine in decreasing cough symptoms 22 and the American College of Chest Physicians does not recommend its use in the treatment of upper respiratory tract infections 15. Cough suppressants should only be used in the treatment of severe dry coughs, for a maximum period of two weeks. They shouldn’t be used in the treatment of productive (“wet”) coughs: If the urge to cough is suppressed, the phlegm won’t be coughed up and out of the lungs 24.
Dextromethorphan is a nonopioid, synthetic derivative of morphine that works centrally to decrease cough. Three placebo-controlled trials show that dextromethorphan, 30 mg, decreased the cough count by 19% to 36% compared with placebo, which is equivalent to eight to 10 fewer coughing bouts per 30 minutes 22.
Benzonatate is a peripherally acting antitussive that is thought to suppress cough via anesthesia of the respiratory stretch receptors. One small study comparing benzonatate, guaifenesin, and placebo showed significant improvement with the combination of benzonatate and guaifenesin, but not with either agent alone 25.
Expectorants
Expectorants are chemicals that help you clear phlegm or mucus from your respiratory tract or your airways. They add moisture into the mucus, making it less sticky and easier to cough up.
Guaifenesin is a commonly used expectorant. It is thought to stimulate respiratory tract secretions, thereby increasing respiratory fluid volumes and decreasing mucus viscosity, and it may also have antitussive properties.
A Cochrane review including three trials of guaifenesin vs. placebo showed some benefit 22. In one trial, patients reported that guaifenesin decreased cough frequency and intensity by 75% at 72 hours compared with 31% in the placebo group (number needed to treat = 2). A second trial showed decreased cough frequency (100% of the guaifenesin group vs. 94% of the placebo group) and improved cough severity (100% of the guaifenesin group vs. 91% of the placebo group) at 36 hours, and reduced sputum thickness (96% of the guaifenesin group vs. 54% of the placebo group). A third trial using an extended-release formulation of guaifenesin showed improved symptom severity at day 4 but no difference at day 7 22.
Beta2 agonists (bronchodilators)
Many patients with acute bronchitis have bronchial hyperreactivity, leading to impaired airflow in a mechanism similar to asthma. Beta2 agonists bronchodilators (medications to widen the airways) are normally used in the form of an inhaler for the treatment of lung conditions that cause the airways to narrow, such as asthma and COPD. A 2015 Cochrane review does not support the routine use of beta2 agonists for acute cough 26. Two trials included children and found no benefit from albuterol in decreasing daily cough scores, daily proportion of cough, or median duration of cough, although both studies excluded children who were wheezing at the time of evaluation or had signs of bronchial obstruction. The studies of adults had mixed results, but the findings suggest that beta2 agonists should be avoided if there is no underlying history of lung disease or evidence of wheeze or airway obstruction. However, beta2 agonists may have some benefit in certain adults, especially those with wheezing at the time of evaluation who do not have a previous diagnosis of asthma or chronic obstructive pulmonary disease. Because there is limited supportive evidence, the use of such medications should be weighed against the risk of adverse effects, including tremor, shakiness, and nervousness 26.
Herbal medicines and preparations
Alternative medications are commonly used in the treatment of acute bronchitis. Pelargonium sidoides (also known as African geranium and South African geranium) has some reported modest effectiveness in the treatment of acute bronchitis, but the quality of evidence is considered low and the studies were all done by the manufacturer in Ukraine and Russia 27. There are insufficient data to recommend for or against the use of Chinese medicinal herbs for the treatment of acute bronchitis, and there are safety concerns 28.
A Cochrane review of honey for acute cough in children included two small trials comparing honey with dextromethorphan, diphenhydramine (Benadryl), and no treatment 29. Honey was found to be better than no treatment in decreasing the frequency and severity of cough, decreasing bothersome cough, and improving quality of sleep. Given the warnings against the use of antitussives in young children, honey is a reasonable alternative for the relief of acute cough in children older than one year 29.
Acute bronchitis prognosis
Acute bronchitis is self-limiting and resolves with symptomatic treatment in most instances. Most cases of acute bronchitis go away on their own in 7 to 10 days. On average, the symptoms of acute bronchitis last only a couple of weeks. The cough associated with acute bronchitis typically lasts about two to three weeks 16. This happens because your bronchial tubes take a while to heal. However, a lasting cough may also signal another problem, such as asthma or pneumonia. Therefore, if you have a cough that won’t go away or if you get sick with bronchitis frequently, it may be the sign of a more serious disease and you should visit your doctor. Secondary pneumonia is possible. Rare cases of acute respiratory distress syndrome (ARDS) and respiratory failure have been reported in the literature 30. Acute respiratory distress syndrome (ARDS) is a rapidly progressive disease that causes fluid to leak into your lungs, making it difficult to get oxygen into your blood. Most people who get ARDS are already in the hospital for their illness. Respiratory failure is a condition in which your blood doesn’t have enough oxygen or has too much carbon dioxide. Sometimes you can have both problems.
You should see your doctor if:
- You continue to wheeze and cough for more than 2 weeks, especially at night when you lie down or when you are active.
- You continue to cough for more than 2 weeks and have a bad-tasting fluid come up into your mouth. This may mean you have gastroesophageal reflux disease (GERD). This is a condition in which stomach acid gets into your esophagus.
- Your cough produces blood, you feel weak, you have an ongoing high fever, and you are short of breath. These symptoms may mean you have pneumonia.
- Woodhead M, Blasi F, Ewig S, et al.; Joint Taskforce of the European Respiratory Society and European Society for Clinical Microbiology and Infectious Diseases. Guidelines for the management of adult lower respiratory tract infections—full version. Clin Microbiol Infect. 2011;17(suppl 6):E1–E59.
- Ebell MH, Lundgren J, Youngpairoj S. How long does a cough last? Comparing patients’ expectations with data from a systematic review of the literature. Ann Fam Med. 2013;11(1):5–13.
- Ward JI, Cherry JD, Chang SJ, et al.; APERT Study Group. Efficacy of an acellular pertussis vaccine among adolescents and adults. N Engl J Med. 2005;353(15):1555–1563.
- van Vugt SF, Verheij TJ, de Jong PA, et al.; GRACE Project Group. Diagnosing pneumonia in patients with acute cough: clinical judgment compared to chest radiography. Eur Respir J. 2013;42(4):1076–1082.
- Gencay M, Roth M, Christ-Crain M, Mueller B, Tamm M, Stolz D. Single and multiple viral infections in lower respiratory tract infection. Respiration. 2010;80(6):560–567.
- Altiner A, Wilm S, Däubener W, et al. Sputum colour for diagnosis of a bacterial infection in patients with acute cough. Scand J Prim Health Care. 2009;27(2):70–73.
- Clark TW, Medina MJ, Batham S, Curran MD, Parmar S, Nicholson KG. Adults hospitalised with acute respiratory illness rarely have detectable bacteria in the absence of COPD or pneumonia; viral infection predominates in a large prospective UK sample. J Infect. 2014;69(5):507–515.
- Bai L, Su X, Zhao D, Zhang Y, Cheng Q, Zhang H, Wang S, Xie M, Su H. Exposure to traffic-related air pollution and acute bronchitis in children: season and age as modifiers. J Epidemiol Community Health. 2018 May;72(5):426-433. doi: 10.1136/jech-2017-209948
- Wadowsky RM, Castilla EA, Laus S, et al. Evaluation of Chlamydia pneumoniae and Mycoplasma pneumoniae as etiologic agents of persistent cough in adolescents and adults. J Clin Microbiol. 2002;40(2):637–640.
- Philipson K, Goodyear-Smith F, Grant CC, Chong A, Turner N, Stewart J. When is acute persistent cough in school-age children and adults whooping cough? Br J Gen Pract. 2013;63(613):e573–e579.
- Altunaiji S, Kukuruzovic R, Curtis N, Massie J. Antibiotics for whooping cough (pertussis). Cochrane Database Syst Rev. 2007;(3):CD004404.
- Tanner M, Karen Roddis J. Antibiotics for acute bronchitis. Nurs Stand. 2018 Feb 28;32(27):41-43. doi: 10.7748/ns.2018.e11123
- Singh A, Avula A, Zahn E. Acute Bronchitis. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448067
- Wenzel RP, Fowler AA 3rd. Clinical practice. Acute bronchitis. N Engl J Med. 2006 Nov 16;355(20):2125-30. doi: 10.1056/NEJMcp061493
- Braman SS. Chronic cough due to acute bronchitis: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 suppl):95S–103S.
- Acute Bronchitis. Am Fam Physician. 2016 Oct 1;94(7):560-565. https://www.aafp.org/afp/2016/1001/p560.html
- Smith, M. P., Lown, M., Singh, S., Ireland, B., Hill, A. T., Linder, J. A., Irwin, R. S., & CHEST Expert Cough Panel (2020). Acute Cough Due to Acute Bronchitis in Immunocompetent Adult Outpatients: CHEST Expert Panel Report. Chest, 157(5), 1256–1265. https://doi.org/10.1016/j.chest.2020.01.044
- American Academy of Pediatrics. Five things physicians and patients should question. https://www.choosingwisely.org/wp-content/uploads/2015/02/AAP-Choosing-Wisely-List.pdf
- Barnett ML, Linder JA. Antibiotic prescribing for adults with acute bronchitis in the United States, 1996–2010. JAMA. 2014;311(19):2020–2022.
- Llor C, Moragas A, Bayona C, et al. Efficacy of anti-inflammatory or antibiotic treatment in patients with non-complicated acute bronchitis and discoloured sputum: randomised placebo controlled trial. BMJ. 2013;347:f5762.
- Little P, Moore M, Kelly J, et al.; PIPS Investigators. Ibuprofen, paracetamol, and steam for patients with respiratory tract infections in primary care. BMJ. 2013;347:f6041.
- Smith SM, Schroeder K, Fahey T. Over-the-counter (OTC) medications for acute cough in children and adults in community settings. Cochrane Database Syst Rev. 2014;(11):CD001831
- Briars LA. The latest update on over-the-counter cough and cold product use in children. J Pediatr Pharmacol Ther. 2009;14(3):127–131.
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Treating acute bronchitis. [Updated 2020 Dec 2]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK458286
- Dicpinigaitis PV, Gayle YE, Solomon G, Gilbert RD. Inhibition of cough-reflex sensitivity by benzonatate and guaifenesin in acute viral cough. Respir Med. 2009;103(6):902–906.
- Becker LA, Hom J, Villasis-Keever M, van der Wouden JC. Beta2agonists for acute cough or a clinical diagnosis of acute bronchitis. Cochrane Database Syst Rev. 2015;(9):CD001726
- Timmer A, Günther J, Motschall E, Rücker G, Antes G, Kern WV. Pelargonium sidoides extract for treating acute respiratory tract infections. Cochrane Database Syst Rev. 2013;(10):CD006323
- Jiang L, Li K, Wu T. Chinese medicinal herbs for acute bronchitis. Cochrane Database Syst Rev. 2012;(2):CD004560
- Oduwole O, Meremikwu MM, Oyo-Ita A, Udoh EE. Honey for acute cough in children. Cochrane Database Syst Rev. 2014;(12):CD007094
- Ngu, S., Pervaiz, S., Avula, A., & Chalhoub, M. (2019). Rhinovirus-induced Rapidly Progressing Acute Respiratory Distress Syndrome in an Immunocompetent Host. Cureus, 11(2), e3997. https://doi.org/10.7759/cureus.3997