What are benzodiazepines?
Benzodiazepines are drugs that belong to the group of medicines called central nervous system (CNS) depressants or sedatives, which are medicines that slows down messages traveling between your brain and your body. Other central nervous system (CNS) depressants include alcohol, cannabis and heroin. The central nervous system (brain and spinal cord) effects of benzodiazepines are believed to be mediated by activation of gamma aminobutyric acid (GABA) A receptors and modulation of their inhibition of neurotransmission 1. Because benzodiazepines are controlled substances with abuse potential, they are available only with your doctor’s prescription with special attention directed toward the patient’s addiction history before these agents are prescribed.
Benzodiazepines are also minor tranquilizers, usually prescribed by doctors to relieve stress and anxiety and to help people sleep. Benzodiazepines can also be used to treat alcohol withdrawal symptoms and epilepsy. However, medical professionals have become concerned about their risks, particularly when they are used for a long time.
Benzodiazepines may be prescribed to:
- treat the symptoms of anxiety disorders
- relieve insomnia
- help with treatment of symptoms experienced by cancer patients
- control epilepsy
- help relax muscles during certain medical procedures (such as endoscopy)
- treat alcohol withdrawal.
Benzodiazepines are relatively safe and, with overdose, rarely result in death. However, used chronically, benzodiazepines can be addicting. These agents are often taken in combination with other drugs of abuse by patients with addiction disorders. Some people misuse benzodiazepines to get high or to help with the ‘come down’ effects of stimulants such as amphetamines or cocaine.
Benzodiazepines can cause a person to overdose, particularly when used with alcohol or other drugs. Benzodiazepines are associated with dependence and withdrawal symptoms, even after a short period of use which is why benzodiazepines are not the first option for pharmacological treatment of insomnia (difficulty falling asleep or staying asleep), anxiety or other health concerns 2.
Benzodiazepines are known by their chemical (generic) name or their brand name. In each case the drug is the same – it’s just made by a different company. Some common benzodiazepines are:
Table 1. Benzodiazepines pharmaceutical names
| Generic name | Brand name | Type |
|---|---|---|
| Diazepam | Ducene®, Valium® | Long-acting |
| Oxazepam | Alepam®, Murelax®, Serepax® | Short-acting |
| Nitrazepam | Alodorm®, Mogadon® | Intermediate-acting |
| Temazepam | Euhypnos®, Normison® | Short-acting |
| Alprazolam | Xanax®, Kalma®, Alprax® | Short-acting |
More than a dozen benzodiazepines are available by prescription. The following is a list of benzodiazepines in current use, with their initial brand name and year of approval: alprazolam (Xanax, 1981), chlordiazepoxide (Librium, 1960), clonazepam (Klonopin, 1997), clorazepate (Tranxene, 1972), diazepam (Valium, 1963), estazolam (ProSom, 1990), flurazepam (Dalmane, 1970), lorazepam (Ativan, 1977), midazolam (Versed, 1985), oxazepam (Serax, 1965), quazepam (Doral, 1985), temazepam (Restoril, 1981), triazolam (Halcion, 1982), and most recently clobazam (2011).
Benzodiazepines all share similar activity and clinical effects, but variability in dosing, pharmacokinetics, rapidity of uptake and half-life make them more suited for one or another of these indications. Thus, estazolam, flurazepam, quazepam, temazepam and triazolam are generally used as sleeping pills, whereas alprazolam, chlordiazepoxide, diazepam, and lorazepam are used largely for the treatment of anxiety. Clobazam, clonazepam, and clorazepate are used as anticonvulsants, and high dose, parenteral diazepam and lorazepam are used for status epilepticus. Parenteral midazolam, diazepam and lorazepam are also used as anesthetics or anesthetic premedications. Alprazolam (Xanax), clonazepam (Klonopin), diazepam (Valium) and lorazepam (Ativan) are listed among the top 100 most commonly prescribed medications in United States 3. According to the American Psychiatric Association report on benzodiazepines, 11 to 15 percent of the adult population has taken a benzodiazepine one or more times during the preceding year, but only 1 to 2 percent have taken benzodiazepines daily for 12 months or longer 4. In psychiatric treatment settings and in substance-abuse populations, however, the prevalence of benzodiazepine use, abuse and dependence is substantially higher than that in the general population 5.
Does alcohol affect my benzodiazepines?
Alcohol can increase the sedative effect of benzodiazepines. If you drink alcohol whilst taking benzodiazepines you are likely to feel more tired.
Can I drive when taking benzodiazepines?
Taking benzodiazepines can affect the way you drive. For example, they can:
- affect your judgement,
- make your reaction times slower, and
- make you tired
If you are affected by your medication you should not drive until the effects wear off.
It is illegal to drive if you are affected by drugs such as benzodiazepines. Ask your doctor if you are safe to drive whilst taking your medication.
You should tell the DMV if you are taking medication that may affect your driving. You should also tell them if you have a medical condition that could affect your driving.
What else should I consider before taking benzodiazepines?
- Sex. Benzodiazepines do not have any known effects on sexual performance. But drowsiness might have an impact on your sex life.
- Pregnancy. Benzodiazepines should not be used regularly during pregnancy. They should only be used to help control seizures. If benzodiazepines are taken during pregnancy, this can affect the baby when it is born. The baby can get withdrawal symptoms. The baby can have breathing problems and low body temperature. Tell your midwife and other healthcare professionals if you’ve been taking benzodiazepines through your pregnancy. But there is no evidence to say that taking benzodiazepines before pregnancy will have a negative effect on pregnancy or birth.
- Breastfeeding. You should not breastfeed while taking benzodiazepines. Medication you take will be in your breast milk.
How do benzodiazepines work?
Benzodiazepines are central nervous system depressants and they all increase activity at receptors for the neurotransmitter gamma-aminobutyric acid (GABA). The inhibitory neurotransmitter gamma-aminobutyric acid (GABA) inhibits the activity of neurons, slowing down the workings of your brain and nervous system. Benzodiazepines enhance the affinity of the recognition site for GABA by inducing conformational changes that make GABA binding more efficacious. Activation of the benzodiazepine-GABA-chloride ionophor complex is responsible for producing the therapeutic anxiolytic effects of benzodiazepines and for mediating many of the side effects and, possibly, dependence and withdrawal from these drugs 6.
Similarly, other sites for drug and neurotransmitter binding are associated with the GABA receptor complex, which serves as a primary site of action of benzodiazepines, barbiturates and other sedative-hypnotics, such as alcohol 6. Benzodiazepines and barbiturates act at separate binding sites on the receptor to potentiate the inhibitory action of GABA. They do so by allosterically altering the receptor (changing its conformation) so that it has a greater binding affinity for GABA. Ethanol modifies the receptor by altering the membrane environment so that it has increased affinity for GABA and the other sedative-hypnotic drugs. That benzodiazepines, barbiturates and ethanol all have related actions on a common receptor type, which explains their pharmacologic synergy and cross tolerance. Thus, benzodiazepines are used during alcohol detoxification.
With long-term high-dose use of benzodiazepines (or ethanol), there is an apparent decrease in the efficacy of GABA-A receptors, presumably a mechanism of tolerance 7. When high-dose benzodiazepines or ethanol are abruptly discontinued, this “down-regulated” state of inhibitory transmission is unmasked, leading to characteristic withdrawal symptoms such as anxiety, insomnia, autonomic hyperactivity and, possibly, seizures.
Benzodiazepines differ mainly in how quickly they are absorbed, how long their effects last, and how long they take to leave the body. Benzodiazepines only treat symptoms of anxiety or insomnia, and do not solve the underlying causes of these conditions.
The effects of benzodiazepines depend on the strength of the dose, the physical make-up of the person taking them and their state of mind.
Common effects of benzodiazepines include:
- relief from anxiety
- muscle relaxation
- sleepiness
- a sense of being disconnected or detached from reality
- dizziness
- loss of inhibitions.
Benzodiazepines can be highly addictive, whether they are taken under medical supervision or used recreationally.
Types of benzodiazepines
There are three types of benzodiazepines: long, intermediate and short-acting. Short-acting benzodiazepines have stronger withdrawal or ‘come down’ effects and can be more addictive than long-acting ones 8.
- Benzodiazepines used as sleeping pills (hypnotics) are shorter acting. They are mostly used for treating sleep problems such as insomnia.
- Benzodiazepines used to treat anxiety (anxiolytics) are longer lasting. They are mostly used for treating anxiety.
Table 2. Benzodiazepines used as sleeping pills (hypnotics)
| Hypnotic Benzodiazepines | ||
| Medicine name | Trade name | Use to treat |
| Flurazepam | Dalmane | Sleep problems |
| Loprazolam | Sleep problems | |
| Lormetazepam | Sleep problems | |
| Nitrazepam | Mogadon | Sleep problems |
| Temazapam | Sleep problems | |
Table 3. Benzodiazepines used to treat anxiety (anxiolytics)
| Anxiolytic Benzodiazepines | ||
| Medicine name | Trade name | Use to treat |
| Alprazolam | Anxiety disorders | |
| Chlordiazepoxide Hydrochloride | Anxiety disorders, alcohol withdrawal | |
| Diazepam | Rimapan | Anxiety disorders, Anxiety with sleep problems, alcohol withdrawal, muscle spasms |
| Lorazepam | Ativan | Anxiety disorders |
| Oxazepam | Anxiety disorders | |
| Clobazam | Tapclob | Anxiety disorder |
Potency and Half-Life of various benzodiazepines
High-potency benzodiazepines
- Drugs with a short half-life
- Alprazolam (Xanax)
- Lorazepam (Ativan)
- Triazolam (Halcion)
- Drugs with a long half-life
- Clonazepam (Klonopin)
Low-potency benzodiazepines
- Drugs with a short half-life
- Oxazepam (Serax)
- Temazepam (Restoril)
- Drugs with a long half-life
- Chlordiazepoxide (Librium)
- Clorazepate (Tranxene)
- Diazepam (Valium)
- Flurazepam (Dalmane)
Benzodiazepines uses
Benzodiazepines are central nervous system (CNS) depressants that are commonly prescribed in medicine to treat anxiety, stress, panic disorders, insomnia, alcohol withdrawal symptoms, muscle relaxation, epilepsy and to sedate people before certain medical procedures. It is generally recommended that benzodiazepines only be used for a short term – just days or weeks at a time.
Benzodiazepines clinical uses 9
- Anxiety disorders
- Acute anxiety
- Generalized anxiety disorder
- Panic disorder
- Phobias (social, simple)
- Post-traumatic stress disorder (PTSD)
- Obsessive-compulsive disorder (OCD)
- Insomnia
- Anxiety associated with medical illness
- Cardiovascular
- Gastrointestinal
- Somatoform disorder
- Convulsive disorders
- Acute status epilepticus
- Neonatal seizures or febrile convulsions
- Preeclampsia
- Tetanus
- Adjunct to other anticonvulsants
- Amnestic (before surgery or procedure)
- Spastic disorders and other types of acute muscle spasm
- Cerebral palsy
- Multiple sclerosis (MS)
- Paraplegia secondary to spinal trauma
- Involuntary movement disorders
- Restless leg syndrome
- Akathisia associated with neuroleptic use
- Choreiform disorders
- Myoclonus
- Detoxification from alcohol and other substances
- Agitation or anxiety associated with other psychiatric conditions
- Acute mania
- Psychotic illness
- Anxiety associated with depression
- Impulse control disorders
- Catatonia or mutism
- Other adjunctive uses
- Surgery
- Dentistry
- Diagnostic studies, such as computed tomography, magnetic resonance imaging and endoscopy
- Cardioversion
- Chemotherapy
Severe anxiety
You may be given benzodiazepines for the short-term relief of severe anxiety. You should not be given them for long term relief.
Panic disorders
You may be given benzodiazepines:
- When you first start taking antidepressants, OR
- if you don’t respond to antidepressants.
Insomnia
Benzodiazepines can be used to treat insomnia. Insomnia means that you find it difficult to fall asleep or stay asleep.
You should only be offered benzodiazepines to treat insomnia if it is severe, disabling or is causing you a lot of distress.
Benzodiazepines should only be offered for short term use.
Acute alcohol withdrawal
Long acting benzodiazepines are used to help with the effects of acute alcohol withdrawal.
You should stay in hospital during alcohol withdrawal if you have severe alcohol dependence. Alcohol withdrawal without medical support can cause dangerous side effects such as seizures.
Recreational use of benzodiazepines
Some people take benzodiazepines illegally for recreational use. They may use them to feel a sense of euphoria (or high) or mix them with other drugs such as stimulants (cocaine, amphetamines, ecstasy) to ‘come down’. Benzodiazepines can be dangerous when mixed with other drugs (including alcohol) and can put you at risk of overdose or harm.
Some people may give them to others intentionally or without their consent (such as spiking their drink).
Benzodiazepines abuse
Benzodiazepines are rarely the preferred or sole drug of abuse. An estimated 80 percent of benzodiazepine abuse is part of polydrug abuse, most commonly with opioids 10. A two-year treatment outcome study by the National Institute on Drug Abuse found that 15 percent of heroin users also used benzodiazepines daily for more than one year, and 73 percent used benzodiazepines more often than weekly 11. Studies indicate that from 5 percent to as many as 90 percent of methadone users are also regular users of benzodiazepines. High-dose benzodiazepine abuse is especially prevalent in patients who are taking methadone 12.
Studies indicate that 3 to 41 percent of alcoholic persons report that they abused benzodiazepines at some time, often to modulate intoxication or withdrawal effects 13. The contemporary alcoholic is usually a multiple-drug user. As many as 80 percent of alcoholics under the age of 30 have been addicted to or use at least one other drug 10.
Medical prescriptions constitute the primary source of supply for people who abuse benzodiazepines. Prescriptions may also have a street value, which encourages rerouting to illicit sources. Benzodiazepines have multiple uses for polydrug addicts: they are used to enhance the euphoriant effects of opioids (such as to “boost” methadone doses), to alleviate withdrawal or abstinence syndromes (such as between heroin “fixes”), to temper cocaine highs, to augment alcohol synergistically and to modulate withdrawal states.
As potential drugs of abuse, short-acting benzodiazepines seem to be preferred among addicts because of the rapidity of their onset of action 14. In general, mood-altering substances are most highly reinforcing in patients with chemical dependence if the agent has a rapid onset of action, a high potency, a brief duration of action, high purity and water solubility (for intravenous use) or high volatility (ability to vaporize if smoked) 15. Data suggest that highly lipophilic benzodiazepines (for example, those that cross the blood-brain barrier more rapidly), such as diazepam, and agents with a short half-life and high potency, such as lorazepam or alprazolam, are the most reinforcing benzodiazepines and, therefore, the ones most likely to be associated with abuse 14.
Clonazepam is a high-potency benzodiazepine with a long half-life. It is widely prescribed for a variety of psychiatric and neurologic conditions. Although clonazepam is perceived as “safe,” addiction medicine specialists have found that it is also frequently abused as a street drug. On the other hand, oxazepam (Serax), clorazepate (Tranxene) and chlordiazepoxide appear to have lower reinforcing effects than other benzodiazepines.
Compared with generic formulations, trade-name prescription drugs can be worth twice as much per tablet when they are sold on the street because they are readily recognizable as the “real thing” when compared with the photographs of tablets in the Physicians’ Desk Reference 15. Generic pills are often unrecognizable and hence are worth less when diverted for street sale. In many U.S. cities, the street value of Xanax or Klonopin may be $5 to $10 per pill, depending on dosage strength.
Benzodiazepine withdrawal syndrome
Benzodiazepines are addictive 16, 17, 18. You should not take them for longer than one month. You should only be prescribed benzodiazepine for the shortest amount of time possible. Taking benzodiazepine regularly for a few weeks or more can lead to addiction. Doctors recommend that you only take benzodiazepine for 2-4 weeks. Intermittent benzodiazepine use may help to avoid addiction. Intermittent means that you don’t take it regularly. For example, you don’t take benzodiazepine every day. The risk of addiction is higher if you have a history of drug or alcohol abuse. Or if you have a personality disorder. For patients on less than 4 weeks of benzodiazepine medication, it should be possible to stop benzodiazepine use without tapering 19, 20. Benzodiazepine discontinuation is usually beneficial as it is followed by improved psychomotor and cognitive functioning, particularly in the elderly 21. However, caution should be exercised with people who are at risk of seizures.
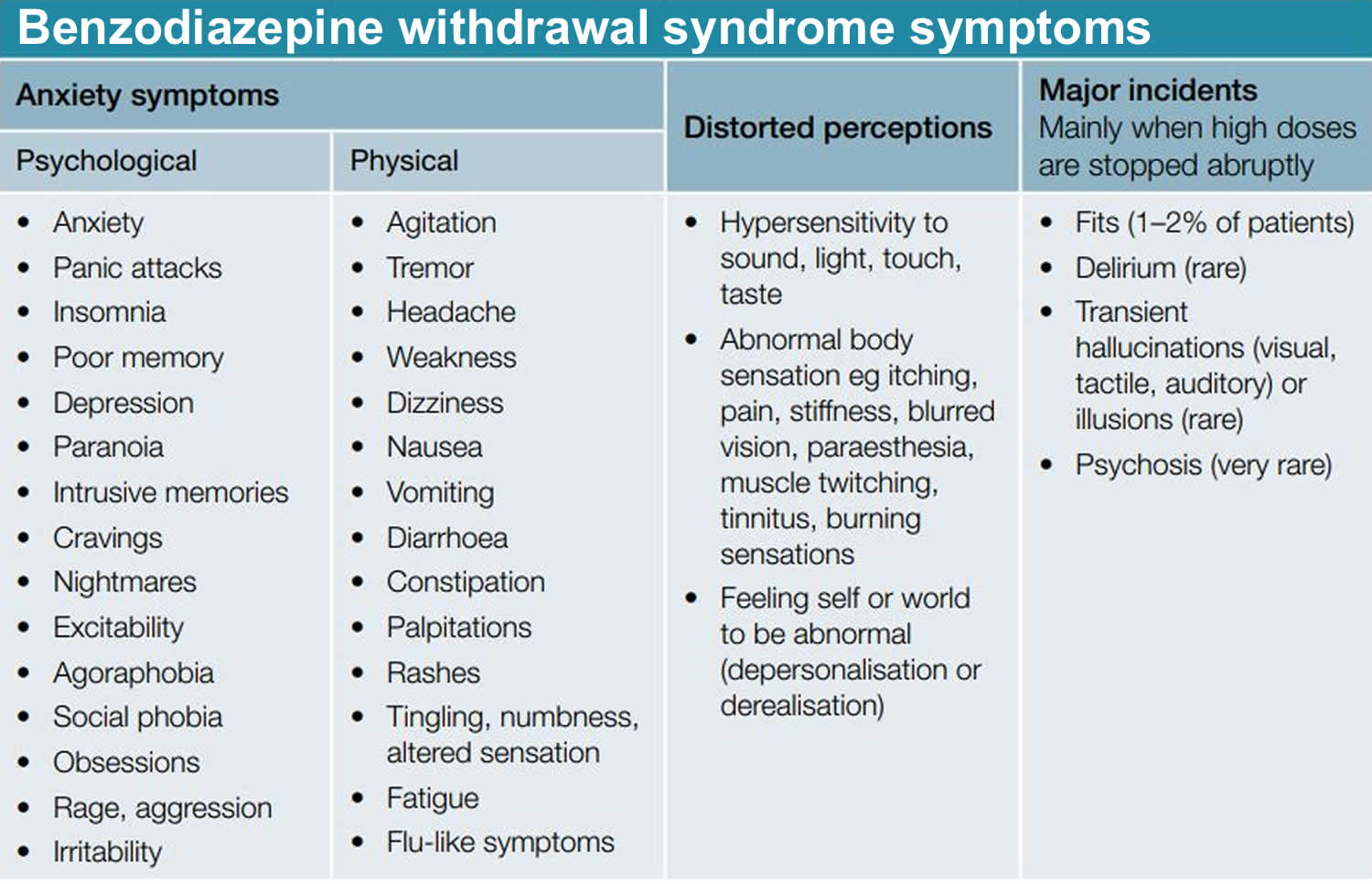
Benzodiazepines withdrawal symptoms may include:
- headaches
- aching or twitching muscles
- dizziness and tremors
- nausea, vomiting and stomach pains
- bizarre dreams, difficulty sleeping and fatigue
- poor concentration
- anxiety and irritability
- altered perception and heightening of senses
- delusions, hallucinations and paranoia
- seizures.
Common physical symptoms of benzodiazepines withdrawal:
- Stiffness
- Weakness
- Stomach problems
- Flu-like symptoms
- Visual problems
Common psychological symptoms of benzodiazepines withdrawal:
- Anxiety
- Insomnia
- Nightmares
- Depersonalization (the persistent feeling of observing oneself from outside one’s body or having a sense that one’s surroundings aren’t real)
- Problems with memory and concentration
- Depression
- Hallucinations. This is when you see, her, smell or feel things that are not there.
- Delusions. This is where you have beliefs that don’t match reality.
Protracted benzodiazepine withdrawal symptoms may include 22:
- Anxiety
- Depression
- Diarrhea, constipation, bloating
- Insomnia
- Irritability
- Muscle aches
- Poor concentration and memory
- Restlessness
- Less commonly, perceptual disturbances and panic attacks
- Occasionally, seizures and symptoms of psychosis.
These protracted benzodiazepine withdrawal symptoms do not occur in all benzodiazepine patients 23, but have a reported incidence between 15% and 44% among those taking benzodiazepines on a regular rather than an as-needed (PRN) basis 24.
Benzodiazepine withdrawal is possible for most people on longer term benzodiazepines, although the process of reduction may be difficult and lengthy 19. Up to 15% of people who experience benzo withdrawal will go on to have protracted symptoms lasting months to years 25. Benzodiazepine withdrawal syndrome can happen if you have been taking benzodiazepine regularly for 4-6 weeks. Benzodiazepine withdrawal symptoms vary from person to person and are different depending on the type of benzodiazepine being taken. The benzodiazepine withdrawal symptoms can last from a few weeks to a year. Talk to your doctor about stopping if you have been taking benzodiazepine regularly for more than 4-6 weeks. They will be able to help you stop taking benzodiazepine. Abruptly discontinuing benzodiazepine after you have been taking it daily for more than one month is potentially dangerous; withdrawal can be severe or even life-threatening 26. It is safer to reduce your benzodiazepine slowly with your doctor’s support and with specialist support where needed. This is because your body will be used to the benzodiazepine and you might experience withdrawal symptoms. It is recommended to withdraw from benzodiazepines slowly, over a period of months, under medical supervision. Benzodiazepine reduction requires a team approach with regular communication between the prescriber and other practitioners involved in the patient’s care (e.g., pharmacist, counsellor, psychiatrist, addiction services).
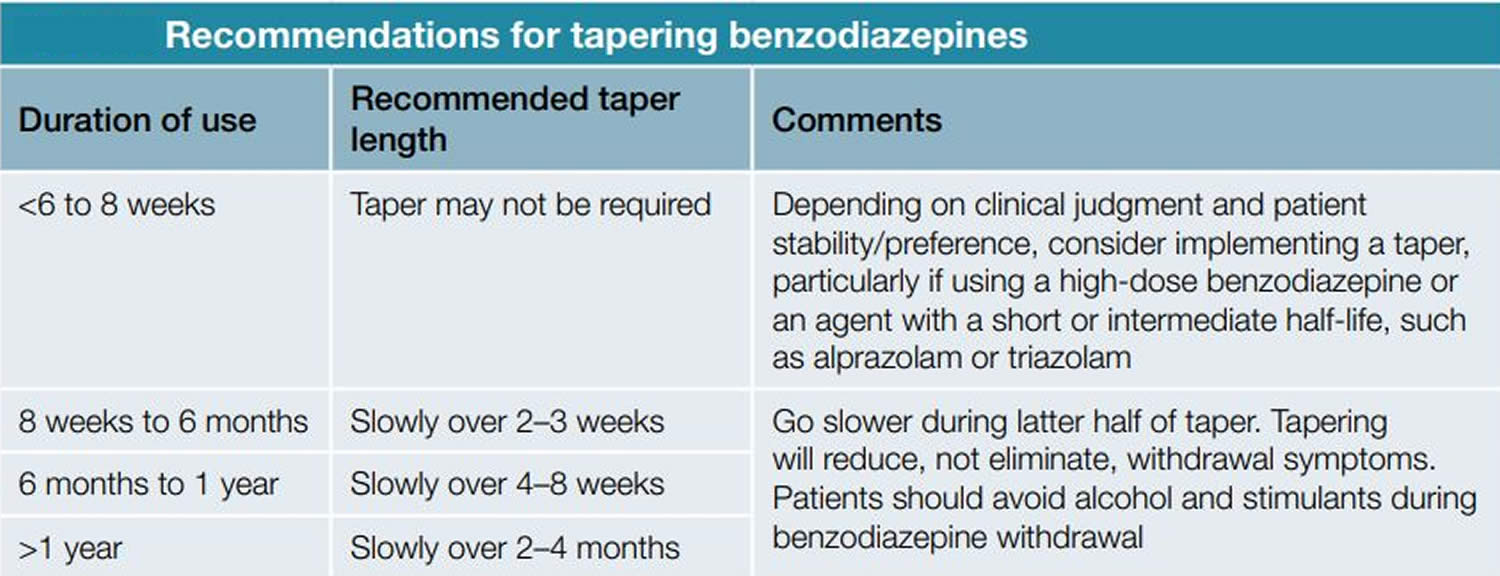
The clearest strategy for withdrawing benzodiazepines is to taper the medication (Figure 2) 21. Benzodiazepine withdrawal strategies should be individualized, considering factors such as lifestyle, personality, environmental stressors, reasons for taking benzodiazepine, the type of dependence (therapeutic dose, prescribed high dose, recreational high dose or polydrug) and amount of available personal and clinical support. Because anticipatory anxiety is often related to benzo withdrawal syndrome, benzodiazepines are commonly tapered slowly, with psychological support emphasized during the process to help patients learn alternative coping skills 21. A common first step in benzo withdrawal is to substitute diazepam for the benzodiazepine being taken 21. Switching to a longer-acting benzodiazepine equivalent may allow for a smoother taper experience 21. The slower elimination of diazepam creates a smoother taper in blood level 27.
Two-thirds of patients can achieve benzodiazepine cessation with gradual reduction of dose alone. Others need additional psychological therapies and a limited number of patients benefit from additional pharmacotherapy 28. Cognitive behavioral therapy (CBT) performed in a single, extended (20-minute) consultation with a doctor, with a handout, has been shown to increase non-use at 1 year from 15% to 45% 29. A systematic review comparing routine care to brief interventions, gradual dose reduction and psychological interventions found all interventions increased benzodiazepine discontinuation over routine care, with gradual dose reduction plus psychological interventions the most effective 28.
Figure 1. Benzodiazepine withdrawal syndrome symptoms
[Source 19 ]Figure 2. Recommendations for tapering benzodiazepines
[Source 19 ]Benzodiazepine withdrawal syndrome treatment
Evidence-based recommendations for general management of benzodiazepine withdrawal are difficult due to a lack of clinical data 19. The following are general principles for managing benzodiazepine withdrawal syndrome 30, 31, 25:
- Review the patients’ prescription records and discuss the situation to those receiving long-term benzodiazepines.
- Send patients letters suggesting methods of tapering off benzodiazepines (this may be enough to motivate them to withdraw).
- Teach patients ways to deal with anxiety and insomnia (either as primary conditions or due to withdrawal).
- Acknowledge that withdrawing from benzodiazepines can be stressful.
- Encourage family and friends to provide encouragement and practical help during withdrawal.
- Refer patients to appropriate services (eg psychologist or support groups). Only refer to drug or alcohol dependence services if the service has shown specific interest in benzodiazepine
- dependence or the patient also has a drug or alcohol problem.
- Advise patients to make changes in lifestyle such as regular exercise.
- Advise patients to avoid alcohol.
- Advise patients to avoid mild stimulants (eg coffee and chocolate [theobromine]) as these can cause anxiety, panic and insomnia.
- Postpone advice on smoking cessation until after the benzodiazepine has been withdrawn 21
Benzodiazepine reduction requires a team approach with regular communication between the prescriber and other practitioners involved in the patient’s care (eg pharmacist, counsellor, psychiatrist, addiction services).
The clearest strategy for withdrawing benzodiazepines is to taper the medication (see Figure 2) 21. There are three basic approaches to taper a benzodiazepine 26, 20:
- Use the same medication for tapering;
- Switch to a longer-acting equivalent; and
- Use add-on medications to help reduce potential withdrawal symptoms.
Slow discontinuation of benzodiazepines is recommended to avoid withdrawal symptoms (e.g., rebound anxiety, agitation, insomnia or seizures) particularly when use exceeds 8 weeks 19. However, clear evidence for the optimal rate of tapering is lacking. The dosage reduction mainly depends on the starting dose and whether the patient is tapering as an inpatient or outpatient. For safety reasons, outpatient tapers usually need to be slower than inpatient tapers. Patients taking higher dosages of benzodiazepines can usually tolerate larger reductions than those taking lower dosages 21, 32. The initial reduction typically ranges between 5% and 25% of the starting dose, with further reductions of 5% to 25% every one to four weeks as tolerated. The British National Formulary recommends a minimum of 6 weeks 33, while Lader recommends a maximum of 6 months 21. The exact rate of benzodiazepine reduction should be individualized according to the drug, dose and duration of treatment. A common first step in benzo withdrawal is to substitute diazepam for the benzodiazepine being taken 21. Switching to a longer-acting benzodiazepine equivalent may allow for a smoother taper experience 21. The slower elimination of diazepam creates a smoother taper in blood level 27. A suggested benzodiazepine taper schedule is available at https://www.va.gov/PAINMANAGEMENT/docs/OSI_6_Toolkit_Taper_Benzodiazepines_Clinicians.pdf
Supratherapeutic doses can initially be reduced by 25% to 30%, then further reduced by 5% to 10% daily, weekly, or monthly as appropriate, based on how well the patient tolerates withdrawal symptoms during the taper. Addition of an anticonvulsant (e.g., gabapentin [Neurontin]) should be considered for high-dosage withdrawal. Studies have shown that add-on medications, such as carbamazepine (Tegretol), imipramine, divalproex (Depakote), and trazodone, can mitigate some of the withdrawal discomfort 21. Use of antidepressants, such as duloxetine (Cymbalta) or amitriptyline, may help patients with chronic pain. There is limited evidence that antidepressants help in benzodiazepine withdrawal, unless depression (or anxiety disorders/panic disorders) are present or emerge during withdrawal 28.
For complex cases, stabilizing the dose at a 50% reduction for several months before resuming the taper may improve tolerability 34. At the end of the taper, some patients may need to reduce the pace with nearly homeopathic dosage reductions to tolerate the withdrawal. Compounding pharmacies can be used to obtain very small doses near the end of the taper.
All patients on a tapering regime must obtain prescriptions from one prescriber and through one pharmacy, where time-limited dispensing may be required (e.g., once or twice a week at a specified time) 19. Plans should be in place to cover absences of the usual prescribing doctor from the practice 19. Consider working closely with the patient’s pharmacist with staged supply or supervised dosing to assist the patient with dose reduction and cessation, if they are unable to manage this themselves 19.
Other considerations
Patients with benzodiazepine use disorder will have more difficulty reducing or stopping the dosage because of cravings. They may report intolerable withdrawal symptoms, request early refills, use benzodiazepines for reasons other than why they were prescribed, or report a need for benzodiazepines to perform normal daily activities. These patients may not be able to taper off without more intensive follow-up and intervention. A taper may be a litmus test for addiction; these patients may benefit from a referral to an addiction specialist 32.
Patients taking ‘therapeutic benzodiazepine doses’
For people who have early or mild benzodiazepine dependence, minimal interventions such as advisory letters, other information provision or doctor advice should be offered. Where benzodiazepine dependence is established, gradual dose reduction of prescribed benzodiazepine is recommended 35.
Switching from a short half-life benzodiazepine to a long half-life benzodiazepine before gradual taper should be reserved for patients having problematic withdrawal symptoms on reduction 35.
Additional psychological therapies increase the effectiveness of gradual dose reduction, particularly in patients with insomnia and panic disorder. Consideration should be given to targeted use of these interventions 35.
Patient taking high doses of benzodiazepines or who are users of illicit drugs (polydrug users)
So called ‘harm-reduction dosing’ or maintenance prescribing of benzodiazepines for patients using polydrugs cannot be recommended on the basis of existing evidence, as prescribing benzodiazepines does not appear to prevent use of other drugs 35. There are some evidence that maintenance dosing of benzodiazepines may reduce high-dose problematic benzodiazepine use in some patients 35.
Benzodiazepines drug interactions
When used alone, benzodiazepines carry an extremely low risk of acute toxicity. However, benzodiazepines often are used with other types of medications, including other drugs with abuse potential, and these drugs can enhance the toxic effects of benzodiazepines. Tell your doctor about any medicines you are taking before you start to take benzodiazepines. This includes any supplements or herbal medicines you take. Benzodiazepines can react with other types of medication and cause more side effects such as extra tiredness or low blood pressure.
Medication that can react with benzodiazepines includes 36:
- antidepressants,
- other hypnotics,
- antipsychotic medication,
- neuroleptics,
- anticonvulsants,
- alcohol,
- antihistamines, and
- beta-blockers.
Fatal overdoses in addicted patients often involve the combination of benzodiazepines and alcohol, with or without opiates 37. In addition, pharmacokinetic drug interactions may occur. For instance, selective serotonin reuptake inhibitors (SSRIs) may increase diazepam blood levels 38 and nefazadone (Serzone) may increase alprazolam levels 39 through hepatic enzyme inhibition, leading to increased sedative-hypnotic effects or side effects.
Benzodiazepines side effects
Benzodiazepines are addictive. You should not take them for longer than one month.
Not everyone who takes benzodiazepines will get side effects. Talk to your doctor if you are worried about side effects.
Benzodiazepines common side effects include:
- drowsiness or sleepiness
- dizziness
- headache
- confusion
- numbed emotions
- reduced awareness
- muscle weakness
- tremor
- Ataxia (impaired balance or coordination). Such as:
- balance and walking
- speaking
- swallowing
- your motor skills, such as writing and eating
- vision
You have an increased risk of falls and associated fractures if you are elderly and use benzodiazepines.
Benzodiazepines rare or less common side effects include:
- stomach upset and diarrhea
- nausea,
- vomiting
- constipation
- depression
- insomnia
- dry mouth
- increased appetite
- memory loss
- delusions
- aggression
Depression and emotional blunting
An association has been noted between benzodiazepine use and depressive symptoms and, in some cases, the emergence of suicidal ideation. Some evidence indicates that higher benzodiazepine dosages are associated with an increased risk of depression and that reducing the dosage or discontinuing therapy may resolve the depressive symptoms 40. Although the mechanism of this action is unclear, benzodiazepine-related depression might occur as a physiologic result of a reduction in central monoamine activity.
“Emotional anesthesia” may also be seen in clinical practice. This effect may be sought by drug addicts who become progressively more incapable of tolerating their emotions and life stressors.
Psychomotor slowing
Psychomotor slowing may be especially profound following initial administration of a benzodiazepine or with a sudden dosage increase. It also may be noted in patients, such as the elderly, who have decreased rates of metabolism or greater susceptibility to central nervous system depression 36. Psychomotor symptoms include drowsiness, poor concentration, ataxia, dysarthria, motor incoordination, diplopia, muscle weakness, vertigo and mental confusion 41. Studies of the psychomotor effects suggest that benzodiazepines slow reaction time and impair driving skills, increasing the risk of motor vehicle crashes in patients who are taking these agents 42.
Memory impairment
Benzodiazepines induce anterograde amnesia, which accounts for the beneficial effects of benzodiazepines such as midazolam (Versed) for presurgical medication. These specific amnestic effects appear to be separate from sedation 41. Episodic memory (the remembering of recent events and the circumstances in which they occurred and their time sequences) is particularly impaired and more markedly so in heavy alcohol drinkers who also use benzodiazepines. Specific deficits in visuospatial ability and sustained attention have also been described in patients who have taken therapeutic doses of benzodiazepines regularly for longer than one year 43.
Paradoxical disinhibition
Increased excitement, irritability, aggression, hostility and impulsivity may occur in some patients who take benzodiazepines. This paradoxical disinhibition may, in rare cases, result in attacks of rage or violence, or other indiscretionary or antisocial behaviors 44. Such reactions may be due to disinhibition of behavioral tendencies normally suppressed by social restraints (as can also be the case with alcohol). These reactions occur most commonly in children, in the elderly and in persons with developmental disabilities.
Benzodiazepines addiction
You should only be prescribed benzodiazepines for the shortest amount of time possible. Taking benzodiazepines regularly for a few weeks or more can lead to addiction. Doctors recommend that you only take them for 2-4 weeks.
Intermittent use may help to avoid addiction. Intermittent means that you don’t take it regularly. For example, you don’t take it every day.
The risk of addiction is higher if you have a history of drug or alcohol abuse. Or if you have a personality disorder.
Benzodiazepines long-term effects
Using benzodiazepines on a regular basis can lead to significant health problems, including:
- impaired thinking or memory loss
- anxiety and depression
- irritability, paranoia and aggression
- personality change
- weakness, lethargy and lack of motivation
- drowsiness, sleepiness and fatigue
- difficulty sleeping or disturbing dreams
- headaches
- nausea
- skin rashes and weight gain
- addiction
- withdrawal symptoms.
What if I want to stop taking benzodiazepines?
Withdrawal symptoms from benzodiazepines can happen if you have been taking the medication regularly for 4-6 weeks. Benzodiazepines withdrawal symptoms vary from person to person and are different depending on the type of benzodiazepine being taken. The benzodiazepines withdrawal symptoms can last from a few weeks to a year. Talk to your doctor about stopping if you have been taking benzodiazepines regularly for more than 4-6 weeks. They will be able to help you stop taking them. Abruptly discontinuing benzodiazepines after you have been taking them daily for more than one month is potentially dangerous; withdrawal can be severe or even life-threatening 26. It is safer to reduce your medication slowly with your doctor’s support. This is because your body will be used to the medication and you might experience withdrawal symptoms. It is recommended to withdraw from benzodiazepines slowly, over a period of months, under medical supervision.
Taper schedules should be individualized, considering factors such as lifestyle, personality, environmental stressors, reasons for taking benzodiazepines, and amount of available personal and clinical support. Because anticipatory anxiety is often related to withdrawal, benzodiazepines are commonly tapered slowly, with psychological support emphasized during the process to help patients learn alternative coping skills 45.
Benzodiazepines withdrawal symptoms may include:
- headaches
- aching or twitching muscles
- dizziness and tremors
- nausea, vomiting and stomach pains
- bizarre dreams, difficulty sleeping and fatigue
- poor concentration
- anxiety and irritability
- altered perception and heightening of senses
- delusions, hallucinations and paranoia
- seizures.
Common physical side effects of benzodiazepines withdrawal:
- Stiffness
- Weakness
- Stomach problems
- Flu-like symptoms
- Visual problems
Common psychological side effects of benzodiazepines withdrawal:
- Anxiety
- Insomnia
- Nightmares
- Depersonalization (the persistent feeling of observing oneself from outside one’s body or having a sense that one’s surroundings aren’t real)
- Problems with memory and concentration
- Depression
- Hallucinations. This is when you see, her, smell or feel things that are not there.
- Delusions. This is where you have beliefs that don’t match reality.
How to taper benzodiazepines
There are three basic approaches to a benzodiazepine taper 26:
- Use the same medication for tapering;
- Switch to a longer-acting equivalent; and
- Use adjunctive medications to help mitigate potential withdrawal symptoms.
The dosage reduction mainly depends on the starting dose and whether the patient is tapering as an inpatient or outpatient. For safety reasons, outpatient tapers usually need to be slower than inpatient tapers. Patients taking higher dosages of benzodiazepines can usually tolerate larger reductions than those taking lower dosages 45, 32. The initial reduction typically ranges between 5% and 25% of the starting dose, with further reductions of 5% to 25% every one to four weeks as tolerated. A suggested taper schedule is available at https://www.va.gov/PAINMANAGEMENT/docs/OSI_6_Toolkit_Taper_Benzodiazepines_Clinicians.pdf
Supratherapeutic doses can initially be reduced by 25% to 30%, then further reduced by 5% to 10% daily, weekly, or monthly as appropriate, based on how well the patient tolerates withdrawal symptoms during the taper. Addition of an anticonvulsant (e.g., gabapentin [Neurontin]) should be considered for high-dosage withdrawal. Studies have shown that adjunctive medications, such as carbamazepine (Tegretol), imipramine, divalproex (Depakote), and trazodone, can mitigate some of the withdrawal discomfort 45. Use of antidepressants, such as duloxetine (Cymbalta) or amitriptyline, may help patients with chronic pain. Switching to a longer-acting benzodiazepine equivalent may allow for a smoother taper experience 45.
For complex cases, stabilizing the dose at a 50% reduction for several months before resuming the taper may improve tolerability 34. At the end of the taper, some patients may need to reduce the pace with nearly homeopathic dosage reductions to tolerate the withdrawal. Compounding pharmacies can be used to obtain very small doses near the end of the taper.
Other considerations
Patients with benzodiazepine use disorder will have more difficulty reducing or stopping the dosage because of cravings. They may report intolerable withdrawal symptoms, request early refills, use benzodiazepines for reasons other than why they were prescribed, or report a need for benzodiazepines to perform normal daily activities. These patients may not be able to taper off without more intensive follow-up and intervention. A taper may be a litmus test for addiction; these patients may benefit from a referral to an addiction specialist 32.
When will benzodiazepines withdrawal side effects stop?
Your benzodiazepines withdrawal side effects will usually stop after a few weeks. But they can last longer for a small amount of people. You may not get benzodiazepines withdrawal side effects when you stop your benzodiazepine medication. You should talk to your doctor or local pharmacist if you are worried about the withdrawal effects of benzodiazepines.
Is there anything that can help with my symptoms through benzodiazepines withdrawal?
Antidepressant and mood stabilizing drugs may help with the withdrawal effects of benzodiazepines.
If you have insomnia you may benefit from treatment with melatonin.
If you have a panic disorder you may benefit from cognitive behavioral therapy (CBT) whilst you are coming off the medication.
Benzodiazepine overdose
In larger doses, benzodiazepines produce a similar effect to drunkenness. Benzodiazepine overdose signs and symptoms may include:
- lose coordination
- slur their speech
- have problems with thinking, concentration and memory
- have severe mood swings and aggression
- be jittery and excitable
- experience nausea
- have sleeping problems.
Benzodiazepines overdoses are usually characterized by slow, shallow breathing which may lead to unconsciousness, coma and potentially death. This is more common if benzodiazepines are combined with other drugs such as alcohol, painkillers, antidepressants, antihistamines, or heroin.
If you suspect an overdose, call your local emergency services number for an ambulance immediately.
Benzodiazepines and pregnancy
There is a risk that benzodiazepines can be harmful to babies. Benzodiazepines cross the placenta and are classified as class D teratogens. If you are pregnant or breastfeeding, it is best to avoid them. Benzodiazepines may lead to the development of dependence and consequent withdrawal symptoms in the fetus 46. Benzodiazepines are excreted in breast milk and thus are usually contraindicated in breast-feeding mothers.
Benzodiazepine dependence
Taking benzodiazepines regularly may not only lead to physical dependence (addiction), but can also lead to psychological dependence where people may feel they need the drug to cope with daily life. Benzodiazepines dependence will develop sooner (such as in one to two months) in a patient who is taking a high dosage of a high-potency agent such as alprazolam than in a patient who is receiving a relatively low dosage of a long-acting, low-potency agent such as chlordiazepoxide. The best way to prevent benzodiazepine dependence for high-risk patients is to adhere to treatment recommendations and emphasize nonpharmacologic therapies for anxiety and insomnia 47. If benzodiazepines are used, they should be prescribed for short-term, intermittent use (two to four weeks at no more than three times per week), intermittent brief courses (daily use for no more than two weeks in cases of extreme stress and anxiety), or occasional doses to limit the potential for new, long-term users 48.
As a result of physiologic dependence, withdrawal symptoms emerge with rapid dose reduction or abrupt discontinuation of the drug.
Psychologically, long-term use of benzodiazepines may lead to overreliance on the need for the agent, loss of self-confidence and varying degrees of drug-seeking behavior 36. Patients may be reluctant to discontinue the drug because of misplaced fears or anticipatory anxiety. Some patients combine alcohol with benzodiazepines when they are not able to acquire the desired or “needed” effects.
Treating benzodiazepine dependence
Treatment options for drug dependence may include detoxification, individual counseling and group therapy. See your doctor for information and referral, or contact an alcohol and drug service (https://www.drugabuse.gov) to find the appropriate referral for you.
Benzodiazepine tolerance
After only a short amount of time, a person can develop a tolerance, which means they need to take larger and larger doses to achieve the same effect. Some people may begin to experience benzodiazepine tolerance after only a few days. Over time, the body comes to depend on benzodiazepines to function at its best.
Tolerance to all of the actions of benzodiazepines can develop, although at variable rates and to different degrees. Tolerance to the hypnotic effects tends to develop rapidly, which may be beneficial in daytime anxiolysis but makes long-term management of insomnia difficult 49. Patients typically notice relief of insomnia initially, followed by a gradual loss of efficacy 50. Tolerance to the anxiolytic effect seems to develop more slowly than does tolerance to the hypnotic effects, but there is little evidence to indicate that benzodiazepines retain their efficacy after four to six months of regular use 51. Benzodiazepine therapy is often continued to suppress withdrawal states, which usually mimic symptoms of anxiety. Dosage escalation often maintains the cycle of tolerance and dependence, and patients may have difficulty discontinuing drug therapy.
Benzodiazepines in elderly patients
Benzodiazepine use in the elderly is associated with an increased rate of falls that cause hip and femur fractures and an increased likelihood of motor vehicle crashes 52. Cognitive impairment is common, although memory impairment may be reversible when benzodiazepines are discontinued 53.
Cognitive deterioration associated with normal aging processes and dementia can be worsened by benzodiazepine side effects. Cortical suppression mechanisms may be disturbed in the elderly, and disinhibited behaviors may increase with benzodiazepine use. With less cognitive and social reserve in the elderly patient, the short- and long-term withdrawal symptoms and other benzodiazepine side effects may lead the patient to frequently visit or telephone the physician. The physician may feel “trapped”into arguing against the use of benzodiazepines and prescribing benzodiazepines to elderly patients. In one study, this impasse was broken by referring elderly patients to inpatient detoxification, which resulted in a dramatic decrease in annual physician visits 54.
Alprazolam
Alprazolam (Xanax or Niravam) is a benzodiazepine that is used to treat anxiety disorders, panic disorders, and anxiety caused by depression. Talk to your doctor about the possible risks of using alprazolam for your condition. Alprazolam is available only with your doctor’s prescription.
Alprazolam is available in the following dosage forms: a tablet, an extended-release tablet, an orally disintegrating tablet (tablet that dissolves quickly in the mouth), and a concentrated solution (liquid) to be taken by mouth. Alprazolam tablet, orally disintegrating tablet, and concentrated solution usually are taken two to four times a day. The extended-release tablet is taken once daily, usually in the morning. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take alprazolam exactly as directed.
To take the concentrated liquid, use only the dropper that came with your prescription. Draw into the dropper the amount prescribed for one dose. Squeeze the dropper contents into a liquid or semisolid food such as water, juice, soda, applesauce, or pudding. Stir the liquid or food gently for a few seconds. The concentrated liquid will blend completely with the food. Drink or eat the entire mixture immediately. Do not store for future use.
Remove the orally disintegrating tablet from the bottle just before it is time for your dose. With dry hands, open the bottle, remove the tablet, and immediately place it on your tongue. The tablet will dissolve and can be swallowed with saliva. The orally disintegrating tablet can be taken with or without water.
Swallow the extended-release tablets whole; do not chew, crush, or break them.
Your doctor will probably start you on a low dose of alprazolam and gradually increase your dose, not more than once every 3 or 4 days.
Alprazolam may increase the risk of serious or life-threatening breathing problems, sedation, or coma if used along with certain medications. Tell your doctor if you are taking or plan to take certain opiate medications for cough such as codeine (in Triacin-C, in Tuzistra XR) or hydrocodone (in Anexsia, in Norco, in Zyfrel) or for pain such as codeine (in Fiorinal), fentanyl (Actiq, Duragesic, Subsys, others), hydromorphone (Dilaudid, Exalgo), meperidine (Demerol), methadone (Dolophine, Methadose), morphine (Astramorph, Duramorph PF, Kadian), oxycodone (in Oxycet, in Percocet, in Roxicet, others), and tramadol (Conzip, Ultram, in Ultracet). Your doctor may need to change the dosages of your medications and will monitor you carefully. If you take alprazolam with any of these medications and you develop any of the following symptoms, call your doctor immediately or seek emergency medical care immediately: unusual dizziness, lightheadedness, extreme sleepiness, slowed or difficult breathing, or unresponsiveness. Be sure that your caregiver or family members know which symptoms may be serious so they can call the doctor or emergency medical care if you are unable to seek treatment on your own.
Alprazolam may be habit forming. Do not take a larger dose, take it more often, or for a longer time than your doctor tells you to. Tell your doctor if you have ever drunk large amounts of alcohol, if you use or have ever used street drugs, or have overused prescription medications. Do not drink alcohol or use street drugs during your treatment. Drinking alcohol or using street drugs during your treatment with alprazolam also increases the risk that you will experience these serious, life-threatening side effects. Also tell your doctor if you have or have ever had depression or another mental illness.
Alprazolam may cause a physical dependence (a condition in which unpleasant physical symptoms occur if a medication is suddenly stopped or taken in smaller doses), especially if you take it for several days to several weeks. Do not stop taking this medication or take fewer doses without talking to your doctor. Stopping alprazolam suddenly can worsen your condition and cause withdrawal symptoms that may last for several weeks to more than 12 months. Your doctor probably will decrease your alprazolam dose gradually. Call your doctor or get emergency medical treatment if you experience any of the following symptoms: unusual movements; ringing in your ears; anxiety; memory problems; difficulty concentrating; sleep problems; seizures; shaking; muscle twitching; changes in mental health; depression; burning or prickling feeling in hands, arms, legs or feet; seeing or hearing things that others do not see or hear; thoughts of harming or killing yourself or others; overexcitement; or losing touch with reality.
Alprazolam special precautions
You should not take alprazolam if:
- you also take antifungal medicine such as itraconazole or ketoconazole; or
- you have a history of allergic reaction to any benzodiazepine (alprazolam, lorazepam, diazepam, Ativan, Valium, Versed, Klonopin, and others).
To make sure alprazolam is safe for you, tell your doctor if you have ever had:
- breathing problems;
- drug or alcohol addiction;
- depression, mood problems, or suicidal thoughts or behavior; or
- kidney or liver disease.
Tell your doctor if you are pregnant or plan to become pregnant. If you use alprazolam during pregnancy, your baby could be born with life-threatening withdrawal symptoms, and may need medical treatment for several weeks.
You should not breastfeed whilst taking alprazolam. If you do breastfeed, tell your doctor if you notice drowsiness or feeding problems in the baby.
Alprazolam is not approved for use by anyone younger than 18 years old.
Before taking alprazolam:
- tell your doctor and pharmacist if you are allergic to alprazolam, chlordiazepoxide (Librium, in Librax), clonazepam (Klonopin), clorazepate (Gen-Xene, Tranxene), diazepam (Diastat, Valium), estazolam, flurazepam, lorazepam (Ativan), oxazepam, quazepam (Doral), temazepam (Restoril), triazolam (Halcion), any other medications, or any of the ingredients in alprazolam products. Ask your pharmacist for a list of the ingredients.
- tell your doctor if you are taking itraconazole (Onmel, Sporanox) or ketoconazole (Nizoral). Your doctor will probably tell you not to take alprazolam.
- tell your doctor and pharmacist what other prescription and nonprescription medications, vitamins, and nutritional supplements, you are taking. Be sure to mention any of the following: amiodarone (Cordarone, Nexterone, Pacerone); antidepressants (‘mood elevators’) such as desipramine (Norpramin), imipramine (Tofranil), and nefazodone; antifungals such as fluconazole (Diflucan), posaconazole (Noxafil), or voriconazole (Vfend); antihistamines; cimetidine (Tagamet); clarithromycin (Biaxin, in Prevpac); cyclosporine (Gengraf, Neoral, Sandimmune); diltiazem (Cardizem, Cartia XT, Tiazac); ergotamine (Ergomar, in Cafergot, in Migergot); erythromycin (E.E.S., ERYC, others); isoniazid (Laniazid, in Rifamate, in Rifater); medications for mental illness and seizures; nicardipine (Cardene); nifedipine (Adalat, Afeditab CR, Procardia); oral contraceptives (birth control pills); selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine (Prozac, Sarafem), fluvoxamine (Luvox), paroxetine (Brisdelle, Paxil, Pexeva), and sertraline (Zoloft); sedatives; sleeping pills; and tranquilizers. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor and pharmacist what herbal products you are taking, especially St. John’s wort.
- tell your doctor if you have glaucoma (increased pressure in the eye that may cause loss of sight). Your doctor may tell you not to take alprazolam.
- tell your doctor if you have or have ever had seizures or lung, kidney, or liver disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. Alprazolam may harm the fetus. If you become pregnant while taking alprazolam, call your doctor.
- talk to your doctor about the risks and benefits of taking this medication if you are 65 years of age or older. Older adults should receive low doses of alprazolam because higher doses may not work better and may cause serious side effects.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking alprazolam.
- you should know that alprazolam may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
Special dietary instructions
Do not eat grapefruit or drink grapefruit juice while you’re taking alprazolam.
Alprazolam drug interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking alprazolam, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using alprazolam with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Boceprevir
- Clarithromycin
- Cobicistat
- Conivaptan
- Flumazenil
- Idelalisib
- Indinavir
- Itraconazole
- Ketoconazole
- Lopinavir
- Nefazodone
- Nelfinavir
- Posaconazole
- Saquinavir
- Telaprevir
- Telithromycin
- Voriconazole
Using alprazolam with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Abametapir
- Acepromazine
- Alfentanil
- Amiodarone
- Amobarbital
- Amprenavir
- Anileridine
- Aprepitant
- Aripiprazole
- Aripiprazole Lauroxil
- Asenapine
- Atazanavir
- Baclofen
- Benperidol
- Benzhydrocodone
- Bromazepam
- Bromopride
- Buprenorphine
- Buspirone
- Butabarbital
- Butalbital
- Butorphanol
- Calcium Oxybate
- Cannabidiol
- Carbamazepine
- Carbinoxamine
- Carisoprodol
- Carphenazine
- Ceritinib
- Cetirizine
- Chloral Hydrate
- Chlordiazepoxide
- Chlorpromazine
- Chlorzoxazone
- Cimetidine
- Ciprofloxacin
- Clobazam
- Clonazepam
- Clorazepate
- Clozapine
- Codeine
- Crizotinib
- Cyclobenzaprine
- Cyclosporine
- Dantrolene
- Darunavir
- Dasabuvir
- Delavirdine
- Dexmedetomidine
- Diacetylmorphine
- Diazepam
- Dichloralphenazone
- Difenoxin
- Digoxin
- Dihydrocodeine
- Diltiazem
- Diphenhydramine
- Diphenoxylate
- Domperidone
- Doxylamine
- Dronedarone
- Droperidol
- Elagolix
- Enflurane
- Erythromycin
- Esketamine
- Estazolam
- Eszopiclone
- Ethchlorvynol
- Ethopropazine
- Ethylmorphine
- Fentanyl
- Fexinidazole
- Flibanserin
- Fluconazole
- Flunitrazepam
- Fluphenazine
- Flurazepam
- Fluspirilene
- Fluvoxamine
- Fosamprenavir
- Fosaprepitant
- Fosnetupitant
- Fospropofol
- Gabapentin
- Gabapentin Enacarbil
- Halazepam
- Halothane
- Hexobarbital
- Hydrocodone
- Hydromorphone
- Hydroxyzine
- Imatinib
- Isoflurane
- Ivacaftor
- Ketamine
- Ketazolam
- Ketobemidone
- Larotrectinib
- Lemborexant
- Letermovir
- Levocetirizine
- Levorphanol
- Lofexidine
- Lomitapide
- Lorazepam
- Loxapine
- Magnesium Oxybate
- Meclizine
- Melperone
- Meperidine
- Mephenesin
- Mephobarbital
- Meprobamate
- Meptazinol
- Mesoridazine
- Metaxalone
- Methadone
- Methdilazine
- Methocarbamol
- Methohexital
- Methotrimeprazine
- Methylene Blue
- Metoclopramide
- Mibefradil
- Midazolam
- Mifepristone
- Mirtazapine
- Molindone
- Moricizine
- Morphine
- Morphine Sulfate Liposome
- Nalbuphine
- Netupitant
- Nicomorphine
- Nilotinib
- Nitrazepam
- Nitrous Oxide
- Olanzapine
- Opium
- Opium Alkaloids
- Orphenadrine
- Oxazepam
- Oxycodone
- Oxymorphone
- Palbociclib
- Papaveretum
- Paregoric
- Pentazocine
- Pentobarbital
- Perampanel
- Perazine
- Periciazine
- Perphenazine
- Phenobarbital
- Pimozide
- Piperacetazine
- Piperaquine
- Pipotiazine
- Piritramide
- Potassium Oxybate
- Prazepam
- Pregabalin
- Primidone
- Prochlorperazine
- Promazine
- Promethazine
- Propofol
- Quazepam
- Quetiapine
- Ramelteon
- Ranitidine
- Ranolazine
- Remifentanil
- Remimazolam
- Remoxipride
- Ritonavir
- Scopolamine
- Secobarbital
- Sertindole
- Sodium Oxybate
- Sufentanil
- Sulpiride
- Suvorexant
- Tapentadol
- Temazepam
- Thiethylperazine
- Thiopental
- Thiopropazate
- Thioridazine
- Tilidine
- Tizanidine
- Tolonium Chloride
- Topiramate
- Tramadol
- Trazodone
- Triazolam
- Trifluoperazine
- Trifluperidol
- Triflupromazine
- Trimeprazine
- Verapamil
- Voxelotor
- Zaleplon
- Zolpidem
- Zopiclone
- Zotepine
Using alprazolam with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Fluoxetine
- Kava
- Rifapentine
- Roxithromycin
- Sertraline
- St John’s Wort
- Theophylline
- Troleandomycin
Other interactions
Using alprazolam with any of the following is usually not recommended, but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use alprazolam, or give you special instructions about the use of food, alcohol, or tobacco.
- Ethanol
- Grapefruit Juice
Other medical problems
The presence of other medical problems may affect the use of alprazolam. Make sure you tell your doctor if you have any other medical problems, especially:
- Alcohol or drug abuse or dependence, history of or
- Depression, or history of or
- Lung or breathing problems (eg, respiratory depression) or
- Mania, or history of or
- Mental health problems, or history of or
- Seizures, or history of—Use with caution. May make these conditions worse.
- Glaucoma, acute narrow angle—Should not be used in patients with this condition.
- Kidney disease or
- Liver disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
Alprazolam uses
Alprazolam is used to treat anxiety disorders and panic disorder (sudden, unexpected attacks of extreme fear and worry about these attacks).
Alprazolam is also sometimes used to treat depression, fear of open spaces (agoraphobia), and premenstrual syndrome.
Alprazolam may also be prescribed for other uses; ask your doctor or pharmacist for more information.
Alprazolam dosage
The dose of alprazolam will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of alprazolam. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
For anxiety
- For oral dosage forms (solution, tablets, or orally disintegrating tablets):
- Adults—At first, 0.25 to 0.5 milligram (mg) 3 times a day. Your doctor may increase your dose as needed. However, the dose is usually not more than 4 mg per day.
- Older adults—At first, 0.25 mg 2 or 3 times a day. Your doctor may increase your dose as needed.
- Children—Use and dose must be determined by your doctor.
For panic disorder
- For oral dosage form (extended-release tablets):
- Adults—At first, 0.5 to 1 milligram (mg) taken in the morning once a day. Your doctor may increase your dose as needed. However, the dose is usually not more than 10 mg per day.
- Older adults—At first, 0.5 mg taken in the morning once a day. Your doctor may increase your dose as needed.
- Children—Use and dose must be determined by your doctor.
- For oral dosage forms (solution, tablets, or orally disintegrating tablets):
- Adults—At first, 0.5 milligram (mg) 3 times a day. Your doctor may increase your dose as needed. However, the dose is usually not more than 10 mg per day.
- Older adults—At first, 0.25 mg 2 or 3 times a day. Your doctor may increase your dose as needed.
- Children—Use and dose must be determined by your doctor.
Missed Dose
If you miss a dose of alprazolam, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not double doses.
Alprazolam side effects
Alprazolam may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- drowsiness
- light-headedness
- headache
- tiredness
- dizziness
- irritability
- talkativeness
- difficulty concentrating
- dry mouth
- increased salivation
- changes in sex drive or ability
- nausea
- constipation
- changes in appetite
- weight changes
- difficulty urinating
- joint pain
Some side effects can be serious. If you experience any of the following symptoms or those listed in the IMPORTANT WARNING section, call your doctor immediately or get emergency medical treatment:
- shortness of breath
- seizures
- severe skin rash
- yellowing of the skin or eyes
- confusion
- problems with speech
- problems with coordination or balance
Alprazolam may cause other side effects. Call your doctor if you have any unusual problems while taking alprazolam.
Chlordiazepoxide
Chlordiazepoxide (Librium) is a benzodiazepine that is used to treat anxiety disorders. Chlordiazepoxide may also be used short-term to treat symptoms of alcohol withdrawal, or anxiety you may have before a surgery. Chlordiazepoxide is sometimes prescribed for other uses; ask your doctor or pharmacist for more information. Chlordiazepoxide is available only with your doctor’s prescription.
Chlordiazepoxide comes as a tablet and capsule to take by mouth. It usually is taken one to four times a day with or without food. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take chlordiazepoxide exactly as directed.
Chlordiazepoxide may increase the risk of serious or life-threatening breathing problems, sedation, or coma if used along with certain medications. Tell your doctor if you are taking or plan to take certain opiate medications for cough such as codeine (in Triacin-C, in Tuzistra XR) or hydrocodone (in Anexsia, in Norco, in Zyfrel) or for pain such as codeine (in Fiorinal), fentanyl (Actiq, Duragesic, Subsys, others), hydromorphone (Dilaudid, Exalgo), meperidine (Demerol), methadone (Dolophine, Methadose), morphine (Astramorph, Duramorph PF, Kadian), oxycodone (in Oxycet, in Percocet, in Roxicet, others), and tramadol (Conzip, Ultram, in Ultracet). Your doctor may need to change the dosages of your medications and will monitor you carefully. If you take chlordiazepoxide with any of these medications and you develop any of the following symptoms, call your doctor immediately or seek emergency medical care immediately: unusual dizziness, lightheadedness, extreme sleepiness, slowed or difficult breathing, or unresponsiveness. Be sure that your caregiver or family members know which symptoms may be serious so they can call the doctor or emergency medical care if you are unable to seek treatment on your own.
Chlordiazepoxide may be habit forming. Do not take a larger dose, take it more often, or for a longer time than your doctor tells you to. Tell your doctor if you have ever drunk large amounts of alcohol, if you use or have ever used street drugs, or have overused prescription medications. Do not drink alcohol or use street drugs during your treatment. Drinking alcohol or using street drugs during your treatment with chlordiazepoxide also increases the risk that you will experience these serious, life-threatening side effects. Also tell your doctor if you have or have ever had depression or another mental illness.
Chlordiazepoxide may cause a physical dependence (a condition in which unpleasant physical symptoms occur if a medication is suddenly stopped or taken in smaller doses), especially if you take it for several days to several weeks. Do not stop taking this medication or take fewer doses without talking to your doctor. Stopping chlordiazepoxide suddenly can worsen your condition and cause withdrawal symptoms that may last for several weeks to more than 12 months. Your doctor probably will decrease your chlordiazepoxide dose gradually. Call your doctor or get emergency medical treatment if you experience any of the following symptoms: unusual movements; ringing in your ears; anxiety; memory problems; difficulty concentrating; sleep problems; seizures; shaking; muscle twitching; changes in mental health; depression; burning or prickling feeling in hands, arms, legs or feet; seeing or hearing things that others do not see or hear; thoughts of harming or killing yourself or others; overexcitement; or losing touch with reality.
Chlordiazepoxide special precautions
You should not use chlordiazepoxide if you are allergic to it.
Tell your doctor if you have ever had:
- depression, a mood disorder, suicidal thoughts or actions;
- alcoholism or drug addiction; or
- liver or kidney disease.
Tell your doctor if you are pregnant or plan to become pregnant. Chlordiazepoxide may harm an unborn baby. Avoid taking chlordiazepoxide during the first trimester of pregnancy.
Ask a doctor if it is safe to breastfeed while using chlordiazepoxide.
Chlordiazepoxide is not approved for use by anyone younger than 6 years old.
Before taking chlordiazepoxide:
- tell your doctor and pharmacist if you are allergic to chlordiazepoxide, alprazolam (Xanax), clonazepam (Klonopin), clorazepate (Gen-Xene, Tranxene), diazepam (Diastat, Valium), estazolam, flurazepam, lorazepam (Ativan), oxazepam, temazepam (Restoril), triazolam (Halcion), any other medications, or any of the ingredients in tablets and capsules. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: antihistamines; cimetidine (Tagamet); digoxin (Lanoxin); disulfiram (Antabuse); fluoxetine (Prozac, Sarafem, Selfemra); isoniazid (Laniazid, in Rifamate, in Rifater); ketoconazole (Nizoral); levodopa (in Ritary, in Sinemet, in Stalevo); medications for depression, seizures, Parkinson’s disease, asthma, colds, or allergies; metoprolol (Lopressor, Toprol XL, others); muscle relaxants; oral contraceptives; probenecid (Probalan, in Col-Probenecid); propranolol (Inderal, Innopran); rifampin (Rifadin, Rimactane, in Rifamate, in Rifater); sedatives; sleeping pills; theophylline (Elixophyllin, Theo 24, Theochron); tranquilizers; and valproic acid (Depakene). Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have or have ever had glaucoma; seizures; or lung, heart, or liver disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking chlordiazepoxide, call your doctor immediately.
- talk to your doctor about the risks and benefits of taking chlordiazepoxide if you are 65 years of age or older. Older adults should not usually take chlordiazepoxide because it is not as safe or effective as other medication(s) that can be used to treat the same condition.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking chlordiazepoxide.
- you should know that this medication may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
Special dietary instructions
Unless your doctor tells you otherwise, continue your normal diet.
Chlordiazepoxide drug interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking chlordiazepoxide, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using chlordiazepoxide with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Flumazenil
Using chlordiazepoxide with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Alfentanil
- Alprazolam
- Amobarbital
- Benzhydrocodone
- Bromazepam
- Bromopride
- Buprenorphine
- Butabarbital
- Butalbital
- Butorphanol
- Calcium Oxybate
- Cannabidiol
- Carbinoxamine
- Carisoprodol
- Cetirizine
- Chloral Hydrate
- Chlorzoxazone
- Clobazam
- Codeine
- Dantrolene
- Dihydrocodeine
- Doxylamine
- Esketamine
- Ethchlorvynol
- Fentanyl
- Flibanserin
- Fospropofol
- Gabapentin
- Gabapentin Enacarbil
- Hydrocodone
- Hydromorphone
- Ketamine
- Lacosamide
- Lemborexant
- Levocetirizine
- Levorphanol
- Lofexidine
- Loxapine
- Magnesium Oxybate
- Meclizine
- Meperidine
- Mephenesin
- Mephobarbital
- Meprobamate
- Metaxalone
- Methadone
- Methocarbamol
- Methohexital
- Metoclopramide
- Midazolam
- Mirtazapine
- Morphine
- Morphine Sulfate Liposome
- Nalbuphine
- Oxycodone
- Oxymorphone
- Pentazocine
- Pentobarbital
- Periciazine
- Phenobarbital
- Potassium Oxybate
- Pregabalin
- Primidone
- Propofol
- Remimazolam
- Scopolamine
- Secobarbital
- Sodium Oxybate
- Sufentanil
- Tapentadol
- Thiopental
- Tramadol
- Trazodone
- Zolpidem
Using chlordiazepoxide with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Ketoconazole
- Rifapentine
- St John’s Wort
- Theophylline
Other interactions
Using chlordiazepoxide with any of the following may cause an increased risk of certain side effects but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use chlordiazepoxide, or give you special instructions about the use of food, alcohol, or tobacco.
- Ethanol
Other medical problems
The presence of other medical problems may affect the use of chlordiazepoxide. Make sure you tell your doctor if you have any other medical problems, especially:
- Kidney disease or
- Liver disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
- Porphyria (genetic disorder)—Use with caution. May make this condition worse.
Chlordiazepoxide uses
Chlordiazepoxide is used to relieve anxiety and to control agitation caused by alcohol withdrawal. Chlordiazepoxide may also be used short-term to treat anxiety you may have before a surgery. Chlordiazepoxide is also used to treat irritable bowel syndrome (IBS).
Chlordiazepoxide dosage
The dose of chlordiazepoxide will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of chlordiazepoxide. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
For oral dosage form (capsules)
- For anxiety:
- Adults—5 to 25 milligrams (mg) three or four times a day.
- Older adults—5 milligrams (mg) two to four times a day.
- Children 6 years of age and older—At first, 5 milligrams (mg) two to four times a day. Your doctor may increase your dose if needed.
- Children younger than 6 years of age—Use and dose must be determined by your doctor.
- For apprehension and anxiety before a surgery:
- Adults—5 to 10 milligrams (mg) three or four times a day, taken several days before the surgery.
- Children—Use and dose must be determined by your doctor.
- For symptoms of alcohol withdrawal:
- Adults—At first, 50 to 100 milligrams (mg). The dose may be repeated until agitation is controlled. However, the dose is usually not more than 300 mg per day.
- Children—Use and dose must be determined by your doctor.
Missed dose
If you take several doses per day and miss a dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
Chlordiazepoxide side effects
Chlordiazepoxide may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- drowsiness
- dizziness
- tiredness
- weakness
- dry mouth
- diarrhea
- upset stomach
- changes in appetite
Tell your doctor if any of these symptoms are severe or do not go away:
- restlessness or excitement
- constipation
- difficulty urinating
- frequent urination
- blurred vision
- changes in sex drive or ability
Some side effects can be serious. If you experience any of the following symptoms or those listed in the IMPORTANT WARNING section, call your doctor immediately or get emergency medical help:
- shuffling walk
- persistent, fine tremor or inability to sit still
- fever
- difficulty breathing or swallowing
- severe skin rash
- yellowing of the skin or eyes
- irregular heartbeat.
Clobazam
Clobazam (Onfi or Sympazan) is a benzodiazepine that is used with other medications to treat seizures caused by Lennox-Gastaut syndrome, in people who are at least 2 years old.
Clobazam comes as a tablet and a suspension (liquid) to take by mouth, and as a film to apply on the tongue. It is usually taken once or twice a day, with or without food. Take clobazam at around the same time(s) every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand.
If you are unable to swallow the tablets whole, you may break them in half on the score mark or crush and mix them with a small amount of applesauce.
The liquid comes an adapter and two oral dosing syringes. Use only one of the two oral dosing syringes to measure your dose and save the second syringe. If the first oral syringe is damaged or lost, the second provided syringe may be used as a replacement.
To take the Clobazam liquid, follow these steps:
- Before the first use, uncap the bottle and firmly insert the adapter into the neck of the bottle until the adapter top is even with the bottle top. Do not remove the adapter during the period of time you are using this bottle.
- Shake the liquid well before each use to mix the medication evenly.
- To measure your dose, push the plunger of the syringe all the way down and insert the syringe into the adapter of the upright bottle. Then turn the bottle upside down and slowly pull the plunger back until the black ring is in line with your prescribed dose.
- Remove the syringe from the bottle adapter and slowly squirt the liquid from the syringe into the corner of your mouth.
- Place the bottle cap over the adapter after each use.
- Wash the oral syringe after each use. To wash the syringe, remove the plunger completely, wash the barrel and plunger with soap and water, rinse, and allow to dry. Do not place the syringe parts in the dishwasher.
To take the Clobazam film, follow these steps:
- Open the foil pouch and remove the film. Be sure that your hands are dry and clean.
- Place the film on the top of your tongue.
- Close your mouth and swallow your saliva normally. Do not chew, spit, or talk while the film dissolves. Do not take with liquids.
- Wash your hands.
If your doctor has told you to take more than one film per dose, wait until the first film has completely dissolved before applying the second film.
Your doctor will probably start you on a low dose of clobazam and gradually increase your dose, not more than once every week.
Some people may respond differently to clobazam based on their heredity or genetic makeup. Your doctor may order a blood test to help find the dose of clobazam that is best for you.
Clobazam may help control your condition but will not cure it. Continue to take clobazam even if you feel well. Do not stop taking clobazam without talking to your doctor.
Clobazam most common side effects are dose related and include dizziness, somnolence, impaired concentration, nervousness, aggression, antegrade amnesia, headache, fatigue, nausea and weakness. Clobazam can also lead to physical dependence and sudden discontinuation can cause withdrawal symptoms and rebound seizure activity.
Clobazam may increase the risk of serious or life-threatening breathing problems, sedation, or coma if used along with certain medications. Tell your doctor if you are taking or plan to take: antidepressants; medications for anxiety, mental illness, and seizures; sedatives; sleeping pills; opioids such as codeine, fentanyl (Duragesic, Subsys), morphine (Astramorph, Kadian), or oxycodone (in Percocet, in Roxicet, others); or tranquilizers. Your doctor may need to change the dosages of your medications and will monitor you carefully. If you take clobazam with any of these medications and you develop any of the following symptoms, call your doctor immediately or seek emergency medical care immediately: unusual dizziness, lightheadedness, extreme sleepiness, slowed or difficult breathing, or unresponsiveness. Be sure that your caregiver or family members know which symptoms may be serious so they can call the doctor or emergency medical care if you are unable to seek treatment on your own.
Clobazam may be habit forming. Do not take a larger dose, take it more often, or for a longer time than your doctor tells you to. Tell your doctor if you have ever drunk large amounts of alcohol, if you use or have ever used street drugs, or have overused prescription medications. Do not drink alcohol or use street drugs during your treatment. Drinking alcohol or using street drugs during your treatment with clobazam also increases the risk that you will experience these serious, life-threatening side effects. Also tell your doctor if you have or have ever had depression or another mental illness.
Clobazam may cause a physical dependence (a condition in which unpleasant physical symptoms occur if a medication is suddenly stopped or taken in smaller doses), especially if you take it for several days to several weeks. Do not stop taking this medication or take fewer doses without talking to your doctor. Stopping clobazam suddenly can worsen your condition and cause withdrawal symptoms that may last for several weeks to more than 12 months. Your doctor probably will decrease your clobazam dose gradually. Call your doctor or get emergency medical treatment if you experience any of the following symptoms: unusual movements; ringing in your ears; anxiety; memory problems; difficulty concentrating; sleep problems; seizures; shaking; muscle twitching; changes in mental health; depression; burning or prickling feeling in hands, arms, legs or feet; seeing or hearing things that others do not see or hear; thoughts of harming or killing yourself or others; overexcitement; or losing touch with reality.
Clobazam special precautions
You should not take clobazam if you are allergic to it.
Tell your doctor if you have ever had:
- breathing problems or lung disease;
- depression, mood problems, or suicidal thoughts or behavior;
- a drug or alcohol addiction; or
- liver or kidney disease.
Some people have thoughts about suicide while taking seizure medicine. Stay alert to changes in your mood or symptoms. Your family or caregivers should also watch for sudden changes in your behavior.
If you use clobazam during pregnancy, your baby could be born with life-threatening withdrawal symptoms, and may need medical treatment for several weeks.
Do not start or stop seizure medication during pregnancy without your doctor’s advice. Clobazam may harm an unborn baby, but having a seizure during pregnancy could harm both mother and baby. Preventing seizures may outweigh these risks. Tell your doctor right away if you become pregnant.
There may be other seizure medications that are safer to use during pregnancy.
Clobazam can make hormonal birth control less effective, including birth control pills, injections, implants, skin patches, and vaginal rings. Use a back-up barrier birth control to prevent pregnancy: condom, diaphragm, cervical cap, or contraceptive sponge. Keep using birth control for at least 28 days after your last dose of clobazam.
If you are breastfeeding, tell your doctor if you notice drowsiness or feeding problems in the nursing baby.
Clobazam is not approved for use by anyone younger than 2 years old.
Before taking clobazam:
- tell your doctor and pharmacist if you are allergic to clobazam, any other medications, or any of the ingredients in clobazam tablets, suspension, or film. Ask your pharmacist or check the Medication Guide for a list of the ingredients.
- tell your doctor and pharmacist what other prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention the medications listed in the IMPORTANT WARNING section and any of the following: antihistamines; dextromethorphan (Delsym, in Nuedexta, in Robitussin DM); fluconazole (Diflucan); fluvoxamine (Luvox); omeprazole (Prilosec, in Zegerid); or ticlopidine. Your doctor may need to change the doses of your medications or monitor you carefully for side effects. Many other medications may also interact with clobazam, so be sure to tell your doctor about all the medications you are taking, even those that do not appear on this list.
- tell your doctor if you have or have ever had thoughts about harming or killing yourself, or planning or trying to do so or lung, kidney, or liver disease.
- tell your doctor if you are pregnant or plan to become pregnant. If you take clobazam regularly during the last few months of your pregnancy, your baby may experience withdrawal symptoms after birth. Tell your baby’s doctor right away if your baby experiences any of the following symptoms: irritability, hyperactivity, abnormal sleep, high-pitched cry, uncontrollable shaking of a part of the body, vomiting, or diarrhea. If you become pregnant while taking clobazam, call your doctor.
- if you are using hormonal contraceptives (birth control pills, patches, rings, implants, injections, or intrauterine devices), you should know that this type of birth control may not work well when used with clobazam. Hormonal contraceptives should not be used as your only method of birth control while you are taking clobazam and for 28 days after your final dose. Talk to your doctor about nonhormonal birth control methods that will work for you.
- tell your doctor if you are breastfeeding. If you are breastfeeding while taking clobazam, tell your doctor if your baby is not feeding well or is extremely drowsy.
- talk to your doctor about the risks and benefits of taking this medication if you are 65 years of age or older. Older adults should receive low doses of clobazam because higher doses may not work better and may cause serious side effects.
- you should know that clobazam may make you drowsy and affect your thinking, ability to make decisions, and coordination. Do not drive a car, operate machinery, or do other dangerous activities until you know how this medication affects you.
- you should know that your mental health may change in unexpected ways and you may become suicidal (thinking about harming or killing yourself or planning or trying to do so) while you are taking clobazam. A small number of adults and children 5 years of age and older (about 1 in 500 people) who took anticonvulsants, such as clobazam, to treat various conditions during clinical studies became suicidal during their treatment. Some of these people developed suicidal thoughts and behavior as early as one week after they started taking the medication. You and your doctor will decide whether the risks of taking an anticonvulsant medication are greater than the risks of not taking the medication. You, your family, or your caregiver should call your doctor right away if you experience any of the following symptoms: panic attacks; agitation or restlessness; new or worsening irritability, anxiety, or depression; acting on dangerous impulses; difficulty falling or staying asleep; aggressive, angry, or violent behavior; mania (frenzied, abnormally excited mood); thinking about harming or killing yourself, or planning or trying to do so; or any other unusual changes in behavior or mood. Be sure that your family or caregiver knows which symptoms may be serious so they can call the doctor if you are unable to seek treatment on your own.
Special dietary instructions
Unless your doctor tells you otherwise, continue your normal diet.
Clobazam drug interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking clobazam, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using clobazam with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Flumazenil
- Thioridazine
Using clobazam with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Acepromazine
- Alfentanil
- Alprazolam
- Anileridine
- Aripiprazole
- Asenapine
- Baclofen
- Benperidol
- Benzhydrocodone
- Bromazepam
- Buprenorphine
- Butorphanol
- Calcifediol
- Calcium Oxybate
- Cannabidiol
- Carbinoxamine
- Carisoprodol
- Carphenazine
- Cetirizine
- Chloral Hydrate
- Chlordiazepoxide
- Chlorpromazine
- Chlorzoxazone
- Clonazepam
- Clorazepate
- Clozapine
- Codeine
- Cyclobenzaprine
- Dantrolene
- Desogestrel
- Dexmedetomidine
- Diacetylmorphine
- Diazepam
- Dichloralphenazone
- Dienogest
- Difenoxin
- Dihydrocodeine
- Diphenhydramine
- Diphenoxylate
- Doxorubicin
- Doxorubicin Hydrochloride Liposome
- Doxylamine
- Droperidol
- Drospirenone
- Enflurane
- Esketamine
- Eslicarbazepine Acetate
- Estazolam
- Estradiol
- Eszopiclone
- Ethchlorvynol
- Ethinyl Estradiol
- Ethopropazine
- Ethylmorphine
- Ethynodiol
- Etonogestrel
- Fentanyl
- Flibanserin
- Flunitrazepam
- Fluphenazine
- Flurazepam
- Fluspirilene
- Fospropofol
- Gabapentin
- Gabapentin Enacarbil
- Gestodene
- Halazepam
- Haloperidol
- Halothane
- Hexobarbital
- Hydrocodone
- Hydromorphone
- Isoflurane
- Ketamine
- Ketazolam
- Ketobemidone
- Lemborexant
- Levocetirizine
- Levonorgestrel
- Levorphanol
- Lofexidine
- Lorazepam
- Loxapine
- Magnesium Oxybate
- Meclizine
- Medroxyprogesterone
- Melperone
- Meperidine
- Mephenesin
- Meprobamate
- Meptazinol
- Mesoridazine
- Mestranol
- Metaxalone
- Methadone
- Methdilazine
- Methocarbamol
- Methotrimeprazine
- Methylene Blue
- Metoclopramide
- Midazolam
- Mirtazapine
- Modafinil
- Molindone
- Moricizine
- Morphine
- Morphine Sulfate Liposome
- Nalbuphine
- Nicomorphine
- Nifedipine
- Nitrazepam
- Nitrous Oxide
- Nomegestrol
- Norelgestromin
- Norethindrone
- Norgestimate
- Norgestrel
- Olanzapine
- Opium
- Opium Alkaloids
- Orlistat
- Orphenadrine
- Oxazepam
- Oxycodone
- Oxymorphone
- Papaveretum
- Paregoric
- Pentazocine
- Perampanel
- Perazine
- Periciazine
- Perphenazine
- Pimozide
- Piperacetazine
- Piperaquine
- Pipotiazine
- Piritramide
- Potassium Oxybate
- Prazepam
- Pregabalin
- Primidone
- Prochlorperazine
- Promazine
- Promethazine
- Propofol
- Quazepam
- Quetiapine
- Ramelteon
- Remifentanil
- Remimazolam
- Remoxipride
- Scopolamine
- Segesterone
- Sertindole
- Sodium Oxybate
- Sufentanil
- Sulpiride
- Suvorexant
- Tamoxifen
- Tapentadol
- Temazepam
- Thiethylperazine
- Thiopropazate
- Tilidine
- Tolonium Chloride
- Topiramate
- Tramadol
- Trazodone
- Triazolam
- Trifluoperazine
- Trifluperidol
- Triflupromazine
- Trimeprazine
- Ulipristal
- Zaleplon
- Zolpidem
- Zopiclone
- Zotepine
Using clobazam with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Etravirine
- Felbamate
- Fosphenytoin
- Ginkgo
- Ketoconazole
- Phenytoin
- Rifapentine
- St John’s Wort
- Theophylline
Other interactions
Using clobazam with any of the following may cause an increased risk of certain side effects but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use clobazam, or give you special instructions about the use of food, alcohol, or tobacco.
- Ethanol
Other medical problems
The presence of other medical problems may affect the use of clobazam. Make sure you tell your doctor if you have any other medical problems, especially:
- Alcohol abuse, or history of or
- Depression, history of or
- Drug abuse or dependence, or history of or
- Lung or breathing problems (eg, respiratory depression) or
- Mood or behavior disorder, history of—Use with caution. May make these conditions worse.
- Liver disease, mild to moderate—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
Clobazam uses
Clobazam was approved for use in the United States in 2011 as an anticonvulsant to be used either alone or in combination with other agents as therapy of the severe form of childhood epilepsy known as Lennox-Gastaut syndrome. Clobazam is used with other medication(s) to control seizures in adults and children 2 years of age and older who have Lennox-Gastaut syndrome (a disorder that causes seizures and often causes developmental delays).
Clobazam dosage
The dose of clobazam will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of clobazam. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
For oral dosage forms (film, suspension, or tablets)
- For seizures:
- Adults and children 2 years of age and older weighing more than 30 kilograms (kg)—Dose is based on body weight and must be determined by your doctor. The starting dose is usually 10 milligrams (mg) per day, given as 2 divided doses per day. Your doctor may adjust your dose as needed. However, the dose is usually not more than 40 mg per day.
- Adults and children 2 years of age and older weighing 30 kg or less—Dose is based on body weight and must be determined by your doctor. The starting dose is usually 5 mg as a single dose per day. Your doctor may adjust your dose as needed. However, the dose is usually not more than 20 mg per day.
- Older adults—Dose is based on body weight and must be determined by your doctor. The starting dose is usually 5 mg as a single dose per day. Your doctor may adjust your dose as needed. However, the dose is usually not more than 40 mg per day.
- Children younger than 2 years of age—Use and dose must be determined by your doctor.
Missed dose
Take the missed dose as soon as you remember it. However, if it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
Clobazam side effects
Clobazam may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- tiredness
- problems with coordination
- difficulty speaking or swallowing
- drooling
- change in appetite
- vomiting
- constipation
- cough
- joint pain
Some side effects can be serious. If you experience any of these symptoms or those listed in the SPECIAL PRECAUTIONS or IMPORTANT WARNING sections, call your doctor immediately or get emergency medical treatment:
- difficult, painful, or frequent urination
- cough, difficulty breathing, fever
- sores in your mouth, rash, hives, peeling or blistering skin
- fever
Clobazam may cause other side effects. Call your doctor if you have any unusual problems while taking clobazam.
Clonazepam
Clonazepam (Klonopin) is a benzodiazepine that is used to treat certain seizure disorders (including absence seizures or Lennox-Gastaut syndrome) in adults and children. Clonazepam is also used to treat panic disorder (including agoraphobia) in adults. Clonazepam is sometimes prescribed for other uses; ask your doctor or pharmacist for more information.
Clonazepam comes as a tablet and an orally disintegrating tablet (tablet that dissolves quickly in the mouth) to take by mouth. Clonazepam usually is taken one to three times a day with or without food. Take clonazepam at around the same time(s) every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand.
Do not try to push the orally disintegrating tablet through the foil. Instead, use dry hands to peel back the foil packaging. Immediately take out the tablet and place it in your mouth. The tablet will quickly dissolve and can be swallowed with or without liquid.
Your doctor will probably start you on a low dose of clonazepam and gradually increase your dose, not more often than once every 3 days.
Clonazepam may help control your condition, but will not cure it. It may take a few weeks or longer before you feel the full benefit of clonazepam. Continue to take clonazepam even if you feel well. Do not stop taking clonazepam without talking to your doctor, even if you experience side effects such as unusual changes in behavior or mood, If you suddenly stop taking clonazepam, you may experience withdrawal symptoms such as new or worsening seizures, hallucinating (seeing things or hearing voices that do not exist), changes in behavior, sweating, uncontrollable shaking of a part of your body, stomach or muscle cramps, anxiety, or difficulty falling asleep or staying asleep. Your doctor will probably decrease your dose gradually.
Clonazepam may increase the risk of serious or life-threatening breathing problems, sedation, or coma if used along with certain medications. Tell your doctor if you are taking or plan to take certain opiate medications for cough such as codeine (in Triacin-C, in Tuzistra XR) or hydrocodone (in Anexsia, in Norco, in Zyfrel) or for pain such as codeine (in Fiorinal), fentanyl (Actiq, Duragesic, Subsys, others), hydromorphone (Dilaudid, Exalgo), meperidine (Demerol), methadone (Dolophine, Methadose), morphine (Astramorph, Duramorph PF, Kadian), oxycodone (in Oxycet, in Percocet, in Roxicet, others), and tramadol (Conzip, Ultram, in Ultracet). Your doctor may need to change the dosages of your medications and will monitor you carefully. If you take clonazepam with any of these medications and you develop any of the following symptoms, call your doctor immediately or seek emergency medical care immediately: unusual dizziness, lightheadedness, extreme sleepiness, slowed or difficult breathing, or unresponsiveness. Be sure that your caregiver or family members know which symptoms may be serious so they can call the doctor or emergency medical care if you are unable to seek treatment on your own.
Clonazepam may be habit forming. Do not take a larger dose, take it more often, or for a longer time than your doctor tells you to. Tell your doctor if you have ever drunk large amounts of alcohol, if you use or have ever used street drugs, or have overused prescription medications. Do not drink alcohol or use street drugs during your treatment. Drinking alcohol or using street drugs during your treatment with clonazepam also increases the risk that you will experience these serious, life-threatening side effects. Also tell your doctor if you have or have ever had depression or another mental illness.
Clonazepam may cause a physical dependence (a condition in which unpleasant physical symptoms occur if a medication is suddenly stopped or taken in smaller doses), especially if you take it for several days to several weeks. Do not stop taking this medication or take fewer doses without talking to your doctor. Stopping clonazepam suddenly can worsen your condition and cause withdrawal symptoms that may last for several weeks to more than 12 months. Your doctor probably will decrease your clonazepam dose gradually. Call your doctor or get emergency medical treatment if you experience any of the following symptoms: unusual movements; ringing in your ears; anxiety; memory problems; difficulty concentrating; sleep problems; seizures; shaking; muscle twitching; changes in mental health; depression; burning or prickling feeling in your hands, arms, legs or feet; seeing or hearing things that others do not see or hear; thoughts of harming or killing yourself or others; overexcitement; or losing touch with reality.
Clonazepam special precautions
You should not take clonazepam if you allergic to it or if you have:
- narrow-angle glaucoma;
- severe liver disease; or
- a history of allergic reaction to any benzodiazepine (including alprazolam, diazepam, lorazepam, Valium, Xanax, Versed, and others).
To make sure clonazepam is safe for you, tell your doctor if you have ever had:
- kidney or liver disease;
- breathing problems;
- depression, mood problems, or suicidal thoughts or behavior; or
- porphyria (a genetic enzyme disorder that causes symptoms affecting the skin or nervous system).
Some people have thoughts about suicide while taking clonazepam. Stay alert to changes in your mood or symptoms. Your family or caregivers should also watch for sudden changes in your behavior.
Tell your doctor if you are pregnant or plan to become pregnant. If you use clonazepam during pregnancy, your baby could be born with life-threatening withdrawal symptoms, and may need medical treatment for several weeks.
Do not start or stop seizure medication during pregnancy without your doctor’s advice. Clonazepam may harm an unborn baby, but having a seizure during pregnancy could harm both mother and baby. Preventing seizures may outweigh these risks. Tell your doctor right away if you become pregnant.
Ask a doctor if it is safe to breastfeed while using clonazepam.
Do not give clonazepam to a child without medical advice. Clonazepam is not approved to treat panic disorder in anyone younger than 18 years old.
Before taking clonazepam:
- tell your doctor and pharmacist if you are allergic to clonazepam, other benzodiazepines such as alprazolam (Xanax), chlordiazepoxide (Librium, in Librax), clorazepate (Gen-Xene, Tranxene), diazepam (Diastat, Valium), estazolam, flurazepam, lorazepam (Ativan), midazolam (Versed), oxazepam, temazepam (Restoril), triazolam (Halcion), any other medications, or any of the ingredients in clonazepam tablets. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what other prescription and nonprescription medications, vitamins, and nutritional supplements you are taking or plan to take. Be sure to mention any of the following: amiodarone (Cordarone, Nexterone, Pacerone); certain antibiotics such as clarithromycin (Biaxin, in Prevpac), erythromycin (Erythrocin, E-mycin, others), and troleandomycin (TAO) (not available in the US); antidepressants; certain antifungal medications such as itraconazole (Onmel. Sporanox) and ketoconazole (Nizoral); antihistamines; certain calcium channel blockers such as diltiazem (Cardizem, Tiazac, others) and verapamil (Calan, Covera, Verelan, in Tarka); cimetidine (Tagamet); HIV protease inhibitors including indinavir (Crixivan), nelfinavir (Viracept), and ritonavir (Norvir, in Kaletra); medications for anxiety, colds or allergies, or mental illness; other medications for seizures such as carbamazepine (Epitol, Tegretol, Teril), phenobarbital, phenytoin (Dilantin, Phenytek), or valproic acid (Depakene); muscle relaxants; nefazodone; rifampin (Rifadin, Rimactane); sedatives; certain selective serotonin reuptake inhibitors (SSRIs) such as fluvoxamine (Luvox); other sleeping pills; and tranquilizers. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor what herbal products you are taking, especially St. John’s wort.
- tell your doctor if you have or have ever had glaucoma (increased pressure in the eye that may cause vision loss) or liver disease. Your doctor may tell you not to take clonazepam.
- tell your doctor if you have or have ever had lung or kidney disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. Clonazepam may harm the fetus. If you become pregnant while taking clonazepam, call your doctor.
- talk to your doctor about the risks and benefits of taking this medication if you are 65 years of age or older. Older adults should receive low doses of clonazepam because higher doses may not work better and may cause serious side effects.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking clonazepam.
- you should know that this medication may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
- you should know that your mental health may change in unexpected ways, and you may become suicidal (thinking about harming or killing yourself or planning or trying to do so) while you are taking clonazepam for the treatment of epilepsy, mental illness, or other conditions. A small number of adults and children 5 years of age and older (about 1 in 500 people) who took anticonvulsants such as clonazepam to treat various conditions during clinical studies became suicidal during their treatment. Some of these people developed suicidal thoughts and behavior as early as one week after they started taking the medication. There is a risk that you may experience changes in your mental health if you take an anticonvulsant medication such as clonazepam, but there may also be a risk that you will experience changes in your mental health if your condition is not treated. You and your doctor will decide whether the risks of taking an anticonvulsant medication are greater than the risks of not taking the medication. You, your family, or your caregiver should call your doctor right away if you experience any of the following symptoms: panic attacks; agitation or restlessness; new or worsening irritability, anxiety, or depression; acting on dangerous impulses; difficulty falling or staying asleep; aggressive, angry, or violent behavior; mania (frenzied, abnormally excited mood), talking or thinking about wanting to hurt yourself or end your life, withdrawing from friends and family; preoccupation with death and dying, giving away prized possessions, or any other unusual changes in behavior or mood. Be sure that your family or caregiver knows which symptoms may be serious so they can call the doctor if you are unable to seek treatment on your own.
Special dietary instructions
Do not eat grapefruit or drink grapefruit juice while you’re taking clonazepam.
Clonazepam drug interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking clonazepam, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using clonazepam with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Flumazenil
Using clonazepam with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Alfentanil
- Alprazolam
- Amobarbital
- Benzhydrocodone
- Bromazepam
- Bromopride
- Buprenorphine
- Butabarbital
- Butalbital
- Butorphanol
- Calcifediol
- Calcium Oxybate
- Cannabidiol
- Carbamazepine
- Carbinoxamine
- Carisoprodol
- Ceritinib
- Cetirizine
- Chloral Hydrate
- Chlorzoxazone
- Clarithromycin
- Clobazam
- Codeine
- Dantrolene
- Dihydrocodeine
- Doxylamine
- Esketamine
- Ethchlorvynol
- Fentanyl
- Flibanserin
- Fospropofol
- Gabapentin
- Gabapentin Enacarbil
- Hydrocodone
- Hydromorphone
- Ketamine
- Ketoconazole
- Lemborexant
- Levocetirizine
- Levorphanol
- Lofexidine
- Loxapine
- Magnesium Oxybate
- Meclizine
- Meperidine
- Mephenesin
- Mephobarbital
- Meprobamate
- Metaxalone
- Methadone
- Methocarbamol
- Methohexital
- Metoclopramide
- Midazolam
- Mirtazapine
- Morphine
- Morphine Sulfate Liposome
- Nalbuphine
- Orlistat
- Oxycodone
- Oxymorphone
- Pentazocine
- Pentobarbital
- Periciazine
- Phenobarbital
- Potassium Oxybate
- Pregabalin
- Primidone
- Propofol
- Remimazolam
- Scopolamine
- Secobarbital
- Sodium Oxybate
- Sufentanil
- Tapentadol
- Thiopental
- Tramadol
- Trazodone
- Zolpidem
Using clonazepam with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Amiodarone
- Desipramine
- Ginkgo
- Nevirapine
- Rifapentine
- Ritonavir
- St John’s Wort
- Theophylline
Other interactions
Using clonazepam with any of the following is usually not recommended, but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use clonazepam, or give you special instructions about the use of food, alcohol, or tobacco.
- Ethanol
Other medical problems
The presence of other medical problems may affect the use of clonazepam. Make sure you tell your doctor if you have any other medical problems, especially:
- Alcohol or drug abuse or dependence, or history of or
- Depression, history of or
- Lung or breathing problems or
- Porphyria—Use with caution. May make these conditions worse.
- Glaucoma, narrow angle, acute or
- Liver disease—Should not be used in patients with these conditions.
- Kidney disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
Clonazepam uses
Clonazepam is a benzodiazepine that works in the brain to prevent seizures. Clonazepam is used alone or in combination with other medications to control certain types of seizures (eg, Lennox-Gastaut syndrome, akinetic, myoclonic, and absence seizures). Clonazepam is also used to treat panic disorder to relieve panic attacks (sudden, unexpected attacks of extreme fear and worry about these attacks).
Clonazepam dosage
The dose of clonazepam will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of clonazepam. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
For oral dosage forms (tablets or disintegrating tablets)
For seizures
- Adults and children 10 years and older—At first, 0.5 milligram (mg) 3 times per day. Your doctor may adjust your dose as needed. However, the dose is usually not more than 20 mg per day.
- Children up to 10 years or 30 kilograms (kg) of body weight—Dose is based on body weight and must be determined by your doctor. The dose is usually 0.01 to 0.03 mg per kg of body weight per day, given in 2 or 3 divided doses. However, the dose is usually not more than 0.05 mg per kg of body weight. Your doctor may adjust your dose as needed.
For panic disorder:
- Adults—At first, 0.25 milligram (mg) 2 times per day. Your doctor may adjust your dose as needed. However, the dose is usually not more than 4 mg per day.
- Children—Use and dose must be determined by your doctor.
Missed dose
If you miss a dose of clonazepam, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not double doses.
Clonazepam side effects
Clonazepam may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- drowsiness
- dizziness
- unsteadiness
- problems with coordination
- difficulty thinking or remembering
- increased saliva
- muscle or joint pain
- frequent urination
- blurred vision
- changes in sex drive or ability
Some side effects can be serious. If you experience any of these symptoms or those listed in the IMPORTANT WARNING section, call your doctor immediately or get emergency medical treatment:
- rash
- hives
- swelling of the eyes, face, lips, tongue, or throat
- difficulty breathing or swallowing
- hoarseness
- difficulty breathing.
Clorazepate
Clorazepate (Tranxene T-Tab or Tranxene SD) is a benzodiazepine that is used to treat anxiety disorders, partial seizures, or alcohol withdrawal symptoms. Clorazepate is available only with your doctor’s prescription.
Clorazepate comes as a tablet to take by mouth. It is usually taken one to three times a day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take clorazepate exactly as directed.
If you are taking clorazepate to treat anxiety or seizures, your doctor will probably start you on a low dose of clorazepate and gradually increase your dose. If you are taking clorazepate to treat alcohol withdrawal, your doctor will probably start you on a high dose of clorazepate and gradually decrease your dose as your symptoms are controlled.
Clorazepate may help to control seizures and anxiety, but it will not cure these conditions. Continue to take clorazepate even if you feel well.
Clorazepate may increase the risk of serious or life-threatening breathing problems, sedation, or coma if used along with certain medications. Tell your doctor if you are taking or plan to take certain opiate medications for cough such as codeine (in Triacin-C, in Tuzistra XR) or hydrocodone (in Anexsia, in Norco, in Zyfrel) or for pain such as codeine (in Fiorinal), fentanyl (Actiq, Duragesic, Subsys, others), hydromorphone (Dilaudid, Exalgo), meperidine (Demerol), methadone (Dolophine, Methadose), morphine (Astramorph, Duramorph PF, Kadian), oxycodone (in Oxycet, in Percocet, in Roxicet, others), and tramadol (Conzip, Ultram, in Ultracet). Your doctor may need to change the dosages of your medications and will monitor you carefully. If you take clorazepate with any of these medications and you develop any of the following symptoms, call your doctor immediately or seek emergency medical care immediately: unusual dizziness, lightheadedness, extreme sleepiness, slowed or difficult breathing, or unresponsiveness. Be sure that your caregiver or family members know which symptoms may be serious so they can call the doctor or emergency medical care if you are unable to seek treatment on your own.
Clorazepate may be habit forming. Do not take a larger dose, take it more often, or for a longer time than your doctor tells you to. Tell your doctor if you have ever drunk large amounts of alcohol, if you use or have ever used street drugs, or have overused prescription medications. Do not drink alcohol or use street drugs during your treatment. Drinking alcohol or using street drugs during your treatment with clorazepate also increases the risk that you will experience these serious, life-threatening side effects. Also tell your doctor if you have or have ever had depression or another mental illness.
Clorazepate may cause a physical dependence (a condition in which unpleasant physical symptoms occur if a medication is suddenly stopped or taken in smaller doses), especially if you take it for several days to several weeks. Do not stop taking this medication or take fewer doses without talking to your doctor. Stopping clorazepate suddenly can worsen your condition and cause withdrawal symptoms that may last for several weeks to more than 12 months. Your doctor probably will decrease your clorazepate dose gradually. Call your doctor or get emergency medical treatment if you experience any of the following symptoms: unusual movements; ringing in your ears; anxiety; memory problems; difficulty concentrating; sleep problems; seizures; shaking; muscle twitching; changes in mental health; depression; burning or prickling feeling in hands, arms, legs or feet; seeing or hearing things that others do not see or hear; thoughts of harming or killing yourself or others; overexcitement; or losing touch with reality.
Clorazepate special precautions
You should not use clorazepate if you are allergic to it, or if you have:
- narrow-angle glaucoma.
Tell your doctor if you have ever had:
- liver or kidney disease;
- mood problems, depression, psychosis; or
- suicidal thoughts or actions.
Some people have thoughts about suicide while taking clorazepate. Stay alert to changes in your mood or symptoms. Your family or caregivers should also watch for sudden changes in your behavior.
Tell your doctor if you are pregnant or plan to become pregnant. Clorazepate may harm an unborn baby. Avoid taking this medicine during the first trimester of pregnancy.
If you use clorazepate during pregnancy, your baby could be born with life-threatening withdrawal symptoms, and may need medical treatment for several weeks.
If you take clorazepate for seizures, do not start or stop taking it during pregnancy without your doctor’s advice. Having a seizure during pregnancy could harm both mother and baby.
Do not breastfeed whilst taking clorazepate.
Clorazepate is not approved for use by anyone younger than 9 years old.
Before taking clorazepate:
- tell your doctor and pharmacist if you are allergic to clorazepate; other benzodiazepines such as alprazolam ( Xanax), chlordiazepoxide (Librium, in Librax), clonazepam (Klonopin), diazepam (Diastat, Valium), estazolam, flurazepam, lorazepam (Ativan), oxazepam, temazepam (Restoril), or triazolam (Halcion); any other medications; or any of the ingredients in clorazepate tablets. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: barbiturates such as phenobarbital and secobarbital (Seconal); chlorpromazine; cimetidine (Tagamet); disulfiram (Antabuse); levodopa (in Ritary, in Sinemet, in Stalevo); or monoamine oxidase inhibitors such as isocarboxazid (Marplan), linezolid (Zyvox), phenelzine (Nardil), selegiline (Eldepryl, Emsam, Zelapar), and tranylcypromine (Parnate); medications for depression, nausea, mental illness, and seizures; sedatives; sleeping pills; and tranquilizers.Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have or have ever had glaucoma. Your doctor may tell you not to take clorazepate.
- tell your doctor if you have or have ever had liver or kidney disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking clorazepate, call your doctor.
- talk to your doctor about the risks and benefits of taking clorazepate if you are 65 years of age or older. Older adults should not usually take clorazepate because it is not as safe or effective as other medications that can be used to treat the same condition.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking clorazepate.
- you should know that this medication may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
- you should know that your mental health may change in unexpected ways, and you may become suicidal (thinking about harming or killing yourself or planning or trying to do so) while you are taking clorazepate for the treatment of epilepsy, mental illness, or other conditions A small number of adults and children 5 years of age and older (about 1 in 500 people) who took anticonvulsants such as clorazepate to treat various conditions during clinical studies became suicidal during their treatment. Some of these people developed suicidal thoughts and behavior as early as one week after they started taking the medication. There is a risk that you may experience changes in your mental health if you take an anticonvulsant medication such as clorazepate, but there may also be a risk that you will experience changes in your mental health if your condition is not treated. You and your doctor will decide whether the risks of taking an anticonvulsant medication are greater than the risks of not taking the medication. You, your family, or your caregiver should call your doctor right away if you experience any of the following symptoms: panic attacks; agitation or restlessness; new or worsening irritability, anxiety, or depression; acting on dangerous impulses; difficulty falling or staying asleep; aggressive, angry, or violent behavior; mania (frenzied, abnormally excited mood), talking or thinking about wanting to hurt yourself or end your life, withdrawing from friends and family; preoccupation with death and dying, giving away prized possessions, or any other unusual changes in behavior or mood. Be sure that your family or caregiver knows which symptoms may be serious so they can call the doctor if you are unable to seek treatment on your own.
Special dietary instructions
Unless your doctor tells you otherwise, continue your normal diet.
Clorazepate drug interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking clorazepate, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using clorazepate with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Flumazenil
Using clorazepate with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Alfentanil
- Alprazolam
- Amobarbital
- Benzhydrocodone
- Bromazepam
- Bromopride
- Buprenorphine
- Butabarbital
- Butalbital
- Butorphanol
- Calcifediol
- Calcium Oxybate
- Cannabidiol
- Carbinoxamine
- Carisoprodol
- Cetirizine
- Chloral Hydrate
- Chlorzoxazone
- Clobazam
- Codeine
- Dantrolene
- Dihydrocodeine
- Doxylamine
- Esketamine
- Ethchlorvynol
- Fentanyl
- Flibanserin
- Fospropofol
- Gabapentin
- Gabapentin Enacarbil
- Hydrocodone
- Hydromorphone
- Ketamine
- Lemborexant
- Levocetirizine
- Levorphanol
- Lofexidine
- Loxapine
- Magnesium Oxybate
- Meclizine
- Meperidine
- Mephenesin
- Mephobarbital
- Meprobamate
- Metaxalone
- Methadone
- Methocarbamol
- Methohexital
- Metoclopramide
- Midazolam
- Mirtazapine
- Morphine
- Morphine Sulfate Liposome
- Nalbuphine
- Omeprazole
- Orlistat
- Oxycodone
- Oxymorphone
- Pentazocine
- Pentobarbital
- Periciazine
- Phenobarbital
- Potassium Oxybate
- Pregabalin
- Primidone
- Propofol
- Remimazolam
- Scopolamine
- Secobarbital
- Sodium Oxybate
- Sufentanil
- Tapentadol
- Thiopental
- Tramadol
- Trazodone
- Zolpidem
Using clorazepate with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Amprenavir
- Ginkgo
- Rifapentine
- St John’s Wort
- Theophylline
Other medical problems
The presence of other medical problems may affect the use of clorazepate. Make sure you tell your doctor if you have any other medical problems, especially:
- Alcohol or drug abuse or dependence, or history of or
- Depression, history of or
- Lung or breathing problems (eg, respiratory depression) or
- Mental health problems, history of—Use with caution. May make these conditions worse.
- Glaucoma, narrow angle—Should not be used in patients with this condition.
- Kidney disease or
- Liver disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
Clorazepate uses
Clorazepate is used to relieve symptoms of anxiety. Clorazepate is also used along with other medications to treat partial seizures. Clorazepate is also used to relieve unpleasant symptoms that may be experienced by people who have stopped drinking alcohol after drinking large amounts for a long time.
Clorazepate dosage
The dose of clorazepate will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of clorazepate. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
For oral dosage form (tablets)
- For anxiety:
- Adults—30 milligrams (mg) per day, taken in divided doses. Your doctor may adjust your dose if needed.
- Older adults—At first, 7.5 to 15 mg per day, taken at bedtime or in divided doses. Your doctor may increase your dose if needed.
- Children—Use and dose must be determined by your doctor.
- For symptoms of alcohol withdrawal:
- Adults—At first, 30 milligrams (mg), followed by 30 to 60 mg in divided doses. Your doctor will set up a schedule that will gradually adjust your dose until your symptoms improve. The dose is usually not more than 90 mg per day.
- Children—Use and dose must be determined by your doctor.
- For partial seizures:
- Adults and children 13 years of age and older—At first, 7.5 milligrams (mg) 3 times a day. Your doctor may increase your dose as needed. However, the dose is usually not more than 90 mg per day.
- Children 9 to 12 years of age—The starting dose is up to 7.5 mg 2 times a day. Your doctor may increase your dose as needed. However, the dose is usually not more than 60 mg per day.
- Children up to 9 years of age—Use is not recommended.
Missed dose
Take the missed dose as soon as you remember. However, if it is almost time for your next dose, skip the missed dose and continue your regular dosing schedule.
Clorazepate side effects
Clorazepate may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- drowsiness
- dizziness
- tiredness
- headache
- nervousness
- confusion
- dry mouth
Some side effects can be serious. If you experience any of the following symptoms or those listed in the IMPORTANT WARNING section, call your doctor immediately or get emergency medical treatment:
- blurred or double vision
- uncontrollable shaking of a part of the body
- slurred speech
- difficulty keeping your balance
- rash
Clorazepate may cause other side effects. Call your doctor if you have any unusual problems while you are taking clorazepate.
Diazepam
Diazepam (Valium) is a benzodiazepine that is used to treat anxiety disorders or alcohol withdrawal symptoms. Diazepam is sometimes also used with other medications to treat muscle spasms and stiffness, or control seizures (eg, seizure clusters, acute repetitive seizures) in patients who have epilepsy. Diazepam is sometimes prescribed for other uses; ask your doctor or pharmacist for more information. Diazepam is available only with your doctor’s prescription.
Diazepam comes as a tablet, a solution, and as a concentrate (liquid) to take by mouth. It is usually taken 1 to 4 times a day and may be taken with or without food. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take diazepam exactly as directed.
Diazepam concentrate comes with a specially marked dropper for measuring the dose. Ask your pharmacist to show you how to use the dropper. Dilute the concentrate in water, juice, or carbonated beverages just before taking it. It also may be mixed with applesauce or pudding just before taking the dose. Stir the mixture gently for a few seconds. Take the entire mixture immediately; do not store it for future use.
If you are taking diazepam along with other medications to control seizures, do not stop taking diazepam without talking to your doctor, even if you experience side effects such as unusual changes in behavior or mood. If you suddenly stop taking diazepam, your seizures may get worse. Your doctor will probably decrease your dose gradually.
Diazepam may increase the risk of serious or life-threatening breathing problems, sedation, or coma if used along with certain medications. Tell your doctor if you are taking or plan to take certain opiate medications for cough such as codeine (in Triacin-C, in Tuzistra XR) or hydrocodone (in Anexsia, in Norco, in Zyfrel) or for pain such as codeine (in Fiorinal), fentanyl (Actiq, Duragesic, Subsys, others), hydromorphone (Dilaudid, Exalgo), meperidine (Demerol), methadone (Dolophine, Methadose), morphine (Astramorph, Duramorph PF, Kadian), oxycodone (in Oxycet, in Percocet, in Roxicet, others), and tramadol (Conzip, Ultram, in Ultracet). Your doctor may need to change the dosages of your medications and will monitor you carefully. If you take diazepam with any of these medications and you develop any of the following symptoms, call your doctor immediately or seek emergency medical care immediately: unusual dizziness, lightheadedness, extreme sleepiness, slowed or difficult breathing, or unresponsiveness. Be sure that your caregiver or family members know which symptoms may be serious so they can call the doctor or emergency medical care if you are unable to seek treatment on your own.
Diazepam may be habit forming. Do not take a larger dose, take it more often, or for a longer time than your doctor tells you to. Tell your doctor if you have ever drunk large amounts of alcohol, if you use or have ever used street drugs, or have overused prescription medications. Do not drink alcohol or use street drugs during your treatment. Drinking alcohol or using street drugs during your treatment with diazepam also increases the risk that you will experience these serious, life-threatening side effects. Also tell your doctor if you have or have ever had depression or another mental illness.
Diazepam may cause a physical dependence (a condition in which unpleasant physical symptoms occur if a medication is suddenly stopped or taken in smaller doses), especially if you take it for several days to several weeks. Do not stop taking this medication or take fewer doses without talking to your doctor. Stopping diazepam suddenly can worsen your condition and cause withdrawal symptoms that may last for several weeks to more than 12 months. Your doctor probably will decrease your diazepam dose gradually. Call your doctor or get emergency medical treatment if you experience any of the following symptoms: unusual movements; ringing in your ears; anxiety; memory problems; difficulty concentrating; sleep problems; seizures; shaking; muscle twitching; changes in mental health; depression; burning or prickling feeling in your hands, arms, legs or feet; seeing or hearing things that others do not see or hear; thoughts of harming or killing yourself or others; overexcitement; or losing touch with reality.
Diazepam special precautions
You should NOT use diazepam if you are allergic to it, or if you have:
- myasthenia gravis (a muscle weakness disorder);
- a severe breathing problem;
- sleep apnea (breathing stops during sleep);
- narrow-angle glaucoma;
- untreated or uncontrolled open-angle glaucoma; or
- severe liver disease.
Diazepam should NOT be given to a child younger than 6 months old. Do NOT give diazepam to a child without a doctor’s advice.
Diazepam may harm an unborn baby. Do not use if you are pregnant or may become pregnant. If you use diazepam during pregnancy, your baby could be born with life-threatening withdrawal symptoms, and may need medical treatment for several weeks. However, do not start or stop seizure medication during pregnancy without your doctor’s advice. Diazepam may harm an unborn baby, but having a seizure during pregnancy could harm both mother and baby. Preventing seizures may outweigh these risks. Tell your doctor right away if you become pregnant. There may be other seizure medications that are safer to use during pregnancy. You should not breastfeed whilst taking diazepam.
Do not stop using diazepam without asking your doctor. You may have increased seizures or life-threatening withdrawal symptoms if you stop using the medicine suddenly after long-term use.
To make sure diazepam is safe for you, tell your doctor if you have ever had:
- breathing problems;
- glaucoma;
- kidney or liver disease;
- seizures (unless you are taking diazepam to treat a seizure disorder);
- a drug or alcohol addiction; or
- depression, a mood disorder, or suicidal thoughts or behavior.
Some people have thoughts about suicide while taking diazepam. Stay alert to changes in your mood or symptoms. Your family or caregivers should also watch for sudden changes in your behavior.
Before taking diazepam:
- tell your doctor and pharmacist if you are allergic to diazepam, alprazolam (Xanax), chlordiazepoxide (Librium, in Librax), clonazepam (Klonopin), clorazepate (Gen-Xene, Tranxene), estazolam, flurazepam, lorazepam (Ativan), oxazepam, temazepam (Restoril), triazolam (Halcion), any other medications, or any of the ingredients in diazepam products. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, and nutritional supplements, you are taking. Be sure to mention any of the following: antihistamines; barbiturates such as phenobarbital (Luminal); cimetidine (Tagamet); digoxin (Lanoxin); disulfiram (Antabuse); fluoxetine (Prozac); fluvoxamine (Luvox); isoniazid (Laniazid, in Rifamate, in Rifater); ketoconazole; medications for anxiety, depression, mental illness, seizures, Parkinson’s disease, asthma, colds, or allergies; metoprolol (Lopressor, Toprol XL); monoamine oxidase (MAO) inhibitors including isocarboxazid (Marplan), linezolid (Zyvox), methylene blue, phenelzine (Nardil), selegiline (Eldepryl, Emsam, Zelapar), and tranylcypromine (Parnate); muscle relaxants; phenothiazine medications for mental illness or nausea such as chlorpromazine, fluphenazine, prochlorperazine (Compro, Procomp), and promethazine (Promethegan); omeprazole (Prilosec); probenecid (Probalan, in Col-Probenecid); propranolol (Hemangeol, Inderal, Innopran); ranitidine (Zantac); rifampin (Rifadin, Rimactane, in Rifamate, in Rifater); sedatives; sleeping pills; theophylline (Elixophyllin, Theo 24, Theochron); tranquilizers; or valproic acid (Depakene). Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have myasthenia gravis (a disorder of the nervous system that causes muscle weakness), sleep apnea (condition in which a person briefly stops breathing many times during the night), or lung or liver disease. Also, tell your doctor if you have narrow angle glaucoma (a serious eye condition that may cause loss of vision. Your doctor will probably tell you not to take diazepam. Diazepam should not be used in infants younger than 6 months of age.
- tell your doctor if you have or have ever had open-angle glaucoma (increase in internal eye pressure that damages the optic nerve); depression or other mental illness; seizures; or heart disease.
- tell your doctor if you are pregnant or plan to become pregnant. If you become pregnant while taking diazepam, call your doctor immediately.
- tell your doctor if you are breastfeeding. Do not breastfeed while you are taking diazepam.
- talk to your doctor about the risks and benefits of taking diazepam if you are 65 years of age or older. Older adults should not usually take diazepam because it is not as safe as other medications that can be used to treat the same conditions.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking diazepam.
- you should know that this drug may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
- you should know that your mental health may change in unexpected ways and you may become suicidal (thinking about harming or killing yourself or planning or trying to do so) while you are taking diazepam for the treatment of epilepsy. A small number of adults and children 5 years of age and older (about 1 in 500 people) who took anticonvulsants such as diazepam to treat various conditions during clinical studies became suicidal during their treatment. Some of these people developed suicidal thoughts and behavior as early as one week after they started taking the medication. There is a risk that you may experience changes in your mental health if you take an anticonvulsant medication such as diazepam, but there may also be a risk that you will experience changes in your mental health if your condition is not treated. You and your doctor will decide whether the risks of taking an anticonvulsant medication are greater than the risks of not taking the medication. You, your family, or your caregiver should call your doctor right away if you experience any of the following symptoms: panic attacks; agitation or restlessness; new or worsening irritability, anxiety, or depression; acting on dangerous impulses; difficulty falling or staying asleep; aggressive, angry, or violent behavior; mania (frenzied, abnormally excited mood); talking or thinking about wanting to hurt yourself or end your life; withdrawing from friends and family; preoccupation with death and dying; giving away prized possessions; or any other unusual changes in behavior or mood. Be sure that your family or caregiver knows which symptoms may be serious so they can call the doctor if you are unable to seek treatment on your own.
Special dietary instructions
Do not eat grapefruit or drink grapefruit juice while you’re taking diazepam.
Diazepam drug interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are receiving diazepam, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using diazepam with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Flumazenil
Using diazepam with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Abametapir
- Alfentanil
- Alprazolam
- Amobarbital
- Anileridine
- Benzhydrocodone
- Bromazepam
- Bromopride
- Buprenorphine
- Butabarbital
- Butalbital
- Butorphanol
- Calcifediol
- Calcium Oxybate
- Cannabidiol
- Carbinoxamine
- Carisoprodol
- Cetirizine
- Chloral Hydrate
- Chlorzoxazone
- Clobazam
- Cobicistat
- Codeine
- Conivaptan
- Dantrolene
- Diacetylmorphine
- Difenoxin
- Dihydrocodeine
- Diphenoxylate
- Doxylamine
- Esketamine
- Eslicarbazepine Acetate
- Ethchlorvynol
- Ethylmorphine
- Etravirine
- Fentanyl
- Fexinidazole
- Flibanserin
- Fosnetupitant
- Fosphenytoin
- Fospropofol
- Gabapentin
- Gabapentin Enacarbil
- Hydrocodone
- Hydromorphone
- Ketamine
- Ketobemidone
- Lemborexant
- Levocetirizine
- Levorphanol
- Lofexidine
- Loxapine
- Magnesium Oxybate
- Meclizine
- Meperidine
- Mephenesin
- Mephobarbital
- Meprobamate
- Metaxalone
- Methadone
- Methocarbamol
- Methohexital
- Metoclopramide
- Midazolam
- Mirtazapine
- Morphine
- Morphine Sulfate Liposome
- Nalbuphine
- Netupitant
- Nicomorphine
- Opium
- Opium Alkaloids
- Orlistat
- Oxycodone
- Oxymorphone
- Papaveretum
- Paregoric
- Pentazocine
- Pentobarbital
- Periciazine
- Phenobarbital
- Phenytoin
- Piritramide
- Potassium Oxybate
- Pregabalin
- Primidone
- Propofol
- Remifentanil
- Remimazolam
- Scopolamine
- Secobarbital
- Sodium Oxybate
- Sufentanil
- Tapentadol
- Thiopental
- Tilidine
- Tramadol
- Trazodone
- Zolpidem
Using diazepam with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Amitriptyline
- Amprenavir
- Clarithromycin
- Dalfopristin
- Desogestrel
- Dienogest
- Disulfiram
- Drospirenone
- Erythromycin
- Estradiol
- Ethinyl Estradiol
- Ethynodiol
- Fluvoxamine
- Gestodene
- Ginkgo
- Isoniazid
- Levonorgestrel
- Mestranol
- Nomegestrol
- Norethindrone
- Norgestimate
- Norgestrel
- Quinupristin
- Rifapentine
- Roxithromycin
- St John’s Wort
- Theophylline
- Troleandomycin
Other medical problems
The presence of other medical problems may affect the use of diazepam. Make sure you tell your doctor if you have any other medical problems, especially:
- Alcohol and drug abuse or dependence, or history of—Dependence on diazepam may develop.
- Glaucoma, acute narrow angle—Should not be used in patients with this condition.
- Glaucoma, open angle or
Lung or breathing problems (eg, asthma, pneumonia)—Use with caution. May make these conditions worse. - Kidney disease or
- Liver disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
Diazepam uses
Diazepam is used to relieve anxiety and to control agitation caused by alcohol withdrawal. Diazepam is also used along with other medications to control muscle spasms and spasticity caused by certain neurological disorders such as cerebral palsy (condition that causes difficulty with movement and balance), paraplegia (inability to move parts of the body), athetosis (abnormal muscle contractions), and stiff-man syndrome (a rare disorder with muscle rigidity and stiffness). Diazepam is also used along with other medications to control seizures.
Diazepam dosage
The dose of diazepam will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of diazepam. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
Adult dose for Anxiety
Use: Management of anxiety disorders and short-term relief of anxiety symptoms
- Oral: 2 to 10 mg orally 2 to 4 times a day
- Parenteral:
- Moderate Anxiety Disorders and Symptoms: 2 to 5 mg IM or IV, repeated in 3 to 4 hours if necessary
- Severe Anxiety Disorders and Symptoms: 5 to 10 mg IM or IV, repeated in 3 to 4 hours if necessary
Comments:
- Oral doses should be determined by the severity of symptoms.
- Anxiety associated with the stress of everyday life usually does not require treatment with this drug.
Adult dose for Muscle Spasm
Use: Adjunctive treatment for the relief of skeletal muscle spasm due to reflex spasm to local pathology, spasticity caused by upper motor neuron disorders, athetosis, and stiff-man syndrome (e.g., inflammation of the muscles/joints secondary to trauma, cerebral palsy, paraplegia)
- Oral: 2 to 10 mg orally 3 to 4 times a day
- Parenteral: 5 to 10 mg IM or IV, then 5 to 10 mg IM or IV in 3 to 4 hours if necessary
Comment: Larger parenteral doses may be necessary for patients with tetanus.
Adult dose for Alcohol Withdrawal
Use: Symptomatic relief of acute agitation, tremor, impending/acute delirium tremens, and hallucinations in acute alcohol withdrawal
- Oral:
- Initial dose: 10 mg orally 3 to 4 times a day for the first 24 hours
- Maintenance dose: 5 mg orally 3 to 4 times a day as needed
- Parenteral: 10 mg IM or IV once, then 5 to 10 mg IM or IV in 3 to 4 hours if necessary
Adult dose for Seizures
Uses:
- Management of selected, refractory patients with epilepsy on stable regimens of antiepileptic drugs who require intermittent use of diazepam to control bouts of increased seizure activity
- Adjunctive treatment for convulsive disorders
Oral: 2 to 10 mg orally 2 to 4 times a day
Rectal:
- Initial dose: 0.2 mg/kg rectally, rounded upward to the next available dose. A 2.5 mg rectal dose may be given as a partial replacement if patients expel a portion of the initial dose
- If necessary, a second dose of 0.2 mg/kg may be given rectally 4 to 12 hours after the first dose.
- Maximum Frequency: May be used to treat up to 1 seizure episode every 5 days, and no more than 5 episodes/month
Adult dose for Status Epilepticus
Use: Adjunct to status epilepticus and severe recurrent convulsive seizures
Parenteral:
- Initial dose: 5 to 10 mg IV once, repeated at 10 to 15 minute intervals to a maximum dose of 30 mg if necessary
Comments:
- The IV route is preferred; however, the IM route may be used if IV administration is impossible.
- Treatment may be repeated every 2 to 4 hours, but active metabolites may persist during readministration.
- Patients with chronic lung disease or unstable cardiovascular conditions should be given this drug with extreme caution.
Geriatric dose for Seizures
Uses:
- Management of selected, refractory patients with epilepsy on stable regimens of antiepileptic drugs who require intermittent use of this drug to control bouts of increased seizure activity
- Adjunctive treatment in convulsive disorders
Oral:
- Initial dose: 2 to 2.5 mg orally once to 2 times a day
Rectal:
- Initial dose: 0.2 mg/kg rectally, rounded downward to the next available dose. A 2.5 mg rectal dose may be given as a partial replacement if patients expel a portion of the initial dose
- If necessary, a second dose of 0.2 mg/kg may be given rectally 4 to 12 hours after the first dose.
- Maximum Frequency: May be used to treat up to 1 seizure episode every 5 days, and no more than 5 episodes/month
Comment: Oral doses may be increased gradually as needed and tolerated, but should be limited to the smallest effective amount
Geriatric dose for Alcohol Withdrawal
Uses:
- Management of anxiety disorders and short-term relief of anxiety symptoms
- Symptomatic relief of acute agitation, tremor, impending/acute delirium tremens, and hallucinations in acute alcohol withdrawal
- Adjunctive treatment for the relief of skeletal muscle spasm due to reflex spasm to local pathology, spasticity caused by upper motor neuron disorders, athetosis, and stiff-man syndrome (e.g., inflammation of the muscles/joints secondary to trauma, cerebral palsy, paraplegia)
Oral:
- Initial dose: 2 to 2.5 mg orally once to 2 times a day
Parenteral:
- Initial dose: 2 to 5 mg IM or IV, repeated in 3 to 4 hours if necessary
Comments:
- Doses may be increased gradually as needed and tolerated, but should be limited to the smallest effective amount.
- Maintenance doses should be determined by clinical need and patient tolerance.
Geriatric dose for Anxiety
Uses:
- Management of anxiety disorders and short-term relief of anxiety symptoms
- Symptomatic relief of acute agitation, tremor, impending/acute delirium tremens, and hallucinations in acute alcohol withdrawal
- Adjunctive treatment for the relief of skeletal muscle spasm due to reflex spasm to local pathology, spasticity caused by upper motor neuron disorders, athetosis, and stiff-man syndrome (e.g., inflammation of the muscles/joints secondary to trauma, cerebral palsy, paraplegia)
Oral:
- Initial dose: 2 to 2.5 mg orally once to 2 times a day
Parenteral:
- Initial dose: 2 to 5 mg IM or IV, repeated in 3 to 4 hours if necessary
Comments:
- Doses may be increased gradually as needed and tolerated, but should be limited to the smallest effective amount.
- Maintenance doses should be determined by clinical need and patient tolerance.
Geriatric dose for Muscle Spasm
Uses:
- Management of anxiety disorders and short-term relief of anxiety symptoms
- Symptomatic relief of acute agitation, tremor, impending/acute delirium tremens, and hallucinations in acute alcohol withdrawal
- Adjunctive treatment for the relief of skeletal muscle spasm due to reflex spasm to local pathology, spasticity caused by upper motor neuron disorders, athetosis, and stiff-man syndrome (e.g., inflammation of the muscles/joints secondary to trauma, cerebral palsy, paraplegia)
Oral:
- Initial dose: 2 to 2.5 mg orally once to 2 times a day
Parenteral:
- Initial dose: 2 to 5 mg IM or IV, repeated in 3 to 4 hours if necessary
Comments:
- Doses may be increased gradually as needed and tolerated, but should be limited to the smallest effective amount.
- Maintenance doses should be determined by clinical need and patient tolerance.
Adult dose for Light Anesthesia
Use: Premedication for the relief of anxiety and tension in patients undergoing surgical procedures
Parenteral:
- Preoperative Medication: 10 mg IM once before surgery
Comments:
- The IM route is preferred when given as a preoperative medication.
- Atropine, scopolamine, and other premedications should be administered in separate syringes.
Adult dose for Endoscopy or Radiology Premedication
Uses:
- Adjunct prior to endoscopic procedures if apprehension, anxiety, or acute stress reactions are present and to diminish recall of the procedures
- Prior to cardioversion for the relief of anxiety and tension and to diminish the patient’s recall of the procedure
Parenteral:
- Cardioversion: 5 to 15 mg IV once 5 to 10 minutes before the procedure
Endoscopic Procedures:
- IV: Usually less than 10 mg, but some patients require up to 20 mg IV, especially when narcotics are omitted
- IV titration: The IV dose should be titrated to desired sedative response (e.g., slurring of speech) with slow administration immediately before the procedure.
- IM: 5 to 10 mg IM once 30 minutes prior to the procedure
Comments:
- Narcotic dosing should be reduced by approximately 33%, and may be omitted in some patients.
- The IV route is preferred, but IM administration may be used if IV administration is not possible.
Pediatric dose for Seizures
Uses:
- Management of selected, refractory patients with epilepsy on stable regimens of antiepileptic drugs who require intermittent use of this drug to control bouts of increased seizure activity
- Adjunctive treatment in convulsive disorders
Oral:
- 6 months and older:
- Initial dose: 1 to 2.5 mg orally 3 to 4 times a day
Rectal:
- 2 to 5 years:
- Initial dose: 0.5 mg/kg rectally, rounded upward to the next available dose. A 2.5 mg rectal dose may be given as a partial replacement if patients expel a portion of the initial dose
- If necessary, a second dose of 0.5 mg/kg may be given rectally 4 to 12 hours after the first dose.
- Maximum Frequency: 1 episode every 5 days, and no more than 5 episodes/month
- 6 to 11 years:
- Initial dose: 0.3 mg/kg rectally, rounded upward to the next available dose. A 2.5 mg rectal dose may be given as a partial replacement if patients expel a portion of the initial dose
- If necessary, a second dose of 0.3 mg/kg may be given rectally 4 to 12 hours after the first dose.
- Maximum Frequency: 1 episode every 5 days, and no more than 5 episodes/month
- 12 years and older:
- Initial dose: 0.2 mg/kg rectally, rounded upward to the next available dose. A 2.5 mg rectal dose may be given as a partial replacement if patients expel a portion of the initial dose
- If necessary, a second dose of 0.2 mg/kg may be given rectally 4 to 12 hours after the first dose.
- Maximum Frequency: May be used to treat up to 1 seizure episode every 5 days, and no more than 5 episodes/month
Comment: Oral doses may be increased gradually as needed and tolerated, but should be limited to the smallest effective amount.
Pediatric dose for Status Epilepticus
Use: Adjunct in status epilepticus and severe recurrent convulsive seizures
Parenteral:
- IV Injection:
- 30 days to less than 5 years: 0.2 to 0.5 mg slow IV injection every 2 to 5 minutes, up to a maximum dose of 5 mg. Repeat in 2 to 4 hours if needed.
- 5 years and older: 1 mg slow IV injection every 2 to 5 minutes, up to a maximum dose of 10 mg. Repeat in 2 to 4 hours if needed.
Comment: EEG monitoring may be helpful to monitor seizure activity.
Pediatric dose for Seizure Prophylaxis
Uses:
- Management of anxiety disorders and short-term relief of anxiety symptoms
- Symptomatic relief of acute agitation, tremor, impending/acute delirium tremens, and hallucinations in acute alcohol withdrawal
- Adjunctive treatment for the relief of skeletal muscle spasm due to reflex spasm to local pathology, spasticity caused by upper motor neuron disorders, athetosis, and stiff-man syndrome (e.g., inflammation of the muscles/joints secondary to trauma, cerebral palsy, paraplegia)
Oral:
- 6 months and older:
- Initial dose: 1 to 2.5 mg orally 3 to 4 times a day
Comments:
- Doses may be increased gradually as needed and tolerated, but should be limited to the smallest effective amount.
- Maintenance doses should be determined by clinical need and patient tolerance.
Pediatric dose for Muscle Spasm
Uses:
- Management of anxiety disorders and short-term relief of anxiety symptoms
- Symptomatic relief of acute agitation, tremor, impending/acute delirium tremens, and hallucinations in acute alcohol withdrawal
- Adjunctive treatment for the relief of skeletal muscle spasm due to reflex spasm to local pathology, spasticity caused by upper motor neuron disorders, athetosis, and stiff-man syndrome (e.g., inflammation of the muscles/joints secondary to trauma, cerebral palsy, paraplegia)
Oral:
- 6 months and older:
- Initial dose: 1 to 2.5 mg orally 3 to 4 times a day
Comments:
- Doses may be increased gradually as needed and tolerated, but should be limited to the smallest effective amount.
- Maintenance doses should be determined by clinical need and patient tolerance.
Pediatric dose for Tetanus
Use: Tetanus
Parenteral:
- 30 days to 5 years: 1 to 2 mg IM or slow IV injection, repeated every 3 to 4 hours as necessary
- 5 years and older: 5 to 10 mg IM or slow IV injection, repeated every 3 to 4 hours as necessary to control spasms
Comment: Respiratory assistance should be available for patients.
Pediatric dose for Anxiety
Uses:
- Management of anxiety disorders and short-term relief of anxiety symptoms
- Symptomatic relief of acute agitation, tremor, impending/acute delirium tremens, and hallucinations in acute alcohol withdrawal
- Adjunctive treatment for the relief of skeletal muscle spasm due to reflex spasm to local pathology, spasticity caused by upper motor neuron disorders, athetosis, and stiff-man syndrome (e.g., inflammation of the muscles/joints secondary to trauma, cerebral palsy, paraplegia)
Oral:
- 6 months and older:
- Initial dose: 1 to 2.5 mg orally 3 to 4 times a day
Comments:
- Doses may be increased gradually as needed and tolerated, but should be limited to the smallest effective amount.
- Maintenance doses should be determined by clinical need and patient tolerance.
Missed dose
Take diazepam as soon as you can, but skip the missed dose if it is almost time for your next dose. Do not take two doses at one time.
Diazepam side effects
Diazepam may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- drowsiness
- dizziness
- tiredness
- muscle weakness
- headache
- dry mouth
- nausea
- constipation
- confusion
- difficulty urinating
- frequent urination
- changes in sex drive or ability
Some side effects can be serious. If you experience any of these symptoms or those listed in the IMPORTANT WARNING section, call your doctor immediately or get emergency medical treatment:
- loss of control of bodily movements
- uncontrollable shaking of a part of the body
- slurred speech
- slowed breathing and heartbeat
Diazepam may cause other side effects. Call your doctor if you have any unusual problems while taking diazepam.
Estazolam
Estazolam (Eurodin or ProSom) is a benzodiazepine that is used for the short-term treatment insomnia (trouble falling or staying asleep). Estazolam is available only with your doctor’s prescription. Your doctor or pharmacist will give you the manufacturer’s patient information sheet (Medication Guide) when you begin treatment with estazolam and each time you refill your prescription. Read the information carefully and ask your doctor or pharmacist if you have any questions.
Estazolam comes as a tablet to take by mouth. It is usually taken as needed at bedtime or after going to bed and having difficulty falling asleep. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take estazolam exactly as directed.
You will probably become very sleepy after you take estazolam and may remain sleepy for some time. Plan to go to bed right after you take estazolam and to stay in bed for a full night. Do not take estazolam if you will be unable to remain asleep for a full night after you take the medication.
Your sleep problems should improve within 7 to 10 days after you start taking estazolam. Call your doctor if your sleep problems do not improve during this time, if they worsen at any time during your treatment, or if you notice any unusual changes in your thoughts or behavior.
If your doctor has told you to take estazolam regularly, talk to your doctor before you stop taking this medication. Your doctor will probably decrease your dose gradually. If you suddenly stop taking estazolam, you may experience withdrawal symptoms such as difficulty falling asleep or staying asleep, uncontrollable shaking of a part of the body, stomach and muscle cramps, vomiting, sweating, sad mood, seeing things or hearing sounds that do not exist, and seizures.
Estazolam may increase the risk of serious or life-threatening breathing problems, sedation, or coma if used along with certain medications. Tell your doctor if you are taking or plan to take certain opiate medications for cough such as codeine (in Triacin-C, in Tuzistra XR) or hydrocodone (in Anexsia, in Norco, in Zyfrel) or for pain such as codeine (in Fiorinal), fentanyl (Actiq, Duragesic, Subsys, others), hydromorphone (Dilaudid, Exalgo), meperidine (Demerol), methadone (Dolophine, Methadose), morphine (Astramorph, Duramorph PF, Kadian), oxycodone (in Oxycet, in Percocet, in Roxicet, others), and tramadol (Conzip, Ultram, in Ultracet). Your doctor may need to change the dosages of your medications and will monitor you carefully. If you take estazolam with any of these medications and you develop any of the following symptoms, call your doctor immediately or seek emergency medical care immediately: unusual dizziness, lightheadedness, extreme sleepiness, slowed or difficult breathing, or unresponsiveness. Be sure that your caregiver or family members know which symptoms may be serious so they can call the doctor or emergency medical care if you are unable to seek treatment on your own.
Estazolam may be habit forming. Do not take a larger dose, take it more often, or for a longer time than your doctor tells you to. Tell your doctor if you have ever drunk large amounts of alcohol, if you use or have ever used street drugs, or have overused prescription medications. Do not drink alcohol or use street drugs during your treatment. Drinking alcohol or using street drugs during your treatment with estazolam also increases the risk that you will experience these serious, life-threatening side effects. Also tell your doctor if you have or have ever had depression or another mental illness.
Estazolam may cause a physical dependence (a condition in which unpleasant physical symptoms occur if a medication is suddenly stopped or taken in smaller doses), especially if you take it for several days to several weeks. Do not stop taking this medication or take fewer doses without talking to your doctor. Stopping estazolam suddenly can worsen your condition and cause withdrawal symptoms that may last for several weeks to more than 12 months. Your doctor probably will decrease your estazolam dose gradually. Call your doctor or get emergency medical treatment if you experience any of the following symptoms: unusual movements; ringing in your ears; anxiety; memory problems; difficulty concentrating; sleep problems; seizures; shaking; muscle twitching; changes in mental health; depression; burning or prickling feeling in your hands, arms, legs or feet; seeing or hearing things that others do not see or hear; thoughts of harming or killing yourself or others; overexcitement; or losing touch with reality.
Estazolam special precautions
You should not use estazolam if you are allergic to it, or:
- if you are pregnant; or
- if you are also using itraconazole or ketoconazole.
Estazolam may cause birth defects. Do not use if you are pregnant. If you use estazolam during pregnancy, your baby could be born with life-threatening withdrawal symptoms, and may need medical treatment for several weeks. Use effective birth control while using estazolam. Tell your doctor if you become pregnant.
Tell your doctor if you have ever had:
- breathing problems;
- drug or alcohol addiction;
- suicidal thoughts or actions;
- depression or mental illness; or
- liver or kidney disease.
Do not breastfeed whilst taking estazolam.
Estazolam is not approved for use by anyone younger than 18 years old.
Before taking estazolam:
- tell your doctor and pharmacist if you are allergic to estazolam; any other medications, or any of the ingredients in estazolam tablets. Ask your doctor or pharmacist for a list of the ingredients.
- tell your doctor if you are taking ketoconazole (Nizoral) or itraconazole (Onmel, Sporanox). Your doctor will probably tell you not to take estazolam if you are taking either of these medications.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: certain antibiotics such as erythromycin (E.E.S., Erythrocin, E-Mycin); antidepressants; antihistamines; barbiturates such as phenobarbital or pentobarbital; cimetidine (Tagamet); digoxin (Lanoxin); diltiazem (Cardizem, Tiazac); disulfiram (Antabuse); fluvoxamine (Luvox); isoniazid (Laniazid, in Rifamate, in Rifater); medications for mental illness or nausea; medications for seizures such as carbamazepine (Equetro, Tegretol, Teril) and phenytoin (Dilantin, Phenytek); monoamine oxidase (MAO) inhibitors, including isocarboxazid (Marplan), phenelzine (Nardil), selegiline (Eldepryl, Emsam, Zelapar), and tranylcypromine (Parnate); nefazodone; rifampin (Rifadin, Rimactane, in Rifamate, in Rifater); sedatives; sleeping pills; and tranquilizers. Many other medications may also interact with estazolam, so be sure to tell your doctor about all the medications you are taking, even those that do not appear on this list. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have ever thought about killing or harming yourself or planned or tried to do so and if you have or have ever had seizures, breathing problems or lung disease, or kidney or liver disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking estazolam, call your doctor immediately.
- talk to your doctor about the risks and benefits of taking estazolam if you are 65 years of age or older. Older adults should not usually take estazolam because it is not as safe as other medications that can be used to treat the same condition.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking estazolam.
- you should know that this medication may make you drowsy during the daytime. Do not drive a car or operate machinery until you know how this medication affects you.
- you should know that some people who took medications for sleep got out of bed and drove their cars, prepared and ate food, had sex, made phone calls, or were involved in other activities while partially asleep. After they woke up, these people were usually unable to remember what they had done. Call your doctor right away if you find out that you have been driving or doing anything else while you were sleeping.
Special dietary instructions
Unless your doctor tells you otherwise, continue your normal diet.
Estazolam drug interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking estazolam, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using estazolam with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Flumazenil
Using estazolam with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Alfentanil
- Alprazolam
- Amobarbital
- Benzhydrocodone
- Bromazepam
- Bromopride
- Buprenorphine
- Butabarbital
- Butalbital
- Butorphanol
- Calcium Oxybate
- Cannabidiol
- Carbinoxamine
- Carisoprodol
- Cetirizine
- Chloral Hydrate
- Chlorzoxazone
- Clarithromycin
- Clobazam
- Cobicistat
- Codeine
- Dantrolene
- Dihydrocodeine
- Doxylamine
- Esketamine
- Ethchlorvynol
- Fentanyl
- Flibanserin
- Fospropofol
- Gabapentin
- Gabapentin Enacarbil
- Hydrocodone
- Hydromorphone
- Ketamine
- Lemborexant
- Levocetirizine
- Levorphanol
- Lofexidine
- Loxapine
- Magnesium Oxybate
- Meclizine
- Meperidine
- Mephenesin
- Mephobarbital
- Meprobamate
- Metaxalone
- Methadone
- Methocarbamol
- Methohexital
- Metoclopramide
- Midazolam
- Mirtazapine
- Morphine
- Morphine Sulfate Liposome
- Nalbuphine
- Oxycodone
- Oxymorphone
- Pentazocine
- Pentobarbital
- Periciazine
- Phenobarbital
- Potassium Oxybate
- Pregabalin
- Primidone
- Propofol
- Remimazolam
- Scopolamine
- Secobarbital
- Sodium Oxybate
- Sufentanil
- Tapentadol
- Thiopental
- Tramadol
- Trazodone
- Zolpidem
Using estazolam with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Rifapentine
- St John’s Wort
- Theophylline
Other medical problems
The presence of other medical problems may affect the use of estazolam. Make sure you tell your doctor if you have any other medical problems, especially:
- Alcohol or drug abuse or dependence, or history of, or
- Breathing problems or lung disease, severe or
- Depression, history of—Use with caution. May make these conditions worse.
- Kidney disease or
- Liver disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
Estazolam uses
Estazolam is used for the short-term treatment of insomnia (difficulty falling asleep or staying asleep). Estazolam is for short-term use only, usually 7 to 10 days.
Estazolam dosage
The dose of estazolam will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of estazolam. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
For oral dosage form (tablets):
- For insomnia:
- Adults—At first, 1 milligram (mg) at bedtime. Your doctor may adjust your dose if needed.
- Older adults—At first, 0.5 milligram (mg) at bedtime. Your doctor may adjust your dose if needed.
- Children—Use and dose must be determined by your doctor.
Missed dose
You will probably be told to take estazolam as needed. If your doctor tells you to take estazolam regularly and you miss a dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one and do not take estazolam unless you are ready to go to bed and stay asleep for a full night.
Estazolam side effects
Estazolam may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- hangover effect (grogginess)
- drowsiness
- dizziness
- weakness
- dry mouth
- constipation
- aggression
- agitation
- changes in behavior
- slowed or uncoordinated movements
- muscle stiffness
- leg pain
Some side effects can be serious. If you experience any of the following symptoms or those listed in the IMPORTANT WARNING section, call your doctor immediately or get emergency medical treatment:
- fever
- blisters
- rash
- hives
- swelling of the eyes, face, lips, tongue, throat, arms, hands, feet, ankles, or lower legs
- difficulty breathing or swallowing
Estazolam may cause other side effects. Call your doctor if you have any unusual problems while you are taking estazolam.
Flurazepam
Flurazepam (Dalmane) is a benzodiazepine that is used to treat insomnia (trouble falling or staying asleep). Flurazepam may be prescribed for other uses; ask your doctor or pharmacist for more information. Flurazepam is available only with your doctor’s prescription.
Flurazepam comes as a capsule to take by mouth. It is usually taken as needed at bedtime. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take flurazepam exactly as directed.
Flurazepam starts working slowly and continues to work for a short time after you stop taking it. You may experience more benefit from flurazepam on the second and third nights after you start taking it. You may continue to feel the effects of flurazepam for one to two nights after you stop taking the medication.
Your sleep problems should improve within 7 to 10 days after you start taking flurazepam. Call your doctor if your sleep problems do not improve during this time, if they get worse at any time during your treatment, or if you notice any changes in your thoughts or behavior.
Flurazepam may increase the risk of serious or life-threatening breathing problems, sedation, or coma if used along with certain medications. Tell your doctor if you are taking or plan to take certain opiate medications for cough such as codeine (in Triacin-C, in Tuzistra XR) or hydrocodone (in Anexsia, in Norco, in Zyfrel) or for pain such as codeine (in Fiorinal), fentanyl (Actiq, Duragesic, Subsys, others), hydromorphone (Dilaudid, Exalgo), meperidine (Demerol), methadone (Dolophine, Methadose), morphine (Astramorph, Duramorph PF, Kadian), oxycodone (in Oxycet, in Percocet, in Roxicet, others), and tramadol (Conzip, Ultram, in Ultracet). Your doctor may need to change the dosages of your medications and will monitor you carefully. If you take flurazepam with any of these medications and you develop any of the following symptoms, call your doctor immediately or seek emergency medical care immediately: unusual dizziness, lightheadedness, extreme sleepiness, slowed or difficult breathing, or unresponsiveness. Be sure that your caregiver or family members know which symptoms may be serious so they can call the doctor or emergency medical care if you are unable to seek treatment on your own.
Flurazepam may be habit forming. Do not take a larger dose, take it more often, or for a longer time than your doctor tells you to. Tell your doctor if you have ever drunk large amounts of alcohol, if you use or have ever used street drugs, or have overused prescription medications. Do not drink alcohol or use street drugs during your treatment. Drinking alcohol or using street drugs during your treatment with flurazepam also increases the risk that you will experience these serious, life-threatening side effects. Also tell your doctor if you have or have ever had depression or another mental illness.
Flurazepam may cause a physical dependence (a condition in which unpleasant physical symptoms occur if a medication is suddenly stopped or taken in smaller doses), especially if you take it for several days to several weeks. Do not stop taking this medication or take fewer doses without talking to your doctor. Stopping flurazepam suddenly can worsen your condition and cause withdrawal symptoms that may last for several weeks to more than 12 months. Your doctor probably will decrease your flurazepam dose gradually. Call your doctor or get emergency medical treatment if you experience any of the following symptoms: unusual movements; ringing in your ears; anxiety; memory problems; difficulty concentrating; sleep problems; seizures; shaking; muscle twitching; changes in mental health; depression; burning or prickling feeling in hands, arms, legs or feet; seeing or hearing things that others do not see or hear; thoughts of harming or killing yourself or others; overexcitement; or losing touch with reality.
Flurazepam special precautions
You should not use flurazepam if you are allergic to any benzodiazepine (flurazepam, alprazolam, diazepam, lorazepam, Valium, Xanax, Versed, Klonopin, and others).
Do not use if you are pregnant. If you use flurazepam during pregnancy, your baby could be born with life-threatening withdrawal symptoms, and may need medical treatment for several weeks. Use effective birth control while using flurazepam. Stop using flurazepam and tell your doctor if you become pregnant.
Tell your doctor if you have ever had:
- drug or alcohol addiction;
- depression or mental illness; or
- suicidal thoughts or actions.
Do not breastfeed whilst taking flurazepam.
Flurazepam is not approved for use by anyone younger than 18 years old.
Before taking flurazepam:
- tell your doctor and pharmacist if you are allergic to flurazepam, any other medications, or any of the ingredients in flurazepam capsules. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take during your treatment with flurazepam and for several days afterward. Be sure to mention any of the following: antihistamines; cimetidine; clozapine (Clozaril, Versacloz); digoxin; medications for anxiety, depression, mental illness, or seizures; muscle relaxants; sedatives; other sleeping pills; and tranquilizers. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have or have ever had sleep apnea (a sleep disorder that causes breathing to stop for short periods during sleep) or lung, kidney, or liver disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking flurazepam, call your doctor immediately.
- talk to your doctor about the risks and benefits of taking flurazepam if you are 65 years of age or older. Older adults should not usually take flurazepam because it is not as safe as other medications that can be used to treat the same condition.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking flurazepam.
- you should know that this medication may make you drowsy and may increase the risk that you could fall. Take extra care to be sure you do not fall, especially if you get out of bed in the middle of the night. Do not drive a car or operate machinery until you know how this medication affects you.
- you should know that some people who took medications for sleep got out of bed and drove their cars, prepared and ate food, had sex, made phone calls, or were involved in other activities while partially asleep. After they woke up, these people were usually unable to remember what they had done. Call your doctor right away if you find out that you have been driving or doing anything else while you were sleeping.
Special dietary instructions
Unless your doctor tells you otherwise, continue your normal diet.
Flurazepam drug interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking flurazepam, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using flurazepam with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Flumazenil
Using flurazepam with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Alfentanil
- Alprazolam
- Amobarbital
- Benzhydrocodone
- Bromazepam
- Bromopride
- Buprenorphine
- Butabarbital
- Butalbital
- Butorphanol
- Calcium Oxybate
- Cannabidiol
- Carbinoxamine
- Carisoprodol
- Cetirizine
- Chloral Hydrate
- Chlorzoxazone
- Clobazam
- Codeine
- Dantrolene
- Dihydrocodeine
- Doxylamine
- Esketamine
- Ethchlorvynol
- Fentanyl
- Flibanserin
- Gabapentin
- Gabapentin Enacarbil
- Hydrocodone
- Hydromorphone
- Ketamine
- Lemborexant
- Levocetirizine
- Levorphanol
- Lofexidine
- Loxapine
- Magnesium Oxybate
- Meclizine
- Meperidine
- Mephenesin
- Mephobarbital
- Meprobamate
- Metaxalone
- Methadone
- Methocarbamol
- Methohexital
- Metoclopramide
- Midazolam
- Mirtazapine
- Morphine
- Morphine Sulfate Liposome
- Nalbuphine
- Oxycodone
- Oxymorphone
- Pentazocine
- Pentobarbital
- Periciazine
- Phenobarbital
- Potassium Oxybate
- Pregabalin
- Primidone
- Remimazolam
- Scopolamine
- Secobarbital
- Sodium Oxybate
- Sufentanil
- Tapentadol
- Thiopental
- Tramadol
- Trazodone
- Zolpidem
Using flurazepam with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Amprenavir
- Rifapentine
- St John’s Wort
- Theophylline
Other medical problems
The presence of other medical problems may affect the use of flurazepam. Make sure you tell your doctor if you have any other medical problems, especially:
- Alcohol abuse, or history of or
- Breathing problems or lung disease or
- Depression, or history of or
- Drug abuse or dependence, or history of or
- Mental health problems, or history of—Use with caution. May make these conditions worse.
- Kidney disease or
- Liver disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
Flurazepam uses
Flurazepam is used to treat insomnia (difficulty falling asleep and staying asleep). Flurazepam helps you get to sleep faster and sleep through the night.
Flurazepam dosage
The dose of flurazepam will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of flurazepam. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
For oral dosage form (capsules)
- For insomnia:
- Adults
- Dalmane®: 30 milligrams (mg) at bedtime. Your doctor may adjust your dose if needed.
- Flurazepam:
- Men: 15 or 30 mg at bedtime. Your doctor may increase your dose if needed.
- Women: At first, 15 mg at bedtime.
- Older adults—15 mg at bedtime. Your doctor may adjust your dose if needed.
- Children—Use and dose must be determined by your doctor.
- Adults
Missed dose
Flurazepam should only be taken at bedtime. If you forget to take flurazepam at bedtime, you are unable to fall asleep, and you will still be able to stay in bed for a full night’s sleep, you may take flurazepam at that time. Do not take a double dose of flurazepam to make up for a missed dose.
Flurazepam side effects
Flurazepam may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- drowsiness
- dizziness or lightheadedness
- loss of coordination
- headache
- heartburn
- nausea
- vomiting
- stomach pain
- diarrhea
- constipation
- nervousness
- irritability
- talking more than usual
- weakness
- joint pain
Some side effects can be serious. If you experience any of the following side effects or those listed in the IMPORTANT WARNING section, call your doctor immediately or get emergency medical treatment:
- rash
- hives
- swelling of the face, throat, tongue, lips, or eyes
- hoarseness
- difficulty breathing or swallowing
- pounding heartbeat
- chest pain
- coma (loss of consciousness for a period of time)
Lorazepam
Lorazepam (Ativan) is a benzodiazepine that is used to treat anxiety disorders. Lorazepam is also used for short-term relief of the symptoms of anxiety or anxiety caused by depression. Lorazepam is available only with your doctor’s prescription. Talk to your doctor about the possible risks of using lorazepam for your condition.
Lorazepam comes as a tablet and concentrate (liquid) to take by mouth. It usually is taken two or three times a day and may be taken with or without food. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take lorazepam exactly as directed.
Lorazepam concentrate (liquid) comes with a specially marked dropper for measuring the dose. Ask your pharmacist to show you how to use the dropper. Dilute the concentrate in 1 ounce (30 milliliters) or more of water, juice, or carbonated beverages just before taking it. It also may be mixed with applesauce or pudding just before taking the dose.
Lorazepam may increase the risk of serious or life-threatening breathing problems, sedation, or coma if used along with certain medications. Tell your doctor if you are taking or plan to take certain opiate medications for cough such as codeine (in Triacin-C, in Tuzistra XR) or hydrocodone (in Anexsia, in Norco, in Zyfrel) or for pain such as codeine (in Fiorinal), fentanyl (Actiq, Duragesic, Subsys, others), hydromorphone (Dilaudid, Exalgo), meperidine (Demerol), methadone (Dolophine, Methadose), morphine (Astramorph, Duramorph PF, Kadian), oxycodone (in Oxycet, in Percocet, in Roxicet, others), and tramadol (Conzip, Ultram, in Ultracet). Your doctor may need to change the dosages of your medications and will monitor you carefully. If you take lorazepam with any of these medications and you develop any of the following symptoms, call your doctor immediately or seek emergency medical care immediately: unusual dizziness, lightheadedness, extreme sleepiness, slowed or difficult breathing, or unresponsiveness. Be sure that your caregiver or family members know which symptoms may be serious so they can call the doctor or emergency medical care if you are unable to seek treatment on your own.
Lorazepam may be habit forming. Do not take a larger dose, take it more often, or for a longer time than your doctor tells you to. Tell your doctor if you have ever drunk large amounts of alcohol, if you use or have ever used street drugs, or have overused prescription medications. Do not drink alcohol or use street drugs during your treatment. Drinking alcohol or using street drugs during your treatment with lorazepam also increases the risk that you will experience these serious, life-threatening side effects. Also tell your doctor if you have or have ever had depression or another mental illness.
Lorazepam may cause a physical dependence (a condition in which unpleasant physical symptoms occur if a medication is suddenly stopped or taken in smaller doses), especially if you take it for several days to several weeks. Do not stop taking this medication or take fewer doses without talking to your doctor. Stopping lorazepam suddenly can worsen your condition and cause withdrawal symptoms that may last for several weeks to more than 12 months. Your doctor probably will decrease your lorazepam dose gradually. Call your doctor or get emergency medical treatment if you experience any of the following symptoms: unusual movements; ringing in your ears; anxiety; memory problems; difficulty concentrating; sleep problems; seizures; shaking; muscle twitching; changes in mental health; depression; burning or prickling feeling in your hands, arms, legs or feet; seeing or hearing things that others do not see or hear; thoughts of harming or killing yourself or others; overexcitement; or losing touch with reality.
Lorazepam special precautions
You should not use lorazepam if you have:
- narrow-angle glaucoma; or
- a history of allergic reaction to any benzodiazepine (lorazepam, alprazolam, diazepam, Valium, Xanax, Versed, Klonopin, and others).
To make sure lorazepam is safe for you, tell your doctor if you have ever had:
- asthma, chronic obstructive pulmonary disease (COPD), sleep apnea, or other breathing disorder;
- drug or alcohol addiction;
- depression, mood problems, or suicidal thoughts or behavior;
- kidney or liver disease;
- seizures; or
- an allergy to aspirin or yellow food dye.
Tell your doctor if you are pregnant or plan to become pregnant. If you use lorazepam during pregnancy, your baby could be born with life-threatening withdrawal symptoms, and may need medical treatment for several weeks.
You should not breastfeed while you are taking lorazepam. If you do breastfeed, tell your doctor if you notice drowsiness, feeding problems, or slow weight gain in the nursing baby.
Lorazepam is not approved for use by anyone younger than 12 years old. Extended-release lorazepam should not be used by anyone younger than 18 years old.
Before taking lorazepam:
- tell your doctor and pharmacist if you are allergic to lorazepam, alprazolam (Xanax), chlordiazepoxide (Librium, in Librax), clonazepam (Klonopin), clorazepate (Gen-Xene, Tranxene), diazepam (Valium), estazolam, flurazepam, oxazepam, temazepam (Restoril), triazolam (Halcion), any other medications, or any of the ingredients in lorazepam tablets or concentrate. Ask your doctor or pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: antihistamines; digoxin (Lanoxin); levodopa (in Ritary, in Sinemet, in Stalevo); medications for depression, seizures, Parkinson’s disease, asthma, colds, or allergies; muscle relaxants; oral contraceptives; probenecid (Probalan, in Col-Probenecid); rifampin (Rifadin, Rimactane, in Rifamate, in Rifater); sedatives; sleeping pills; theophylline (Elixophyllin, Theo 24, Theochron); tranquilizers; and valproic acid (Depakene).Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have glaucoma. Your doctor will probably tell you not to take lorazepam.
- tell your doctor if you have or have ever had seizures; or lung, heart, or liver disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking lorazepam, call your doctor immediately.
- talk to your doctor about the risks and benefits of taking this medication if you are 65 years of age or older. Older adults should take lower doses of lorazepam because higher doses may not be more effective and are more likely to cause serious side effects.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking lorazepam.
- you should know that this medication may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
Special dietary instructions
Unless your doctor tells you otherwise, continue your normal diet.
Lorazepam drug interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking lorazepam, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using lorazepam with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Flumazenil
Using lorazepam with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Alfentanil
- Alprazolam
- Amobarbital
- Anileridine
- Benzhydrocodone
- Bromazepam
- Bromopride
- Buprenorphine
- Butabarbital
- Butalbital
- Butorphanol
- Calcifediol
- Calcium Oxybate
- Cannabidiol
- Carbinoxamine
- Carisoprodol
- Cetirizine
- Chloral Hydrate
- Chlorzoxazone
- Clobazam
- Codeine
- Dantrolene
- Dezocine
- Diacetylmorphine
- Difenoxin
- Dihydrocodeine
- Diphenoxylate
- Doxylamine
- Esketamine
- Ethchlorvynol
- Ethylmorphine
- Fentanyl
- Flibanserin
- Fospropofol
- Gabapentin
- Gabapentin Enacarbil
- Hydrocodone
- Hydromorphone
- Ketamine
- Ketobemidone
- Lemborexant
- Levocetirizine
- Levorphanol
- Lofexidine
- Loxapine
- Magnesium Oxybate
- Meclizine
- Meperidine
- Mephenesin
- Mephobarbital
- Meprobamate
- Meptazinol
- Metaxalone
- Methadone
- Methocarbamol
- Methohexital
- Metoclopramide
- Midazolam
- Mirtazapine
- Morphine
- Morphine Sulfate Liposome
- Nalbuphine
- Nicomorphine
- Opium
- Opium Alkaloids
- Orlistat
- Oxycodone
- Oxymorphone
- Papaveretum
- Paregoric
- Pentazocine
- Pentobarbital
- Periciazine
- Phenobarbital
- Piritramide
- Potassium Oxybate
- Pregabalin
- Primidone
- Propofol
- Remifentanil
- Remimazolam
- Scopolamine
- Secobarbital
- Sodium Oxybate
- Sufentanil
- Tapentadol
- Thiopental
- Tilidine
- Tramadol
- Trazodone
- Zolpidem
Using lorazepam with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Desogestrel
- Dienogest
- Drospirenone
- Estradiol
- Ethinyl Estradiol
- Ethynodiol
- Gestodene
- Levonorgestrel
- Mestranol
- Nomegestrol
- Norethindrone
- Norgestimate
- Norgestrel
- Posaconazole
- Probenecid
- Pyrimethamine
- Rifapentine
- St John’s Wort
- Theophylline
- Valproic Acid
Other medical problems
The presence of other medical problems may affect the use of lorazepam. Make sure you tell your doctor if you have any other medical problems, especially:
- Alcohol or drug abuse or dependence, or history of or
- Lung or breathing problems (eg, COPD, respiratory depression, sleep apnea) or
- Seizures, or history of—Use with caution. May make these conditions worse.
- Depression or
- Mental problems (eg, psychosis)—Use is not recommended in patients with these conditions.
- Glaucoma, acute narrow-angle—Should not be used in patients with this condition.
- Kidney disease or
- Liver disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
Lorazepam uses
Lorazepam is used to treat anxiety disorders. Lorazepam is also used to treat irritable bowel syndrome (IBS), epilepsy, insomnia, and nausea and vomiting from cancer treatment and to control agitation caused by alcohol withdrawal.
Lorazepam dosage
The dose of lorazepam will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of lorazepam. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
For oral dosage form (oral solution)
- For anxiety:
- Adults and children 12 years of age and older—2 to 6 milligrams (mg) in divided doses per day. Your doctor may adjust your dose as needed.
- Older adults—At first, 1 to 2 mg in divided doses per day. Your doctor may adjust your dose as needed.
- Children younger than 12 years of age—Use and dose must be determined by your doctor.
For oral dosage form (tablets):
- For anxiety:
- Adults and children 12 years of age and older—At first, 2 to 3 milligrams (mg) in divided doses per day. Your doctor may adjust your dose as needed.
- Older adults—At first, 1 to 2 mg in divided doses per day. Your doctor may adjust your dose as needed and tolerated.
- Children younger than 12 years of age—Use and dose must be determined by your doctor.
- For insomnia caused by anxiety or transient situational stress:
- Adults and children 12 years of age and older—2 to 4 milligrams (mg) taken as a single dose at bedtime. Your doctor may adjust your dose as needed.
- Children younger than 12 years of age—Use and dose must be determined by your doctor.
For oral dosage form (extended-release capsules):
- For anxiety:
- Adults—One capsule once a day in the morning. Dose is based on the total daily dose of lorazepam tablets, which you take three times a day in equally divided doses. Your doctor may adjust your dose as needed.
- Children—Use and dose must be determined by your doctor.
Missed dose
If you take several doses per day and miss a dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
Lorazepam side effects
Lorazepam may cause side effects. Call your doctor if any of the following symptoms are severe or do not go away:
- drowsiness
- dizziness
- tiredness
- weakness
- dry mouth
- diarrhea
- nausea
- changes in appetite
- restlessness or excitement
- constipation
- difficulty urinating
- frequent urination
- blurred vision
- changes in sex drive or ability
Some side effects can be serious. If you experience any of these symptoms or those listed in the IMPORTANT WARNINGS section, call your doctor immediately or get emergency medical treatment:
- shuffling walk
- persistent, fine tremor or inability to sit still
- fever
- severe skin rash
- yellowing of skin or eyes
- irregular heartbeat
Lorazepam may cause other side effects. Call your doctor if you have any unusual problems while you are taking lorazepam.
Midazolam
Midazolam (Versed) is a benzodiazepine that is used to help you relax before having a minor surgery, dental work, or other medical procedure. Midazolam is given only by or under the immediate supervision of a doctor trained to use this medicine.
Midazolam comes as a syrup to take by mouth. It is usually given as a single dose by a doctor or nurse before a medical procedure or surgery.
Midazolam may cause serious or life-threatening breathing problems such as shallow, slowed, or temporarily stopped breathing. Your child should only receive this medication in a hospital or doctor’s office that has the equipment that is needed to monitor his or her heart and lungs and to provide life-saving medical treatment quickly if his or her breathing slows or stops. Your child’s doctor or nurse will watch your child closely after he or she receives this medication to make sure that he or she is breathing properly. Tell your child’s doctor if your child has a severe infection or if he or she has or has ever had any airway or breathing problems or heart or lung disease. Tell your child’s doctor and pharmacist if your child is taking any of the following medications: antidepressants; barbiturates such as secobarbital (Seconal); droperidol (Inapsine); medications for anxiety, mental illness, or seizures; narcotic medications for pain such as fentanyl (Actiq, Duragesic, Sublimaze, others), morphine (Avinza, Kadian, MS Contin, others), and meperidine (Demerol); sedatives; sleeping pills; or tranquilizers.
Midazolam special precautions
You should not use midazolam if you are allergic to it, or if you have:
- narrow-angle glaucoma;
- untreated or uncontrolled open-angle glaucoma; or
- an allergy to cherries.
Tell your doctor if you have ever had:
- glaucoma;
- breathing problems; or
- congestive heart failure.
Tell your doctor if you are pregnant or breastfeeding.
Before your child receives midazolam:
- tell your child’s doctor and pharmacist if he or she is allergic to midazolam, any other medications, or cherries.
- tell your child’s doctor if your child is taking certain medications for human immunodeficiency virus (HIV) including amprenavir (Agenerase), atazanavir (Reyataz), darunavir (Prezista), delavirdine (Rescriptor), efavirenz (Sustiva, in Atripla), fosamprenavir (Lexiva), indinavir (Crixivan),lopinavir (in Kaletra), nelfinavir (Viracept), ritonavir (Norvir, in Kaletra), saquinavir (Invirase), and tipranavir (Aptivus). Your child’s doctor may decide not to give midazolam to your child if he or she is taking one or more of these medications.
- tell your child’s doctor and pharmacist what other prescription and nonprescription medications, vitamins, and nutritional supplements your child is taking or plans to take. Be sure to mention the medications listed in the IMPORTANT WARNING section and any of the following: amiodarone (Cordarone, Pacerone); aminophylline (Truphylline); antifungals such as fluconazole (Diflucan), itraconazole (Sporanox), and ketoconazole (Nizoral); certain calcium channel blockers such as diltiazem (Cartia, Cardizem, Tiazac, others) and verapamil (Calan, Isoptin, Verelan, others); cimetidine (Tagamet); clarithromycin (Biaxin); dalfopristin-quinupristin (Synercid); erythromycin (E-mycin, E.E.S.); fluvoxamine (Luvox); certain medications for seizures such as carbamazepine (Tegretol), phenobarbital, and phenytoin (Dilantin); methylphenidate (Concerta, Metadate, Ritalin, others); nefazodone; ranitidine (Zantac); rifabutin (Mycobutin); and rifampin (Rifadin, Rimactane). Your child’s doctor may need to change the doses of your child’s medications or monitor your child carefully for side effects. Many other medications may also interact with midazolam, so be sure to tell your child’s doctor about all the medications your child is taking, even those that do not appear on this list.
- tell your child’s doctor what herbal products your child is taking, especially St. John’s wort.
- tell your child’s doctor if your child has glaucoma. Your child’s doctor may decide not to give your child midazolam.
- tell your child’s doctor if your child has or has ever had kidney or liver disease.
- tell your child’s doctor if your child is or may be pregnant, or is breast-feeding.
- you should know that midazolam may make your child very drowsy and may affect his or her memory, thinking, and movements. Do not allow your child to ride a bicycle, drive a car, or do other activities that require him or her to be fully alert for at least 24 hours after receiving midazolam and until the effects of the medication have worn off. Watch your child carefully to be sure that he or she does not fall while walking during this time.
- you should know that alcohol can make the side effects of midazolam worse.
Special dietary instructions
Do not let your child eat grapefruit or drink grapefruit juice while taking midazolam.
Midazolam drug interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are receiving midazolam, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using midazolam with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Amprenavir
- Atazanavir
- Boceprevir
- Cobicistat
- Darunavir
- Delavirdine
- Flumazenil
- Fosamprenavir
- Indinavir
- Itraconazole
- Ketoconazole
- Lopinavir
- Nelfinavir
- Ritonavir
- Saquinavir
- Telaprevir
- Tipranavir
Using midazolam with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Alfentanil
- Alprazolam
- Amobarbital
- Anileridine
- Aprobarbital
- Baclofen
- Belzutifan
- Benzhydrocodone
- Bromazepam
- Bromopride
- Buprenorphine
- Buspirone
- Butabarbital
- Butalbital
- Butorphanol
- Calcifediol
- Calcium Oxybate
- Cannabidiol
- Carbinoxamine
- Carisoprodol
- Ceritinib
- Cetirizine
- Chloral Hydrate
- Chlordiazepoxide
- Chlorpromazine
- Chlorzoxazone
- Ciprofloxacin
- Clarithromycin
- Clobazam
- Clonazepam
- Clorazepate
- Codeine
- Conivaptan
- Cyclobenzaprine
- Dantrolene
- Dexmedetomidine
- Dezocine
- Diacetylmorphine
- Diazepam
- Difenoxin
- Dihydrocodeine
- Diphenhydramine
- Diphenoxylate
- Doxylamine
- Dronedarone
- Duvelisib
- Elagolix
- Esketamine
- Estazolam
- Eszopiclone
- Ethchlorvynol
- Ethylmorphine
- Fentanyl
- Fexinidazole
- Flibanserin
- Flunitrazepam
- Flurazepam
- Fosnetupitant
- Fospropofol
- Gabapentin
- Gabapentin Enacarbil
- Halazepam
- Hydrocodone
- Hydromorphone
- Hydroxyzine
- Idelalisib
- Imatinib
- Isavuconazonium Sulfate
- Ivosidenib
- Ketamine
- Ketazolam
- Ketobemidone
- Larotrectinib
- Lefamulin
- Lemborexant
- Letermovir
- Levocetirizine
- Levorphanol
- Lofexidine
- Lorazepam
- Lorlatinib
- Loxapine
- Lumacaftor
- Magnesium Oxybate
- Meclizine
- Meperidine
- Mephenesin
- Mephobarbital
- Meprobamate
- Meptazinol
- Metaxalone
- Methadone
- Methocarbamol
- Methohexital
- Methotrimeprazine
- Metoclopramide
- Mirtazapine
- Morphine
- Morphine Sulfate Liposome
- Nalbuphine
- Nefazodone
- Netupitant
- Nicomorphine
- Nilotinib
- Nitrazepam
- Opium
- Opium Alkaloids
- Orlistat
- Orphenadrine
- Oxazepam
- Oxycodone
- Oxymorphone
- Papaveretum
- Paregoric
- Pentazocine
- Pentobarbital
- Perampanel
- Periciazine
- Phenobarbital
- Piritramide
- Posaconazole
- Potassium Oxybate
- Prazepam
- Pregabalin
- Primidone
- Promethazine
- Propofol
- Quazepam
- Ramelteon
- Remifentanil
- Remimazolam
- Ribociclib
- Scopolamine
- Secobarbital
- Simeprevir
- Sodium Oxybate
- Sufentanil
- Tapentadol
- Temazepam
- Thiopental
- Thioridazine
- Tilidine
- Tizanidine
- Topiramate
- Tramadol
- Trazodone
- Triazolam
- Zaleplon
- Zolpidem
- Zopiclone
Using midazolam with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Aprepitant
- Armodafinil
- Carbamazepine
- Cimetidine
- Crizotinib
- Cyclosporine
- Dalfopristin
- Diltiazem
- Echinacea
- Erythromycin
- Fluconazole
- Fluvoxamine
- Fosaprepitant
- Fosphenytoin
- Ginkgo Biloba
- Goldenseal
- Halothane
- Laropiprant
- Mitotane
- Phenytoin
- Quinupristin
- Rifapentine
- Roxithromycin
- St John’s Wort
- Telithromycin
- Theophylline
- Verapamil
- Voriconazole
Other interactions
Using midazolam with any of the following is usually not recommended, but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use midazolam, or give you special instructions about the use of food, alcohol, or tobacco.
- Ethanol
Using midazolam with any of the following may cause an increased risk of certain side effects but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use midazolam, or give you special instructions about the use of food, alcohol, or tobacco.
- Grapefruit Juice
Other medical problems
The presence of other medical problems may affect the use of midazolam. Make sure you tell your doctor if you have any other medical problems, especially:
- Apnea (temporary stopping of breathing) or
- Heart disease or
- Hypoventilation (slow breathing) or
- Infections or
- Lung disease, severe or
- Lung or airway blockage—Use with caution. May increase risks for more serious side effects.
- Congestive heart failure or
- Kidney disease or
- Liver disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
- Glaucoma, acute narrow-angle—Should not be used in patients with this condition.
Midazolam uses
Midazolam is used to produce sleepiness or drowsiness and to relieve anxiety before a minor surgery, dental work, or other medical procedure. Midazolam is also given to produce amnesia (loss of memory) so that the patient will not remember any discomfort or undesirable effects that may occur after a surgery or procedure. Midazolam is given to children before medical procedures or before anesthesia for surgery to cause drowsiness, relieve anxiety, and prevent any memory of the event.
Midazolam dosage
Midazolam will be given to you or to your child in a hospital or clinic by a doctor trained to use this medicine. If you or your child will be receiving midazolam during surgery, your doctor or anesthesiologist will give you the medicine.
After you receive midazolam, you or your child will be watched closely to make sure this medicine is working. Your breathing, blood pressure, nervous system, and heart will also be watched closely to make sure the medicine is not causing unwanted side effects.
Midazolam side effects
Midazolam may cause side effects. Tell your child’s doctor if any of these symptoms are severe or do not go away:
- nausea
- vomiting
- rash
Some side effects can be serious. If your child experiences any of these symptoms, call his or her doctor immediately:
- agitation
- restlessness
- uncontrollable shaking of a part of the body
- stiffening and jerking of the arms and legs
- aggression
- slow or irregular heartbeat
Midazolam may cause other side effects. Call your child’s doctor if your child has any unusual problems while taking midazolam.
Oxazepam
Oxazepam (Serax) is a benzodiazepine that is used to treat anxiety disorders, including anxiety caused by depression. Oxazepam may also be used short-term to treat symptoms of alcohol withdrawal. Oxazepam can also be used to treat tension, agitation, and irritability in older patients. Oxazepam may be prescribed for other uses (e.g., irritable bowel syndrome). Talk to your doctor about the possible risks of using this medication for your condition. Oxazepam is available only with your doctor’s prescription.
Oxazepam comes as a capsule to take by mouth. It is usually taken three or four times a day and may be taken with or without food. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take oxazepam exactly as directed.
Oxazepam may help control your symptoms but will not cure your condition. Continue to take oxazepam even if you feel well. Do not skip doses even if you feel that you do not need them.
Oxazepam may increase the risk of serious or life-threatening breathing problems, sedation, or coma if used along with certain medications. Tell your doctor if you are taking or plan to take certain opiate medications for cough such as codeine (in Triacin-C, in Tuzistra XR) or hydrocodone (in Anexsia, in Norco, in Zyfrel) or for pain such as codeine (in Fiorinal), fentanyl (Actiq, Duragesic, Subsys, others), hydromorphone (Dilaudid, Exalgo), meperidine (Demerol), methadone (Dolophine, Methadose), morphine (Astramorph, Duramorph PF, Kadian), oxycodone (in Oxycet, in Percocet, in Roxicet, others), and tramadol (Conzip, Ultram, in Ultracet). Your doctor may need to change the dosages of your medications and will monitor you carefully. If you take oxazepam with any of these medications and you develop any of the following symptoms, call your doctor immediately or seek emergency medical care immediately: unusual dizziness, lightheadedness, extreme sleepiness, slowed or difficult breathing, or unresponsiveness. Be sure that your caregiver or family members know which symptoms may be serious so they can call the doctor or emergency medical care if you are unable to seek treatment on your own.
Oxazepam may be habit forming. Do not take a larger dose, take it more often, or for a longer time than your doctor tells you to. Tell your doctor if you have ever drunk large amounts of alcohol, if you use or have ever used street drugs, or have overused prescription medications. Do not drink alcohol or use street drugs during your treatment. Drinking alcohol or using street drugs during your treatment with oxazepam also increases the risk that you will experience these serious, life-threatening side effects. Also tell your doctor if you have or have ever had depression or another mental illness.
Oxazepam may cause a physical dependence (a condition in which unpleasant physical symptoms occur if a medication is suddenly stopped or taken in smaller doses), especially if you take it for several days to several weeks. Do not stop taking this medication or take fewer doses without talking to your doctor. Stopping oxazepam suddenly can worsen your condition and cause withdrawal symptoms that may last for several weeks to more than 12 months. Your doctor probably will decrease your oxazepam dose gradually. Call your doctor or get emergency medical treatment if you experience any of the following symptoms: unusual movements; ringing in your ears; anxiety; memory problems; difficulty concentrating; sleep problems; seizures; shaking; muscle twitching; changes in mental health; depression; burning or prickling feeling in your hands, arms, legs or feet; seeing or hearing things that others do not see or hear; thoughts of harming or killing yourself or others; overexcitement; or losing touch with reality.
Oxazepam special precautions
You should not use oxazepam if you are allergic to oxazepam, or if you have mental illness and psychosis.
Tell your doctor if you have ever had:
- depression, mental illness, suicidal thoughts;
- alcoholism or drug addiction; or
- low blood pressure.
Oxazepam may harm an unborn baby. Avoid taking oxazepam during the first trimester of pregnancy.
If you use oxazepam during pregnancy, your baby could be born with life-threatening withdrawal symptoms, and may need medical treatment for several weeks.
Ask a doctor if it is safe to breastfeed while using oxazepam.
Oxazepam is not approved for use by anyone younger than 6 years old.
Before taking oxazepam:
- tell your doctor and pharmacist if you are allergic to oxazepam, any other medications, or any of the ingredients in oxazepam capsules. Ask your doctor or pharmacist for more information.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: antihistamines; digoxin (Lanoxin); levodopa (in Ritary, in Sinemet, in Stalevo); medication for depression, seizures, Parkinson’s disease, asthma, colds, or allergies; muscle relaxants; oral contraceptives; phenytoin (Dilantin, Phenytek); probenecid (Probalan, in Col-Probenecid); rifampin (Rifadin, Rimactane, in Rifamate, in Rifater); sedatives; sleeping pills; theophylline (Elixophyllin, Theo 24, Theochron); or tranquilizers. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have or have ever had glaucoma or seizures, or lung, heart, or liver disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking oxazepam, call your doctor immediately.
- talk to your doctor about the risks and benefits of taking oxazepam if you are 65 years of age or older. Older adults should take lower doses of oxazepam because higher doses may not be more effective and are more likely to cause serious side effects.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking oxazepam.
- you should know that this medication may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
Special dietary instructions
Unless your doctor tells you otherwise, continue your normal diet.
Oxazepam drug interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking oxazepam, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using oxazepam with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Flumazenil
Using oxazepam with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Alfentanil
- Alprazolam
- Amobarbital
- Benzhydrocodone
- Bromazepam
- Bromopride
- Buprenorphine
- Butabarbital
- Butalbital
- Butorphanol
- Calcium Oxybate
- Cannabidiol
- Carbinoxamine
- Carisoprodol
- Cetirizine
- Chloral Hydrate
- Chlorzoxazone
- Clobazam
- Codeine
- Dantrolene
- Dihydrocodeine
- Doxylamine
- Esketamine
- Ethchlorvynol
- Fentanyl
- Flibanserin
- Fospropofol
- Gabapentin
- Gabapentin Enacarbil
- Hydrocodone
- Hydromorphone
- Ketamine
- Lemborexant
- Levocetirizine
- Levorphanol
- Lofexidine
- Loxapine
- Magnesium Oxybate
- Meclizine
- Meperidine
- Mephenesin
- Mephobarbital
- Meprobamate
- Metaxalone
- Methadone
- Methocarbamol
- Methohexital
- Metoclopramide
- Midazolam
- Mirtazapine
- Morphine
- Morphine Sulfate Liposome
- Nalbuphine
- Oxycodone
- Oxymorphone
- Pentazocine
- Pentobarbital
- Periciazine
- Phenobarbital
- Potassium Oxybate
- Pregabalin
- Primidone
- Propofol
- Remimazolam
- Scopolamine
- Secobarbital
- Sodium Oxybate
- Sufentanil
- Tapentadol
- Thiopental
- Tramadol
- Trazodone
- Zolpidem
Using oxazepam with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Rifapentine
- St John’s Wort
- Theophylline
Other interactions
Using oxazepam with any of the following may cause an increased risk of certain side effects but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use oxazepam, or give you special instructions about the use of food, alcohol, or tobacco.
- Cabbage
Other medical problems
The presence of other medical problems may affect the use of oxazepam. Make sure you tell your doctor if you have any other medical problems, especially:
- Alcohol or drug abuse or dependence, or history of or
- Depression, or history of or
- Hypotension (low blood pressure) or
- Lung or breathing problems (eg, respiratory depression) or
- Mental health problems, or history of—Use with caution. May make these conditions worse.
- Kidney disease or
- Liver disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
- Mental illness (eg, bipolar disorder, schizophrenia)—Should not be used in patients with this condition.
Oxazepam uses
Oxazepam is used to relieve symptoms of anxiety, including anxiety caused by depression, and including anxiety caused by alcohol withdrawal (symptoms that may develop in people who stop drinking alcohol after drinking large amounts for a long time). Oxazepam can also be used to treat tension, agitation, and irritability in older patients. Oxazepam is also used to treat irritable bowel syndrome (IBS).
Oxazepam dosage
The dose of oxazepam will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of oxazepam. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
For oral dosage form (capsules):
- For anxiety:
- Adults—10 to 30 milligrams (mg) 3 or 4 times a day.
- Older adults—At first, 10 mg 3 times a day. Your doctor may increase your dose if needed.
- Children 6 years of age and older—Use and dose must be determined by your doctor.
- Children younger than 6 years of age—Use is not recommended.
For alcohol withdrawal:
- Adults—15 to 30 milligrams (mg) 3 or 4 times a day.
- Children—Use and dose must be determined by your doctor.
Missed dose
Take the missed dose as soon as you remember it. However, if it is almost time for your next dose skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
Oxazepam side effects
Oxazepam may cause side effects. Call your doctor if any of the symptoms are severe or do not go away:
- drowsiness
- dizziness
- tiredness
- weakness
- dry mouth
- diarrhea
- upset stomach
- changes in appetite
- restlessness or excitement
- constipation
- difficulty urinating
- frequent urination
- blurred vision
- changes in sex drive or ability
Some side effects can be serious. If you experience any of the following symptoms or those listed in the IMPORTANT WARNING section, call your doctor immediately or get emergency medical treatment:
- shuffling walk
- persistent, fine tremor or inability to sit still
- fever
- difficulty breathing or swallowing
- severe skin rash
- yellowing of the skin or eyes
- irregular heartbeat
Oxazepam may cause other side effects. Call your doctor if you experience any unusual problems during your treatment with oxazepam.
Quazepam
Quazepam (Doral) is a benzodiazepine that is used to treat insomnia (trouble falling or staying asleep). Quazepam is for short-term (usually 7 to 10 days) use only. Quazepam is available only with your doctor’s prescription.
Quazepam was approved in the United States in 2007, but is now not commonly used, having been replaced by non-benzodiazepines that bind to the benzodiazepine receptor on the GABA-A receptor complex, which have a shorter duration of action and are better tolerated. Quazepam is available in tablets of 7.5 and 15 mg under the brand name Doral. The recommended initial oral dose for adults is 15 mg at bedtime, which can be decreased to 7.5 mg nightly.
Quazepam most common side effects are dose related and include daytime drowsiness, lethargy, ataxia, dysarthria and dizziness. Tolerance develops to these side effects, but tolerance may also develop to the effects on insomnia.
Quazepam special precautions
You should not use quazepam if you are allergic to it, or if you have:
- a chronic breathing disorder;
- sleep apnea (breathing stops during sleep); or
- an allergy to sleep medicine or to other benzodiazepines (such as alprazolam, diazepam, lorazepam, midazolam, Ativan, Valium, Tranxene, Versed, Xanax, and others).
May cause birth defects. Do not use if you are pregnant. If you use quazepam during pregnancy, your baby could be born with life-threatening withdrawal symptoms, and may need medical treatment for several weeks. Use effective birth control while using quazepam. Tell your doctor if you become pregnant.
Tell your doctor if you have ever had:
- breathing problems;
- drug or alcohol addiction;
- suicidal thoughts or actions;
- depression or mental illness; or
- liver or kidney disease.
Do not breastfeed whilst taking quazepam.
Quazepam is not approved for use by anyone younger than 18 years old.
Quazepam drug interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking quazepam, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using quazepam with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Flumazenil
Using quazepam with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Alfentanil
- Alprazolam
- Amobarbital
- Benzhydrocodone
- Bromazepam
- Bromopride
- Buprenorphine
- Butabarbital
- Butalbital
- Butorphanol
- Calcium Oxybate
- Cannabidiol
- Carbinoxamine
- Carisoprodol
- Cetirizine
- Chloral Hydrate
- Chlorzoxazone
- Clobazam
- Codeine
- Dantrolene
- Dihydrocodeine
- Doxylamine
- Esketamine
- Ethchlorvynol
- Fentanyl
- Flibanserin
- Gabapentin
- Gabapentin Enacarbil
- Hydrocodone
- Hydromorphone
- Ketamine
- Lemborexant
- Levocetirizine
- Levorphanol
- Lofexidine
- Loxapine
- Magnesium Oxybate
- Meclizine
- Meperidine
- Mephenesin
- Mephobarbital
- Meprobamate
- Metaxalone
- Methadone
- Methocarbamol
- Methohexital
- Metoclopramide
- Midazolam
- Mirtazapine
- Morphine
- Morphine Sulfate Liposome
- Nalbuphine
- Oxycodone
- Oxymorphone
- Pentazocine
- Pentobarbital
- Periciazine
- Phenobarbital
- Potassium Oxybate
- Pregabalin
- Primidone
- Remimazolam
- Scopolamine
- Secobarbital
- Sodium Oxybate
- Sufentanil
- Tapentadol
- Thiopental
- Tramadol
- Trazodone
- Zolpidem
Using quazepam with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Rifapentine
- St John’s Wort
- Theophylline
Other medical problems
The presence of other medical problems may affect the use of quazepam. Make sure you tell your doctor if you have any other medical problems, especially:
- Alcohol or drug abuse or dependence, history of or
- Breathing problems or lung disease or
- Depression, history of or
- Mental health problems, history of—Use with caution. May make these conditions worse.
- Pulmonary insufficiency or
- Sleep apnea (temporary stopping of breathing during sleep)—Should not be used in patients with these conditions.
Quazepam uses
Quazepam is used to treat insomnia (trouble sleeping). Quazepam is for short-term (usually 7 to 10 days) use only.
Quazepam dosage
The dose of quazepam will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of quazepam. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
For oral dosage form (tablets)
- For insomnia:
- Adults and older adults—At first, 7.5 milligrams (mg) (half-tablet) at bedtime. Your doctor may adjust your dose as needed.
- Children—Use and dose must be determined by your doctor.
Missed dose
If you miss a dose of quazepam, skip the missed dose and go back to your regular dosing schedule. Do not double doses.
Use quazepam only when you cannot sleep. You do not need to keep a regular dosage schedule for taking it. Do not use two doses at the same time.
Quazepam side effects
Quazepam may cause a severe allergic reaction. Get emergency medical help if you have signs of an allergic reaction: hives; difficult breathing; nausea, vomiting; swelling of your face, lips, tongue, or throat.
Quazepam can slow or stop your breathing, especially if you have recently used an opioid medication or alcohol. A person caring for you should seek emergency medical attention if you have slow breathing with long pauses, blue colored lips, or if you are hard to wake up.
Call your doctor at once if you have:
- confusion, agitation, hallucinations;
- unusual thoughts or behavior;
- suicidal thoughts; or
- worsening depression.
Some people using quazepam have engaged in activity such as driving, eating, walking, making phone calls, or having sex and later having no memory of the activity. Tell your doctor if this happens to you.
Drowsiness or dizziness may last longer in older adults. Use caution to avoid falling or accidental injury.
Quazepam common side effects may include:
- drowsiness, dizziness;
- headache;
- feeling tired;
- dry mouth; or
- upset stomach.
After you stop using quazepam, get medical help right away if you have symptoms such as: unusual muscle movements, being more active or talkative, sudden and severe changes in mood or behavior, confusion, hallucinations, seizures, suicidal thoughts or actions.
Some withdrawal symptoms may last up to 12 months or longer after stopping this medicine suddenly. Tell your doctor if you have ongoing anxiety, depression, problems with memory or thinking, trouble sleeping, ringing in your ears, a burning or prickly feeling, or a crawling sensation under your skin.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects.
Temazepam
Temazepam (Restoril) is a benzodiazepine that is used short term to treat insomnia (trouble falling or staying asleep). Temazepam is for short-term (usually 7 to 10 days) use only. Temazepam may be prescribed for other uses; ask your doctor or pharmacist for more information. Temazepam is available only with your doctor’s prescription. Your doctor or pharmacist will give you the manufacturer’s patient information sheet (Medication Guide) when you begin treatment with temazepam and each time you refill your prescription.
Temazepam comes as a capsule to take by mouth. It is usually taken as needed at bedtime. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take temazepam exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
You will probably become very sleepy soon after you take temazepam and will remain sleepy for some time after you take the medication. Plan to go to bed right after you take temazepam and to stay in bed for 7 to 8 hours. Do not take temazepam if you will be unable to remain asleep for 7 to 8 hours after taking the medication. If you get up too soon after taking temazepam, you may experience memory problems.
Your sleep problems should improve within 7 to 10 days after you start taking temazepam. Call your doctor if your sleep problems do not improve during this time, if they get worse at any time during your treatment, or if you notice any changes in your thoughts or behavior.
Temazepam may increase the risk of serious or life-threatening breathing problems, sedation, or coma if used along with certain medications. Tell your doctor if you are taking or plan to take certain opiate medications for cough such as codeine (in Triacin-C, in Tuzistra XR) or hydrocodone (in Anexsia, in Norco, in Zyfrel) or for pain such as codeine (in Fiorinal), fentanyl (Actiq, Duragesic, Subsys, others), hydromorphone (Dilaudid, Exalgo), meperidine (Demerol), methadone (Dolophine, Methadose), morphine (Astramorph, Duramorph PF, Kadian), oxycodone (in Oxycet, in Percocet, in Roxicet, others), and tramadol (Conzip, Ultram, in Ultracet). Your doctor may need to change the dosages of your medications and will monitor you carefully. If you take temazepam with any of these medications and you develop any of the following symptoms, call your doctor immediately or seek emergency medical care immediately: unusual dizziness, lightheadedness, extreme sleepiness, slowed or difficult breathing, or unresponsiveness. Be sure that your caregiver or family members know which symptoms may be serious so they can call the doctor or emergency medical care if you are unable to seek treatment on your own.
Temazepam may be habit forming. Do not take a larger dose, take it more often, or for a longer time than your doctor tells you to. Tell your doctor if you have ever drunk large amounts of alcohol, if you use or have ever used street drugs, or have overused prescription medications. Do not drink alcohol or use street drugs during your treatment. Drinking alcohol or using street drugs during your treatment with temazepam also increases the risk that you will experience these serious, life-threatening side effects. Also tell your doctor if you have or have ever had depression or another mental illness.
Temazepam may cause a physical dependence (a condition in which unpleasant physical symptoms occur if a medication is suddenly stopped or taken in smaller doses), especially if you take it for several days to several weeks. Do not stop taking this medication or take fewer doses without talking to your doctor. Stopping temazepam suddenly can worsen your condition and cause withdrawal symptoms that may last for several weeks to more than 12 months. Your doctor probably will decrease your temazepam dose gradually. Call your doctor or get emergency medical treatment if you experience any of the following symptoms: unusual movements; ringing in your ears; anxiety; memory problems; difficulty concentrating; sleep problems; seizures; shaking; muscle twitching; changes in mental health; depression; burning or prickling feeling in hands, arms, legs or feet; seeing or hearing things that others do not see or hear; thoughts of harming or killing yourself or others; overexcitement; or losing touch with reality.
Temazepam special precautions
You should not use temazepam if you are allergic to it.
Do not use temazepam if you are pregnant or may become pregnant. This medicine could harm the unborn baby.
To make sure temazepam is safe for you, tell your doctor if you have ever had:
- lung disease or breathing problems;
- depression, mental illness, suicidal thoughts;
- alcoholism or drug addiction; or
- liver or kidney disease.
Ask a doctor if it is safe to breastfeed while using temazepam.
Temazepam is not approved for use by anyone younger than 18 years old.
Before taking temazepam:
- tell your doctor and pharmacist if you are allergic to temazepam, any other medications, or any of the ingredients in temazepam capsules. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: antidepressants; antihistamines such as diphenhydramine (Benadryl); digoxin (Lanoxin); and medications for anxiety, mental illness, or seizures; sedatives; other sleeping pills; and tranquilizers. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have ever thought about killing yourself or tried to do so, and if you have or have ever had any condition that affects your breathing, seizures, or kidney or liver disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. You should not take temazepam if you are pregnant or planning to become pregnant. If you become pregnant while taking temazepam, call your doctor immediately. Temazepam may harm the fetus.
- talk to your doctor about the risks and benefits of taking temazepam if you are 65 years of age or older. Older adults should usually take lower doses of temazepam because higher doses may not be more effective and are more likely to cause serious side effects.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking temazepam.
- you should know that this medication may make you drowsy during the daytime, may decrease your mental alertness, and may increase the risk that you could fall. Take extra care to be sure
- you do not fall, especially if you get out of bed in the middle of the night. Do not drive a car or operate machinery until you know how this medication affects you.
- you should know that some people who took medications for sleep got out of bed and drove their cars, prepared and ate food, had sex, made phone calls, or were involved in other activities while partially asleep. After they woke up, these people were usually unable to remember what they had done. Call your doctor right away if you find out that you have been driving or doing anything else while you were sleeping.
- you should know that your mental health may change in unexpected ways while you are taking this medication. It is hard to tell if these changes are caused by temazepam or if they are caused by physical or mental illnesses that you already have or suddenly develop. Tell your doctor right away if you experience any of the following symptoms: aggressiveness, strange or unusually outgoing behavior, hallucinations (seeing things or hearing voices that do not exist), feeling as if you are outside of your body, memory problems, difficulty concentrating, new or worsening depression, thinking about killing yourself, confusion, and any other changes in your usual thoughts, mood, or behavior. Be sure that your family knows which symptoms may be serious so that they can call the doctor if you are unable to seek treatment on your own.
Special dietary instructions
Unless your doctor tells you otherwise, continue your normal diet.
Temazepam drug interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking temazepam, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using temazepam with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Flumazenil
Using temazepam with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Alfentanil
- Alprazolam
- Amobarbital
- Benzhydrocodone
- Bromazepam
- Bromopride
- Buprenorphine
- Butabarbital
- Butalbital
- Butorphanol
- Calcium Oxybate
- Cannabidiol
- Carbinoxamine
- Carisoprodol
- Cetirizine
- Chloral Hydrate
- Chlorzoxazone
- Clobazam
- Codeine
- Dantrolene
- Dihydrocodeine
- Doxylamine
- Esketamine
- Ethchlorvynol
- Fentanyl
- Flibanserin
- Fospropofol
- Gabapentin
- Gabapentin Enacarbil
- Hydrocodone
- Hydromorphone
- Ketamine
- Lemborexant
- Levocetirizine
- Levorphanol
- Lofexidine
- Loxapine
- Magnesium Oxybate
- Meclizine
- Meperidine
- Mephenesin
- Mephobarbital
- Meprobamate
- Metaxalone
- Methadone
- Methocarbamol
- Methohexital
- Metoclopramide
- Midazolam
- Mirtazapine
- Morphine
- Morphine Sulfate Liposome
- Nalbuphine
- Oxycodone
- Oxymorphone
- Pentazocine
- Pentobarbital
- Periciazine
- Phenobarbital
- Potassium Oxybate
- Pregabalin
- Primidone
- Propofol
- Remimazolam
- Scopolamine
- Secobarbital
- Sodium Oxybate
- Tapentadol
- Thiopental
- Tramadol
- Trazodone
- Zolpidem
Using temazepam with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Desogestrel
- Dienogest
- Drospirenone
- Estradiol
- Ethinyl Estradiol
- Ethynodiol
- Gestodene
- Levonorgestrel
- Mestranol
- Nomegestrol
- Norethindrone
- Norgestimate
- Norgestrel
- Rifapentine
- St John’s Wort
- Theophylline
Other interactions
Using temazepam with any of the following may cause an increased risk of certain side effects but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use temazepam, or give you special instructions about the use of food, alcohol, or tobacco.
- Ethanol
Other medical problems
The presence of other medical problems may affect the use of temazepam. Make sure you tell your doctor if you have any other medical problems, especially:
- Alcohol or drug abuse or dependence, or history of or
- Breathing problems or lung disease or
- Depression, history of or
- Mental health problems, history of—Use with caution. May make these conditions worse.
- Kidney disease or
- Liver disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
Temazepam uses
Temazepam is used on a short-term basis to treat insomnia (difficulty falling asleep or staying asleep). Temazepam is for short-term (usually 7 to 10 days) use only.
Temazepam dosage
The dose of temazepam will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of temazepam. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
For oral dosage form (capsules):
- For insomnia (trouble sleeping):
- Adults—The usual dose is 15 milligrams (mg) at bedtime. Some patients may need 7.5 mg or 30 mg. Your doctor may adjust your dose as needed.
- Older adults—At first, 7.5 mg at bedtime. Your doctor may adjust your dose if needed.
- Children—Use and dose must be determined by your doctor.
Missed dose
Temazepam should only be taken at bedtime. If you did not take temazepam at bedtime and you are unable to fall asleep, you may take temazepam if you will be able to remain in bed for 7 to 8 hours afterwards. Do not take temazepam if you are not ready to go to sleep right away and stay asleep for at least 7 to 8 hours.
Temazepam side effects
Temazepam may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- hangover effect (feeling groggy the day after you take temazepam)
- drowsiness
- dizziness
- nausea
- vomiting
Some side effects can be serious. If you experience any of the following symptoms, or those listed in the IMPORTANT WARNING and special precautions sections, call your doctor immediately or get emergency medical treatment:
- rash
- hives
- swelling of the face, throat, tongue, lips, or eyes
- hoarseness
- difficulty breathing or swallowing
Temazepam may cause other side effects. Call your doctor if you have any unusual problems while you are taking temazepam.
Triazolam
Triazolam (Halcion) is a benzodiazepine that is used short term (7 to 10 days) to treat insomnia (difficulty falling asleep or staying asleep). Triazolam works by slowing activity in your brain to allow sleep. Triazolam is usually taken as needed at bedtime but not with or shortly after a meal. Triazolam may not work well if it is taken with food. Triazolam may also be prescribed for other uses; ask your doctor or pharmacist for more information. Triazolam is classified as a schedule 4 controlled substance, indicating that it has a potential for physical and psychological dependence and abuse. Your doctor or pharmacist will give you the manufacturer’s patient information sheet (Medication Guide) when you begin treatment with triazolam and each time you refill your prescription. Read the information carefully and ask your doctor or pharmacist if you have any questions.
Triazolam was approved in the United States in 1982 and was formerly the most common prescription sleeping pill used in the United States 55. Concerns over its safety led to its withdrawal from use in the UK, and the availability of other potent, shorter acting sleeping pills has caused its decrease in general use in the United States. Current indications are for the short term management of insomnia.
Triazolam comes as a tablet to be taken by mouth and is available in multiple generic forms and under the brand name Halcion in tablets of 0.125 and 0.25 mg. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take triazolam exactly as directed.
Triazolam recommended initial dose for adults is 0.125 mg immediately before bedtime, increasing to 0.25 as needed; rarely, higher doses are used.
You will probably become very sleepy soon after you take triazolam and will remain sleepy for some time after you take the medication. Plan to go to bed right after you take triazolam and to stay in bed for 7 to 8 hours. Do not take triazolam if you will be unable to remain asleep for 7 to 8 hours after taking the medication. If you get up too soon after taking triazolam, you may experience memory problems.
Your sleep problems should improve within 7 to 10 days after you start taking triazolam. Call your doctor if your sleep problems do not improve during this time, if they get worse at any time during your treatment, or if you notice any changes in your thoughts or behavior.
Triazolam should normally be taken for short periods of time (usually 7 to 10 days). You should not take triazolam for more than 2 to 3 weeks without talking to your doctor. If you take triazolam for 7 to 10 days or longer, triazolam may not help you sleep as well as it did when you first began to take the medication, and you may wake up more easily during the last third of the night. You may also start to feel anxious or nervous during the day, and you may develop dependence (‘addiction’; a need to continue taking the medication) on triazolam. Talk to your doctor about the risks of taking triazolam for 2 weeks or longer.
You may have more difficulty falling asleep or staying asleep on the first few nights after you stop taking triazolam than you did before you started taking the medication. This is normal and usually gets better without treatment after one or two nights.
The most common side effects of triazolam are dose related and include daytime drowsiness, lethargy, ataxia, dysarthria and dizziness. Tolerance develops to these side effects, but tolerance may also develop to the soporific effects.
Triazolam may increase the risk of serious or life-threatening breathing problems, sedation, or coma if used along with certain medications. Tell your doctor if you are taking or plan to take certain opiate medications for cough such as codeine (in Triacin-C, in Tuzistra XR) or hydrocodone (in Anexsia, in Norco, in Zyfrel) or for pain such as codeine (in Fiorinal), fentanyl (Actiq, Duragesic, Subsys, others), hydromorphone (Dilaudid, Exalgo), meperidine (Demerol), methadone (Dolophine, Methadose), morphine (Astramorph, Duramorph PF, Kadian), oxycodone (in Oxycet, in Percocet, in Roxicet, others), and tramadol (Conzip, Ultram, in Ultracet). Your doctor may need to change the dosages of your medications and will monitor you carefully. If you take triazolam with any of these medications and you develop any of the following symptoms, call your doctor immediately or seek emergency medical care immediately: unusual dizziness, lightheadedness, extreme sleepiness, slowed or difficult breathing, or unresponsiveness. Be sure that your caregiver or family members know which symptoms may be serious so they can call the doctor or emergency medical care if you are unable to seek treatment on your own.
Triazolam may be habit forming. Do not take a larger dose, take it more often, or for a longer time than your doctor tells you to. Tell your doctor if you have ever drunk large amounts of alcohol, if you use or have ever used street drugs, or have overused prescription medications. Do not drink alcohol or use street drugs during your treatment. Drinking alcohol or using street drugs during your treatment with triazolam also increases the risk that you will experience these serious, life-threatening side effects. Also tell your doctor if you have or have ever had depression or another mental illness.
Triazolam may cause a physical dependence (a condition in which unpleasant physical symptoms occur if a medication is suddenly stopped or taken in smaller doses), especially if you take it for several days to several weeks. Do not stop taking this medication or take fewer doses without talking to your doctor. Stopping triazolam suddenly can worsen your condition and cause withdrawal symptoms that may last for several weeks to more than 12 months. Your doctor probably will decrease your triazolam dose gradually. Call your doctor or get emergency medical treatment if you experience any of the following symptoms: unusual movements; ringing in your ears; anxiety; memory problems; difficulty concentrating; sleep problems; seizures; shaking; muscle twitching; changes in mental health; depression; burning or prickling feeling in hands, arms, legs or feet; seeing or hearing things that others do not see or hear; thoughts of harming or killing yourself or others; overexcitement; or losing touch with reality.
Triazolam special precautions
You should not use triazolam if you are allergic to triazolam or similar medicines (such as alprazolam, diazepam, lorazepam, Valium, Xanax, Versed, Klonopin, and others).
Before taking triazolam:
- tell your doctor and pharmacist if you are allergic to triazolam; other benzodiazepines; any other medications; or any of the ingredients in triazolam tablets. Ask your pharmacist for a list of the ingredients.
- tell your doctor if you are taking any of the following medications: antifungal medications including itraconazole (Onmel, Sporanox) and ketoconazole (Nizoral); certain medications for human immunodeficiency virus (HIV) or acquired immunodeficiency syndrome (AIDS) including indinavir (Crixivan), lopinavir (in Kaletra), nelfinavir (Viracept), ritonavir (Norvir, in Kaletra), and saquinavir (Invirase); and nefazodone. Your doctor will probably tell you not to take triazolam.
- tell your doctor and pharmacist what other prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: amiodarone (Nexterone, Pacerone); certain antibiotics such as clarithromycin (Biaxin, in Prevpac), erythromycin (Erythrocin, E-mycin), telithromycin (Ketek), and troleandomycin (TAO) (not available in the US); antidepressants; certain antifungal medications; antihistamines; certain calcium channel blockers such as diltiazem (Cardizem, Dilacor, Tiazac, others), nicardipine (Cardene), nifedipine (Adalat, Afeditab, Procardia), and verapamil (Calan, Verelan); cyclosporine (Gengraf, Neoral, Sandimmune); ergotamine (Cafergot, Ergomar, Migranal, others); certain histamine-2 receptor blockers (H2 blockers) such as cimetidine (Tagamet) and ranitidine (Zantac); hormonal contraceptives (birth control pills, patches, rings, implants, or injections); isoniazid (Laniazid, in Rifamate, in Rifater); medications for anxiety, colds or allergies, mental illness, or seizures; muscle relaxants; sedatives; certain selective serotonin reuptake inhibitors (SSRIs) such as fluvoxamine (Luvox), paroxetine (Brisdelle, Paxil, Pexeva), and sertraline (Zoloft); other sleeping pills; and tranquilizers. Your doctor may need to change the doses of your medications or monitor you carefully for side effects. Many other medications may also interact with triazolam, so be sure to tell your doctor about all the medications you are taking, even those that do not appear on this list.
- tell your doctor if you have ever thought about killing yourself or tried to do so, and if you have or have ever had any condition that affects your breathing, sleep apnea (condition in which a person briefly stops breathing many times during the night), seizures, or kidney or liver disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking triazolam, call your doctor immediately. Triazolam may harm the fetus.
- talk to your doctor about the safe use of triazolam if you are 65 years of age or older. Older adults should usually take lower doses of triazolam because higher doses may not be more effective and are more likely to cause serious side effects.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking triazolam.
- you should know that triazolam may make you drowsy during the daytime, may decrease your mental alertness, and may increase the risk that you could fall. Take extra care to be sure you do not fall, especially if you get out of bed in the middle of the night. Do not drive a car or operate machinery until you know how this medication affects you.
- you should know that some people who took medications for sleep got out of bed and drove their cars, prepared and ate food, had sex, made phone calls, or were involved in other activities while partially asleep. After they woke up, these people were usually unable to remember what they had done. Call your doctor right away if you find out that you have been driving or doing anything else while you were sleeping.
- you should know that your mental health may change in unexpected ways while you are taking this medication. It is hard to tell if these changes are caused by triazolam or if they are caused by physical or mental illnesses that you already have or suddenly develop. Tell your doctor right away if you experience any of the following symptoms: aggressiveness, strange or unusually outgoing behavior, hallucinations (seeing things or hearing voices that do not exist), feeling as if you are outside of your body, memory problems, difficulty concentrating, slowed speech or movements, new or worsening depression, thinking about killing yourself, confusion, and any other changes in your usual thoughts, mood, or behavior. Be sure that your family knows which symptoms may be serious so that they can call the doctor if you are unable to seek treatment on your own.
Special dietary instructions
Do not eat grapefruit or drink grapefruit juice while you’re taking triazolam.
Triazolam drug interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking triazolam, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using triazolam with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Amprenavir
- Atazanavir
- Boceprevir
- Cobicistat
- Darunavir
- Delavirdine
- Flumazenil
- Fosamprenavir
- Idelalisib
- Indinavir
- Itraconazole
- Ketoconazole
- Lopinavir
- Nefazodone
- Nelfinavir
- Ritonavir
- Saquinavir
- Telaprevir
- Tipranavir
Using triazolam with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Alfentanil
- Alprazolam
- Amobarbital
- Aprobarbital
- Belzutifan
- Benzhydrocodone
- Bromazepam
- Bromopride
- Buprenorphine
- Butabarbital
- Butalbital
- Butorphanol
- Calcium Oxybate
- Cannabidiol
- Carbinoxamine
- Carisoprodol
- Ceritinib
- Cetirizine
- Chloral Hydrate
- Chlorzoxazone
- Clarithromycin
- Clobazam
- Codeine
- Conivaptan
- Dantrolene
- Dihydrocodeine
- Doxylamine
- Duvelisib
- Esketamine
- Ethchlorvynol
- Fentanyl
- Flibanserin
- Fluconazole
- Fosnetupitant
- Fospropofol
- Gabapentin
- Gabapentin Enacarbil
- Hydrocodone
- Hydromorphone
- Ivosidenib
- Ketamine
- Larotrectinib
- Lefamulin
- Lemborexant
- Levocetirizine
- Levorphanol
- Lofexidine
- Lorlatinib
- Loxapine
- Lumacaftor
- Magnesium Oxybate
- Meclizine
- Meperidine
- Mephenesin
- Mephobarbital
- Meprobamate
- Metaxalone
- Methadone
- Methocarbamol
- Methohexital
- Metoclopramide
- Mibefradil
- Midazolam
- Mirtazapine
- Morphine
- Morphine Sulfate Liposome
- Nalbuphine
- Netupitant
- Oxycodone
- Oxymorphone
- Pentazocine
- Pentobarbital
- Periciazine
- Phenobarbital
- Potassium Oxybate
- Pregabalin
- Primidone
- Propofol
- Remimazolam
- Scopolamine
- Secobarbital
- Simeprevir
- Sodium Oxybate
- Sufentanil
- Tapentadol
- Thiopental
- Tramadol
- Trazodone
- Voriconazole
- Zolpidem
Using triazolam with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Dehydroepiandrosterone
- Desogestrel
- Dienogest
- Diltiazem
- Drospirenone
- Erythromycin
- Estradiol
- Ethinyl Estradiol
- Ethynodiol
- Fluvoxamine
- Gestodene
- Levonorgestrel
- Mestranol
- Modafinil
- Nomegestrol
- Norethindrone
- Norgestimate
- Norgestrel
- Omeprazole
- Ranitidine
- Rifampin
- Rifapentine
- Roxithromycin
- Rufinamide
- St John’s Wort
- Theophylline
- Troleandomycin
Other interactions
Using triazolam with any of the following is usually not recommended, but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use triazolam, or give you special instructions about the use of food, alcohol, or tobacco.
- Grapefruit Juice
Using triazolam with any of the following may cause an increased risk of certain side effects but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use triazolam, or give you special instructions about the use of food, alcohol, or tobacco.
- Ethanol
Other medical problems
The presence of other medical problems may affect the use of triazolam. Make sure you tell your doctor if you have any other medical problems, especially:
- Alcohol or drug abuse or dependence, or history of or
- Breathing problems or lung disease, severe or
- Depression, or history of or
- Sleep apnea (temporary stopping of breathing during sleep)—Use with caution. May make these conditions worse.
- Kidney disease or
- Liver disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
Triazolam uses
Triazolam is a benzodiazepine that is widely used as a sleeping aid in the therapy of insomnia. Triazolam should only be taken at bedtime. If you did not take triazolam at bedtime and you are unable to fall asleep, you may take triazolam if you will be able to remain in bed for 7 to 8 hours afterward. Do not take triazolam if you are not ready to go to sleep right away and stay asleep for at least 7 to 8 hours.
Triazolam dosage
The dose of triazolam will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of triazolam. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
- For oral dosage form (tablets):
- For insomnia:
- Adults—0.125 to 0.25 milligram (mg) at bedtime. Your doctor may adjust your dose as needed. However, the dose is usually not more than 0.5 mg per day.
- Older adults—At first, 0.125 mg at bedtime. Your doctor may adjust your dose as needed. However, the dose is usually not more than 0.25 mg per day.
- Children—Use and dose must be determined by your doctor.
- For insomnia:
Missed dose
If you miss a dose of this medicine, skip the missed dose and go back to your regular dosing schedule. Do not double doses.
Use triazolam only when you cannot sleep. You do not need to keep a schedule for taking it. Do not use two doses at the same time.
Triazolam side effects
Triazolam may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- drowsiness
- dizziness
- lightheadedness
- headache
- problems with coordination
- nervousness
- tingling of the skin
- nausea
- vomiting
Some side effects can be serious. If you experience any of these symptoms or those listed in the special precautions or IMPORTANT WARNING sections, call your doctor immediately or get emergency medical help:
- rash
- hives
- itching
- swelling of the eyes, face, lips, tongue, or throat
- feeling that the throat is closing
- difficulty breathing or swallowing
- hoarseness
Triazolam may cause other side effects. Call your doctor if you have any unusual problems while taking triazolam.
References- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Benzodiazepines. [Updated 2017 Jan 24]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548298
- Brands B, Sproule B & Marshman J. (eds) (1998) Drugs & Drug Abuse (3rd ed.) Ontario: Addiction Research Foundation.
- American Druggist. Top 200 drugs of 1995. New York, N.Y.: Hearst Corp, 1996:18–26.
- Salzman C, for Task Force on Benzodiazepine Dependency, American Psychiatric Association. Benzodiazepine dependence, toxicity, and abuse: a task force report of the American Psychiatric Association. Washington, D.C.: American Psychiatric Association, 1990.
- Busto UE, Romach MK, Sellers EM. Multiple drug use and psychiatric comorbidity in patients admitted to the hospital with severe benzodiazepine dependence. J Clin Psychopharmacol. 1996;16:51–7.
- Arana GW, Hyman SE. Handbook of psychiatric drug therapy. 2d ed. Boston: Little, Brown, 1991: 128–61.
- Miller LG. Chronic benzodiazepine administration: from the patient to the gene. J Clin Pharmacol. 1991;31:492–5.
- Benzodiazepines drug profile. https://www.emcdda.europa.eu/publications/drug-profiles/benzodiazepines_en
- Hollister L, Muller-Oerlinghausen B, Rickels K, Shader R. Clinical uses of benzodiazepines. J Clin Psychopharmacol 1993;13(suppl 1):1–169.
- Gold MS, Miller NS, Stennie K, Populla-Vardi C. Epidemology of benzodiazepine use and dependence. Psychiatric Annals. 1995;25:*146–8.
- Dumont RL. Abuse of benzodiazepines—the problems and the solutions. A report of a Committee of the Institute for Behavior and Health, Inc. Am J Drug Alcohol Abuse. 1988;14(suppl 1):1–69.
- Iguchi MY, Griffiths RR, Bickel WK, et al. Relative abuse liability of benzodiazepines in methadonemaintained populations in three cities. In: Harris LS, ed. Problems of drug dependence, 1988: proceedings of the 50th Annual Scientific Meeting, the Committee on Problems of Drug Dependence, Inc. Rockville, Md.: U.S. Department of Health and Human Services, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration,National Institute on Drug Abuse, Office of Science, 1989. DHHS publication no. (ADM) 89-1605.
- Ciraulo DA, Sands BF, Shader RI. Critical review of liability for benzodiazepine abuse among alcoholics. Am J Psychiatry. 1988;145:1501–6.
- Roache JD, Meisch RA. Findings from self-administration research on the addiction potential of benzodiazepines. Psychiatric Annals. 1995;25(3):153–7.
- Parran TV. Prescription drug abuse. A question of balance. Med Clin North Am. 1997;81:967–78.
- Baldwin DS, Aitchison K, Bateson A, Curran HV, Davies S, Leonard B, Nutt DJ, Stephens DN, Wilson S. Benzodiazepines: risks and benefits. A reconsideration. J Psychopharmacol. 2013 Nov;27(11):967-71. doi: 10.1177/0269881113503509
- Seldenrijk A, Vis R, Henstra M, Ho Pian K, van Grootheest D, Salomons T, Overmeire F, de Boer M, Scheers T, Doornebal-Bakker R, Ruhé HG, Vinkers CH. Aandacht voor bijwerkingen van benzodiazepinen is belangrijk: een systematisch overzicht [Systematic review of the side effects of benzodiazepines]. Ned Tijdschr Geneeskd. 2017;161:D1052. Dutch.
- Janhsen K, Roser P, Hoffmann K. The problems of long-term treatment with benzodiazepines and related substances. Dtsch Arztebl Int. 2015 Jan 5;112(1-2):1-7. doi: 10.3238/arztebl.2015.0001
- Discontinuing benzodiazepines. https://www.racgp.org.au/clinical-resources/clinical-guidelines/key-racgp-guidelines/view-all-racgp-guidelines/drugs-of-dependence/part-b/discontinuing-benzodiazepines
- Guidance for the use and reduction of misuse of benzodiazepines and other hypnotics and anxiolytics in general practice. https://www.addictionprofessionals.org.uk/Handlers/Download.ashx?IDMF=8f776bd7-8127-485f-8550-b93603ea275f
- Lader M, Tylee A, Donoghue J. Withdrawing benzodiazepines in primary care. CNS Drugs. 2009;23(1):19-34. doi: 10.2165/0023210-200923010-00002
- Mental Health and Drug and Alcohol Office (MHDAO). NSW Drug and Alcohol Withdrawal Clinical Practice Guidelines. Sydney: MHDAO; 2008.
- Pergolizzi JV Jr, LeQuang JA, Raffa RB. Benzodiazepines: Thinking outside the black box. J Clin Pharm Ther. 2021 Jun;46(3):554-559. doi: 10.1111/jcpt.13333
- Lugoboni F, Quaglio G. Exploring the dark side of the moon: the treatment of benzodiazepine tolerance. Br J Clin Pharmacol. 2014 Feb;77(2):239-41. doi: 10.1111/bcp.12148
- Ashton H. The diagnosis and management of benzodiazepine dependence. Curr Opin Psychiatry. 2005 May;18(3):249-55. doi: 10.1097/01.yco.0000165594.60434.84
- Tapering Patients Off of Benzodiazepines. Am Fam Physician. 2017 Nov 1;96(9):606-608. https://www.aafp.org/afp/2017/1101/p606.html
- Ministry of Health Singapore. Prescribing of Benzodiazepines: MOH Clinical Practice Guidelines 2/2008. Singapore: MOH; 2008.
- Parr JM, Kavanagh DJ, Cahill L, Mitchell G, McD Young R. Effectiveness of current treatment approaches for benzodiazepine discontinuation: a meta-analysis. Addiction. 2009 Jan;104(1):13-24. doi: 10.1111/j.1360-0443.2008.02364.x
- Vicens C, Bejarano F, Sempere E, Mateu C, Fiol F, Socias I, Aragonès E, Palop V, Beltran JL, Piñol JL, Lera G, Folch S, Mengual M, Basora J, Esteva M, Llobera J, Roca M, Gili M, Leiva A. Comparative efficacy of two interventions to discontinue long-term benzodiazepine use: cluster randomised controlled trial in primary care. Br J Psychiatry. 2014 Jun;204(6):471-9. doi: 10.1192/bjp.bp.113.134650
- Wright S. Benzodiazepine withdrawal: clinical aspects. In: Peppin J, Pergolizzi J, Raffa R, et al. (eds) The benzodizapeines crisis: the ramifications of an over-used drug class. New York: Oxford University Press, 2020, pp. 117–148.
- Horowitz MA, Taylor D. How to reduce and stop psychiatric medication. Eur Neuropsychopharmacol. 2022 Feb;55:4-7. https://doi.org/10.1016/j.euroneuro.2021.10.001
- Ashton H. The treatment of benzodiazepine dependence. Addiction. 1994;89(11):1535–1541.
- Joint National Formulary Committee. British National Formulary. London: British Medical Association and Royal Pharmaceutical Society of Great Britain; 2011.
- National Center for PTSD. Effective treatments for PTSD: helping patients taper from benzodiazepines. 2013. https://www.va.gov/PAINMANAGEMENT/docs/OSI_6_Toolkit_Taper_Benzodiazepines_Clinicians.pdf
- Lingford-Hughes AR, Welch S, Peters L, Nutt DJ; British Association for Psychopharmacology, Expert Reviewers Group. BAP updated guidelines: evidence-based guidelines for the pharmacological management of substance abuse, harmful use, addiction and comorbidity: recommendations from BAP. J Psychopharmacol. 2012 Jul;26(7):899-952. doi: 10.1177/0269881112444324
- Ashton H. Toxicity and adverse consequences of benzodiazepine use. Psychiatric Annals. 1995;25:158–65.
- Addiction: Part I. Benzodiazepines—Side Effects, Abuse Risk and Alternatives. Am Fam Physician. 2000 Apr 1;61(7):2121-2128. https://www.aafp.org/afp/2000/0401/p2121.html
- Janicak PG, Davis JM, Preskhorn SH, Ayd FJ. Principles and practice of psychopharmacotherapy. Baltimore: Williams & Wilkins 1993:287.
- Geene DS, Dockens RC, Salazar DE, et al. Coadministration of nefazadone and benzodiazepines. I. pharmacokinetic assessment [Abstract]. Clin Pharmacol Ther. 1994;55:141.
- Smith BD, Salzman C. Do benzodiazepines cause depression? Hosp Comm Psychiatry. 1991;42:1101–2.
- Lader M. Long-term benzodiazepine use and psychological functioning. In: Freeman HL, Rue Y, eds. The benzodiazepines in current clinical practice. International congress and symposium series: proceedings of a symposium sponsored by Wyeth Laboratories. London: Royal Society of Medicine Services, 1987:55–69.
- Barbone F, McMahon AD, Davey PG, Morris AD, Reid IC, McDevitt DC, et al. Association of road-traffic accidents with benzodiazepine use. Lancet. 1998;352:1331–6.
- Curran V. Memory functions, alertness, and mood of long-term benzodiazepine users: a preliminary investigation of the effects of normal daily dose. J Psychopharmacol. 1992;6:69–75.
- van der Bijl P, Roelofse JA. Disinhibitory reactions to benzodiazepines: a review. J Oral Maxillofac Surg. 1991;49:519–23.
- Lader M, Tylee A, Donoghue J. Withdrawing benzodiazepines in primary care. CNS Drugs. 2009;23(1):19–34.
- Bergman U, Rosa FW, Baum C, Wiholm BE, Faich GA. Effects of exposure to benzodiazepines during fetal life. Lancet. 1992;340:694–7.
- Lader M, Russell J. Guidelines for the prevention and treatment of benzodiazepine dependence: summary of a report from the Mental Health Foundation. Addict. 1993;88(12):1707–1708.
- Ashton H. The diagnosis and management of benzodiazepine dependence. Curr Opin Psychiatry. 2005;18(3):249–255.
- Kales A, Scharf MB, Kales JD. Rebound insomnia: a new clinical syndrome. Science. 1978;201:1039–41.
- Schneider-Helmert D. Why low-dose benzodiazepine-dependent insomniacs can’t escape their sleeping pills. Acta Psychiatr Scand. 1988;78:706–11.
- Marriott S, Tyrer P. Benzodiazepine dependence. Avoidance and withdrawal. Drug Saf. 1993;9:93–103.
- Hemmelgarn B, Suissa S, Huang A, Boivin IF, Pinard G. Benzodiazepine use and the risk of motor vehicle crash in the elderly. JAMA. 1997;278:27–31.
- Salzman C, Fisher J, Nobelk Glassman R, Wolfson A, Kelly M. Cognitive improvement following benzodiazepine discontinuation in elderly nursing home residents. Int J Geriatr Psychiatry. 1992;7:89–93.
- Burke KC, Meek WJ, Krych R, Nisbett R, et al. Medical services use by patients before and after detoxification from benzodiazepine dependence. Psychiatric Services. 1995;46(2):157–60.
- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Triazolam. [Updated 2017 Jan 24]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547843