What is back pain
Back pain or lower back pain also called lumbago, is very common and affects people of all ages. Approximately 80% of individuals will experience an episode of lower back pain at some time during their life. Fortunately however, in most cases — even severe back pain — isn’t caused by anything serious and may not even be identified by the doctor and will usually improve in a few days or sometimes weeks. But in 5% of people lower back pain can continue for a long period and go on to develop a chronic condition.
Lower back pain is the fifth leading reason for patients visiting a doctor and the leading cause of work-related disability.
Back pain usually feels like an ache, tension or stiffness in the back. For some people, back pain is simply an annoyance. For others, it can be excruciating and disabling.
Most people will experience acute lower back pain during their lifetime. The first episode usually occurs between 20 and 40 years of age. For many, acute lower back pain is the first reason to seek medical care as an adult. Lower back pain can be moderate to severe and debilitating, causing anxiety. It disables 5.4 million Americans and costs at least $90 billion in medical and non-medical expenses 1. Many cases are self-limited and resolve with little intervention. However, 31 percent of people with lower back pain will not fully recover within six months 2, although most will improve. Recurrent back pain occurs in 25 to 62 percent of people within one to two years, with up to 33 percent having moderate pain and 15 percent having severe pain 3.
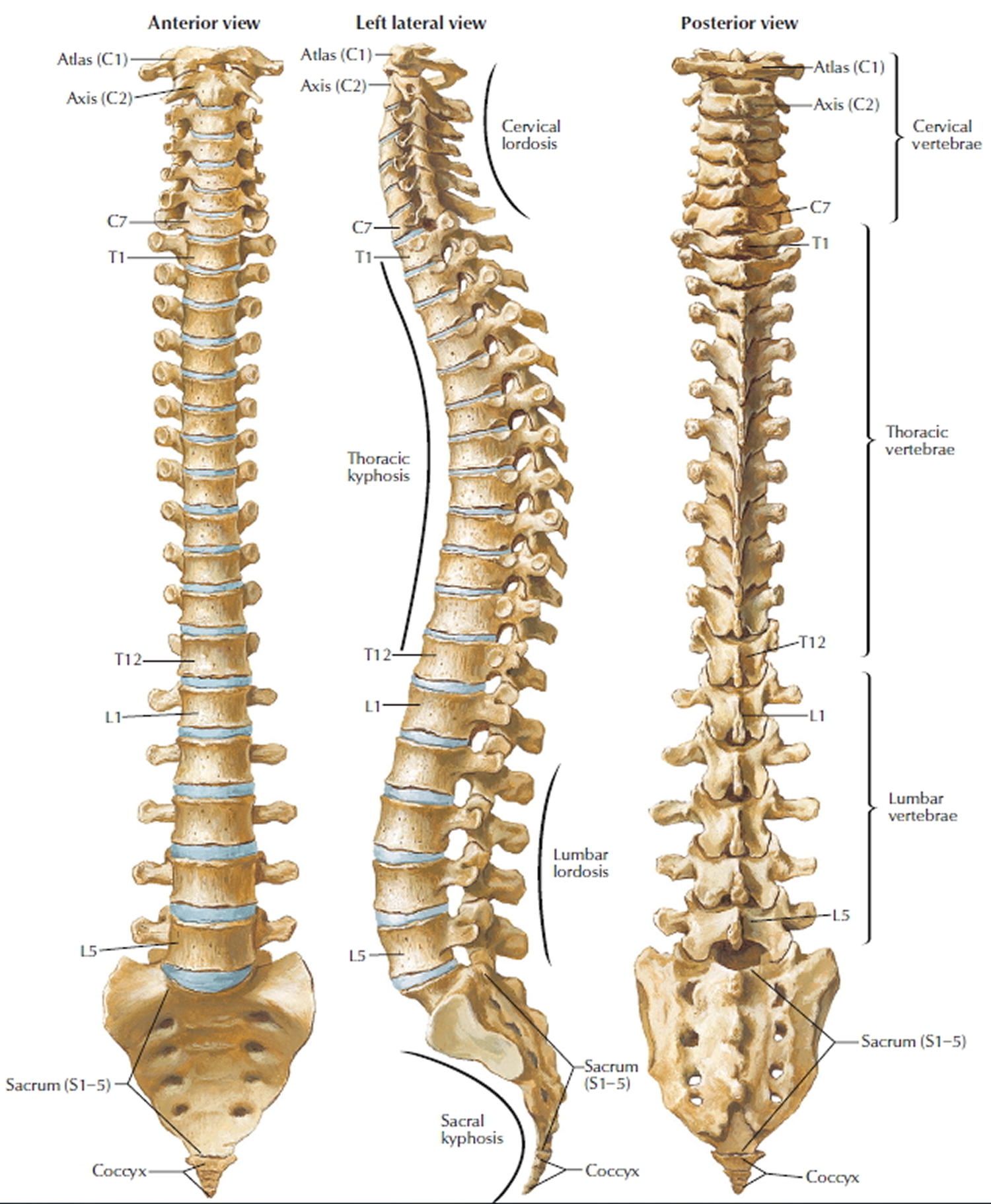
Figure 1. Vertebral column
Adults
Men and women are equally affected by lower back pain but the underlying causes of the pain may differ. For example, women suffer back pain during pregnancy and menstruation or from conditions such as osteoporosis f(bone thinning) or osteoarthritis (joint destruction) which are correspondingly more common in females. Men may be more likely to suffer lower back pain secondary to trauma from sporting or labor-intensive work activities.
The point prevalence of lower back pain in men and women is approximately 5%. The onset of pain is most common between the ages of 20 and 40 years in both men and women.
Children
Lower back pain is not common in children and when present is more likely to represent a serious underlying pathology such as malignancy (cancer) or infection. All lower back pain in children should be considered seriously and medical advice should always be sought if the pain persists longer than a few days.
See your doctor if your back pain hasn’t improved after a week of home treatment or if your back pain:
- Is constant or intense, especially at night or when you lie down
- Spreads down one or both legs, especially if the pain extends below your knee
- Causes weakness, numbness or tingling in one or both legs
- Occurs with unintended weight loss
- Occurs with swelling or redness on your back
If you have any of the following symptoms in addition to your back pain, see your doctor straight away. You may need immediate medical help.
- Fever of 100º F (38º C) or above
- Unexplained weight loss
- Swelling of the back
- Constant back pain that does not ease after lying down
- Pain in your chest or high up in your back
- Pain down your legs and below the knees
- Pain caused by a recent trauma or injury to your back
- Loss of bladder control
- Inability to pass urine
- Loss of bowel control
- Numbness (loss of feeling, or a tingling sensation) around your genitals, buttocks or anal area
- Pain that is worse at night.
There are things you can do to help relieve it. But sometimes the pain can last a long time or keep coming back. Surgery is rarely needed for back pain and is generally considered only as a last resort.
Lower back pain causes
Your spine is a column of bones (vertebrae) held together by muscles, tendons and ligaments and cushioned by shock-absorbing disks. A problem in any part of your spine can cause back pain. A precise cause for the back pain is only identifiable in around 15% of cases.
Most back pain is what’s known as “non-specific” (there’s no obvious cause) or “mechanical” (the pain originates from the joints, bones or soft tissues in and around the spine).
A common cause of back pain is injury to a muscle (strain) or ligament (sprain). Strains and sprains can occur for many reasons, including improper lifting, poor posture and lack of regular exercise. Being overweight may increase your risk of strains and sprains affecting your back.
This type of back pain “non-specific” (there’s no obvious cause):
- tends to get better or worse depending on your position – for example, it may feel better when sitting or lying down
- typically feels worse when moving – but it’s not a good idea to avoid moving your back completely, as this can make things worse
- can develop suddenly or gradually
- might sometimes be the result of poor posture or lifting something awkwardly, but often occurs for no apparent reason
- may be due to a minor injury such as sprain (pulled ligament) or strain (pulled muscle)
- can be associated with feeling stressed or run down
- will usually start to get better within a few weeks
Back pain can also result from more-serious injuries, such as a vertebral fracture or ruptured disk; from arthritis and other age-related changes in your spine; and from certain infections.
There are many causes of low back pain, but they can be grouped roughly as follows:
- Trauma;
- Spinal fractures
- Mechanical:
- Sprains and strains;
- Muscular pain;
- Vertebral dysfunction;
- Prolapsed or herniated disc (slipped disk) – where a disc of cartilage in the spine presses on a nearby nerve. This can cause back pain and numbness, tingling and weakness in other parts of the body;
- Narrowing of bony canals (spinal stenosis);
- Osteoarthritis;
- Fibromyalgia: Generalized aches and pains;
- Incorrect bone positions and articulation;
- Poor posture;
- Pregnancy;
- Obesity;
- Sciatica – irritation of the sciatic nerve that runs from the pelvis to the feet. This can cause pain, numbness, tingling and weakness in the lower back, buttocks, legs and feet;
- Scoliosis;
- Meralgia paresthetica;
- Spondylolisthesis (a bone in the spine slipping out of position) – this can cause lower back pain and stiffness, as well as numbness and a tingling sensation
- Inflammatory;
- Rheumatoid arthritis
- Infective lesions of the spine; Osteomyelitis
- Ankylosing spondylitis/ sacroileitis – this causes pain and stiffness that’s usually worse in the morning and improves with movement;
- Metabolic:
- Osteoporosis, fracture particularly in elderly, post-menopausal women;
- Paget’s disease of bone;
- Neoplastic (tumors/cancer):
- Metastases from tumors of other organs;
- Primary bone tumors;
- Multiple myeloma;
- Vascular: Disruption of the blood supply to the spinal cord (spinal claudication);
- Referred pain: Pain spreads to the back from somewhere else, for example to urinary tract (e.g. kidney infection). More common in elderly men;
- Cauda equina syndrome (where the nerves in the lower back become severely compressed);
- Depression.
Children
Back pain in children is more likely to have a serious cause. The following may be present:
- Developmental disorders: Arthritis of the spine (spondylolysis) or slipping of the vertebral bodies across one another (spondylolisthesis);
- Disc herniation (slipped disc);
- Scheuermann disease: Typically in adolescent males where there is weakening of the vertebral end-plates causing crushing and painless kyphosis (increased curvature of the back producing a ‘hunch’);
- Tumors of the bone or spinal cord;
- Infection of the discs (discitis) or bone (osteomyelitis) mostly in children less than 10 years old;
- Congenital disorders such as scoliosis (lateral curvature of the spine).
Acute lower back pain
Acute lower back pain can be defined as six to 12 weeks of pain between the costal angles and gluteal folds that may radiate down one or both legs (sciatica). Acute low back pain is often nonspecific and therefore cannot be attributed to a definite cause. However, possible causes of acute low back pain (e.g., infection, tumor, osteoporosis, fracture, inflammatory arthritis) need to be considered based on the person’s history and physical examination. Table 1 presents the differential diagnosis of acute low back pain 4.
Table 1. Differential Diagnosis of Acute Low Back Pain
| Diagnosis | Key clinical clues |
|---|---|
| Intrinsic spine | |
| Compression fracture | History of trauma (unless osteoporotic), point tenderness at spine level, pain worsens with flexion, and while pulling up from a supine to sitting position and from a sitting to standing position |
| Herniated nucleus pulposus | Leg pain is greater than back pain and worsens when sitting; pain from L1-L3 nerve roots radiates to hip and/or anterior thigh, pain from L4-S1 nerve roots radiates to below the knee |
| Lumbar strain/sprain | Diffuse back pain with or without buttock pain, pain worsens with movement and improves with rest |
| Spinal stenosis | Leg pain is greater than back pain; pain worsens with standing and walking, and improves with rest or when the spine is flexed; pain may be unilateral (foraminal stenosis) or bilateral (central or bilateral foraminal stenosis) |
| Spondylolisthesis | Leg pain is greater than back pain; pain worsens with standing and walking, and improves with rest or when the spine is flexed; pain may be unilateral or bilateral |
| Spondylolysis | Can cause back pain in adolescents, although it is unclear whether it causes back pain in adults; pain worsens with spine extension and activity |
| Spondylosis (degenerative disk or facet joint arthropathy) | Similar to lumbar strain; disk pain often worsens with flexion activity or sitting, facet pain often worsens with extension activity, standing, or walking |
| Systemic | |
| Connective tissue disease | Multiple joint arthralgias, fever, weight loss, fatigue, spinous process tenderness, other joint tenderness |
| Inflammatory spondyloarthropathy | Intermittent pain at night, morning pain and stiffness, inability to reverse from lumbar lordosis to lumbar flexion |
| Malignancy | Pain worsens in prone position, spinous process tenderness, recent weight loss, fatigue |
| Vertebral diskitis/ osteomyelitis | Constant pain, spinous process tenderness, often no fever, normal complete blood count, elevated erythrocyte sedimentation rate and/ or C-reactive protein level |
| Referred | |
| Abdominal aortic aneurysm | Abdominal discomfort, pulsatile abdominal mass |
| Gastrointestinal conditions: pancreatitis, peptic ulcer disease, cholecystitis | Abdominal discomfort, nausea\vomiting, symptoms often associated with eating |
| Herpes zoster | Unilateral dermatomal pain, often allodynia, vesicular rash |
| Pelvic conditions: endometriosis, pelvic inflammatory disease, prostatitis | Discomfort in lower abdomen, pelvis, or hip |
| Retroperitoneal conditions: renal colic, pyelonephritis | Costovertebral angle pain, abnormal urinalysis results, possible fever |
Medical conditions causing back pain
Pain in the legs, neck and shoulders can also be felt as back pain. However, it may be caused by another condition and you should consider seeing your doctor if you think the following might apply to you:
- pain in the lower back that moves down the buttocks into one or both of the legs may be a symptom of sciatica (caused by pressure on the nerve endings that come out of the spine)
- soreness in the lower back, muscle weakness, tight muscles and loss of bladder control may be the result of a slipped disc
- back pain, buttock pain, swollen joints and tendons and extreme tiredness are common symptoms of ankylosing spondylitis
- lower back pain, stiffness, numbness and tingling can be caused by spondylolisthesis (a bone in the spine slipping out of position)
- pain in the joints (including the back) when walking, and stiffness first thing in the morning are symptoms of arthritis
- painful stiffness of the shoulder, which makes it very difficult to dress, drive or sleep, may be a sign of a frozen shoulder
- neck pain and stiffness, headaches and lower back pain following an accident are common symptoms of whiplash.
The following serious conditions can also cause back pain:
- a broken bone in the spine
- an infection
- cancer.
Most cases of back pain, however, are not caused by disease or serious damage but by sprains, minor strains, minor injuries or a pinched or irritated nerve.
Table 2. Red Flags for Serious Causes of Acute Low Back Pain
| Possible cause | History findings | Physical examination findings |
|---|---|---|
| Cancer | Strong: Cancer metastatic to bone Intermediate: Unexplained weight loss | Weak: Vertebral tenderness, limited spine range of motion |
| Weak: Cancer, pain increased or unrelieved by rest | ||
| Cauda equina syndrome | Strong: Bladder or bowel incontinence, urinary retention, progressive motor or sensory loss | Strong: Major motor weakness or sensory deficit, loss of anal sphincter tone, saddle anesthesia |
| Weak: Limited spine range of motion | ||
| Fracture | Strong: Significant trauma related to age* | Weak: Vertebral tenderness, limited spine range of motion |
| Intermediate: Prolonged use of steroids | ||
| Weak: Age older than 70 years, history of osteoporosis | ||
| Infection | Strong: Severe pain and lumbar spine surgery within the past year | Strong: Fever, urinary tract infection, wound in spine region |
| Intermediate: Intravenous drug use, immunosuppression, severe pain and distant lumbar spine surgery | Weak: Vertebral tenderness, limited spine range of motion | |
| Weak: Pain increased or unrelieved by rest |
Footnote: Presence of one or two weak or intermediate red flags may warrant observation because few patients will be significantly harmed if diagnosis of a serious cause is delayed for four to six weeks. Presence of any strong red flag warrants more urgent workup and probable referral to a spine subspecialist.
*—Fall from a height or motor vehicle crash in a young patient, minor fall or heavy lifting in a patient with osteoporosis or possible osteoporosis.
Back pain triggers
Back pain can be brought on, or ‘triggered’, by everyday activities either at home or at work. Pain can also develop over time as a result of sitting, standing or lifting badly. Common triggers that can cause back pain include:
- bending awkwardly
- lifting, carrying, pushing or pulling incorrectly
- slouching in chairs
- standing or bending down for long periods
- twisting
- overstretching
- driving in a hunched position
- driving for long periods without taking a break
- overuse of the muscles, usually due to sport or repetitive movements (repetitive strain injury).
Sometimes the pain develops suddenly and for no apparent reason. A person can wake up with back pain and have no idea what has caused it.
Risk factors for lower back pain
Some conditions increase the risk that someone will develop back pain. These include:
- being overweight – the extra weight puts pressure on the spine. Use the healthy weight body mass index BMI calculator to find out if you need to lose weight
- smoking – this could be due to damage to tissue in the back caused by smoking, or because smokers tend to have unhealthier lifestyles than non-smokers – get help quitting here
- being pregnant – carrying a baby means extra weight, which can place additional strain on the back
- long-term use of medicines that are known to weaken the bones, such as corticosteroids
- stress – it is thought that stress can cause tension in the muscles of the back, which can cause back pain
- depression – back pain can make people feel depressed, which can sometimes result in weight gain leading to more severe pain and a cycle of worsening depression.
Back pain prevention
To avoid back pain, you must reduce excess stresses and strains on your back and ensure your back is strong and supple.
If you have recurring bouts of back pain, consider:
- do regular back exercises and stretches – your doctor or a physiotherapist may be able to advise you about exercises to try
- stay active – doing regular exercise can help keep your back strong; adults are advised to do 150 minutes of exercise a week
- avoid sitting for too long when driving or at work
- take care when lifting – read some safe lifting tips
- check your posture when sitting, using computers and watching television – find out how to sit correctly and tips for laptop users
- ensure the mattress on your bed supports you properly
- losing any excess weight – lose weight through a combination of a healthy diet and regular exercise if you’re overweight – being overweight can increase your risk of developing back pain. You can use the body mass index BMI calculator to find out whether you are a healthy weight for your height
- wearing flat shoes with cushioned soles – these can reduce the stress on your back
- avoiding sudden movements or muscle strain
- trying to reduce any stress, anxiety and tension.
Posture
How you sit, stand and lie down can have an important effect on your back. The following tips should help you maintain a good posture.
Standing
Stand upright, with your head facing forward and your back straight. Balance your weight evenly on both feet and keep your legs straight.
Sitting
You should be able sit upright with support in the small of your back. Your knees and hips should be level and your feet should be flat on the floor (use a footstool if necessary). Some people find it useful to use a small cushion or rolled-up towel to support the small of the back.
If you use a keyboard, make sure that your forearms are horizontal and your elbows are at right angles.
Driving
Make sure that your lower back is properly supported. Correctly positioning your wing mirrors will prevent you from having to twist around. Foot controls should be squarely in front of your feet. If driving long distances, take regular breaks so that you can stretch your legs.
Sleeping
Your mattress should be firm enough to support your body while supporting the weight of your shoulders and buttocks, keeping your spine straight. If your mattress is too soft, place a firm board – ideally 2cm thick – on top of the base of your bed and under the mattress. Support your head with a pillow, but make sure that your neck is not forced up at a steep angle.
Exercise
Exercise is both an excellent way to prevent back pain and to reduce any back pain you might have. However, if you have chronic back pain (back pain that has lasted for more than 3 months), consult your doctor or physiotherapist before starting any exercise program.
Exercises such as walking or swimming strengthen the muscles that support your back without putting any strain on it or subjecting it to a sudden jolt.
Activities such as yoga or pilates can improve the flexibility and the strength of your back muscles. It is important that you carry out these activities under the guidance of a properly qualified instructor.
Many people injure their back when doing everyday chores at home or work, such as lifting, gardening or using a vacuum cleaner. ‘Warming up’ your back with some gentle stretching before you start these chores can help to prevent injury.
Lifting and handling
One of the biggest causes of back injury, especially at work, is lifting or handling objects incorrectly. Learning and following the correct method for lifting and handling objects can help to prevent back pain.
- Think before you lift – can you manage the lift? Are there any handling aids you can use? Where is the load going?
- Start in a good position – your feet should be apart, with one leg slightly forward to maintain balance. When lifting, let your legs take the strain – bend your back, knees and hips slightly, but do not stoop or squat. Tighten your stomach muscles to pull your pelvis in. Do not straighten your legs before lifting as you may strain your back on the way up.
- Keep the load close to your waist for as long as possible, with the heaviest end nearest to you.
- Avoid twisting your back or leaning sideways, especially when your back is bent. Your shoulders should be level and should face in the same direction as your hips. Turning by moving your feet is better than lifting and twisting at the same time.
- Keep your head up – once you have the load secure, look ahead, not down at the load.
- Know your limits – there is a big difference between what you can lift and what you can safely lift. If in doubt, get help.
- Push rather than pull – if you have to move a heavy object across the floor, it is better to push it rather than pull it.
- Distribute the weight evenly – if you are carrying shopping bags or luggage, try to distribute the weight evenly on both sides of your body.
Back pain diagnosis
At your first appointment, the doctor will discuss your symptoms with you and examine your back. An accurate history and physical examination are essential for evaluating acute low back pain.
Often, patients awaken with morning pain or develop pain after minor forward bending, twisting, or lifting. It is also important to note whether it is a first episode or a recurrent episode. Recurrent episodes usually are more painful with increased symptoms. Red flags are often used to distinguish a common, benign episode from a more significant problem that requires urgent workup and treatment (see Table 2 above). A recent study shows that some red flags are more important than others, and that red flags overall are poor at ruling in more serious causes of low back pain. Patients with back pain in the primary care setting (80 percent) tend to have one or more red flags, but rarely have a serious condition. There are certain signs and symptoms of more serious causes of lower back pain such as cauda equina syndrome, major intra-abdominal pathology, infections, malignancy, and fractures (Tables 1 and 2). Cauda equina syndrome and infections require immediate referral.
They will usually assess your ability to sit, stand, walk and lift your legs as well as test the range of movement in your back. To help them diagnose the cause of the pain, they may ask questions about any illnesses or injuries you may have had, your lifestyle and your work. Your back is a complex structure, so finding the exact cause can often be difficult.
Below are some of the questions your doctor may ask. It might be helpful to consider these before your appointment:
- When did the back pain start?
- Where are you feeling pain?
- Is your pain worse at night?
- Constant back pain that does not ease after lying down?
- Numbness (loss of feeling, or a tingling sensation) around your genitals, buttocks or anal area?
- Have you had any back problems before?
- Can you describe the pain?
- What makes the pain better or worse?
- Do you have any weakness or numbness?
- Loss of bowel or bladder function?
- Inability to pass urine
- Do you use illicit drugs (intravenous drug use)?
- Severe pain?
- Do you have fever?
- Do you have unexplained weight loss?
They will first want to make sure your pain is not being caused by a more serious condition. They will ask questions to rule out cancer, a fracture or an infection, although these conditions are uncommon.
If your doctor thinks there may be a more serious cause you will be referred for further tests.
Without signs and symptoms indicating a serious underlying condition, imaging (x-ray or an MRI scan) won’t help the diagnosis of your back pain and does not improve clinical outcomes in these patients 5.
Even with a few weaker red flags, four to six weeks of treatment is appropriate before consideration of imaging studies 6. If a serious condition is suspected, magnetic resonance imaging (MRI) is usually most appropriate. Computed tomography is an alternative if MRI is contraindicated or unavailable 6. Clinical correlation of MRI or computed tomography findings is essential because the likelihood of false-positive results increases with age 7. Radiography may be helpful to screen for serious conditions, but usually has little diagnostic value because of its low sensitivity and specificity.
Laboratory tests such as complete blood count with differential, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level may be beneficial if infection or bone marrow neoplasm is suspected. These tests may be most sensitive in cases of spinal infection because lack of fever and a normal complete blood count are common in patients with spinal infection 8. Because laboratory testing lacks specificity, MRI with and without contrast media and, in many cases, biopsy are essential for accurate diagnosis 8.
Lower back pain treatment
The goals of treatment for acute low back pain are to relieve pain, improve function, reduce time away from work, and develop coping strategies through education. Many treatments are available for acute low back pain, but strong evidence for their benefit is lacking.
Most cases of back pain don’t require medical attention and can be treated with over-the-counter pain relief medication and self-care.
Most people prefer to take paracetamol (acetaminophen) or anti-inflammatory drugs such as ibuprofen, although research shows these have only a small effect. A stronger pain relief medicine, such as codeine (an opioid), is an option and is sometimes taken as well as paracetamol (acetaminophen).
Optimizing treatment may minimize the development of chronic pain, which accounts for most of the health care costs related to low back pain 9. Based on the evidence, a reasonable approach to treatment is described in Table 3.
Table 3. Approach to the Treatment of Nonspecific Acute Low Back Pain
| First visit | |
| Patient education | |
| Reassure the patient that the prognosis is often good, with most cases resolving with little intervention | |
| Advise the patient to stay active, avoiding bed rest as much as possible, and to return to normal activities as soon as possible | |
| Advise the patient to avoid twisting and bending | |
| Initiate trial of a nonsteroidal anti-inflammatory drug (NSAID) or acetaminophen | |
| Consider a muscle relaxant based on pain severity | |
| Consider a short course of opioid therapy if pain is severe | |
| Consider referral for physical therapy (McKenzie method and/or spine stabilization) if it is not the first episode | |
| Second visit* | |
| Consider changing to a different nonsteroidal anti-inflammatory drug (NSAID) | |
| Consider referral for physical therapy (McKenzie method and/or spine stabilization) if not done at initial visit | |
| Consider referral to a spine subspecialist if pain is severe or limits function | |
Footnote: *—Two to four weeks after the initial visit, if the patient has not significantly improved. McKenzie method see Youtbe video below
Lower back pain relief
Recommended
Nonsteroidal anti-inflammatory drugs (NSAIDs) are often first-line therapy for low back pain. Low-quality evidence suggests that they are effective for short-term symptom relief, compared with placebo 10. No patient characteristics at baseline can predict the success of NSAID therapy 11. Moderate evidence suggests that no one NSAID is superior, and switching to a different NSAID may be considered if the first is ineffective. Whether NSAIDs are more effective than acetaminophen is unknown, but the addition of an NSAID to acetaminophen therapy is no more beneficial than acetaminophen alone 10.
Moderate-quality evidence shows that non-benzodiazepine muscle relaxants (e.g., cyclobenzaprine [Flexeril], tizanidine [Zanaflex], metaxalone [Skelaxin]) are beneficial in the treatment of acute low back pain. Most pain reduction from these medications occurs in the first seven to 14 days, but the benefit may continue for up to four weeks 12. However, nonbenzodiazepine muscle relaxants do not affect disability status 13. Very low-quality evidence shows that a short course (up to five days) of oral diazepam (Valium) may also be beneficial for pain relief 13. Because all muscle relaxants have adverse effects, such as drowsiness, dizziness, and nausea, they should be used cautiously. Diazepam and carisoprodol (Soma) use should be brief to decrease the risk of abuse and dependence. There is also moderate-quality evidence that muscle relaxants combined with NSAIDs may have additive benefit for reducing pain 13.
Opioids are commonly prescribed for patients with severe acute low back pain; however, there is little evidence of benefit. Three studies showed no difference in pain relief or time to return to work between oral opioids and NSAIDs or acetaminophen, and there is risk of harmful dose escalation over time with opioids, especially with purer formulations 14. Although epidural steroid injections are not beneficial for isolated acute low back pain, they may be helpful for radicular pain that does not respond to two to six weeks of noninvasive treatment. Transforaminal injections appear to have more favorable short- and long-term benefit than traditional interlaminar injections 15.
Patient Education. Patient education involves a discussion of the often benign nature of acute back pain and reassurance that most patients need little intervention for significant improvement. Patients should be advised to stay as active as possible, within pain limits; to avoid twisting and bending, particularly when lifting; and to return to normal activities as soon as possible. The goal is to reduce worry about back pain and to teach ways to avoid worsening of pain or pain recurrence.
High-quality evidence shows that individual patient education of greater than two hours is more effective than no education or less-intense education for pain that persists for four weeks or more 16. Moderate-quality evidence shows that less-intense individual education and advice to stay active have small benefits and are at least as effective as other back pain interventions 17. It is unclear whether patient education and advice for patients with acute low back pain are cost-effective 18.
Acceptable
Physical Therapy. Physical therapists often recommend the McKenzie method or spine stabilization exercises for the treatment of low back pain. The McKenzie method is described in a Youtube video below. The McKenzie method has been shown to be slightly more effective than other common low back pain treatments; however, the difference is not clinically significant 19 and evidence on its effect on disability is conflicting 20. There also do not appear to be good long-term benefits with the McKenzie method, other than decreased need for health care services 19. Spine stabilization exercises have been shown to decrease pain, disability, and risk of recurrence after a first episode of back pain 21.
According to moderate-quality evidence, physical therapist–directed home exercise programs for acute back pain can reduce the rate of recurrence, increase the time between episodes of back pain, and decrease the need for health care services. Therefore, most of these exercise programs are cost-effective treatments for acute low back pain 22, 23.
Application of Ice or Heat. Low-quality evidence shows that in the first five days of acute low back pain, the use of heat treatments may be more effective for reducing pain and disability than nonheat wraps, NSAIDs, or acetaminophen, but shows no difference between heat application and McKenzie therapy at seven days 24. A low-quality study found that heat therapy in conjunction with education or NSAIDs is more effective than education or NSAIDs alone at 14 days 25. Ice and heat therapy have similar analgesic effects 24.
How to relieve back pain
The following tips may help reduce your backache and speed up your recovery:
- stay as active as possible and try to continue your daily activities – this is one of the most important things you can do, as resting for long periods is likely to make the pain worse
- try exercises and stretches for back pain; other activities such as walking, swimming, yoga and pilates may also be helpful
- take anti-inflammatory painkillers, such as ibuprofen – remember to check the medicine is safe for you to take first and ask a pharmacist if you’re not sure
- use hot or cold compression packs for short-term relief – you can buy these from your local pharmacy, or a hot water bottle and a bag of frozen vegetables wrapped in a cloth will work just as well
Although it can be difficult, it helps if you stay optimistic and recognize that your pain should get better, as people who manage to stay positive despite their pain tend to recover quicker.
Stay active
One of the most important things you can do is to keep moving and continue with your normal activities as much as possible.
It used to be thought that bed rest would help you recover from a bad back, but it’s now known that people who remain active are likely to recover more quickly.
This may be difficult at first, but don’t be discouraged – your pain will start to improve eventually. Consider taking painkillers if the pain is stopping you from carrying on as normal.
There’s no need to wait until you’re completely pain-free before returning to work. Going back to work will help you return to a normal pattern of activity and may distract you from the pain.
Exercises for lower back pain
Exercise is commonly advised as one of the best ways to help prevent and man age most back pain. The type of exercise you do does not matter as long as you do something and remain active. Some people find that swimming helps them, others swear by yoga, while many people enjoy walking or running. The choice of exercise is yours because if you enjoy what you are doing, you will be more likely to continue and see the benefits.
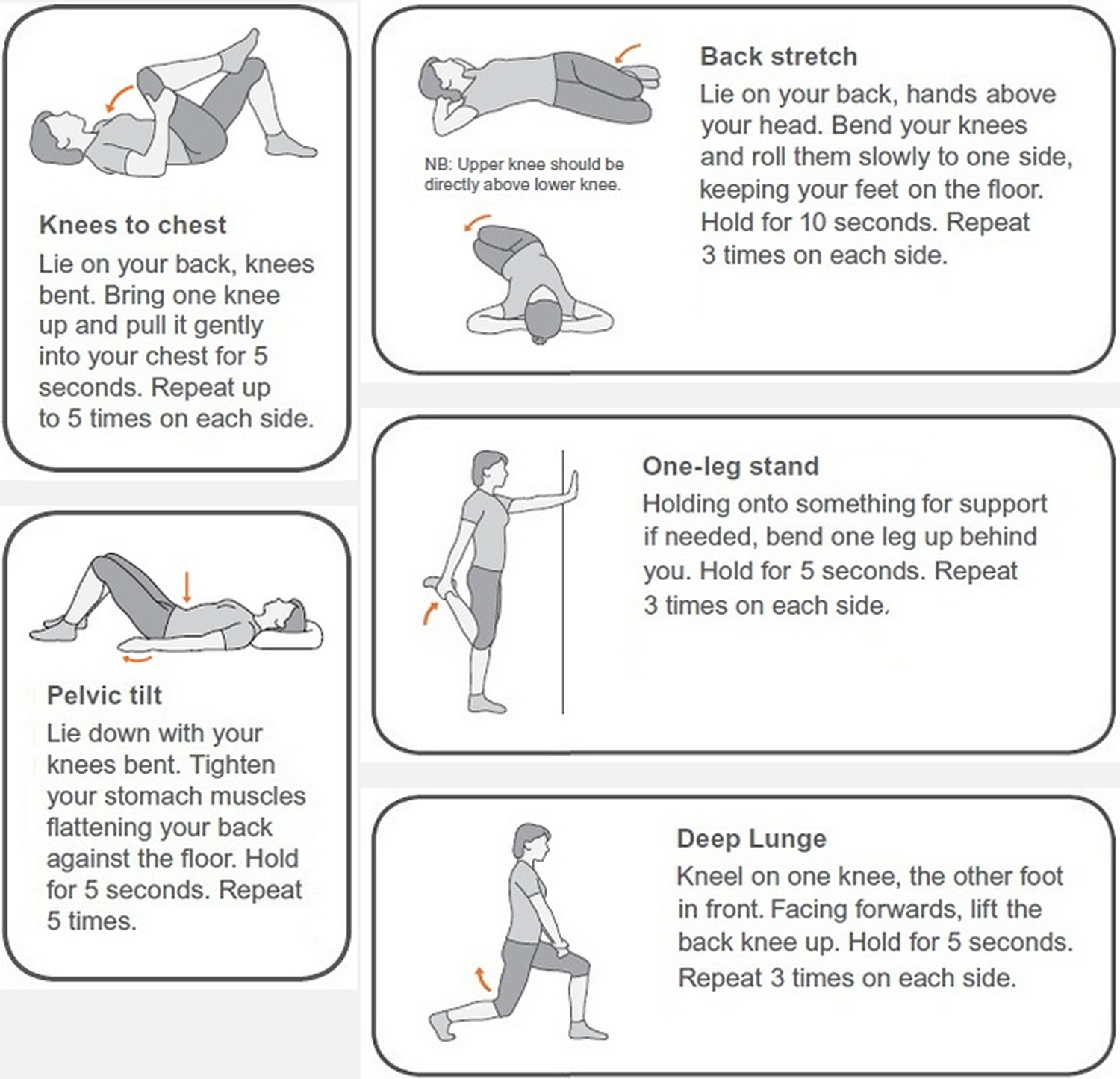
There are some simple back exercises and stretches you can do at home to help ease lower back pain and improve your strength and flexibility.
Common exercises beneficial for back pain:
- Swimming – the water environment takes the strain off joints and muscles while working out the entire body
- Yoga – strengthens core and back muscles and increases flexibility
- Pilates – strengthens muscles and the spinal column and promotes good posture
- Exercise programmes – provide a cardiovascular work out and all over body conditioning which includes the back and core muscles
There are many other exercises that you could do which would be helpful. Although structured exercises are extremely beneficial, there are also some exercises you can do on your own at home without specialist equipment that can help to strengthen your back and prevent and ease back pain. If you find that any of the exercises exacerbates your back pain, try another one or seek advice from your doctor or health professional. You should, however, expect some minor discomfort after starting an exercise programme, since your body may not be used to exercise.
Figure 2. Exercises for lower back pain
Aim to do these exercises every day, along with other activities like walking, swimming or yoga.
Your pain should start to ease within 2 weeks and will usually pass in about 4 to 6 weeks.
See a doctor if:
- your pain doesn’t improve within a few weeks
- you experience severe pain while trying any of these exercises
Stretches for lower back pain
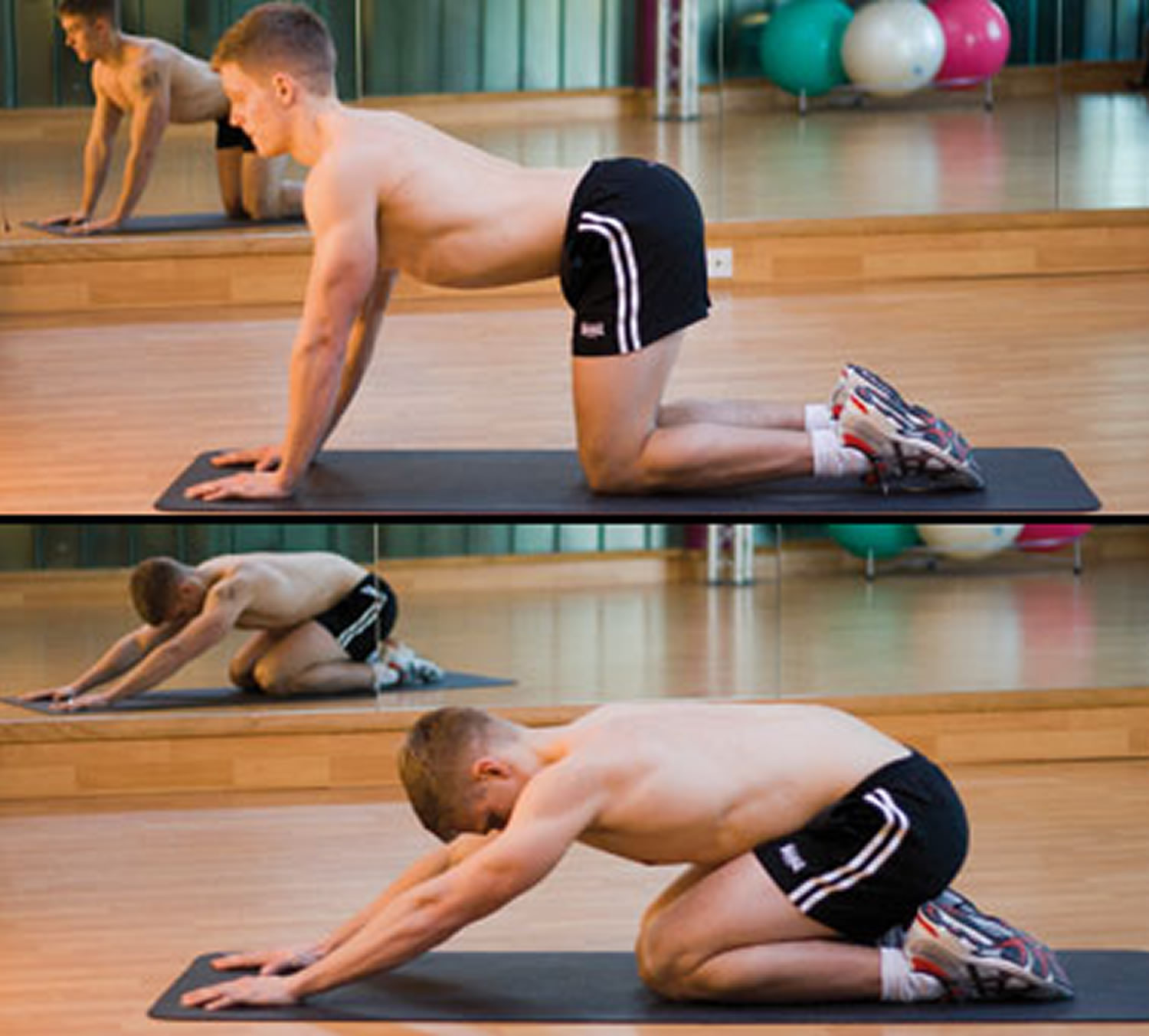
Bottom to heels stretch
Start position: Kneel on all fours, with your knees under your hips and hands under your shoulders. Try to keep your back and neck fairly straight, and don’t lock your elbows.
Action: Slowly move your bottom back towards your heels. Hold the stretch for one deep breath and return to the starting position.
Repeat 8 to 10 times.
Tips:
- avoid going right back onto your heels if you have a knee problem
- ensure correct positioning with the help of a mirror
- only stretch as far as feels comfortable
Figure 3. Bottom to heels stretch
Knee rolls
Start position: Lie on your back. Place a small flat cushion or book under your head. Keep your knees bent and together. Keep your upper body relaxed and your chin gently tucked in.
Action: Roll your knees to one side, keeping both shoulders on the floor. Hold the stretch for one deep breath and return to the starting position.
Repeat 8 to 10 times, alternating sides.
Tips:
- only move as far as feels comfortable
- place a pillow between your knees for comfort
Figure 4. Knee rolls exercise
Back extensions
Start position: Lie on your front and rest on your forearms, with your elbows bent at your sides. Look towards the floor and keep your neck straight.
Action: Keeping your neck straight, arch your back up by pushing down on your hands. You should feel a gentle stretch in the stomach muscles. Breathe and hold for 5 to 10 seconds. Return to the starting position.
Repeat 8 to 10 times.
Tips:
- don’t bend your neck backwards
- keep your hips on the floor
Figure 5. Back extensions
Deep abdominal strengthening
Start position: Lie on your back. Place a small, flat cushion or book under your head. Bend your knees, keeping your feet straight and hip-width apart. Keep your upper body relaxed and your chin gently tucked in.
Action: As you breathe out, gently tense the muscles in your pelvis and lower tummy so they’re pulled up towards your chest. Hold for 5 to 10 breaths and relax.
Repeat 5 times.
Tips:
- this is a slow, gentle exercise – don’t try to tense your muscles too quickly or too hard
- make sure you don’t tense up through the neck, shoulders or legs
Figure 6. Deep abdominal strengthening exercise
Pelvic tilts
Start position: Lie on your back. Place a small, flat cushion or book under your head. Bend your knees, keeping your feet straight and hip-width apart. Keep your upper body relaxed and your chin gently tucked in.
Action: Gently flatten your lower back into the floor and tense your stomach muscles. Now tilt your pelvis towards your heels until you feel a gentle arch in your lower back and return to the starting position.
Repeat 10 to 15 times, tilting your pelvis back and forth in a slow rocking motion.
Tips:
- don’t press down through your neck, shoulders or feet
- place one hand on your stomach and the other under your lower back – if you’re doing the exercise correctly, you should feel the muscles working in these areas
Figure 7. Pelvic tilts exercise
Back pain pilates workout
A pilates-inspired exercise video suitable for people with chronic back pain.
This 29-minute class focuses on improving posture and improving the strength and flexibility of the muscles that support the back.
Regular pilates practice can help improve posture, muscle tone, balance and joint mobility, as well as relieve stress and tension.
UNSUPPORTED
Oral Steroids. A short course of oral corticosteroids has questionable benefit for patients with acute radicular leg pain 26. However, there are no studies to support the use of oral steroids for isolated acute low back pain.
Acupuncture. Several low-quality trials show that acupuncture has minimal or no benefit over sham treatment, naproxen (Naprosyn), or the Chinese herbal therapy moxibustion 27. Although evidence to support its effectiveness is limited, acupuncture may be cost-effective in patients with pain lasting longer than four weeks 18.
Exercise. Aerobic conditioning, strengthening exercises, flexibility exercises, or a combination of these exercises is no more effective than other treatments in patients with acute low back pain 28.
Lumbar Support. It is unclear whether lumbar support is more effective than no intervention or other treatments for acute low back pain 29.
Massage. There is insufficient evidence to recommend for or against massage therapy for acute low back pain 30. It is unlikely to be cost-effective 18.
Spinal Manipulation and Chiropractic Techniques. Low-quality evidence shows that spinal manipulation may be more effective than sham treatments in the short-term reduction of pain (less than six weeks), but no more effective in reducing disability 31. There is little evidence that manipulation is cost-effective for treating acute low back pain 18.
Although chiropractic techniques are considered safe if performed by a well-trained chiropractor, a systematic review found that these techniques (e.g., manipulation, temperature modalities, exercises, mechanical devices, patient education) provide no clinically relevant improvement in pain or disability compared with other treatments 32.
Traction. High-quality trials show no evidence of benefit with traction, as a single treatment or in combination with other treatments, in patients with acute or chronic back pain 33. There are no studies on acute low back pain alone.
INADVISABLE
Bed Rest. Bed rest should not be recommended for patients with nonspecific acute low back pain. Moderate-quality evidence suggests that bed rest is less effective at reducing pain and improving function at three to 12 weeks than advice to stay active 34. Prolonged bed rest can also cause adverse effects such as joint stiffness, muscle wasting, loss of bone mineral density, pressure ulcers, and venous thromboembolism 35.
Back pain home remedies
If you have back pain, there are several ways you can manage the condition yourself. They include the following:
Keep moving
- Avoid prolonged bed rest – people who remain active are likely to recover more quickly.
- Try to move around as soon as you are able and aim to do a little more each day. Activity can range from walking around the house to walking to the shops.
- You will have to accept some discomfort but avoid anything that causes a lot of pain.
- Gradual, gentle stretching exercises should be done before any activity.
- Avoid heavy lifting and movements such as punching or pulling. You should also avoid repetitive bending and twisting.
Hot and cold treatments
- Heat – for example a hot bath, heat wraps or a hot water bottle placed on the affected area – can help ease the pain.
- Cold – such as an ice pack or a bag of frozen peas applied to the painful area – can also be effective. Don’t put the ice directly on your skin since it might cause a cold burn. Wrap the frozen pack in a wet cloth before applying it to the affected area.
- Another option is to alternate between hot and cold using ice packs and hot compression packs. Hot compression packs can be bought at most larger pharmacies.
If you are experiencing any numbness, however, do not apply any heat or cold – including heat or ice packs – to the area.
Sleeping position
By changing your sleeping position, you can take some of the strain off your back and ease the pain:
- If you sleep on your side, draw your legs up slightly towards your chest and put a pillow between your legs.
- If you sleep on your back, placing a pillow under your knees will help maintain the normal curve of your lower back.
Relaxation
Trying to relax is a crucial part of easing back pain since muscle tension caused by worrying about your condition can make things worse. Research suggests that people who manage to stay positive despite the pain tend to recover faster and avoid long-term back pain.
At work
- If your job involves sitting down for long periods, try using a chair with lumbar support. You can make your own lumbar support using a rolled up towel or pillow which should be placed in the small (curve) of the lower back.
- Your seat should not press on the back of your thighs or knees.
- Avoid wearing high-heeled shoes if standing for long periods of time. When standing, rest one foot on a small box or stool from time to time.
- Avoid bending over continuously when working.
- If performing repetitive tasks, take frequent short breaks to stretch or relax, even if it’s only for 30 seconds every 10-15 minutes.
When to see a doctor
In some cases, it is better for you to see a doctor for advice and help:
- If you are in pain, get advice on medicines you can take.
- If your back pain lasts for more than 6 weeks, you should make an appointment to see your doctor.
- You should also see your doctor if you develop numbness or pain in the buttocks, leg or foot.
- See your doctor urgently or go to the emergency department if you lose control of your bladder or bowels.
- Back Pain. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Living-Well-with-Rheumatic-Disease/Back-Pain
- Carey TS, Garrett J, Jackman A, McLaughlin C, Fryer J, Smucker DR. The outcomes and costs of care for acute low back pain among patients seen by primary care practitioners, chiropractors, and orthopedic surgeons. The North Carolina Back Pain Project. N Engl J Med. 1995;333(14):913–917.
- Stanton TR, Henschke N, Maher CG, Refshauge KM, Latimer J, McAuley JH. After an episode of acute low back pain, recurrence is unpredictable and not as common as previously thought. Spine (Phila Pa 1976). 2008;33(26):2923–2928.
- Diagnosis and Treatment of Acute Low Back Pain. Am Fam Physician. 2012 Feb 15;85(4):343-350. https://www.aafp.org/afp/2012/0215/p343.html
- Henschke N, Maher CG, Refshauge KM, et al. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum. 2009;60(10):3072–3080.
- https://www.acr.org/
- Cheung KM, Karppinen J, Chan D, et al. Prevalence and pattern of lumbar magnetic resonance imaging changes in a population study of one thousand forty-three individuals. Spine (Phila Pa 1976). 2009;34(9):934–940.
- Acosta FL Jr, Galvez LF, Aryan HE, Ames CP. Recent advances: infections of the spine. Curr Infect Dis Rep. 2006;8(5):390–393.
- Becker A, Held H, Redaelli M, et al. Low back pain in primary care: costs of care and prediction of future health care utilization. Spine (Phila Pa 1976). 2010;35(18):1714–1720.
- Roelofs PD, Deyo RA, Koes BW, Scholten RJ, van Tul-der MW. Non-steroidal anti-inflammatory drugs for low back pain. Cochrane Database Syst Rev. 2008;(1):CD000396.
- Hancock MJ, Maher CG, Latimer J, McLachlan AJ, Day RO, Davies RA. Can predictors of response to NSAIDs be identified in patients with acute low back pain? Clin J Pain. 2009;25(8):659–665.
- Hoiriis KT, Pfleger B, McDuffie FC, et al. A randomized clinical trial comparing chiropractic adjustments to muscle relaxants for subacute low back pain. J Manipulative Physiol Ther. 2004;27(6):388–398
- van Tulder MW, Touray T, Furlan AD, Solway S, Bouter LM. Muscle relaxants for non-specific low back pain. Cochrane Database Syst Rev. 2003;(2):CD004252.
- Cifuentes M, Webster B, Genevay S, Pransky G. The course of opioid prescribing for a new episode of disabling low back pain: opioid features and dose escalation. Pain. 2010;151(1):22–29.
- Roberts ST, Willick SE, Rho ME, Rittenberg JD. Efficacy of lumbosacral transforaminal epidural steroid injections: a systematic review. PM R. 2009;1(7):657–668.
- Engers A, Jellema P, Wensing M, van der Windt DA, Grol R, van Tulder MW. Individual patient education for low back pain. Cochrane Database Syst Rev. 2008;(1):CD004057.
- Dahm KT, Brurberg KG, Jamtvedt G, Hagen KB. Advice to rest in bed versus advice to stay active for acute low-back pain and sciatica. Cochrane Database Syst Rev. 2010;(6):CD007612.
- Lin CW, Haas M, Maher CG, Machado LA, van Tulder MW. Cost-effectiveness of guideline-endorsed treatments for low back pain: a systematic review. Eur Spine J. 2011;20(7):1024–1038.
- Machado LA, Maher CG, Herbert RD, Clare H, McAuley JH. The effectiveness of the McKenzie method in addition to first-line care for acute low back pain: a randomized controlled trial. BMC Med. 2010;8:10.
- Machado LA, de Souza MS, Ferreira PH, Ferreira ML. The McKenzie method for low back pain: a systematic review of the literature with a meta-analysis approach. Spine (Phila Pa 1976). 2006;31(9):E254–E262.
- Hides JA, Jull GA, Richardson CA. Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine (Phila Pa 1976). 2001;26(11):E243–E248.
- Choi BK, Verbeek JH, Tam WW, Jiang JY. Exercises for prevention of recurrences of low-back pain. Cochrane Database Syst Rev. 2010;(1):CD006555.
- Fritz JM, Cleland JA, Speckman M, Brennan GP, Hunter SJ. Physical therapy for acute low back pain: associations with subsequent healthcare costs. Spine (Phila Pa 1976). 2008;33(16):1800–1805.
- French SD, Cameron M, Walker BF, Reggars JW, Ester-man AJ. Superficial heat or cold for low back pain. Cochrane Database Syst Rev. 2006;(1):CD004750.
- Tao XG, Bernacki EJ. A randomized clinical trial of continuous low-level heat therapy for acute muscular low back pain in the workplace. J Occup Environ Med. 2005;47(12):1298–1306.
- Holve RL, Barkan H. Oral steroids in initial treatment of acute sciatica. J Am Board Fam Med. 2008;21(5):469–474.
- Kennedy S, Baxter GD, Kerr DP, Bradbury I, Park J, McDonough SM. Acupuncture for acute non-specific low back pain: a pilot randomised non-penetrating sham controlled trial. Complement Ther Med. 2008;16(3):139–146.
- Lau PM, Chow DH, Pope MH. Early physiotherapy intervention in an accident and emergency department reduces pain and improves satisfaction for patients with acute low back pain: a randomised trial. Aust J Physiother. 2008;54(4):243–249.
- van Duijvenbode IC, Jellema P, van Poppel MN, van Tulder MW. Lumbar supports for prevention and treatment of low back pain. Cochrane Database Syst Rev. 2008;(2):CD001823.
- Furlan AD, Imamura M, Dryden T, Irvin E. Massage for low back pain: an updated systematic review within the framework of the Cochrane Back Review Group. Spine (Phila Pa 1976). 2009;34(16):1669–1684.
- Hancock MJ, Maher CG, Latimer J, et al. Assessment of diclofenac or spinal manipulative therapy, or both, in addition to recommended first-line treatment for acute low back pain: a randomised controlled trial. Lancet. 2007;370(9599):1638–1643.
- Walker BF, French SD, Grant W, Green S. A Cochrane review of combined chiropractic interventions for low-back pain. Spine (Phila Pa 1976). 2011;36(3):230–242.
- Clarke JA, van Tulder MW, Blomberg SE, et al. Traction for low-back pain with or without sciatica. Cochrane Database Syst Rev. 2007;(2):CD003010.
- Hagen KB, Hilde G, Jamtvedt G, Winnem M. Bed rest for acute low-back pain and sciatica. Cochrane Database Syst Rev. 2004;(4):CD001254.
- Casazza BA, Young JL, Herring SA. The role of exercise in the prevention and management of acute low back pain. Occup Med. 1998;13(1):47–60.