What is adiposis dolorosa
Adiposis dolorosa also known as Dercum disease, is a rare condition characterized by the growth of multiple, painful, lipomas (benign, fatty tumors). The lipomas may occur anywhere on the body and can cause severe pain. Other symptoms may include weakness, fatigue, memory disturbances, painful subcutaneous plaques and ecchymoses (bruises) without noticed trauma. Adiposis dolorosa may be associated with obesity and emotional upset. Adiposis dolorosa (Dercum disease) usually occurs in adults, and women are more commonly affected than men. Adiposis dolorosa is chronic and tends to be progressive. Adiposis dolorosa was first described in 1892, by Dercum, who named the disease “adiposis dolorosa” to describe the painful adiposities (fat accumulations) seen in his 3 patients.
Adiposis dolorosa exact cause is unknown. Most cases are sporadic (not inherited) but a few familial cases with autosomal dominant inheritance have been reported.
Adiposis dolorosa (Dercum disease) affects females more often than males with some reports citing the disease is as 20 times more common in women. Adiposis dolorosa (Dercum disease) can affect individuals of any age. The majority of cases are women between the ages of 45-60, especially overweight, postmenopausal women. Although an extremely rare occurrence, it has been reported in children.
The pain associated with adiposis dolorosa is difficult to treat. Conventional pain medicines do not seem to reduce the discomfort associated with adiposis dolorosa. Some reports do suggest that a local anesthetic injection or patch can provide relief for intractable pain. Surgical removal or liposuction may help, but lipomas may recur 1. Adiposis dolorosa seems to benefit from the patient losing weight. Surgical excision or liposuction of selected lipomas may help, especially when they are in inconvenient locations. Surgical excision of many lipomas is not usually thought to be helpful and risks surgical complications.
Who gets adiposis dolorosa?
- Adiposis dolorosa affects women more frequently than men (it’s reportedly, 5–30 times more common in women than in men).
- Adiposis dolorosa usually appears between 35 and 50 years of age.
- Adiposis dolorosa may be more common in people with obesity.
Most people with adiposis dolorosa do not have a family history of adiposis dolorosa. However, the disease has been reported as showing an autosomal dominant pattern of inheritance in some families (ie the children of someone with adiposis dolorosa have a 1-in-2 likelihood of also developing it.)
What causes adiposis dolorosa?
The exact cause of adiposis dolorosa is unknown. In most cases, adiposis dolorosa appears to occur spontaneously for no apparent reason (sporadic).
Some reports in the medical literature have suggested that adiposis dolorosa may be an autoimmune disorder- a disorder in which the body’s immune system mistakenly attacks healthy tissue. Disturbances in endocrine function and improper breakdown (metabolism) of fat have also been proposed as potentially playing a role the development of the disorder. One cases reported in the medical literature was linked to the use of high-doses of corticosteroids.
Some cases of adiposis dolorosa have run in families and several reports in the medical literature cite the possibility that the disorder may be inherited as an autosomal dominant trait in these cases. Genetic diseases are determined by the combination of genes for a particular trait that are on the chromosomes received from the father and the mother.
Dominant genetic disorders occur when only a single copy of an abnormal gene is necessary for the appearance of the disease. The abnormal gene can be inherited from either parent, or can be the result of a new mutation (gene change) in the affected individual. The risk of passing the abnormal gene from affected parent to offspring is 50 percent for each pregnancy regardless of the sex of the resulting child.
Adiposis dolorosa symptoms
Adiposis dolorosa symptoms vary significantly by person; not all people have all symptoms.
Adiposis dolorosa symptoms may include:
- Painful lipomas in subcutaneous adipose tissues, present >3 months, upon palpation, sporadic or spontaneous.
- Cognitive: expressive language difficulties and memory deficits
- Vascular: angiolipomas, easy bruising, flushing
- Dermatologic: multiple cherry angiomas and petechiae
- Gastro-intestinal: gastroesophageal reflux disease (GERD), irritable bowel syndrome (IBS), early satiety
- Musculoskeletal: joint pain/stiffness increased in areas of fat deposits; muscle pain/stiffness pronounced at standing after period of inactivity and after physical activity
- Cardio/Pulmonary: tachycardia ranging from palpations to supraventricular tachycardia requiring pharmacologic intervention; shortness of breath
- General: sleep disturbance, insomnia, depression, anxiety, weight gain, heavy or prolonged menstrual bleeding, migraines, fatigue increased by activities of daily living and exercise
- Symptoms may progress to immobility
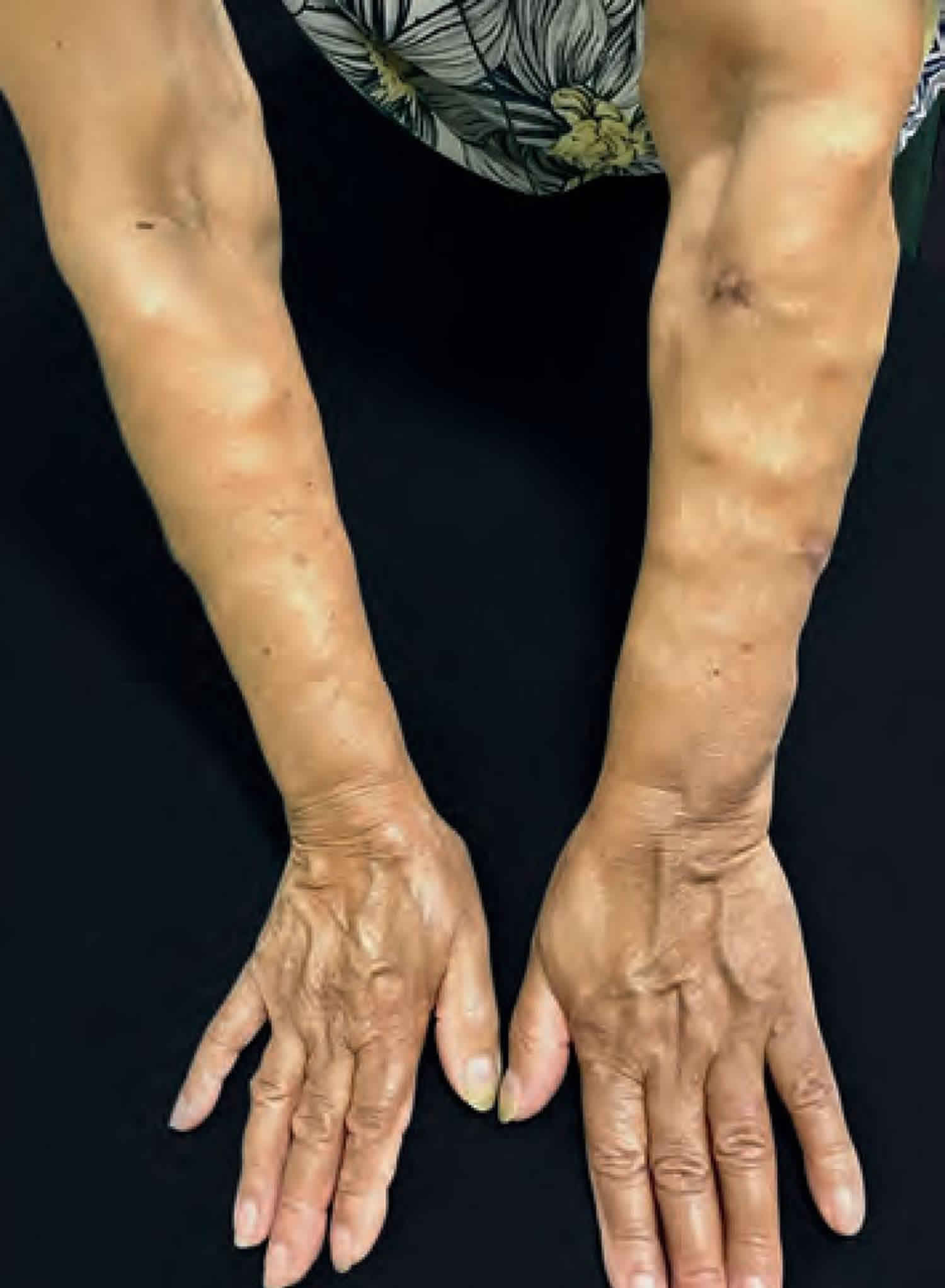
The characteristic finding of adiposis dolorosa is the slow formation of multiple, painful growths consisting of fatty tissue (lipomas) that are found just below the surface of the skin. Pain may vary from mild discomfort when a growth is pressed or touched to severe pain that is disproportionate to the physical findings. Some affected individuals feel that “all fat hurts.” Pain can last for hours and may come and go or last continuously. In severe cases, pain may worsen with movement. The exact reason for pain associated with adiposis dolorosa is unknown, but may occur because the lipomas press on nearby nerves. Lipomas may be found in any part of the body, although they are rare in the head and neck. The trunk, upper arms and upper legs are most often affected.
Some individuals with Dercum’s may experience swelling of various areas of the body, especially the hands. Swelling occurs for no apparent reason and often disappears without treatment. Significant weight gain is a common occurrence for most individuals affected by adiposis dolorosa.
Additional symptoms may occur in individuals with adiposis dolorosa including fatigue, generalized weakness, a tendency to bruise easily, headaches, irritability, and stiffness after resting, especially in the morning. An association with bouts of depression, memory or concentration problems, and a susceptibility to infection has been noted in some cases.
Additional reports in the medical literature have linked adiposis dolorosa to a variety of conditions including arthritis, high blood pressure (hypertension), congestive heart failure, sleep disorders, dry eyes, and myxedema, a condition due to an underactive thyroid that is characterized by dry skin, swelling around the lips and nose, and mental deterioration.
Adiposis dolorosa diagnosis
A diagnosis of adiposis dolorosa can be made through a detailed patient history, a systematic physical examination and identification of the characteristic triad of features (multiple lipomas, painful plaques and obesity). Surgical removal and microscopic study (biopsy) of affect tissue confirms that these growths are lipomas. A biopsy may be helpful to distinguish a lipoma from an angiolipoma (another type of painful fat overgrowth).
Multiple lipomas may also be features of:
- Multiple lipomatosis (familial or sporadic)
- Fibromyalgia
- Panniculitis
- Obesity without painful plaques
- Cushing syndrome, which may also lead to abnormal fat distribution and ecchymoses
Other lesions that may mimic lipomas include:
- Epidermoid cysts (which usually have a central punctum)
- Hibernoma (a benign growth of brown fat)
- Lipofascial hernia (a hernia in the anal or perianal region)
- Lipoedema
Adiposis dolorosa treatment
Management of adiposis dolorosa is difficult. No treatments that are currently available have led to long-lasting, complete pain reduction 1. Treatment is directed toward the specific symptoms that are apparent in each individual and is primarily focus on easing the characteristic painful episodes. Surgical removal of particularly burdensome lesions and/or liposuction may be helpful for some people. However, lipomas have been known to reoccur and even increase in number at the same site or a nearby location. Weight reduction may help with joint pain in some individuals, but has proven to be difficult to achieve and generally doesn’t offer significant relief of symptoms 2.
There is currently no drug known to change the course of adiposis dolorosa. Available medications mainly focus on alleviating symptoms and may include:[2]
- prednisone or intravenous lidocaine for pain
- traditional pain medicines such nonsteroidal anti-inflammatory drugs (which are often ineffective), or acetaminophen combined with an opioid analgesic
- a cortisone/anesthetic injection for localized pain
- diuretics for swelling of the fingers
Various painkillers (analgesics) have been tried with limited effectiveness. Injections of corticosteroids have also been used to treat individuals with adiposis dolorosa. However, in one reported case in the medical literature, the use of high-doses of corticosteroids was linked as a possible cause of the disease. Intravenous administration of the pain reliever lidocaine may provide temporary relief from pain in some cases. Cortisone injections to treat localized pain may also provide relief.
Other treatments that have led to some pain reduction in some affected people include methotrexate and infliximab; interferon α-2b; calcium-channel modulators; and rapid cycling hypobaric pressure 1. Adjunctive therapies may include acupuncture, cognitive behavioral therapy, hypnosis, and biofeedback 3.
Surgical excision of fatty tissue deposits around joints may temporarily relieve symptoms although recurrences often develop. Liposuction has been used as a supportive treatment for some individuals with adiposis dolorosa and may provide an initial reduction in pain and improvement in quality of life. These effects may lessen over time.
Psychotherapy and consultation with pain management specialists may be helpful for enabling affected individuals to cope with long-term intense pain. Other treatment is symptomatic and supportive.
Adiposis dolorosa prognosis
The course is of Dercum disease (adiposis dolorosa) chronic and progressive.
References- Emma Hansson, Henry Svensson, and Håkan Brorson. Review of Dercum’s disease and proposal of diagnostic criteria, diagnostic methods, classification and management. Orphanet J Rare Dis. 2012; 7 https://ojrd.biomedcentral.com/articles/10.1186/1750-1172-7-23
- Dercum’s Disease. https://www.fatdisorders.org/dercums/
- Adiposis Dolorosa. https://emedicine.medscape.com/article/1082083-overview