Anterior cruciate ligament injury
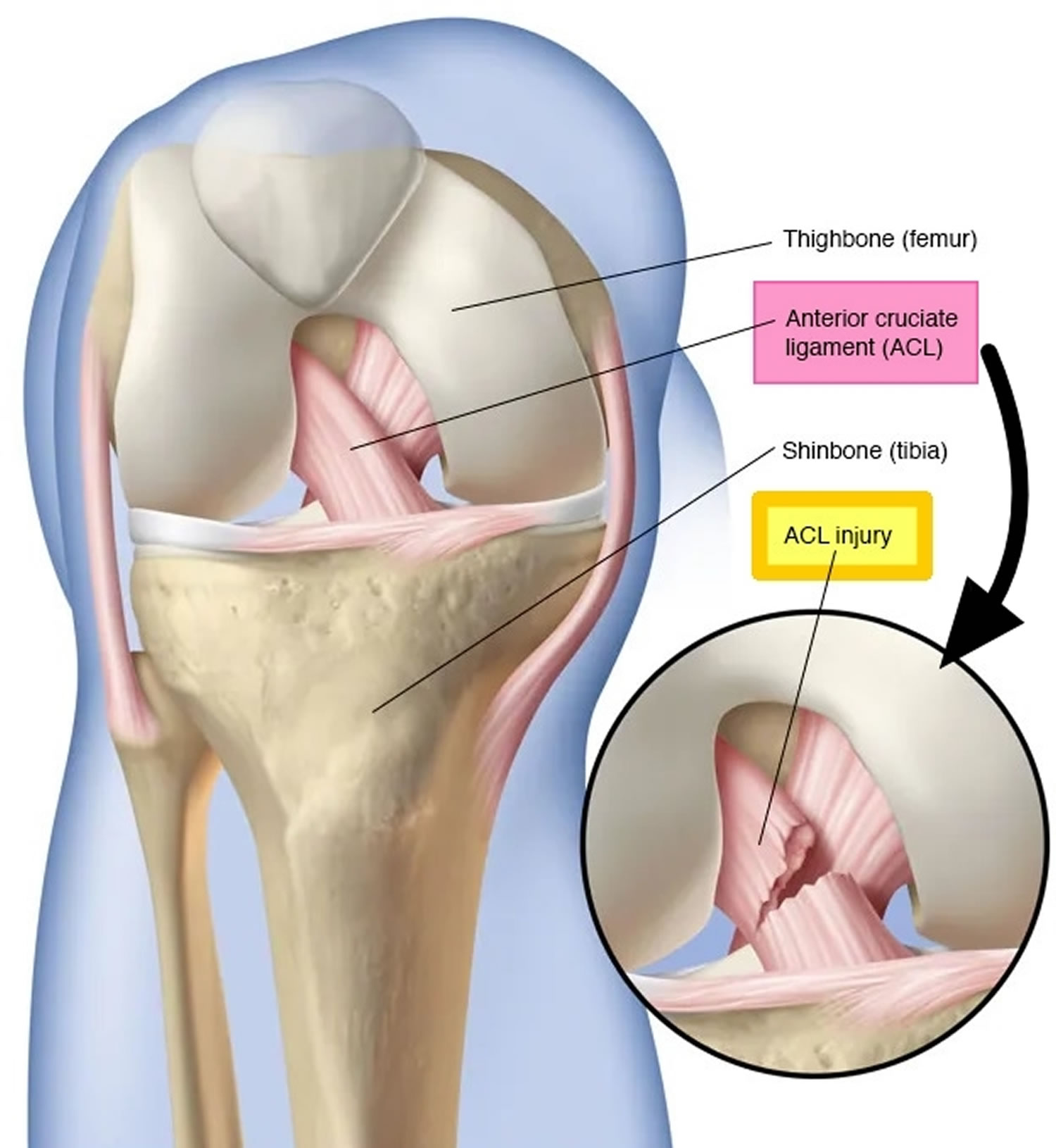
Anterior cruciate ligament injury also known as ACL tear, is a very common sporting knee injury 1. Ligaments are strong bands of tissue that attach one bone to another bone. The anterior cruciate ligament is one of two ligaments that crosses the middle of your knee that connects your thighbone (femur) to your shinbone (tibia) and helps stabilize your knee joint (Figures 1 and 2). The anterior cruciate ligament (ACL) limits hyperextension of the knee (which normally does not occur at this joint) and prevents the anterior sliding of the tibia on the femur. When the anterior cruciate ligament is damaged, there is usually a partial or complete tear of the ligament. A mild ACL tear may stretch the ligament but leave it intact. Many people hear or feel a “pop” in the knee when an anterior cruciate ligament injury occurs. Your knee may swell, feel unstable, may feel like it gives way and become too painful to bear weight.
ACL injuries most commonly occur during sports that involve sudden stops, jumping or changes in direction — such as basketball, soccer, football, tennis, downhill skiing, volleyball and gymnastics.
Anterior cruciate ligament (ACL) injuries have an incidence of approximately 252,000 yearly 2. Approximately half of anterior cruciate ligament injuries occur in combination with damage to the meniscus, articular cartilage, or other ligaments. Additionally, patients may have bruises of the bone beneath the cartilage surface. These may be seen on a magnetic resonance imaging (MRI) scan and may indicate injury to the overlying articular cartilage. Persons who experience anterior cruciate ligament injuries have an increased risk of arthritis.
Women are two to eight times more likely to have an anterior cruciate ligament injury than similarly trained men 3, 4, 5, 6, 7. It has been proposed that this is due to differences in physical conditioning, muscular strength, and neuromuscular control. Other hypothesized causes of this gender-related difference in anterior cruciate ligament injury rates include pelvis and lower extremity (leg) alignment, increased ligamentous laxity, and the effects of estrogen on ligament properties.
An anterior cruciate ligament tear can happen when you change direction rapidly, slow down when running, land after a jump, or receive a direct blow to your knee. Athletes who participate in high demand sports like soccer, skiing and basketball are sports where anterior cruciate ligament knee injuries can happen.
Injuries to the posterior cruciate ligament (PCL) are less common. It can be injured during a direct blow to the tibia when the knee is bent, or when the knee is over-straightened.
The patient with an anterior cruciate ligament injury should be referred to the orthopedic surgeon to discuss treatment options and a physical therapist (PT) for rehabilitation.
Depending on the severity of your anterior cruciate ligament injury and your activity level, treatment may include rest and rehabilitation exercises to help you regain strength and stability or surgery to replace the torn ligament followed by rehabilitation. A proper training program may help reduce the risk of an anterior cruciate ligament injury.
To treat the immediate ACL injury:
- Use R.I.C.E. model of self-care at home (rest, ice, compression, elevation)
- Take pain relievers such as ibuprofen as needed
- You can use an elastic bandage around your knee
- Use a splint or walk with crutches if needed
ACL injuries, depending upon their severity, can be managed nonoperatively or operatively.
Nonoperative treatment is typically reserved for those with low functional demands, type and severity of ACL tear, time of injury, and subsequent assessment. Continued monitoring and treatment by an orthopedic surgeon and physical therapist is necessary and will improve your functional status and stability post-injury. Of note, about half of the patients who initially choose the non-operative pathway will later choose to undergo surgical repair.
The decision to undergo operative treatment is based upon many factors such as the patient’s baseline level of physical activity, functional demands, age, occupation, and other associated injuries, if present 8. Athletes and individuals who are younger and more active tend to opt for surgical repair and reconstruction. Other surgical repair/reconstruction candidates are those with significant instability of the knee and/or multiple knee structures injured. Operative treatment is typical with a tissue graft. In a recent systematic review, 81% of those involved treated with ACL reconstruction returned to some athletic activity, 65% returned to the preinjury level of competition, and 55% of high-level athletes returned to normal play and competition. Although, it has been reported that of those who undergo surgical repair, overall 90% return to near-normal functioning. The factors that may contribute to a lower percentage of return to play may be secondary to external factors such as fear of reinjury.
Your doctor may recommend surgery if:
- You’re an athlete and want to continue in your sport, especially if the sport involves jumping, cutting or pivoting
- More than one ligament or the fibrous cartilage in your knee also is injured
- The injury is causing your knee to buckle during everyday activities
During ACL reconstruction, the surgeon removes the damaged ligament and replaces it with a segment of tendon — tissue similar to a ligament that connects muscle to bone. This replacement tissue is called a graft.
Your surgeon will use a piece of tendon from another part of your knee or a tendon from a deceased donor.
After surgery you’ll resume another course of rehabilitative therapy. Successful ACL reconstruction paired with rigorous rehabilitation can usually restore stability and function to your knee.
There’s no set time frame for athletes to return to play. Recent research indicates that up to one-third of athletes sustain another tear in the same or opposite knee within two years. A longer recovery period may reduce the risk of re-injury.
In general, it takes as long as a year or more before athletes can safely return to play. Doctors and physical therapists will perform tests to gauge your knee’s stability, strength, function and readiness to return to sports activities at various intervals during your rehabilitation. It’s important to ensure that strength, stability and movement patterns are optimized before you return to an activity with a risk of ACL injury.
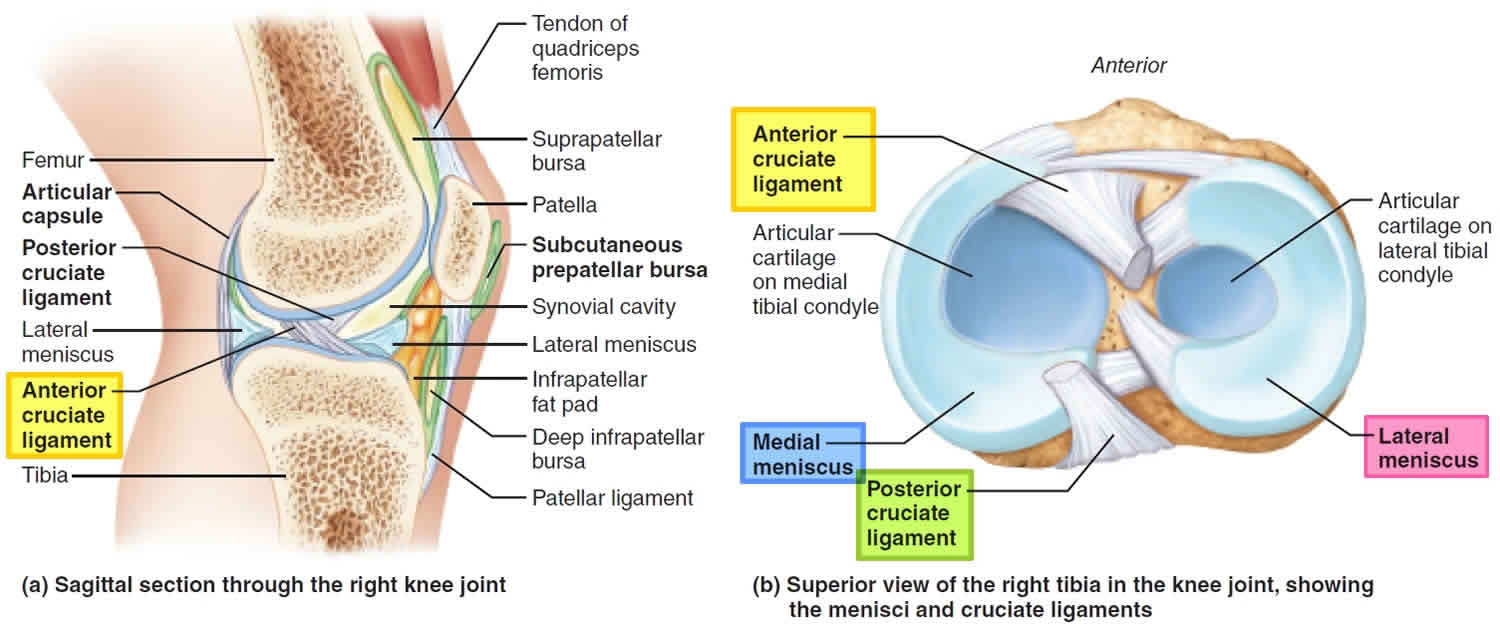
Figure 1. Anterior cruciate ligament anatomy
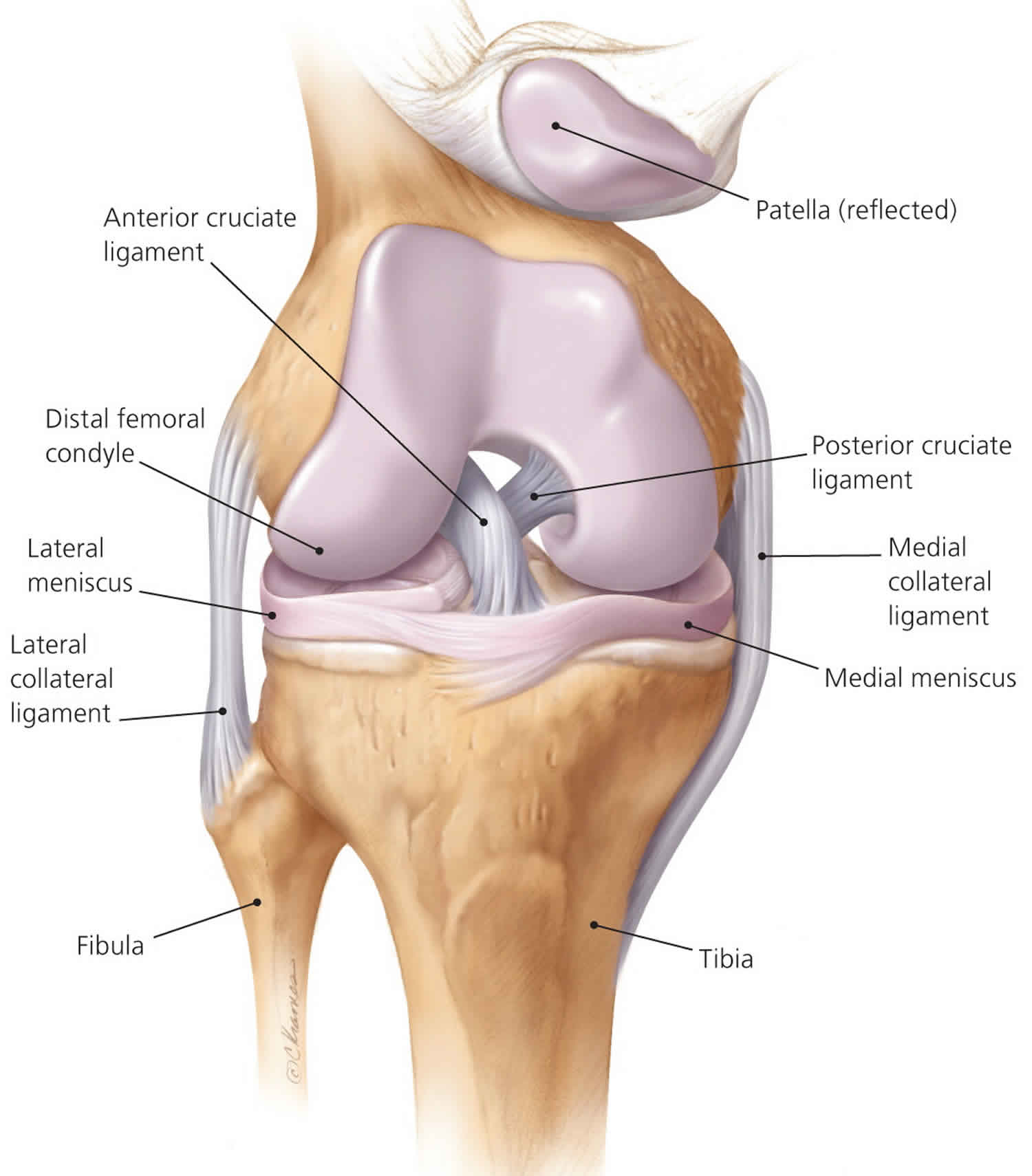
Figure 2. Knee joint ligaments (posterior view)
Figure 3. Anterior cruciate ligament injury
What can I do to prevent an ACL tear?
Properly supervised training, including “jump training” which teaches athletes how to jump and land properly can reduce serious knee ligament injuries by around 50%. Jump training includes plyometrics and should also include strength training of supporting muscles such as the hip and core muscles to round out the program. Plyometrics also known as jump training or plyos, is a type of exercise training that uses speed and force of different movements to build muscle power. Plyometrics training can improve your physical performance and ability to do different activities.
How do you know when ACL reconstruction surgery is necessary?
If your ACL is torn and you play basketball, soccer, rugby, lacrosse, football, hockey, or enjoy rock climbing and do not want to give up these activities, ACL reconstruction may be the best choice for you. It should also be considered if you have a job that requires manual labor. If you are not athletic but your knee continues to give way or feel that it is “coming apart,” the surgery may be a consideration.
When deciding whether to have ACL surgery, the following factors should be taken into consideration:
- your age – older people who are not very active may be less likely to need surgery
- your lifestyle – for example, whether you’ll be able to follow the rehabilitation programme after having surgery
- how often you play sports – you may need to have surgery if you play sports regularly
- your occupation – for example, whether you do any form of manual labor
- how unstable your knee is – if your knee is very unstable, you’re at increased risk of doing further damage if you do not have surgery
- whether you have any other injuries – for example, your menisci (small discs of cartilage that act as shock absorbers) may also be torn and may heal better when repaired at the same time as ACL reconstruction
When surgical treatment is indicated for an acute isolated ACL tear, early reconstruction is preferred because the risk of additional cartilage and meniscal injury starts to increase within 3 months 9. Furthermore, ACL tears indicated for surgery should be treated with ACL reconstruction rather than repair because of the lower risk of revision surgery 9.
What do I need to do after the anterior cruciate ligament surgery?
Rehabilitation after surgery is just as important as the surgery itself. It takes time and effort to restore range of motion (how far your knee will bend and straighten) and strength. If you are not willing to do daily exercise for several weeks then surgery may not be for you.
Are there risks in deciding not to have surgery?
Long term instability may lead to arthritis. If you opt not to have surgery it’s important to minimize the giving way episodes by restricting your activities, strengthening your leg muscles and wearing a brace if necessary.
Anterior cruciate ligament anatomy
The knee is comprised of the bottom end of the femur (thigh) and the upper end of the tibia (shin) and the patella (knee cap). The knee joint (tibiofemoral joint) is the largest and most complex joint of your body. The knee joint is a modified hinge joint (because its primary movement is a uniaxial hinge movement) that consists of three joints within a single synovial cavity:
- Laterally is a tibiofemoral joint, between the lateral condyle of the femur, lateral meniscus, and lateral condyle of the tibia, which is the weight-bearing bone of the leg.
- Medially is another tibiofemoral joint, between the medial condyle of the femur, medial meniscus, and medial condyle of the tibia.
- An intermediate patellofemoral joint is between the patella and the patellar surface of the femur.
The knee being a hinge joint, it is structured to perform two principal actions – flexion (bending) and extension (straightening). The muscles which act at the knee are predominantly the quadriceps (extension) and the hamstrings (flexion). The major ligaments of the knee are the anterior cruciate ligament (ACL), the posterior cruciate ligament (PCL), and the medial collateral ligament (MCL) and lateral collateral ligament (LCL). These, along with the muscles acting on the knee, provide the joint’s stability.
The joint capsule of the knee is reinforced by several capsular and extracapsular ligaments, all of which become taut when the knee is extended to prevent hyperextension of the leg at the knee.
- The extracapsular fibular and tibial collateral ligaments are located on the lateral and medial sides of the joint capsule, respectively. The fibular collateral ligament descends from the lateral epicondyle of the femur to the head of the fibula. The tibial collateral ligament runs from the medial epicondyle of the femur to the medial condyle of the tibia. Besides halting leg extension and preventing hyperextension, these collateral ligaments prevent the leg from moving laterally and medially at the knee.
- The oblique popliteal ligament (“back of the knee”) crosses the posterior aspect of the capsule. Actually it is a part of the tendon of the semimembranosus muscle that fuses with the joint capsule and helps stabilize the joint.
- The arcuate popliteal ligament arcs superiorly from the head of the fibula over the popliteus muscle to the posterior aspect of the joint capsule.
In addition, the knee joint is stabilized by two strong intracapsular ligaments called cruciate ligaments because they cross each other like an X (cross) (Figure 1). Each runs from the tibia to the femur and is named for its site of attachment to the tibia. The anterior cruciate ligament (ACL) attaches to the anterior part of the tibia, in the intercondylar area. From there, it passes posteriorly to attach to the femur on the medial side of the lateral condyle. The anterior cruciate ligament (ACL) is intracapsular but is located outside the synovial fluid. The anterior cruciate ligament is the primary restraint to anterior translation of the tibia, as well as tibial internal rotation. The posterior cruciate ligament (PCL) arises from the posterior intercondylar area of the tibia and passes anteriorly to attach to the femur on the lateral side of the medial condyle.
Functionally, the cruciate ligaments act as restraining straps to prevent undesirable movements at the knee joint. The anterior cruciate helps prevent anterior
sliding of the tibia. The posterior cruciate, which is even stronger than the anterior cruciate, prevents forward sliding of the femur or backward displacement of the tibia. The two cruciates also function together to lock the knee when you stand.
The knee joint is prone to injury because of its complexity and weight-bearing function. It is made up of the tibia, femur, and patella, which are stabilized by the medial collateral ligament, lateral collateral ligament, posterior cruciate ligament, and anterior cruciate ligament (ACL). The medial and lateral menisci act as shock absorbers, distributing weight evenly with each step or turn.
Anterior cruciate ligament function
During movement of the knee, the anterior cruciate ligament (ACL) prevents anterior sliding of the tibia; the posterior cruciate ligament prevents posterior sliding of the tibia.
When the knee is fully extended, both cruciate ligaments are taut and the knee is locked.
The anterior cruciate ligament (ACL) limits hyperextension of the knee (which normally does not occur at this joint) and prevents the anterior sliding of the tibia on the femur. Anterior cruciate ligament is stretched or torn in about 70% of all serious knee injuries.
Anterior cruciate ligament injury causes
Most ACL injuries happen during sports and fitness activities that can put stress on the knee:
- Suddenly slowing down and changing direction (cutting)
- Pivoting with your foot firmly planted
- Landing from a jump incorrectly
- Stopping suddenly
- Receiving a direct blow to the knee
An anterior cruciate ligament injury can occur if you:
- Get hit very hard on the side of your knee, such as during a football tackle
- Overextending your knee joint
- Quickly stop moving and change direction while running, landing from a jump, or turning
ACL rupture is typically the result of a traumatic, sports-related injury. This injury may be contact or non-contact. The majority of anterior cruciate ligament (ACL) injuries are non-contact
injuries 10, 11, 12. Basketball, football, soccer, martial arts, gymnastics and skiing are common sports linked to anterior cruciate ligament tears. This is because they involve jumping, running with sharp turns, quick stops and pivoting.
Anterior cruciate ligament injuries often occur with other injuries. For example, an anterior cruciate ligament tear often occurs along with tears to the MCL (medial collateral ligament) and the shock-absorbing cartilage in the knee (meniscus).
Most anterior cruciate ligament tears occur in the middle of the ligament, or the ligament is pulled off the thigh bone. These injuries form a gap between the torn edges, and do not heal on their own.
Mechanism of anterior cruciate ligament injury
Patients who sustain anterior cruciate ligament injuries classically describe a popping sound, followed by immediate pain and swelling of the knee. The feeling of instability or giving-way episodes typically limit the ability to participate in activities. Patients might describe the feeling of instability with the “double fist sign” (i.e., fists facing each other, rotating in a grinding motion).
Anterior cruciate ligament injuries caused by contact require a fixed lower leg (i.e., when planted) and torque with enough force to cause a tear. Contact injuries account for only about 30 percent of anterior cruciate ligament injuries 13. The remaining 70 percent of anterior cruciate ligament tears are noncontact injuries occurring primarily during deceleration of the lower extremity, with the quadriceps maximally contracted and the knee at or near full extension 14, 11, 12. In noncontact scenarios, the stress on the anterior cruciate ligament resembles that of a collision of the knee. When the knee is at or near full extension, quadriceps contraction increases anterior cruciate ligament tensile force. The hamstrings, which stabilize the anterior cruciate ligament posteriorly, are often minimally contracted during these injuries, particularly if the hip is extended and the body weight is on the heel, allowing for excessive forward shifting of the femur on the tibia 15. Examples of this type of noncontact injury include skiers or snowboarders whose ankles are locked when they fall backward onto the snow; soccer players who execute sudden cutting maneuvers; or basketball players who land on an internally rotated knee without full flexion 16.
Risk factors for anterior cruciate ligament injury
There are a number of factors that increase your risk of an ACL injury, including:
- Being female — possibly due to differences in anatomy, muscle strength and hormonal influences. Female athletes have been reported to sustain non-contact ACL injuries at a rate higher than their male counterparts. Recent studies indicate a 2 to 8 fold increase in females compared to similarly trained males 4, 5, 6, 7
- Participating in certain sports, such as soccer, football, basketball, gymnastics and downhill skiing
- Poor conditioning
- Using faulty movement patterns, such as moving the knees inward during a squat
- Wearing footwear that doesn’t fit properly 17
- Using poorly maintained sports equipment, such as ski bindings that aren’t adjusted properly
- Playing on artificial turf 18
Greatest predictors for anterior cruciate ligament injury include anterior knee laxity, increased body mass index (BMI) and family history 19. Additional factors may include biomechanical differences, increased posterior tibial slope, and hormones (with a greater proportion of injuries occurring in the follicular phase as compared to the luteal phase of the menstrual cycle) 20, 21, 22.
Other risk factors for ACL injury include inclement weather, intercondylar notch stenosis, variations in sagittal condylar shape, increased tibial slope, increased posterior slope, and potential genetic influence 23, 24.
Anterior cruciate ligament injury signs and symptoms
Signs and symptoms that you may notice at the time of ACL injury may include:
- A sudden “pop” sound or or a “popping” sensation in your knee
- Rapid swelling of the knee within minutes to hours of the injury. This is caused by bleeding into the knee
- Moderate to severe pain in your knee and inability to continue activity
- Loss of range of motion
Symptoms that may occur days to weeks after the ACL injury include:
- A feeling of instability or “giving way” with weight bearing: After the swelling improves you may feel a sense of ‘instability’ in the injured knee. This means the knee moves around too much and may lead to the knee giving way. This is often felt during activities such as squatting, walking down stairs, pivoting on the knee or stepping sideways.
- Ongoing knee pain
- Ongoing swelling (usually less severe than at the time of injury)
Seek immediate care if any injury to your knee causes signs or symptoms of an ACL injury. The knee joint is a complex structure of bones, ligaments, tendons and other tissues that work together. It’s important to get a prompt and accurate diagnosis to determine the severity of the injury and get proper treatment. Generally the longer you take to seek treatment the longer it will take to recover.
Types of ACL tears
About half of all injuries to the anterior cruciate ligament occur along with damage to other structures in the knee, such as articular cartilage, meniscus, or other ligaments.
Injured ligaments are considered “sprains” and are graded on a severity scale.
- Grade 1 Sprains. The ligament is mildly damaged in a Grade 1 Sprain. It has been slightly stretched, but is still able to help keep the knee joint stable.
- Grade 2 Sprains. A Grade 2 Sprain stretches the ligament to the point where it becomes loose. This is often referred to as a partial tear of the ligament.
- Grade 3 Sprains. This type of sprain is most commonly referred to as a complete tear of the ligament. The ligament has been split into two pieces, and the knee joint is unstable.
Partial tears of the anterior cruciate ligament are rare; most ACL injuries are complete or near complete tears.
Anterior cruciate ligament injury complications
A short term complication is that you will need to take it easy until your injured ligament has healed.
Other complications may include:
- Torn meniscus: As the ACL and meniscus are both structures in your knee which are quite close, if you injure one you may have injured the other. An injured meniscus can increase the risk of joint problems later on, however, evidence thus far has not yet supported meniscus repairs to minimize or delay the rate of osteoarthritis 25, 26, 27.
- Arthritis: People who experience an ACL injury have a higher risk of developing osteoarthritis in the knee. This is when your joint cartilage gets rough over time leaving it deficient. Osteoarthritis may occur even if you have surgery to reconstruct the anterior cruciate ligament. This is a very common complication that arises as a long term complication. About half the people with an ACL tear develop osteoarthritis in the involved joint 10 to 20 years later. Multiple factors likely influence the risk of arthritis, such as the severity of the original injury, the presence of related injuries in the knee joint or the level of activity after treatment.
Anterior cruciate ligament injury prevention
Proper training and exercise can help reduce the risk of ACL injury. A sports medicine physician, physical therapist, athletic trainer or other specialist in sports medicine can provide assessment, instruction and feedback that can help you reduce risks.
Programs to reduce ACL injury include:
- Exercises to strengthen the core — including the hips, pelvis and lower abdomen — with a goal of training athletes to avoid moving the knee inward during a squat
- Exercises that strengthen leg muscles, particularly hamstring exercises, to ensure an overall balance in leg muscle strength
- Training and exercise emphasizing proper technique and knee position when jumping and landing from jumps
- Training to improve technique when performing pivoting and cutting movements
Training to strengthen muscles of the legs, hips and core — as well as training to improve jumping and landing techniques and to prevent inward movement of the knee — may help to reduce the higher ACL injury risk in female athletes.
Gear
Wear footwear and padding that is appropriate for your sport to help prevent injury. If you downhill ski, make sure your ski bindings are adjusted correctly by a trained professional so that your skis will release appropriately if you fall.
Wearing a knee brace doesn’t appear to prevent ACL injury or reduce the risk of recurring injury after surgery.
Anterior cruciate ligament injury diagnosis
History and physical examination are important to diagnosing an ACL injury. Explaining to your doctor what movement caused your injury helps determine which part of your knee was damaged. It is common to hear or feel a “pop” at the time of injury.
During the physical exam, your doctor will check your knee for swelling and tenderness — comparing your injured knee to your uninjured knee. He or she may also move your knee into a variety of positions to assess range of motion and overall function of the joint.
Often the diagnosis of ACL tear can be made on the basis of the physical exam alone, but you may need tests to rule out other causes and to determine the severity of the injury. These tests may include:
- X-rays. X-rays may be needed to rule out a bone fracture. However, X-rays don’t show soft tissues, such as ligaments and tendons.
- Magnetic resonance imaging (MRI). An MRI uses radio waves and a strong magnetic field to create images of both hard and soft tissues in your body. An MRI can show the extent of an ACL injury and signs of damage to other tissues in the knee, including the cartilage.
- Ultrasound. Using sound waves to visualize internal structures, ultrasound may be used to check for injuries in the ligaments, tendons and muscles of the knee.
Evaluation of the anterior cruciate ligament should be performed immediately after an injury, if possible, but is often limited by swelling and pain. The evaluation should begin by observing the patient’s gait, as well as the position of comfort he or she assumes on the examination table. The physician should note any asymmetry, including loss of the peripatellar groove indicating an effusion, hemarthrosis, or both. In a study of 132 athletes with acute knee injury and hemarthrosis, 77 percent had a partial or complete tear of the anterior cruciate ligament 28.
A more subtle effusion can be detected by compressing the medial and superior aspects of the knee, then tapping the lateral aspect to create a fluid wave. The physician can also attempt to palpate the patella with suprapatellar compression, which will feel spongy if effusion is present.
When hemarthrosis is present, the increased intraarticular volume produces considerable pain on range of motion. This pain results in extensive guarding and spasm of the hamstring muscle group, further limiting the knee’s range of motion and making an accurate examination difficult. The patient may not be able to fully flex the knee, but the loss of hyperextension is more indicative of an anterior cruciate ligament disruption. The torn anterior cruciate ligament stump compressed between the tibia and femur, as well as the joint effusion, prevents full extension 29. Inability to achieve full extension also raises the possibility of a locked displaced meniscal tear.
If performed properly, a complete knee examination for anterior cruciate ligament injury can be highly accurate, with a sensitivity and specificity of 82 and 94 percent, respectively 30. The likelihood ratio is 25.0 for a positive examination and 0.04 for a negative examination.24 The three most accurate tests for detecting an anterior cruciate ligament tear are the Lachman test (sensitivity of 60 to 100 percent; mean 84 percent), the anterior drawer test (sensitivity of 9 to 93 percent; mean 62 percent), and the pivot shift test (sensitivity of 27 to 95 percent; mean 62 percent) 30.
A radiographic knee series, including anterior-posterior, lateral, tunnel, and sunrise views, should be the initial imaging study to assess for fractures, evaluate knee alignment, determine skeletal maturity, and identify degenerative changes in middleaged patients. Magnetic resonance imaging (MRI) is the primary study used to diagnose anterior cruciate ligament injury in the United States. It has the added benefit of identifying meniscal injury, collateral ligament tear, and bone contusions. Approximately 60 to 75 percent of anterior cruciate ligament injuries are associated with meniscal tears, up to 46 percent have collateral ligament injuries, and 5 to 24 percent are associated with complete tear of a collateral ligament 31. The sensitivity and specificity of MRI for detecting an anterior cruciate ligament tear is 86 and 95 percent, respectively, as confirmed on arthroscopy 32.
Anterior cruciate ligament injury treatment
If you have suffered an ACL injury, treatment depends on many factors, including the severity, your lifestyle, work, sport and age. Right after an ACL injury, an ACL tear is treated with the “RICE” therapy, which includes rest, ice, compression of the affected knee (with an elastic bandage), and elevation of the affected knee. For pain relief, you may need over-the-counter pain medicine such as acetaminophen (Tylenol or store brand) or ibuprofen (Advil, Motrin, or store brand).
ACL injuries can be managed nonoperatively or surgically. The patient with an anterior cruciate ligament injury should be referred to the orthopedic surgeon to discuss treatment options and a physical therapist for rehabilitation.
Most partial tears can be treated with bracing and physical therapy (PT). A person might need to use crutches as the tear heals.
Some complete ACL tears need surgery. The need for surgery depends on many things, including:
- the type of the activities (or sports) the person wants to do
- if the person is an athlete
- age
- other injuries to the knee
- if the knee “gives way” or feels unstable
Your expectations for knee function or performance may play a role in determining whether ACL reconstruction is needed. With an ACL tear, your knee is usually unstable. This instability may cause your knee to “give way” or feel unstable which will significantly influence knee function. A course of physical therapy may successfully treat an ACL injury for people who are relatively inactive, engage in moderate exercise and recreational activities, or play sports that put less stress on the knees.
If physiotherapy and the possibly the use of a special ACL brace do not improve the stability of the joint, your doctor may recommend surgical reconstruction. Your Sports physician will also consider whether there are additional knee injuries which make surgery necessary, such as a meniscal tear and discuss fully your options of treatment.
Anterior cruciate ligament tear first-aid care
Prompt first-aid care can reduce pain and swelling immediately after an ACL injury to your knee. Follow the R.I.C.E. model of self-care at home:
- Rest. General rest is necessary for healing and limits weight bearing on your knee.
- Ice. When you’re awake, try to ice your knee at least every two hours for 20 minutes at a time.
- Compression. Wrap an elastic bandage or compression wrap around your knee.
- Elevation. Lie down with your knee propped up on pillows.
Rehabilitation
With an ACL tear, your knee is usually unstable. This instability may cause your knee to “give way” or feel unstable which will significantly influence knee function. Medical treatment for an ACL injury begins with several weeks of rehabilitative therapy. A physical therapist will teach you exercises that you will perform either with continued supervision or at home. You may also wear a brace to stabilize your knee and use crutches for a while to avoid putting weight on your knee.
The goal of rehabilitation is to reduce pain and swelling, restore your knee’s full range of motion, and strengthen muscles. This course of physical therapy may successfully treat an ACL injury for individuals who are relatively inactive, engage in moderate exercise and recreational activities, or play sports that put less stress on the knees.
Properly supervised training, including “jump training” which teaches athletes how to jump and land properly can reduce serious knee ligament injuries by around 50%. Jump training includes plyometrics and should also include strength training of supporting muscles such as the hip and core muscles to round out the program. Plyometrics also known as jump training or plyos, is a type of exercise training that uses speed and force of different movements to build muscle power. Plyometrics training can improve your physical performance and ability to do different activities.
Anterior cruciate ligament reconstruction surgery
Before your surgery, you’ll likely undergo several weeks of physical therapy. The goal before surgery is to reduce pain and swelling, restore your knee’s full range of motion, and strengthen muscles. People who go into surgery with a stiff, swollen knee may not regain full range of motion after surgery.
When surgical treatment is indicated for an acute isolated ACL tear, early reconstruction is preferred because the risk of additional cartilage and meniscal injury starts to increase within 3 months 9. Furthermore, ACL tears indicated for surgery should be treated with ACL reconstruction rather than repair because of the lower risk of revision surgery 9.
Anterior cruciate ligament reconstruction is an outpatient surgery to replace a torn anterior cruciate ligament (ACL), so you’ll be able to go home the same day. Reconstruction of the anterior cruciate ligament involves replacing it with a substitute ligament. This substitute can come from a variety of sources, but the two most common are from your own hamstring tendons or patella tendon. ACL reconstruction is performed by a doctor who specializes in surgical procedures of the bones and joints (orthopedic surgeon).
Your doctor may recommend surgery if:
- You’re an athlete and want to continue in your sport, especially if the sport involves jumping, cutting or pivoting
- More than one ligament is injured
- You have a torn meniscus that requires repair
- The injury is causing your knee to buckle during everyday activities
- You’re young (though other factors, such as activity level and knee instability, are more important than age)
General anesthesia is typically used during ACL reconstruction, so you’ll be unconscious during the procedure. Anterior cruciate ligament reconstruction is usually done through small incisions — one to hold a thin, tube-like video camera and others to allow surgical instruments access to the joint space.
During ACL reconstruction, your surgeon will remove the torn anterior cruciate ligament and replaced it with a band of tissue that usually connects muscle to bone (tendon). This replacement tissue is called a graft and it comes from another part of your knee, the two most common are from your own hamstring tendons or patella tendon or a tendon from a deceased donor.
Your surgeon will drill sockets or tunnels into your thighbone and shinbone to accurately position the graft, which is then secured to your bones with screws or other devices. The graft will serve as scaffolding on which new ligament tissue can grow.
Who may not need surgery?
- If you do not participate in sporting activities and do not have symptoms of instability (the knee giving way), then you may not need an ACL reconstruction.
- Alternatives non-surgical treatment options include:
- Activity modification – avoiding sporting or work related activities that require pivoting
- Physiotherapy for strength, balance, range of motion training and further injury prevention
Anterior cruciate ligament reconstruction risks and complications
ACL reconstruction is a surgical procedure. And, as with any surgery, bleeding and infection at the surgical site are potential risks. Other risks associated with ACL reconstruction include:
- Knee pain or stiffness
- Poor healing of the graft
- Graft failure after returning to sport
Complications are problems that occur during the operation or after the operation. Most people DO NOT have complications. There are some complications that may occur for any operation. These include:
- A reaction to the anaesthetic
- Infection of the wound or joint
- Excessive blood loss
- A blood clot, usually in a vein of the leg (known as a deep vein thrombosis or DVT)
Complications that are specific for ACL reconstructive surgery include:
- Tearing or ‘failure’ of the repaired cruciate ligament: Sometimes the repaired ligament may be torn and the original problem returns. Depending on the type of activities you perform after your operation and the extent of the original injury you may be at a greater or lesser risk of this occurring.
- Pain in the front of the knee: After an ACL reconstruction you may have ongoing pain in the front of the knee. The pain may be particularly felt when kneeling. Pain in the front of the knee is more common in people who have had the patella tendon used as the graft for their surgery
- Knee stiffness: After an ACL reconstruction, the knee may be stiffer than before the operation. It is important to complete the rehabilitation recommended by your physiotherapist in order to get the best outcome.
- Instability: Although the aim of the ACL reconstruction is to make the knee strong and stable, sometimes the replaced tendon may stretch which can lead to instability of the knee. This may lead to pain or giving way of the knee.
- Nerve damage: You may be left with an area of numbness on the inner side of your leg after the ACL reconstruction. This may be permanent or may improve slowly after the surgery.
- Fracture of surrounding bones (broken bones): A very rare complication of ACL reconstruction is a fracture in the tibia (leg bone) or femur (thigh bone). This is a very rare complication relating to the site of the graft insertion or where the graft was taken from.
If the ACL reconstruction tears, you may need to have another ACL reconstruction. A second ACL reconstruction does not last as well as the first one and can be torn more easily than the first one.
Anterior cruciate ligament reconstruction surgery recovery
Once you recover from the anesthesia, you can go home the same day. Before you go home, you’ll practice walking with crutches, and your surgeon may ask you to wear a knee brace or splint to help protect the graft. Follow your surgeon’s advice on when to ice your knee, how long to use crutches and when it’s safe to bear weight on your knee. You’ll also be told when you can shower or bathe, when you should change dressings on the wound, and how to manage post-surgery care.
Your doctor will ask you to rest when you first go home. You will be told to:
- Keep your leg propped up on 1 or 2 pillows. Place the pillows under your foot or calf muscle. This helps keep swelling down. Do this 4 to 6 times a day for the first week after surgery. Do not put the pillow behind your knee. Keep your knee straight.
- Be careful not to get the dressing on your knee wet.
- Apply a cold wrap or ice to your knee, but do not use a heating pad.
- Medications to help with pain relief include over-the-counter drugs such as acetaminophen (Tylenol), ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve). Your doctor might prescribe stronger medications, such as meloxicam (Mobic), tramadol (Ultram, Qdolo, ConZip) or oxycodone (OxyContin, Roxicodone, others). If opioids are prescribed, they should be taken only for breakthrough pain as they have many side effects and a significant risk of addiction.
You may need to wear special support stockings to help prevent blood clots from forming. Your doctor will also give you exercises to keep the blood moving in your foot, ankle, and leg. These exercises will also lower your risk for blood clots.
You may be able to begin putting your full weight on your repaired leg without crutches 2 to 3 weeks after surgery, if your surgeon says it is OK. If you had work on your knee in addition to ACL reconstruction, it may take 4 to 8 weeks to regain full use of your knee. Ask your surgeon how long you will need to be on crutches.
You may also need to wear a special knee brace. The brace will be set so that your knee can move only a certain amount in any direction. Do not change the settings on the brace yourself.
- Ask your doctor or physical therapist about sleeping without the brace and removing it for showers.
- When the brace is off for any reason, be careful not to move your knee more than you can when you have the brace on.
You will need to learn how to go up and down stairs using crutches or with a knee brace on.
Physical therapy most often begins about 1 to 2 weeks after surgery to strengthen the muscles around your knee and improve flexibility, however you can do some simple postoperative knee exercises immediately after surgery. A physical therapist will teach you how to do exercises that you will perform either with continued supervision or at home. The duration of physical therapy may last 2 to 6 months. You will need to limit your activity and movement while your knee mends. Your physical therapist will give you an exercise program to help you build strength in your knee and avoid injury. Following the rehabilitation plan is important for proper healing and achieving the best possible outcomes.
- Staying active and building strength in the muscles of your legs will help speed your recovery.
- Getting full range of motion in your leg soon after surgery is also important.
Successful ACL reconstruction paired with focused rehabilitation can usually restore stability and function to your knee. Within the first few weeks after surgery, you should strive to regain a range of motion equal to that of your opposite knee. Recovery generally takes about nine months.
It may take eight to 12 months or more before athletes can return to their sports.
Anterior cruciate ligament injury prognosis
Return to activity is variable and patient-dependent 33. ACL injuries can be managed nonoperatively or surgically. The patient with an anterior cruciate ligament injury should be referred to the orthopedic surgeon to discuss treatment options and a physical therapist for rehabilitation.
Most partial tears can be treated with bracing and physical therapy (PT). A person might need to use crutches as the tear heals.
Some complete ACL tears need surgery. The need for surgery depends on many things, including:
- the type of the activities (or sports) the person wants to do
- if the person is an athlete
- age
- other injuries to the knee
- if the knee “gives way” or feels unstable
Your expectations for knee function or performance may play a role in determining whether ACL reconstruction is needed. With an ACL tear, your knee is usually unstable. This instability may cause your knee to “give way” or feel unstable which will significantly influence knee function. A course of physical therapy may successfully treat an ACL injury for people who are relatively inactive, engage in moderate exercise and recreational activities, or play sports that put less stress on the knees.
If physiotherapy and the possibly the use of a special ACL brace do not improve the stability of the joint, your doctor may recommend surgical reconstruction. Your Sports physician will also consider whether there are additional knee injuries which make surgery necessary, such as a meniscal tear and discuss fully your options of treatment.
Your doctor may recommend surgery if:
- You’re an athlete and want to continue in your sport, especially if the sport involves jumping, cutting or pivoting
- More than one ligament or the fibrous cartilage in your knee also is injured
- The injury is causing your knee to buckle during everyday activities
The average return to full activity and/or sports participation is estimated to be between 6 to 12 months after surgical reconstruction, depending upon their progress with physical therapist and the type of sport/activity to which they are returning. However, some studies have shown up to 18 months or more for the graft to become fully functional and incorporated. Early/premature return to activity can lead to re-injury and graft failure.
References- Beynnon BD, Vacek PM, Newell MK, Tourville TW, Smith HC, Shultz SJ, Slauterbeck JR, Johnson RJ. The Effects of Level of Competition, Sport, and Sex on the Incidence of First-Time Noncontact Anterior Cruciate Ligament Injury. Am J Sports Med. 2014 Aug;42(8):1806-12. doi: 10.1177/0363546514540862
- Management of anterior cruciate ligament Injuries: Clinical Practice Guideline from the AAOS. Am Fam Physician. 2015 Aug 1;92(3):232-234. https://www.aafp.org/afp/2015/0801/p232.html
- Mattu AT, Ghali B, Linton V, Zheng A, Pike I. Prevention of Non-Contact Anterior Cruciate Ligament Injuries among Youth Female Athletes: An Umbrella Review. Int J Environ Res Public Health. 2022 Apr 12;19(8):4648. doi: 10.3390/ijerph19084648
- Agel J, Arendt EA, Bershadsky B. Anterior cruciate ligament injury in national collegiate athletic association basketball and soccer: a 13-year review. Am J Sports Med. 2005 Apr;33(4):524-30. doi: 10.1177/0363546504269937
- Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am J Sports Med. 1995 Nov-Dec;23(6):694-701. doi: 10.1177/036354659502300611
- Gornitzky AL, Lott A, Yellin JL, Fabricant PD, Lawrence JT, Ganley TJ. Sport-Specific Yearly Risk and Incidence of Anterior Cruciate Ligament Tears in High School Athletes: A Systematic Review and Meta-analysis. Am J Sports Med. 2016 Oct;44(10):2716-2723. doi: 10.1177/0363546515617742
- Vacek PM, Slauterbeck JR, Tourville TW, Sturnick DR, Holterman LA, Smith HC, Shultz SJ, Johnson RJ, Tourville KJ, Beynnon BD. Multivariate Analysis of the Risk Factors for First-Time Noncontact ACL Injury in High School and College Athletes: A Prospective Cohort Study With a Nested, Matched Case-Control Analysis. Am J Sports Med. 2016 Jun;44(6):1492-501. doi: 10.1177/0363546516634682
- Benjaminse A, Webster KE, Kimp A, Meijer M, Gokeler A. Revised Approach to the Role of Fatigue in Anterior Cruciate Ligament Injury Prevention: A Systematic Review with Meta-Analyses. Sports Med. 2019 Apr;49(4):565-586. doi: 10.1007/s40279-019-01052-6
- American Academy of Orthopaedic Surgeons Management of Anterior Cruciate Ligament Injuries Evidence-Based Clinical Practice Guideline www.aaos.org/aclcpg Published August 22, 2022. https://www.aaos.org/globalassets/quality-and-practice-resources/anterior-cruciate-ligament-injuries/aclcpg.pdf
- Boden BP, Dean GS, Feagin JA Jr, Garrett WE Jr. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000 Jun;23(6):573-8. doi: 10.3928/0147-7447-20000601-15
- Boden BP, Sheehan FT, Torg JS, Hewett TE. Noncontact anterior cruciate ligament injuries: mechanisms and risk factors. J Am Acad Orthop Surg. 2010 Sep;18(9):520-7. doi: 10.5435/00124635-201009000-00003
- Agel J, Olson DE, Dick R, Arendt EA, Marshall SW, Sikka RS. Descriptive epidemiology of collegiate women’s basketball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007 Apr-Jun;42(2):202-10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1941290/
- Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes: Part 1, mechanisms and risk factors. Am J Sports Med. 2006;34(2):299–311.
- Shimokochi Y, Shultz SJ. Mechanisms of noncontact anterior cruciate ligament injury. J Athl Train. 2008;43(4):396–408
- Alentorn-Geli E, Myer GD, Silvers HJ, et al. Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 1: Mechanisms of injury and underlying risk factors. Knee Surg Sports Traumatol Arthrosc. 2009;17(7):705–729.
- Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8(3):141–150.
- Serpell BG, Scarvell JM, Ball NB, Smith PN. Mechanisms and risk factors for noncontact ACL injury in age mature athletes who engage in field or court sports: a summary of the literature since 1980. J Strength Cond Res. 2012 Nov;26(11):3160-76. doi: 10.1519/JSC.0b013e318243fb5a
- Balazs GC, Pavey GJ, Brelin AM, Pickett A, Keblish DJ, Rue JP. Risk of Anterior Cruciate Ligament Injury in Athletes on Synthetic Playing Surfaces: A Systematic Review. Am J Sports Med. 2015 Jul;43(7):1798-804. doi: 10.1177/0363546514545864
- Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med. 2003 Nov-Dec;31(6):831-42. doi: 10.1177/03635465030310061801
- Somerson JS, Isby IJ, Hagen MS, Kweon CY, Gee AO. The Menstrual Cycle May Affect Anterior Knee Laxity and the Rate of Anterior Cruciate Ligament Rupture: A Systematic Review and Meta-Analysis. JBJS Rev. 2019 Sep;7(9):e2. doi: 10.2106/JBJS.RVW.18.00198
- Herzberg SD, Motu’apuaka ML, Lambert W, Fu R, Brady J, Guise JM. The Effect of Menstrual Cycle and Contraceptives on ACL Injuries and Laxity: A Systematic Review and Meta-analysis. Orthop J Sports Med. 2017 Jul 21;5(7):2325967117718781. doi: 10.1177/2325967117718781
- Balachandar V, Marciniak JL, Wall O, Balachandar C. Effects of the menstrual cycle on lower-limb biomechanics, neuromuscular control, and anterior cruciate ligament injury risk: a systematic review. Muscles Ligaments Tendons J. 2017 May 10;7(1):136-146. doi: 10.11138/mltj/2017.7.1.136
- Pfeifer CE, Beattie PF, Sacko RS, Hand A. RISK FACTORS ASSOCIATED WITH NON-CONTACT ANTERIOR CRUCIATE LIGAMENT INJURY: A SYSTEMATIC REVIEW. Int J Sports Phys Ther. 2018 Aug;13(4):575-587. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6088120/
- Bayer S, Meredith SJ, Wilson KW, de Sa D, Pauyo T, Byrne K, McDonough CM, Musahl V. Knee Morphological Risk Factors for Anterior Cruciate Ligament Injury: A Systematic Review. J Bone Joint Surg Am. 2020 Apr 15;102(8):703-718. doi: 10.2106/JBJS.19.00535. Erratum in: J Bone Joint Surg Am. 2020 Jul 15;102(14):e85.
- Hoshino T, Nakagawa Y, Inomata K, Ohara T, Katagiri H, Otabe K, Hiyama K, Katagiri K, Katakura M, Ueki H, Hayashi M, Nagase T, Sekiya I, Ogiuchi T, Muneta T, Koga H; Tokyo Medical and Dental University (TMDU) Multicenter Arthroscopic Knee Surgery (MAKS) Group. Effects of different surgical procedures for meniscus injury on two-year clinical and radiological outcomes after anterior cruciate ligament reconstructions. -TMDU MAKS study. J Orthop Sci. 2022 Jan;27(1):199-206. doi: 10.1016/j.jos.2020.12.010
- Eken G, Misir A, Demirag B, Ulusaloglu C, Kizkapan TB. Delayed or neglected meniscus tear repair and meniscectomy in addition to ACL reconstruction have similar clinical outcome. Knee Surg Sports Traumatol Arthrosc. 2020 Nov;28(11):3511-3516. doi: 10.1007/s00167-020-05931-8
- Cristiani R, Mikkelsen C, Edman G, Forssblad M, Engström B, Stålman A. Age, gender, quadriceps strength and hop test performance are the most important factors affecting the achievement of a patient-acceptable symptom state after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020 Feb;28(2):369-380. doi: 10.1007/s00167-019-05576-2
- Hardaker WT Jr, Garrett WE Jr, Bassett FH III. Evaluation of acute traumatic hemarthrosis of the knee joint. South Med J. 1990;83(6):640–644.
- Shelbourne KD, Rowdon GA. Anterior cruciate ligament injury. The competitive athlete. Sports Med. 1994;17(2):132–140.
- Solomon DH, et al. The rational clinical examination. Does this patient have a torn meniscus or ligament of the knee? Value of the physical examination. JAMA. 2001;286(13):1610–1620.
- Spindler KP, Wright RW. Clinical practice. Anterior cruciate ligament tear. N Engl J Med. 2008;359(20):2135–2142.
- Crawford R, et al. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull. 2007;84:5–23.
- Evans J, Nielson Jl. Anterior Cruciate Ligament Knee Injuries. [Updated 2022 May 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499848