Anti-GBM disease
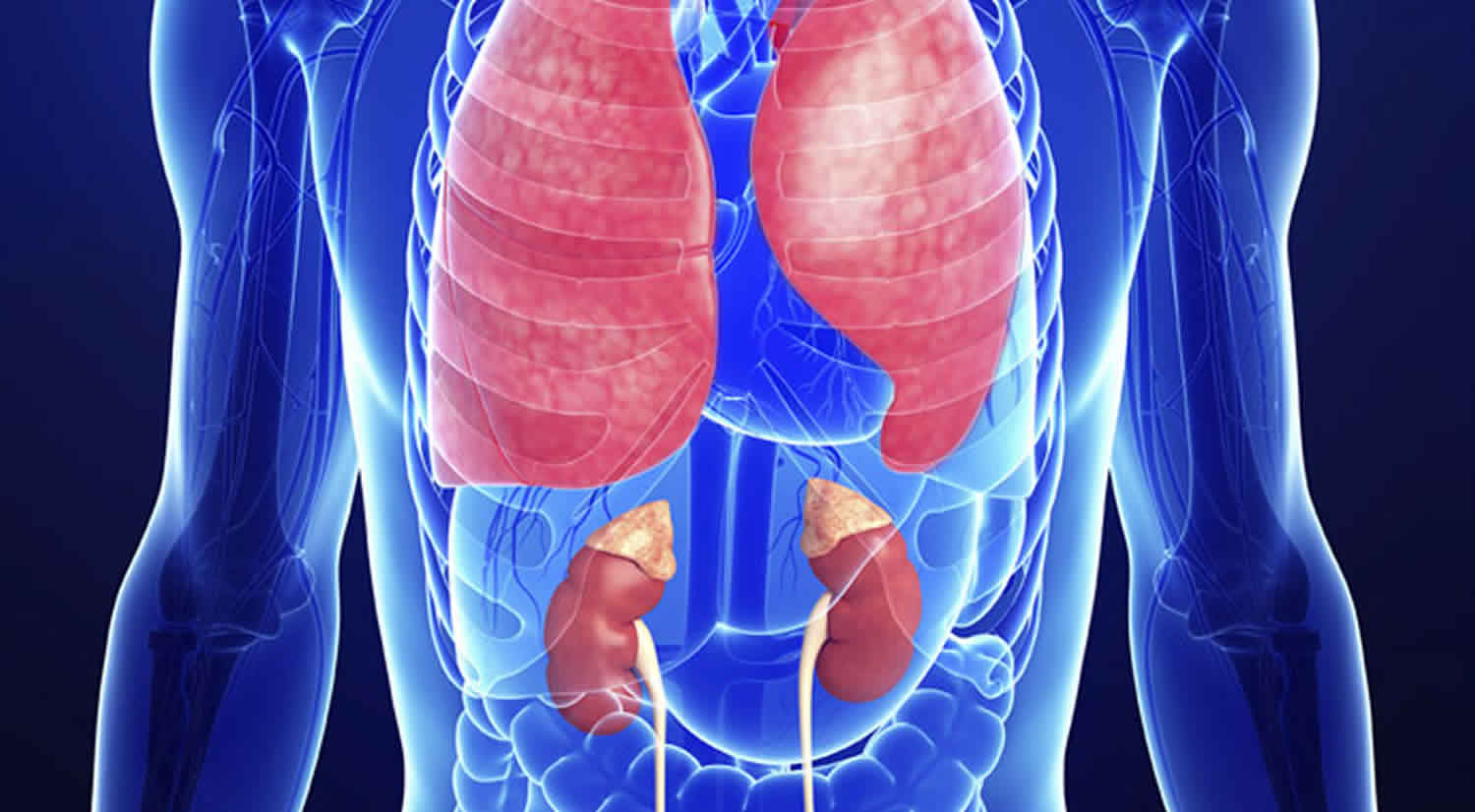
Anti-GBM disease short for anti–glomerular basement membrane antibody disease, is a rare autoimmune disorder in which circulating antibodies are directed against an antigen normally present in the glomerular basement membrane (GBM) and alveolar basement membrane 1. The target antigen is the alpha-3 chain of type IV collagen. The resultant clinical syndrome encompasses a spectrum ranging from mild or no renal involvement to rapidly progressive glomerulonephritis 2. The pathologic hallmark is linear staining of GBMs (glomerular basement membranes) for deposited immunoglobulin G (IgG), usually accompanied by serum autoantibodies to the collagen IV alpha-3 constituents of GBMs 3. Tissue injury typically manifests as diffuse necrotizing and crescentic glomerulonephritis 4.
About 20-40% of anti-GBM disease have only kidney involvement, which is called “renal limited” anti-GBM disease or anti-GBM glomerulonephritis. This is a form of inflammation, which is injury to tissue caused by white blood cells (leukocytes). Glomerulonephritis due to Anti-GBM antibody disease is rare. It occurs in less than 1 case per million persons. It affects mostly young, white men aged 15-35. After age 50, women are more likely to be affected. The sexes overall are affected approximately at a male-female ratio of 3:2. Anti-GBM disease is seen very rarely in children 5.
About 50% of anti-GBM disease patients develop pulmonary hemorrhage, and most individuals have signs of a generalized systemic illness 3. Anti-glomerular basement membrane (anti-GBM) disease with the combination of glomerulonephritis and pulmonary hemorrhage is commonly referred to as Goodpasture syndrome 6. Pulmonary and/or renal manifestations can be encountered in various conditions, such as antineutrophilic cytoplasmic antibody (ANCA)–positive vasculitis and other autoimmune disorders. As a consequence, the identification of anti-GBM antibodies in the patient’s serum or tissues is of paramount importance in the diagnosis of Goodpasture disease. However, some clinicians may use several terms interchangeably, including anti-GBM disease (anti-glomerular basement membrane disease), Goodpasture syndrome, and Goodpasture disease 7. The latter is the most specific term, and refers to the presence of renal and pulmonary involvement, along with anti-glomerular basement membrane antibodies. Symptoms may include chills and fever, nausea and vomiting, weight loss, chest pain, bleeding may cause anemia, respiratory failure, and kidney failure.
Anti-GBM antibodies can be demonstrated in serum with conventional enzyme-linked immunosorbent assay (ELISA) in 87–90% of patients 4. Given the intensity of the renal injury, most patients present with markedly elevated serum creatinine, blood in urine (hematuria) and active urine sediment with or without pulmonary hemorrhage. These features may be preceded by malaise and a viral-like prodrome 3.
Patients presenting with Goodpasture syndrome (both glomerulonephritis and pulmonary hemorrhage) may be critically ill on presentation. Hospitalization is required for prompt diagnosis and treatment, close monitoring, and supportive care in patients with anti-glomerular basement membrane (GBM) antibody disease. Treatment of anti-GBM disease is focused on removing the anti-GBM antibody from the blood.
The treatment of choice is plasmapheresis in conjunction with prednisone and cyclophosphamide. The three main goals for the treatment are:
- Rapidly remove circulating antibody, primarily by plasmapheresis.
- Stop further production of antibodies using immunosuppression with medications, namely, corticosteroids (e.g., prednisone) and cyclophosphamide. In children, plasmapheresis is done together with corticosteroids and cyclophosphamide. The duration of the immunosuppressive treatment varies but is typically 6 months for corticosteroids and 3 months for cyclophosphamide.
- Remove offending agents that may have initiated the antibody production.
If the person smokes, it is recommended he or she stop. Also, if the patient is exposed to hydrocarbon in his or her occupation, he or she should consider changing jobs, as exposure to hydrocarbon has been shown to increase a person’s chances of disease recurrence.
Upon diagnosis, patients should be started on prednisone, cyclophosphamide, and daily plasmapheresis to improve overall mortality in general, and renal survival in particular. If therapy can start before the patient progresses to the point of needing renal replacement therapy, the overall renal prognosis is better. All patients with pulmonary symptoms should be started on combined therapy regardless of their renal status. For patients, without pulmonary symptoms in whom renal recovery is very unlikely (i.e., for those that presented with the urgent need for dialysis within the first 72 hours) the risk of plasmapheresis and immunosuppressive may outweigh the benefits. The choice to withhold treatment in these cases remains controversial as the disease has not been well-studied in controlled trials, and it remains difficult to predict who in this group exactly will respond and recover renal function. Overall return of renal function in this group is approximately 8%, yet many clinicians still opt for a trial of aggressive combined therapy at this time.
Typically, daily plasmapheresis is performed until anti-glomerular basement membrane antibodies are undetectable, with steroid and cyclophosphamide continuing after that for 3 to 6 months until full remission is achieved. This can be gauged by checking repeated titers following plasmapheresis, as well as any time new symptoms develop that could be a harbinger of relapse. Overall, relapse remains rare.
After hospital discharge, patients require long-term regular visits for monitoring kidney function and for immunosuppressive therapy. If kidney function does not return, dialysis is continued indefinitely and the patient should be referred for kidney transplantation.
Anti GBM disease causes
Anti-GBM disease is an autoimmune condition of known pathogenesis but unclear cause. Some evidence suggests that genetics may play an important role in this disease. At this point, a triggering stimulus has not been identified for the development of anti-glomerular basement membrane antibodies. However, there are certain human leukocyte antigen (HLA) subtypes that have been implicated in conferring increased genetic susceptibility to Goodpasture syndrome, most notably HLA-DR15 8.
In autoimmune disorders, the body makes antibodies that attacks its own tissues. In the case of Goodpasture syndrome, antibodies form against a certain type of protein called collagen. Collagen is present in many tissues in the body. In Goodpasture syndrome, collagen in the alveoli (tiny air sacs in the lungs) and in the glomeruli (the filtering units of the kidney) is attacked. This leads to bleeding in the air sacs and inflammation in the glomeruli of the kidney. Symptoms of the antibody attack may include shortness of breath, cough, bloody sputum, blood and protein in the urine, and kidney failure 9.
Genetic predisposition to Goodpasture syndrome involves the human leukocyte antigen (HLA) system. The HLA system is involved in helping your immune system know the difference between “self” and “non-self.” Human leukocyte antigens determine a person’s tissue type. Each person has 3 pairs of major HLA antigens. You inherit one set from each of your parents (and pass one of your two sets on to each of your children) 10.
Some facts regarding HLA antigens and Goodpasture syndrome:
- A certain HLA antigen, HLA-DR15 (previously known as HLA-DR2), is found in 88% of patients with Goodpasture syndrome, as compared to 25-32% of those without it.
- People with Goodpasture syndrome who have two types of HLA antigens: HLA-B8 and HLA-DR2 tend to have a worse prognosis.
- HLA antigen types HLA-DR7 and HLA-DR1 are thought to confer some protection against developing Goodpasture syndrome.
Several factors play a permissive role in anti GBM disease initiation 11:
- Respiratory infections (eg, influenza) or inhaled toxins (eg, hydrocarbons, gasoline vapors, hypercarbic oxygen, tobacco, hairspray) may trigger pulmonary involvement.
- Factors associated with renal manifestations are renal injury from ischemia, membranous glomerulonephritis, and, possibly, extracorporeal shock-wave lithotripsy. Only 3 cases of anti-GBM disease occurring after lithotripsy have been described, although several million procedures have been performed. Therefore, the number of cases is too small to establish a causative association. However, consider testing for anti-GBM antibodies when patients have declining renal function after lithotripsy.
- Individuals with Alport syndrome lack the Goodpasture epitopes. The transplantation of a kidney from a healthy donor to a patient with an Alport syndrome introduces the Goodpasture epitopes as neoantigens. Approximately 50% of kidney recipients with Alport syndrome develop anti-GBM antibodies; only a few of these patients have graft failure because of anti-GBM disease.
- In a review of 118 male patients with the X-linked dominant form of Alport syndrome, anti-GBM glomerulonephritis developed in only 3 (2.5%) 12. All had a large deletion in the COLA4A5 gene. Sixteen other patients with a large rearrangement in COLA4A5 and 32 with a small mutation that was expected to produce a truncated alpha-5 (type IV collagen) protein lacking the NC1 domain did not develop anti-GBM glomerulonephritis in the graft.
- In some patients, the anti-GBM antibody has immunoblotting characteristics different from those of patients with the primary form of Goodpasture syndrome. These characteristics may result from differences in antigenic expression caused by the interaction of the various alpha chains in the basement membrane. This difference also may explain why the clinical expression of the disease is milder in patients with Alport syndrome than in those with the primary form of Goodpasture syndrome. The low incidence of the syndrome and its mild clinical manifestations make renal transplantation the treatment of choice for patients with Alport syndrome who have end-stage renal disease.
- Anti-GBM antibody disease has a strong positive association with the HLA-DR15 haplotype, particularly the DRB1*1501 allele, which is found in more that 80% of patients with anti-GBM antibody disease. Furthermore, a strong dominant protection from the disease is associated with the expression of DRB1*0701 such that individuals inheriting DRB1*1501 and DRB1*0701 have no higher risk of disease than does the general population. The DRB1*01 allele offers relatively weak protection.
People who smoke or use hair dyes appear to be at increased risk for Goodpasture syndrome. Exposure to hydrocarbon fumes, metallic dust, and certain drugs, such as cocaine, may also raise a person’s risk. Genetics may also play a part, as a small number of cases have been reported in more than one family member.
Goodpasture syndrome is due to circulating auto-antibodies directed at the glomerular basement membrane. The resulting crescentic glomerulonephritis is the result of the antigen-antibody complexes that form at the basement membrane 13. The inflammatory response in that area results in the typical glomerulonephritis clinical picture.
Alveolar basement membrane shares the same collagen target as that of the glomerulus. Despite the presence of circulating antibodies in anti-glomerular basement membrane disease, pulmonary symptoms are not always observed. An inciting lung injury seems to make pulmonary symptoms more likely.
Anti GBM disease symptoms
Anti GBM disease signs and symptoms related to the kidney disease may include 14:
- Blood in urine (hematuria)
- Protein in urine (proteinuria)
- Abnormal kidney function
- Hypertension (high blood pressure) can be present but is not very common (reported in 4-17% of adult patients and very rare in children)
Anti GBM disease signs and symptoms related to the lung disease may include 14:
- Bleeding from the nose (hemoptysis), which occur before the kidney disease in about two thirds of cases and is present in 82%-90% of the adults
- Cough (40%-60% of the cases)
- Breathing difficulty (dyspnea) in about 57%-72% of the cases
- Pallor (the most common clinical sign)
- Crackles and rhonchi (low-pitched, rattling sound)
- Heart murmur (20-25% of the cases)
- Enlarged liver (hepatomegaly)
- Edema
Prompt diagnosis of pulmonary hemorrhage is vital because it is the principal cause of early death in patients with anti-GBM antibody disease.
Patients with anti-glomerular basement membrane antibody syndrome will initially present similarly to other forms of rapidly progressive glomerulonephritis with acute renal failure 6. There are no symptoms specific to anti-glomerular basement membrane that distinguish it from other diseases causing similar organ dysfunction, and careful and expedient workup must be undertaken for accurate diagnosis. The pulmonary symptoms are typically present at the time of the initial encounter, or shortly after that. Hemoptysis of varying degrees is typical when there is pulmonary involvement, ranging from serious and life-threatening bleeding to more subtle diffuse hemorrhage that is only apparent on more careful evaluation. It is more typical for younger patients affected by the anti-glomerular basement membrane disease to present with simultaneous renal and pulmonary symptoms (Goodpasture syndrome) and to be critically ill on presentation. Patients over 50 years old tend to present with glomerulonephritis alone and follow a less severe course.
Careful physical examination of patients presenting with finding suspicious for the anti-glomerular basement membrane disease should be done, particularly for other signs such as a purpuric rash. This finding may suggest so-called “double-positive” patients who have concurrent ANCA-associated vasculitis (granulomatosis with polyangiitis).
Anti GBM disease diagnosis
A kidney biopsy is the gold standard for diagnosis but is not required either to begin treatment or to continue treatment if a biopsy is not feasible 6. When performed, biopsy provides important information regarding the activity and chronicity of renal involvement that may help guide therapy. However, some doctors recommend doing a kidney biopsy in all cases while others suggest only doing the biopsy when the diagnosis is still in doubt. Light microscopy usually shows a feature known as crescentic glomerulonephritis, whereas immunofluorescence microscopy demonstrates a finding that is characteristic of this disease, of “linear deposition of IgG along the glomerular capillaries”. Patients in whom the diagnosis of lung hemorrhage is still unclear should have bronchoscopy 15.
In children, the most consistent feature is ‘crescentic glomerulonephritis’ with either circulating anti-GBM antibodies or linear staining of IgG on the immunofluorescence. Clinical features include severe kidney malfunction in all patients and lung hemorrhage in half of them.
It is essential to promptly diagnose pulmonary hemorrhage because this is the principal cause of early death when untreated 15.
Conditions that affect the lung and kidney (pulmonary-renal syndromes) are important to consider and need to be ruled out when the diagnosis is not confirmed. These include granulomatosis with polyangiitis (Wegener granulomatosis), Churg-Strauss syndrome, systemic lupus erythematosus, microscopic polyangiitis, rheumathoid arthritis, IgA-mediated disorders (eg, IgA nephropathy or Henoch-Schönlein purpura) and of immune complex–mediated renal disease (eg, essential mixed cryoglobulinemia), community-acquired pneumonia and undifferentiated connective-tissue disease 14. In children, other diseases that also need to be ruled out are Behcet Syndrome, hemosiderosis (bleeding into the lung and iron accumulation) and Legionella infection 14.
Anti GBM blood test
Serologic testing for ELISA assay for circulating anti-GBM antibodies should be done immediately on suspicion of the disease. Specifically, it is important that the alpha3 NC1 domain area of collagen IV be used as the target in this assay as false positives may be seen in less specific testing 16. Quantitative titers are followed during treatment phases to guide treatment decisions.
The presence of anti-GBM antibodies is pathognomonic. Detection of the anti-GBM antibodies is achieved by means of direct enzyme-linked immunoassay (ELISA). This test can be performed with less than 1 mL of blood. ELISA requires the use of native or recombinant human alpha-3 (type IV collagen) NC1 antigen as a substrate, which makes this method more sensitive and specific than others.
The specificity of the antibody can be confirmed with Western blotting.
False-negative rates are less than 5% and may occur in patients with low anti-GBM antibody titers or in some patients with Alport syndrome who develop anti-GBM disease after transplantation. A false-positive rate of less than 1% is related to the detection of antibodies directed against other chains of type IV collagen.
Indirect immunofluorescent staining is rarely performed and requires an experienced renal pathologist. This test is performed by incubating normal renal tissue with the patient’s serum and then treating it with fluorescein-labeled anti–IgG. Immunofluorescence indicates of immunoglobulin G (IgG) deposition and is diagnostic. False-negative results are seen in 10-40% of patients.
Other tests
Serum electrolytes and renal function
Renal function ranges from normal to rapidly deteriorating over a few weeks to months. Doubling of the serum creatinine level and halving of the glomerular filtration rate (GFR) within 3 months indicates rapidly progressive glomerulonephritis.
Electrolyte abnormalities, such as hyponatremia, hyperkalemia, hyperphosphatemia, and acidemia, may be seen with advanced disease.
Urine
Gross or microscopic hematuria may be present.
Urinalysis may reveal nephritic urinary sediment with dysmorphic RBCs and RBC casts.
Proteinuria is usually present, but protein levels are not in the nephrotic range.
Blood cells
A CBC count may reveal hypochromic microcytic anemia secondary to iron deficiency.
Mild thrombocytopenia may be detected.
Complements
The C3 level is below the reference range in 30-80% of pediatric patients.
Sputum: Hemosiderin-laden macrophages indicate pulmonary hemorrhage.
Antineutrophilic cytoplasmic antibodies (ANCA)
ANCA are autoantibodies directed against constituents of the primary granules of neutrophils and the peroxidase positive lysosomes of monocytes.
ANCA is detectable in as many as 30% of patients with anti-GBM disease. Titers of ANCA and anti-GBM antibodies tend to be inversely related.
The detection of ANCA is clinically relevant in anti-GBM disease because patients with this disease are more likely to respond to therapy.
Besides having prognostic value in anti-GBM disease, ANCA is an important diagnostic marker in the ANCA associated small-vessel vasculitis, such as Wegener granulomatosis, microscopic polyangiitis, Churg-Strauss syndrome, and some forms of drug-induced vasculitis (eg, thiouracil). These conditions are included in the differential diagnosis of anti-GBM disease. Therefore, patients presenting with acute glomerulonephritis with or without pulmonary hemorrhage are routinely tested for ANCA.
Imaging Studies
- Renal ultrasonography usually reveals kidneys of normal size, with no anatomic abnormalities.
- When pulmonary hemorrhage is present, chest radiography may reveal alveolar infiltrates spreading from the hilum.
- Chest CT scanning is more accurate than chest radiography for the diagnosis of pulmonary hemorrhage.
Anti GBM disease treatment
Hospitalization is required for prompt diagnosis and treatment, close monitoring, and supportive care in patients with anti-glomerular basement membrane (GBM) antibody disease. Patients may initially require intensive care.
The therapeutic regimen depends on the patient’s potential to respond.
- Patients with moderate glomerulonephritis (serum creatinine level < 5 mg/dL and crescents in < 50-75% of glomeruli) and patients with acute disease (brief illness, lack of chronicity on histology) are likely to respond to therapy. The treatment of choice consists of daily plasmapheresis combined with glucocorticosteroids and cyclophosphamide.
- If therapy can start before the patient progresses to the point of needing renal replacement therapy, the overall renal prognosis is better 6. All patients with pulmonary symptoms should be started on combined therapy regardless of their renal status. For patients, without pulmonary symptoms in whom renal recovery is very unlikely (i.e., for those that presented with the urgent need for dialysis within the first 72 hours) the risk of plasmapheresis and immunosuppressive may outweigh the benefits. The choice to withhold treatment in these cases remains controversial as the disease has not been well-studied in controlled trials, and it remains difficult to predict who in this group exactly will respond and recover renal function. Overall return of renal function in this group is approximately 8%, yet many clinicians still opt for a trial of aggressive combined therapy at this time.
- Typically, daily plasmapheresis is performed until anti-glomerular basement membrane antibodies are undetectable, with steroid and cyclophosphamide continuing after that for 3 to 6 months until full remission is achieved. This can be gauged by checking repeated titers following plasmapheresis, as well as any time new symptoms develop that could be a harbinger of relapse. Overall, relapse remains rare.
- Patients with advanced disease (serum creatinine level >5 mg/dL and crescents in >75% of glomeruli) and histologic signs of chronicity are unlikely to improve with any therapy and should be spared the clinically significant risks of aggressive treatment. Supportive care and eventual renal transplantation are recommended. In patients with irreversible renal failure, renal transplantation is usually deferred for at least 1 year to decrease the risk of recurrence.
- Patients who are antineutrophilic cytoplasmic antibody (ANCA) positive with clinical presentations consistent with vasculitis are likely to benefit from aggressive therapy independent of the severity of disease 17.
- Most patients with pulmonary hemorrhage respond rapidly to methylprednisolone pulses, plasma exchange, or plasmapheresis.
- Patients with mild renal disease who do not have pulmonary hemorrhage may be successfully treated with prednisone alone.
In patients with renal insufficiency, treatment should be commensurate with the severity of disease and includes therapy for hypertension, fluid overload, and electrolyte and acid-base imbalances.
Early plasmapheresis removes circulating anti-GBM antibodies and other mediators of inflammation and has been advocated as the treatment of choice.
- Plasmapheresis with immunosuppression is effective in the treatment of pulmonary hemorrhage and substantially improves renal function in patients with serum creatinine levels of less than 7 mg/dL or with crescents in less than 50% of the glomeruli.
- Therapy usually consists of 14 treatments during 2-3 weeks.
- Concomitant administration of cyclophosphamide and steroids is essential to prevent rebound antibody formation.
- Additional plasmapheresis may be required if anti-GBM antibody titers remain elevated after the treatments.
- Patients undergoing plasmapheresis who develop serious infections benefit from intravenous administration of immunoglobulins.
Experimental and future treatment
Preliminary data suggest that removal of anti-GBM antibody by means of immunoadsorption may be beneficial in patients with Goodpasture disease. These results must be verified before immunoadsorption can be recommended.
A retrospective review of 10 anti-GBM patients treated with immunoadsorption reported a reduction in antibodies to negative levels in all patients by the first 9 immunoadsorption treatments and that renal survival was 40% at diagnosis, 70% after the end of immunoadsorption, and 63% after one year 18.
The effect of blocking CD28-B7, the costimulatory pathway for T-cell activation, was evaluated in a rat model of anti-GBM disease. The rationale for this attempt was the observation that T-cell–mediated mechanisms may play a direct role in the glomerular and alveolar injury that occurs in anti-GBM disease.
Anti GBM disease prognosis
Prognosis for anti GBM disease is overall good, provided the disease is identified efficiently, and treatment started promptly. Overall survival, and renal recovery track along with the degree of renal impairment on presentation.
Recurrence is rare but possible, and patients typically do well with recurrent episodes. This is most likely due to heightened clinical suspicion. Treatment in recurrent cases is identical to the initial episode 19.
Patients that do not recover renal function and remain dependent on renal replacement therapy may qualify for renal transplantation. Anti-glomerular basement membrane antibody titers should be negative for at least 6 months before transplantation 20. These patients rarely experience recurrent disease in the current era following transplant, but it has been reported in the literature 21. It has been theorized that long-term use of immunosuppressive agents aimed at protecting the graft from rejection simultaneously keeps the autoimmune disease from recurring 22.
References- Anti-GBM Antibody Disease. https://emedicine.medscape.com/article/981258-overview
- Kambham N. Crescentic Glomerulonephritis: An Update on Pauci-immune and Anti-GBM Diseases. Adv Anat Pathol. 2012 Mar. 19(2):111-24.
- Troxell ML, Houghton DC. Atypical anti-glomerular basement membrane disease. Clin Kidney J. 2016;9(2):211–221. doi:10.1093/ckj/sfv140 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4792615
- Jennette JC, Nickeleit V. Anti-glomerular basement membrane glomerulonephritis and Goodpasture syndrome. In: Jennette JC, Silva FG, Olson JL, et al., editors. (eds). Heptinstall’s Pathology of the Kidney. 7th edn Philadelphia, PA: Wolters Kluwer, 2015, pp. 657–684.
- Anti-GBM/Anti-TBM nephritis. https://www.aarda.org/diseaseinfo/anti-gbmanti-tbm-nephritis/
- DeVrieze BW, Hurley JA. Goodpasture Syndrome (Anti-glomerular Basement Membrane Antibody Disease) [Updated 2019 Mar 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459291
- Hellmark T, Segelmark M. Diagnosis and classification of Goodpasture’s disease (anti-GBM). J. Autoimmun. 2014 Feb-Mar;48-49:108-12.
- Phelps RG, Rees AJ. The HLA complex in Goodpasture’s disease: a model for analyzing susceptibility to autoimmunity. Kidney Int. 1999 Nov;56(5):1638-53.
- Goodpasture syndrome. https://medlineplus.gov/ency/article/000142.htm
- Stem Cell Transplant for Cancer. http://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/stem-cell-transplant.html
- Anti-GBM Antibody Disease Clinical Presentation. https://emedicine.medscape.com/article/981258-clinical
- Jais JP, Knebelmann B, Giatras I, et al. X-linked Alport syndrome: natural history in 195 families and genotype- phenotype correlations in males. J Am Soc Nephrol. 2000 Apr. 11(4):649-57.
- Salama AD, Levy JB, Lightstone L, Pusey CD. Goodpasture’s disease. Lancet. 2001 Sep 15;358(9285):917-20.
- Goodpasture Syndrome. https://emedicine.medscape.com/article/240556-overview
- Pediatric Anti-GBM Disease (Goodpasture Syndrome). https://emedicine.medscape.com/article/1001872-overview
- Kalluri R, Wilson CB, Weber M, Gunwar S, Chonko AM, Neilson EG, Hudson BG. Identification of the alpha 3 chain of type IV collagen as the common autoantigen in antibasement membrane disease and Goodpasture syndrome. J. Am. Soc. Nephrol. 1995 Oct;6(4):1178-85.
- McAdoo SP, Tanna A, Hrušková Z, Holm L, Weiner M, Arulkumaran N, et al. Patients double-seropositive for ANCA and anti-GBM antibodies have varied renal survival, frequency of relapse, and outcomes compared to single-seropositive patients. Kidney Int. 2017 May 12.
- Biesenbach P, Kain R, Derfler K, Perkmann T, Soleiman A, Benharkou A, et al. Long-term outcome of anti-glomerular basement membrane antibody disease treated with immunoadsorption. PLoS One. 2014. 9 (7):e103568.
- Levy JB, Lachmann RH, Pusey CD. Recurrent Goodpasture’s disease. Am. J. Kidney Dis. 1996 Apr;27(4):573-8.
- Beck L, Bomback AS, Choi MJ, Holzman LB, Langford C, Mariani LH, Somers MJ, Trachtman H, Waldman M. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for glomerulonephritis. Am. J. Kidney Dis. 2013 Sep;62(3):403-41.
- Tang W, McDonald SP, Hawley CM, Badve SV, Boudville NC, Brown FG, Clayton PA, Campbell SB, de Zoysa JR, Johnson DW. Anti-glomerular basement membrane antibody disease is an uncommon cause of end-stage renal disease. Kidney Int. 2013 Mar;83(3):503-10.
- Sauter M, Schmid H, Anders HJ, Heller F, Weiss M, Sitter T. Loss of a renal graft due to recurrence of anti-GBM disease despite rituximab therapy. Clin Transplant. 2009 Jan-Feb;23(1):132-6.