What is arachnoiditis
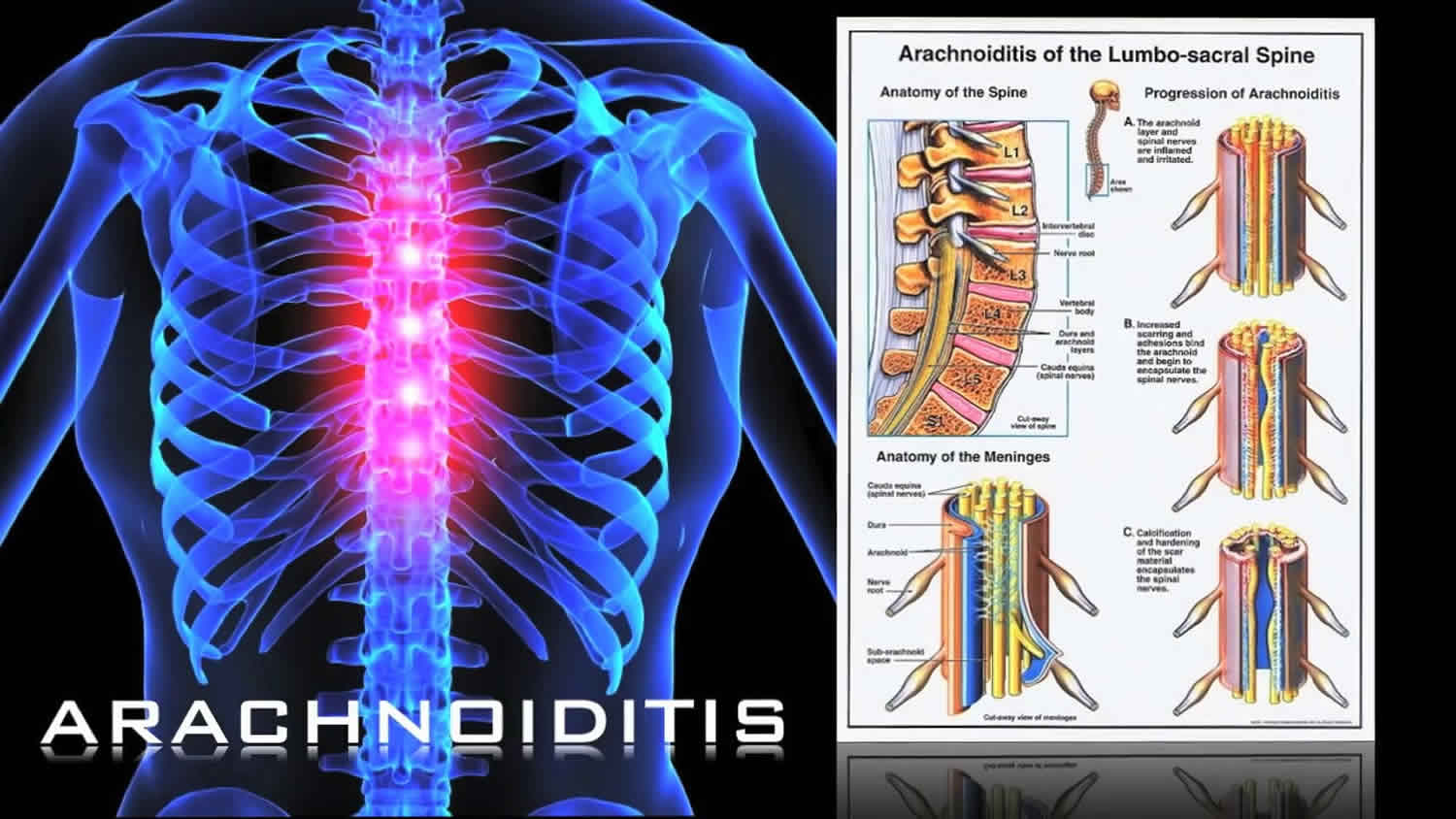
Arachnoiditis is a painful disorder caused by the inflammation of the arachnoid mater (middle layer) and/or the dura mater (outermost layer), two of the connective tissue membranes that surround and protect the nerves of the spinal cord 1. The arachnoid can become inflamed because of an irritation from chemicals, infection from bacteria or viruses, as the result of direct injury to the spine, chronic compression of spinal nerves, or complications from spinal surgery or other invasive spinal procedures. The initial symptoms of arachnoiditis are caused by inflammation of the arachnoid, and the formation of scar tissue and adhesions later cause the more severe symptoms as the condition progresses. Inflammation can sometimes lead to the formation of scar tissue and adhesions, which cause the spinal nerves to “stick” together. If arachnoiditis begins to interfere with the function of one or more of these nerves, it can cause a number of symptoms, including chronic and persistent pain, numbness, tingling, and a characteristic stinging and burning pain in the lower back or legs. Some people with arachnoiditis will have debilitating muscle cramps, twitches, or spasms. It may also affect bladder, bowel, and sexual function. In severe cases, arachnoiditis may cause paralysis of the legs.
Arachnoiditis can affect any age group, but is more common in adults between 40 and 60 years of age. It is equally common in both genders. The prevalence is unknown. Arachnoiditis is uncommon, however, the number of cases is increasing worldwide due to the increasing number of immunocompromised patients including diabetics, alcoholics and intravenous drug abusers, people with AIDS, and transplantation and chemotherapy patients. About 25,000 cases of arachnoiditis occur each year, mostly in North and South America, Asia and Europe, where spinal operations are more prevalent 2.
Diagnosis of arachnoiditis is by MRI with intravenous contrast is preferred. The intrathecal injection of some dyes is potentially hazardous and should be avoided.
Arachnoiditis remains a difficult condition to treat, and long-term outcomes are unpredictable. Most treatments for arachnoiditis are focused on chronic pain relief and the improvement of symptoms that impair daily function. A regimen of pain management, physiotheraphy, exercise, and psychotheraphy is often recommended. Surgical intervention is controversial since the outcomes are generally poor and provide only short-term relief and may increase formation of scar tissue 1.
The outlook for someone with arachnoiditis is complicated by the fact that the disorder has no predictable pattern or severity of symptoms.
There are three connective tissue membranes called meninges, which are protective, connective tissue coverings that lie just external to the brain and spinal cord (the central nervous system): the dura mater (outermost layer), arachnoid mater (middle layer) and pia mater (deepest layer). Their functions are to cover and protect the central nervous system (the spinal cord and brain); enclose and protect the blood vessels that supply the central nervous system (CNS); contain the cerebrospinal fluid (CSF). The arachnoid membrane (arachnoid mater) lies just deep to the dura mater (outermost layer). Deep to the arachnoid membrane is the wide subarachnoid space, which is spanned by weblike threads that hold the arachnoid mater to the underlying pia mater. This web is the basis of the name arachnoid, which means “spiderlike.” The subarachnoid space is filled with cerebrospinal fluid (CSF) and it also contains the largest blood vessels that supply the brain. Because the arachnoid is fine and elastic, these vessels are rather poorly protected.
Arachnoid cysts appear on the arachnoid membrane, and they may also expand into the space between the pia mater and arachnoid membranes (subarachnoid space).
Cerebrospinal fluid (CSF) is a watery broth that fills the subarachnoid space and the central hollow cavities of the brain and spinal cord. Cerebrospinal fluid (CSF) aids in protecting and nourishing the neural tissue.
- Cerebrospinal fluid (CSF) a liquid medium that surrounds and gives buoyancy to the central nervous system. The brain and spinal cord actually float in the cerebrospinal fluid (CSF), which prevents these delicate organs from being crushed under their own weight.
- The layer of cerebrospinal fluid (CSF) surrounding the central nervous system resists compressive forces and cushions the brain and spinal cord from blows and jolts.
- Cerebrospinal fluid (CSF) helps to nourish the brain, to remove wastes produced by neurons, and to carry chemical signals such as hormones between different parts of the central nervous system. Although similar in composition to the blood plasma from which it arises, cerebrospinal fluid (CSF) contains more sodium and chloride ions and less protein.
Amazingly, very little CSF is needed to perform these functions: only 100–160 ml, about half a cup, is present at any time. Cerebrospinal fluid (CSF) is produced in the ventricles of the brain, circulates through the hollow central cavities of the central nervous system (the spinal cord and brain) and the subarachnoid space, and is reabsorbed back into the blood in the dural venous sinuses (see Figure 3).
Figure 1. Meninges of the spinal cord
 Figure 2. Spinal cord
Figure 2. Spinal cord

Figure 3. Cerebrospinal fluid formation, absorption and circulation around and within the brain
 Can two back surgeries, multiple spinal injections and one epidural anesthetic cause arachnoiditis or adhesive arachnoiditis?
Can two back surgeries, multiple spinal injections and one epidural anesthetic cause arachnoiditis or adhesive arachnoiditis?
Arachnoiditis, which may progress to adhesive arachnoiditis, has been reported to occur due to spinal surgeries, steroid epidural injections, other types of injections into the spinal cord, and anesthetic spinal interventions 2. About 60% of cases are associated with spinal surgeries, and about 22% of cases may be due to spinal and epidural anesthesia 2. After a person has arachnoiditis, injections or any other invasions of the spine may worsen the disease significantly 2. However, experts are unable to say whether specific interventions have caused arachnoiditis (or progression to adhesive arachnoiditis) in any one person. People with questions or concerns about arachnoiditis for themselves or family members are encouraged to speak with a spine specialist or other health care provider familiar with the condition.
How does arachnoiditis progress to adhesive arachnoiditis?
Generally, arachnoiditis occurs as a progression of inflammatory changes. First it is characterized by inflammation of the arachnoid membrane (the “inflammatory phase”), which invades the space beneath the membrane. Over a period of time, the nerve roots may become inflamed and begin to adhere to each other and to the inner layer of the arachnoid membrane or the thecal sac. This is referred to as the “adhesive phase” or “proliferation stage” of arachnoiditis. The adhesions may then exert pressure on the nerve roots and may eventually result in scarring and fibrosis (thickening of tissue). Scarring and fibrosis may restrict blood flow to the affected area and eventually impede the free flow of cerebral spinal fluid.
Unfortunately, the disorder has no predictable pattern or severity of symptoms. Therefore, it is not possible to predict if or when arachnoiditis may progress. However, surgeries, injections or any other invasions of the spine may worsen the disease significantly.
Arachnoiditis prognosis
Arachnoiditis causes chronic pain and neurological deficits. Arachnoiditis does not improve significantly with treatment and does not have a predictable pattern of symptoms, severity, or progression 3. Some people with arachnoiditis may have milder symptoms which do not get much worse over time, although the aging process usually does add to the severity of the symptoms. Others may quickly progress to severe neurological symptoms that lead to paralysis. The majority of people with arachnoiditis appear to fall somewhere between these extremes 2.
Arachnoiditis symptoms
The severity of spinal arachnoiditis symptoms usually depends on the extent and location of the injurious event, direct injury to the spinal cord or to the nerve roots resulting in immediate, severe pain in the corresponding area of innervation (i.e. the area that is supplied by the affected nerves). Arachnoiditis can cause a number of symptoms including numbness; tingling; loss of temperature sensation; and a characteristic stinging and burning pain in the lower back, limbs, and trunk. Pain is often made worse by activity. Some people have debilitating muscle cramps or spasms; loss of balance; tinnitus; problems with vision and hearing; or bladder, bowel, or sexual dysfunction. In severe cases, arachnoiditis may lead to paralysis of the legs. In most cases the pain is intense, accompanied by tingling or burning on the legs and feet; skin sensations like “bugs crawling” or “water dripping”.
Chronic severe pain is mostly localized in the lower back, perineum (area between the anus and the scrotum or vulva), legs and feet; it may appear weeks after a spinal surgical intervention or an injection into the spinal cord that went astray.
Frequently patients complain of severe pain radiating to the lower extremities, muscle cramps, gait abnormalities and alterations of proprioception. Moreover, patients may suffer from severe headaches, vision disturbances, hearing problems, dizziness and nausea. Bowel, bladder and sexual dysfunction as well as “electric shocks” type of pain are common in patients with severe arachnoiditis. All the symptoms are caused by the alteration and impediment of the cerebrospinal fluid (CSF) circulation resulting from clumped nerve roots, scar tissue and fibrosis.
Severe complications from multiple operative procedures in the spine may ensue in spinal cord damage, like “softening” (myelomalacia) or elongation of the nerve roots as in cases when the nerve roots and/or the spinal cord adhere to the dural sac wall. Some patients may develop arachnoid cysts and or syringomyelia.
Most symptoms are initially due to progressive inflammation around where damage to the arachnoid membrane was produced. Because in the early stages, arachnoiditis is usually a progressive disorder, first it is characterized by inflammation of the arachnoid membrane and invasion of the subarachnoid space. Eventually, the nerve roots undergo an inflammatory stage in the affected areas and after three months, they begin to adhere to each other and to the inner layer of the arachnoid initiating the adhesive phase of arachnoiditis. Subsequently, these adhesions can exert undue pressure upon the nerve roots or the dural sac wall and eventually result in scarring and fibrosis which in turn may restrict blood flow to the affected area and eventually also impede the free flow of the cerebrospinal fluid (CSF). In this manner of distribution, the rotation of the cerebrospinal fluid (CSF) can spread infections, disseminate malignant tumors, and disperse fungi.
Arachnoiditis causes
Arachnoiditis can be mechanically (localized) or chemically (diffuse) induced, and is often associated with spinal operations (60% of cases), neuroaxial (spinal and epidural) anesthesia (22%), spinal taps (7%), myelography (3%), pain relief procedures and secondary infections 2. Arachnoiditis can also be caused by bacterial and viral spinal infections (7%) and repeated subarachnoid injections of anticancer drugs or antimetabolites 2. Syringomyelia, cauda equina syndrome, pseudomeningoceles, intrathecal cysts or tethering of the spinal cord and nerve roots may complicate lumbosacral arachnoiditis. Arachnoiditis occurs as a progression of inflammatory changes. In the early (inflammatory) phase nerve roots are edematous (enhanced), while in the late proliferation stage (adhesive arachnoiditis) nerve roots are clumped and asymmetric. The flow of cerebrospinal fluid (CSF) from the distal dural sac to the brain is impeded, intrathecal pressure increases and this causes back pain and postural headache. In some cases the scar tissue calcifies (arachnoiditis ossificans).
There are numerous causes of arachnoiditis:
- Mechanical injury during spinal surgery, or complications from spinal surgery (about 60% of cases), dural cut/tear caused by surgical interventions, especially repeat spinal operations, after fusions or minimally invasive procedures requiring corrective surgeries.
- Trauma to the spinal cord.
- Epidural disc prolapse.
- Repeat manipulation during catheter or leads insertion.
- One or multiple spinal taps.
- Several steroid epidural injections.
- Injections of epidural steroids gone intrathecal.
- Difficult epidural blood patches (injection >20ml).
- Injection of myelogram dye into the spinal cord (myelography).
- Infections that may cause meningitis (viral, fungal or bacterial)
- Spinal and epidural anesthesia
Arachnoiditis is a rare disorder affecting more females than males, probably because two thirds of the pregnant women in the USA, Latin America and most other countries receive spinal or epidural anesthesia for the delivery 1. It is estimated that about 4% of them develop arachnoiditis due to complications of anesthesia.
Individuals who have had spinal surgery, intrathecal injection of toxic fluids (i.e. hyaluronidase, blood, dyes, steroids and local anesthetics with preservatives) into the spinal dural sac, or have had injuries to the spine or head, may be at greater risk to develop this disorder. However, the precise prevalence and incidence of arachnoiditis is unknown. According to one estimate, approximately 11,000 new cases occur each year in the USA; however the cause varies, ranging from back surgery, pain relief procedures and diagnostic interventions mostly performed in North and South America, Europe and Asia, with an undetermined number in Africa. Obviously, the greater number of surgical and anesthetic spinal interventions has increased the number of cases considerably. For different reasons, some cases of arachnoiditis may go misdiagnosed or undiagnosed, making it difficult to determine its real frequency in the general population.
Arachnoiditis is generally not an inherited condition and typically results from inflammation due to prior spinal surgery, other procedures on the spine (such as injections), trauma, or infection. Familial cases of arachnoiditis have very rarely been reported. Only two families with multiple affected family members have been described in the literature, with possible autosomal dominant or multigenic inheritance (due to the interaction of multiple genes) 4.
Risk factors for arachnoiditis
Factors that increase the risk of arachnoiditis include:
- Infection from bacteria or viruses;
- Patients with decreased immune function: diabetes, alcoholism, AIDS, chemotherapy and organ transplant patients;
- Surgery involving the brain or spinal cord;
- Contrast media, anaesthetics and steroids given intrathecally (into the subarachnoid space).
Arachnoiditis diagnosis
A diagnosis of arachnoiditis is based upon the antecedents of having had an invasive procedure or serious illness within the spine and a complete clinical exam, a detailed patient history, identification of key symptoms and a variety of specialized tests of which radiological confirmation is essential. Since most cases occur in the lumbosacral spine, an MRI with contrast is the optimal examination to verify the extent of the illness. A complete history and physical may define the extent and severity of the illness, including the injury caused by prior trauma, surgery and other interventions into the spine. The symptoms of arachnoiditis resemble those associated with other spinal conditions including back pain, muscle spasms, referred pain, headache, dizziness and alterations of balance. When the intensity of the pain increases post surgery or certain procedures such as manipulations or punctures of the spine are followed by intense headache, back pain and or by visual disturbances, proper radiological studies are indicated, nerve conduction studies are non-contributory.
Clinical Testing and Work-Up
Of preference, a magnetic resonance imaging (MRI) of the lumbosacral spine with contrast is ideal, more precise and less injurious. The MRI uses a magnetic field and radio waves to produce cross-sectional images of particular organs and bodily tissues. To obtain the best results is imperative that an intravenous dye is administered only a few minutes before the test in order to be able to have the optimal images, especially within the dural sac, ideally obtaining axial and saggital views of the lumbosacral region. However, the presence of certain non-titanium metal objects (screws, wires, etc.) makes the MRI contraindicated since it may heat certain metals. If an MRI is contraindicated, the diagnosis of arachnoiditis will have to be made using a computed tomography (CT) scan, which requires the administration of contrast media into the intrathecal compartment; however the images are not as informative as those obtained from an MRI. The intrathecal injection of a dye (myelogram) presents one more obstacle, as it may be hazardous, especially in cases of infections. An intrathecal injection refers to injecting a substance directly into the cerebrospinal fluid that surrounds the brain and spinal cord.
Physical examinations of patients with arachnoiditis can reveal changes in reflexes, sensory deficits, strength, and/or weakness. Furthermore it confirms the physical findings between the right and the left side when compared with radiological images. Of great use is the exploration of proprioception which confirms the alteration of balance.
Arachnoiditis treatment
Currently, there is no complete cure for arachnoiditis, but there are therapies which, if implemented, may lessen pain and suffering. Treatment options for arachnoiditis are similar to those for other chronic pain conditions. Most treatments focus on relieving pain and improving ability to perform daily activities. Often, healthcare professionals recommend a program of pain management, physiotherapy, exercise, and psychotherapy. Multimodal medication management with Schedule 3 drugs should be employed for chronic indications. Any Schedule 2 opiates are to be used with great caution as there is a risk of dependence and development of side effects of continuous tolerance will require progressively higher dosages.
Mild physical therapy is recommended for affected individuals to restore motion, preserve function and to help them remain active. It may include massage, mild exercise (without producing pain), hydrotherapy, and hot or cold compresses.
Psychotherapy may be helpful for most patients with arachnoiditis, as there is a strong element of depression. Patients need to be able to cope with their disease problems and the detrimental effects of continuous severe pain.
Surgery as a treatment of arachnoiditis is generally not recommended because of the possibility of scar tissue and fibrosis formation.
References- Arachnoiditis. https://rarediseases.org/rare-diseases/arachnoiditis/
- Arachnoiditis. https://www.orpha.net/consor4.01/www/cgi-bin/OC_Exp.php?lng=EN&Expert=137817
- Arachnoiditis Information Page. https://www.ninds.nih.gov/Disorders/All-Disorders/Arachnoiditis-Information-Page
- Pasoglou V., et. al. Familial adhesive arachnoiditis associated with syringomyelia. AJNR Am J Neuroradiol. June, 2014; 35(6):1232-1236.