What is aphasia
Aphasia also called dysphasia, is a disturbance in the ability to comprehend or use language when you have brain damage. Aphasia may make it hard for you to understand, speak, read, or write 1. Aphasia impairs your ability to speak and understand others, and most people with aphasia experience difficulty reading and writing. Aphasia is always due to injury to the language centers of the brain (cerebral cortex) most commonly from a stroke, particularly in older individuals. Annually, approximately 170,000 new cases of aphasia are related to stroke 2. However, any type of brain damage can cause aphasia. This includes brain tumors, traumatic brain injury, brain infections and brain disorders that get worse over time. Aphasia is also a symptom of degenerative dementing illnesses such as Alzheimer disease. With dementing illness, patients develop gradual progressive language deficits as opposed to a sudden onset of loss of language function that is seen in an ischemic stroke 3. Brain damage can also cause other problems along with aphasia. You may have muscle weakness in your mouth, called dysarthria. Dysarthria occurs when the muscles used to breath and speak are weakened or paralysed, making speech slurred and hard to understand. You may have trouble getting the muscles of your mouth to move the right way to say words, called apraxia. You can also have swallowing problems, called dysphagia.
Aphasia affects a person’s language, but it doesn’t affect a person’s intelligence.
Aphasia involves varying degrees of impairment in four primary areas:
- Spoken language expression
- Spoken language comprehension
- Written expression
- Reading comprehension
Your brain has two halves. Language skills are in the left half of the brain in most people. Scientists and clinicians who study how language is stored in the brain have learned that different aspects of language are located in different parts of the left hemisphere of the brain. Damage on the language centers of the brain (left half of the brain in most people) may lead to language problems. For example, areas in the back portions allow you to understand words. When a stroke affects this posterior or back part of the left hemisphere of the brain, people can have great difficulty understanding what they hear or read. Aphasia does not make you less smart or cause problems with the way you think. On the other hand, damage on the right side of your brain may cause other problems, like poor attention or memory.
A person with aphasia may select the wrong words in conversing and may have problems interpreting verbal messages 4. Children born with aphasia may not talk at all. Aphasia can be so severe as to make communication with the patient almost impossible, or it can be very mild. Aphasia may affect mainly a single aspect of language use, such as the ability to retrieve the names of objects, or the ability to put words together into sentences, or the ability to read. More commonly, however, multiple aspects of communication are impaired, while some channels remain accessible for a limited exchange of information.
Talking problem in aphasia
You may find that you:
- Can’t think of the words you want to say.
- Say the wrong word. Sometimes, you may say something related, like “fish” instead of “chicken.” Or you might say a word that does not make much sense, like “radio” for “ball.”
- Switch sounds in words. For example, you might say “wish dasher” for “dishwasher.”
- Use made-up words.
- Have a hard time saying sentences. Single words may be easier.
- Put made-up words and real words together into sentences that do not make sense.
Understanding problem in aphasia
You may:
- Not understand what others say. This may happen more when they speak fast, such as on the news. You might have more trouble with longer sentences, too.
- Find it hard to understand what others say when it is noisy or you are in a group.
- Have trouble understanding jokes.
Reading and writing problem in aphasia
You may have trouble with the following things:
- Reading forms, books, and computer screens.
- Spelling and putting words together to write sentences.
- Using numbers or doing math. For example, it may be hard to tell time, count money, or add and subtract.
Aphasia affects about two million Americans and is more common than Parkinson’s Disease, cerebral palsy or muscular dystrophy. Nearly 180,000 Americans acquire the disorder each year. However, most people have never heard of it.
While aphasia is most common among older people, it can occur in people of all ages, races, nationalities and gender.
The severity of a person’s aphasia depends on the location and type of injury sustained by the brain. Aphasia typically occurs suddenly after a stroke or a head injury. But it can also come on gradually from a slow-growing brain tumor or a disease that causes progressive, permanent damage (degenerative). Where and how bad the brain damage is and what caused it determine the degree of disability.
Aphasia can occur by itself or alongside other disorders, such as visual difficulties, mobility problems, limb weakness and cognitive changes.
Aphasia can make it hard for you to read, write, and say what you mean to say. Aphasia is most common in adults who have had a stroke. Brain tumors, infections, injuries, and dementia can also cause it. The type of problem you have and how bad it is depends on which part of your brain is damaged and how much damage there is.
People with aphasia make mistakes with the words they use, sometimes using the wrong sounds in a word, choosing the wrong word, or putting words together incorrectly.
Aphasia also affects speaking and writing in the same way. Many people with the condition find it difficult to understand words and sentences they hear or read. A speech therapist may assess the quality and extent of the Aphasia, and help to educate those people who most commonly interact with the affected individual in methods to help communication.
In some instances, an individual will completely recover from aphasia without treatment. In most cases, however, language therapy should begin as soon as possible and be tailored to the individual needs of the person. Rehabilitation with a speech pathologist involves extensive exercises in which individuals read, write, follow directions, and repeat what they hear. Computer-aided therapy may supplement standard language therapy.
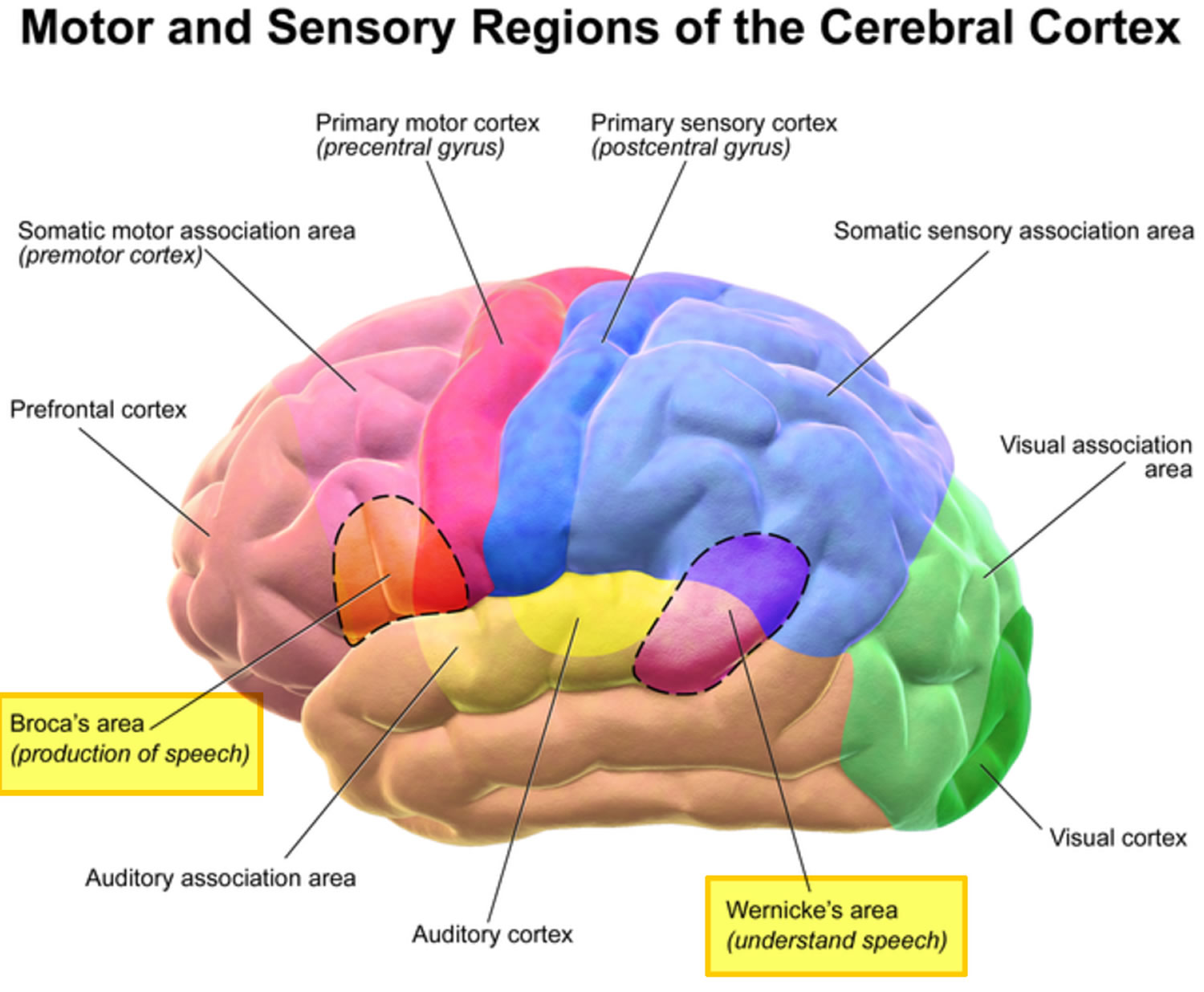
Figure 1. Brain anatomy showing the region of the brain (Brodmann’s area) that contains motor neurons involved in the production of speech (Broca’s area) and understanding of speech (Wernicke’s area).
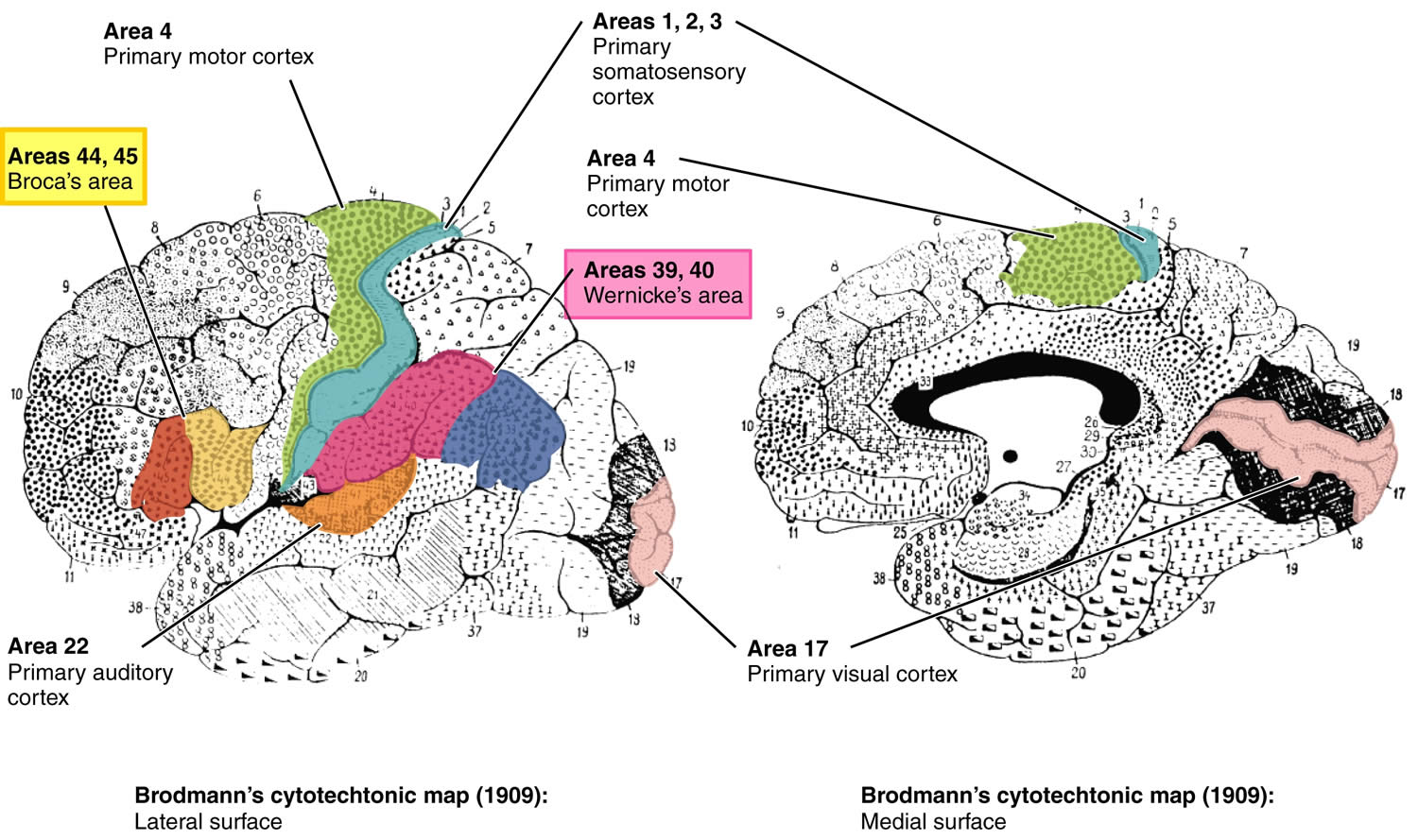
Figure 2. Broadmann areas
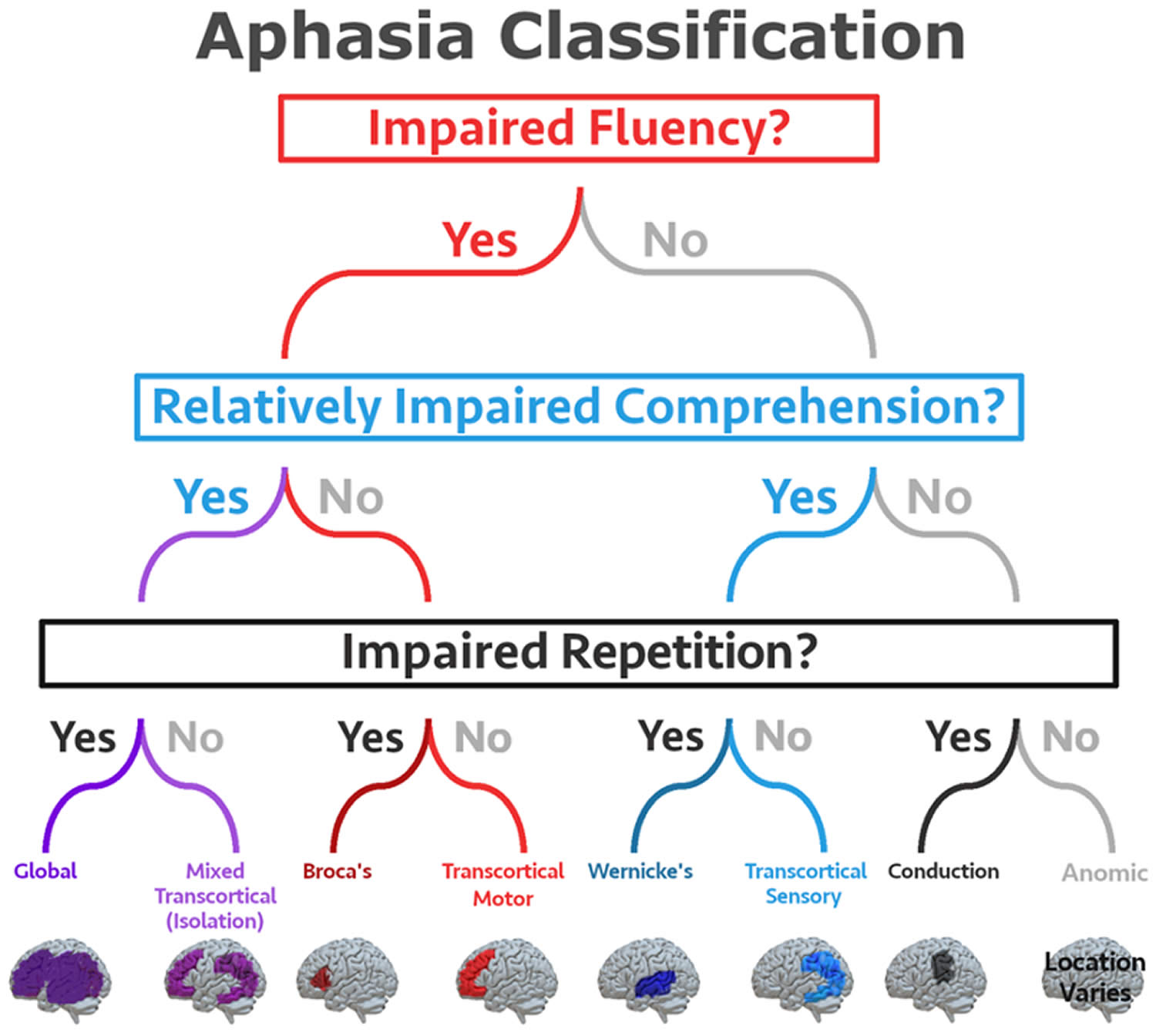
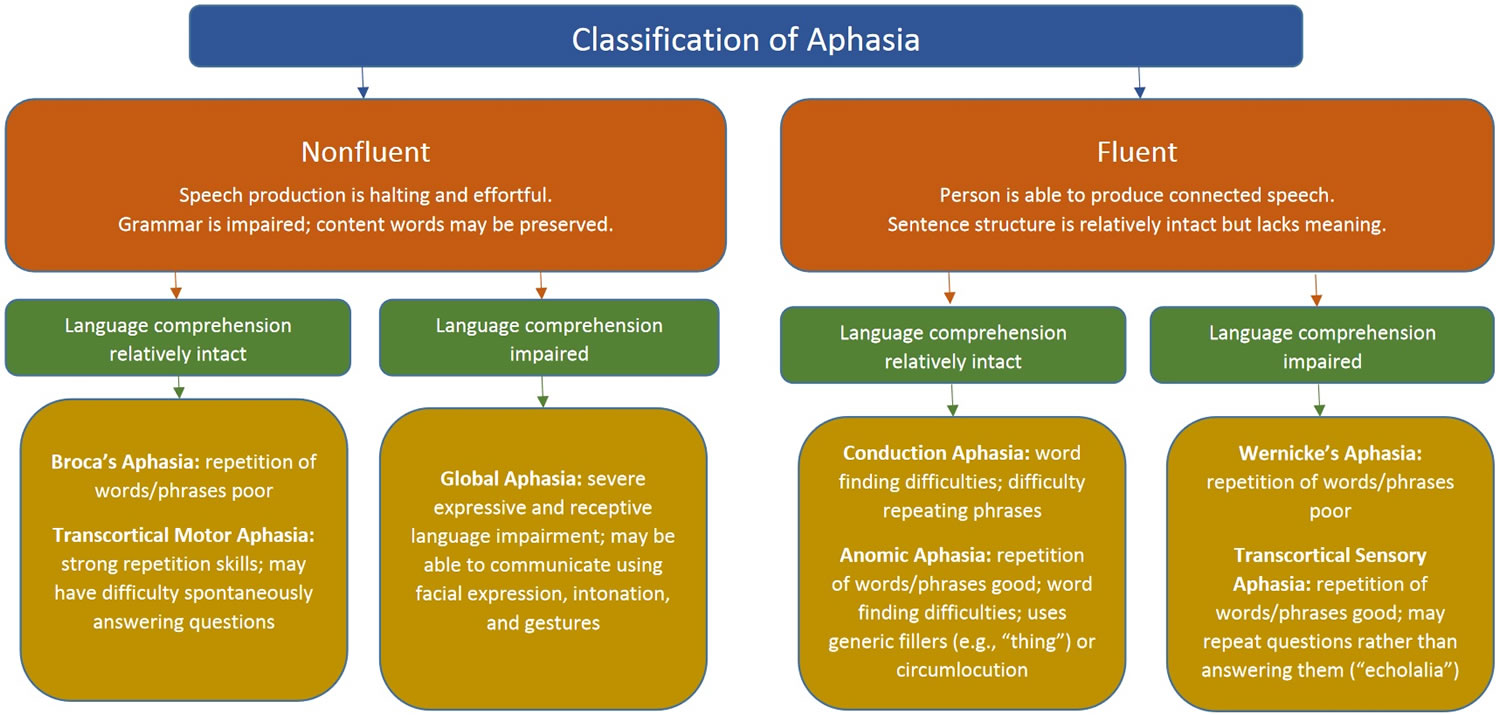
Figure 3. Aphasia classification
Footnotes: The eight aphasia subtypes identified by the Boston neoclassical system are defined based on measures of fluency, comprehension, and repetition. Note the figure depicts lesions that are often associated with each subtype of aphasia, however there is inherent heterogeneity in stroke patients and a patient may present with a specific subtype of aphasia even if their lesion does not match the area depicted in this figure.
[Source 5 ]Because aphasia is often a sign of a serious problem, such as a stroke, seek emergency medical care if you suddenly develop:
- Difficulty speaking
- Trouble understanding speech
- Difficulty with word recall
- Problems with reading or writing
How Long Does it Take to Recover from Aphasia?
If the symptoms of aphasia last longer than two or three months after a stroke, a complete recovery is unlikely. However, it is important to note that some people continue to improve over a period of years and even decades. Improvement is a slow process that usually involves both helping the individual and family understand the nature of aphasia and learning compensatory strategies for communicating.
Some people recover from aphasia without treatment. Most, however, need language therapy as soon as possible.
Once the cause has been addressed, the main treatment for aphasia is speech and language therapy. The person with aphasia relearns and practices language skills and learns to use other ways to communicate. Family members often participate in the process, helping the person communicate.
Does Aphasia Affect a Person’s Intelligence?
NO. A person with aphasia may have difficulty retrieving words and names, but the person’s intelligence is basically intact. Aphasia is not like Alzheimer’s disease; for people with aphasia it is the ability to access ideas and thoughts through language – not the ideas and thoughts themselves- that is disrupted. But because people with aphasia have difficulty communicating, others often mistakenly assume they are mentally ill or have mental retardation.
Can people who have Aphasia return to their jobs?
Sometimes. Since most jobs require speech and language skills, aphasia can make some types of work difficult. Individuals with mild or even moderate aphasia are sometimes able to work, but they may have to change jobs.
Apraxia and aphasia
Apraxia is a disorder of the brain and nervous system that is characterized by the inability to perform skilled or learned (familiar) movements on command, even though the command is understood and there is a willingness to perform the movement 6. Both the desire and the capacity to move are present but the person simply cannot execute the act 7. Person with apraxia is unable to perform tasks or movements when asked, even though:
- The request or command is understood
- They are willing to perform the task
- The muscles needed to perform the task work properly
- The task may have already been learned
Patients with apraxia cannot use tools or perform such acts as tying shoelaces or button shirts etc. The requirements of daily living are difficult to meet. Apraxia is sometimes also referred to a motor speech disorder that makes it hard to move the mouth in the way needed to produce sounds and words to speak. Apraxia of speech is often present along with another speech disorder called aphasia. Depending on the cause of apraxia, a number of other brain or nervous system problems may be present.
Apraxia is seen in various neurological disorders, including stroke and neurodegenerative disorders such as Alzheimer’s disease, Parkinson’s disease and atypical Parkinsonism [common examples are corticobasal syndrome (CBS); previously termed corticobasal degeneration, or progressive supranuclear palsy (PSP)] 8, 9. In patients with left hemispheric stroke, apraxia has been reported to be prevalent in approximately one-third of this population 10. In clinical practice, it is not uncommon that more than one type of apraxia is present in a single affected patient 11.
Childhood apraxia of speech is sometimes called apraxia of speech, verbal dyspraxia or developmental verbal dyspraxia. A child with childhood apraxia of speech knows what they want to say. The problem is not how the child thinks but how the brain tells the mouth muscles to move. In order for speech to occur, messages need to go from your brain to your mouth. These messages tell the muscles how and when to move to make sounds. When a child has apraxia of speech, the messages do not get through correctly. The child might not be able to move their lips or tongue in the right ways, even though their muscles are not weak. Sometimes, the child might not be able to say much at all.
Apraxia is believed to be caused by a lesion in the neural pathways of the brain that contain the learned patterns of movement 7. Apraxia is often a symptom of neurological, metabolic, or other disorders that can involve the brain.
Childhood apraxia of speech or apraxia of speech treatment involves working with a speech therapist to learn how to form the right sounds. The earlier the therapy starts, the better. Treatment works best if done several times a week by a therapist who has experience in apraxia of speech. As time goes on, the person may need therapy less often.
There are different types of therapy programs, depending on the age of the person with apraxia of speech. The treatment aims to teach them how to make certain sounds, words or phrases more clearly. For example, they might be taught to put a finger on their lips when they say the sound ‘p’ to remind them to close their lips.
People with apraxia must practise a lot to get better at speaking. It can be very tiring and frustrating for a child. Seeing a counselor or psychologist might help. People with apraxia may also be seen by a physiotherapist or occupational therapist. In severe cases, someone with apraxia of speech might need to learn different ways of communicating, such as sign language, using a computer or pointing to a book.
Aphasia is a neurological disorder caused by damage to the portions of the brain that are responsible for language production or processing. Aphasia may occur suddenly or progressively, depending on the type and location of brain tissue involved. Primary signs of aphasia include difficulty in expressing oneself when speaking, trouble understanding speech, and difficulty with reading and writing. Aphasia is not a disease, but a symptom of brain damage. Although aphasia is primarily seen in individuals who have suffered a stroke, aphasia can also result from a brain tumor, brain infection, brain inflammation, head injury, or dementia that affect language-associated regions of the brain. It is estimated that about 1 million people in the United States today suffer from aphasia. The type and severity of language dysfunction depends on the precise location and extent of the damaged brain tissue.
Generally, aphasia can be divided into four broad categories:
- Expressive aphasia also called Broca’s aphasia, involves difficulty in conveying thoughts through speech or writing. The person knows what she/he wants to say, but cannot find the words he needs.
- Receptive aphasia also called Wernicke’s aphasia involves difficulty understanding spoken or written language. The individual hears the voice or sees the print but cannot make sense of the words.
- Global aphasia results from severe and extensive damage to the language areas of the brain. People lose almost all language function, both comprehension and expression. They cannot speak or understand speech, nor can they read or write.
- Individuals with anomic or amnesia aphasia, the least severe form of aphasia, have difficulty in using the correct names for particular objects, people, places, or events.
Your doctor may also refer to aphasia as nonfluent, fluent or global.
Types of aphasia
The most popular classification of aphasia is the Boston classification system, which was developed in the 1960s by Norman Geschwind, Frank Benson, Harold Goodglass, and Edith Kaplan, who updated classical descriptions of aphasia subtypes 5.
The Boston neoclassical classification system includes eight aphasia subtypes:
- Expressive aphasia also called Broca’s aphasia – involves difficulty in conveying thoughts through speech or writing. The person knows what she/he wants to say, but have trouble saying or writing.
- Receptive aphasia also called Wernicke’s aphasia – involves difficulty understanding spoken or written language. The individual hears the voice or sees the print but cannot make sense of the words.
- Global aphasia – results from severe and extensive damage to the language areas of the brain. People lose almost all language function, both comprehension and expression. They cannot speak or understand speech, nor can they read or write.
- Anomic aphasia also called amnesia aphasia – the least severe form of aphasia, have difficulty in using the correct names for particular objects, people, places, or events.
- Transcortical motor aphasia
- Transcortical sensory aphasia
- Mixed transcortical aphasia also called isolation aphasia
- Conduction aphasia
Each of these subtypes is characterized by a specific profile of symptoms based on fluency of verbal expression (i.e., fluent vs. non-fluent speech), language comprehension skills, and repetition abilities (see Figure 3 and 4). It should be noted that most people with aphasia will have some level of difficulty with comprehension, spontaneous speech, reading, and writing. Typically, aphasia assessment is focused on identifying areas with the most profound impairment. These classical profiles are sometimes termed cortical aphasias, and are based on an understanding of classic left hemisphere cortical language regions such as Broca’s area and Wernicke’s area. Each subtype was theorized to be associated with damage to particular cortical regions, with some potential extension into subcortical regions, although the reliability of these predictions is debated in literature 12, 13. For example, Kasselimis and colleagues 12 classified 65 patients using the Boston classification system and also obtained neuroimaging in each patient. Lesions were only located in the regions predicted by the Boston system in 36.5% of cases. On the other hand, Yourganov and colleagues 13 found a high correlation between aphasia syndrome and predicted lesion location.
Figure 4. Types of aphasia
[Source 4 ]Figure 5. Classification of Aphasia
Broca’s aphasia (Nonfluent aphasia)
Broca’s aphasia is also known as non-fluent aphasia or expressive aphasia. Individuals with Broca’s aphasia have trouble speaking fluently but their comprehension can be relatively preserved. Broca’s aphasia is characterized by halting, effortful, non-fluent speech that has reduced phrase length, impaired melody, and diminished words per minute. Broca’s aphasia language output (both written and spoken) is agrammatic, meaning it consists mostly of content words with few, if any, function words. Repetition is typically impaired. Comprehension of single words and syntactically simpler sentences (e.g., active sentences) are often spared; comprehension of syntactically complex sentences (e.g., passive sentences) is often impaired. Individuals with Broca’s aphasia have a range of reading and writing skills. Individuals with Broca’s aphasia may be able to read but be limited in writing.
Broca’s aphasia is named after the French scientist, Paul Broca, who in 1861 first related a set of deficits associated with this type of aphasia to localized brain damage in a patient who could only say the word “tan”. Broca’s aphasia has been named in different ways, including: aphemia, efferent or kinetic motor aphasia, verbal aphasia and syntactic aphasia15. Like in other types of aphasia, intellectual and cognitive capabilities not related to speech and language may be fully preserved.
People with Broca’s aphasia struggle to get words out, speak in very short sentences and omit words. A person might say “Want food” or “Walk park today.” A listener can usually understand the meaning. People with Broca’s aphasia may understand what other people say better than they can speak. Producing the right sounds or finding the right words is often a laborious process. Some persons have more difficulty using verbs than using nouns. Patients with Broca aphasia are often very upset about their difficulty communicating. This may be due to the deficit itself or may be due to damage to adjacent frontal lobe structures which control the inhibition of negative emotions. Broca aphasia can accompany other neurological deficits such as right facial weakness, right-sided paralysis (hemiplegia) or weakness (hemiparesis) and apraxia 16.
Broca aphasia often has a devastating effect on the ability of individuals to carry out their normal activities. It affects the patient’s ability to communicate and often leads to loss of productivity and vocation and can also lead to social isolation 17, 18.
A person with Broca’s aphasia may understand speech relatively well, particularly when the grammatical structure of the spoken language is simple. However they may have harder times understanding sentences with more complex grammatical construct. For example the sentence “Mary gave John balloons” may be easy to understand but “The balloons were given to John by Mary” may pose a challenge when interpreting the meaning of who gave the balloons to whom.
There is a loss of normal grammatical structure (agrammatic speech). Specifically, small linking words, conjunctions (and, or, but), and the use of prepositions are lost. As an example, a sentence like “I took the dog for a walk.” may become “I walk dog.” Patients can exhibit interjectional speech where there is a long latency, and the words that are expressed are produced as if under pressure. The ability to repeat phrases is also impaired. Despite these impairments, the words that are produced are often intelligible and contextually correct. In pure Broca aphasia, comprehension is intact.
Broca’s aphasia results from injury to speech and language brain areas such the frontal part of the left hemisphere of the brain (posterior inferior frontal gyrus [pars opercularis and pars triangularis]), also called Broca area or convolution of Broca. This area, located in the frontal part of the left hemisphere of the brain, was discovered in 1861 by French surgeon Paul Broca, who found that it serves a vital role in the generation of articulate speech 19, 20. Language function localizes to the left cerebral hemisphere in almost all right-handed people and 70% of left-handed people 21. The Broca area lies specifically in the third frontal convolution, just anterior to the face area of the motor cortex and just above the Sylvian fissure. It is made up of two areas: the pars opercularis (Brodmann area 44) and the pars triangularis (Brodmann area 45). Various pathways connect Broca area to the frontal lobe, basal ganglia, cerebellum, and contralateral hemisphere. Such damage is often a result of stroke but may also occur due to brain trauma, brain tumors, and brain infections. A stroke in Broca area is usually due to thrombus or emboli in the middle cerebral artery or internal carotid artery.
As a result of a lesion in Broca area, there is a breakdown between one’s thoughts and one’s language abilities. Thus, patients often feel that they know what they wish to say but are unable to produce the words. That is, they are unable to translate their mental images and representations to words. This affects the normal fluency of speech. The loss of language function may be because Broca area serves a role in ordering sounds into words, and words into sentences, and thus creates relationships between linguistic elements.
While Broca’s aphasia is associated with damage to Broca’s area, in chronic Broca’s aphasia the damage often extends into surrounding frontal lobe areas, insula, and sometimes subcortical structures 22. Because Broca’s area is located near the motor strip, it is also often accompanied by right hemiplegia.
Broca’s aphasia treatment
Currently, there is no standard treatment for Broca aphasia or expressive aphasia 16. Treatments should be tailored to each patient’s needs. Speech and language therapy is the mainstay of care for patients with aphasia. It is essential to provide aphasic patients a means to communicate their wants and needs, so these may be addressed. Often this is done by providing a board with various objects so that the patient can point to the object that they want. Involvement of a speech therapist, neuropsychologist, and neurologist in the development of a care plan for the patient with Broca aphasia is very helpful in obtaining a good outcome. One innovative treatment option for patients with Broca aphasia is melodic intonation. Melodic intonation relies on the fact that musical ability is often spared in Broca aphasia. Thus, the speech therapist encourages the patient with poor speech production to try to express their words with musical tones. This approach has shown promise in clinical trials.
Medical treatment of aphasia is currently under investigation in clinical trials. Drug therapies have included catecholaminergic agents (bromocriptine, levodopa, amantadine, dexamphetamine), piracetam and related compounds, acetylcholine esterase inhibitors, and neurotrophic factors. Previous studies have been small, and further studies are needed to determine the efficacy of these pharmacological agents. Also, transcranial magnetic stimulation and transcranial direct stimulation trials for aphasia are currently underway.
When the cause of Broca aphasia is a stroke, recovery of language function peaks within two to six months, after which time further progress is limited. However, patients should be encouraged to work on speech production, because cases of improvement have been seen long after a stroke. There are commercial software products available that claim to improve language function, but for the most part, these have not been rigorously tested in randomized clinical trials.
It is important to address issues of post-stroke depression and post-stroke cognitive impairment, as well as disorders of executive function, awareness, neglect, and hemiparesis during the rehabilitation process to optimize the outcome for an individual patient. Family and social support are extremely important to keep patients with language deficits engaged in social and leisure activities which can greatly influence the aphasic patient’s quality of life.
Wernicke’s aphasia (Fluent aphasia)
In Wernicke’s aphasia the ability to grasp the meaning of spoken words and sentences is impaired, while the ease of producing connected speech is not very affected. Therefore Wernicke’s aphasia is also referred to as ‘fluent aphasia’ or ‘receptive aphasia’. Wernicke aphasia has also been named in many different ways: sensory aphasia, receptive aphasia, central aphasia, verbal
agnosia and others 15. An individual with Wernicke’s aphasia has difficulty understanding language (poor speech comprehension); speech is typically fluent but is empty of content and characterized by circumlocutions, a high incidence of vague words like “thing,” and sometimes neologisms and senseless “word salad” (speak in long, garbled sentences).
Wernicke’s aphasia and Wernicke’s area are named after the German neurologist Carl Wernicke who first related this specific type of speech deficit to a damage in a left posterior temporal area of the brain.
The Wernicke area is located in the posterior third of the upper temporal convolution of the left hemisphere of the brain (Brodmann area 22) (see Figure 1). This area lies close to the auditory cortex. This area appears to be uniquely important for the comprehension of speech sounds and is considered to be the receptive language, or language comprehension, center. Language function localizes to the left cerebral hemisphere in almost all right-handed people and 70% of left-handed people 21.
Wernicke aphasia usually involves the posterior one third of the superior temporal gyrus 23. If there is involvement of the middle/inferior temporal gyri or the inferior parietal lobule, recovery is unlikely. Recovery also depends on area and size of damage, patient age and status of the contralateral cortex 23.
The most common cause of Wernicke’s aphasia is an ischemic stroke affecting the posterior temporal lobe of the dominant hemisphere 23. In most patients the cause of Wernicke’s aphasia is an embolic stroke that affects the inferior division of the middle cerebral artery, which supplies the temporal cortex.
Other causes of Wernicke’s aphasia are brain trauma, cerebral tumors, central nervous system (CNS) infections, and degenerative brain disorders 24, 25.
Reading and writing are often severely impaired. As in other forms of aphasia, individuals can have completely preserved intellectual and cognitive capabilities unrelated to speech and language.
In Wernicke’s aphasia language output is fluent with a normal rate and intonation. Persons with Wernicke’s aphasia can produce many words and they often speak using grammatically correct sentences with normal rate and prosody. However, often what they say doesn’t make a lot of sense or they pepper their sentences with non-existent, incorrect or irrelevant words because of paraphrastic errors. They may fail to realize that they are using the wrong words or using a non-existent word and often they are not fully aware that what they say doesn’t make sense. They usually don’t understand spoken language well and often don’t realize that others can’t understand them.
Paraphasic errors come in two forms: semantic paraphasia errors where one word is substituted for another and phenomic paraphrastic errors where one sound or syllable is substituted for another. An example of a semantic paraphasia error would be a patient saying “watch” instead of “clock.” An example of a phonemic paraphasic error would be a patient saying “dock” instead of “clock.” In severe cases, these errors can result in neologisms (new words) or word salad which makes communication nearly unintelligible. Because of these deficits, patients may find it easier to substitute a generic word such as “thing” or “stuff” instead of saying the word they wish to say. Reading involves the comprehension of written words, and thus reading is also often impaired in Wernicke’s aphasia. As with Broca’s aphasia, repetition is also impaired.
Patients with Wernicke’s aphasia usually have profound language comprehension deficits, even for single words or simple sentences. This is because in Wernicke’s aphasia individuals have damage in brain areas that are important for processing the meaning of words and spoken language. Such damage includes left posterior temporal regions of the brain, which are part of what is knows as Wernicke’s area, hence the name of the aphasia.
In general, patients with wernicke aphasia are not aware of their deficits; in the long run they do become frustrated that others are not able to understand what they are saying. Sometimes, the patient may become aware of the errors in language if it is presented to them in an audio format.
Unlike Broca’s aphasia, patients with Wernicke’s aphasia speak with normal fluency and prosody and follow grammatical rules with normal sentence structure. Associated neurological symptoms depend on the size and location of the lesion and include visual field deficits, trouble with the calculation (acalculia), and writing (agraphia). As opposed to Broca’s aphasia, patients with Wernicke’s aphasia often do not have hemiparesis accompanying the language deficit. They also do not display the same degree of emotional outbursts and depression seen with Broca’s aphasia.
Repetition and naming items isusually abnormal. In some cases, there is impairment in reading. even when they are able to write fluently, the choice of words and spelling is abnormal. An early clue to Wernicke aphasia is the abnormal spelling.
Wernicke’s aphasia treatment
Currently, there is no standard treatment for Wernicke’s aphasia. Speech and language therapy is the mainstay of care for patients with aphasia. Because comprehension is impaired, patients may lack insight into their deficit. This makes remediation efforts very challenging. A care plan developed with a speech therapist, neuropsychologist, and neurologist would be the best way to try to optimize patient outcome. The treatment plan aims to allow the patient to better use remaining language function, improve language skill, and communicate in alternative ways so that their wants and needs can be addressed. Group therapy can give patients a chance to practice their communication skills and may lead to decreased feels of social isolation. Many commercial software vendors claim that their products will improve language function. However, these products, for the most part, have not been thoroughly vetted with rigorous clinical trials 26, 27.
Researchers are currently studying medical treatment of aphasia in randomized clinical trials. They are also developing pharmacological treatments that include drugs that affect the catecholaminergic system (bromocriptine, levodopa, amantadine, dexamphetamine), nootropic drugs such as piracetam, and medications used to treat Alzheimer Disease such as donepezil and memantine. Non-pharmacological approaches include transcranial magnetic stimulation and transcranial direct stimulation. Trials to date have been small with mixed results. Further studies are needed to determine the effectiveness of these approaches.
When the cause of Wernicke’s aphasia is a stroke, recovery of language function peaks within two to six months, after which time further progress is limited. However, efforts should be made to try to improve communication, since an improvement in aphasia has been documented long after a stroke. Family support and social support are essential to a good outcome. Treatment of post-stroke depression and post-stroke cognitive issues, as well as remediation of other neurological disorders such as neglect, agnosia, and hemiparesis, should be addressed during rehabilitation to optimize patient outcome.
Transcortical sensory aphasia
Transcortical sensory aphasia also known as extrasylvian sensory aphasia, is a controversial syndrome frequently considered as a subtype of Wernicke’s aphasia 15. Some authors have even simply denied the existence of such a syndrome. In general, it is considered that transcortical sensory aphasia includes the following elements 15:
- Good repetition (the patient repeats words and sentences presented by the examiner, regardless if they are incorrect and even in a foreign language);
- Fluent conversational language;
- Significant amount of verbal paraphasias and neologisms; and
- Empty speech.
Transcortical sensory aphasia presents similar deficits as in Wernicke’s aphasia, except repetition skills are intact and phoneme discrimination impairments are not found 15. Some authors also include a semantic jargon in the definition of transcortical sensory aphasia 28. But jargon is not a required symptom for the diagnosis of transcortical sensory aphasia. By the same token, other language impairments can also be found, such as poor naming, and preserved oral reading with impaired reading comprehension, but their presence is not essential to establish the diagnosis of transcortical sensory aphasia 29.
No motor (including articulatory) defects are observed; but because of its location in the brain, cortical sensory function can be defective and ideomotora apraxia can be present, depending upon the extension of the pathology to the parietal lobe 15. Similarly, the extension of the damage to the occipital lobe may result in visual agnosia and visual field defects.
Because repetition is spared, phonological processing is assumed to be preserved, at least partially, while lexical-semantic information included in the word meaning is impaired 30. Usually, it is accepted that transcortical sensory aphasia is associated with relatively extensive posterior lesions including the temporo-parieto-occipital junction of the left hemisphere but sparing the
areas around the primary auditory cortex 29. Damasio 31 observed that transcortical sensory aphasia is associated with lesions involving the temporal-occipital area (Brodmann area 37), the angular gyrus (Brodmann area 39) or the white matter underlying these regions, but sparing the primary auditory cortex (Brodmann area 41 and 42), and Brodmann area 22 (Wernicke’s area). Damasio suggested that the core area for transcortical sensory aphasia is the temporal-occipital area (Broadmann area 37) with variable extension to the occipital lobe and the angular gyrus 31.
Transcortical sensory aphasia is associated with lesions surrounding Wernicke’s area, between the areas of the brain fed by the middle cerebral artery and the posterior cerebral artery 32, 33, generally involving large portions of the temporal-parietal-occipital areas. According to Alexander, Hiltbrunner, and Fischer 34, the critical lesion for transcortical sensory aphasia in these patients involved pathways in the posterior periventricular white matter adjacent to the posterior temporal isthmus, pathways that are most likely converging on the inferolateral temporo-occipital cortex. However, frequently the variability in the lesions responsible for transcortical sensory aphasia account for the variability observed in its clinical manifestations, suggesting that transcortical sensory aphasia does not necessarily represent a single aphasic syndrome. When the lesions are restricted to Brodmann area 37 or Brodmann area 39, specific and well-described language impairments are observed 35. With more extended lesions, additional clinical manifestations, such as jargon, can be found. These additional clinical manifestations are only observed in the acute stage of the brain pathology, and progressively disappear 36. Dronkers and Larsen 37 state that ‘‘transcortical sensory aphasia always resolves into mild anomic aphasia’’.
Transcortical motor aphasia
Transcortical motor aphasia also known as extrasylvian motor aphasia, dynamic aphasia or loss of verbal initiative, is characterized by non fluent language, good comprehension, and good repetition 15. Prosody, articulation, and grammar are preserved 15. Transcortical motor aphasia presents very similarly to Broca’s aphasia, except repetition of words and sentences is relatively preserved. More fluent speech is observed when a patient is repeating words, phrases, or sentences, compared to their spontaneous speech output. Patients have great difficulty initiating speech, and often present with echolalia 38.
Transcortical motor aphasia patient presents long latencies in language when beginning to speak or when answering questions. Open questions are slow and incomplete, and the patient tends to repeat the words included in the question. Expressive language is limited with some tendency to echolalia and perseveration; occasionally verbal paraphasias are observed. Transcortical motor aphasia could be interpreted as a language disturbance at the pragmatic level (use of the language according to the specific social context).
Alexander 39 suggested that transcortical motor aphasia could be more accurately defined as an executive function disorder rather than aphasia. He proposed that the
progression of clinical disorders from aphasia to discourse impairments can be interpreted as a sequence of procedural impairments from basic morpho-syntax to elaborated grammar to
narrative language, correlated with a progression of the focus of the damage from posterior frontal to polar and/or lateral frontal to medial frontal. It is noteworthy that successful functional
communication is significantly associated with executive function in aphasia 40.
Transcortical motor aphasia is associated with lesions just anterior or superior to Broca’s area in the medial frontal cortex and the presupplementary motor area 38. Depending upon extension of the damage, some motor weakness may exist, but quite frequently, strength is normal and no articulation defects (dysarthria) are found. However, the patient usually presents primitive (pathological) reflexes (reflexes normal in newborns, that disappear with the maturation of the brain; they can reappear en cases of frontal lobe damage) such as palmar grasp reflex, palm mental reflex, snout reflex, and plantar reflex (Babinski sign). No somatosensory abnormalities, visual field defects, apraxia, or agnosia are observed.
Mixed transcortical aphasia
Mixed transcortical aphasia is an extremely unusual aphasic syndrome and just some few cases have been reported in the aphasia literature 41. Mixed transcortical aphasia is also referred as “isolation syndrome”, because supposedly the language area becomes isolated from the rest of the brain 15. In mixed transcortical aphasia, Broca’s and Wernicke’s areas are intact but their surrounding areas are impaired. It is thought that damage to these association areas leaves Broca’s and Wernicke’s areas completely isolated from the rest of the language system, thus precluding the production of spontaneous speech and the comprehension of spoken and written language. The most common cause of mixed transcortical aphasia is a watershed zone (areas of the brain along the “border zones” between major arteries receiving dual blood supply) stroke of the language association areas as a result of severe internal carotid stenosis 42.
In mixed transcortical aphasia, spontaneous language is absent and speech production is virtually limited to repetition; frequently echolalia is observed, but articulation is good and automatic
language is relatively preserved. In mixed transcortical aphasia the only difference with global aphasia is the relatively preserved language repetition ability 15.
Global aphasia
Global Aphasia is the most severe form of aphasia and is applied to patients who can produce few recognizable words and understand little or no spoken language. People with global aphasia have severe disabilities with expression and comprehension. People with global aphasia can neither read nor write. Like in other milder forms of aphasia, individuals can have fully preserved intellectual and cognitive capabilities unrelated to language and speech.
Global Aphasia is caused by injuries to multiple language-processing areas of the brain, including those known as Wernicke’s and Broca’s areas. These brain areas are particularly important for understanding spoken language, accessing vocabulary, using grammar, and producing words and sentences.
Global aphasia may often be seen immediately after the patient has suffered a stroke or a brain trauma. Symptoms may rapidly improve in the first few months after stroke if the damage has not been too extensive. However, with greater brain damage, severe and lasting disability may result. It is important to speak with your doctor about finding speech and language therapy as soon as possible after Global Aphasia has been diagnosed.
Non-fluent aphasia
According to the American Hearing Language Association’s classification of aphasia, the types of non-fluent aphasia include Broca’s aphasia and Global Aphasia 14.
Mixed Non-fluent Aphasia
Mixed non-fluent aphasia applies to persons who have sparse and effortful speech, resembling severe Broca’s aphasia. However, unlike individuals with Broca’s aphasia, mixed non-fluent aphasia patients remain limited in their comprehension of speech, similar to people with Wernicke’s aphasia. Individuals with mixed non-fluent aphasia do not read or write beyond an elementary level.
Conduction aphasia
Conduction aphasia also known as motor or kinesthetic afferent aphasia, central aphasia or efferent conduction aphasia, is a rare form of aphasia where both expression and comprehension remain intact, but the patient shows an isolated impairment in the ability to repeat simple phrases 43. Patients with conduction aphasia have fluent speech with phonemic distortions, relatively good comprehension, and mild to moderate naming deficits. Patients with conduction aphasia have difficulties or are unable to repeat what is spoken to them. Repetition skills are disproportionally impaired relative to comprehension and expression.
Conduction aphasia was classically associated with damage to left arcuate fasciculus, which is the neural pathway connecting Wernicke’s and Broca’s areas 44. However, more recent evidence suggests that lesions of the left superior temporal gyrus, the left supramarginal gyrus, the left inferior parietal lobe (Brodmann area 40), the left primary auditory cortices (Brodmann area 41 and 42), and the insula, can all lead to conduction aphasia 45. This injury leads to impaired repetition. Thus, the patient can comprehend the speech but cannot transmit the information to the speech production centers in the Broca area to allow repetition to occur. Recent research based on the anatomically distributed modular networks model shows that patients with conduction aphasia clinically often have lesions in the supramarginal gyrus or deep parietal matter, which suggests that damage to anatomically related structures may also lead to a disconnection between Broca and Wernicke areas.
The findings in conduction aphasia may be subtle because of the lack of neurological findings 46. The patient may complain of trouble coming up with words, or making errors when he/she tries to speak. During the assessment of aphasia, the clinician should examine the patient’s verbal fluency, comprehension, repetition, reading, writing, and naming. A patient with relatively well-preserved auditory comprehension, fluent speech production, reading, writing, but poor speech repetition may have conduction aphasia. Patients may display well-articulated responses similar to the target word and continue to repeat words or phrases to correct the error (conduit d’approache). The rest of the neurological exam (cranial nerves, motor, sensory, reflexes, gait, coordination) is typically normal.
Conduction aphasia example:
- Examiner: Please repeat after me; boy.
- Patient: Boy.
- Examiner: Seventy-nine.
- Patient: Ninety-seven…no… seventy sine… seventy-nice
According to Benson et al. 47, conduction aphasia has three fundamental and five secondary characteristics; so-called secondary characteristics are frequently but not necessarily found in conduction aphasia. The three basic characteristics are: (1) fluent conversational language; (2) comprehension almost normal; and (3) significant impairments in repetition. Secondary characteristics include: (1) impairments in naming; (2) reading impairments; (3) variable writing difficulties (apraxic agraphia); (4) ideomotor apraxia; and (5) additional neurological impairments. Bartha and Benke 48 report that conduction aphasia patients present as relatively homogenic in their aphasic manifestations: severe impairment of repetition and fluent expressive language functions with frequent phonemic paraphasias, repetitive self-corrections, word-finding difficulties, and paraphrasing. Repetitive self-corrections frequently result in so-called conduit d’approche (behavior of approximation). Language comprehension (auditory and reading) is only mildly impaired.
Some neurological abnormalities can be found in conduction aphasia; mild hemiparesis is frequent at the onset of aphasia, but tend to disappear, unless the damage extends to the frontal lobe 15. Articulation is usually normal, but frequently somatosensory defects
(such as hypoesthesia, difficulties for localizing tactile stimuli, etc.) are found. Ideomotor apraxia is generally found, and even some authors have proposed that conduction aphasia could be interpreted as a segmentary ideomotor apraxia 49. Visual field defects and visual agnosia are not expected to be found.
Anomic Aphasia
Anomic aphasia is one of the milder forms of aphasia. The term is applied to persons who are left with a persistent inability to supply the words for the very things they want to talk about, particularly the significant nouns and verbs. Your speech is fluent and grammatically correct but it is full of vague words (such as ‘thing’) and circumlocutions (attempts to describe the word they are trying to find). The feeling is often that of having the word on the tip of one’s tongue, which results in their speech having lots of expressions of frustration. People with anomic aphasia understand speech well and they can repeat words and sentences. In most cases they can read adequately. Difficulty finding words is as evident in writing as it is in speech.
Other varieties
In addition to the foregoing syndromes that are seen repeatedly by speech clinicians, there are many other possible combinations of deficits that do not exactly fit into these categories.Some of the components of a complex aphasia syndrome may also occur in isolation. This may be the case for disorders of reading (alexia) or disorders affecting both reading and writing (alexia and agraphia), following a stroke. Severe impairments of calculation often accompany aphasia, yet in some instances patients retain excellent calculation in spite of the loss of language.
Subcortical aphasia
More recently subcortical aphasias have also been identified, where damage is confined to subcortical areas alone. In the review of eight neoclassic syndromes it was noted that subcortical damage may accompany cortical damage. However, in subcortical aphasias, only subcortical damage is present. Subcortical aphasias are often divided into two groups: thalamic aphasia, and striato-capsular aphasia. Thalamic aphasia is characterized by severe anomia, presence of verbal paraphasias, reduced spontaneous verbal output, with variable comprehension skills 50, 51, 52. Variability in comprehension findings across studies of patients with thalamic aphasia may be due to the involvement of specific thalamic nuclei or subnuclei 50. Striato-capsular aphasia is associated with lesions in basal ganglia (head of caudate nucleus, putamen, anterior limb of the internal capsule). Researchers have attempted to define clinical syndromes associated with specific areas of basal ganglia damage 53, 54, but no strong clinical consensus has been reached 55. Mounting evidence 55, 56, 57 suggests that basal ganglia lesions are associated with hypoperfusion in cortical areas, which in turn explains symptoms of aphasia.
Crossed aphasia
Crossed aphasia is the term used to describe aphasia that results from damage to the hemisphere non-dominant for language (in most individuals this is the right hemisphere). Crossed aphasia is rare, but appears to result from a small minority of people who have reversed asymmetry of language functions in the right hemisphere even when they are right-handed. Crossed aphasia can be a mirror image of the left hemisphere profile so each of the neoclassical syndromes discussed above could potentially occur 58, 59. However, in about 40% of cases anomalous profiles also occur where the extent and site of lesion doesn’t map well to the associated symptoms 59.
Alexia and agraphia
In addition to broad language comprehension and production deficits, stroke can also cause reading and writing deficits. Alexia refers to reading deficits and agraphia refers to writing deficits. In cases of pure alexia, patients demonstrate reading impairments in the absence of any other deficits 60, 61. Pure alexia is associated with simultaneous damage to 1) left occipital cortex, which causes right homonymous hemianopsia where visual information is initially processed in the right occipital cortex, and 2) splenium of the corpus callosum, which then prevents visual information in the right hemisphere from crossing over to the left hemisphere, where language is processed 62. Pure agraphia refers to cases where writing impairments are present in the absence of other difficulties (35). Spelling deficits are associated with damage to left inferior parietal cortex and left occipitotemporal cortex 63.
Primary Progressive Aphasia
Primary progressive aphasia (PPA) is a clinical syndrome characterized by progressive impairment of speech and language caused by neurodegeneration of language networks with preservation of other mental functions and of activities of daily living, for at least two years, first defined by Mesulam and colleagues 64, 65. Primary progressive aphasia is not Alzheimer’s disease. However, because of primary progressive aphasia close relation to Alzheimer disease and Pick disease, the classification and diagnosis of primary progressive aphasia can sometimes be controversial 66.
Primary Progressive Aphasia is a disorder of language; and signs and symptoms of other clinical syndromes are not found through tests routinely used to determine the presence of other conditions. Most people with primary progressive aphasia maintain ability to take care of themselves, pursue hobbies, and, in some instances, remain employed.
Primary Progressive Aphasia also called progressive aphasia without dementia, is a rare neurological syndrome in which language capabilities become slowly and progressively impaired. Unlike other forms of aphasia that result from stroke or brain injury, primary progressive aphasia is caused by neurodegenerative diseases, such as Alzheimer’s Disease or Frontotemporal Lobar Degeneration. Primary Progressive Aphasia results from deterioration of brain tissue important for speech and language. Although the first symptoms are problems with speech and language, other problems associated with the underlying disease, such as memory loss, often occur later.
In 2011, an international group of experts introduced a common framework in which primary progressive aphasia (PPA) was classified into three different variants, based on specific cognitive and neuroimaging features 65:
- semantic primary progressive aphasia (svPPA),
- nonfluent/agrammatic primary progressive aphasia (nfvPPA) also known as progressive nonfluent aphasia and as PPA-agrammatic,
- logopenic variants primary progressive aphasia (lvPPA).
Recent clinicopathological studies demonstrated that each variant is associated with different probabilities of neuropathological changes and, rarely, genetic mutations. Table 1 presents the 2011 primary progressive aphasia classification, including the diagnostic algorithm allowing for three diagnostic levels: clinical, imaging-supported, and definite diagnosis.
Table 1. Primary progressive aphasia 2011 diagnostic consensus criteria algorithm
| Primary progressive aphasia (PPA) clinical diagnostic criteria | |||
| Inclusion criteria | |||
| (1) Most prominent clinical feature is difficulty with language | |||
| (2) Aphasia should be the most prominent deficit at symptom onset and for the initial phases of the disease | |||
| (3) These deficits are the principal cause of impaired daily living activities | |||
| Exclusion criteria | |||
| (1) Pattern of deficits is better accounted for by other nondegenerative nervous system or medical disorders | |||
| (2) Cognitive disturbance is better accounted for by a psychiatric diagnosis | |||
| (3) Prominent initial episodic memory, visual memory, and visuoperceptual impairments | |||
| (4) Prominent initial behavioral disturbance | |||
| Nonfluent/Agrammatic variant primary progressive aphasia (PPA) | Semantic variant primary progressive aphasia (PPA) | Logopenic variant primary progressive aphasia (PPA) | |
| Clinical diagnosis | Core features: (at least 1) (1) Agrammatism in language production (2) Effortful, halting speech with inconsistent speech sound errors and distortions (apraxia of speech)Supporting features: (at least 2) (1) Impaired comprehension of syntactically complex sentences (2) Spared single-word comprehension (3) Spared object knowledge | Core features: (both) (1) Impaired confrontation naming (2) Impaired single-word comprehensionSupporting features: (at least 3) (1) Impaired object knowledge, particularly for low frequency or low familiarity items (2) Surface dyslexia or dysgraphia (3) Spared repetition (4) Spared speech production (grammar and motor speech) | Core features: (both) (1) Impaired single-word retrieval in spontaneous speech and naming (2) Impaired repetition of sentences and phrases Supporting features: (at least 3) (1) Speech (phonologic) errors in spontaneous speech and naming (2) Spared single-word comprehension and object knowledge (3) Spared motor speech (4) Absence of frank agrammatism |
| Imaging supported diagnosis (both present) | (1) Clinical diagnosis of nonfluent/agrammatic primary progressive aphasia (nfvPPA) | (1) Clinical diagnosis of semantic primary progressive aphasia (svPPA) | (1) Clinical diagnosis of logopenic variants primary progressive aphasia (lvPPA) |
| (2) Imaging: (at least 1) | (2) Imaging: (at least 1) | (2) Imaging: (at least 1) | |
| (a) Predominant left posterior frontoinsular atrophy on MRI | (a) Predominant anterior temporal lobe atrophy on MRI | (a) Predominant left posterior perisylvian or parietal atrophy on MRI | |
| (b) Predominant left posterior frontoinsular hypoperfusion or hypometabolism on SPECT or PET | (b) Predominant anterior temporal hypoperfusion or hypometabolism on SPECT or PET | (b) Predominant left posterior perisylvian or parietal hypoperfusion or hypometabolism on SPECT or PET | |
| PPA with definite diagnosis | Clinical diagnosis fulfilled | ||
| AND | |||
| (1) Histopathologic evidence of a specific neurodegenerative disorder (e.g. FTLD-tau, FTLD-TDP, AD, other) | |||
| OR | |||
| (2) Presence of a known pathogenic mutation | |||
Abbreviations: AD = Alzheimer’s disease; FTLD-tau = frontotemporal lobar degeneration-tau; FTLD-TDP = frontotemporal lobar degeneration–TAR DNA-binding protein; lvPPA = logopenic variant primary progressive aphasia; nfvPPA = nonfluent/agrammatic primary progressive aphasia; PPA = primary progressive aphasia; svPPA = semantic variant primary progressive aphasia.
[Source 67 ]The type or pattern of the language disorder may differ from patient to patient. As with aphasia secondary to stroke, the manifestations of primary progressive aphasia depend on what parts of the left hemisphere are relatively more damaged at any given point in the illness. The initial language disturbance may be fluent aphasia (i.e., the person may have normal or even increased rate of word production) or non-fluent (it is an effort for the person to speak and he or she produces fewer words). The person with primary progressive aphasia may or may not have difficulty understanding speech. Eventually, almost all patients become mute and unable to understand spoken or written language, even if their behavior seems otherwise normal.
The average age of onset is 60; most people with primary progressive aphasia are between the ages of about 40 to 80. Men are affected twice as often as women. About half of primary progressive aphasia patients have a family history of dementia in a parent or sibling, indicating the existence of a genetic component. Half of all people with primary progressive aphasia will eventually develop cognitive or behavioral problems consistent with a more pervasive dementia syndrome, such as Alzheimer’s disease or Fronto-Temporal-Limbic Dementia, after an average of five years. In other people, primary progressive aphasia may remain relatively isolated or even be the sole manifestation for as long as 15 years. In general, the longer the duration of aphasia as an isolated symptom, the less likely that other signs of dementia will develop.
Although primary progressive aphasia may take a number of forms, it commonly appears initially as a disorder of speaking (an articulatory problem), progressing to nearly total inability to speak in its most severe stage, while comprehension remains relatively preserved. A less common variety begins with impaired word finding and progressive deterioration of naming and comprehension, with relatively preserved articulation. However, other neurological disorders exist in which progressive deterioration of language is only one component of a broad, progressive decline of mental functions, including memory, attention, visuospatial skills, reasoning, and the carrying out of complex motor activities. These diseases, such as Alzheimer’s disease, Pick’s disease, and Creutzfeld Jakob disease, should be excluded by appropriate neurologic examinations, when a person experiences progressive language decline.
Primary Progressive Aphasia commonly begins as a subtle disorder of language, progressing to a nearly total inability to speak, in its most severe stage. The type or pattern of the language deficit may differ from patient to patient. The initial language disturbance may be fluent aphasia (i.e., the person may have normal or even increased rate of word production) or non-fluent aphasia (speech becomes effortful and the person produces fewer words). A less common variety begins with impaired word-finding and progressive deterioration of naming and comprehension, with relatively preserved articulation.
As with aphasia that results from stroke or brain trauma, the manifestations of primary progressive aphasia depend on what parts of the left hemisphere are relatively more damaged at any given point in the illness. The person may or may not have difficulty understanding speech. Eventually, almost all patients become mute and unable to understand spoken or written language, even if their behavior seems otherwise normal.
Signs and symptoms of other clinical syndromes are not found through tests used to determine the presence of other conditions. Primary Progressive Aphasia is not Alzheimer’s disease. Most people with primary progressive aphasia maintain ability to take care of themselves, pursue hobbies, and, in some instances, remain employed.
Is there any treatment or assistance for people with primary progressive aphasia?
People with primary progressive aphasia are fighting against a condition in which they will continue to lose their ability to speak, read, write, and/or understand what they hear. Usually people with aphasia that results from stroke or head injury will experience improvement over time, often aided by speech therapy. This is not the case for people with primary progressive aphasia. However, individuals with primary progressive aphasia may benefit during the course of their illness by acquiring new communication strategies from speech-language pathologists. Some families have also learned new strategies through participation in Aphasia Community Groups.
Many people with aphasia find it helpful to carry identification cards and other materials that can help explain the person’s condition to others. ID cards are available from the the National Aphasia Association website 68. Some communication-assistive devices may also be helpful. Non-verbal techniques for communicating, such as gesturing and pointing to pictures, may help people with primary progressive aphasia express themselves.
Primary progressive aphasia diagnosis
As with other “degenerative” brain diseases, including Alzheimer’s disease, there are no totally reliable non-invasive diagnostic tests for primary progressive aphasia. Whether or not the aphasia is “pure”, that is, unaccompanied by other cognitive impairments, may in some cases be difficult to establish through psychological assessments because aphasia can affect performance on “non-language “ (e.g., memory) portions of the test. CT scans, MRI, EEG (electroencephalography) often suggest left hemispheric damage, but these tests may also be normal even though the person has primary progressive aphasia. “Metabolic” imaging studies such as single photon emission computed tomography (SPECT), positron emission tomography (PET), and Functional MRI indicate left hemispheric dysfunction when a person has primary progressive aphasia, but other disorders with different symptoms may also cause the same radiologic
abnormalities.
The cause of primary progressive aphasia and other degenerative brain disorders is unknown. A variety of brain abnormalities in people with primary progressive aphasia have been seen during autopsies. These abnormalities have involved the left hemisphere either exclusively or to a much greater extent than the right hemisphere. Most often, brain abnormalities are consistent with Fronto-Temporal-Limbic Dementia, itself a syndrome — not a single disease — with variable symptoms and microscopic abnormalities. Although Fronto-Temporal-Limbic Dementia is usually associated initially with progressive changes in personality, sometimes it presents as primary progressive aphasia, personality deterioration occurring years later. Alzheimer’s disease has been proven the cause of primary progressive aphasia in a minority of patients. People with primary progressive aphasia due to Alzheimer’s disease usually have fluent aphasia.
Primary Progressive Aphasia Treatment
There is currently no cure for primary progressive aphasia.
The primary approaches to managing primary progressive aphasia at this time are behavioral. That is, there are things that the person with primary progressive aphasia can do that may lessen the impact of the disease. Behavioral approaches emphasize practice, drill, and counseling to (1) enhance the ability to communicate, or (2) compensate for the inability to communicate in conventional ways.
Some behavioral approaches for primary progressive aphasia are directed at improving or maintaining (in the short term) impaired language abilities. The decision to pursue this type of therapy should take into account the following considerations. First, the person with primary progressive aphasia must still have some capacity for insight, motivation and learning. Without them the possibility of meaningful improvement is greatly reduced. Also, the individual’s significant others must be motivated and involved as well. They play an important role in working on practice activities beyond formal therapy sessions and in providing cues for using effective communication strategies.
Finally, everyone involved must understand that therapy will not eliminate difficulties with communication. Even if there is improvement in communication ability, it will not reverse the progression of the disease.
The skills targeted for therapy are generally based on three factors: those abilities that are declining, those that may be relatively preserved, and those that are most important to the affected person. In all instances, therapy requires work that might be called “focused exercise of the brain’s language system.”
At this time a small number of reports all of which are based on only one person or a few carefully selected people with primary progressive aphasia – have documented improvements in abilities targeted by therapy. Skills that have improved include comprehension of spoken instructions and questions, production of sentences, retrieval of words, and number reading. It is premature to conclude that such treatments are likely to be effective for many people with primary progressive aphasia. However, these reports do suggest that for some affected individuals, and for some deficits, therapy may be beneficial. Whether these benefits continue beyond the period of formal therapy is not known.
Compensatory Strategies for both Patients and Families
Other behavioral approaches emphasize compensatory strategies that can improve communication, although not necessarily in conventional ways. Compensatory strategies can be “patient-oriented” or “other-oriented,” or a combination of both. Patient-oriented strategies reflect things that the person with primary progressive aphasia can do to enhance communication, such as establishing the topic at the outset of a conversation, using gestures, and using pictures, writing or drawing. “Other-oriented” strategies include paying full attention to the affected person, giving feedback about the need for clarification, providing more time for communication, confirming information, keeping statements relatively brief, and supplementing speech with gestures. Joint efforts on the part of both the person with primary progressive aphasia and others include speaking in environments that are conducive to effective communication (such as face-to-face conversations with minimal noise and other distractions). People with primary progressive aphasia and their significant others often benefit from following the rule that communicating requires everyone’s full attention. The notion that people with primary progressive aphasia require all the fuel in their “language tank” when communicating is a useful analogy and one to keep in mind when engaged in speaking, listening, reading or writing activities.
It can be very helpful to consult with a speech-language pathologist to identify important communication needs, learn how and when compensatory strategies can best be used, and practice their use. The speech-language pathologist can help to identify specific strategies and investigate whether augmentative strategies (for example, gesture, pantomime, and drawing) may supplement or sometimes replace verbal communication. Such strategies have been reported as helpful in some people with primary progressive aphasia.
Electronic/computer devices may be able to supplement or replace speech in some people with primary progressive aphasia. Because they require a person to use conventional language or other symbols, they may not be helpful for those whose language skills are already severely impaired. Some people with primary progressive aphasia also have an apraxia of speech a problem with the programming of movements for speech rather than a language problem). They may have speech that is far more impaired than their language comprehension or ability to read and write. As long as their ability to control movements of body parts needed to use the devices is relatively intact, those with apraxia of speech and relatively mild primary progressive aphasia may be good candidates for electronic/computer alternatives to speech. Generally, the development, practice and learning of augmentative or alternative means of communication should occur well before there is an actual need to use them, so they are readily available and more easily used when and if the need emerges.
Finally, there can be little doubt that simply learning about primary progressive aphasia is beneficial, both psychologically and practically. As discussed above, speech-language pathologists who have experience working with people with aphasia and degenerative neurological diseases can address questions about aphasia in general, and primary progressive aphasia in particular, and can help plan for future communication needs. Free or low-cost evaluations and therapy may be available from university speech language clinics. Some primary progressive aphasia patients and/or spouses benefit from joining an Aphasia Community Group or Stroke Support Group 69 that has others with aphasia in it. This is true even if the others do not have aphasia that is progressive. The National Aphasia Association 68 provides information about primary progressive aphasia and listings of support groups. The American Heart Association resources can make referrals to stroke support groups 70.
Viewed in the most positive sense, the diagnosis of primary progressive aphasia does not mean the end of communication. It can be the first step to identifying ways to maintain communication abilities for as long as possible.
Medications
From the medical perspective, there are currently no drugs or other interventions specifically designed for primary progressive aphasia. This partly reflects doctors limited understanding of what causes primary progressive aphasia and the likelihood that it has more than a single cause. Neurologists sometimes prescribe drugs that are used for people with Alzheimer’s disease under the assumption that primary progressive aphasia and Alzheimer’s disease may share a common cause. This assumption is unlikely to be true in the majority of cases. Currently, there are only anecdotal reports that the same drugs that target Alzheimer’s disease are helpful in relieving the signs and symptoms of primary progressive aphasia.
Aphasia prognosis
The outcome of aphasia is difficult to predict given the wide range of variability of the condition and varies significantly from person to person. Generally, people who are younger or have less extensive brain damage fare better 71. The location of the injury is also important and is another clue to prognosis. Other predictors of long-term recovery include age, gender, education level, and other comorbidities 72. In general, people tend to recover skills in language comprehension more completely than those skills involving expression.
Aphasia complications
Aphasia can create numerous quality-of-life problems because communication is so much a part of your life. Communication difficulty may affect your:
- Job
- Relationships
- Day-to-day function
Language barriers may lead to embarrassment, depression, anxiety and relationship problems.
If you’re concerned about someone with aphasia, encourage them to discuss any problems with their doctor or a member of their care team to access the relevant support.
If the person is unable to do this themselves, they may require someone to communicate on their behalf.
Aphasia causes
Aphasia is the result of damage to the parts of the brain involved in speaking, reading, writing and understanding others. Any damage to the language areas of the brain can result in loss of function, leading to aphasia.
The severity of a person’s aphasia depends on the location and type of injury sustained by the brain.
Aphasia can occur by itself or alongside other disorders, such as visual difficulties, mobility problems, limb weakness and cognitive changes.
Aphasia affects a person’s language, but it doesn’t affect a person’s intelligence.
Common causes include:
- Stroke – thought to be the most common cause, around one in three people experience some degree of aphasia after having a stroke 24
- Ischemic stroke caused by a blockage that disrupts blood flow to a region of the brain
- Hemorrhagic stroke caused by a ruptured blood vessel that damages surrounding brain tissue
- Severe head injury
- Brain tumor
- Progressive neurological conditions – conditions that, over time, cause progressive brain and nervous system damage e.g. dementia, progressive supranuclear palsy or corticobasal degeneration
- Infections that affect the brain – such as meningitis (an infection of the outer layer of the brain) and encephalitis (an infection of the brain itself), although this is a much rarer cause of aphasia
- Brain surgery
The most common cause of aphasia is brain damage resulting from a stroke (about 25-40% of stroke survivors acquire aphasia) — the blockage or rupture of a blood vessel in the brain. Loss of blood to the brain leads to brain cell death or damage in areas that control language.
Brain damage caused by a severe head injury, a tumor, an infection or a degenerative process also can cause aphasia. In these cases, the aphasia usually occurs with other types of cognitive problems, such as memory problems or confusion.
Primary progressive aphasia is the term used for language difficulty that develops gradually. This is due to the gradual degeneration of brain cells located in the language networks. Sometimes this type of aphasia will progress to a more generalized dementia.
Sometimes temporary episodes of aphasia can occur. These can be due to migraines, seizures or a transient ischemic attack (TIA). A TIA occurs when blood flow is temporarily blocked to an area of the brain. People who’ve had a transient ischemic attack (TIA) are at an increased risk of having a stroke in the near future.
Aphasia prevention
You can help prevent aphasia by:
- Making heart-healthy lifestyle changes to lower your chance of having:
- A stroke
- Heart disease
- Vascular disease (problems with your blood vessels)
- Protecting your brain from injury:
- Wearing the right helmet for sports safety, such as when riding a bike
- Taking action to prevent falls
- Always wearing your seatbelt and driving safely
Aphasia symptoms
Aphasia is a sign of some other condition, such as a stroke or a brain tumor.
In cases where aphasia has been caused by a sudden brain injury, such as a stroke or a severe head injury, symptoms will usually develop straight after the injury.
In cases where there is gradual damage to the brain as a result of a condition that gets worse over time, such as dementia or a brain tumour, the symptoms may develop gradually.
A person with aphasia may:
- Speak in short or incomplete sentences
- Speak in sentences that don’t make sense
- Substitute one word for another or one sound for another
- Speak unrecognizable words
- Not understand other people’s conversation
- Write sentences that don’t make sense
The severity and scope of the problems depend on the extent of damage and the area of the brain affected.
Expressive aphasia
Someone with expressive aphasia experiences difficulty communicating their thoughts, ideas and messages to others.
This may affect speech, writing, gestures or drawing, and causes problems with everyday tasks such as using the telephone, writing an email, or speaking to family and friends.
People with expressive aphasia may have some of the following signs and symptoms:
- slow and halting speech
- they may struggle to get certain words out, such as the names of objects, places or people
- the content of their speech is stripped down to simple elements and only contains basic nouns and verbs – for example, “want drink” or “go town today”
- spelling or grammatical errors
- using the wrong word, such as saying “chair” instead of “table”
- difficulty constructing a sentence
- being able to write or speak fluently, using long sentences, but often including nonsense words or their speech lacks meaning
Receptive aphasia
A person with receptive aphasia experiences difficulty understanding things they hear or read. They may also have difficulty interpreting gestures, drawings, numbers and pictures.
This can affect everyday activities such as reading an email, managing finances, having conversations, listening to the radio, or following TV programmes.
People with receptive aphasia may have some of the following signs and symptoms:
- difficulty understanding what people say
- difficulty understanding written words
- misinterpreting the meaning of words, gestures, pictures or drawings
- giving responses that may not make sense if they’ve misunderstood questions or comments
- not being aware of their difficulties with understanding
Primary progressive aphasia
This type of aphasia occurs in people with a specific type of dementia. As it’s a primary progressive condition, the symptoms get worse over time.
Usually, the first problem people with primary progressive aphasia (primary progressive aphasia) notice is difficulty finding the right word or remembering somebody’s name.
The problems gradually get worse and can include:
- speech becoming hesitant and difficult, and making mistakes with the sounds of words or grammar
- speech becomes slow with short, simple sentences
- forgetting the meaning of complicated words, and later also simple ones, making it more difficult for them to understand other people
- speech becomes more vague, and the person has difficulty being specific or clarifying what they’re saying
- becoming less and less likely to join in with or start conversations
A person with primary progressive aphasia may also experience other symptoms later in their illness, including changes in their personality and behaviour, difficulties with memory and thinking similar to Alzheimer’s disease, or difficulties with movement similar to Parkinson’s disease.
Can a person have Aphasia without having a physical disability?
Yes, but many people with aphasia also have weakness or paralysis of their right leg and right arm. When a person acquires aphasia it is usually due to damage on the left side of the brain, which controls movements on the right side of the body.
Aphasia diagnosis
You should see a doctor if you are having trouble speaking or understanding what people say. A doctor will determine if there is a medical cause for your problem. Professionals known as speech-language pathologists play a key role in diagnosing and treating aphasia. A speech-language pathologist will test your speech and language skills. Because there is no single symptom or test that can be used to diagnose aphasia, the person making the diagnosis generally looks for the presence of several of a group of symptoms, including those described earlier. Ruling out other conditions, such as muscle weakness or language production problems, can help with the diagnostic process.
Your speech and language therapist will likely give you a physical and a neurological exam, test your strength, feeling and reflexes, and listen to your heart and the vessels in your neck. He or she will likely request an imaging test, usually an MRI scan, to quickly identify what’s causing the aphasia.
The following tests may be done if the cause of the disorder is not known:
- CT or MRI scans of the brain may help show a tumor, stroke, or other brain injury.
- An electroencephalogram (EEG) may be used to rule out epilepsy as a cause of the aphasia.
- A spinal tap or lumbar puncture may be done to check for inflammation or an infection that affects the brain.
Standardized language and intellectual tests should be done if apraxia of speech is suspected. Testing for other learning disabilities may also be needed.
You’ll also likely undergo tests and informal observations to assess your language skills, such as the ability to:
- Name common objects
- Engage in a conversation
- Understand and use words correctly
- Answer questions about something read or heard
- Repeat words and sentences
- Follow instructions
- Answer yes-no questions and respond to open-ended questions about common subjects
- Read and write.
The Boston Diagnostic Aphasia Examination, 3rd edition (BDAE) 73 and the Western Aphasia Battery – Revised (WAB-R) 74 are the most common comprehensive aphasia assessments. Both the Boston Diagnostic Aphasia Examination, 3rd edition (BDAE) 73 and the Western Aphasia Battery – Revised (WAB-R) 74 allow clinicians to classify patients into syndromes. The BDAE assesses spontaneous speech (conversational and narrative), auditory comprehension, repetition, reading, and writing. The BDAE has a short form that takes about 30-45 minutes to complete, and an extended standard form. The BDAE also includes the Boston Naming Test (BNT), which is a widely used measure of confrontation object naming. Similarly, the WAB-R assesses spoken language production and comprehension, reading and writing, praxis, and constructional and visuospatial skills.
However, a growing number of researchers and clinicians are moving away from the syndrome-based approach. Instead there is an emphasis on identifying specific deficits rather than trying to fit individual patients into a “syndrome” box. In line with this new way of thinking, the Comprehensive Aphasia Test (CAT) 75 is a comprehensive assessment that does not assign patients to syndrome classifications. The CAT consists of an initial screening for cognitive deficits that may impact performance on the aphasia battery, a comprehensive language performance assessment (the main body of the test), and a disability questionnaire. The disability questionnaire asks the individual with aphasia to assess their degree of disability in all four language modalities, and is designed to ascertain the emotional consequences and impact that language difficulties have on their daily life.
Aphasia treatment
If the brain damage is mild, a person may recover language skills without treatment. However, most people undergo speech and language therapy to rehabilitate their language skills and supplement their communication experiences. Researchers are currently investigating the use of medications, alone or in combination with speech therapy, to help people with aphasia.
A speech and language therapist usually diagnoses the condition by testing your language capabilities. They can also help arrange treatment.
Speech and language therapy is the main type of treatment for people with aphasia. This aims to help restore some of your ability to communicate, as well as help you develop alternative ways of communicating, if necessary.
You may receive speech and language therapy on an individual basis or in a group, depending on your needs and the service provided.
An increasing number of computer-based applications are available to support people with aphasia. However, it’s important to start using these with the assistance of a speech and language therapist.
How successful treatment is differs from person to person, but most people with aphasia make some degree of recovery, and some recover fully. Even if aphasia persists, it does not mean a person is unable to live an independent and meaningful life.
However, the chances of recovery for people with aphasia related to progressive neurological conditions is poor. This is because there is no way of repairing or preventing the ongoing injury to the brain.
When aphasia is caused by a progressive condition, treatment focuses on making the most of what people can still do and developing other ways of communicating to prepare for a time when speaking will be more difficult.
Speech and language rehabilitation
Recovery of language skills is usually a relatively slow process. Although most people make significant progress, few people regain full pre-injury communication levels.
For aphasia, speech and language therapy tries to improve the person’s ability to communicate by restoring as much language as possible, teaching how to compensate for lost language skills and finding other methods of communicating.
Evidence suggests speech and language therapy is more effective if it’s started as soon as possible.
For many people, the most obvious recovery happens in the first six months. However, improvements can continue to be seen for much longer after this, even many years later.
How the therapy is carried out will depend on your circumstances. An intensive course of speech and language therapy may be recommended for some people. This involves a number of sessions spread out over a shorter period of time.
However, speech and language therapy can be exhausting, and an intensive course of treatment will not be suitable for everyone. For some people, shorter and less intensive sessions may be recommended.
Therapy may be individual sessions, groups, or using technology such as computer programmes or apps.
Therapy:
- Starts early. Some studies have found that therapy is most effective when it begins soon after the brain injury.
- Often works in groups. In a group setting, people with aphasia can try out their communication skills in a safe environment. Participants can practice initiating conversations, speaking in turn, clarifying misunderstandings and fixing conversations that have completely broken down.
- May include use of computers. Using computer-assisted therapy can be especially helpful for relearning verbs and word sounds (phonemes).
Speech and language therapy techniques
The specific techniques used and the aims of the treatment will depend on each person’s circumstances. Some examples are described below.
If you have difficulty understanding words, your speech and language therapist may ask you to carry out tasks such as matching words to pictures or sorting words by their meaning.
The aim of these tasks is to improve your ability to remember meanings and link them with other words.
If you have difficulty expressing yourself, your speech and language therapist may ask you to practise naming pictures or judge whether certain words rhyme. They may also ask you to repeat words that they say, with prompting if necessary.
If you are able to complete tasks with single words, your therapist will work on your ability to construct sentences.
Some techniques may involve working with a computer. Other methods may include group therapy with other people with aphasia, or working with family members.
This will allow you to practise conversational skills or rehearse common situations, such as making a telephone call.
An increasing number of computer-based programmes and apps are available to help people with aphasia improve their language abilities.
However, it’s important to start using these alongside a speech and language therapist.
Alternative methods of communication
An important part of speech therapy is finding different ways for you to communicate. Your therapist will help you develop alternatives to talking, such as using gesture, writing, drawing or communication charts.
Communication charts are large grids containing letters, words or pictures. They allow someone with aphasia to communicate by pointing at the word or letter to indicate what they want to say.
For some people, specially designed electronic devices, such as voice output communication aids (VOCAs), may be useful. Voice output communication aids use a computer-generated voice to play messages aloud.
This can help if you have difficulty speaking but are able to write or type. There are also apps available on smartphones and computer tablets that can do this.
If a communication device is felt to be beneficial, funding for the purchase of an individual device can be discussed with a speech and language therapist.
Constraint-induced therapies (CIT) have received a good deal of attention in the popular press recently.
An early researcher, Dr. Edward Taub, examined the notion that much of the long-term disability of stroke survivors resulted from a learned tendency to avoid using the impaired arm and hand, instead of focusing on compensating by using the remaining good limb. Taub proposed the term “learned non-use” to describe this process by which the survivor increasingly avoids using the impaired limb and is thus unable to capitalize on the value this limb might offer.
Principles of constraint-induced therapies (CIT)
Based on this theory, Dr. Taub developed a set of treatment principles designed to counteract learned non-use and enhance the underlying residual abilities of the impaired limb. There were three treatment principles:
- Constraint – avoid the compensation, in this case, by tying down the good limb (paw) of the animals he studied;
- Forced use – require use of the impaired limb by placing the animals in circumstances where they needed to use it to achieve a meaningful goal (for example, acquiring food pellets); and
- Massed practice – require the constraint and forced use every day and all day long.
In the last decade, Dr. Taub and many others have applied these three principles to humans. Results of these experiments suggest constraint-induced therapies (CIT) is helpful in some cases. Emerging results of a randomized controlled trial by Dr. Steve Wolf of Emory University and others endorse the value of this approach at least with regard to arm rehabilitation.
Constraint-induced therapies (CIT) and aphasia
Recently these same constraint-induced therapies (CIT) principles have been applied to aphasia rehabilitation. In speech therapy, constraint means avoiding the use of compensatory strategies such as gesturing, drawing, writing, etc. Forced use means communicating only by talking; and massed practice refers to therapy occurring 2–4 hours per day.
The activities used in applying CIT principles to aphasia rehabilitation don’t differ substantially from what might be found in more traditional treatment approaches. However, what does differ are the demands placed on the speaker in the context of relevant, communicative exchange.
Preliminary investigations suggest that constraint-induced therapies (CIT) principles may be effective in aphasia rehabilitation. However, this investigation is only beginning, and scientists are not able to say any more about its efficacy than that in some cases it appears to be helpful. Not only will further study be needed to confirm that CIT is effective with aphasia, these same studies are needed to confirm its safety. For example, some of the animal work by Dr. Tim Shallart and colleagues suggested that intensive CIT may be harmful when performed too early after a stroke. Thus the application of CIT to aphasia rehabilitation must be pursued with both enthusiasm and caution.
Evaluating new treatment approaches
Whenever a new intervention or approach to rehabilitation is considered, it is best to gather as much information as possible. Before beginning any rehabilitation program, you should determine that the provider is qualified, informed and experienced. However, when considering a product or program that is new or experimental, such as CIT applied to aphasia rehabilitation, it is equally important to evaluate how the program is portrayed and the evidence that supports it. Testimonials on promotional materials and uncontrolled case reports are considered the lowest level of evidence and should be supported by research published in professional journals.
Research is currently being carried out to study whether other treatments can benefit people with aphasia.
These include:
- medication – such as piracetam, bifemelane, piribedil, bromocriptine and idebenone
- transcranial magnetic stimulation – where an electromagnet placed on the scalp is stimulated for a short time using an electric current to stimulate parts of the brain affected by aphasia
Although some studies have suggested these treatments may benefit some people with aphasia, further research is necessary.
Medications
Certain drugs are currently being studied for the treatment of aphasia. These include drugs that may improve blood flow to the brain, enhance the brain’s recovery ability or help replace depleted chemicals in the brain (neurotransmitters). Several medications, such as memantine (Namenda) and piracetam, have shown promise in small studies. But more research is needed before these treatments can be recommended.
Coping and support
People with aphasia
If you have aphasia, the following tips may help you communicate with others:
- Carry a card explaining that you have aphasia and what aphasia is.
- Carry identification and information on how to contact significant others.
- Carry a pencil and a small pad of paper with you at all times.
- Use drawings, diagrams or photos as shortcuts.
- Use gestures or point to objects.
Family and friends
Family members and friends can use the following tips when communicating with a person with aphasia:
- Simplify your sentences and slow your pace.
- Ask yes/no questions.
- Paraphrase periodically during conversation.
- Modify the length and complexity of conversations.
- Use gestures to emphasize important points.
- Establish a topic before beginning conversation.
- Keep conversations one-on-one initially.
- Allow the person time to talk.
- Don’t finish sentences or correct errors.
- Reduce distracting noise in the environment. Practice conversation in a quiet, distraction-free environment.
- Keep paper and pencils or pens available.
- Write a key word or a short sentence to help explain something.
- Help the person with aphasia create a book of words, pictures and photos to assist with conversations.
- Use drawings or gestures when you aren’t understood.
- Involve the person with aphasia in conversations as much as possible.
- Check for comprehension or summarize what you’ve discussed.
Communication Strategies: Some Dos and Don’ts
The impact of aphasia on relationships may be profound, or only slight. No two people with aphasia are alike with respect to severity, former speech and language skills, or personality. But in all cases it is essential for the person to communicate as successfully as possible from the very beginning of the recovery process.
Here are some suggestions to help communicate with a person with aphasia:
- Make sure you have the person’s attention before you start.
- Minimize or eliminate background noise (TV, radio, other people).
- Keep your own voice at a normal level, unless the person has indicated otherwise.
- Keep communication simple, but adult. Simplify your own sentence structure and reduce your rate of speech. Emphasize key words. Don’t “talk down” to the person with aphasia.
- Give them time to speak. Resist the urge to finish sentences or offer words.
- Communicate with drawings, gestures, writing and facial expressions in addition to speech.
- Confirm that you are communicating successfully with “yes” and “no” questions.
- Praise all attempts to speak and downplay any errors. Avoid insisting that that each word be produced perfectly.
- Engage in normal activities whenever possible. Do not shield people with aphasia from family or ignore them in a group conversation. Rather, try to involve them in family decision-making as much as possible. Keep them informed of events but avoid burdening them with day to day details.
- Encourage independence and avoid being overprotective.
Support groups
Local chapters of such organizations as the National Aphasia Association 68, the American Stroke Association, the American Heart Association and some medical centers may offer support groups for people with aphasia and others affected by the disorder. These groups provide people with a sense of community, a place to air frustrations and learn coping strategies. Ask your doctor or speech-language pathologist if he or she knows of any local support groups.
Medications
Drug therapy for aphasia are mainly designed to strengthen networks subserving language and language-related cognitive functions such as attention and memory 76. Pharmacological agents are increasingly used alone and in combination with speech and language therapy to boost language recovery. The theoretical rationale for drug therapy in aphasia is based on the notion that re-establishing the activity of specific neurotransmitters that are dysfunctional, but not irretrievably damaged, brain regions may strengthen neural activity in networks mediating attention, word learning, and memory 77.
Catecholaminergic, cholinergic, nootropic and serotonergic drugs are the main classes of drugs investigated for the treatment of aphasia. Bromocriptine, a catecholaminergic drug has been the most studied drug for patients with aphasia. Positive effects of Bromocriptine have been seen mainly in non-fluent chronic aphasias 78, 79, but these studies were mostly case studies or open label trials. In addition, language gains were only specific to certain language subtests, but were not effective in moderate to severe cases. Randomized, double-blind controlled trials failed to replicate positive results of Bromocriptine 80, 81. It should be noted that the use of bromocriptine is no longer recommended due to high frequency of contraindications (> 40 %) 82 and the increased risk of inducing off-target effects such as valvular heart disease 83 and painful hemidystonia in aphasic persons with hemiparesis 84.
Donepezil is the mostly commonly investigated cholinergic drug in the treatment of aphasia. Cholinergic agents specifically acetylcholinesterase inhibitors such as Donepezil, are widely used in the treatment of Alzheimer’s disease. Donepezil has been reported to result in improvement of spontaneous speech, naming and comprehension in chronic post-stroke aphasia in randomized trials, open label trials, and case studies 85, 86. It also has a well-tolerated safety profile. Piracetam, the nootropic agent is another drug that is commonly used in the treatment of aphasia 87, 88. However, studies assessing the efficacy of piracetam on post-stroke aphasia have produced inconsistent results 89. In addition, piracetam acts on the initial phase of stroke 90, but its beneficial effects disappear in the chronic stage 87. Memantine is an uncompetitive N-methyl-D-aspartate (NMDA) receptor antagonist. Like Piracetam, the initial enthusiasm to evaluate the potential efficacy of memantine in post-stroke aphasia was prompted by the beneficial effects obtained with this drug in language and communication among patients with Alzheimer’s disease 76. Two studies showed that memantine alone and combined with constraint-induced aphasia therapy improved aphasia severity 91, 92.
Interest in serotonin selective reuptake inhibitors (SSRIs) after stroke has been renewed by a better knowledge of post-stroke depression. The issue of depression is important to consider in the treatment of post-stroke aphasia. There is a high rate of post-stroke depression ranging from 30-60% of stroke survivors 93. Furthermore, untreated depression can impede not only language performance, but also motivation to participate in speech and language therapy 94. The SSRI fluvoxamine has showed significant improvements in naming, reduced perseverations, and mood after a 4-week treatment compared to controls 95. A recent study showed that patients with damage to left posterior superior temporal gyrus and/or superior longitudinal fasciculus/arcuate fasciculus showed better naming outcome if they took SSRIs for 3 months after stroke 96.
It is important to keep in mind that drugs prescribed for the treatment of other diseases or stroke complications (e.g. epilepsy) can interfere with aphasia recovery 97. For example, although seizures are common following stroke, anticonvulsant drugs such as the use of topiramate and zonisamide should not be recommended as first-choice medications because they can impair attention, psychomotor speed, short-term and working memories, as well as expressive language 98.
Reperfusion therapies
Over the last two decades, various therapeutic approaches have been developed for treating acute ischemic stroke. Reperfusion therapies are medical treatments in acute stroke that restore blood flow either by surgical removal of a blood clot or with medications that dissolve clots. Reperfusion therapies, particularly intravenous thrombolysis with recombinant tissue plasminogen activator (rTPA), have been shown to be effective in improving language after acute ischemic stroke in the left hemisphere 99, 100. For example, a recent study in patients with ischemic stroke showed significantly higher percentage of resolved aphasia in patients treated with recombinant tissue plasminogen activator (rtPA) compared to the non-treated group, and a higher percentage of global aphasia was observed in the non-treated group compared to treated patients 101. However, many stroke patients do not receive this treatment due to the narrow treatment window (<4.5 hours) 102.
Carotid stenting, with or without angioplasty, is a common procedure to restore blood flow, prevent stroke, and/or improve tissue function. For example, Hillis and colleagues 103 have shown that acute aphasia resolved after left carotid stenting associated with reperfusion of the language cortex. Increasing blood pressure is another approach that investigators have used to improve stroke symptoms. In a series of studies, Hillis et al. 104, 105 showed that restoring blood flow to specific cortical regions in the left hemisphere after acute stroke results in improved language performance.
Non-invasive brain stimulation
There has been an increasing interest in the use of non-invasive brain stimulation techniques (NIBS) such as transcranial direct current stimulation (tDCS) and transcranial magnetic stimulation (TMS) to enhance recovery of aphasia. This interest stems from the growing body of evidence indicating that non-invasive brain stimulation techniques can induce long-lasting changes in neural excitability resulting in functional reorganization and improved speech and language performance.
Transcranial direct current stimulation
Transcranial direct current stimulation (tDCS) is usually administered via saline-soaked surface sponge electrodes attached to the scalp and connected to a direct current stimulator with low intensities (1-2 mA). transcranial direct current stimulation can increase or decrease cortical excitability due to a shift of the resting membrane potential of the nerve cells in the brain 106. Anodal stimulation typically increases cortical excitability, whereas cathodal stimulation lowers cortical excitability. The majority of the transcranial direct current stimulation studies in aphasia have focused on excitatory, anodal stimulation applied to the left hemisphere perilesional or ipsilesional regions 107, 108, 109. Other transcranial direct current stimulation studies have focused on inhibitory, cathodal stimulation to the healthy right hemisphere regions to inhibit cross-hemisphere inhibition, allowing greater activation of the lesioned left hemisphere 110. A few studies have focused on bihemispheric transcranial direct current stimulation, aiming at concomitantly increasing left hemisphere excitability with anodal stimulation and decreasing right hemisphere excitability with cathodal stimulation 111, 112. The newest approach to neuromodulation for aphasia is targeting the right cerebellum 113, 114, a region that is structurally and functionally connected to the left hemisphere language region. This is particularly well suited for patients who have large left hemisphere stroke where it may be difficult to find viable tissue to stimulate in the left hemisphere.
The results of transcranial direct current stimulation studies in aphasia have been mostly positive indicating that transcranial direct current stimulation can augment aphasia therapy; however, the majority of the studies are small. So far, only two transcranial direct current stimulation studies have included more than 50 patients 115, 108. The largest clinical trial of transcranial direct current stimulation to augment naming treatment for post stroke aphasia was done by Fridriksson and colleagues 108 using a randomized, double-blind, sham-controlled design. In this study of 74 chronic stroke patients with aphasia, transcranial direct current stimulation electrode placement was individualized for each participant based on the area of greatest activation in the left hemisphere during spoken naming pre-treatment functional magnetic resonance imaging (fMRI). Patients received 15 sessions of transcranial direct current stimulation combined with computerized aphasia treatment. transcranial direct current stimulation was associated with significantly greater change in number of correctly naming pictured objects compared to sham. Spielmann and colleagues 115 studied the effect of transcranial direct current stimulation on naming outcome in 58 patients with subacute (first three months) post stroke aphasia. Using a randomized, double-blind, sham-controlled design, participants received anodal stimulation to the left inferior frontal gyrus combined with naming treatment for 10 days. The study by Spielmann and colleagues 115 failed to show significant effects of transcranial direct current stimulation. The authors hypothesized that an effect of transcranial direct current stimulation might be difficult to achieve in the subacute phase, as spontaneous recovery is rather high in this phase compared with the relatively stable chronic phase.
Transcranial magnetic stimulation
Transcranial magnetic stimulation (TMS) is a non-invasive brain stimulation method that induces changes in neuronal firing via electromagnetic induction. Typically, a brief and strong current is delivered through a stimulation coil over the scalp, which induces a perpendicular time-varying magnetic field that penetrates the scalp without attenuation. This magnetic field will induce a weak and short-lived current at the site of stimulation 27. Repetitive transcranial magnetic stimulation (rTMS) can be delivered at both high frequency (excitatory) and low frequency (inhibitory).
The majority of transcranial magnetic stimulation studies have applied low-frequency rtranscranial magnetic stimulation to right hemisphere regions to inhibit right hemisphere activation during language-related tasks and to encourage perilesional left hemisphere activation 116, 117, 118. Other studies have focused on facilitating activation of residual left hemisphere regions 119 or facilitating activation of right hemisphere regions 120 via high frequency rtranscranial magnetic stimulation. Theta burst stimulation (TBS) is another type of rtranscranial magnetic stimulation protocol that has recently gained interest. Theta burst stimulation (TBS) protocols induce robust, long-lasting changes in activation in much shorter time periods than are necessary for traditional rtranscranial magnetic stimulation 121.
Both low-frequency and high-frequency repetitive transcranial magnetic stimulation have been beneficial in improving language outcomes for subacute and chronic aphasia. However, the majority of studies are small. There are only a few relatively large randomized sham-controlled trials 117, 122. Hu et al. 122 showed that that both high and low frequency rtranscranial magnetic stimulation of the right IFG can be effective in chronic post stroke aphasia. Ren et al. 117, results indicate that inhibitory low frequency rtranscranial magnetic stimulation of right inferior frontal gyrus and right superior temporal gyrus both lead to language improvements in subacute aphasia, demonstrating that targets beyond right inferior frontal gyrus can be effective.
Both transcranial direct current stimulation and transcranial magnetic stimulation are promising tools for the treatment of aphasia. However, it is unclear which approach is beneficial for improving language skills. There is an increased interest in using transcranial direct current stimulation compared to transcranial magnetic stimulation because transcranial direct current stimulation (tDCS) is less expensive and portable; and does not carry a risk of inducing seizures 123, 124. In addition, transcranial direct current stimulation (tDCS) is more easily paired with simultaneous speech therapy, making it more amenable to widespread clinical use.
References- Aphasia. https://www.asha.org/public/speech/disorders/aphasia
- Cattaneo L. Language. Handb Clin Neurol. 2013;116:681-91. doi: 10.1016/B978-0-444-53497-2.00054-1
- Fridriksson J, Fillmore P, Guo D, Rorden C. Chronic Broca’s Aphasia Is Caused by Damage to Broca’s and Wernicke’s Areas. Cereb Cortex. 2015 Dec;25(12):4689-96. doi: 10.1093/cercor/bhu152
- Aphasia Definitions. https://www.aphasia.org/aphasia-definitions
- Sheppard SM, Sebastian R. Diagnosing and managing post-stroke aphasia. Expert Rev Neurother. 2021 Feb;21(2):221-234. doi: 10.1080/14737175.2020.1855976
- Park JE. Apraxia: Review and Update. J Clin Neurol. 2017 Oct;13(4):317-324. doi: 10.3988/jcn.2017.13.4.317
- Apraxia. https://rarediseases.org/rare-diseases/apraxia
- Gross RG, Grossman M. Update on apraxia. Curr Neurol Neurosci Rep. 2008 Nov;8(6):490-6. doi: 10.1007/s11910-008-0078-y
- Zadikoff C, Lang AE. Apraxia in movement disorders. Brain. 2005 Jul;128(Pt 7):1480-97. doi: 10.1093/brain/awh560
- Donkervoort M, Dekker J, van den Ende E, Stehmann-Saris JC, Deelman BG. Prevalence of apraxia among patients with a first left hemisphere stroke in rehabilitation centres and nursing homes. Clin Rehabil. 2000 Apr;14(2):130-6. doi: 10.1191/026921500668935800
- Wheaton LA, Hallett M. Ideomotor apraxia: a review. J Neurol Sci. 2007 Sep 15;260(1-2):1-10. doi: 10.1016/j.jns.2007.04.014
- Kasselimis DS, Simos PG, Peppas C, Evdokimidis I, Potagas C. The unbridged gap between clinical diagnosis and contemporary research on aphasia: A short discussion on the validity and clinical utility of taxonomic categories. Brain Lang. 2017 Jan;164:63-67. doi: 10.1016/j.bandl.2016.10.005
- Yourganov G, Smith KG, Fridriksson J, Rorden C. Predicting aphasia type from brain damage measured with structural MRI. Cortex. 2015 Dec;73:203-15. doi: 10.1016/j.cortex.2015.09.005
- Classification of Aphasia. https://www.asha.org/siteassets/practice-portal/aphasia/common-classifications-of-aphasia.pdf
- Ardila, Alfredo. (2014). Aphasia Handbook. https://www.researchgate.net/publication/266558490_Aphasia_Handbook
- Acharya AB, Wroten M. Broca Aphasia. [Updated 2022 May 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK436010
- Ali N, Rafi MS, Ghayas Khan MS, Mahfooz U. The effectiveness of script training to restore lost communication in a patient with Broca’s aphasia. J Pak Med Assoc. 2018 Jul;68(7):1070-1075
- Hartwigsen G, Saur D. Neuroimaging of stroke recovery from aphasia – Insights into plasticity of the human language network. Neuroimage. 2019 Apr 15;190:14-31. doi: 10.1016/j.neuroimage.2017.11.056
- Foundas AL, Leonard CM, Gilmore RL, Fennell EB, Heilman KM. Pars triangularis asymmetry and language dominance. Proc Natl Acad Sci U S A. 1996 Jan 23;93(2):719-22. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC40120/pdf/pnas01506-0184.pdf
- Tomaiuolo F, MacDonald JD, Caramanos Z, Posner G, Chiavaras M, Evans AC, Petrides M. Morphology, morphometry and probability mapping of the pars opercularis of the inferior frontal gyrus: an in vivo MRI analysis. Eur J Neurosci. 1999 Sep;11(9):3033-46. doi: 10.1046/j.1460-9568.1999.00718.x
- Rasmussen T, Milner B. The role of early left-brain injury in determining lateralization of cerebral speech functions. Ann N Y Acad Sci. 1977 Sep 30;299:355-69. doi: 10.1111/j.1749-6632.1977.tb41921.x
- Kang EK, Sohn HM, Han MK, Kim W, Han TR, Paik NJ. Severity of post-stroke aphasia according to aphasia type and lesion location in Koreans. J Korean Med Sci. 2010 Jan;25(1):123-7. doi: 10.3346/jkms.2010.25.1.123
- Acharya AB, Wroten M. Wernicke Aphasia. [Updated 2022 May 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441951
- Fridriksson J, den Ouden DB, Hillis AE, Hickok G, Rorden C, Basilakos A, Yourganov G, Bonilha L. Anatomy of aphasia revisited. Brain. 2018 Mar 1;141(3):848-862. doi: 10.1093/brain/awx363
- Binder JR. Current Controversies on Wernicke’s Area and its Role in Language. Curr Neurol Neurosci Rep. 2017 Aug;17(8):58. doi: 10.1007/s11910-017-0764-8
- Bonilha L, Fridriksson J. Home-based therapy for chronic Wernicke’s aphasia. J Neurol Neurosurg Psychiatry. 2017 Jul;88(7):539. doi: 10.1136/jnnp-2017-315842
- Hartwigsen G. The neurophysiology of language: Insights from non-invasive brain stimulation in the healthy human brain. Brain Lang. 2015 Sep;148:81-94. doi: 10.1016/j.bandl.2014.10.007
- Goodglass, H. (1993). Understanding aphasia. New York: Academic Press
- Berthier, M. (1999). Transcortical aphasias. Hove, UK: Psychology Press.
- Boatman D, Gordon B, Hart J, Selnes O, Miglioretti D, Lenz F. Transcortical sensory aphasia: revisited and revised. Brain. 2000 Aug;123 ( Pt 8):1634-42. doi: 10.1093/brain/123.8.1634
- Damasio, H. (1991). Neuroanatomical correlates of the aphasias. In M. Taylor Sarno (Ed.), Acquired aphasia. New York: Academic Press.
- Davis GA. Aphasiology: Disorders and Clinical Practice. 2nd Ed Boston: Pearson; 2007
- Alexander MP, Hiltbrunner B, Fischer RS. Distributed anatomy of transcortical sensory aphasia. Arch Neurol. 1989 Aug;46(8):885-92. doi: 10.1001/archneur.1989.00520440075023
- Alexander MP, Naeser MA, Palumbo CL. Correlations of subcortical CT lesion sites and aphasia profiles. Brain. 1987 Aug;110 ( Pt 4):961-91. doi: 10.1093/brain/110.4.961
- Benson, D. F., & Ardila, A. (1996). Aphasia: A clinical perspective. New York: Oxford University Press.
- Kertesz, A. (1979). Aphasia and associated disorders. New York: Grune & Stratton.
- Dronkers, N. F., & Larsen, J. (2001). Neuroanatomy of the classical aphasia syndromes. In R. D. Berndt (Ed.), Handbook of neuropsychology, vol 3: Language and aphasia. Amsterdam: Elsevier.
- Crosson B, Ford A, Raymer AM. Transcortical motor aphasia In: Raymer AM, Gonzalez Rothi LJ, editors. Handbook of aphasia and language disorders Oxford University Press, New York: New York: Oxford University Press; 2017
- Alexander MP. Impairments of procedures for implementing complex language are due to disruption of frontal attention processes. J Int Neuropsychol Soc. 2006 Mar;12(2):236-47. doi: 10.1017/S1355617706060309
- Fridriksson J, Nettles C, Davis M, Morrow L, Montgomery A. Functional communication and executive function in aphasia. Clin Linguist Phon. 2006 Aug;20(6):401-10. doi: 10.1080/02699200500075781
- Carota A, Annoni JM, Marangolo P. Repeating through the insula: evidence from two consecutive strokes. Neuroreport. 2007 Aug 27;18(13):1367-70. doi: 10.1097/WNR.0b013e328277ef72
- Cauquil-Michon C, Flamand-Roze C, Denier C. Borderzone strokes and transcortical aphasia. Curr Neurol Neurosci Rep. 2011 Dec;11(6):570-7. doi: 10.1007/s11910-011-0221-z
- Ardila A. A review of conduction aphasia. Curr Neurol Neurosci Rep. 2010 Nov;10(6):499-503. doi: 10.1007/s11910-010-0142-2
- Chang EF, Raygor KP, Berger MS. Contemporary model of language organization: an overview for neurosurgeons. J Neurosurg. 2015 Feb;122(2):250-61. doi: 10.3171/2014.10.JNS132647
- Jiménez de la Peña MM, Gómez Vicente L, García Cobos R, Martínez de Vega V. Neuroradiologic correlation with aphasias. Cortico-subcortical map of language. Radiologia (Engl Ed). 2018 May-Jun;60(3):250-261. English, Spanish. doi: 10.1016/j.rx.2017.12.008
- Acharya AB, Maani CV. Conduction Aphasia. [Updated 2022 Jul 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537006
- Benson DF, Sheremata WA, Bouchard R, Segarra JM, Price D, Geschwind N. Conduction aphasia. A clinicopathological study. Arch Neurol. 1973 May;28(5):339-46. doi: 10.1001/archneur.1973.00490230075011
- Bartha L, Benke T. Acute conduction aphasia: an analysis of 20 cases. Brain Lang. 2003 Apr;85(1):93-108. doi: 10.1016/s0093-934x(02)00502-3
- Luria, A. R. (1976). Basic problems of neurolinguistics. New York: Mouton
- Crosson B. Thalamic mechanisms in language: a reconsideration based on recent findings and concepts. Brain Lang. 2013 Jul;126(1):73-88. doi: 10.1016/j.bandl.2012.06.011
- Benson DF, Ardila A. Aphasia, a clinical perspective New York: Oxford University Press; 1996
- Raymer AM, Moberg P, Crosson B, Nadeau S, Rothi LJ. Lexical-semantic deficits in two patients with dominant thalamic infarction. Neuropsychologia. 1997 Feb;35(2):211-9. doi: 10.1016/s0028-3932(96)00069-3
- Cappa SF, Cavallotti G, Guidotti M, Papagno C, Vignolo LA. Subcortical aphasia: two clinical-CT scan correlation studies. Cortex. 1983 Jun;19(2):227-41. doi: 10.1016/s0010-9452(83)80016-1
- Naeser MA, Alexander MP, Helm-Estabrooks N, Levine HL, Laughlin SA, Geschwind N. Aphasia with predominantly subcortical lesion sites: description of three capsular/putaminal aphasia syndromes. Arch Neurol. 1982 Jan;39(1):2-14. doi: 10.1001/archneur.1982.00510130004002
- Radanovic M, Mansur LL. Aphasia in vascular lesions of the basal ganglia: A comprehensive review. Brain Lang. 2017 Oct;173:20-32. doi: 10.1016/j.bandl.2017.05.003
- Choi JY, Lee KH, Na DL, Byun HS, Lee SJ, Kim H, Kwon M, Lee KH, Kim BT. Subcortical aphasia after striatocapsular infarction: quantitative analysis of brain perfusion SPECT using statistical parametric mapping and a statistical probabilistic anatomic map. J Nucl Med. 2007 Feb;48(2):194-200.
- Hillis AE, Barker PB, Wityk RJ, Aldrich EM, Restrepo L, Breese EL, Work M. Variability in subcortical aphasia is due to variable sites of cortical hypoperfusion. Brain Lang. 2004 Jun;89(3):524-30. doi: 10.1016/j.bandl.2004.01.007
- Alexander MP, Fischette MR, Fischer RS. Crossed aphasias can be mirror image or anomalous. Case reports, review and hypothesis. Brain. 1989 Aug;112 ( Pt 4):953-73. doi: 10.1093/brain/112.4.953
- Mariën P, Paghera B, De Deyn PP, Vignolo LA. Adult crossed aphasia in dextrals revisited. Cortex. 2004 Feb;40(1):41-74. doi: 10.1016/s0010-9452(08)70920-1
- Barton JJS. Disorders of higher visual processing In: Kennard C, Leigh RJ, editors. Handbook of Clinical Neurology. Elsevier; 2011. [cited 2020 Jul 15]. p. 223–61. (Neuro-ophthalmology; vol. 102). https://doi.org/10.1016/B978-0-444-52903-9.00015-7
- Hillis AE. Chapter 15 Cognitive processes underlying reading and writing and their neural substrates In: Handbook of Clinical Neurology. Elsevier; 2008. [cited 2020 Jul 15]. p. 311–22. (Neuropsychology and Behavioral Neurology; vol. 88). https://doi.org/10.1016/S0072-9752(07)88015-8
- Hillis AE. Aphasia: progress in the last quarter of a century. Neurology. 2007 Jul 10;69(2):200-13. doi: 10.1212/01.wnl.0000265600.69385.6f
- Rapcsak SZ, Beeson PM. Neuroanatomical correlates of spelling and writing In: The handbook of adult language disorders, 2nd ed New York, NY, US: Psychology Press; 2015. p. 87–116
- Mesulam M. M. Slowly progressive aphasia without dementia. Annals of Neurology, 11:592-598, 1982.
- Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, Ogar JM, Rohrer JD, Black S, Boeve BF, Manes F, Dronkers NF, Vandenberghe R, Rascovsky K, Patterson K, Miller BL, Knopman DS, Hodges JR, Mesulam MM, Grossman M. Classification of primary progressive aphasia and its variants. Neurology. 2011 Mar 15;76(11):1006-14. doi: 10.1212/WNL.0b013e31821103e6
- Habib M, Pelletier J, Khalil R. Aphasie progressive primaire (syndrome de Mesulam) [Primary progressive aphasia (Mesulam syndrome)]. Presse Med. 1993 May 1-8;22(16):757-64. French.
- Tee BL, Gorno-Tempini ML. Primary progressive aphasia: a model for neurodegenerative disease. Curr Opin Neurol. 2019 Apr;32(2):255-265. doi: 10.1097/WCO.0000000000000673
- National Aphasia Association. https://www.aphasia.org/
- Stroke Support Group. http://www.strokeassociation.org
- American Heart Association. https://www.heart.org
- Plowman E, Hentz B, Ellis C Jr. Post-stroke aphasia prognosis: a review of patient-related and stroke-related factors. J Eval Clin Pract. 2012 Jun;18(3):689-94. doi: 10.1111/j.1365-2753.2011.01650.x
- Payabvash S, Kamalian S, Fung S, Wang Y, Passanese J, Kamalian S, Souza LC, Kemmling A, Harris GJ, Halpern EF, González RG, Furie KL, Lev MH. Predicting language improvement in acute stroke patients presenting with aphasia: a multivariate logistic model using location-weighted atlas-based analysis of admission CT perfusion scans. AJNR Am J Neuroradiol. 2010 Oct;31(9):1661-8. doi: 10.3174/ajnr.A2125
- Goodglass H, Barresi B. Boston Diagnostic Aphasia Examination – Third Edition (BDAE-3). San Antonio, TX: Pearson; 2000
- Kertesz A Western Aphasia Battery – Revised. San Antonio, TX: Harcourt Assessment, Inc.; 2007
- Swinburn K, Porter G, Howard D. Comprehensive aphasia test. Taylor & Francis; 2004
- Berthier ML, Pulvermüller F, Dávila G, Casares NG, Gutiérrez A. Drug therapy of post-stroke aphasia: a review of current evidence. Neuropsychol Rev. 2011 Sep;21(3):302-17. doi: 10.1007/s11065-011-9177-7
- Berthier ML, Pulvermüller F. Neuroscience insights improve neurorehabilitation of poststroke aphasia. Nat Rev Neurol. 2011 Feb;7(2):86-97. doi: 10.1038/nrneurol.2010.201
- Bragoni M, Altieri M, Di Piero V, Padovani A, Mostardini C, Lenzi GL. Bromocriptine and speech therapy in non-fluent chronic aphasia after stroke. Neurol Sci. 2000 Feb;21(1):19-22. doi: 10.1007/s100720070114
- Gold M, VanDam D, Silliman ER. An open-label trial of bromocriptine in nonfluent aphasia: a qualitative analysis of word storage and retrieval. Brain Lang. 2000 Sep;74(2):141-56. doi: 10.1006/brln.2000.2332
- Ashtary F, Janghorbani M, Chitsaz A, Reisi M, Bahrami A. A randomized, double-blind trial of bromocriptine efficacy in nonfluent aphasia after stroke. Neurology. 2006 Mar 28;66(6):914-6. doi: 10.1212/01.wnl.0000203119.91762.0c
- Gupta SR, Mlcoch AG, Scolaro C, Moritz T. Bromocriptine treatment of nonfluent aphasia. Neurology. 1995 Dec;45(12):2170-3. doi: 10.1212/wnl.45.12.2170
- Altieri M, Di Piero V, Lenzi GL. Drugs and recovery: a challenge for a few? Stroke. 2002 Apr;33(4):1170; author reply 1170. doi: 10.1161/01.str.0000012265.78381.ed
- Tan LC, Ng KK, Au WL, Lee RK, Chan YH, Tan NC. Bromocriptine use and the risk of valvular heart disease. Mov Disord. 2009 Feb 15;24(3):344-9. doi: 10.1002/mds.22228
- Leiguarda R, Merello M, Sabe L, Starkstein S. Bromocriptine-induced dystonia in patients with aphasia and hemiparesis. Neurology. 1993 Nov;43(11):2319-22. doi: 10.1212/wnl.43.11.2319
- Berthier ML, Green C, Higueras C, Fernández I, Hinojosa J, Martín MC. A randomized, placebo-controlled study of donepezil in poststroke aphasia. Neurology. 2006 Nov 14;67(9):1687-9. doi: 10.1212/01.wnl.0000242626.69666.e2
- Berthier ML, Hinojosa J, Martín Mdel C, Fernández I. Open-label study of donepezil in chronic poststroke aphasia. Neurology. 2003 Apr 8;60(7):1218-9. doi: 10.1212/01.wnl.0000055871.82308.41
- Güngör L, Terzi M, Onar MK. Does long term use of piracetam improve speech disturbances due to ischemic cerebrovascular diseases? Brain Lang. 2011 Apr;117(1):23-7. doi: 10.1016/j.bandl.2010.11.003
- Orgogozo JM. Piracetam in the treatment of acute stroke. Pharmacopsychiatry. 1999 Mar;32 Suppl 1:25-32. doi: 10.1055/s-2007-979233
- Saxena S, Hillis AE. An update on medications and noninvasive brain stimulation to augment language rehabilitation in post-stroke aphasia. Expert Rev Neurother. 2017 Nov;17(11):1091-1107. doi: 10.1080/14737175.2017.1373020
- De Deyn PP, Reuck JD, Deberdt W, Vlietinck R, Orgogozo JM. Treatment of acute ischemic stroke with piracetam. Members of the Piracetam in Acute Stroke Study (PASS) Group. Stroke. 1997 Dec;28(12):2347-52. doi: 10.1161/01.str.28.12.2347
- Barbancho MA, Berthier ML, Navas-Sánchez P, Dávila G, Green-Heredia C, García-Alberca JM, Ruiz-Cruces R, López-González MV, Dawid-Milner MS, Pulvermüller F, Lara JP. Bilateral brain reorganization with memantine and constraint-induced aphasia therapy in chronic post-stroke aphasia: An ERP study. Brain Lang. 2015 Jun-Jul;145-146:1-10. doi: 10.1016/j.bandl.2015.04.003
- Berthier ML, Green C, Lara JP, Higueras C, Barbancho MA, Dávila G, Pulvermüller F. Memantine and constraint-induced aphasia therapy in chronic poststroke aphasia. Ann Neurol. 2009 May;65(5):577-85. doi: 10.1002/ana.21597
- Barker-Collo SL. Depression and anxiety 3 months post stroke: prevalence and correlates. Arch Clin Neuropsychol. 2007 May;22(4):519-31. doi: 10.1016/j.acn.2007.03.002
- Skidmore ER, Whyte EM, Holm MB, Becker JT, Butters MA, Dew MA, Munin MC, Lenze EJ. Cognitive and affective predictors of rehabilitation participation after stroke. Arch Phys Med Rehabil. 2010 Feb;91(2):203-7. doi: 10.1016/j.apmr.2009.10.026
- Tanaka Y, Albert M, Aketa S, et al. Serotonergic Therapy for Fluent Aphasia: P02. 150. Neurology. 2004;62
- Hillis AE, Beh YY, Sebastian R, Breining B, Tippett DC, Wright A, Saxena S, Rorden C, Bonilha L, Basilakos A, Yourganov G, Fridriksson J. Predicting recovery in acute poststroke aphasia. Ann Neurol. 2018 Mar;83(3):612-622. doi: 10.1002/ana.25184
- Marcotte K, Adrover-Roig D, Damien B, de Préaumont M, Généreux S, Hubert M, Ansaldo AI. Therapy-induced neuroplasticity in chronic aphasia. Neuropsychologia. 2012 Jul;50(8):1776-86. doi: 10.1016/j.neuropsychologia.2012.04.001
- Cappa SF, Ortelli P, Garibotto V, Zamboni M. Reversible nonfluent aphasia and left frontal hypoperfusion during topiramate treatment. Epilepsy Behav. 2007 Feb;10(1):192-4. doi: 10.1016/j.yebeh.2006.11.001
- Furlanis G, Ridolfi M, Polverino P, Menichelli A, Caruso P, Naccarato M, Sartori A, Torelli L, Pesavento V, Manganotti P. Early Recovery of Aphasia through Thrombolysis: The Significance of Spontaneous Speech. J Stroke Cerebrovasc Dis. 2018 Jul;27(7):1937-1948. doi: 10.1016/j.jstrokecerebrovasdis.2018.02.043
- Martins IP, Fonseca J, Morgado J, Leal G, Farrajota L, Fonseca AC, Melo TP. Language improvement one week after thrombolysis in acute stroke. Acta Neurol Scand. 2017 Mar;135(3):339-345. doi: 10.1111/ane.12604
- Menichelli A, Furlanis G, Sartori A, Ridolfi M, Naccarato M, Caruso P, Pesavento V, Manganotti P. Thrombolysis’ benefits on early post-stroke language recovery in aphasia patients. J Clin Neurosci. 2019 Dec;70:92-95. doi: 10.1016/j.jocn.2019.08.064
- Zhou Z, Lu J, Liu WW, Manaenko A, Hou X, Mei Q, Huang JL, Tang J, Zhang JH, Yao H, Hu Q. Advances in stroke pharmacology. Pharmacol Ther. 2018 Nov;191:23-42. doi: 10.1016/j.pharmthera.2018.05.012
- Hillis AE, Wityk RJ, Barker PB, Beauchamp NJ, Gailloud P, Murphy K, Cooper O, Metter EJ. Subcortical aphasia and neglect in acute stroke: the role of cortical hypoperfusion. Brain. 2002 May;125(Pt 5):1094-104. doi: 10.1093/brain/awf113
- Hillis AE, Kleinman JT, Newhart M, Heidler-Gary J, Gottesman R, Barker PB, Aldrich E, Llinas R, Wityk R, Chaudhry P. Restoring cerebral blood flow reveals neural regions critical for naming. J Neurosci. 2006 Aug 2;26(31):8069-73. doi: 10.1523/JNEUROSCI.2088-06.2006
- Hillis AE, Ulatowski JA, Barker PB, Torbey M, Ziai W, Beauchamp NJ, Oh S, Wityk RJ. A pilot randomized trial of induced blood pressure elevation: effects on function and focal perfusion in acute and subacute stroke. Cerebrovasc Dis. 2003;16(3):236-46. doi: 10.1159/000071122
- Floel A, Cohen LG. Recovery of function in humans: cortical stimulation and pharmacological treatments after stroke. Neurobiol Dis. 2010 Feb;37(2):243-51. doi: 10.1016/j.nbd.2009.05.027
- Darkow R, Martin A, Würtz A, Flöel A, Meinzer M. Transcranial direct current stimulation effects on neural processing in post-stroke aphasia. Hum Brain Mapp. 2017 Mar;38(3):1518-1531. doi: 10.1002/hbm.23469
- Fridriksson J, Rorden C, Elm J, Sen S, George MS, Bonilha L. Transcranial Direct Current Stimulation vs Sham Stimulation to Treat Aphasia After Stroke: A Randomized Clinical Trial. JAMA Neurol. 2018 Dec 1;75(12):1470-1476. doi: 10.1001/jamaneurol.2018.2287
- Pestalozzi MI, Di Pietro M, Martins Gaytanidis C, Spierer L, Schnider A, Chouiter L, Colombo F, Annoni JM, Jost LB. Effects of Prefrontal Transcranial Direct Current Stimulation on Lexical Access in Chronic Poststroke Aphasia. Neurorehabil Neural Repair. 2018 Oct;32(10):913-923. doi: 10.1177/1545968318801551
- Silva FRD, Mac-Kay APMG, Chao JC, Santos MDD, Gagliadi RJ. Transcranial direct current stimulation: a study on naming performance in aphasic individuals. Codas. 2018 Aug 30;30(5):e20170242. Portuguese, English. doi: 10.1590/2317-1782/20182017242
- Feil S, Eisenhut P, Strakeljahn F, Müller S, Nauer C, Bansi J, Weber S, Liebs A, Lefaucheur JP, Kesselring J, Gonzenbach R, Mylius V. Left Shifting of Language Related Activity Induced by Bihemispheric tDCS in Postacute Aphasia Following Stroke. Front Neurosci. 2019 Apr 26;13:295. doi: 10.3389/fnins.2019.00295
- Marangolo P, Fiori V, Sabatini U, De Pasquale G, Razzano C, Caltagirone C, Gili T. Bilateral Transcranial Direct Current Stimulation Language Treatment Enhances Functional Connectivity in the Left Hemisphere: Preliminary Data from Aphasia. J Cogn Neurosci. 2016 May;28(5):724-38. doi: 10.1162/jocn_a_00927
- Sebastian R, Saxena S, Tsapkini K, Faria AV, Long C, Wright A, Davis C, Tippett DC, Mourdoukoutas AP, Bikson M, Celnik P, Hillis AE. Cerebellar tDCS: A Novel Approach to Augment Language Treatment Post-stroke. Front Hum Neurosci. 2017 Jan 12;10:695. doi: 10.3389/fnhum.2016.00695
- Marangolo P, Fiori V, Caltagirone C, Pisano F, Priori A. Transcranial Cerebellar Direct Current Stimulation Enhances Verb Generation but Not Verb Naming in Poststroke Aphasia. J Cogn Neurosci. 2018 Feb;30(2):188-199. doi: 10.1162/jocn_a_01201
- Spielmann K, van de Sandt-Koenderman WME, Heijenbrok-Kal MH, Ribbers GM. Transcranial Direct Current Stimulation Does Not Improve Language Outcome in Subacute Poststroke Aphasia. Stroke. 2018 Apr;49(4):1018-1020. doi: 10.1161/STROKEAHA.117.020197
- Haghighi M, Mazdeh M, Ranjbar N, Seifrabie MA. Further Evidence of the Positive Influence of Repetitive Transcranial Magnetic Stimulation on Speech and Language in Patients with Aphasia after Stroke: Results from a Double-Blind Intervention with Sham Condition. Neuropsychobiology. 2017;75(4):185-192. doi: 10.1159/000486144
- Ren C, Zhang G, Xu X, Hao J, Fang H, Chen P, Li Z, Ji Y, Cai Q, Gao F. The Effect of rTMS over the Different Targets on Language Recovery in Stroke Patients with Global Aphasia: A Randomized Sham-Controlled Study. Biomed Res Int. 2019 Jul 29;2019:4589056. doi: 10.1155/2019/4589056
- Harvey DY, Podell J, Turkeltaub PE, Faseyitan O, Coslett HB, Hamilton RH. Functional Reorganization of Right Prefrontal Cortex Underlies Sustained Naming Improvements in Chronic Aphasia via Repetitive Transcranial Magnetic Stimulation. Cogn Behav Neurol. 2017 Dec;30(4):133-144. doi: 10.1097/WNN.0000000000000141
- Zhang H, Chen Y, Hu R, Yang L, Wang M, Zhang J, Lu H, Wu Y, Du X. rTMS treatments combined with speech training for a conduction aphasia patient: A case report with MRI study. Medicine (Baltimore). 2017 Aug;96(32):e7399. doi: 10.1097/MD.0000000000007399
- Hara T, Abo M, Kobayashi K, Watanabe M, Kakuda W, Senoo A. Effects of low-frequency repetitive transcranial magnetic stimulation combined with intensive speech therapy on cerebral blood flow in post-stroke aphasia. Transl Stroke Res. 2015 Oct;6(5):365-74. doi: 10.1007/s12975-015-0417-7
- Griffis JC, Nenert R, Allendorfer JB, Szaflarski JP. Interhemispheric Plasticity following Intermittent Theta Burst Stimulation in Chronic Poststroke Aphasia. Neural Plast. 2016;2016:4796906. doi: 10.1155/2016/4796906
- Hu XY, Zhang T, Rajah GB, Stone C, Liu LX, He JJ, Shan L, Yang LY, Liu P, Gao F, Yang YQ, Wu XL, Ye CQ, Chen YD. Effects of different frequencies of repetitive transcranial magnetic stimulation in stroke patients with non-fluent aphasia: a randomized, sham-controlled study. Neurol Res. 2018 Jun;40(6):459-465. doi: 10.1080/01616412.2018.1453980
- Turkeltaub PE. Brain Stimulation and the Role of the Right Hemisphere in Aphasia Recovery. Curr Neurol Neurosci Rep. 2015 Nov;15(11):72. doi: 10.1007/s11910-015-0593-6
- Holland R, Crinion J. Can tDCS enhance treatment of aphasia after stroke? Aphasiology. 2012 Sep;26(9):1169-1191. doi: 10.1080/02687038.2011.616925