Ankyloglossia
Ankyloglossia also known as tongue-tie, is where an unusually thick or tight band of tissue under the baby’s tongue called the lingual frenulum connecting the bottom of the tongue’s tip to the floor of their mouth is shorter than usual and restricts the movement of the tongue. In ankyloglossia, the tongue is literally “tied,” or tethered, to the floor of the mouth, sometimes inhibiting both speech and eating. A child is born with ankyloglossia. Before you are born, a strong cord of tissue that guides development of mouth structures is positioned in the center of the mouth. It is called a frenulum. After birth, the lingual frenulum continues to guide the position of incoming teeth. As you grow, it recedes and thins. This frenulum is visible and easily felt if you look in the mirror under your tongue. In some children, the frenulum is especially tight or fails to recede and may cause tongue mobility problems.
Tongue-tie is sometimes diagnosed during a baby’s routine newborn check, but it’s not always easy to spot. It may not become apparent until your baby has problems feeding.
The tongue is one of the most important muscles for speech and swallowing. Without the tongue’s free range of motion, these activities can be impaired. For this reason having tongue-tie can lead to eating or speech problems, which may be serious in some individuals. However, the severity of tongue tie varies among children, so the condition may be detected early or later in life.
Tongue-tie affects around 4 to 11% of newborn babies. Tongue-tie or ankyloglossia is three times more common in boys than girls, and sometimes runs in families.
Some babies who have tongue-tie don’t seem to be bothered by it. In others, tongue tie can restrict the tongue’s movement, making it harder to breastfeed.
Some babies with tongue-tie are able to attach to the breast and suck well. However, severe ankyloglossia can cause breastfeeding problems, such as nipple damage (maternal nipple pain or bleeding), prolonged feeding times, poor milk transfer, inadequate milk intake and rarely low weight gains in the baby or failure to thrive, and possibly blocked ducts or mastitis due to ineffective milk removal 1, 2. Poor latching because of restricted tongue movements seems to be the underlying cause. Some newborns with symptoms may show spontaneous improvements in breastfeeding by learning to compensate 3.
See your doctor if you’re concerned about your baby’s feeding and think he/she may have tongue-tie.
Sometimes tongue-tie may not cause problems. Some cases may require a simple surgical procedure for correction. If necessary, tongue-tie can be treated with a surgical cut to release the frenulum called frenotomy. Tongue-tie release (frenotomy) procedure should be reserved for newborns who are having difficulties with breastfeeding due to severe ankyloglossia 4. Consultation with a health care professional who has expertise in breastfeeding, such as lactation consultants, neonatal nurses and occupational therapists, is recommended before referring a child for frenotomy 5. Infants are allowed to breastfeed immediately after the procedure, and complications are extremely rare 6. Complications historically attributed to frenotomy include infection, bleeding caused by severance of the lingual artery, and asphyxia (suffocation) caused by the released tongue falling back into the airway 7, 8. If additional repair is needed or the lingual frenulum is too thick for a frenotomy, a more extensive procedure known as a frenuloplasty might be an option.
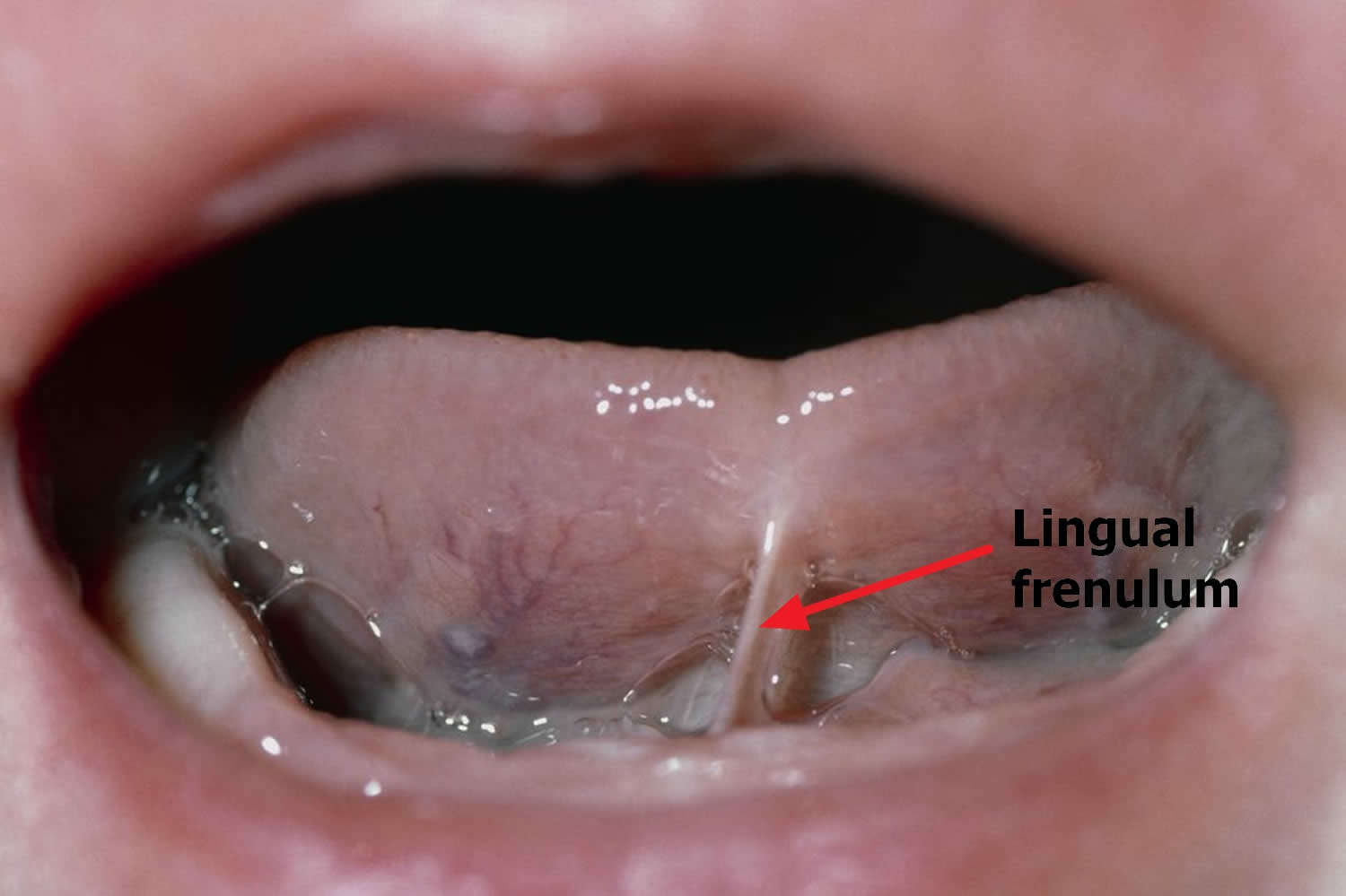
Figure 1. Infant tongue tie (ankyloglossia)
When Is Tongue-tie a Problem That Needs Treatment?
In Infants
Feeding
A new baby with a too tight frenulum can have trouble sucking and may have poor weight gain. Such feeding problems should be discussed with your child’s pediatrician who may refer you to a head and neck surgeon (ear, nose, and throat specialist) for additional treatment.
NOTE: Nursing mothers who experience significant pain while nursing or whose baby has trouble latching on should have their child evaluated for tongue tie. Although it is often overlooked, tongue tie can be an underlying cause of feeding problems that not only affect a child’s weight gain, but lead many mothers to abandon breast feeding altogether.
In Toddlers and Older Children
Speech
While the tongue is remarkably able to compensate and many children have no speech impediments due to tongue-tie, others may. Around the age of three, speech problems, especially articulation of the sounds – l, r, t, d, n, th, sh, and z may be noticeable. Evaluation may be needed if more than half of a three year old child’s speech is not understood outside of the family circle. Although, there is no obvious way to tell in infancy which children with ankyloglossia will have speech difficulties later, the following associated characteristics are common:
- V-shaped notch at the tip of the tongue
- Inability to stick out the tongue past the upper gums
- Inability to touch the roof of the mouth
- Difficulty moving the tongue from side to side
As a simple test, caregivers or parents might ask themselves if the child can lick an ice cream cone or lollipop without much difficulty. If the answer is no, they cannot, then it may be time to consult a physician.
For older children with tongue-tie, appearance can be affected by persistent dental problems such as a gap between the bottom two front teeth. Your child’s physician can guide you in the diagnosis and treatment of tongue-tie. If he/she recommends surgery, a head and neck surgeon (ear, nose, and throat specialist), can perform a surgical procedure called a frenulectomy.
Newborn tongue tie and breastfeeding problems
To breastfeed successfully, the baby needs to latch on to both the breast tissue and nipple, and their tongue needs to cover the lower gum so the nipple is protected from damage.
A baby needs to be able to have good tongue function to be able to remove milk from the breast well. If the tongue is anchored to the floor of the mouth due to a tongue -tie, the baby cannot do this as well. The baby may not be able to take in a full mouthful of breast tissue. This can result in ‘nipple-feeding’ because the nipple is not drawn far enough back in the baby’s mouth and constantly rubs against the baby’s hard palate as he feeds. As a result, the mother is likely to suffer nipple trauma.
Babies with tongue-tie aren’t able to open their mouths wide enough to latch on to the breast properly.
If you’re breastfeeding your baby and he/she has tongue-tie he/she may:
- have difficulty attaching to the breast or staying attached for a full feed
- feed for a long time, have a short break, then feed again
- be unsettled and seem to be hungry all the time
- not gain weight as quickly as he/she should
- make a “clicking” sound as he/she feed – this can also be a sign you need support with the positioning and attachment of your baby at the breast
Tongue-tie can also sometimes cause problems for a breastfeeding mother. Problems can include:
- sore or cracked nipples
- low milk supply
- mastitis (inflammation of the breast), which may keep recurring
Most breastfeeding problems, however, aren’t caused by tongue-tie and can be overcome with the right support.
If you’re finding breastfeeding difficult, ask your midwife, your family doctor or a breastfeeding specialist for help.
Ankyloglossia definition
There is a lack of a universal, unambiguous and commonly accepted definition and objective diagnostic criteria of ankyloglossia 9. There are many classifications of ankyloglossia in newborns proposed in the literature 10. Kotlow 11 introduced a simple anatomical classification based on measuring the “free tongue” length (between the lingual frenulum attachment to the tongue and the tongue’s tip) (see Table 1).
The study by Walker et al. 12 demonstrated a correlation between the tip-frenulum length and difficulties in breastfeeding which manifested mainly as mothers’ nipple pain. The average “free tongue” length in this study, in a group of 100 generally healthy newborns was found to be 9.07 mm. Coryllos’ classification 13 also includes types 3 and 4 of ankyloglossia, which meet the diagnostic criteria of ankyloglossia posterior. Due to their uncharacteristic appearance, they may easily remain unrecognized on examination (see Table 2).
However, there is no confirmed correlation between the type of lingual frenulum according to Coryllos’ classification and the degree of breastfeeding problems 14. The Hazelbaker questionnaire (The Hazelbaker Assessment Tool for Lingual Frenulum Function – HATLFF) 15, in turn, presented in the form of a point scale, includes both anatomical (5 items) and functional (7 items) criteria. Significant ankylogossia, which requires frenulotomy, is diagnosed with the appearance score <8, and the function score <11 (see Table 3).
Nevertheless, an unambiguous correlation between the Hazelbaker score and the degree of breastfeeding difficulties has not been confirmed 9. Moreover, it is found that problems with breastfeeding are not directly correlated with lingual frenulum appearance, and may occur in both anterior and posterior ankyloglossia 16. According to Ricke et al. 17 80% of the newborns with diagnosed ankyloglossia are able to effectively suck a breast without any surgical intervention, due to the tongue’s adaptability, despite the incorrect appearance of the lingual frenulum. In the study by Kumar et al. 18 half of the examined children with a short lingual frenulum were diagnosed with asymptomatic ankyloglosia that did not cause any obstacles in breastfeeding. Therefore, in order to adequately qualify for surgical intervention, it is necessary to include breastfeeding criteria. Surgical procedure itself should be performed only in those ankyloglossia cases in which breastfeeding difficulties occur 19. FDRBI (Frenotomy Decision Rule for Breastfeeding Infants) proposed by Srinivasan et al. 20 may be a helpful tool. According to the questionnaire, only a short lingual frenulum that coexists with breastfeeding difficulties (persistent nipple pain and/or inadequate latch and/or poor weight gain <15 g per day) and improper tongue function (inability to protrude beyond the alveolar ridge, to lift the tongue to the roof of the mouth or to adequately cup the nipple-areolar complex) may be qualified for frenulotomy. Moreover, the LATCH index, which includes 5 categories: L (latch), A (audible swallowing), T (type of nipple), C (comfort) and H (hold) and scores them from 0 to 2, may also be applied for objective and quantitative assessment of breastfeeding quality 21. Table 4 presents an accurate description of the LATCH index, together with proposed example questions that may be helpful during conversations with mothers that experience breastfeeding problems.
Infant Breastfeeding Assessment Tool (IBFAT) is a similar scale, that consists of 4 questions for mothers describing their experience during breastfeeding, scored from 0 to 3 (see Table 5) 12.
The study by Altuntas et al. 22 confirms the reliability of both indexes (LATCH and Infant Breastfeeding Assessment Tool [IBFAT]) in breastfeeding quality assessment.
Table 1. Classification of ankyloglossia according to Kotlow (based on the “free tongue” length)
| Normal, clinically acceptable range of “free tongue” >16mm | |
| Class 1: Mild ankyloglossia | 12-16 mm |
| Class 2: Moderate ankyloglossia | 8-11 mm |
| Class 3: Severe ankyloglossia | 3-7 mm |
| Class 4: Complete ankyloglossia | <3 mm |
Table 2. Classification of ankyloglossia according to Coryllos
| Type 1 | Fine and elastic frenulum; the tongue is anchored from the tip to the alveolar ridge and it is found to be heart-shaped |
| Type 2 | Fine and elastic frenulum; the tongue is anchored 2-4 mm from the tip near the alveolar ridge |
| Type 3 | Thick, fibrous non-elastic frenulum; the tongue is anchored from its middle to the floor of the mouth |
| Type 4 | The frenulum cannot be seen but palpated; it has a fibrous and/or thick and shiny submucous anchoring from the base of the tongue to the floor of the month |
Table 3. Diagnostics of ankyloglossia according to Hazelbaker (Hazelbaker, The Assessment Tool for Lingual Frenulum Function)
| Function items | Appearance items |
|---|---|
| Lateralization | Appearance of tongue when lifted |
| 2 – complete | 2– round or square |
| 1 – body of tongue but not tongue tip | 1 – slight cleft in tip apparent |
| 0–none | 0– heart-shaped |
| Lift of tongue | |
| 2–tip to mid-mouth | Elasticity of frenulum |
| 1 – only edges to mid-mouth | 2–very elastic |
| 0 – tip stays at alveolar ridge or tip rises to mid-mouth with jaw closure | 1 – moderately elastic |
| 0 – little or no elasticity | |
| Extension of tongue | Length of lingual frenulum when tongue lifted |
| 2–tip over lower lip | 2–>1 cm |
| 1 – tip over lower gum only | 1–1 cm |
| 0 – neither of the above or mid-tongue humps | 0–<1 cm |
| Spread of anerior tongue | Attachment of lingua frenulum to tongue |
| 2 – complete | 2 – posterior to tip |
| 1 – partial | 1 – at tip |
| 0– little or none | 0– notched |
| Cupping of tongue | Attachment of lingual frenulum to inferior alveolar ridge |
| 2 – entire edge, firm cup | 2 – attached to floor of mouth or well below ridge |
| 1 – side edges only, moderate cup | 1 – attached just below the ridge |
| 0 – poor or no cup | 0– attached at ridge |
| Peristalsis | |
| 2 – complete anterior to posterior (originates at tip) | |
| 1 – partial (orignates posteriori to tip) | |
| 0 – none or reverse peristalsis | |
| Snap-back | |
| 2 – none | |
| 1 – periodic | |
| 0 – frequent or with each suck | |
| Scoring: | |
| 14 – perfect score | |
| 11 – acceptable if appearance item score is 10 | |
| <11 – tongue function impaired (frenotomy should be considered) | |
| Frenotomy is necessary if function score is <11 and appearance score is <8 | |
Table 4. LATCH scale (includes 5 categories: L (latch), A (audible swallowing), T (type of nipple), C (comfort) and H (hold) and scores them from 0 to 2)
| 0 | 1 | 2 | Example questions | |
|---|---|---|---|---|
| L– latch | Too sleepy or reluctant No latch obtained | Repeated attempts Must hold nipple in mouth Must stimulate to suck | Grasps breast Tongue down and forward Lips flanged Rhythmic suckling | How did your baby grasp your breast? Did you baby suckle on his own or did you have to work with him? |
| A–audible swallow | None | A few with stimulation | Spontaneous | Did your you baby hear swallow? How frequently? |
| T– type of nipple | Inverted | Flat | Everted (after stimulation) | Do your nipples stand out or do they flatten easily? |
| C– comfort | Engorged Cracked, bleeding, large blisters or bruises Severe discomfort | Filling Small or bruises blisters Mother complains of pinching Mild/moderate discomfort | Soft Tender Intact nipples (no damage) | Are your nipples tender? Are your breasts becoming full and heavy? |
| H– hold | Full assist (Staff holds infant at breast) | Minimal assist (i.e. elevate head of bed, place pillows) Teach one side mother does other Staff help, mother takes over feeding | No assist from staff Mother able to position/ /hold infant | Did someone help you put your baby to breast? Do you need help with the next feeding? |
Table 5. Infant Breastfeeding Assessment Tool (IBFAT)
| 3 | 2 | 1 | 0 | |
|---|---|---|---|---|
| To get the baby to begin this feed, did you have to: | Just place the baby on the breast, as no effort was needed | Use mild stimulation, such as unbundling, patting, burping | Unbundle baby, sit baby back and forward, rub baby’s body or limbs at the beginning and during the feed | Could not be aroused |
| Rooting (at touch of nipple to cheek, baby’s head turns toward the nipple, the mouth opens, and baby attempts to fix mouth on the nipple) When the baby was placed at the breast he/she: | Rooted effectively at once. | Needed some coaxing, prompting/ /encouragement to root | Rooted poorly even with coaxing | Did not try to root |
| How long from placing baby he/she at the latch breast does on and start to feed well? | 0–3 minutes | 3–10 minutes | Over 10 minutes | Did latch not at all |
| Which of the following phrases best describes the baby’s feeding pattern at this feed? | Sucked well on one or both breasts | Sucked fairly well (sucked off and on but needed some encouragement) | Sucked poorly, weak sucking, some sucking for short periods | Baby did not suck |
Ankyloglossia symptoms
Children are born with tongue-tie, but depending on its severity, tongue tie can have a range of effects that are noticeable at different times. Here are the most common signs and symptoms that may indicate your baby has tongue-tie:
- A newborn who has trouble latching on or sucking from the breast; the infant might chew instead of suck (tongue tie poses less of a problem with bottle feeding)
- Your baby has difficulty lifting their tongue up or moving it from side to side
- Mother in significant pain while nursing
- A baby who constantly fusses at the breast
- Your baby has difficulty sticking his/her tongue out past the lower front teeth
- Poor weight gain and failure to thrive in an infant
- V-shaped or heart-shaped notch at the tip of the tongue when it’s stuck out (because the middle is pulled in by the tight band)
- A toddler’s difficulty in licking a lollipop or ice cream cone, touching the roof of their mouth, moving their tongue from side to side, or sticking out their tongue past the upper gums
- Enunciation problems that continue after age 3, especially when articulating these sounds: “t”, “d”, “l”, “r”, “n”, “th”, “s”, and “z”
- Persistent dental problems, such as a gap between the front lower teeth and tooth decay or gingivitis (gum inflammation) because your child can’t get rid of food debris naturally with her tongue
- Difficulty chewing age-appropriate solid foods
- Gagging or choking on foods
- Pocketing of food or withholding it in the cheeks
- Persistent dribbling
See a doctor if:
- Your baby has signs of tongue-tie that cause problems, such as having trouble breast-feeding
- A speech-language pathologist thinks your child’s speech is affected by tongue-tie
- Your older child complains of tongue problems that interfere with eating, speaking or reaching the back teeth
- You’re bothered by your own symptoms of tongue-tie
There are reports of older children and adults undergoing tongue-tie release (frenotomy) to improve articulation and to relieve mechanical problems related to limited tongue movement (e.g., kissing and licking lips) 4. However, definitive studies addressing the association between ankyloglossia and speech are lacking 5. A formal assessment by a speech pathologist may provide diagnostic information, and noninvasive therapeutic strategies may be instituted.
Ankyloglossia complications
Tongue-tie can affect a baby’s oral development, as well as the way he or she eats, speaks and swallows.
For example, tongue-tie can lead to:
- Breast-feeding problems. Breast-feeding requires a baby to keep his or her tongue over the lower gum while sucking. If unable to move the tongue or keep it in the right position, the baby might chew instead of suck on the nipple. This can cause significant nipple pain and interfere with a baby’s ability to get breast milk. Ultimately, poor breast-feeding can lead to inadequate nutrition and failure to thrive.
- Speech difficulties. Tongue-tie can interfere with the ability to make certain sounds — such as “t,” “d,” “z,” “s,” “th,” “r” and “l.”
- Poor oral hygiene. For an older child or adult, tongue-tie can make it difficult to sweep food debris from the teeth. This can contribute to tooth decay and inflammation of the gums (gingivitis). Tongue-tie can also lead to the formation of a gap or space between the two bottom front teeth.
- Challenges with other oral activities. Tongue-tie can interfere with activities such as licking an ice cream cone, licking the lips, kissing or playing a wind instrument.
Ankyloglossia causes
Tongue tie occurs when the lingual frenulum (the band of tissue under the tongue) fails to separate from the tongue before birth. With tongue-tie, the lingual frenulum remains attached to the bottom of the tongue. Why this happens is largely unknown, although some cases of tongue-tie have been associated with certain genetic factors. The band stays connected as the child grows because it’s unusually short or thick, creating a tightness to the tongue that limits its mobility. Tongue tie is usually seen as an isolated condition, without any other disorders in a child. However, it is occasionally associated with other syndromes. A genetic cause of ankyloglossia has been reported as X linked cleft palate syndrome. A gene mutation on TBX22 causes this 23.
Ankyloglossia diagnosis
Tongue-tie is typically diagnosed during a physical exam. During the evaluation, your child’s doctor may:
- Ask questions about your child’s feeding behavior
- Perform a physical exam of your child’s mouth and teeth and use a tongue depressor to elevate the tip of your child’s tongue
- Ask your older child to perform various exercises with their tongue to demonstrate maximum range of motion
- Ask your older child to articulate certain sounds, like “n”s and “l”s
- If being evaluated via telemedicine, you may be asked to upload photos of your child’s tongue though the patient portal
For infants, the doctor might use a screening tool to score various aspects of the tongue’s appearance and ability to move.
Ankyloglossia treatment
Treatment for tongue-tie is controversial 24. Some doctors and lactation consultants recommend correcting it right away — even before a newborn is discharged from the hospital. Others prefer to take a wait-and-see approach.
The lingual frenulum may loosen over time, resolving tongue-tie. In other cases, tongue-tie persists without causing problems. In some cases, consultation with a lactation consultant can assist with breast-feeding, and speech therapy with a speech-language pathologist may help improve speech sounds.
Surgical treatment of tongue-tie may be needed for infants, children or adults if tongue-tie causes problems. Surgical procedures include a frenotomy or frenuloplasty.
Ankyloglossia surgery
Frenotomy
A simple surgical procedure called a frenotomy can be done with or without local anesthesia in the hospital nursery or doctor’s office 25. The doctor examines the lingual frenulum and then uses sterile scissors to snip the frenulum free after stabilizing the tongue with the fingers or spatula. The incision should begin at the free margin of the frenulum and proceed posteriorly adjacent to the tongue with care not to injure inferiorly based submandibular salivary ducts. The procedure is quick and discomfort is minimal since there are few nerve endings or blood vessels in the lingual frenulum. If any bleeding occurs, it’s likely to be only a drop or two of blood and can be controlled with gauze and light pressure, no suture is required 9. After the procedure, a baby can breast-feed immediately 25, while during the next 7-10 days tongue mobilizing exercises that prevent reattachment of the frenulum are advised 26.
Nowadays diode laser is increasingly popular as an alternative in tongue-tie release 27. Its application decreases the bleeding in the operating field, minimalizes swelling and post-operative pain 28.
Complications of a frenotomy are rare — but could include bleeding or infection, or damage to the tongue or salivary glands. It’s also possible to have scarring or for the frenulum to reattach to the base of the tongue.
Frenuloplasty
A more extensive procedure known as a frenuloplasty might be recommended if additional repair is needed or the lingual frenulum is too thick for a frenotomy.
A frenuloplasty is done under general anesthesia with surgical tools. After the frenulum is released, the wound is usually closed with sutures that absorb on their own as the tongue heals. Your child will go home the same day as the operation and will most likely not need to stay in the hospital overnight.
Possible complications of a frenuloplasty are similar to a frenotomy and are rare include bleeding or infection, or damage to the tongue or salivary glands. Scarring is possible due to the more extensive nature of the procedure, as are reactions to general anesthesia.
After a frenuloplasty, tongue exercises might be recommended to enhance tongue movement and reduce the potential for scarring.
Follow-up care
With an in-office frenotomy procedure, the frenulum is snipped and there is usually no need for a follow-up appointment. In an infant, breastfeeding can provide the pain relief and infection-fighting properties that promote a prompt recovery.
With frenuloplasty, a follow-up appointment may be scheduled to check on your child’s healing in the treated area. There is no need for the removal of stitches, however, because they will absorb on their own.
Your child may be required to do tongue movement exercises to encourage proper movement and reduce the risk of scarring. Depending on your child’s speech, your child’s primary care provider may recommend working with a speech therapist, to correct enunciation problems.
Ankyloglossia prognosis
In the vast majority of cases, treatment for ankyloglossia or tongue tie permanently corrects the condition and prevents the eating, speech, and dental problems that frequently go along with tongue tie. Occasionally, the simple frenotomy procedure fails to eliminate tongue tie and the problem recurs. Follow-up treatment with a frenuloplasty is then recommended.
Older children whose speech was impaired by tongue tie generally overcome their enunciation problems within a year or two, with the aid of a speech therapist.
References- Buryk M, Bloom D, Shope T. Efficacy of neonatal release of ankyloglossia: a randomized trial. Pediatrics. 2011 Aug;128(2):280-8. https://doi.org/10.1542/peds.2011-0077
- Messner AH, Lalakea ML, Aby J, Macmahon J, Bair E. Ankyloglossia: incidence and associated feeding difficulties. Arch Otolaryngol Head Neck Surg. 2000 Jan;126(1):36-9. https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/404076
- Ballard JL, Auer CE, Khoury JC. Ankyloglossia: assessment, incidence, and effect of frenuloplasty on the breastfeeding dyad. Pediatrics. 2002 Nov;110(5):e63. https://doi.org/10.1542/peds.110.5.e63
- Segal LM, Stephenson R, Dawes M, Feldman P. Prevalence, diagnosis, and treatment of ankyloglossia: methodologic review. Can Fam Physician. 2007 Jun;53(6):1027-33. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1949218
- Hong P. Five things to know about…ankyloglossia (tongue-tie). CMAJ. 2013 Feb 5;185(2):E128. doi: 10.1503/cmaj.120785
- Masaitis NS, Kaempf JW. Developing a frenotomy policy at one medical center: a case study approach. J Hum Lact. 1996 Sep;12(3):229-32. doi: 10.1177/089033449601200321
- Mathewson R, Siegel M, McCanna D. Ankyloglossia: a review of the literature and a case report. J Dent Child. 1966;33:238–43.
- Marmet C, Shell E, Marmet R. Neonatal frenotomy may be necessary to correct breastfeeding problems. J Hum Lact. 1990 Sep;6(3):117-21. doi: 10.1177/089033449000600318
- Brzęcka D, Garbacz M, Micał M, Zych B, Lewandowski B. Diagnosis, classification and management of ankyloglossia including its influence on breastfeeding. Dev Period Med. 2019;23(1):79-87. doi: 10.34763/devperiodmed.20192301.7985
- Murias I, Grzech-Leśniak K, Murias A, Walicka-Cupryś K, Dominiak M, Golob Deeb J, Matys J. Efficacy of Various Laser Wavelengths in the Surgical Treatment of Ankyloglossia: A Systematic Review. Life (Basel). 2022 Apr 8;12(4):558. doi: 10.3390/life12040558
- Kotlow LA. Ankyloglossia (tongue-tie): a diagnostic and treatment quandary. Quintessence Int. 1999 Apr;30(4):259-62.
- Walker RD, Messing S, Rosen-Carole C, McKenna Benoit M. Defining Tip-Frenulum Length for Ankyloglossia and Its Impact on Breastfeeding: A Prospective Cohort Study. Breastfeed Med. 2018 Apr;13(3):204-210. doi: 10.1089/bfm.2017.0116
- Coryllos, E. & Genna, Catherine & Salloum, A.C.. (2004). Congenital tongue-tie and its impact on breastfeeding. American Academy of Pediatrics Section on Breastfeeding. 1-6. https://www.researchgate.net/publication/301346077_Congenital_tongue-tie_and_its_impact_on_breastfeeding
- Haham A, Marom R, Mangel L, Botzer E, Dollberg S. Prevalence of breastfeeding difficulties in newborns with a lingual frenulum: a prospective cohort series. Breastfeed Med. 2014 Nov;9(9):438-41. doi: 10.1089/bfm.2014.0040
- Amir LH, James JP, Donath SM. Reliability of the hazelbaker assessment tool for lingual frenulum function. Int Breastfeed J. 2006 Mar 9;1(1):3. doi: 10.1186/1746-4358-1-3
- Hong P, Lago D, Seargeant J, Pellman L, Magit AE, Pransky SM. Defining ankyloglossia: a case series of anterior and posterior tongue ties. Int J Pediatr Otorhinolaryngol. 2010 Sep;74(9):1003-6. doi: 10.1016/j.ijporl.2010.05.025
- Ricke LA, Baker NJ, Madlon-Kay DJ, DeFor TA. Newborn tongue-tie: prevalence and effect on breast-feeding. J Am Board Fam Pract. 2005 Jan-Feb;18(1):1-7. doi: 10.3122/jabfm.18.1.1
- Kumar RK, Nayana Prabha PC, Kumar P, Patterson R, Nagar N. Ankyloglossia in Infancy: An Indian Experience. Indian Pediatr. 2017 Feb 15;54(2):125-127. doi: 10.1007/s13312-017-1014-5
- Messner AH, Lalakea ML, Aby J, Macmahon J, Bair E. Ankyloglossia: incidence and associated feeding difficulties. Arch Otolaryngol Head Neck Surg. 2000 Jan;126(1):36-9. doi: 10.1001/archotol.126.1.36
- Srinivasan A, Dobrich C, Mitnick H, Feldman P. Ankyloglossia in breastfeeding infants: the effect of frenotomy on maternal nipple pain and latch. Breastfeed Med. 2006 Winter;1(4):216-24. doi: 10.1089/bfm.2006.1.216
- Jensen D, Wallace S, Kelsay P. LATCH: a breastfeeding charting system and documentation tool. J Obstet Gynecol Neonatal Nurs. 1994 Jan;23(1):27-32. doi: 10.1111/j.1552-6909.1994.tb01847.x
- Altuntas N, Turkyilmaz C, Yildiz H, Kulali F, Hirfanoglu I, Onal E, Ergenekon E, Koç E, Atalay Y. Validity and reliability of the infant breastfeeding assessment tool, the mother baby assessment tool, and the LATCH scoring system. Breastfeed Med. 2014 May;9(4):191-5. doi: 10.1089/bfm.2014.0018
- Becker S, Mendez MD. Ankyloglossia. [Updated 2022 Mar 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482295
- Hill, RR, Pados, BF. Symptoms of problematic feeding in infants under 1 year of age undergoing frenotomy: A review article. Acta Paediatr. 2020; 109: 2502– 2514. https://doi.org/10.1111/apa.15473
- Kupietzky A, Botzer E. Ankyloglossia in the infant and young child: clinical suggestions for diagnosis and management. Pediatr Dent. 2005 Jan-Feb;27(1):40-6.
- Kenny-Scherber AC, Newman J. Office-based frenotomy for ankyloglossia and problematic breastfeeding. Can Fam Physician. 2016 Jul;62(7):570-1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4955087
- Ghaheri BA, Cole M, Fausel SC, Chuop M, Mace JC. Breastfeeding improvement following tongue-tie and lip-tie release: A prospective cohort study. Laryngoscope. 2017 May;127(5):1217-1223. doi: 10.1002/lary.26306
- Nicoloso GF, dos Santos IS, Flores JA, da Silveira BL, Oliveira MD. An Alternative Method to Treat Ankyloglossia. J Clin Pediatr Dent. 2016;40(4):319-21. doi: 10.17796/1053-4628-40.4.319