What is aseptic technique
Aseptic technique is the range of infection prevention and control practices which are used to minimize the presence of pathogenic microorganisms during clinical procedures. Previously, the terms ‘sterile technique,’ ‘clean technique’ and ‘aseptic technique’ have been used interchangeably. The correct terminology and practice is ‘aseptic technique’. ‘Aseptic technique’ aims to prevent pathogenic microorganisms, from being introduced to the patient via hands, surfaces and equipment. Aseptic technique is used during clinical procedures to identify and prevent microbial contamination of aseptic parts and sites by ensuring that they are not touched either directly or indirectly. Aseptic technique protects patients during invasive clinical procedures by employing infection control measures that minimize, as far as practicably possible, the presence of pathogenic organisms. A widely used method of aseptic technique is known as Aseptic Non Touch Technique (ANTT®). Asepsis is achieved by protecting key-parts and key-sites from microorganisms transferred from the healthcare worker and the immediate environment. For example, when applying or changing dressings, an aseptic technique is used in order to avoid introducing infections into a wound 1. Even if a wound is already infected, an aseptic technique should be used as it is important that no further infection is introduced. Aseptic technique should be used when the patient has a surgical or non-surgical wound in or around the eye.
Some examples of procedures requiring aseptic technique include:
- preparation and administration of intravenous (IV) fluids or medications
- simple or complex wound dressings
- insertion of urinary catheters
- insertion of an intravenous (IV) cannula or central venous catheter (CVC)
- emptying or changing drainage bags
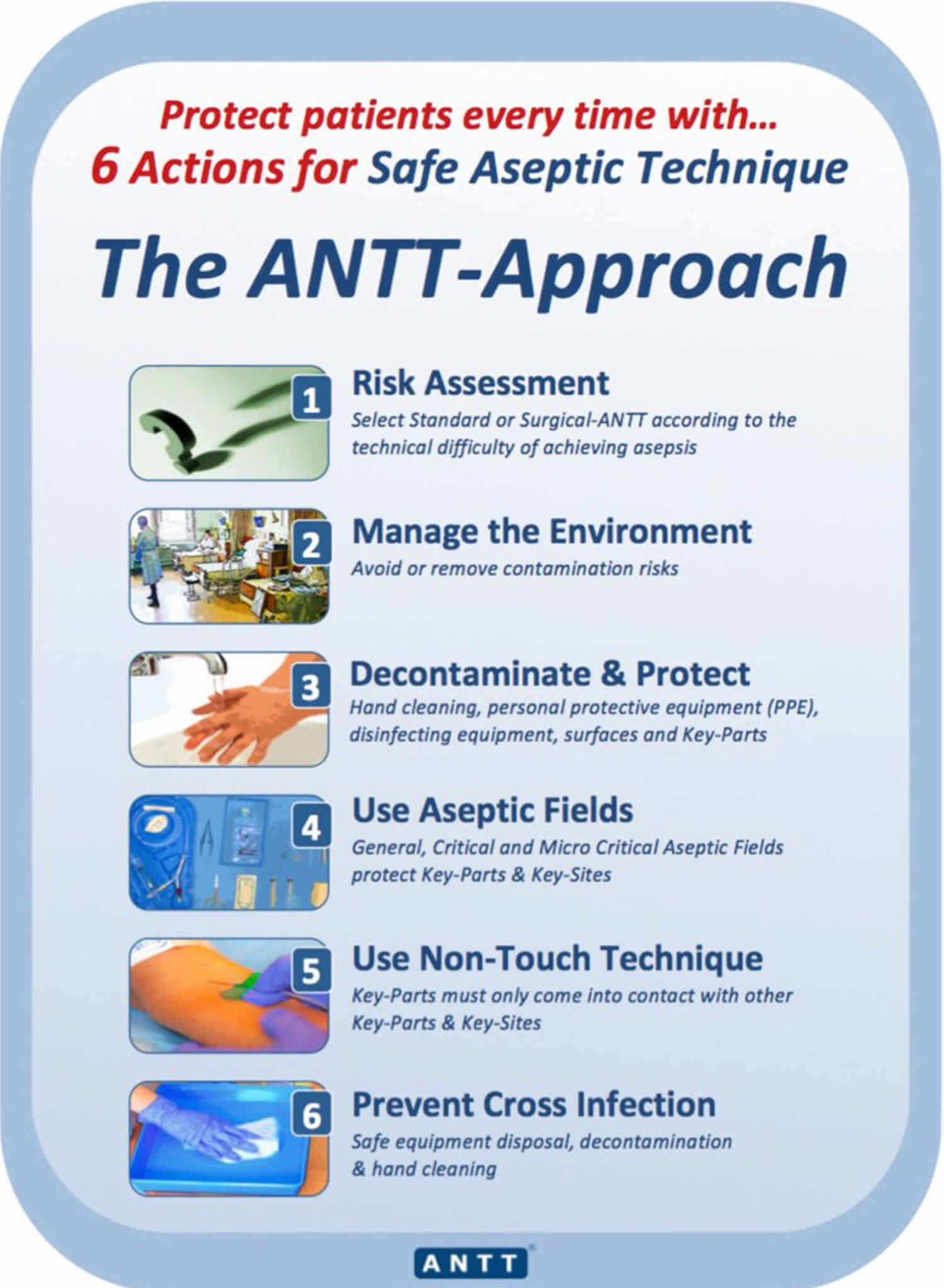
The six core elements of aseptic technique from the Aseptic Non Touch Technique (ANTT®):
- Hand hygiene: strict adherence to effective hand cleaning, using a systematic method, performed prior to, during, if required following contamination, and following invasive clinical procedures 2
- Correct glove use: appropriate use of gloves and other personal protective equipment to reduce the transmission of harmful microorganisms 3
- Key-Part and Key-Site protection: a method of identifying and strictly not touching and protecting from touch contamination the most critical parts of the procedure equipment 4
- Non-touch technique: the skill of not touching any critical part(s) or site(s) of an invasive clinical procedure 5
- Key-Part disinfection: the disinfection of the most critical parts of procedure equipment that could provide a port of entry for harmful microorganisms 3
- Aseptic field management: selecting appropriate types of aseptic fields to protect the Key-Parts of procedure equipment prior to and during invasive clinical procedures 4
Key sites are any breaches in skin integrity which could be a portal of entry for microorganisms to colonize the patient. This includes wounds and puncture sites.
Key parts are any parts of the equipment which come into contact with procedural equipment or the patient. This includes invasive devices connected to the patient and liquid infusions. Examples include:
- IV cannula bungs
- Needle tips
- Sterile gauze used to clean a wound
If key parts become contaminated they can transfer microorganisms to the patient.
What is the purpose of aseptic technique?
Aseptic technique is an important infection prevention competency for protecting patients from healthcare-associated infection 6.
Why is aseptic technique important?
It is widely accepted that poor standards of aseptic technique are a major cause of preventable infections. Healthcare-associated infection is defined by The Association for Safe Aseptic Practice as an infection acquired by a patient as a consequence of exposure to pathogenic organisms via healthcare staff or healthcare facilities 7. In the European Union and European Economic Area it has been estimated that approximately 3.2 million patients per year will have at least one healthcare-associated infection 8. The Centers for Disease Control and Prevention (CDC) reports research indicating that healthcare providers and practitioners taking specific targeted steps can reduce some healthcare-associated infection (e.g. central-line associated bloodstream infections) by more than 70% 9.
Healthcare acquired infections result in significant mortality and morbidity internationally. It is estimated that 30% of healthcare acquired infections are preventable. Due to the invasive nature of clinical procedures involving aseptic technique, health care workers are inherently a significant vector of infection.
The importance of aseptic technique is highlighted by the Department of Health in the Health and Social Care act 2008 10; it requires healthcare providers to have a single standard aseptic technique demonstrable by training and audit. Importantly, when aseptic techniques are used as a method of preventing infection, it is essential that they are theoretically sound and carried out correctly 11. Aseptic technique is variously and confusingly described in the literature and problematic in practice. Hartley 12 reports that aseptic technique is not carried out to a high standard across the UK and Flores 13 suggested that there was a theory–practice gap along with much confusion and complacency in professional practice regarding aseptic technique. The vocabulary of aseptic technique is often inaccurate, used interchangeably, confusing and lacking in evidence, all of which appears to have contributed to practice variability, inadequate risk assessment and uncontrolled standards of practice 4.
Failures of aseptic technique have long been thought to be associated with practice compromises 14. Pellowe describes ‘Poor adherence to evidence-based infection prevention measures and the subsequently increased risks to patients’ 15. Increasingly, modern technology enabling organisms to be tracked around the procedure environment is providing evidence for the role of failed aseptic technique in the transmission of infection 16.
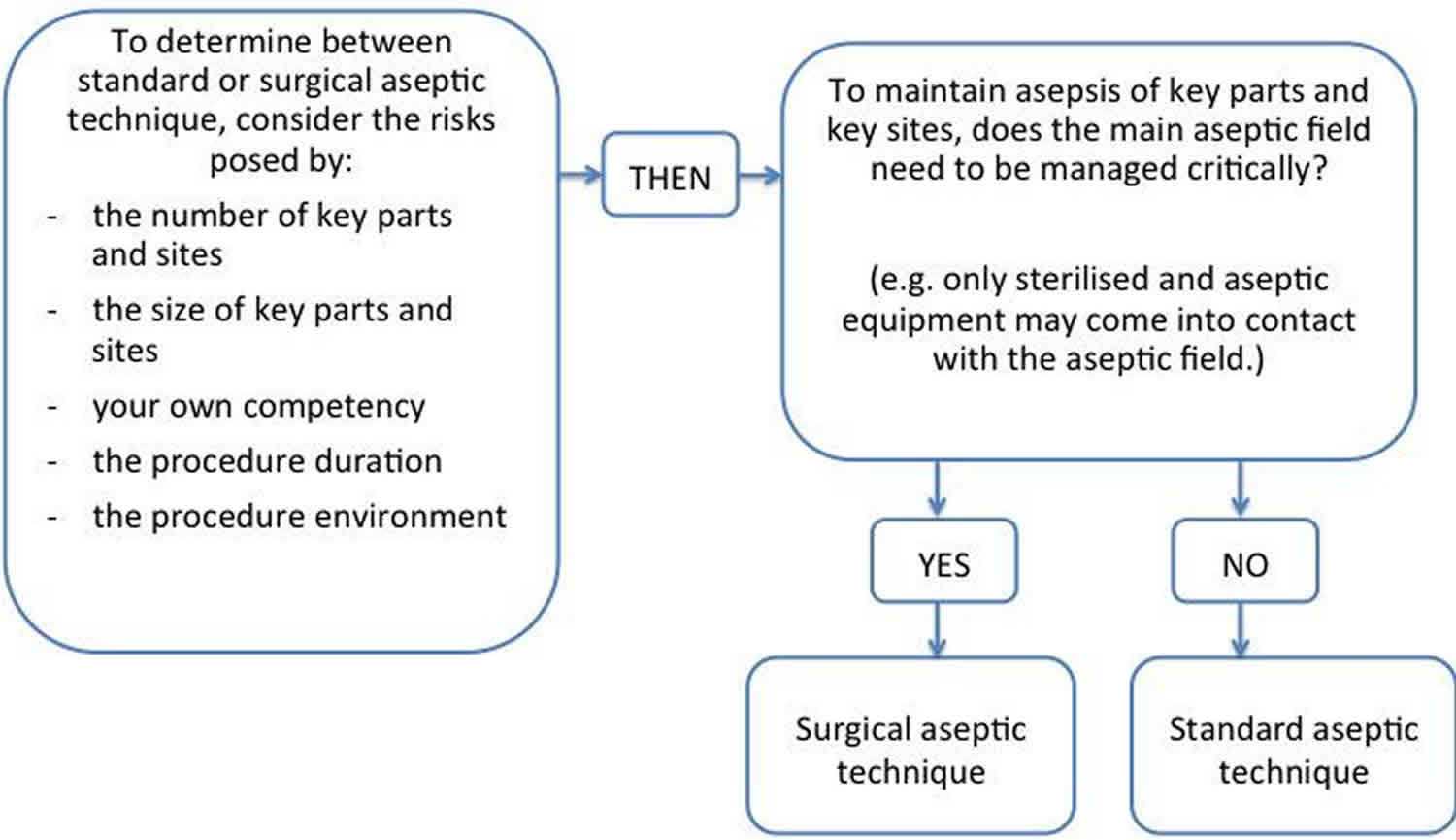
The decision to use standard or surgical aseptic technique should be determined by the clinician undertaking the procedure. This decision must be based on a risk assessment which considers:
- the complexity of the procedure
- their own competence with the procedure
- whether or not the procedure can be completed without directly touching any key parts or key sites
- patient and environmental factors
Figure 1. Aseptic technique algorithm
Aseptic technique vs sterile
Sterile means free from bacteria or other living microorganisms. The term ‘sterile technique’ should not be used in place of the term aseptic technique. It would be nearly impossible to achieve sterile technique during all procedures due to the large numbers of microorganisms present on the human body and in the health care environment. Controlled environments such as specially equipped operating theaters can achieve near-sterile techniques.
Core infection control components
The aim of every procedure should be to maintain asepsis at all times by protecting the key parts and key sites from contact contamination by microorganisms. This can be achieved through correct hand hygiene, a non-touch technique, glove use and ensuring asepsis and sterility of equipment.
Hand Hygiene
Effective hand hygiene is the single most important measure to prevent transmission of infection in health care settings. It aims to:
- protect patients from becoming colonized or infected:
- via the clinician’s hands
- from their own flora
- protect clinicians from:
- becoming colonized or infected by pathogenic microorganisms
- spreading infectious agents
The 5 moments of hand hygiene
The 5 moments of hand hygiene must always be used in conjunction with both standard and surgical aseptic technique.
Hand hygiene must be performed:
- Before touching a patient.
- Before performing any procedures on a patient.
- After any body fluid exposure or risk.
- After touching a patient.
- After touching the patient’s surroundings or equipment.
Non touch technique
The safest way to protect a key part or key site from contamination is to use a non touch technique. This means that the safest way to protect a key part or key site is not to touch it, even if wearing gloves.
Gloves
Gloves are a single-use item. They help to reduce the risk of:
- contamination for the patient
- body fluid exposure for the clinician
Sterile gloves should be worn if a key part or key site needs to be touched, or if it is likely that they may accidentally be touched, during the procedure.
Otherwise, non sterile gloves may be used.
Ensuring asepsis and sterility of equipment
Key part and key site identification and protection
During all procedures, key parts and key sites need to be identified and protected. Aseptic key parts must only come into contact with:
- other aseptic key parts
- key sites
For example, the needle (key part) used to draw up a medication must only come into contact with a disinfected port on an IV line (an aseptic key part) or the intramuscular injection puncture site (a key site).
Decontamination
When performing an aseptic procedure, key parts that are contaminated must be made aseptic prior to use. For example, an IV cannula which has been disconnected from fluids but left in situ is no longer aseptic. Prior to accessing the IV again, it needs to be made aseptic once more.
It is important to decontaminate equipment such as trolleys prior to use.
Environmental control
Prior to performing an aseptic procedure, clinicians need to ensure that there are no environmental risks to the procedure. Risks may include:
- nearby bed making
- open windows
- bedside curtains
- patients using commodes
- nearby air conditioners or heaters
Aseptic fields
An aseptic field is a designated work space that contains and protects procedural equipment from becoming contaminated. There are three types of aseptic fields. They are used in different situations and require different management. The choice of aseptic field should be made to ensure protection of key parts and sites.
Critical aseptic fields
A critical aseptic field ensures asepsis during procedures. It is used when key parts or key sites cannot be easily protected from contamination during a procedure. This may be because the key parts or key sites:
- are large
- are numerous
- can’t be protected by caps and covers
- can’t be handled with non touch technique at all times
Critical aseptic fields should be managed as a key part. They should be handled with a non touch technique where possible, or with sterile gloves if touching is unavoidable. Procedures which may require a critical aseptic field include:
- insertion of PICC lines
- urinary catheter insertion
- complex wound care
- theater procedures
Micro critical aseptic fields
The micro critical aseptic field is a smaller version of the critical aseptic field and is used to protect a single key part. A micro critical aseptic field is usually the sterile packaging, cover, cap or sheath of a key part.
General aseptic fields
A general aseptic field promotes asepsis during procedures. Micro critical aseptic fields and a non touch technique are used to protect key parts from contamination.
Standard aseptic technique
Standard aseptic technique can be used when procedures:
- involve a small number of key parts and key sites
- involve small key parts and key sites
- are technically simple
- are short in duration (e.g. less than 20 minutes)
Standard aseptic technique requires the clinician to:
- identify key parts and key sites
- protect those key parts and key sites from contamination during the procedure
- decontaminate non aseptic key parts as required
- create and maintain aseptic fields
- perform hand hygiene
- wear gloves
- use a non touch technique
- control environmental risks
Examples of procedures that may use standard aseptic technique include:
- preparation and administration of IV fluids or medications
- simple wound dressings
- insertion of an IV cannula
- emptying or changing drainage bags
These procedures may involve general aseptic fields and micro critical aseptic fields.
Surgical aseptic technique
Surgical aseptic technique is required when procedures:
- involve a large number of key parts or key sites
- involve large sized key parts or key sites
- are technically complex
- are long in duration (e.g. more than 20 minutes)
Surgical aseptic technique requires the clinician to:
- identify key parts and key sites
- protect those key parts and key sites from contamination during the procedure
- decontaminate non aseptic key parts as required
- maintain aseptic fields
- perform hand hygiene
- wear sterile gloves
- use a non touch technique whenever possible
- control environmental risks
Examples of procedures that may use surgical aseptic technique include:
- complex wound dressings
- insertion of a PICC or CVC
- surgery
Due to the high risk of contamination of key parts or key sites, a critical aseptic field and sterile gloves are required. Surgical aseptic technique should still use micro critical aseptic fields and a non touch technique where possible.
Aseptic technique steps
Infection Control Components of Aseptic Non Touch Technique (ANTT®)
Perform aseptic technique using the following core components:
- Identify and protect key parts and sites.
- A ‘key part’ is the part of the equipment that must remain sterile, such as a syringe hub, and must only contact other key parts or key sites.
- A ‘key site’ is the area on the patient such as a wound, or IV insertion site that must be protected from microorganisms.
- Ensure aseptic key parts only contact other aseptic key parts/sites.
- Use hand hygiene, non-touch technique, a defined aseptic field, sterile equipment and/or clean existing key parts, such as an IV access port, to a standard that renders them aseptic prior to use.
- Attempt not to touch key parts/sites directly but… if this is necessary, wear sterile gloves.
- Sequence your practice to ensure efficient, logical and safe order of tasks.
Key sites are any breaches in skin integrity which could be a portal of entry for microorganisms to colonise the patient. This includes wounds and puncture sites.
Key parts are any parts of the equipment which come into contact with procedural equipment or the patient. This includes invasive devices connected to the patient and liquid infusions. Examples include:
- IV cannula bungs
- Needle tips
- Sterile gauze used to clean a wound
If key parts become contaminated they can transfer microorganisms to the patient.
Figure 2. Aseptic technique steps
Aseptic Fields – provide a controlled working space that either ensures or promotes asepsis.
Critical aseptic fields that ensure asepsis are used when:
- key parts/sites are large or numerous and can’t be easily protected by covers or caps or can’t be handled with a non-touch technique
- invasive procedures require a large aseptic working area
- the critical aseptic field is managed as a key part so that only sterile equipment can come into contact with it
- sterile gloves and often, full barrier precautions (sterile gown, mask and hair covering and the use of sterile drapes) are required.
General aseptic fields that promote asepsis are used when:
- key parts are easily protected by critical micro aseptic fields and non-touch technique
- critical micro aseptic fields are those key parts protected by syringe caps, sheathed needles, covers or packaging
- the main aseptic field does not have to be managed as a key part
- non sterile gloves can be used unless key parts must be touched, when sterile gloves must be worn.
Performing Aseptic Non Touch Technique
- Perform hand hygiene.
- Clean trolley/work surface with detergent and water or detergent wipe.
- Identify and gather equipment for procedure.
- Perform hand hygiene and prepare field:
- open procedure pack using corners
- drop sterile equipment into sterile field.
- Perform hand hygiene.
- Prepare patient – use gloves where appropriate such as when removing a bloodstained dressing.
- Remove gloves, perform hand hygiene, re-apply new gloves.
- Perform procedure ensuring all key parts/components are protected:
- sterile items are used once and disposed into waste bag
- only sterile items contact the key site
- sterile items do not come into contact with non-sterile items.
- Remove gloves and perform hand hygiene.
- Clean trolley/work surface after use and perform hand hygiene.
Aseptic technique summary
- The aim of every clinical procedure should be to maintain asepsis at all times by protecting the key parts and key sites from contact contamination by microorganisms.
- Effective hand hygiene is the single most important measure to prevent transmission of infection in health care settings.
- The safest way to protect a key part or site from contamination is to use a non touch technique.
- Sterile gloves should be worn if a touch a key part or key site needs to be touched, or if it is likely that they may accidentally be touched, during the procedure. Otherwise, non sterile gloves may be used.
- During all procedures, key parts and key sites need to be identified and protected.
- Key parts that are not aseptic must be made aseptic prior to use in an aseptic procedure.
- Prior to performing an aseptic procedure, clinicians need to ensure that there are no environmental risks to the procedure.
- A critical aseptic field ensures asepsis during procedures when key parts or key sites cannot be easily protected.
- Critical aseptic fields should be managed as a key part.
- The micro critical aseptic field is a smaller version of the critical aseptic field and is used to protect a single key part.
- A general aseptic field promotes asepsis during procedures.
- The choice of aseptic field should be made to ensure protection of key parts and key sites.
- The decision to use standard or surgical aseptic technique must be based on a risk assessment.
- Pickering D, Marsden J. Techniques for aseptic dressing and procedures. Community Eye Health. 2015;28(89):17. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4579997/
- World Health Organization. (2009) World Health Organization Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care is Safer Care. Geneva: WHO https://apps.who.int/iris/bitstream/handle/10665/44102/9789241597906_eng.pdf;jsessionid=7AAA5AFC0959E127F30FB838787F4BB0?sequence=1
- Epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. Loveday HP, Wilson JA, Pratt RJ, Golsorkhi M, Tingle A, Bak A, Browne J, Prieto J, Wilcox M, UK Department of Health. J Hosp Infect. 2014 Jan; 86 Suppl 1():S1-70.
- Rowley S, Clare S, Macqueen S, Molyneux R. (2010) ANTT v2: An updated practice framework for aseptic technique. British Journal of Nursing 19: S5–S11.
- National Institute for Health and Care Excellence. (2008) Surgical Site Infections: Prevention and Treatment. London: NICE
- Implementing the Aseptic Non Touch Technique (ANTT®) clinical practice framework for aseptic technique: a pragmatic evaluation using a mixed methods approach in two London hospitals. J Infect Prev. 2018 Jan; 19(1): 6–15. doi: 10.1177/1757177417720996 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5753945/
- Association for Safe Aseptic Practice. http://antt.org/ANTT_Site/home.html
- European Centre for Disease Prevention and Control. (2013) Point prevalence survey of healthcare-associated infections and antimicrobial use in European acute care hospitals 2011–2012. https://ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/healthcare-associated-infections-antimicrobial-use-PPS.pdf
- Centers for Disease Control and Prevention. (2009) National and State Healthcare Associated Infections Progress Report. Atlanta, GA: https://www.cdc.gov/HAI/pdfs/progress-report/hai-progress-report.pdf
- Department of Health (2015) The Health and Social Care Act 2008: Code of Practice on the prevention and control of infections and related guidance.
- Variations in aseptic technique and implications for infection control. Aziz AM. Br J Nurs. 2009 Jan 8-21; 18(1):26-31
- Hartley J. (2005) Aseptic technique to be part of Essence of Care Guidance. Nursing Times 101: 6.
- Sterile versus non-sterile glove use and aseptic technique. Flores A. Nurs Stand. 2008 Oct 15-21; 23(6):35-9.
- Are contaminated flush solutions an overlooked source for catheter-related sepsis? Worthington T, Tebbs S, Moss H, Bevan V, Kilburn J, Elliott TS. J Hosp Infect. 2001 Sep; 49(1):81-3.
- Managing and leading the infection prevention initiative. Pellowe C. J Nurs Manag. 2007 Sep; 15(6):567-73.
- Multiple reservoirs contribute to intraoperative bacterial transmission. Loftus RW, Brown JR, Koff MD, Reddy S, Heard SO, Patel HM, Fernandez PG, Beach ML, Corwin HL, Jensen JT, Kispert D, Huysman B, Dodds TM, Ruoff KL, Yeager MP. Anesth Analg. 2012 Jun; 114(6):1236-48.