What is atrial fibrillation
Atrial fibrillation also called AFib or AF, is a heart condition that causes an irregular and often abnormally fast heart rate. Atrial fibrillation is a quivering or irregular heartbeat (arrhythmia) that can lead to blood clots, stroke, heart failure and other heart-related complications. During atrial fibrillation, the heart’s two upper chambers (the atria) beat chaotically and irregularly — out of coordination with the two lower chambers (the ventricles) of the heart. When this happens, the lower chambers do not fill completely or pump enough blood to your lungs and body. This can make you feel tired, lightheaded, or dizzy. You may also feel like your heart is skipping a beat, fluttering, pounding, or beating too hard or fast. You may also feel chest pain. Blood may pool in your heart, which increases your risk of forming clots and can lead to strokes or other complications. Atrial fibrillation can also occur without any symptoms, which can make it hard to diagnose. Atrial fibrillation may cause heart disease or worsen existing heart disease. . If left untreated, atrial fibrillation can lead to serious and even life-threatening complications, like stroke or heart failure
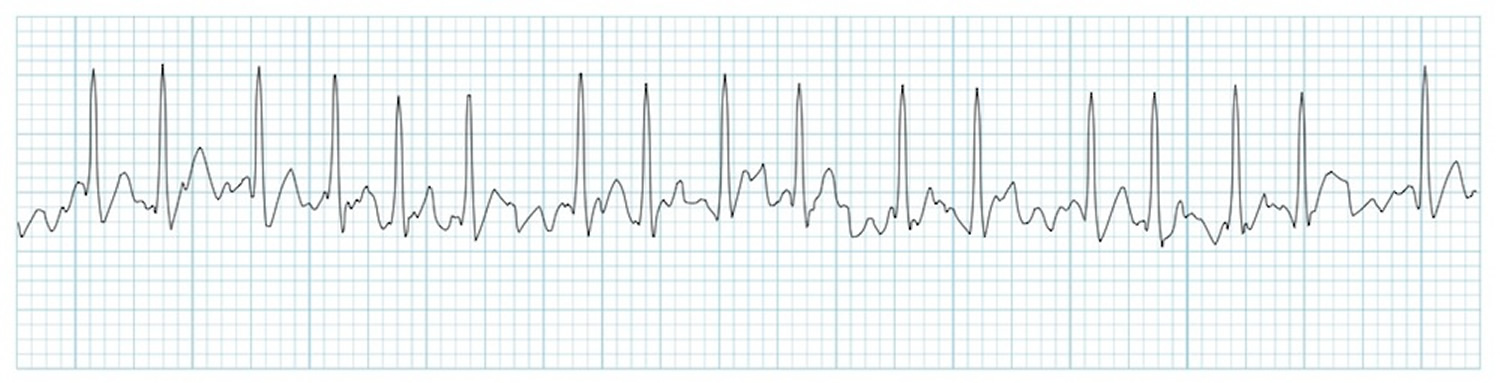
Atrial fibrillation is a common supraventricular arrhythmia that is characterized by rapid and irregular activation in the atria without discrete P waves on the surface electrocardiogram (ECG). Atrial fibrillation can be diagnosed with a surface ECG, an intracardiac atrial electrogram, or both. An arrhythmia that has the ECG characteristics of atrial fibrillation and lasts sufficiently long for a 12-lead ECG to be recorded, or is otherwise documented to last for at least 30 seconds, should be considered to be an atrial fibrillation episode 1. The 30-second duration was selected based on previous published consensus statements and is used as the minimal duration to define recurrence of atrial fibrillation after catheter ablation 2. This duration of atrial fibrillation has not been linked to a specific outcome of atrial fibrillation. In addition to the duration requirements listed above, the diagnosis of atrial fibrillation requires an ECG or rhythm strip demonstrating: (1) “absolutely” irregular R-R intervals (in the absence of complete atrioventricular [AV] block); (2) no distinct P waves on the surface ECG; and (3) an atrial cycle length (when visible) that is usually less than 200 ms 3.
Sometimes atrial fibrillation goes away on its own. For some people, atrial fibrillation is an ongoing heart problem that lasts for years. Over time, the irregular heart rhythm may happen more often and each episode may last longer. Your healthcare provider may recommend medicines, medical procedures, and lifestyle changes to treat your atrial fibrillation. Treatment may restore normal heart rhythm, help control your heart rate and symptoms, and prevent complications.
Table 1. Atrial fibrillation definitions
| Atrial fibrillation episode | An atrial fibrillation episode is defined as atrial fibrillation that is documented by ECG monitoring or intracardiac electrogram monitoring and has a duration of at least 30 seconds, or if less than 30 seconds, is present throughout the ECG monitoring tracing. The presence of subsequent episodes of atrial fibrillation requires that sinus rhythm be documented by ECG monitoring between atrial fibrillation episodes. |
| Chronic atrial fibrillation | Chronic atrial fibrillation has variable definitions and should not be used to describe populations of atrial fibrillation patients undergoing atrial fibrillation ablation. |
| Early persistent atrial fibrillation | Early persistent atrial fibrillation is defined as atrial fibrillation that is sustained beyond 7 days but is less than 3 months in duration. |
| Lone atrial fibrillation | Lone atrial fibrillation is a historical descriptor that is potentially confusing and should not be used to describe populations of patients with atrial fibrillation undergoing atrial fibrillation ablation. |
| Long-standing persistent atrial fibrillation | Long-standing persistent atrial fibrillation is defined as continuous atrial fibrillation of greater than 12 months’ duration. |
| Paroxysmal atrial fibrillation | Paroxysmal atrial fibrillation is defined as atrial fibrillation that terminates spontaneously or with intervention within 7 days of onset. |
| Permanent atrial fibrillation | Permanent atrial fibrillation is defined as the presence of atrial fibrillation that is accepted by the patient and physician, and for which no further attempts to restore or maintain sinus rhythm will be undertaken. The term permanent atrial fibrillation represents a therapeutic attitude on the part of the patient and physician rather than an inherent pathophysiological attribute of atrial fibrillation. The term permanent atrial fibrillation should not be used within the context of a rhythm control strategy with antiarrhythmic drug therapy or atrial fibrillation ablation. |
| Persistent atrial fibrillation | Persistent atrial fibrillation is defined as continuous atrial fibrillation that is sustained beyond 7 days. |
| Silent atrial fibrillation | Silent atrial fibrillation is defined as asymptomatic atrial fibrillation diagnosed with an opportune ECG or rhythm strip. |
At least 2.7 million Americans are living with atrial fibrillation 4.
Atrial fibrillation is the most common significant cardiac rhythm disorder and is also the most powerful common risk factor for stroke: about 15-20% of all strokes in the U.S. are attributable to atrial fibrillation 5.
- Even though untreated atrial fibrillation doubles the risk of heart-related deaths and is associated with a 5-fold increased risk for stroke, many patients are unaware that atrial fibrillation is a serious condition.
A normal heart rate should be regular and between 60 and 100 beats a minute when you’re resting. You can measure your heart rate by feeling the pulse in your neck or wrist.
- In atrial fibrillation, the heart rate is irregular and can sometimes be very fast. In some cases, it can be considerably higher than 100 beats a minute.
- In atrial fibrillation, the upper chambers of the heart (the atria) beat irregularly (quiver) instead of beating effectively to move blood into the ventricles.
Episodes of atrial fibrillation can come and go, or you may develop atrial fibrillation that doesn’t go away and may require treatment. Although atrial fibrillation itself usually isn’t life-threatening, it is a serious medical condition that sometimes requires emergency treatment.
It may lead to complications. Atrial fibrillation can lead to blood clots forming in the heart and if a clot breaks off, enters the bloodstream and blocked an artery leading to the brain, a stroke results. About 15–20 percent of people who have strokes have atrial fibrillation. This clot risk is why patients with this condition are put on blood thinners.
Sometimes, atrial fibrillation doesn’t cause any symptoms and a person with it is completely unaware that their heart rate isn’t regular.
Atrial fibrillation can cause problems including dizziness, shortness of breath and tiredness. You may be aware of noticeable heart palpitations, where your heart feels like it’s pounding, fluttering or beating irregularly, often for a few seconds or, in some cases, a few minutes.
Treatments for atrial fibrillation may include medications and other interventions to try to alter the heart’s electrical system. Typically, a cardioversion (where the heart is given a controlled electric shock to restore normal rhythm) is carried out. At this point, many people feel much better and realise that they hadn’t been feeling normal.
Chest Discomfort
- Most heart attacks involve discomfort in the center of the chest that lasts more than a few minutes, or that goes away and comes back. It can feel like uncomfortable pressure, squeezing, fullness or pain.
Discomfort in Other Areas of the Upper Body
- Symptoms can include pain or discomfort in one or both arms, the back, neck, jaw or stomach.
Shortness of Breath with or without chest discomfort.
Other signs may include breaking out in a cold sweat, nausea or lightheadedness.
- Don’t Wait–Get Help Quickly
- Quick Action Can Save Your Life
- If you think you or someone else is having a heart attack, even if you’re not sure, don’t feel embarrassed to call your local emergency number right away !
- Do not drive to the hospital or let someone else drive you. Call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room. Take a nitroglycerin pill if your doctor has prescribed this type of treatment.
Spot a stroke F.A.S.T.:
- Face Drooping. Does one side of the face droop or is it numb? Ask the person to smile.
- Arm Weakness. Is one arm weak or numb? Ask the person to raise both arms. Does one arm drift downward?
- Speech Difficulty. Is speech slurred, are they unable to speak, or are they hard to understand? Ask the person to repeat a simple sentence, like “the sky is blue.” Is the sentence repeated correctly?
- Time to call your local emergency number if the person shows any of these symptoms, even if the symptoms go away, call your local emergency number and get them to the hospital immediately.
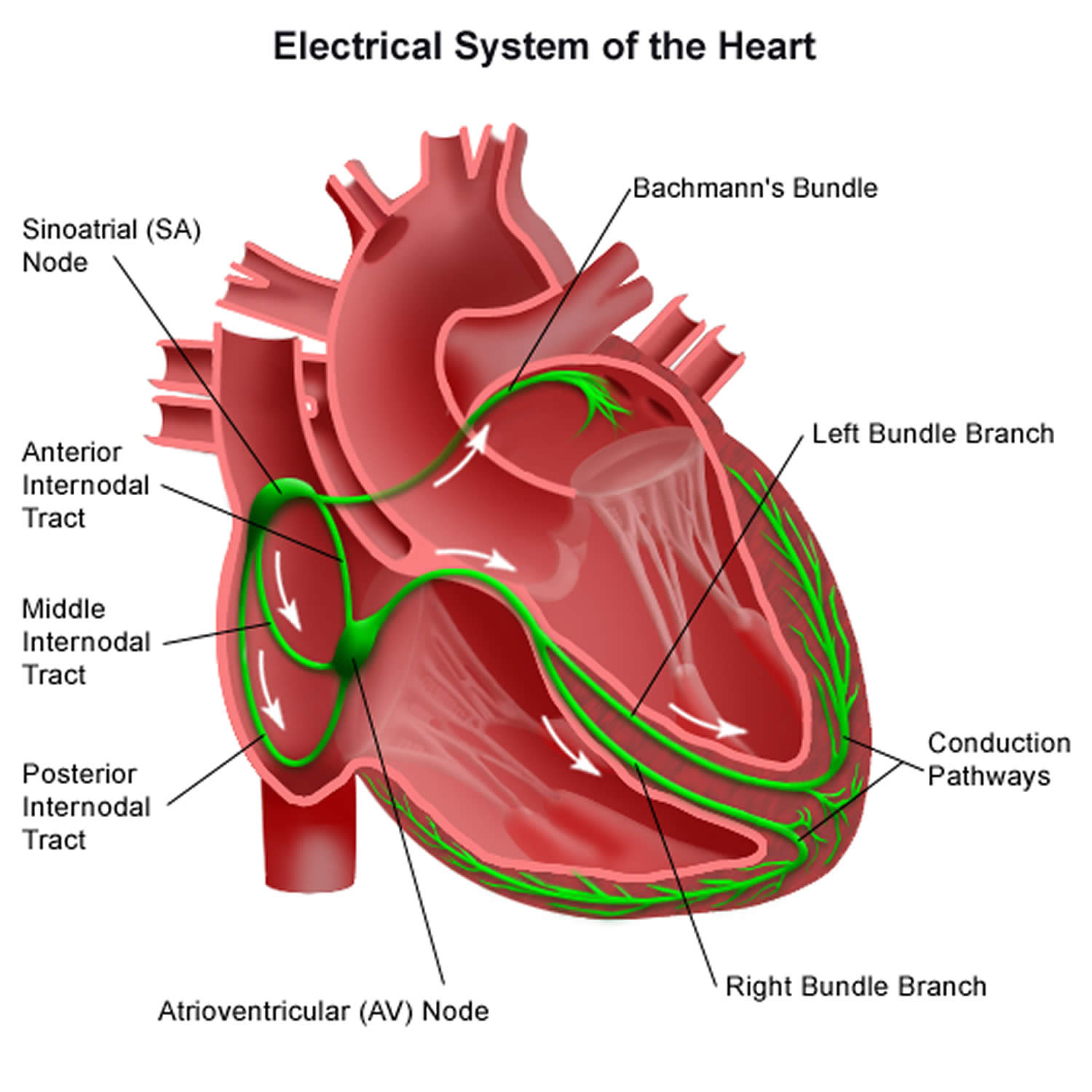
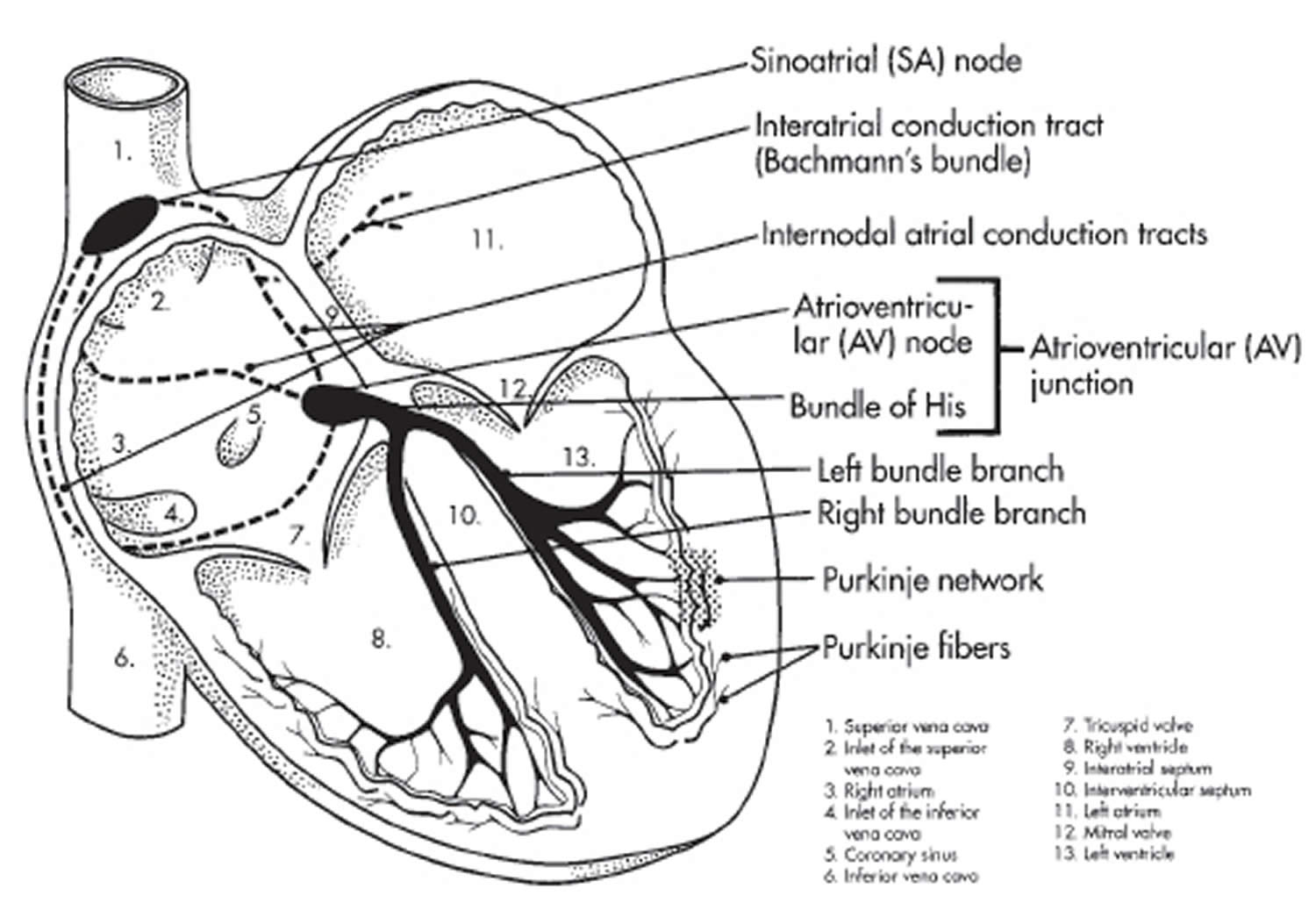
Heart’s Electrical System
To understand atrial fibrillation, it helps to understand the heart’s internal electrical system. The heart’s electrical system controls the rate and rhythm of the heartbeat (see Figure 1).
Your heartbeat is the contraction of your heart to pump blood to your lungs and the rest of your body. Your heart’s electrical system determines how fast your heart beats. The contraction of the atria and ventricles makes a heartbeat. After your atria pump blood into the ventricles, the valves between the atria and ventricles close to prevent backflow. After your ventricles contract to pump blood away from the heart, the aortic and pulmonary valves close.
Your heart’s electrical system is made up of three main parts:
- The sinoatrial (SA) node, located in the right atrium of your heart
- The atrioventricular (AV) node, located on the interatrial septum close to the tricuspid valve
- The His-Purkinje system, located along the walls of your heart’s ventricles
Each beat of your heart is set in motion by an electrical signal from within your heart muscle. The signal is generated as the vena cavae fill your heart’s right atrium with blood from other parts of your body. The signal spreads across the cells of your heart’s right and left atria. In a normal, healthy heart, each beat begins with a signal from the natural pacemaker called the sinoatrial (SA) node — or sinus node — an area of specialized cells in the right atrium. This is why the sinoatrial (SA) node sometimes is called your heart’s natural pacemaker. Your pulse, or heart rate, is the number of signals the SA node produces per minute. In a healthy adult heart at rest, the SA node sends an electrical signal to begin a new heartbeat 60 to 100 times a minute. (This rate may be slower in very fit athletes.)
The sinoatrial (SA) node produces electrical impulses that normally start each heartbeat. This natural pacemaker produces the electrical impulses that trigger the normal heartbeat. From the sinus node, electrical impulses travel across the atria to the ventricles, causing them to contract and pump blood to your lungs and body.
From the sinoatrial (SA) node, electrical impulses travel across the atria, causing the atrial muscles to contract and pump blood into the ventricles.
The electrical impulses then arrive at a cluster of cells called the atrioventricular (AV) node — usually the only pathway for signals to travel from the atria to the ventricles.
The atrioventricular (AV) node slows down the electrical signal before sending it to the ventricles. This slight delay allows the ventricles to fill with blood.
The signal is released and moves along a pathway called the bundle of His, which is located in the walls of your heart’s ventricles. From the bundle of His, the signal fibers divide into left and right bundle branches through the Purkinje fibers. These fibers connect directly to the cells in the walls of your heart’s left and right ventricles.
The signal spreads across the cells of your ventricle walls, and both ventricles contract. However, this doesn’t happen at exactly the same moment.
The left ventricle contracts an instant before the right ventricle. This pushes blood through the pulmonary valve (for the right ventricle) to your lungs, and through the aortic valve (for the left ventricle) to the rest of your body.
As the signal passes, the walls of the ventricles relax and await the next signal.
This process continues over and over as the atria refill with blood and more electrical signals come from the SA node.
When electrical impulses reach the muscles of the ventricles, they contract, causing them to pump blood either to the lungs or to the rest of your body.
When anything disrupts this complex system, it can cause the heart to beat too fast (tachycardia), too slow (bradycardia) or with an irregular rhythm.
Your heart’s electrical system controls all the events that occur when your heart pumps blood. The electrical system also is called the cardiac conduction system. If you’ve ever seen the heart test called an EKG (electrocardiogram), you’ve seen a graphical picture of the heart’s electrical activity.
Figure 1. The heart’s electrical system
Electrical Problem in Atrial Fibrillation
In atrial fibrillation, the heart’s electrical signals don’t begin in the SA node. Instead, they begin in another part of the atria or in the nearby pulmonary veins. The signals don’t travel normally. They may spread throughout the atria in a rapid, disorganized way. This can cause the atria to fibrillate (quiver).
The faulty signals flood the AV node with electrical impulses. As a result, the ventricles also begin to beat very fast. However, the AV node can’t send the signals to the ventricles as fast as they arrive. So, even though the ventricles are beating faster than normal, they aren’t beating as fast as the atria.
Thus, the atria and ventricles no longer beat in a coordinated way. This creates a fast and irregular heart rhythm. In atrial fibrillation, the ventricles may beat 100 to 175 times a minute, in contrast to the normal rate of 60 to 100 beats a minute.
If this happens, blood isn’t pumped into the ventricles as well as it should be. Also, the amount of blood pumped out of the ventricles to the body is based on the random atrial beats.
The body may get rapid, small amounts of blood and occasional larger amounts of blood. The amount will depend on how much blood has flowed from the atria to the ventricles with each beat.
Most of the symptoms of atrial fibrillation are related to how fast the heart is beating. If medicines or age slow the heart rate, the symptoms are minimized.
Atrial fibrillation may be brief, with symptoms that come and go and end on their own [paroxysmal atrial fibrillation]. Or, the condition may be ongoing and require treatment. Sometimes atrial fibrillation is permanent, and medicines or other treatments can’t restore a normal heart rhythm.
Types of atrial fibrillation
The symptoms are generally the same; however the duration of the atrial fibrillation and underlying reasons for the condition help doctors classify the type of atrial fibrillation problems.
- All types of atrial fibrillation can increase your risk of stroke. Even if you have no symptoms at all, you are nearly 5 times more likely to have a stroke than someone who doesn’t have atrial fibrillation.
Paroxysmal atrial fibrillation
Paroxysmal atrial fibrillation is when the heart returns to a normal rhythm on its own, or with intervention, within 7 days of its start. People who have this type of atrial fibrillation may have episodes only a few times a year or their symptoms may occur every day. These symptoms are very unpredictable and often can turn into a permanent form of atrial fibrillation.
Over a period of time, paroxysmal fibrillation may become more frequent and longer lasting, sometimes leading to permanent or chronic atrial fibrillation.
Persistent atrial fibrillation
Persistent atrial fibrillation is defined as an irregular rhythm that lasts for longer than 7 days. This type of atrial fibrillation will not return to normal sinus rhythm on its own and will require some form of treatment such as an electrical shock procedure called cardioversion or medications in order to restore your heart rhythm.
Long-standing atrial fibrillation
Long-standing atrial fibrillation is when the heart is consistently in an irregular rhythm that lasts longer than 12 months.
Permanent atrial fibrillation
Permanent atrial fibrillation occurs when the condition lasts indefinitely and the patient and doctor have decided not to continue further attempts to restore normal rhythm. You’ll often require medications to control your heart rate and to prevent blood clots.
Nonvalvular atrial fibrillation
Nonvalvular atrial fibrillation is atrial fibrillation not caused by a heart valve issue.
Complications of atrial fibrillation
Sometimes atrial fibrillation can lead to the following complications:
Stroke
In atrial fibrillation, the chaotic rhythm may cause blood to pool in your heart’s upper chambers (atria) and form clots. If a blood clot forms, it could dislodge from your heart and travel to your brain. There it might block blood flow, causing a stroke.
The risk of a stroke in atrial fibrillation depends on your age (you have a higher risk as you age) and on whether you have high blood pressure, diabetes, a history of heart failure or previous stroke, and other factors. Certain medications, such as blood thinners, can greatly lower your risk of a stroke or the damage to other organs caused by blood clots.
Heart Failure
Atrial fibrillation, especially if not controlled, may weaken the heart and lead to heart failure — a condition in which your heart can’t circulate enough blood to meet your body’s needs.
Fatigue and shortness of breath are common symptoms of heart failure. A buildup of fluid in the lungs causes these symptoms. Fluid also can build up in the feet, ankles, and legs, causing weight gain.
Lifestyle changes, medicines, and procedures or surgery (rarely, a mechanical heart pump or heart transplant) are the main treatments for heart failure.
Atrial fibrillation symptoms
Some people with atrial fibrillation, particularly older people, don’t have any symptoms. Also, over time, some people get used to their symptoms or think they have them just because they’re getting older.
The abnormality in heart rhythm (also known as an arrhythmia) is often only discovered during routine tests or investigations for another condition. Sometimes AF is diagnosed after a person goes to see their doctor because they can feel their heart beating fast or with an irregular rhythm. Your doctor will only be able to confirm that you have AF once you have had an electrocardiogram (ECG).
People often attribute tiredness and feeling lethargic to ageing, but once normal rhythm is restored, they realize that these symptoms were caused by atrial fibrillation.
The way the heart beats in atrial fibrillation reduces the heart’s performance and efficiency. This can lead to low blood pressure (hypotension) and heart failure.
Your symptoms depend partly on the type of atrial fibrillation (AF) you have. Those who do have atrial fibrillation symptoms may experience signs and symptoms such as:
- Palpitations, which are sensations of a racing, uncomfortable, irregular heartbeat or a flip-flopping in your chest. Palpitations are a common symptom of AF.
- Weakness
- Reduced ability to exercise
- Fatigue or feeling tired
- Lightheadedness or feeling faint at times
- Dizziness
- Shortness of breath
- Chest pain
You should see your doctor immediately if you notice a sudden change in your heartbeat and experience chest pain.
- Chest pain or pressure is a medical emergency. You may be having a heart attack. Call your local emergency number immediately!
- Don’t Wait–Get Help Quickly
- Quick Action Can Save Your Life
- If you think you or someone else is having a heart attack, even if you’re not sure, don’t feel embarrassed to call your local emergency number right away !
- Do not drive to the hospital or let someone else drive you. Call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room. Take a nitroglycerin pill if your doctor has prescribed this type of treatment.
Those who do have atrial fibrillation symptoms may experience signs and symptoms such as:
Heart palpitations
The most obvious symptom of atrial fibrillation is heart palpitations – where your heart may feel like it’s pounding, fluttering or beating irregularly, often for a few seconds or possibly a few minutes.
As well as an irregular heartbeat, your heart may also beat very fast (often considerably higher than 100 beats per minute).
You can work out your heart rate by checking the pulse in your neck or wrist.
Other symptoms you may experience if you have atrial fibrillation include:
- General fatigue
- Tiredness, and being less able to exercise
- Breathlessness
- Feeling faint or lightheaded
- Chest pain or pressure**
- Rapid and irregular heartbeat
- Fluttering or “thumping” in the chest
- Dizziness
- Shortness of breath and anxiety
- Weakness
- Faintness or confusion
- Fatigue when exercising
- Sweating
**Chest pain or pressure is a medical emergency. You may be having a heart attack. Call your local emergency number immediately!
- Don’t Wait–Get Help Quickly
- Quick Action Can Save Your Life
- If you think you or someone else is having a heart attack, even if you’re not sure, don’t feel embarrassed to call your local emergency number right away !
- Do not drive to the hospital or let someone else drive you. Call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room. Take a nitroglycerin pill if your doctor has prescribed this type of treatment.
How are heart attack symptoms different from atrial fibrillation symptoms?
Fluttering and palpitations are key symptoms of atrial fibrillation and is the key difference, but many heart problems have similar warning signs.
- If you think you may be having a heart attack, DON’T DELAY. Get emergency help by calling local emergency number immediately.
- A heart attack is a blockage of blood flow to the heart, often caused by a clot or build-up of plaque lodging in the coronary artery (a blood vessel that carries blood to part of the heart muscle).
- A heart attack can damage or destroy part of your heart muscle. Some heart attacks are sudden and intense. But most heart attacks start slowly, with mild pain or discomfort. Often people affected aren’t sure what’s wrong and wait too long before getting help. Call your local emergency number immediately!
How to check your pulse
You can check to see if you might have atrial fibrillation by feeling your pulse at your wrist. A normal pulse should follow a steady beat. If you have atrial fibrillation (AF), your pulse will feel irregular, erratic and possibly fast, and the strength will vary. If your pulse feels like this, or if you’re concerned, see your doctor.
Finding your pulse
The easiest places to find your pulse are:
Your wrist
- Put one of your hands out so you’re looking at your palm.
- Use the first finger (your index finger) and middle finger of your other hand and place the pads of these fingers on the inside of your wrist, at the base of your thumb.
- Press lightly and feel the pulse. If you can’t feel anything press slightly harder or move your fingers around until you feel your pulse.
How to check your pulse
Once you’ve found your pulse, continue to feel it for about 20-30 seconds. Feel your pulse and check if it’s regular or irregular. You can work out your heart rate in beats per minute (bpm) by:
- counting the number of beats in your pulse after 60 seconds, or
- counting the beats for 30 seconds and multiplying by two.
If your pulse feels irregular, you should check for a full 60 seconds.
What should you check?
Your heart rate:
- Most adults have a resting heart rate between 60 and 100 bpm
- Your heart rate may be lower if you do lots of exercise and are very fit. Some athletes have heart rates ranging from 40 to 60 bpm.
Your heart rhythm:
- Occasional irregularities such as missed beats are very common and usually nothing to worry about, but it is still best to check this with your doctor.
- An irregular pulse could also be a sign of an arrhythmia (an abnormal heart rhythm), such as Atrial Fibrillation (AF). This is more likely if you are 65 or older.
Listen to the example heart rhythms below to help you spot an irregular heart beat:
Regular pulse
Irregular pulse
Living With Atrial Fibrillation
People who have atrial fibrillation—even permanent atrial fibrillation—can live normal, active lives. If you have atrial fibrillation, ongoing medical care is important.
Keep all your medical appointments. Bring a list of all the medicines you’re taking to every doctor and emergency room visit. This will help your doctor know exactly what medicines you’re taking.
Follow your doctor’s instructions for taking medicines. Be careful about taking over-the-counter medicines, nutritional supplements, and cold and allergy medicines. Some of these products contain stimulants that can trigger rapid heart rhythms. Also, some over-the-counter medicines can have harmful interactions with heart rhythm medicines.
Tell your doctor if your medicines are causing side effects, if your symptoms are getting worse, or if you have new symptoms.
If you’re taking blood-thinning medicines, you’ll need to be carefully monitored. For example, you may need routine blood tests to check how the medicines are working. Also, talk with your doctor about your diet. Some foods, such as leafy green vegetables, may interfere with warfarin, a blood-thinning medicine.
Ask your doctor about physical activity, weight control, and alcohol use. Find out what steps you can take to manage your condition.
I have atrial fibrillation. Should I participate in physical activity?
Regular physical activity is an important way for you to live a healthy lifestyle, which can make you feel better and decrease symptoms while dealing with heart conditions such as atrial fibrillation, a common heart rhythm disorder. Getting active can also help prevent other heart diseases or strokes.
One study found that moderate physical activity is safe and effective for people with atrial fibrillation. Physical activity also helped improve their quality of life and increase their ability to exercise and participate in daily living activities.
However, research is conflicting regarding the effects of vigorous physical activity in people with atrial fibrillation. More research is needed to determine the effects of physical activity in people with atrial fibrillation.
Be sure to ask your doctor before beginning an exercise program to ensure it is safe and effective for you. Sometimes you may need medications, such as beta blockers, to prevent your heart from beating too fast at rest and with exercise. You may also benefit from cardiac rehabilitation.
The American Heart Association recommends at least 150 minutes of moderate physical activity for adults each week. Also, aim to include strength training exercises at least twice a week. You may want to do stretching exercises as part of your exercise routine.
Physical activity can include many options, such as:
- Climbing stairs
- Walking
- Jogging
- Swimming
- Biking
- Playing sports
It’s OK if you can’t exercise for long periods of time when you first begin. Even 10 minutes of exercise three times each day can reap health benefits.
So start moving. Even if you can only exercise for a short time at first, do what you can. Work your way toward larger fitness goals as you’re able.
Sex
Sex is similar to any other physical activity so, as long as your symptoms are well controlled, having AF should not stop you from having sex.
Travel
You should be able to travel by air as long as you take your anticoagulant medicine in the way your doctor has prescribed and your symptoms are well controlled. It is best to check with your doctor before you travel.
You should find out where your nearest anticoagulation clinic or hospital is at your destination. If you are traveling long distances that involve a change in time, you will need to ask your anticoagulation specialist or doctor for advice about adjusting the timings of your anticoagulation.
It’s also important that you tell your travel insurance company that you have AF. If you don’t, this could invalidate your insurance.
What causes atrial fibrillation
Atrial fibrillation (AF) occurs if the heart’s electrical signals don’t travel through the heart in a normal way. Instead, they become very rapid and disorganized.
Damage to the heart’s electrical system causes atrial fibrillation. The damage most often is the result of other conditions that affect the health of the heart, such as high blood pressure and coronary heart disease.
The risk of atrial fibrillation increases as you age. Inflammation also is thought to play a role in causing atrial fibrillation.
Sometimes, the cause of atrial fibrillation is unknown.
Possible causes of atrial fibrillation
- Abnormalities or damage to the heart’s structure are the most common cause of atrial fibrillation.
Possible causes of atrial fibrillation include:
- High blood pressure
- Heart attacks
- Coronary artery disease
- Abnormal heart valves
- Heart defects you’re born with (congenital)
- An overactive thyroid gland or other metabolic imbalance
- Exposure to stimulants, such as medications, caffeine, tobacco or alcohol
- Sick sinus syndrome — improper functioning of the heart’s natural pacemaker
- Lung diseases
- Previous heart surgery
- Viral infections
- Stress due to pneumonia, surgery or other illnesses
- Sleep apnea
However, some people who have atrial fibrillation don’t have any heart defects or damage, a condition called lone atrial fibrillation. In lone atrial fibrillation, the cause is often unclear, and serious complications are rare.
Atrial flutter
Atrial flutter is similar to atrial fibrillation, but the rhythm in your atria is more organized and less chaotic than the abnormal patterns common with atrial fibrillation. Sometimes you may have atrial flutter that develops into atrial fibrillation and vice versa.
The risk factors for and the symptoms and causes of atrial flutter are similar to those of atrial fibrillation. For example, strokes are also a concern in someone with atrial flutter. As with atrial fibrillation, atrial flutter is usually not life-threatening when it’s properly treated.
Major Risk factors for Atrial Fibrillation
Atrial fibrillation is more common in people who have:
- High blood pressure. Having high blood pressure, especially if it’s not well-controlled with lifestyle changes or medications, can increase your risk of atrial fibrillation.
- Coronary heart disease (coronary artery disease)
- Heart failure
- Rheumatic heart disease
- Structural heart defects, such as mitral valve prolapse
- Heart disease. Anyone with heart disease — such as heart valve problems, congenital heart disease, congestive heart failure, coronary artery disease, or a history of heart attack or heart surgery — has an increased risk of atrial fibrillation.
- Pericarditis (a condition in which the membrane, or sac, around your heart is inflamed)
- Congenital heart defects
- Sick sinus syndrome (a condition in which the heart’s electrical signals don’t fire properly and the heart rate slows down; sometimes the heart will switch back and forth between a slow rate and a fast rate)
Atrial fibrillation also is more common in people who are having heart attacks or who have just had surgery.
Certain factors may increase your risk of developing atrial fibrillation.
These include:
- Age. The older you are, the greater your risk of developing atrial fibrillation.
- Other chronic conditions. People with certain chronic conditions such as thyroid problems, sleep apnea, metabolic syndrome, diabetes, chronic kidney disease or lung disease have an increased risk of atrial fibrillation.
- Drinking alcohol. For some people, drinking alcohol can trigger an episode of atrial fibrillation. Binge drinking may put you at an even higher risk.
- Obesity. People who are obese are at higher risk of developing atrial fibrillation.
- Metabolic syndrome also raises your risk for atrial fibrillation. Metabolic syndrome is the name for a group of risk factors that raises your risk for coronary heart disease and other health problems, such as diabetes and stroke.
- Family history. An increased risk of atrial fibrillation is present in some families.
- Caffeine or psychological stress also may trigger atrial fibrillation in some people.
- Some data suggest that people who have sleep apnea are at greater risk for atrial fibrillation. Sleep apnea is a common disorder that causes one or more pauses in breathing or shallow breaths while you sleep.
- Research suggests that people who receive high-dose steroid (corticosteroid) therapy are at increased risk for atrial fibrillation. This therapy is used for asthma and some inflammatory conditions. It may act as a trigger in people who have other atrial fibrillation risk factors.
- Genetic factors also may play a role in causing atrial fibrillation. However, their role isn’t fully known.
Atrial fibrillation prevention
Following a healthy lifestyle and taking steps to lower your risk for heart disease may help you prevent atrial fibrillation. These steps include:
- Following a heart healthy diet that’s low in saturated fat, trans fat, and cholesterol. A healthy diet includes a variety of whole grains, fruits, and vegetables daily.
- Not smoking.
- Being physically active.
- Maintaining a healthy weight.
If you already have heart disease or other atrial fibrillation risk factors, work with your doctor to manage your condition. In addition to adopting the healthy habits above, which can help control heart disease, your doctor may advise you to:
- Follow the DASH (Dietary Approaches to Stop Hypertension) eating plan to help lower your blood pressure.
- Keep your cholesterol and triglycerides at healthy levels with dietary changes and medicines (if prescribed).
- Limit or avoid alcohol.
- Control your blood sugar level if you have diabetes.
- Get ongoing medical care and take your medicines as prescribed.
Atrial fibrillation diagnosis
A healthcare professional can identify an irregular heartbeat by checking your pulse or listening to your heart with a stethoscope, but an electrocardiogram (ECG or EKG) is the most reliable method to detect and confirm the presence of atrial fibrillation. If the atrial fibrillation comes and goes intermittently (paroxysmal atrial fibrillation), it may be necessary for you to wear a Holter monitor (a portable ECG monitor) or an event recorder to detect it.
Electrocardiogram
Electrocardiogram (ECG) or EKG is the most useful test for diagnosing atrial fibrillation.
It’s only possible to confirm a diagnosis of atrial fibrillation after you’ve had an electrocardiogram (ECG). This is a test that records the rhythm and electrical activity of your heart.
An ECG shows how fast your heart is beating and its rhythm (steady or irregular). It also records the strength and timing of electrical signals as they pass through your heart.
A standard ECG only records the heartbeat for a few seconds. It won’t detect atrial fibrillation that doesn’t happen during the test. To diagnose paroxysmal atrial fibrillation, your doctor may ask you to wear a portable ECG monitor that can record your heartbeat for longer periods.
The two most common types of portable ECGs are Holter and event monitors.
Holter and Event Monitors
A Holter monitor records the heart’s electrical activity for a full 24- or 48-hour period. You wear small patches called electrodes on your chest. Wires connect these patches to a small, portable recorder. The recorder can be clipped to a belt, kept in a pocket, or hung around your neck.
You wear the Holter monitor while you do your normal daily activities. This allows the monitor to record your heart for a longer time than a standard ECG.
An event monitor is similar to a Holter monitor. You wear an event monitor while doing your normal activities. However, an event monitor only records your heart’s electrical activity at certain times while you’re wearing it.
For many event monitors, you push a button to start the monitor when you feel symptoms. Other event monitors start automatically when they sense abnormal heart rhythms.
You can wear an event monitor for weeks or until symptoms occur.
Figure 2. Atrial fibrillation ECG (EKG)
 Stress Test
Stress Test
Some heart problems are easier to diagnose when your heart is working hard and beating fast. During stress testing, you exercise to make your heart work hard and beat fast while heart tests are done. If you can’t exercise, you may be given medicine to make your heart work hard and beat fast.
Echocardiography
Echocardiography (echo) uses sound waves to create a moving picture of your heart. The test shows the size and shape of your heart and how well your heart chambers and valves are working.
Echo also can identify areas of poor blood flow to the heart, areas of heart muscle that aren’t contracting normally, and previous injury to the heart muscle caused by poor blood flow.
This test sometimes is called transthoracic echocardiography. It’s painless and noninvasive (no instruments are inserted into the body). For the test, a device called a transducer is moved back and forth over your chest. The device sends special sound waves through your chest wall to your heart.
The sound waves bounce off the structures of your heart, and a computer converts them into pictures on a screen.
Transesophageal Echocardiography
Transesophageal echo, or TEE, uses sound waves to take pictures of your heart through the esophagus. The esophagus is the passage leading from your mouth to your stomach.
Your heart’s upper chambers, the atria, are deep in your chest. They often can’t be seen very well using transthoracic echo. Your doctor can see the atria much better using transesophageal echo (TEE).
During this test, the transducer is attached to the end of a flexible tube. The tube is guided down your throat and into your esophagus. You’ll likely be given medicine to help you relax during the procedure.
Transesophageal echo is used to detect blood clots that may be forming in the atria because of atrial fibrillation.
Chest X Ray
A chest x ray is a painless test that creates pictures of the structures in your chest, such as your heart and lungs. This test can show fluid buildup in the lungs and signs of other atrial fibrillation complications.
Blood Tests
Blood tests check the level of thyroid hormone in your body and the balance of your body’s electrolytes. Electrolytes are minerals that help maintain fluid levels and acid-base balance in the body. They’re essential for normal health and functioning of your body’s cells and organs.
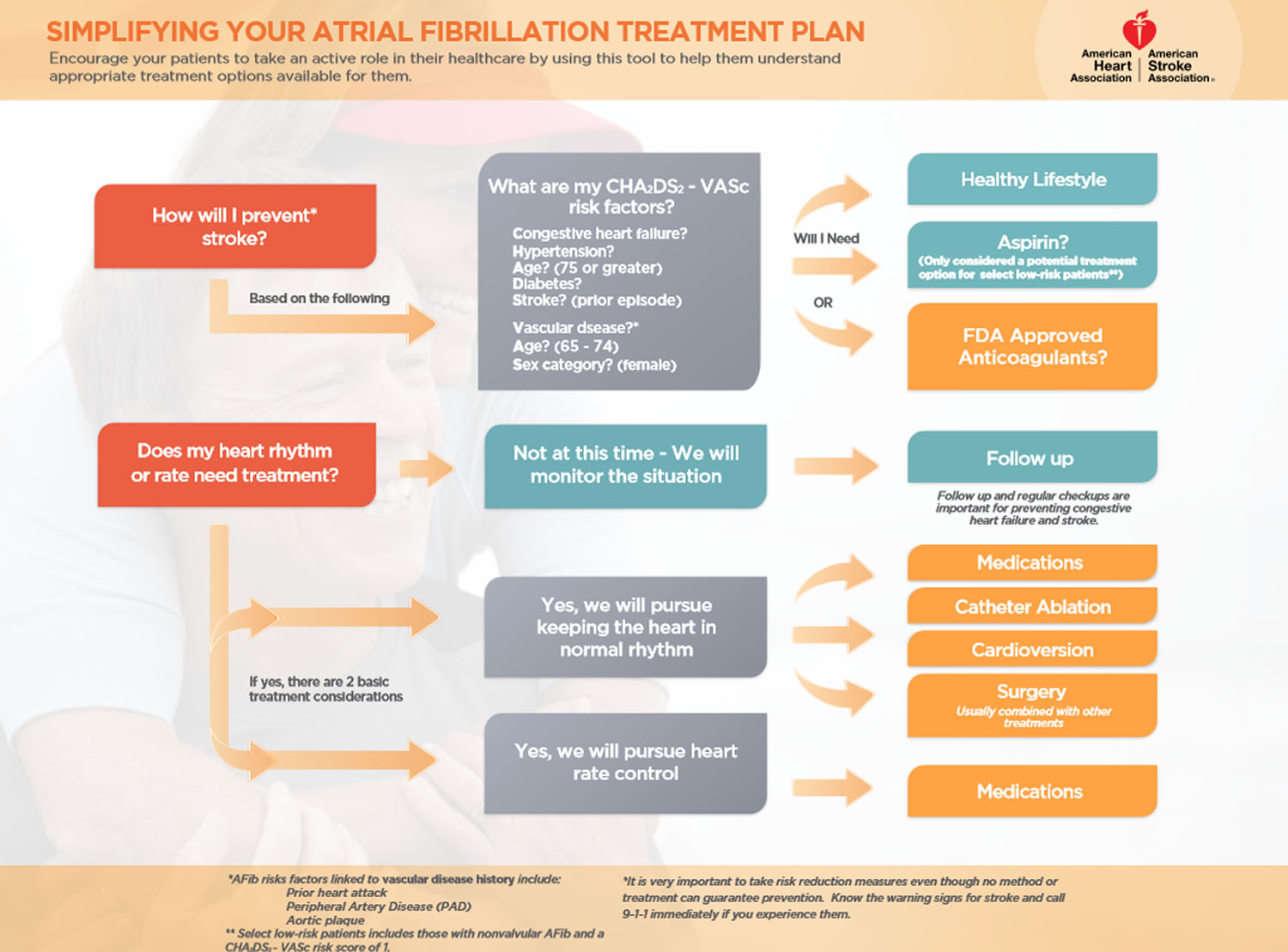
Atrial fibrillation treatment
Treatment for atrial fibrillation depends on how often you have symptoms, how severe they are, and whether you already have heart disease. General treatment options include medicines, medical procedures, and lifestyle changes.
Your doctor will assess your risk of having a stroke or another major complication. This will help to decide on the best treatment for you. The assessment – known as the CHA2DS2-VASc points system (see below) – takes into account:
- your age (the older you are, the greater your risk of having a stroke)
- how well your heart is working
- if you already have heart disease
- if you have diabetes
- your gender
- if you have already had a stroke or symptoms of a stroke, and
- your blood pressure.
CHA2DS2–VASc
- Congestive heart failure
- Hypertension
- Age (75 or greater)
- Diabetes
- Stroke (prior episode)
- Vascular disease (prior heart attack, peripheral artery disease or aortic plaque)
- Age 65-74
- Sex (female)
The main aims in treating your atrial fibrillation are:
- to reduce your risk of developing a blood clot and
- to control your heart rate and rhythm, which should help to control any symptoms you’re having.
Your doctor may decide to give you a medicine, called an anticoagulant, to reduce the risk of blood clots forming and causing a stroke. If your CHA2DS2-VASc score is more than 1 on the points system, you will probably be offered an anticoagulant. Many people have spells of atrial fibrillation and don’t even know it — so you may need lifelong anticoagulants even after your rhythm has been restored to normal. However, not everyone will be prescribed an anticoagulant to reduce their risk. For a small number of people, the risk of having a stroke caused by bleeding in the brain may be greater than the risk of having a stroke caused by a clot. If this applies to you, you can discuss it with your doctor.
If you are unable to take either warfarin or the new oral anticoagulants or if there is a clinical reason that makes it unsafe for you to take them, you may be offered a procedure called a left atrial appendage closure. This is where a special device is inserted into your heart. If any blood clots form, the device helps to prevent them from traveling to your brain and causing a stroke.
Doctors use several procedures to restore a normal heart rhythm. For example, they may use electrical cardioversion to treat a fast or irregular heartbeat. For this procedure, low-energy shocks are given to your heart to trigger a normal rhythm. You’re temporarily put to sleep before you receive the shocks.
Electrical cardioversion isn’t the same as the emergency heart shocking procedure often seen on TV programs. It’s planned in advance and done under carefully controlled conditions.
Before doing electrical cardioversion, your doctor may recommend transesophageal echocardiography (TEE). This test can rule out the presence of blood clots in the atria. If clots are present, you may need to take blood-thinning medicines before the procedure. These medicines can help get rid of the clots.
Goals of Atrial Fibrillation Treatment
The goals of treating atrial fibrillation include:
- Preventing blood clots from forming, thus lowering the risk of stroke (called prevention of thromboembolism such as stroke).
- Controlling how many times a minute the ventricles contract. This is called rate control. Rate control is important because it allows the ventricles enough time to completely fill with blood. With this approach, the abnormal heart rhythm continues, but you feel better and have fewer symptoms.
- Restoring a normal heart rhythm. This is called rhythm control. Rhythm control allows the atria and ventricles to work together to efficiently pump blood to the body.
- Treating any underlying disorder that’s causing or raising the risk of atrial fibrillation—for example, hyperthyroidism (too much thyroid hormone).
- Managing risk factors for stroke
- Preventing additional heart rhythm problems
- Preventing heart failure
The strategy you and your doctor choose depends on many factors, including whether you have other problems with your heart and if you’re able to take medications that can control your heart rhythm. In some cases, you may need a more invasive treatment, such as medical procedures using catheters or surgery.
In some people, a specific event or an underlying condition, such as a thyroid disorder, may trigger atrial fibrillation. Treating the condition causing atrial fibrillation may help relieve your heart rhythm problems. If your symptoms are bothersome or if this is your first episode of atrial fibrillation, your doctor may attempt to reset the rhythm.
Resetting your heart’s rhythm
Ideally, to treat atrial fibrillation, the heart rate and rhythm are reset to normal. To correct your condition, doctors may be able to reset your heart to its regular rhythm (sinus rhythm) using a procedure called cardioversion, depending on the underlying cause of atrial fibrillation and how long you’ve had it.
Cardioversion can be done in two ways:
- Electrical cardioversion. In this brief procedure, an electrical shock is delivered to your heart through paddles or patches placed on your chest. The shock stops your heart’s electrical activity for a short moment. The goal is to reset your heart’s normal rhythm. You will be given a sedative before the procedure, so you shouldn’t feel the electric shock. You may also receive medications to help restore a normal heartbeat (anti-arrhythmics) before the procedure.
- Cardioversion with drugs. This form of cardioversion uses medications called anti-arrhythmics to help restore normal sinus rhythm. Depending on your heart condition, you may receive medications through an IV or by mouth to help return your heart to normal rhythm. This is often done in the hospital with continuous monitoring of your heart rate. If your heart rhythm returns to normal, your doctor often will prescribe the same anti-arrhythmic medication or a similar one to try to prevent more spells of atrial fibrillation.
Before cardioversion, you may be given warfarin or another blood-thinning medication for several weeks to reduce the risk of blood clots and strokes. If your episode of atrial fibrillation lasted more than 48 hours, you may need to take this type of medication for at least a month after the procedure to prevent blood clots in the heart.
Maintaining a normal heart rhythm
After electrical cardioversion, your doctor may prescribe anti-arrhythmic medications to help prevent future episodes of atrial fibrillation. Medications may include:
- Dofetilide
- Flecainide
- Propafenone
- Amiodarone
- Sotalol
Although these drugs may help maintain a normal heart rhythm, they can cause side effects, including:
- Nausea
- Dizziness
- Fatigue
Rarely, they may cause ventricular arrhythmias — life-threatening rhythm disturbances originating in the heart’s lower chambers. These medications may be needed indefinitely. Even with medications, there is a chance of another episode of atrial fibrillation.
Heart rate control
You may be prescribed medications to control how fast your heart beats and restore it to a normal rate.
- Digoxin. This medication may control the heart rate at rest, but not as well during activity. Most people need additional or alternative medications, such as calcium channel blockers or beta blockers.
- Beta blockers. These medications can help to slow the heart rate at rest and during activity. They may cause side effects such as low blood pressure (hypotension).
- Calcium channel blockers. These medicines also can control your heart rate, but may need to be avoided if you have heart failure or low blood pressure.
Catheter and surgical procedures
Sometimes medications or cardioversion to control atrial fibrillation doesn’t work. In those cases, your doctor may recommend a procedure to destroy the area of heart tissue that’s causing the erratic electrical signals and restore your heart to a normal rhythm.
Treating Underlying Causes and Reducing Risk Factors
Your doctor may recommend treatments for an underlying cause of atrial fibrillation or to reduce atrial fibrillation risk factors. For example, he or she may prescribe medicines to treat an overactive thyroid, lower high blood pressure, or manage high blood cholesterol.
Your doctor also may recommend lifestyle changes, such as following a healthy diet, cutting back on salt intake (to help lower blood pressure), quitting smoking, and reducing stress.
Limiting or avoiding alcohol, caffeine, or other stimulants that may increase your heart rate also can help reduce your risk for atrial fibrillation.
Who Needs Treatment for Atrial Fibrillation?
People who have atrial fibrillation but don’t have symptoms or related heart problems may not need treatment. Atrial fibrillation may even go back to a normal heart rhythm on its own. (This also can occur in people who have atrial fibrillation with symptoms.)
In some people who have atrial fibrillation for the first time, doctors may choose to use an electrical procedure or medicine to restore a normal heart rhythm.
Repeat episodes of atrial fibrillation tend to cause changes to the heart’s electrical system, leading to persistent or permanent atrial fibrillation. Most people who have persistent or permanent AF need treatment to control their heart rate and prevent complications.
Atrial Fibrillation Treatment guideline
The American Heart Association Atrial Fibrillation Treatment guidelines 6 are written by a panel of experts to document the science that helps healthcare providers choose the right treatments. The guidelines spell out what is proven most helpful to the greatest number of people. Although the guidelines for atrial fibrillation are about 170 pages long, there are some basic decisions outlined in the treatment guidelines that every atrial fibrillation patient should understand.
- How will I prevent stroke?
Depending on your risk, you will likely either need some type of antithrombotic medication (such as warfarin, one of the new direct-acting oral anticoagulants or DOACs – dabigitran, apixaban, rivoraxaban or edoxaban) or maybe aspirin. - Do I need anticoagulant therapy?
Are there additional lifestyle modifications important for stroke prevention? - What is my CHA2DS2–VASc risk?
- Congestive heart failure
- Hypertension
- Age (75 or greater)
- Diabetes
- Stroke (prior episode)
- Vascular disease (prior heart attack, peripheral artery disease or aortic plaque)
- Age 65-74
- Sex (female)
- Are there options to control my heart rate and this irregular heart rhythm?
Based on your past medical history and risk for having a future stroke, there are several options for you and your healthcare provider to discuss in order to manage your atrial fibrillation.
Figure 3. Atrial fibrillation treatment guideline (American Heart Association)
[Source 6]Scoring Details for CHA2DS2–VASc
Ischemic stroke risk in patients with nonvalvular atrial fibrillation can be quantified by the CHA2DS2–VASc scoring algorithm. CHA2DS2–VASc assigns 1 point for each of the following risk factors:
- Congestive heart failure,
- Hypertension,
- Age 65 – 74,
- Diabetes,
- Vascular disease (prior myocardial infarction, peripheral arterial disease, or aortic
plaque), and - female Sex category (Table 2).
- Two points are assigned for a history of Stroke or transient ischemic attack, and Age ≥ 75 years.
Table 2. Annual Rate of Ischemic Stroke based on CHA2DS2–VASc Score.
| CHA2DS2–VASc | Annual rate of ischemic stroke (%/year) |
| 0 | 0.66 |
| 1 | 1.45 |
| 2 | 2.92 |
| 3 | 4.28 |
| 4 | 6.46 |
| 5 | 9.97 |
| 6 | 12.52 |
| 7 | 13.96 |
| 8 | 14.1 |
| 9 | 15.89 |
Scoring Details for HAS-BLED
Risk of major bleeding in patients with nonvalvular atrial fibrillation receiving treatment with warfarin can be quantified by the HAS-BLED scoring algorithm. HAS-BLED assigns 1 point for each of the following risk factors:
- poorly controlled Hypertension (systolic blood pressure ≥ 160 mmHg),
- Abnormal renal or liver function (one point each – renal transplantation or dialysis, or serum creatinine ≥ 2.26 mg/dl or 200 umol/L; chronic hepatitis or biochemical evidence of significant hepatic derangement – bilirubin > 2 x upper limit of normal in conjunction with AST/ALT > 3 x upper limit of normal),
- Stroke history, Bleeding history (history of previous bleed or predisposition to bleeding,
- Labile INR (time in therapeutic range < 60%), Elderly (age ≥65),
- Drugs or alcohol (one point each – alcohol abuse, or concomitant use of antiplatelet or non-steroidal anti-inflammatory drugs).
Table 3. Annual Rate of Major Bleeding while receiving warfarin based on HAS-BLED Score
| HAS-BLED Score | Annual rate of major bleeding (%/year) |
| 0 | 0 |
| 1 | 0.7 |
| 2 | 1.9 |
| 3 | 2.4 |
| 4 | 3.4 |
| 5 | 5.7 |
| 6 | 15.5 |
Blood Clot Prevention
People who have atrial fibrillation are at increased risk for stroke. This is because blood can pool in the heart’s upper chambers (the atria), causing a blood clot to form. If the clot breaks off and travels to the brain, it can cause a stroke.
Many people with atrial fibrillation or those who are undergoing certain treatments for atrial fibrillation are at especially high risk of blood clots that can lead to a stroke. The risk is even higher if other heart disease is present along with atrial fibrillation.
Preventing blood clots from forming is probably the most important part of treating atrial fibrillation. The benefits of this type of treatment have been proven in multiple studies.
Doctors prescribe blood-thinning medicines (anticoagulants) to prevent blood clots. These medicines include warfarin (Coumadin®), dabigatran, heparin, and aspirin.
Warfarin may be prescribed to prevent blood clots. If you’re prescribed warfarin, carefully follow your doctor’s instructions. Warfarin is a powerful medication that may cause dangerous bleeding. You’ll need to have regular blood tests to monitor warfarin’s effects.
Newer anticoagulants. Several newer blood-thinning medications (anticoagulants) are available. These medications include dabigatran, rivaroxaban, apixaban and edoxaban. These medications are shorter acting than warfarin and don’t require monitoring. Also, these medications are not approved for people who have mechanical heart valves. It’s very important to take these medications exactly as prescribed.
Dabigatran (Pradaxa) is an anticoagulant medication that’s as effective as warfarin at preventing blood clots that can lead to strokes, and doesn’t require blood tests to make sure you’re getting the proper dose.
You shouldn’t take dabigatran if you have a mechanical heart valve due to an increased risk of stroke or heart attack. Talk to your doctor about taking dabigatran as an alternative to warfarin if you’re concerned about your risk of stroke.
Rivaroxaban (Xarelto) is another anticoagulant medication that’s as effective as warfarin for preventing strokes. Rivaroxaban is a once-daily medication. Like any other anticoagulant, follow your doctor’s dosing instructions carefully and don’t stop taking rivaroxaban without talking to your doctor first.
Apixaban (Eliquis) is another anticoagulant medication that’s as effective as warfarin for preventing strokes.
People taking blood-thinning medicines need regular blood tests to check how well the medicines are working.
If you are unable to take either warfarin or new oral anticoagulants or if there is a clinical reason that makes it unsafe for you to take them, you may be offered a procedure called a left atrial appendage closure. This is where a special device is inserted into your heart. If any blood clots form, the device helps to prevent them from traveling to your brain and causing a stroke.
Rate Control
Doctors can prescribe medicines to slow down the rate at which the ventricles are beating. These medicines help bring the heart rate to a normal level.
Rate control is the recommended treatment for most patients who have atrial fibrillation, even though an abnormal heart rhythm continues and the heart doesn’t work as well as it should. Most people feel better and can function well if their heart rates are well-controlled.
Atrial fibrillation medications
Medicines used to control the heart rate include beta blockers (for example, metoprolol and atenolol), calcium channel blockers (diltiazem and verapamil), and digitalis (digoxin). Several other medicines also are available.
Rhythm Control
Restoring and maintaining a normal heart rhythm is a treatment approach recommended for people who aren’t doing well with rate control treatment. This treatment also may be used for people who have only recently started having atrial fibrillation. The long-term benefits of rhythm control have not been proven conclusively yet.
Doctors use medicines or procedures to control the heart’s rhythm. Patients often begin rhythm control treatment in a hospital so that their hearts can be closely watched.
The longer you have atrial fibrillation, the less likely it is that doctors can restore a normal heart rhythm. This is especially true for people who have had AF for 6 months or more.
Restoring a normal rhythm also becomes less likely if the atria are enlarged or if any underlying heart disease worsens. In these cases, the chance that AF will recur is high, even if you’re taking medicine to help convert atrial fibrillation to a normal rhythm.
Atrial fibrillation medications
Medicines used to control the heart rhythm include amiodarone, sotalol, flecainide, propafenone, dofetilide, and ibutilide. Sometimes older medicines—such as quinidine, procainamide, and disopyramide—are used.
Your doctor will carefully tailor the dose and type of medicines he or she prescribes to treat your atrial fibrillation. This is because medicines used to treat atrial fibrillation can cause a different kind of arrhythmia.
- These medicines also can harm people who have underlying diseases of the heart or other organs. This is especially true for patients who have an unusual heart rhythm problem called Wolff-Parkinson-White syndrome.
Your doctor may start you on a small dose of medicine and then gradually increase the dose until your symptoms are controlled. Medicines used for rhythm control can be given regularly by injection at a doctor’s office, clinic, or hospital. Or, you may routinely take pills to try to control atrial fibrillation or prevent repeat episodes.
If your doctor knows how you’ll react to a medicine, a specific dose may be prescribed for you to take on an as-needed basis if you have an episode of atrial fibrillation.
The ‘pill in the pocket’ approach
If you have paroxysmal atrial fibrillation (the type that comes and goes), your doctor may give you medicine to take only when the paroxysms (attacks or episodes) happen. This is known as the ‘pill in the pocket’ approach. Examples of medicines that are used for this approach include flecainide, sotalol and propafenone.
Your doctor is more likely to use this approach if:
- your heart is otherwise normal and the episodes of AF don’t happen very often, and
- when the episodes do happen, they respond quickly to your medicine.
You should only take this medicine when your AF happens, and it is important that you take only the dose you have been prescribed. If you feel very unwell even after taking the medicine, call your
doctor for advice.
Catheter and surgical procedures
Sometimes medications or cardioversion to control atrial fibrillation doesn’t work. In those cases, your doctor may recommend a procedure to destroy the area of heart tissue that’s causing the erratic electrical signals and restore your heart to a normal rhythm.
These options can include:
Catheter ablation
Catheter ablation may be used to restore a normal heart rhythm if medicines or electrical cardioversion don’t work. Your doctor may recommend this procedure if you have atrial fibrillation and an otherwise normal heart and medication has not improved your symptoms. It may also be helpful for heart failure patients who have an implanted device and cannot take or tolerate anti-arrhythmic medications.
In catheter ablation, a doctor inserts long, thin tubes (catheters) into a vein in your leg or arm and guides them through blood vessels to your heart. Electrodes at the catheter tips can use radiofrequency energy, extreme cold (cryotherapy) or heat to destroy these hot spots (areas of heart tissue that are causing rapid and irregular heartbeats), scarring the tissue so that the erratic signals are normalized. Cardiac ablation may correct the arrhythmia without the need for medications or implantable devices.
Approximately one-third of atrial fibrillation ablation procedures are currently performed in patients with persistent or long-standing persistent atrial fibrillation 7. In many people who have atrial fibrillation and an otherwise normal heart, atrial fibrillation is caused by rapidly discharging triggers, or “hot spots.” These hot spots are like abnormal pacemaker cells that fire so rapidly that the upper chambers of your heart quiver instead of beating efficiently.
Radio wave energy is sent through the wire to destroy abnormal tissue that may be disrupting the normal flow of electrical signals. An electrophysiologist usually does this procedure in a hospital. Your doctor may recommend a TEE before catheter ablation to check for blood clots in the atria.
Sometimes doctors use catheter ablation to destroy the atrioventricular (AV) node. The AV node is where the heart’s electrical signals pass from the atria to the ventricles (the heart’s lower chambers). This procedure requires your doctor to surgically implant a device called a pacemaker, which helps maintain a normal heart rhythm.
Research on the benefits of catheter ablation as a treatment for atrial fibrillation is still ongoing.
Table 4. Clinical factors that contribute to recurrent atrial fibrillation after catheter ablation and potential interventions that could reduce their impact on recurrent atrial fibrillation
| Factor associated with recurrent AF | Possible intervention |
| Age | None available |
| Chronic kidney disease | ? |
| Diabetes | Weight reduction, regular exercise (?) |
| Obesity | Weight reduction, regular exercise |
| Hypertension | Antihypertensive therapy, possibly including monoxidine and renin–angiotensin aldosterone inhibition |
| Heart failure | Therapy of HFrEF with ACE inhibitors, β blockers, mineralocorticoid antagonists, etc. |
| High ventricular rate | Rate control therapy (?) |
| Left atrial diameter | None available |
| Duration of continuous AF prior to ablation | Early rhythm control therapy (?) |
Abbreviations: ACE = angiotensin converting enzyme; AF = atrial fibrillation; HFrEF = heart failure with reduced ejection fraction; RAAS = renin–angiotensin aldosterone.
[Source 7]Maze procedure
There are several variations of the maze procedure. The doctor may use a scalpel, radiofrequency or extreme cold (cryotherapy) to create a pattern of scar tissue that interferes with stray electrical impulses that cause atrial fibrillation. The maze procedures have a high success rate, but atrial fibrillation may come back. If this happens, you may need another cardiac ablation or other heart treatment.
Because the surgical maze procedure (using a scalpel) requires open-heart surgery, it’s generally reserved for people who don’t get better with other treatments or when it can be done during a necessary heart surgery, such as coronary artery bypass surgery or heart valve repair. For this procedure, the surgeon makes small cuts or burns in the atria. These cuts or burns prevent the spread of disorganized electrical signals.
Because scar tissue doesn’t carry electricity, it interferes with stray electrical impulses that cause atrial fibrillation. Radiofrequency or cryotherapy also can be used to create the scars, and there are several variations of the surgical maze technique.
These procedures have a high success rate, but atrial fibrillation may recur. Some people may need catheter ablation or other treatment if atrial fibrillation recurs.
Atrioventricular (AV) node ablation
If medications or other forms of catheter ablation don’t work, or if you have side effects or are not a good candidate for other procedures, AV node ablation may be another option. The procedure involves applying radiofrequency energy to the pathway connecting the upper chambers (atria) and lower chambers (ventricles) of your heart (AV node) through a catheter to destroy this small area of tissue.
The procedure prevents the atria from sending electrical impulses to the ventricles. The atria continue to fibrillate, though. A pacemaker is then implanted to keep the ventricles beating properly. After AV node ablation, you’ll need to continue to take blood-thinning medications to reduce the risk of stroke because your heart rhythm is still atrial fibrillation.
Left atrial appendage closure
Your doctor may also consider a procedure called left atrial appendage closure. In this procedure, doctors insert a catheter through a vein in the leg and guide it to the upper right heart chamber (right atrium). Doctors then make a small hole in the wall between the upper heart chambers and guide the catheter to the upper left heart chamber (left atrium). A device called a left atrial appendage closure device is then inserted through the catheter to close a small sac (appendage) in the left atrium.
This may reduce the risk of blood clots in certain people with atrial fibrillation, as many blood clots that occur in atrial fibrillation form in the left atrial appendage. People who may be candidates for this procedure include those who don’t have heart valve problems, who have an increased risk of blood clots and bleeding, and who are aren’t able to take anticoagulants or they aren’t effective. Your doctor will evaluate you and determine if you’re a candidate for the procedure.
Pulmonary vein isolation
Atrial fibrillation is often triggered by electrical impulses from cells within the pulmonary veins – the veins that take blood from the lungs to the left atrium of the heart. Pulmonary vein isolation aims to stop these triggers from entering the heart and causing the atrial fibrillation. Most people who are offered pulmonary vein isolation treatment have tried several types of medicines first. You are more likely to be offered this treatment if you are getting symptoms with your atrial fibrillation even after being treated with medicines.
Pulmonary vein isolation procedure is often carried out using a local anesthetic in your groin, and a sedative to help you relax. A very small number of people have a general anesthetic instead of a local one. The procedure takes place in a specialized X-ray room called a catheter laboratory. You will be lying down on a bed while the procedure is carried out. Very thin wires called electrode catheters are passed into a vein at the top of your leg. They are then gently moved into position in your heart. Using radiofrequency waves or a freezing technique called cryoablation, the treatment produces a small circular scar around the pulmonary vein. The scar blocks the abnormal electrical impulses in this part of your heart.
Pulmonary vein isolation procedure can take several hours. It can be uncomfortable, but the sedative and anaesthetic should help ease the discomfort. After the procedure, you will need to stay lying down to rest for a few hours.
Your doctor may prescribe a different medicine for your atrial fibrillation depending on the result of the procedure, or they may ask you to take your usual medicine. You’ll also need to carry on taking your anticoagulant for a few weeks. The atrial fibrillation may continue for several weeks after the treatment before it settles down.
The most serious risk of a pulmonary vein isolation procedure is the risk of having a stroke either during the procedure or soon afterwards. Your doctor will discuss your individual risk with you.
Ablate and pace
If your medicines are not controlling your symptoms well but your doctor does not think you are suitable for a pulmonary vein isolation procedure, you may be offered a treatment called ablate and pace. Ablate and pace involves ‘ablating’ (destroying) the AV node and implanting an artificial pacemaker. You will need to go into hospital for the treatment and will probably have to stay in hospital for one night after the procedure.
You are more likely to be offered this type of treatment if you are in your late 70s or in your 80s, as it provides the most benefits for people in this age group. In some cases, a younger person may be offered this treatment if he or she has long-standing persistent atrial fibrillation that is very poorly controlled and that causes lots of symptoms.
You will be given a local anesthetic in your groin. Very thin wires called electrode catheters are then passed into your body through a vein at the top of your leg. They are then gently moved into position in your heart. The ablation technique involves using radiofrequency waves to destroy the AV node. An artificial pacemaker is then implanted immediately afterwards. Or, sometimes the pacemaker is implanted first, and the AV node ablation is performed a few days or weeks later.
This treatment means that you will still have atrial fibrillation, but your heart rate and rhythm will be better controlled by the artificial pacemaker. You will still need to take an anticoagulant medicine, because you will still have AF.
Lifestyle and home remedies
You may need to make lifestyle changes that improve the overall health of your heart, especially to prevent or treat conditions such as high blood pressure and heart disease. Your doctor may suggest several lifestyle changes, including:
- Eat heart-healthy foods. Eat a healthy diet that’s low in salt and solid fats and rich in fruits, vegetables and whole grains.
- Exercise regularly. Exercise daily and increase your physical activity. It’s recommended that adults do at least 150 minutes of moderate-intensity physical activity a week. ‘Moderate-intensity’ means activity that makes your heart beat faster, makes you feel warmer, and makes you breathe faster, although you should still be able to speak in full sentences. You could do the 150 minutes as 30 minutes’ activity a day on five days a week, for example. Or you can break the 30 minutes into three 10-minute sessions. Some people with AF find that they become tired more easily on exertion. However, if you build up your activity gradually, your energy levels will improve and you will gradually be able to do more exercise. If you feel dizzy or light-headed, or if you get palpitations or any other symptoms during physical activity, stop and rest straight away. If you have any concerns about physical activity, discuss it with your doctor.
- Quit smoking. If you smoke and can’t quit on your own, talk to your doctor about strategies or programs to help you break a smoking habit.
- Maintain a healthy weight. Being overweight increases your risk of developing heart disease.
- Keep blood pressure and cholesterol levels under control. Make lifestyle changes and take medications as prescribed to correct high blood pressure (hypertension) or high cholesterol.
- Drink alcohol in moderation. For healthy adults, that means up to one drink a day for women of all ages and men older than age 65, and up to two drinks a day for men age 65 and younger.
- Maintain follow-up care. Take your medications as prescribed and have regular follow-up appointments with your doctor. Tell your doctor if your symptoms worsen.
- Calkins H, Hindricks G, Cappato R, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017;14(10):e275-e444. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6019327
- Camm AJ, et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC) Europace. 2010;12(10):1360–1420.
- Calkins H, et al. 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Heart Rhythm. 2012;9(4):632–696.e21
- Atrial fibrillation. http://www.heart.org/HEARTORG/Conditions/Arrhythmia/AboutArrhythmia/What-is-Atrial-Fibrillation-AFib-or-AF_UCM_423748_Article.jsp
- Eckman MH, Wise RE, Naylor K, et al. Developing an Atrial Fibrillation Guideline Support Tool (AFGuST) for Shared Decision Making. Current medical research and opinion. 2015;31(4):603-614. doi:10.1185/03007995.2015.1019608. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4708062/
- Treatment Guidelines of Atrial Fibrillation (AFib or AF). http://www.heart.org/idc/groups/heart-public/@wcm/@hcm/documents/downloadable/ucm_324032.pdf
- Kirchhof P, Calkins H. Catheter ablation in patients with persistent atrial fibrillation. European Heart Journal. 2017;38(1):20-26. doi:10.1093/eurheartj/ehw260. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5353871/