What is alpha 1 antitrypsin deficiency
Alpha-1 antitrypsin deficiency also called AAT deficiency, is a inherited condition in which your liver does not make enough of alpha-1 antitrypsin, a protein that protects your lungs and liver from damage. Alpha-1 antitrypsin deficiency can lead to COPD (chronic obstructive pulmonary disease) like emphysema especially if you smoke and liver disease (cirrhosis). The signs and symptoms of alpha-1 antitrypsin deficiency and the age at which they appear vary among individuals. Some people who have severe alpha-1 antitrypsin deficiency develop emphysema often when they’re only in their forties or fifties. Emphysema is a serious lung disease in which damage to the airways makes it hard to breathe. A small number of people who have alpha-1 antitrypsin deficiency develop cirrhosis and other serious liver diseases. Cirrhosis is a disease in which the liver becomes scarred. The scarring prevents your liver from working well. In people who have alpha-1 antitrypsin deficiency, cirrhosis and other liver diseases usually occur in infancy and early childhood.
A very small number of people who have alpha-1 antitrypsin deficiency have a rare skin disease called necrotizing panniculitis. This disease can cause painful lumps under or on the surface of the skin.
Normally, the alpha-1 antitrypsin protein travels through the bloodstream. Alpha-1 antitrypsin helps protect your body’s organs from the harmful effects of other proteins. The lungs are one of the main organs that the alpha-1 antitrypsin protein protects.
Alpha-1 antitrypsin deficiency occurs if the alpha-1 antitrypsin proteins made in the liver aren’t the right shape. They get stuck inside liver cells and can’t get into the bloodstream.
As a result, not enough alpha-1 antitrypsin proteins travel to the lungs to protect them. This increases the risk of lung disease. Also, because too many alpha-1 antitrypsin proteins are stuck in the liver, liver disease can develop.
Severe alpha-1 antitrypsin deficiency occurs if blood levels of the alpha-1 antitrypsin protein fall below the lowest amount needed to protect the lungs.
Alpha-1 antitrypsin deficiency occurs worldwide, but its prevalence varies by population. Doctors don’t know how many people have alpha-1 antitrypsin deficiency. Many people who have alpha-1 antitrypsin deficiency may not know they have it. Estimates of how many people have alpha-1 antitrypsin deficiency range from about 1 in every 1,500 people to about 1 in every 5,000 individuals with European ancestry. Alpha-1 antitrypsin deficiency is uncommon in people of Asian descent. Many individuals with alpha-1 antitrypsin deficiency are likely undiagnosed, particularly people with a lung condition called chronic obstructive pulmonary disease (COPD). COPD can be caused by alpha-1 antitrypsin deficiency; however, the alpha-1 antitrypsin deficiency is often never diagnosed. Some people with alpha-1 antitrypsin deficiency are misdiagnosed with asthma.
Alpha 1 antitrypsin deficiency has no cure, but treatments are available. Treatments often are based on the type of disease you develop.
Is alpha 1 antitrypsin deficiency fatal?
No. Although alpha 1 antitrypsin deficiency has no cure, but treatments are available. Treatments often are based on the type of disease you develop.
People who have alpha 1 antitrypsin deficiency may not have serious complications, and they may live close to a normal lifespan.
People who have alpha-1 antitrypsin deficiency don’t always develop serious lung or liver diseases. This means that you can have alpha 1 antitrypsin deficiency and not even know it.
If you already know you have alpha 1 antitrypsin deficiency, you probably also have a related lung or liver disease. Ongoing medical care and lifestyle changes can help you manage your health.
Some risk factors make it more likely that you’ll develop lung disease if you have alpha 1 antitrypsin deficiency. Environmental factors, such as exposure to tobacco smoke, chemicals, and dust, likely impact the severity of alpha-1 antitrypsin deficiency.
Smoking is the leading risk factor for serious lung disease if you have alpha 1 antitrypsin deficiency. Your risk for lung disease also may go up if you’re exposed to dust, fumes, or other toxic substances.
Among people with alpha 1 antitrypsin deficiency who have a related lung or liver disease, about 3 percent die each year.
Smoking is the leading risk factor for life-threatening lung disease if you have alpha 1 antitrypsin deficiency. Smoking or exposure to tobacco smoke increases your risk of earlier lung-related symptoms and lung damage. If you have severe alpha 1 antitrypsin deficiency, smoking can shorten your life by as much as 20 years.
Alpha 1 antitrypsin deficiency causes
Alpha-1 antitrypsin deficiency is an inherited condition. “Inherited” means it’s passed from parents to children through genes.
The way each person’s body makes Alpha-1 antitrypsin is determined by genes. Everyone has two copies of the alpha-1 gene, one inherited from each parent.
Children who have alpha 1 antitrypsin deficiency inherit two faulty alpha 1 antitrypsin genes, one from each parent. These genes tell cells in the body how to make alpha 1 antitrypsin proteins.
In alpha 1 antitrypsin deficiency, the alpha 1 antitrypsin proteins made in the liver aren’t the right shape. Thus, they get stuck in the liver cells. The proteins can’t get to the organs in the body that they protect, such as the lungs. Without the alpha 1 antitrypsin proteins protecting the organs, diseases can develop.
The most common faulty gene that can cause alpha 1 antitrypsin deficiency is called SERPINA1 gene. If you inherit two SERPINA1 genes (one from each parent), you’ll have alpha 1 antitrypsin deficiency.
The SERPINA1 gene provides instructions for making alpha-1 antitrypsin protein, which is a type of serine protease inhibitor (serpin). Serpins help control several types of chemical reactions by blocking (inhibiting) the activity of certain enzymes. Alpha-1 antitrypsin prevents the digestive enzyme trypsin from breaking down proteins until trypsin reaches the intestines. Alpha-1 antitrypsin also inhibits other enzymes, including a powerful enzyme called neutrophil elastase that is released from white blood cells to fight infection.
Mutations in the SERPINA1 gene can lead to a shortage (deficiency) of alpha-1 antitrypsin or an abnormal form of the protein that cannot control neutrophil elastase. Without enough functional alpha-1 antitrypsin, neutrophil elastase destroys alveoli and causes lung disease. Abnormal alpha-1 antitrypsin can also accumulate in the liver and damage this organ.
If you inherit a SERPINA1 gene from one parent and a normal alpha 1 antitrypsin gene from the other parent, you won’t have alpha 1 antitrypsin deficiency. However, you might pass the SERPINA1 gene to your children.
Even if you inherit two faulty alpha 1 antitrypsin SERPINA1 genes, you may not have any related complications. You may never even realize that you have alpha 1 antitrypsin deficiency.
Alpha 1 antitrypsin deficiency inheritance
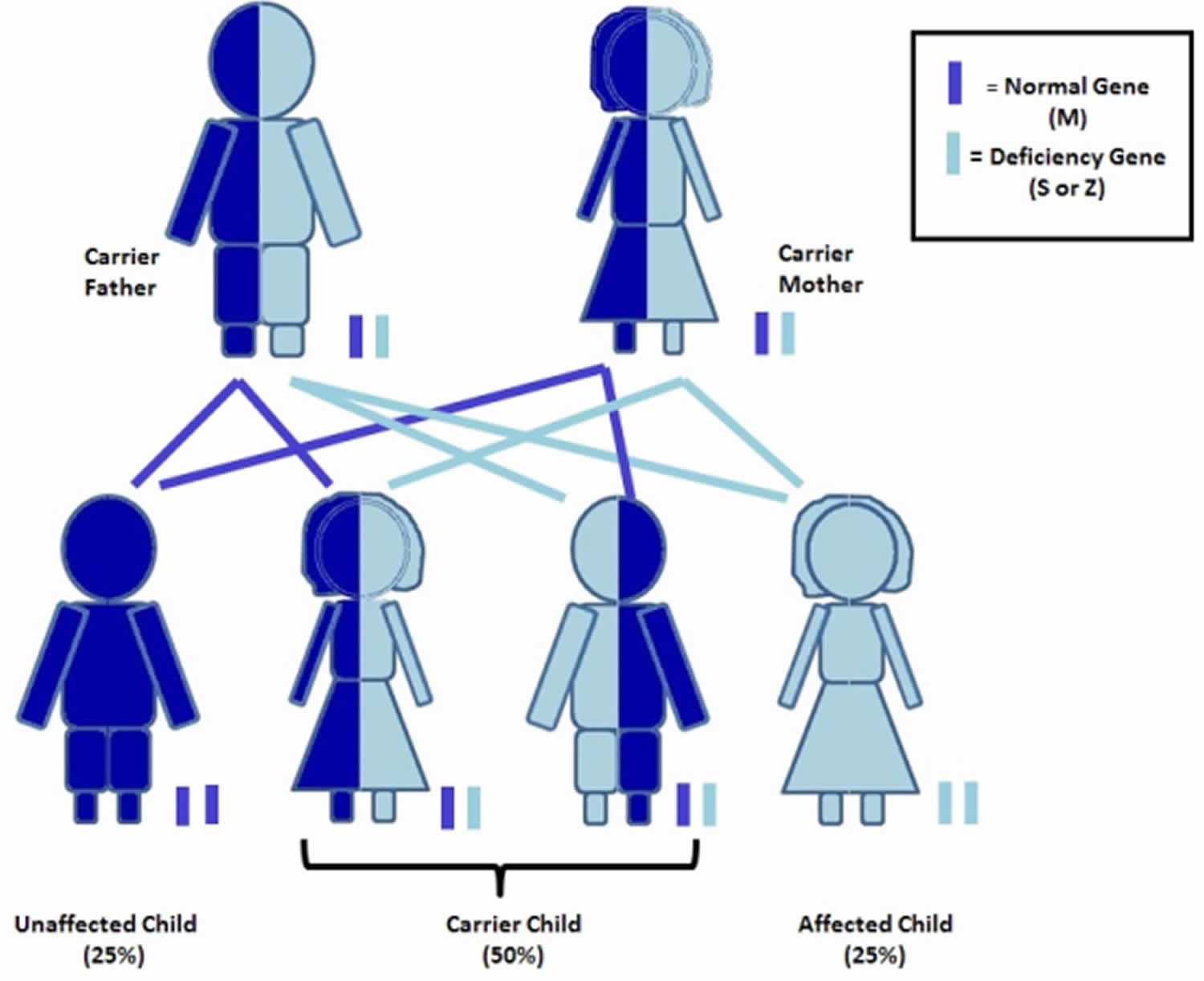
Alpha 1 antitrypsin deficiency is inherited in an autosomal codominant pattern 1. Codominance means that two different versions of the gene may be active (expressed), and both versions contribute to the genetic trait.
The most common version (allele) of the SERPINA1 gene, called M (normal gene for alpha-1), produces normal levels of alpha-1 antitrypsin. Most people in the general population have two copies of the M allele (MM) in each cell (normal gene combination). Other versions of the SERPINA1 gene lead to reduced levels of alpha-1 antitrypsin. For example, the S allele produces moderately low levels of this protein, and the Z allele produces very little alpha-1 antitrypsin. Individuals with two copies of the Z allele (ZZ) in each cell are likely to have alpha-1 antitrypsin deficiency. Those with the SZ combination have an increased risk of developing lung diseases (such as emphysema), particularly if they smoke. People with two Z genes (ZZ) have high lifetime risks for lung and liver disease. There are other mutations that can cause Alpha-1, too. For example, the S, F, and I mutations are different abnormal versions of the gene.
Worldwide, it is estimated that 161 million people have one copy of the S or Z allele and one copy of the M allele in each cell (MS or MZ). Individuals with an MS (or SS) combination usually produce enough alpha-1 antitrypsin to protect the lungs. People with MZ alleles, however, have a slightly increased risk of impaired lung or liver function.
Figure 1. Alpha 1 antitrypsin deficiency autosomal codominant inheritance pattern
What does it mean to be a alpha 1 antitrypsin deficiency carrier?
Alpha-1 carriers are people who have one normal Alpha-1 gene (called M) and one abnormal Alpha-1 gene (S, Z, F, I, other). Carrier genotypes include MS, MZ, MF, MI, M-Other.
Carriers may be termed “mildly deficient” because this combination of genes leads to a lower Alpha-1 level than expected for most people with two normal genes (MM) but higher than that of someone with severe deficiency caused by two abnormal genes (ZZ, SZ).
Most carriers do not develop Alpha-1 related symptoms; however, recent research has shown that MZ carriers who smoke are at high risk for COPD. MZ carriers also have a small increased risk for liver disease. Carriers should avoid smoking and live a healthy lifestyle.
There are over 20 million Alpha-1 carriers in the US. Being an Alpha-1 carrier is more common than many people know. About 2-3% of North Americans are carriers of the Z mutation (MZ) and about 5% carry the S (MS). Carriers of other mutations such as the F, I, and rare/null mutations are less common and exact rates are not known. A person’s individual chance to be a carrier depends on their ethnic background and family history.
The good news is that most carriers never have health problems due to their Alpha-1 mutation. However, research continues to better define select groups of people with higher risk for COPD. It is possible that certain carrier sub-groups with higher risk will be defined in the future. Any person experiencing symptoms or a change in their health should see a healthcare provider for personal evaluation.
Carriers have a 50% chance of passing on their abnormal Alpha-1 gene to each child, so, any child of a carrier has a 50% chance to be a carrier, too. If two carriers have children together, there is a risk to have a child with severe Alpha-1 antitrypsin deficiency. This happens when the child inherits an abnormal gene from both the mother and the father.
What is a Pi type?
Pi stands for Protease Inhibitor. Alpha-1 antitrypsin is a type of protein called a protease inhibitor, so Pi type is the type(s) of Alpha-1 protein produced by your body (in your liver).
The normal Pi type is M. Normal M variants include M1, M2 and M3. Abnormal Pi types included Z, S, F, I and others.
In most cases your Pi type and your genotype are the same since the genes instruct the alpha-1 antitrypsin your body makes (e.g. genotype MZ will have Pi MZ). Exceptions include people on augmentation therapy and who have had a liver transplant. In these cases a normal Pi M is detected due to the treatment and may not correlate with the person’s genes.
Contact the genetic counselor if you have questions about your Pi type.
What are alleles?
Alleles are different versions of the same gene. The normal Alpha-1 allele is called “M.” Abnormal allelles, also called mutations, occur due to changes in the DNA of the Alpha-1 gene that affect how Alpha-1 is made. Mutations result in an abnormal quantity and/or abnormal function of alpha-1 antitrypsin.
The most common deficiency alleles are “S” and “Z.” There are also more than 100 other rarer deficiency alleles (such as F and I and null alleles). The M allele (M1, M2, M3) produces normal Alpha-1 protein (normal quantity and normal function). Different deficiency alleles have different effects on Alpha-1 level and function, thus different allele combinations (genotypes) lead to different disease risks.
- M – The M allele is normal (normal alpha-1 antitrypsin quantity and function).
- F – The F mutation produces a dysfunctional alpha-1 protein product.
- Z – The Z mutation produces an abnormal protein product that gets trapped in the liver and reduces the quantity of alpha-1 antitrypsin (AAT) in the blood.
- S – The S mutation causes a moderate reduction in the quantity of alpha-1 antitrypsin (AAT) in the blood.
- I – The I mutation results in a reduced quantity of Alpha-1 protein in the blood.
- Null – Null mutations make no alpha-1 antitrypsin (AAT); no AAT is produced in the liver or found in the blood as a result of null mutations. There are many different null mutations.
- Rare – Rare mutations may make altered forms of alpha-1 antitrypsin (AAT). There are many different rare mutations. Most rare mutations reduce the quantity of alpha-1 antitrypsin (AAT) in the blood. A few rare mutations cause alpha-1 trapping in the liver or altered alpha-1 function. Contact the genetic counselor for information about any specific rare mutation.
What are genotypes?
A genotype is the combination of Alpha-1 alleles you have. The normal genotype is MM (two copies of the normal M allele). Carrier genotypes include MS, MZ, MF, MI, Mnull and other genotypes where one allele is a normal M and the other is abnormal.
Deficiency genotypes include ZZ, SZ, FZ, IZ, Znull and some others where a person has two abnormal genes.
There are many more rare Alpha-1 genotypes. Contact the genetic counselor if you have questions about finding out your genotype or what your genotype means.
What are genes?
Genes are the genetic “blueprint” for how our bodies develop and function. Genes are units of DNA. People have about 25,000 genes. They are found inside the nucleus of our cells. Genes are passed from parent to child. People get one copy of each gene from their mother and one from their father (sex chromosome genes excluded).
Everyone has changes in their genes that make them unique. Changes in genes can be neutral variants or cause problems. Changes that cause disease or raise risks are called mutations. Mutations in one specific gene cause Alpha-1 deficiency. The gene for Alpha-1 is called SERPINA1.
Alpha-1 antitrypsin deficiency prevention
You can’t prevent alpha-1 antitrypsin deficiency because the condition is inherited (passed from parents to children through genes).
If you inherit two faulty SERPINA1 genes, you’ll have alpha 1 antitrypsin deficiency. Even so, you may never develop one of the diseases related to the condition.
You can take steps to prevent or delay lung diseases related to alpha 1 antitrypsin deficiency. One important step is to quit smoking. If you don’t smoke, don’t start.
Talk with your doctor about programs and products that can help you quit smoking. If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking.
Also, try to avoid secondhand smoke and places with dust, fumes, or other toxic substances that you may inhale.
Check your living and working spaces for things that may irritate your lungs. Examples include flower and tree pollen, ash, allergens, air pollution, wood burning stoves, paint fumes, and fumes from cleaning products and other household items.
Alpha 1 antitrypsin deficiency test
According to the 2016 Guidelines for The Diagnosis and Management of Alpha-1 Antitrypsin Deficiency in the Adult 2:
- All individuals with COPD regardless of age or ethnicity should be tested for alpha 1 antitrypsin deficiency.
- All individuals with unexplained chronic liver disease should be tested for alpha 1 antitrypsin deficiency.
- All individuals with necrotizing panniculitis, granulomatosis with polyangiitis, or unexplained bronchiectasis should be tested for alpha 1 antitrypsin deficiency.
- Parents, siblings, and children, as well as extended family of individuals identified with an abnormal gene for alpha 1 antitrypsin, should be provided genetic counseling and offered testing for alpha 1 antitrypsin deficiency (see guideline document for special considerations about testing minors) 2.
Call the genetic counselor if you have questions or concerns about whether to have alpha-1 testing. Decisions can be made in the context of your personal and family history, as well as your unique situation and goals.
There are several options for getting Alpha-1 Antitrypsin Deficiency tested
- The Alpha-1 Coded Testing (ACT) Study is a free and confidential testing program supported by the Alpha-1 Foundation. Testing through this program is voluntary and nobody gets your results except you. You will receive your results in the mail. The genetic counselor is available to help you understand your results. To receive an ACT kit, complete the informed consent and research questionnaire at (https://alphaoneregistry.org/). Adults (18 and over) are required to complete their own forms. Parents and legal guardians may complete the forms for their minor children and those in legal guardianship. Results are delivered to you by mail approximately 4 weeks after you submit your blood sample for testing.
- You may ask your healthcare provider to order testing for Alpha-1. Many labs offer Alpha-1 testing. Several Alpha-1 specialty labs (GeneAidyx, Biocerna LLC and AlphaCenter) provide free testing. Ask your healthcare provider if you have questions about which test is being ordered and details of the test. If your healthcare provider orders your test, the results will go to that healthcare provider to be shared with you.
What does alpha 1 antitrypsin deficiency testing involve?
Alpha-1 antitrypsin deficiency testing requires a blood sample. This may be dried blood spots which are obtained by a finger stick or a blood draw.
Only a blood test can diagnose or rule out Alpha-1.
What does the lab do to test for alpha-1 antitrypsin deficiency?
It depends on the lab. There are several ways to test for alpha-1 antitrypsin deficiency. Some labs use more than one to ensure accuracy.
An immunoassay, also called a ‘level’, measures the quantity of alpha-1 antitrypsin in your blood. This is done on one of two scales, either uM or mg/dL, and is reported as a number. This is helpful to see if you have a low level that indicates deficiency.
Phenotyping looks at the Alpha-1 protein(s) in your blood using a technique called isoelectric focusing. The results are two letters called a Pi type, which includes one or two letters (e.g. Pi M, Pi Z, Pi MZ).*
Genotyping spot checks the Alpha-1 gene for specific mutations. The results are two letters called a genotype* or describe whether 0, 1 or 2 mutations were found.
Genotyping and phenotyping give you the same result in most cases.
Gene sequencing spells out the DNA sequence of the Alpha-1 gene. This is useful for clarification of less common Alpha-1 gene mutations.
Alpha 1 antitrypsin deficiency symptoms
The first lung-related symptoms of alpha-1 antitrypsin deficiency may include shortness of breath, less ability to be physically active, and wheezing. These signs and symptoms most often begin between the ages of 20 and 40.
Symptoms may include any of the following:
- Shortness of breath with and without exertion, and other symptoms of COPD
- Symptoms of liver failure
- Loss of weight without trying
- Wheezing
Other signs and symptoms may include repeated lung infections, tiredness, a rapid heartbeat upon standing, vision problems, and weight loss.
Some people who have severe alpha 1 antitrypsin deficiency develop emphysema often when they’re only in their forties or fifties. Signs and symptoms of emphysema include problems breathing, wheezing, and a chronic (ongoing) cough.
At first, many people who have alpha 1 antitrypsin deficiency are diagnosed with asthma. This is because wheezing also is a symptom of asthma. Also, people who have alpha 1 antitrypsin deficiency respond well to asthma medicines.
Your health care provider may suspect you of having alpha 1 antitrypsin deficiency if you develop:
- COPD before age 45
- COPD but you have never smoked or been exposed to toxins
- COPD and you have a family history of the condition
- Cirrhosis and no other cause can be found
- Cirrhosis and you have a family history of liver disease
Alpha 1 antitrypsin deficiency possible complications
Complications of alpha 1 antitrypsin deficiency include:
- Bronchiectasis (damage of the large airways)
- Chronic obstructive pulmonary disease (COPD)
- Liver failure or cancer
Alpha 1 antitrypsin deficiency diagnosis
Alpha-1 antitrypsin deficiency usually is diagnosed after you develop a lung or liver disease that’s related to the condition.
Your doctor may suspect alpha 1 antitrypsin deficiency if you have signs or symptoms of a serious lung condition, especially emphysema, without any obvious cause. He or she also may suspect alpha 1 antitrypsin deficiency if you develop emphysema when you’re 45 years old or younger.
Specialists involved
Many doctors may be involved in the diagnosis of alpha 1 antitrypsin deficiency. These include primary care doctors, pulmonologists (lung specialists), and hepatologists (liver specialists).
To diagnose alpha 1 antitrypsin deficiency, your doctor will:
- Ask about possible risk factors. Risk factors include smoking and exposure to dust, fumes, and other toxic substances.
- Ask about your medical history. A common sign of alpha 1 antitrypsin deficiency is if you have a lung or liver disease without any obvious causes or risk factors. Another sign is if you have emphysema at an unusually early age (45 years or younger).
- Ask about your family’s medical history. If you have bloodline relatives who have alpha 1 antitrypsin deficiency, you’re more likely to have the condition.
Diagnostic tests
Your doctor may recommend tests to confirm a diagnosis of alpha 1 antitrypsin deficiency. He or she also may recommend tests to check for lung- or liver-related conditions.
A genetic test is the most certain way to check for alpha 1 antitrypsin deficiency. This test will show whether you have faulty alpha 1 antitrypsin genes.
A blood test also may be used. This test checks the level of alpha 1 antitrypsin protein in your blood. If the level is a lot lower than normal, it’s likely that you have alpha 1 antitrypsin deficiency.
Lung-related tests
If you have a lung disease related to alpha 1 antitrypsin deficiency, your doctor may recommend lung function tests and high-resolution computed tomography scanning, also called CT scanning.
Lung function tests measure how much air you can breathe in and out, how fast you can breathe air out, and how well your lungs deliver oxygen to your blood. These tests may show how severe your lung disease is and how well treatment is working.
High-resolution CT scanning uses x rays to create detailed pictures of parts of the body. A CT scan can show whether you have emphysema or another lung disease and how severe it is.
Alpha 1 antitrypsin deficiency treatment
Alpha-1 antitrypsin deficiency has no cure, but its related lung diseases have many treatments. Most of these treatments are the same as the ones used for a lung disease called COPD (chronic obstructive pulmonary disease).
If you have symptoms related to alpha 1 antitrypsin deficiency, your doctor may recommend:
- Medicines called inhaled bronchodilators and inhaled steroids. These medicines help open your airways and make breathing easier. They also are used to treat asthma and COPD.
- Flu and pneumococcal vaccines to protect you from illnesses that could make your condition worse. Prompt treatment of lung infections also can help protect your lungs.
- Pulmonary rehabilitation (rehab). Rehab involves treatment by a team of experts at a special clinic. In rehab, you’ll learn how to manage your condition and function at your best.
- Extra oxygen, if needed.
- A lung transplant. A lung transplant may be an option if you have severe breathing problems. If you have a good chance of surviving the transplant surgery, you may be a candidate for it.
Augmentation therapy is a treatment used only for people who have alpha 1 antitrypsin-related lung diseases. This therapy involves getting infusions of the alpha 1 antitrypsin protein. The infusions raise the level of the protein in your blood and lungs.
Not enough research has been done to show how well this therapy works. However, some research suggests that this therapy may slow the development of alpha 1 antitrypsin deficiency in people who don’t have severe disease.
According to the 2016 Guidelines for The Diagnosis and Management of Alpha-1 Antitrypsin Deficiency in the Adult 2:
Intravenous augmentation therapy in those with alpha 1 antitrypsin deficiency is recommended for 2:
- Individuals with an FEV1 less than or equal to 65% predicted.
- For those with lung disease related to alpha 1 antitrypsin deficiency and an FEV1 greater than 65%, we recommend discussion with each individual regarding the potential benefits of reducing lung function decline with consideration of the cost of therapy and lack of evidence for such benefit.
- Individuals with necrotizing panniculitis.
Intravenous augmentation therapy is NOT recommended for 2:
- Individuals with the MZ genotype of alpha 1 antitrypsin deficiency.
- Individuals with lung disease due to alpha 1 antitrypsin deficiency who continue to smoke.
- Individuals with alpha 1 antitrypsin deficiency and emphysema or bronchiectasis who do not have airflow obstruction.
- The treatment of liver disease due to alpha 1 antitrypsin deficiency.
- Individuals who have undergone liver transplantation.
Additional recommendations regarding dosing of intravenous augmentation therapy 2:
- Weekly doses higher than the current FDA-approved dose are not recommended.
- Monitoring of trough alpha 1 antitrypsin blood levels to evaluate the adequacy of alpha 1 antitrypsin augmentation dosing is not recommended.
People who have alpha 1 antitrypsin deficiency and develop related liver or skin diseases will be referred to doctors who treat those diseases.
Future Treatments
Researchers are working on possible treatments that will target the faulty alpha 1 antitrypsin genes and replace them with healthy genes. These treatments are in the early stages of development.
Researchers also are studying therapies that will help misshapen alpha 1 antitrypsin proteins move from the liver into the bloodstream. They’re also studying a type of augmentation therapy in which the alpha 1 antitrypsin protein is inhaled instead of injected into a vein.
If you’re interested in new treatments, ask your doctor about ongoing clinical trials for alpha 1 antitrypsin deficiency.
Alpha 1 antitrypsin deficiency diet
A healthy diet is an important part of a healthy lifestyle. A healthy diet includes a variety of vegetables and fruits. It also includes whole grains, fat-free or low-fat dairy products, and protein foods, such as lean meats, poultry without skin, seafood, processed soy products, nuts, seeds, beans, and peas.
A healthy diet is low in sodium (salt), added sugars, solid fats, and refined grains. Solid fats are saturated fat and trans fatty acids. Refined grains come from processing whole grains, which results in a loss of nutrients (such as dietary fiber).
Alpha 1 antitrypsin deficiency life expectancy
People who have alpha 1 antitrypsin deficiency may not have serious complications, and they may live close to a normal lifespan.
Among people with alpha 1 antitrypsin deficiency who have a related lung or liver disease, about 3 percent die each year.
Smoking is the leading risk factor for life-threatening lung disease if you have alpha 1 antitrypsin deficiency. Smoking or exposure to tobacco smoke increases your risk of earlier lung-related symptoms and lung damage. If you have severe alpha 1 antitrypsin deficiency, smoking can shorten your life by as much as 20 years.
Living with alpha 1 antitrypsin deficiency
Ongoing Medical Care
If you have alpha 1 antitrypsin deficiency, you’ll need ongoing medical care. Talk with your doctor about how often you should schedule medical visits.
Take all of your medicines as prescribed, and follow your treatment plan. Get flu and pneumococcal vaccines to protect you from illnesses that may worsen your condition. If you have a lung infection, get treatment right away.
You also should get treatment right away for any breathing problems. If treatment includes pulmonary rehabilitation, work with your health care team to learn how to manage your condition and function at your best.
Quit Smoking and Avoid Lung Irritants
If you smoke, quit. If you don’t smoke, don’t start. Smoking is the leading risk factor for life-threatening lung disease if you have alpha 1 antitrypsin deficiency.
Talk with your doctor about programs and products that can help you quit smoking. If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking.
Also, try to avoid secondhand smoke and other lung irritants, such as dust, fumes, or toxins. Check your living and working spaces for things that may irritate your lungs. Examples include flower and tree pollen, ash, allergens, air pollution, wood burning stoves, paint fumes, and fumes from cleaning products and other household items.
Because alpha 1 antitrypsin deficiency is inherited, your children may have the condition or carry the gene for it. Advise them to avoid smoking and to stay away from places where they might inhale irritants or toxins.
References- Alpha-1 antitrypsin deficiency. https://ghr.nlm.nih.gov/condition/alpha-1-antitrypsin-deficiency#inheritance
- Sandhaus RA, Turino G, Brantly ML, et al. The diagnosis and management of alpha-1 antitrypsin deficiency in the adult. Chronic Obstr Pulm Dis. 2016; 3(3): 668-682. doi: http://doi.org/10.15326/jcopdf.3.3.2015.0182





