What is Aldolase
Aldolase is an enzyme that helps convert glucose (sugar) into energy. Aldolase is found throughout your body but is primarily found in high levels in muscle tissue. Aldolase test can be done to measure the amount of aldolase in your blood. Aldolase levels in the blood rise when a person has muscle damage. The aldolase blood test may be ordered to diagnose and monitor certain conditions related to skeletal muscle. Aldolase test largely has been replaced by other muscle enzyme tests, especially CK (creatine kinase). However, a minority of people with muscle pain may have an elevated aldolase level even though their creatine kinase is normal. Therefore, aldolase test may sometimes be requested by rheumatologists in addition to creatine kinase.
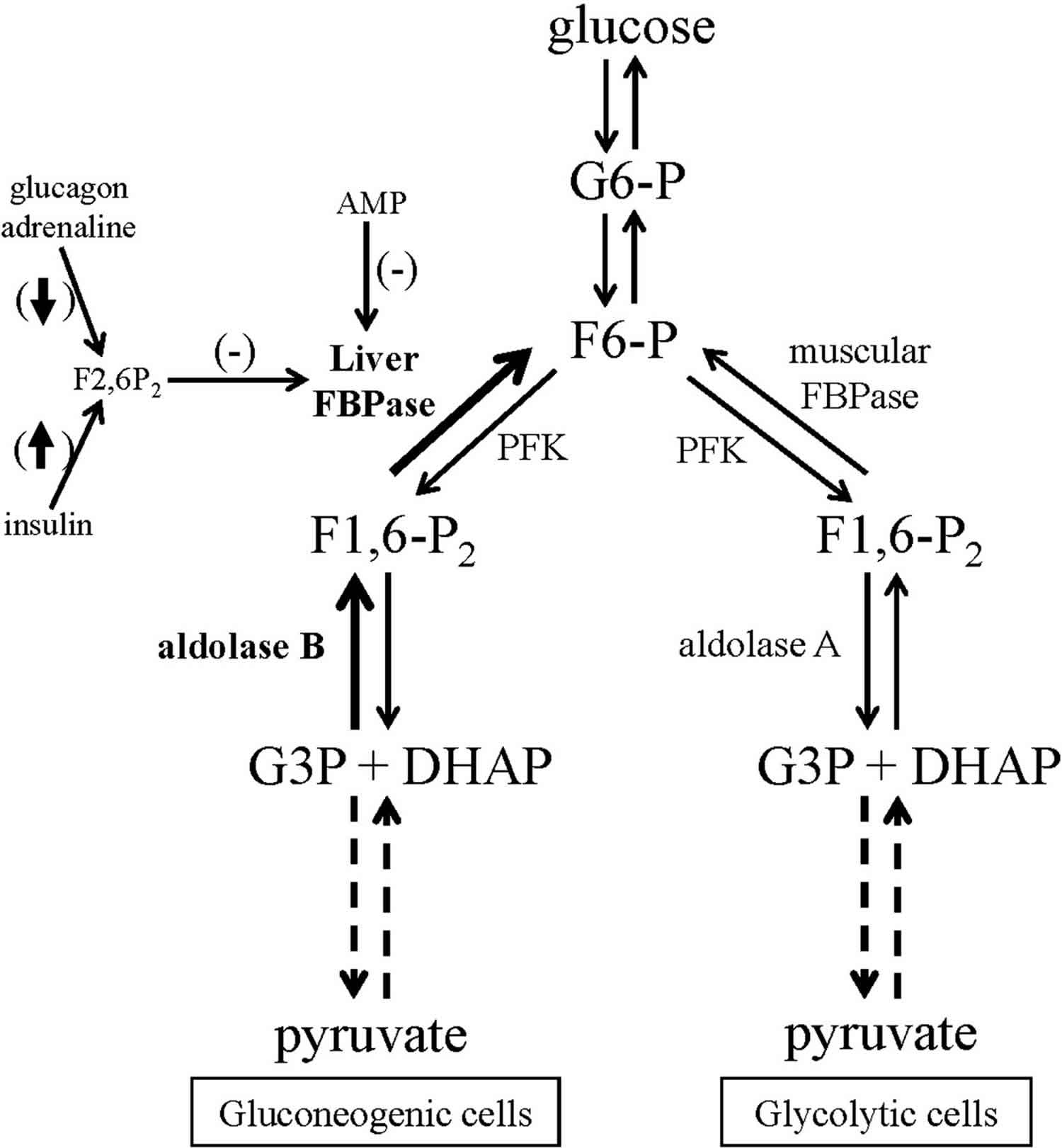
Aldolase specifically catalyzes the reversible reaction of converting fructose 1,6-bisphosphate into dihydroxyacetone phosphate (DHAP) and glyceraldehydes 3-phosphate.
The aldolase enzyme works on six reversible reactions in gluconeogensis and glycolysis. In gluconeogenesis, aldolase catalyzes the reduction of phosphoenolpyruvate to fructose 1,6-bisphosphate 1. In glycolysis, aldolase catalyzes fructose 1,6-bisphosphate to phosphoenolpyruvate through an oxidative reaction 2. Aldolase also reversibly cleaves fructose 1-phosphate to glyceraldehyde and dihydroxyacetone phosphate 3. Subgroup B works in both gluconeogenesis and glycolysis whereas subgroups A and C focus primary on glycolysis.
Aldolase A is primary contained in the muscle and erythrocytes. The liver, enterocytes and kidney contain aldolase B and the brain contains both aldolase A and C.
Figure 1. Aldolase
Aldolase test
Aldolase test can be done to measure the amount of aldolase in your blood to diagnose or monitor muscle or liver damage. However, aldolase test largely has been replaced by other muscle enzyme tests, especially CK (creatine kinase). However, a minority of people with muscle pain may have an elevated aldolase level even though their creatine kinase is normal. Therefore, aldolase test may sometimes be requested by rheumatologists in addition to creatine kinase.
Other tests that may be ordered to check for liver damage include:
- ALT (alanine aminotransferase) test
- AST (aspartate aminotransferase) test
Other tests that may be ordered to check for muscle cell damage include:
- CPK (creatine phosphokinase) test
- LDH (lactate dehydrogenase) test
You may be told not to eat or drink anything for 6 to 12 hours before the test. You may be also told to avoid vigorous exercise for 12 hours before the test. Your health care provider will tell you if it is necessary to stop taking any medicines that may interfere with this test. Tell your provider about all the medicines you are taking, both prescription and nonprescription.
Aldolase normal levels
Normal results range between 1.0 to 7.5 units per liter (0.02 to 0.13 microkat/L). There is a slight difference between men and women.
Reference ranges for aldolase +/- 2 units are as follows 1:
- Age 0-2 years: < 16 U/L (approximation)
- Age 3-16 years: < 8 U/L (approximation)
- Age 17 years and older: < 7.5 U/L (approximation)
Normal value ranges may vary slightly among different laboratories. Some labs use different measurements or test different samples. Talk to your provider about the meaning of your specific test results.
Aldolase abnormal levels
A higher than normal level may be due to:
- Damage to skeletal muscles
- Heart attack
- Liver, pancreatic, or prostate cancer
- Muscle disease such as dermatomyositis, muscular dystrophy, polymyositis
- Swelling and inflammation of the liver (hepatitis)
- Viral infection called mononucleosis
An aldolase blood test is used to help identify injury to organs such as muscle, liver, kidney, or heart. There are three subclasses of aldolase; A, B, and C. Aldolase A is expressed in muscle, erythrocytes, and the brain; aldolase B is expressed in the liver, kidneys, and enterocytes; aldolase C is expressed in the brain.
Aldolase levels are measured in units per liter and range from 1.0-16. There are slight variations in reference ranges between men and women based on height, weight, muscle mass and methods used in laboratories.
Elevated aldolase levels may be seen in conditions such as damage to the skeletal muscle (trauma), dermatomyositis, polymyositis, infectious mononucleosis, muscular dystrophy, myocardial infarction, nonspherocytic hemolytic anemia, viral / auto-immune hepatitis or hepatic cancer, colon cancer, pancreatic cancer, prostate cancer, and osteosarcoma 4.
Interpreting results requires understanding of the subclasses of aldolase. When damage occurs to aldolase containing cells, aldolase is released into the bloodstream at high levels. For certain diseases, monitoring aldolase can help direct treatment therapy. For example, aldolase A is contained in muscle tissue and used to monitor the course of muscular dystrophy.
Measurement of aldolase A can also help differentiate between muscle versus neurological myopathy. If aldolase A is elevated, the primary cause of myopathy may be related to an inflammatory state of the muscle. If aldolase A is not elevated, the pathology may be related to a secondary cause. An example is a patient with a history of multiple sclerosis who presents with muscle weakness and has normal aldolase A levels.
Aldolase B levels are elevated in liver disease or heart disease (myocardial infarction). This particular marker is not widely used because other blood tests are more specific for liver and heart-related diseases (LFT’s and Cardiac enzymes).
Aldolase deficiency
Hereditary fructose intolerance also called aldolase B deficiency or fructose aldolase B-deficiency, is a metabolic disease caused by the absence of aldolase B that affects a person’s ability to digest the sugar fructose 5. Fructose is a simple sugar found primarily in fruits. In people with hereditary fructose intolerance, ingestion of fructose (fruit sugar) and sucrose (cane or beet sugar, table sugar) causes severe hypoglycemia (low blood sugar) and the build up of dangerous substances in the liver. After ingesting fructose, individuals with hereditary fructose intolerance may experience nausea, bloating, abdominal pain, diarrhea, vomiting, and low blood sugar (hypoglycemia). Affected infants may fail to grow and gain weight at the expected rate (failure to thrive).
Repeated ingestion of fructose-containing foods can lead to liver and kidney damage. The liver damage can result in a yellowing of the skin and whites of the eyes (jaundice), an enlarged liver (hepatomegaly), and chronic liver disease (cirrhosis). Continued exposure to fructose may result in seizures, coma, and ultimately death from liver and kidney failure. Due to the severity of symptoms experienced when fructose is ingested, most people with hereditary fructose intolerance develop a dislike for fruits, juices, and other foods containing fructose.
Hereditary fructose intolerance may be relatively mild or a very severe disease 6. Hereditary fructose intolerance is caused by mutations in the ALDOB gene. Hereditary fructose intolerance is inherited in an autosomal recessive pattern 7. Treatment involves eliminating fructose and sucrose from the diet. In the severe form, eliminating these sugars from the diet may not prevent progressive liver disease.
The incidence of hereditary fructose intolerance is estimated to be 1 in 20,000 to 30,000 individuals each year worldwide.
Hereditary fructose intolerance should not be confused with a condition called fructose malabsorption. In people with fructose malabsorption, the cells of the intestine cannot absorb fructose normally, leading to bloating, diarrhea or constipation, flatulence, and stomach pain. Fructose malabsorption is thought to affect approximately 40 percent of individuals in the Western hemisphere; its cause is unknown.
Hereditary fructose intolerance causes
Mutations in the ALDOB gene cause hereditary fructose intolerance. The responsible gene has been mapped to the long arm (q) of chromosome 9 at gene map locus 9q22.3. The ALDOB gene provides instructions for making the aldolase B enzyme. Aldolase B enzyme is found primarily in the liver and is involved in the breakdown (metabolism) of fructose so this sugar can be used as energy. Aldolase B is responsible for the second step in the metabolism of fructose, which breaks down the molecule fructose-1-phosphate into other molecules called glyceraldehyde and dihydroxyacetone phosphate.
ALDOB gene mutations reduce the function of the enzyme, impairing its ability to metabolize fructose. A lack of functional aldolase B results in an accumulation of fructose-1-phosphate in liver cells. This buildup is toxic, resulting in the death of liver cells over time. Additionally, the breakdown products of fructose-1-phosphase are needed in the body to produce energy and to maintain blood sugar levels. The combination of decreased cellular energy, low blood sugar, and liver cell death leads to the features of hereditary fructose intolerance.
Hereditary fructose intolerance inheritance pattern
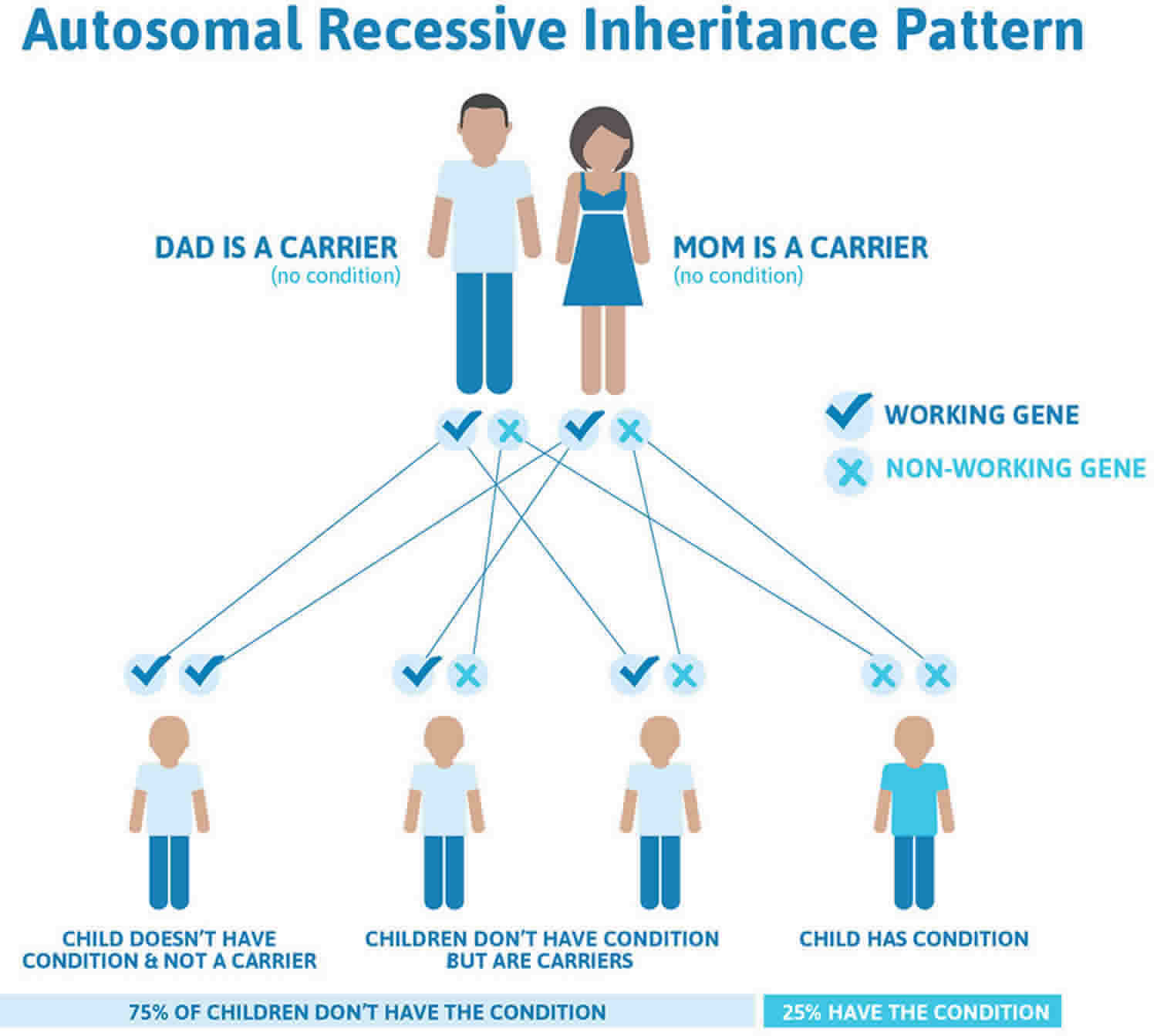
This condition is inherited in an autosomal recessive pattern, which means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition.
It is rare to see any history of autosomal recessive conditions within a family because if someone is a carrier for one of these conditions, they would have to have a child with someone who is also a carrier for the same condition. Autosomal recessive conditions are individually pretty rare, so the chance that you and your partner are carriers for the same recessive genetic condition are likely low. Even if both partners are a carrier for the same condition, there is only a 25% chance that they will both pass down the non-working copy of the gene to the baby, thus causing a genetic condition. This chance is the same with each pregnancy, no matter how many children they have with or without the condition.
- If both partners are carriers of the same abnormal gene, they may pass on either their normal gene or their abnormal gene to their child. This occurs randomly.
- Each child of parents who both carry the same abnormal gene therefore has a 25% (1 in 4) chance of inheriting a abnormal gene from both parents and being affected by the condition.
- This also means that there is a 75% ( 3 in 4) chance that a child will not be affected by the condition. This chance remains the same in every pregnancy and is the same for boys or girls.
- There is also a 50% (2 in 4) chance that the child will inherit just one copy of the abnormal gene from a parent. If this happens, then they will be healthy carriers like their parents.
- Lastly, there is a 25% (1 in 4) chance that the child will inherit both normal copies of the gene. In this case the child will not have the condition, and will not be a carrier.
These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
Figure 1 illustrates autosomal recessive inheritance. The example below shows what happens when both dad and mum is a carrier of the abnormal gene, there is only a 25% chance that they will both pass down the abnormal gene to the baby, thus causing a genetic condition.
Figure 2. Hereditary fructose intolerance autosomal recessive inheritance pattern
Hereditary fructose intolerance prevention
Couples with a family history of fructose intolerance who wish to have a baby may consider genetic counseling.
Most of the damaging effects of the disease can be prevented by decreasing fructose and sucrose intake.
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Hereditary fructose intolerance symptoms
Symptoms can be seen after a baby starts eating food or formula.
The early symptoms of fructose intolerance are similar to those of galactosemia (inability to use the sugar galactose). Later symptoms relate more to liver disease.
Hereditary fructose intolerance symptoms may include:
- Convulsions
- Excessive sleepiness
- Irritability
- Yellow skin or whites of the eyes (jaundice) – increased or prolonged neonatal jaundice
- Poor feeding as a baby
- Problems after eating fruits and other foods that contain fructose or sucrose
- Vomiting
- Intolerance for fruits
- Avoidance of fruits and fructose/sucrose-containing foods
- Doing well after eating foods without fructose/sucrose
The early symptoms of fructose intolerance may resemble those of galactosemia: irritability, jaundice, vomiting, convulsions and an enlarged liver and spleen. Later problems relate more to liver disease.
Hereditary fructose intolerance possible complications
These complications may occur:
- Avoidance of fructose-containing foods due to their effects
- Bleeding
- Gout
- Illness from eating foods containing fructose or sucrose
- Liver failure
- Low blood sugar (hypoglycemia)
- Seizures
- Death
Hereditary fructose intolerance diagnosis
Making a diagnosis for a genetic or rare disease can often be challenging. Healthcare professionals typically look at a person’s medical history, symptoms, physical exam, and laboratory test results in order to make a diagnosis. If you have questions about getting a diagnosis, you should contact a healthcare professional.
A diagnosis of hereditary fructose intolerance can be definitively confirmed by either of two tests: an enzyme assay, requiring a liver biopsy, to determine the level of aldolase activity or a fructose tolerance test in which the patient’s response to intravenous fructose feeding is carefully monitored. It should be carefully noted, however, that each of these tests carries with it a substantial risk, especially to a newborn child. A non-invasive DNA test is increasingly being recommended instead.
Physical examination may show:
- Enlarged liver and spleen
- Jaundice
Tests that confirm the diagnosis include:
- Blood clotting tests
- Blood sugar test
- Enzyme studies
- Genetic testing
- Kidney function tests
- Liver function tests
- Liver biopsy
- Uric acid blood test
- Urinalysis
Blood sugar will be low, especially after receiving fructose or sucrose. Uric acid levels will be high.
Hereditary fructose intolerance treatment
The standard therapy is a fructose-free diet. As long as patients with hereditary fructose intolerance do not ingest fructose, they can lead normal lives. However, it is important that this disorder be diagnosed early, and the special diet adopted, to prevent permanent physical damage.
Complications may be treated. For example, some people can take a medicine to lower the level of uric acid in their blood and decrease their risk for gout.
Hereditary fructose intolerance prognosis
Hereditary fructose intolerance may be mild or severe.
Avoiding fructose and sucrose helps most children with this condition. The prognosis is good in most cases.
A few children with a severe form of the disease will develop severe liver disease. Even removing fructose and sucrose from the diet may not prevent severe liver disease in these children.
How well a person does depends on:
- How soon the diagnosis is made
- How soon fructose and sucrose can be removed from the diet
- How well the enzyme works in the body
- Aldolase. https://emedicine.medscape.com/article/2087158-overview
- Szekrenyi A, Soler A, Garrabou X, Guérard-Hélaine C, Parella T, Joglar J, et al. Engineering the donor selectivity of d-fructose-6-phosphate aldolase for biocatalytic asymmetric cross-aldol additions of glycolaldehyde. Chemistry. 2014 Sep 22. 20(39):12572-83.
- Bouteldja N, Timson DJ. The biochemical basis of hereditary fructose intolerance. J Inherit Metab Dis. 2010 Apr. 33(2):105-12
- Long F, Cai X, Luo W, Chen L, Li K. Role of aldolase A in osteosarcoma progression and metastasis: In vitro and in vivo evidence. Oncol Rep. 2014 Sep 10
- https://rarediseases.info.nih.gov/diseases/6622/hereditary-fructose-intolerance
- Hereditary fructose intolerance. https://medlineplus.gov/ency/article/000359.htm
- Hereditary fructose intolerance. https://ghr.nlm.nih.gov/condition/hereditary-fructose-intolerance