Best diet for heart health
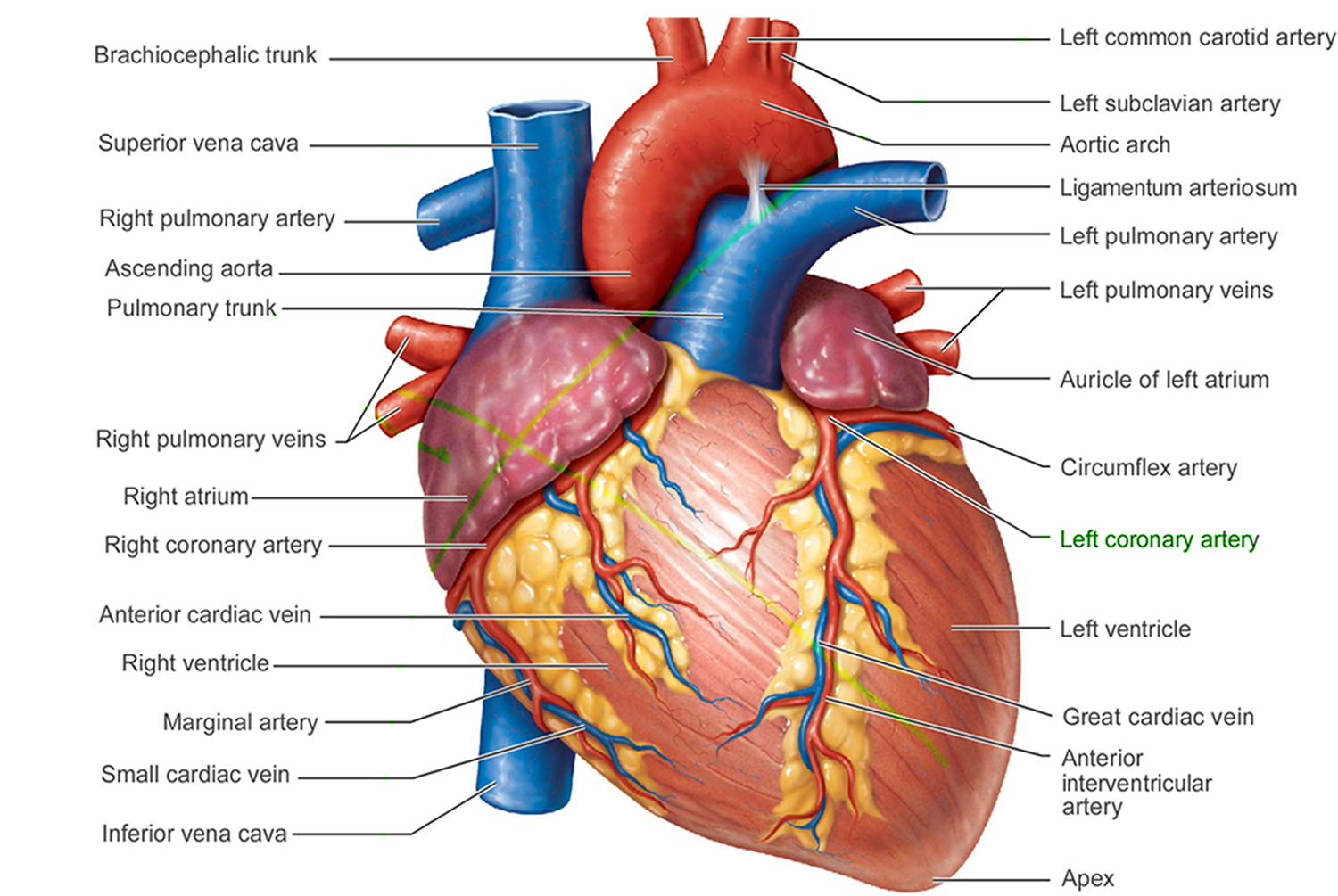
Heart disease also called cardiovascular disease, is the number one killer in the U.S. Heart disease is also a major cause of disability. The most common cause of heart disease is narrowing or blockage of your coronary arteries also called coronary artery disease, the coronary arteries are the blood vessels that supply blood to your heart. A buildup of fatty deposits or plaques in your arteries (also known as atherosclerosis) is the most common cause of coronary artery disease. Atherosclerosis is not part of normal aging and can be serious. Unhealthy lifestyle habits, such as a poor diet, lack of exercise, being overweight and smoking, can lead to atherosclerosis. Coronary artery disease happens slowly over time. It’s the major reason people have heart attacks. Other kinds of heart problems may happen to the valves in the heart or the heart may not pump well and cause heart failure. Some people are born with heart disease also known as congenital heart disease.
Heart disease describes a range of conditions that affect your heart. Heart diseases include:
- Blood vessel disease, such as coronary artery disease
- Heart rhythm problems (arrhythmias)
- Heart defects you’re born with (congenital heart defects)
- Heart valve disease
- Disease of the heart muscle
- Heart infection
Many forms of heart disease can be prevented or treated with healthy lifestyle choices.
Risk factors are conditions or habits that increase your risk of developing a disease. The following are risk factors that can increase your chance of developing heart disease and cardiovascular disease:
- High blood cholesterol (hypercholesterolemia). High levels of cholesterol in your blood can increase the risk of plaque formation and atherosclerosis.
- High blood pressure (hypertension). Uncontrolled high blood pressure can result in hardening and thickening of your arteries, narrowing the vessels through which blood flows. Blood pressure is considered high if it stays at or above 140/90 mmHg over time. If you have diabetes or chronic kidney disease, high blood pressure is defined as 130/80 mmHg or higher. (The mmHg is millimeters of mercury—the units used to measure blood pressure.)
- Diabetes. Diabetes increases your risk of heart disease. Both conditions share similar risk factors, such as obesity and high blood pressure.
- Insulin resistance. This condition occurs if the body can’t use its own insulin properly. Insulin is a hormone that helps move blood sugar into cells where it’s used for energy. Insulin resistance may lead to diabetes.
- Obesity or being overweight. Excess weight typically worsens other heart disease risk factors.
- Metabolic syndrome. Metabolic syndrome occurs when you have obesity, high blood pressure and high blood sugar. Having metabolic syndrome makes you twice as likely to develop heart disease than if you don’t have it.
- Smoking. Nicotine tightens your blood vessels, and carbon monoxide can damage their inner lining, making them more susceptible to atherosclerosis. Heart attacks are more common in smokers than in nonsmokers.
- Poor diet. A diet that’s high in fat, salt, sugar and cholesterol can contribute to the development of heart disease. A healthy diet can help reduce your risk of developing coronary heart disease and stop you gaining weight, reducing your risk of diabetes and high blood pressure.
- Physical inactivity. Lack of exercise also is associated with many forms of heart disease and some of its other risk factors as well.
- Ethnicity. African Americans, Mexican Americans, Native Americans, and native Hawaiians are at greater risk.
- Family history. A family history of heart disease increases your risk of coronary artery disease, especially if a parent developed it at an early age (before age 55 for a male relative, such as your brother or father, and 65 for a female relative, such as your mother or sister).
- Air pollution. Air pollution is harmful to your heart and circulation. Research shows that air pollution can affect your heart and circulation by:
- damaging the inside walls of your blood vessels, causing them to become narrower and harder
- restricting the movement of your blood vessels, which can increase your blood pressure and add to the strain on your heart
- making your blood more likely to clot
- affecting the normal electrical functioning of your heart which could cause abnormal heart rhythms
- causing small changes to the structure of your heart like those that are seen in the early stages of heart failure.
- This damage can contribute to the development of new health problems, or put people with existing heart and circulatory conditions at increased risk of events like a heart attack or stroke.
- Poor dental health. It’s important to brush and floss your teeth and gums often, and have regular dental checkups. If your teeth and gums aren’t healthy, germs can enter your bloodstream and travel to your heart, causing endocarditis.
- Stress. Unrelieved stress may damage your arteries and worsen other risk factors for heart disease. Research suggests that an emotionally upsetting event, particularly one involving anger, can serve as a trigger for a heart attack or angina in some people. Stress can contribute to high blood pressure and other heart disease risk factors. Some of the ways people cope with stress—drinking alcohol, using other substances, smoking, or overeating—are not healthy ways to manage stress.
- Drug abuse. Using stimulant drugs, such as cocaine or amphetamines, can trigger a spasm of your coronary arteries that can cause a heart attack.
- Excessive use of alcohol or caffeine. Heavy drinking can damage the heart muscle and worsen other coronary heart disease risk factors. Men should have no more than two drinks containing alcohol a day. Women should have no more than one drink containing alcohol a day. If you do not drink, you should not start. You should not drink if you are pregnant, are under the age of 21, taking certain medicines, or if you have certain medical conditions, including heart failure.
- Alcohol can:
- Add calories to your daily diet and possibly cause you to gain weight.
- Raise your blood pressure and levels of triglyceride fats in your blood.
- Contribute to or worsen heart failure in some people, such as some people who have cardiomyopathy.
- Raise your risk of other diseases such as cancer.
- Alcohol can:
- Age. Growing older increases your risk of damaged and narrowed arteries and a weakened or thickened heart muscle. Genetic or lifestyle factors cause plaque to build up in your arteries as you age. In men, the risk for coronary heart disease increases starting at age 45. In women, the risk for coronary heart disease increases starting at age 55. About 83% of people who die from heart disease are 65 or older.
- Sex. Men are generally at greater risk of heart disease. The risk for women increases after menopause.
- Sleep apnea. Sleep apnea is a common disorder in which you have one or more pauses in breathing or shallow breaths while you sleep. Untreated sleep apnea can increase your risk for high blood pressure, diabetes, and even a heart attack or stroke.
- Preeclampsia. Preeclampsia (high blood pressure during pregnancy) can occur during pregnancy. The two main signs of preeclampsia are a rise in blood pressure and excess protein in the urine. Preeclampsia is linked to an increased lifetime risk of heart disease, including coronary heart disease, heart attack, heart failure, and high blood pressure. Preeclampsia (high blood pressure during pregnancy) is a risk factor that you can’t control. However, if you’ve had the condition, you should take extra care to monitor your blood pressure and try to lower other heart disease risk factors.
- An autoimmune condition. Having a condition such as rheumatoid arthritis or lupus can increase your risk of a heart attack.
- Mental health problems. Some common mental health conditions include:
- Depression, which is a long-lasting low mood disorder
- Anxiety disorders such as social anxiety disorder, phobias and post-traumatic stress disorder (PTSD)
- Personality disorders such as paranoia, borderline personality disorder and obsessive-compulsive disorder (OCD)
- Bipolar disorder (BPD), previously called manic depression, which causes extreme and unpredictable mood changes
- Psychosis and schizophrenia, which is when a person experiences an altered state of reality
The good news is many heart and cardiovascular diseases are caused by risk factors that can be controlled, treated or modified.
Complications of heart disease include:
- Heart failure. One of the most common complications of heart disease, heart failure occurs when your heart can’t pump enough blood to meet your body’s needs. Heart failure can result from many forms of heart disease, including heart defects, cardiovascular disease, valvular heart disease, heart infections or cardiomyopathy.
- Heart attack. A blood clot blocking the blood flow through a blood vessel that feeds the heart causes a heart attack, possibly damaging or destroying a part of the heart muscle. Atherosclerosis can cause a heart attack.
- Stroke. The risk factors that lead to cardiovascular disease can also lead to an ischemic stroke, which happens when the arteries to your brain are narrowed or blocked so that too little blood reaches your brain. A stroke is a medical emergency — brain tissue begins to die within just a few minutes of a stroke.
- Aneurysm. A serious complication that can occur anywhere in your body, an aneurysm is a bulge in the wall of your artery. If an aneurysm bursts, you may face life-threatening internal bleeding.
- Peripheral artery disease. When you develop peripheral artery disease, your extremities — usually your legs — don’t receive enough blood flow. This causes symptoms, most notably leg pain when walking (claudication). Atherosclerosis also can lead to peripheral artery disease.
- Sudden cardiac arrest. Sudden cardiac arrest is the sudden, unexpected loss of heart function, breathing and consciousness, often caused by an arrhythmia. Sudden cardiac arrest is a medical emergency. If not treated immediately, it results in sudden cardiac death.
You can help reduce your risk of heart disease by taking steps to control factors that put you at greater risk:
- Control your blood pressure. Ask your doctor for a blood pressure measurement at least every two years. He or she may recommend more frequent measurements if your blood pressure is higher than normal or you have a history of heart disease. Optimal blood pressure is less than 120 systolic and 80 diastolic, as measured in millimeters of mercury (mm Hg).
- Lower your cholesterol. Ask your doctor for a baseline cholesterol test when you’re in your 20s and then at least every five years. You may need to start testing earlier if high cholesterol is in your family. If your test results aren’t within desirable ranges, your doctor may recommend more-frequent measurements. Most people should aim for a low-density lipoprotein (LDL or “bad” cholesterol) level below 130 milligrams per deciliter (mg/dL), or 3.4 millimoles per liter (mmol/L). If you have other risk factors for heart disease, you should aim for an LDL level below 100 mg/dL (2.6 mmol/L). If you’re at very high risk of heart disease — if you’ve already had a heart attack or have diabetes, for example — aim for an LDL level below 70 mg/dL (1.8 mmol/L).
- Keep diabetes under control. If you have diabetes, tight blood sugar control can help reduce the risk of heart disease.
- Don’t smoke. Smoking is a major risk factor for heart disease, especially atherosclerosis. One of the best things you can do for your heart is to stop smoking or using smokeless tobacco. Quitting is the best way to reduce your risk of heart disease and its complications. Even if you’re not a smoker, be sure to avoid secondhand smoke. Chemicals in tobacco can damage your heart and blood vessels. Cigarette smoke reduces the oxygen in your blood, which increases your blood pressure and heart rate because your heart has to work harder to supply enough oxygen to your body and brain. There’s good news though. Your risk of heart disease starts to drop in as little as a day after quitting. After a year without cigarettes, your risk of heart disease drops to about half that of a smoker. No matter how long or how much you smoked, you’ll start reaping rewards as soon as you quit.
- Don’t drink or limit your alcohol intake. Alcohol can cause abnormal heart rhythms, high blood pressure, damage to your heart muscle and other diseases such as stroke, liver problems and some cancers. Alcohol is also high in calories so it can lead to weight gain. It also lowers your inhibitions which might mean you find it harder to stick to your healthy eating plans when you have been drinking. If you are trying to lose weight, cut down on alcohol. Drinking more than the recommended amount of alcohol can have a harmful effect on your heart and general health.
- Get enough exercise. Regular, daily physical activity can lower your risk of heart disease. Physical activity helps you achieve and maintain a healthy weight and control diabetes, high cholesterol and high blood pressure — all risk factors for heart disease. If you have a heart arrhythmia or heart defect, there may be some restrictions on the activities you can do, so talk to your doctor. Exercise at least 30 to 60 minutes most days of the week. If you haven’t been active for a while, you may need to slowly work your way up to these goals, but in general, you should aim for at least:
- 150 minutes a week of moderate aerobic exercise, such as walking at a brisk pace
- 75 minutes a week of vigorous aerobic activity, such as running
- Two or more strength training sessions a week
- Even shorter bouts of activity offer heart benefits, so if you can’t meet those guidelines, don’t give up. Just five minutes of moving can help, and activities such as gardening, housekeeping, taking the stairs and walking the dog all count toward your total. You don’t have to exercise strenuously to achieve benefits, but you can see bigger benefits by increasing the intensity, duration and frequency of your workouts.
- Get enough good-quality sleep. Quality sleep is good for your heart. It can be a challenge to make time for good sleep, but it’s important. For two weeks try to get 8 hours of good, quality sleep each night. Yes, each person’s sleep needs vary slightly, but eight is a good number to shoot for.
- Eat healthy foods. A heart-healthy diet based on fruits, vegetables and whole grains — and low in saturated fat, salt (sodium), cholesterol and added sugar — can help you control your weight, blood pressure and cholesterol.
- Maintain a healthy weight. Being overweight increases your risk of heart disease. A body mass index (BMI) of less than 25 and a waist circumference of 35 inches (88.9 centimeters) or less is the goal for preventing and treating heart disease.
- Reduce and manage stress. Reduce stress as much as possible. Practice techniques for managing stress, such as muscle relaxation and deep breathing.
- Get treatment for depression. Being depressed can increase your risk of heart disease significantly. Talk to your doctor if you feel hopeless or uninterested in your life.
- Practice good hygiene. Regularly wash your hands and brush and floss your teeth to keep yourself well.
- Get regular medical checkups. Early detection and treatment can set the stage for a lifetime of better heart health.
Foods that are good for your heart and arteries
A healthy diet can help protect your heart, improve your blood pressure and cholesterol, and reduce your risk of type 2 diabetes. A heart-healthy eating plan includes:
- Vegetables and fruits
- Beans or other legumes
- Lean meats and fish
- Low-fat or fat-free dairy foods
- Whole grains
- Healthy fats, such as olive oil
The following foods are the foundation of a heart-healthy eating plan:
- Vegetables such as leafy greens (spinach, collard greens, kale, cabbage), broccoli, and carrots
- Fruits such as apples, bananas, oranges, pears, grapes, and prunes
- Whole grains such as plain oatmeal, brown rice, and whole-grain bread or tortillas
- Fat-free or low-fat dairy foods such as milk, cheese, or yogurt
- Protein-rich foods:
- Fish high in omega-3 fatty acids (salmon, tuna, and trout)
- Lean meats such as 95% lean ground beef or pork tenderloin or skinless chicken or turkey
- Eggs
- Nuts, seeds, and soy products (tofu)
- Legumes such as kidney beans, lentils, chickpeas, black-eyed peas, and lima beans
- Oils and foods high in monounsaturated and polyunsaturated fats:
- Canola, corn, olive, safflower, sesame, sunflower, and soybean oils (not coconut or palm oil)
- Nuts such as walnuts, almonds, and pine nuts
- Nut and seed butters
- Salmon and trout
- Seeds (sesame, sunflower, pumpkin, or flax)
- Avocados
- Tofu
Research shows that the best foods that protect your heart and blood vessels, include the following:
- Fruits and Vegetables. Current World Health Organization (WHO) recommendations for fruit intake combined with vegetable intake are a minimum 400 g/day 1. A recent meta-analysis indicated that the intake of 800 g/day of fruit was associated with a 27% reductions in relative risk of cardiovascular disease 2.
- Fatty fish (Omega-3 fatty acids). Omega-3 fatty acid is a polyunsaturated fatty acid that must be obtained through dietary intake from fish as well as other types of seafood as it is not produced naturally in the human body 3. Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are essential fatty acids present in omega-3 4. Fatty fish such as salmon, sardines and mackerel are abundant sources of omega-3 fatty acids, healthy unsaturated fats that have been linked to lower blood levels of beta-amyloid—the protein that forms damaging clumps in the brains of people with Alzheimer’s disease. Omega-3 fatty acids are thought to help keep your blood vessels healthy and to help to reduce blood pressure. Research into this style of eating has shown a reduced risk of developing problems such as type 2 diabetes, high blood pressure and raised cholesterol, which are all risk factors for heart disease 5. The American Heart Association recommends eating 2 servings of fish (particularly fatty fish) per week. A serving is 3.5 ounce cooked, or about ¾ cup of flaked fish. Fatty fish like salmon, mackerel, herring, lake trout, sardines and albacore tuna are high in omega-3 fatty acids 6. Eating oily fish is a nutritious choice which can form part of the Mediterranean diet (more bread, fruit, vegetables, fish and less meat, and replacing butter with unsaturated fat spreads). Researchers have also found that people who closely follow a traditional Mediterranean style diet are more likely to live a longer life and also are less likely to become obese. Try to eat fish at least twice a week, but choose varieties that are low in mercury, such as salmon, cod, canned light tuna, and pollack. If you’re not a fan of fish, ask your doctor about taking an omega-3 supplement, or choose terrestrial omega-3 sources such as flaxseeds, avocados, and walnuts. Plant sources of omega-3 fatty acids include flaxseed, oils (olive, canola, flaxseed, soybean), nuts and other seeds (walnuts, butternut squash and sunflower). Replacements for vegans/vegetarians exist that are not supplements, but the evidence is not as robust for plant sources of omega-3 fatty acids.
- Berries. Researchers credit the high levels of flavonoids in berries with the benefit 7. Flavonoids, the natural plant pigments that give berries their brilliant hues, also help improve memory, research shows. Berries contain a particularly high amount of flavonoids called anthocyanidins that are capable of crossing the blood brain barrier and localizing themselves in the hippocampus, an area of the brain known for memory and learning. Epidemiological evidence has established strong inverse associations between flavonoid-rich fruit (e.g. strawberries, grapefruit) and coronary heart disease mortality in cardiovascular disease-free postmenopausal women after multivariate adjustment 8. In a 20-year study of over 16,000 older adult women (aged ≥70 years), those who ate the most blueberries and strawberries had the slowest rates of cognitive decline by up to two-and-a-half years 7.
- Walnuts. Nuts are excellent sources of protein, fat-soluble vitamin E and healthy fats, and one type of nut in particular might also improve memory. A 2015 study from UCLA linked higher walnut consumption to improved cognitive test scores. Walnuts are high in a type of omega-3 fatty acid called alpha-linolenic acid (ALA). Diets rich in alpha-linolenic acid and other omega-3 fatty acids have been linked to lower blood pressure and cleaner arteries. That’s good for both the heart and brain.
- Meat-free meals. Heart-healthy eating encourages consuming meat sparingly. Beans, lentils and soybeans, which pack protein and fiber, make a worthy substitute. They’ll keep you full and are rich in B vitamins, which are important for brain health. In one study analyzing the diets of older adults, those who had the lowest intakes of legumes had greater cognitive decline than those who ate more.
The American Heart Association suggests these daily amounts:
- Vegetables – canned, dried, fresh and frozen vegetables; 5 servings
- Fruits – canned, dried, fresh and frozen fruits; 4 servings
- Whole grains – barley, brown rice, millet, oatmeal, popcorn and whole wheat bread, crackers and pasta; 3-6 servings
- Dairy – low fat (1%) and fat-free dairy products; 3 servings
- Proteins – eggs, fish, lean meat, legumes, nuts, poultry and seeds; 1-2 servings. Eat a variety of fish at least twice a week, especially fish containing omega-3 fatty acids (for example, salmon, trout and herring).
- Oils – polyunsaturated and monounsaturated canola, olive, peanut, safflower and sesame oil; 3 tablespoons
- Limit – sugary drinks, sweets, fatty meats, and salty or highly processed foods
- Choose foods with less salt (sodium) and prepare foods with little or no salt. To lower blood pressure, aim to eat no more than 2,300 milligrams of sodium per day. Reducing daily intake to 1,500 mg is desirable because it can lower blood pressure even further.
- Limit saturated fat and trans fat and replace them with the better fats, monounsaturated and polyunsaturated. If you need to lower your blood cholesterol, reduce saturated fat to no more than 5 to 6 percent of total calories. For someone eating 2,000 calories a day, that’s about 13 grams of saturated fat.
- Avoid – partially hydrogenated oils, tropical oils, and excessive calories
- Replace – highly processed foods with homemade or less-processed options
- If you drink alcohol, drink in moderation. That means no more than one drink per day if you’re a woman and no more than two drinks per day if you’re a man.
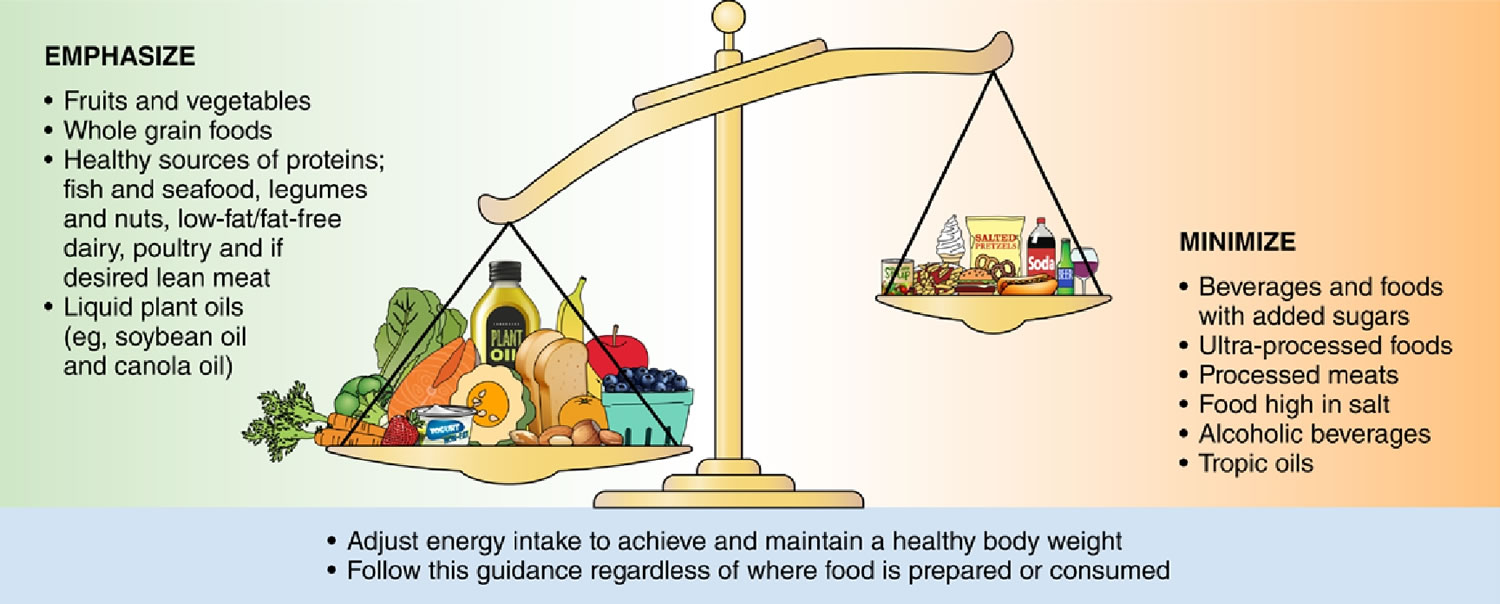
Figure 1. Dietary patterns to promote cardiovascular health
[Source 9 ]2021 American Heart Association Dietary Guidance to Improve Cardiovascular Health
Poor diet is strongly associated with elevated risk of cardiovascular disease morbidity and mortality 9. The American Heart Association evidence-based dietary pattern guidance to promote cardiometabolic health includes the following 9:
- Adjust energy intake and expenditure to achieve and maintain a healthy body weight. To counter the shift toward higher energy intake and more sedentary lifestyles over the past 3 decades, the statement recommends at least 150 minutes of moderate physical activity per week, adjusted for individual’s age, activity level, sex, and size.
- Eat plenty of fruits and vegetables; choose a wide variety. Observational and intervention studies document that dietary patterns rich in varied fruits and vegetables, with the exception of white potatoes, are linked to a lower risk of cardiovascular disease (CVD). Also, whole fruits and vegetables, which more readily provide fiber and satiety, are preferred over juices.
- Choose whole grain foods and products made mostly with whole grains rather than refined grains. Evidence from observational, interventional, and clinical studies confirm the benefits of frequent consumption of whole grains over infrequent consumption or over refined grains in terms of cardiovascular disease risk, coronary heart disease (coronary artery disease), stroke, metabolic syndrome, cardiometabolic risk factors, laxation, and gut microbiota.
- Choose healthy sources of protein, mostly from plants (legumes and nuts).
- Higher intake of legumes, which are rich in protein and fiber, is associated with lower cardiovascular disease risk, while higher nut intake is associated with lower risks of cardiovascular disease, coronary artery disease, and stroke mortality/incidence. Replacing animal-source foods with plant-source whole foods, beyond health benefits, lowers the diet’s carbon footprint. Meat alternatives are often ultraprocessed and evidence on their short- and long-term health effects is limited. Unsaturated fats are preferred, as are lean, nonprocessed meats.
- Use liquid plant oils rather than tropical oils (coconut, palm, and palm kernel), animal fats (butter and lard), and partially hydrogenated fats. Saturated and trans fats (animal and dairy fats, and partially hydrogenated fat) should be replaced with nontropical liquid plant oils. Evidence supports cardiovascular benefits of dietary unsaturated fats, especially polyunsaturated fats primarily from plant oils (e.g. soybean, corn, safflower and sunflower oils, walnuts, and flax seeds).
- Choose minimally processed foods instead of ultraprocessed foods. Because of their proven association with adverse health outcomes, including overweight and obesity, cardiometabolic disorders (type 2 diabetes, cardiovascular disease), and all-cause mortality, the consumption of many ultraprocessed foods is of concern. Ultraprocessed foods include artificial colors and flavors and preservatives that promote shelf stability, preserve texture, and increase palatability. A general principle is to emphasize unprocessed or minimally processed foods.
- Minimize intake of beverages and foods with added sugars. Added sugars (commonly glucose, dextrose, sucrose, corn syrup, honey, maple syrup, and concentrated fruit juice) are tied to elevated risk for type 2 diabetes, high cholesterol, and excess body weight. Findings from meta-analyses on body weight and metabolic outcomes for replacing added sugars with low-energy sweeteners are mixed, and the possibility of reverse causality has been raised.
- Choose and prepare foods with little or no salt. In general, the effects of sodium reduction on blood pressure tend to be higher in Black people, middle-aged and older people, and those with hypertension. In the United States, the main combined sources of sodium intake are processed foods, those prepared outside the home, packaged foods, and restaurant foods. Potassium-enriched salts are a promising alternative.
- If you don’t drink alcohol, don’t start; if you choose to drink, limit intake. While relationships between alcohol intake and cardiovascular outcomes are complex, the 2020 Dietary Guidelines Advisory Committee recently concluded that those who do drink should consume no more than one drink per day and should not drink alcohol in binges; the 2020 Dietary Guidelines for Americans continues to recommend no more than one drink per day for women and two drinks per day for men 10.
- Adhere to this guidance regardless of where food is prepared or consumed.
Carbohydrate
Carbohydrate (starch) is the body’s main energy (fuel) source. Starch is broken down to produce glucose which is used by your body for energy.
Starchy foods are an important part of the healthy diet. They should make up about a third of all the food that you eat. You don’t have to avoid or restrict them because they are ‘fattening’. Instead, be aware of the total amount of starch that you eat. Cutting out one food group, such as carbohydrate can cause dietary imbalance. Starchy foods include bread, potatoes, rice and pasta. Wholegrain options are healthier choices.
Fiber rich foods help your gut to function properly and have many other health benefits. Studies have shown that people who are overweight or obese tend to lose weight if they include plenty of high fiber, starchy carbohydrate in their diets.
Sugar
Sugar is a type of carbohydrate. Like starch, it breaks down into glucose, to provide energy for your body. ‘Free’ sugars are often added to foods during manufacture and include refined sugars such as sucrose (table sugar). This kind of sugar is also found naturally, in unsweetened fruit juices, and in syrups and honey.
Excess consumption of free sugars is linked to the risk of obesity, type 2 diabetes and tooth decay. Many of the free sugars that you consume, are in sugary drinks. A regular can of cola for instance, can contain the equivalent of seven teaspoons of sugar (35g). The guidance about free sugar consumption suggests a daily limit of 30g. This is equivalent to six teaspoons.
The natural sugars found in milk and in whole fruits and vegetables are not free sugars and do not need to be restricted in the same way.
Fruit and vegetables
Fruit and vegetables contain high levels of ‘micronutrients’. These include vitamins, minerals and antioxidants. Micronutrients are essential to the body’s many biochemical processes.
Fruit and vegetables are often high in fiber. They are generally low in calorie and they taste good. The current Dietary Guidelines for Americans recommends at least five portions of different fruit and vegetable per day 11. Like carbohydrate, fruit and vegetable should account for about one third of what you eat, per day. Dried, frozen, tinned, as well as fresh, fruit and veg are all included. One portion of pulses (baked beans, lentils, dried peas) can also count towards your five a day.
Dietary fiber
Fiber comes from plant-based foods, including fruits, vegetables and wholegrains. Dietary fiber is the part of plants that you eat but which doesn’t get digested in your small intestine. Instead, it is completely or partially broken down (fermented) by bacteria in your large intestine. Once broken down in your large intestine, it has been suggested that dietary fibers increase the beneficial bacteria in your gut. This improves your immune system. Fibre includes carbohydrates called polysaccharides and resistant oligosaccharides. Recent research suggests that fiber should be categorized by its physical characteristics; how well it dissolves (solubility), how thick it is (viscosity) and how well it breaks down (fermentability). Some commonly known terms are described below:
- Soluble fiber including pectins and beta glucans is found in foods like fruit and oats.
- Insoluble fiber including cellulose is found in wheat bran and nuts.
- Resistant starch is a soluble fiber that is highly fermentable in the gut. It gets broken down by good bacteria to produce short chain fatty acids (SCFAs). Resistant starch is naturally present in some foods such as bananas, potatoes, grains and pulses.
- Prebiotics are types of carbohydrate that only our gut bacteria can feed upon. Some examples are onions, garlic, asparagus and banana
Fibre is essential for your gut to work normally. It increases good bacteria which supports your immunity against inflammatory disorders and allergies. A high fiber diet seems to reduce the risk of chronic diseases such as heart disease, type 2 diabetes and bowel cancer.
Eating a range of dietary fiber can:
- Improve the diversity of your microbiota
- Improve constipation and lactose intolerance
- Enhance immunity
- Reduce inflammation in your gut
For example, high quality randomized controlled trials have shown that eating oat bran leads to lower blood pressure and lower total cholesterol.
Benefits of a high-fiber diet:
- Normalizes bowel movements. Dietary fiber increases the weight and size of your stool and softens it. A bulky stool is easier to pass, decreasing your chance of constipation. If you have loose, watery stools, fiber may help to solidify the stool because it absorbs water and adds bulk to stool.
- Helps maintain bowel health. A high-fiber diet may lower your risk of developing hemorrhoids and small pouches in your colon (diverticular disease). Studies have also found that a high-fiber diet likely lowers the risk of colorectal cancer. Some fiber is fermented in the colon. Researchers are looking at how this may play a role in preventing diseases of the colon.
- Lowers cholesterol levels. Soluble fiber found in beans, oats, flaxseed and oat bran may help lower total blood cholesterol levels by lowering low-density lipoprotein, or “bad,” cholesterol levels. Studies also have shown that high-fiber foods may have other heart-health benefits, such as reducing blood pressure and inflammation.
- Helps control blood sugar levels. In people with diabetes, fiber — particularly soluble fiber — can slow the absorption of sugar and help improve blood sugar levels. A healthy diet that includes insoluble fiber may also reduce the risk of developing type 2 diabetes.
- Aids in achieving healthy weight. High-fiber foods tend to be more filling than low-fiber foods, so you’re likely to eat less and stay satisfied longer. And high-fiber foods tend to take longer to eat and to be less “energy dense,” which means they have fewer calories for the same volume of food.
- Helps you live longer. Studies suggest that increasing your dietary fiber intake — especially cereal fiber — is associated with a reduced risk of dying from cardiovascular disease and all cancers.
Good sources of dietary fiber include:
- Pulses (like lentils and peas) and beans and legumes (think navy beans, small white beans, split peas, chickpeas, lentils, pinto beans)
- Fruits and vegetables, vegetables such as carrots, broccoli, green peas, and collard greens; fruits especially those with edible skin (like pears and apples with the skin on) and those with edible seeds (like berries)
- Nuts—try different kinds (pumpkin seeds, almonds, sunflower seeds, pistachios and peanuts are a good source of fiber and healthy fats, but be mindful of portion sizes, because they also contain a lot of calories in a small amount!)
- Whole grains such as:
- Quinoa, barley, bulgur, oats, brown rice and farro
- Whole wheat pasta
- Whole grain cereals, including those made from whole wheat, wheat bran and oats
Choose fiber rich foods from a variety of sources including wholegrains, fruit and vegetable, nuts and seeds, beans and pulses. When you read food labels check for the grams of fiber per serving or per 100g. Foods that are naturally high in fiber and contain at least 3 grams per 100 gram are often labeled as a “good source,” and foods labeled as “excellent source” contain more than 5 grams of fiber per serving.
Depending on your age and sex, adults should get 25 to 31 grams of fiber a day 12. Older adults sometimes don’t get enough fiber because they may lose interest in food.
- Men over the age of 50 should get at least 38 grams of fiber per day.
- Women over the age of 50 should get 25 grams per day.
- Children ages 1 to 3 should get 19 grams of fiber per day.
- Children between 4 and 8 years old should get 25 grams per day.
- Girls between 9 and 18 should get 26 grams of fiber each day. Boys of the same age range should get between 31 and 38 grams of fiber per day.
You may wish to see a dietitian if you:
- are unsure about how much and/or what types of fiber you currently have in your diet
- suffer with constipation or diarrhea (e.g. irritable bowel syndrome [IBS])
- have a condition which can restrict your fiber intake (e.g. inflammatory bowel disease)
Keep in mind that if you haven’t been eating a lot of foods high in fiber on a daily basis, it’s important to increase your intake slowly to allow your body to adjust. A sudden increase in eating foods high in fiber (especially foods with added fiber or when using supplements) can cause gas, bloating or constipation. Be sure you are drinking enough water too, because fiber needs water to move through your body.
Protein
Protein is vital. It is your body’s main building block. Proteins help build and maintain muscle, bone, skin, connective tissue, internal organs, and blood. They help fight disease and heal wounds. Protein is found in foods from plants and animals. Animal products such as meat, fish, eggs and dairy are good sources of dietary protein. Meat and fish also provide your body with a form of iron (heme), which is easy to absorb. Fish also contains essential fatty acids (e.g, Omega-3).
Protein also comes from foods of plant origin. Pulses, nuts, and seeds are all high in protein. Pulses are a very good meat alternative, whether or not you are vegetarian or vegan. Most people eat both types of protein. Talk to your dietitian about how to choose the right combination of protein foods for you.
Cutting back on consumption of red meat (beef, lamb, goat, pork) especially, is better for your health and for the environment: current advice is to have no more than 300g of red meat per week. Try to avoid processed meats such as bacon, salami, hot dogs, ham. Consumption of these cured meat products has been linked to a much higher risk of certain gut cancers.
All protein isn’t alike. Protein is built from building blocks called amino acids. Your body makes amino acids in two different ways: Either from scratch, or by modifying others. A few amino acids (known as the essential amino acids) must come from food.
Food protein containing all 9 amino acids in adequate amounts is called complete or high-quality protein.
- ANIMAL FOODS with complete protein include liver (chicken, pork, beef), goose, duck, turkey, chicken, lamb, pork, most fish, rabbit, eggs, milk, cheese (cottage, gjetost, cream, swiss, ricotta, limburger, gruyere, gouda, fontina, edam) and certain beef cuts. Animal foods with incomplete protein include certain yogurts and beef cuts.
- PLANT FOODS with complete protein include spinach, beans (black, cranberry, french, pink, white, winged, yellow), soy, split peas, chickpeas, chestnuts, pistachios, pumpkin seeds, avocado, potatoes, quinoa, a seaweed spirulina, tofu and hummus. Common plant foods with incomplete protein: rice (white and brown), white bread (including whole-wheat), pasta, beans (adzuki, baked, kidney, lima, pinto, snap), peas, lentils, nuts (walnuts, peanuts, hazelnuts, almonds, coconut), sunflower seeds, kamut.
In determining the effectiveness of a protein is accomplished by determining its quality and digestibility. Quality refers to the availability of amino acids that it supplies, and digestibility considers how the protein is best utilized. Typically, all dietary animal protein sources are considered to be complete proteins. That is, a protein that contains all of the essential amino acids 13. Proteins from vegetable sources are incomplete in that they are generally lacking one or two essential amino acids. Thus, someone who desires to get their protein from vegetable sources (i.e. vegetarian, vegan) will need to consume a variety of vegetables, fruits, grains, and legumes to ensure consumption of all essential amino acids. As such, individuals are able to achieve necessary protein requirements without consuming beef, poultry, or dairy 13. Protein digestibility ratings usually involve measuring how the body can efficiently utilize dietary sources of protein. Typically, vegetable protein sources do not score as high in ratings of biological value, net protein utilization, protein digestibility corrected amino acid score and protein efficiency ratio as animal proteins.
Vegetarians need to be aware of this. People who don’t eat meat, fish, poultry, eggs, or dairy products need to eat a variety of protein-containing foods each day in order to get all the amino acids needed to make new protein.
- Animal Protein Foods : Animal sources of protein tend to deliver all the amino acids we need. Meat, such as pork, beef, chicken, turkey, duck / Eggs / Dairy products, such as milk, yogurt, cheese / Fish
- Plant (Vegetable) Protein Foods : Other protein sources, such as fruits, vegetables, grains, nuts and seeds, lack one or more essential amino acids.
- High Protein Plant Foods: Beans, peas, lentils / Soy foods, such as soy milk, tofu / Nuts and nut spreads, such as almond butter, pea
/ nut butter, soy nut butter /Sunflower seeds 14 - Low Protein Plant Foods: Bread, tortillas / Oatmeal, grits, cereals / Pasta, noodles, rice / Rice milk (not enriched).
Finding balance, choosing the right kind and amount of protein.
- When choosing protein, opt for low-fat options, such as lean meats, skim milk or other foods with high levels of protein. Legumes, for example, can pack about 16 grams of protein per cup and are a low-fat and inexpensive alternative to meat.
Choose main dishes that combine meat and vegetables together, such as low-fat soups, or a stir-fry that emphasizes veggies.
- Some high-protein foods are healthier than others because of what comes along with the protein: healthy fats or harmful ones, beneficial fiber or hidden salt. It’s this protein package that’s likely to make a difference for health. For example, a 6-ounce broiled porterhouse steak is a great source of protein—about 40 grams worth. But it also delivers about 12 grams of saturated fat 15. For someone who eats a 2,000 calorie per day diet, that’s more than 60 percent of the recommended daily intake for saturated fat.
- Watch portion size. Aim for 2- to 3-ounce servings.
- If you’re having an appetizer, try a plate of raw veggies instead of a cheese plate. Cheese adds protein, but also fat.
- A 6-ounce ham steak has only about 2.5 grams of saturated fat, but it’s loaded with sodium—2,000 milligrams worth, or about 500 milligrams more than the daily sodium max.
6-ounces of wild salmon has about 34 grams of protein and is naturally low in sodium, and contains only 1.7 grams of saturated fat 15. Salmon and other fatty fish are also excellent sources of omega-3 fats, a type of fat that’s especially good for the heart. Alternatively, a cup of cooked lentils provides about 18 grams of protein and 15 grams of fiber, and it has virtually no saturated fat or sodium 15.
The Vegetarian Society’s Vegetarian sources of protein include 16:
- Nuts, beans and pulses, such as quinoa – these have very high levels of protein
- Cheese
- Eggs – have the perfect balance of amino acids
- Soya is very versatile and found in soya milk, tofu, miso and ready made products such as burgers and sausages
- Quorn is a form of myco-protein and sold in a range of forms
- Rice, grains, pasta, bread and potatoes, although not generally known for their protein, play an important part in your protein intake
Vegetarian food of animal origin such as cheese, milk and eggs have a good balance of essential amino acids. However, food groups such as cereals, rice and legumes (peas, lentils and beans) have an imbalance of 2 of the essential amino acids. To provide a ‘complete’ protein, containing a balance of all 8 essential amino acids, it is recommended to consume a combination of cereals and legumes in your diet e.g. beans on toast.
Dairy
Dairy products and calcium-fortified alternatives are your body’s main source of calcium, which is necessary for the growth, development and maintenance of healthy bones and teeth. Dairy products and alternatives are also a source of protein. Milk, cheese, cream and milk-based sauces and yogurts can have a high saturated fat content. Fat reduced options are recommended, and small quantities.
Fats
Fats also known as lipids, is an essential nutrient (a primary storage form of energy, a kilojoule-dense nutrient) your body need for energy and to help your gut absorb vitamins A, D, E and K from foods. Fat has twice as many calories as proteins or carbohydrates. There are nine calories (37kJ) in every gram of fat, regardless of what type of fat it is. Fats are more energy-dense than carbohydrates and proteins, which provide four calories (17kJ) per gram. Dietary fat also plays a major role in your cholesterol levels. You need some fat in your diet but not too much. There are different types of fats, some are “good” and some are “bad”, however, you should try to avoid “bad” fats. When it comes to dietary fat, what matters most is the type of fat you eat. Contrary to past dietary advice promoting low-fat diets, newer research shows that healthy fats are necessary and beneficial for health.
Healthy fats are unsaturated. They keep cholesterol levels within a healthy range, reduce your risk of heart problems and may be good for the skin, eyes and brain. Unsaturated fats are the best choice for a healthy diet.
Unhealthy fats are saturated and trans fats, which can raise levels of ‘bad’ cholesterol and increase the risk of heart disease. Multiple studies have linked high levels of saturated fat with cognitive decline. A diet that is higher in unsaturated fats and lower in saturated fats is linked to better cognition.
- Saturated fats such as butter, solid shortening, and lard. Eating foods that contain saturated fats raises the level of cholesterol in your blood. High levels of LDL cholesterol (low-density lipoprotein or “bad” cholesterol) in your blood increase your risk of heart disease and stroke. The American Heart Association recommends aiming for a dietary pattern that achieves 5% to 6% of calories from saturated fat. For example, if you need about 2,000 calories a day, no more than 120 of them should come from saturated fat. That’s about 13 grams of saturated fat per day 17.
- Trans fats also known as trans fatty acids or “partially hydrogenated oils”. These are found in vegetable shortenings, some margarines, crackers, cookies, snack foods, and other foods made with or fried in partially hydrogenated oils. By 2018, most U.S. companies will not be allowed to add partially hydrogenated oils to food.
“Bad” fats, such as artificial trans fats and saturated fats, are guilty of the unhealthy things all fats have been blamed for—weight gain, clogged arteries, an increased risk of certain diseases, and so forth. Large studies have found that replacing saturated fats in your diet with unsaturated fats and omega-3 fatty acids can reduce your risk of heart disease by about the same amount as cholesterol-lowering drugs. Since fat is an important part of a healthy diet, rather than adopting a low-fat diet, it’s more important to focus on eating more beneficial “good” fats and limiting harmful “bad” fats. For good health, the majority of the fats that you eat should be monounsaturated or polyunsaturated. Eat foods containing monounsaturated fats and/or polyunsaturated fats such as canola oil, olive oil, safflower oil, sesame oil or sunflower oil instead of foods that contain saturated fats and/or trans fats.
For years you’ve been told that eating fat will add inches to your waistline, raise cholesterol, and cause a myriad of health problems. When food manufacturers reduce fat, they often replace it with carbohydrates from sugar, refined grains, or other starches. Your body digests these refined carbohydrates and starches very quickly, affecting your blood sugar and insulin levels and possibly resulting in weight gain and disease 18. But now scientists know that not all fat is the same. Research has shown that unsaturated fats are good for you. Healthy fats play a huge role in helping you manage your moods, stay on top of your mental game, fight fatigue, and even control your weight. These fats come mostly from plant sources. Cooking oils that are liquid at room temperature, such as canola, peanut, safflower, soybean, and olive oil, contain mostly unsaturated fat. Nuts, seeds, and avocados are also good sources. Fatty fish—such as salmon, sardines, and herring—are rich in unsaturated fats, too. You should actively make unsaturated fats a part of your diet. Of course, eating too much fat will put on the pounds too. Note also that by swapping animal fats for refined carbohydrates—such as replacing your breakfast bacon with a bagel or pastry—won’t have the same benefits. In fact eating refined carbohydrates or sugary foods can have a similar negative effect on your cholesterol levels, your risk for heart disease, and your weight. Limiting your intake of saturated fat can still help improve your health—as long as you take care to replace it with good fat rather than refined carbs. In other words, don’t go no fat, go good fat.
Healthy-eating tips:
- Use olive oil in cooking.
- Replace saturated fats with unsaturated fats; for example, use avocado, tahini, nut or seed butter instead of dairy butter.
- Eat fish, especially oily fish, twice a week.
- Consume legume- or bean-based meals twice a week.
- Snack on nuts or add them to your cooking.
- Throw avocado in salads.
- Choose lean meats and trim any fat you can see (including chicken skin).
- Use table spreads that have less than 0.1g of trans fats per 100g.
Saturated fats
Saturated fats are fat molecules that are “saturated” with hydrogen molecules. Saturated fats are normally solid at room temperature. Saturated fats occur naturally in many foods — primarily meat and dairy foods (butter, cream, full-fat milk and cheese). Beef, lamb, pork on poultry (with the skin on) contain saturated fats, as do butter, cream and cheese made from whole or 2% milk. Plant-based foods that contain saturated fats include coconut, coconut oil, coconut milk and coconut cream, cooking margarine, and cocoa butter, as well as palm oil and palm kernel oil (often called tropical oils). Saturated fats are also found in snacks like chips, cakes, biscuits and pastries, and takeaway foods. Consuming more than the recommended amount of saturated fat is linked to heart disease and high cholesterol.
The American Dietary Guidelines recommend that:
- men should not eat more than 30g of saturated fat a day
- women should not eat more than 20g of saturated fat a day
- children should have less
For people who need to lower their cholesterol, the American Heart Association recommends reducing saturated fat to less than 6% of total daily calories. For someone eating 2,000 calories a day, that’s about 11 to 13 grams of saturated fat 17.
Examples of foods with saturated fat are:
- fatty beef,
- lamb,
- pork,
- poultry with skin,
- beef fat (tallow),
- meat products including sausages and pies,
- lard and cream,
- butter and ghee,
- cheese especially hard cheese like cheddar,
- other dairy products made from whole or reduced-fat (2 percent) milk,
- cream, soured cream and ice cream,
- some savory snacks, like cheese crackers and some popcorns,
- chocolate confectionery,
- biscuits, cakes, and pastries
In addition, many baked goods and fried foods can contain high levels of saturated fats. Some plant-based oils, such as palm oil, palm kernel oil, coconut oil and coconut cream, also contain primarily saturated fats, but do not contain cholesterol.
Unsaturated Fats
If you want to reduce your risk of heart disease, it’s best to reduce your overall fat intake and swap saturated fats for unsaturated fats. Unsaturated fats are in fish, such as salmon, trout and herring, and plant-based foods such as avocados, olives and walnuts. Liquid vegetable oils, such as soybean, corn, safflower, canola, olive and sunflower, also contain unsaturated fats.
There are 2 types of unsaturated fats: monounsaturated and polyunsaturated. Unsaturated fats help reduce your risk of heart disease and lower your cholesterol levels.
- Polyunsaturated fats such as omega-3 and omega-6 fats are found in fish, nuts, and safflower and soybean oil.
- Monounsaturated fats are found in olive and canola oil, avocado, cashews and almonds.
Monounsaturated fats have one (“mono”) unsaturated carbon bond in the molecule. Polyunsaturated fats have more than one (“poly,” for many) unsaturated carbon bonds. Both of these unsaturated fats are typically liquid at room temperature.
Eaten in moderation, both kinds of unsaturated fats may help improve your blood cholesterol when used in place of saturated and trans fats.
Polyunsaturated fats
Polyunsaturated fats are simply fat molecules that have more than one unsaturated carbon bond in the molecule, this is also called a double bond. Oils that contain polyunsaturated fats are typically liquid at room temperature but start to turn solid when chilled. Olive oil is an example of a type of oil that contains polyunsaturated fats.
There are 2 main types of polyunsaturated fats: omega-3 and omega-6. Oils rich in polyunsaturated fats also provide essential fats that your body needs but can’t produce itself – such as omega-6 and omega-3 fatty acids. You must get essential fats through food. Omega-6 and omega-3 fatty acids are important for many functions in the body. A deficiency of essential fatty acids—either omega-3s or omega-6s—can cause rough, scaly skin and dermatitis 19.
Polyunsaturated fats can help reduce bad cholesterol levels in your blood which can lower your risk of heart disease and stroke. Polyunsaturated fats also provide nutrients to help develop and maintain your body’s cells. Oils rich in polyunsaturated fats also contribute vitamin E to the diet, an antioxidant vitamin most Americans need more of.
Foods high in polyunsaturated fat include a number of plant-based oils, including:
- soybean oil
- corn oil
- sunflower oil
Other sources include some nuts and seeds such as walnuts and sunflower seeds, tofu and soybeans.
Omega-6 fats are found in vegetable oils, such as:
- rapeseed
- corn
- sunflower
- some nuts
Omega-3 fats are found in oily fish, such as:
- kippers
- herring
- trout
- sardines
- salmon
- mackerel
The American Heart Association also recommends eating tofu and other forms of soybeans, canola, walnut and flaxseed, and their oils. These foods contain alpha-linolenic acid (ALA), another omega-3 fatty acid.
Polyunsaturated fats (PUFAs) are frequently designated by their number of carbon atoms and double bonds. Alpha-linolenic acid (ALA), for example, is known as C18:3n-3 because it has 18 carbons and 3 double bonds and is an omega-3 fatty acid. Similarly, eicosapentaenoic acid (EPA) is known as C20:5n-3 and docosahexaenoic acid (DHA) as C22:6n-3. Omega-6 fatty acids (omega-6s) have a carbon–carbon double bond that is six carbons away from the methyl end of the fatty acid chain. Linoleic acid (LA) known as C18:2n-6 and arachidonic acid (AA) known as C20:4n-6 are two of the major omega-6s.
The human body can only form carbon–carbon double bonds after the 9th carbon from the methyl end of a fatty acid 20. Therefore, alpha-linolenic acid (ALA) and linoleic acid (LA) are considered essential fatty acids, meaning that they must be obtained from the diet 21. Alpha-linolenic acid (ALA) can be converted into eicosapentaenoic acid (EPA) and then to docosahexaenoic acid (DHA), but the conversion (which occurs primarily in the liver) is very limited, with reported rates of less than 15% 22. Therefore, consuming EPA and DHA directly from foods and/or dietary supplements is the only practical way to increase levels of these fatty acids in the body.
Alpha-linolenic acid (ALA) is present in plant oils, such as flaxseed, soybean, and canola oils 22. Docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) are present in fish, fish oils, and krill oils, but they are originally synthesized by microalgae, not by the fish. When fish consume phytoplankton that consumed microalgae, they accumulate the omega-3s in their tissues 22.
Some researchers propose that the relative intakes of omega-6s and omega-3s—the omega-6/omega-3 ratio—may have important implications for the pathogenesis of many chronic diseases, such as cardiovascular disease and cancer 23, but the optimal ratio—if any—has not been defined 24. Others have concluded that such ratios are too non-specific and are insensitive to individual fatty acid levels 25. Most agree that raising eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) blood levels is far more important than lowering linoleic acid (LA) or arachidonic acid levels.
Currently, most clinicians do not assess omega-3 status, but it can be done by measuring individual omega-3s in plasma or serum phospholipids and expressing them as the percentage of total phospholipid fatty acids by weight 26. Experts have not established normal ranges, but mean values for serum or plasma phospholipid eicosapentaenoic acid (EPA) plus docosahexaenoic acid (DHA) among U.S. adults not taking omega-3 supplements are about 3%–4% 26. Plasma and serum fatty acid values, however, can vary substantially based on an individual’s most recent meal, so they do not reflect long-term dietary consumption 27.
It is also possible to assess omega-3 status via analysis of erythrocyte fatty acids, a measurement that reflects longer-term intakes over approximately the previous 120 days 28. The “omega-3 index” proposed by Harris and von Schacky reflects the content of eicosapentaenoic acid (EPA) plus docosahexaenoic acid (DHA) in erythrocyte membranes expressed as a percentage of total erythrocyte fatty acids 29. This index can be used as a surrogate for assessing tissue levels of eicosapentaenoic acid (EPA) plus docosahexaenoic acid (DHA) 30. Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) typically comprise about 3%–5% of erythrocyte fatty acids in Western populations with low fish intakes. In Japan, where fish consumption is high, erythrocyte eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) levels are about twice those of Western populations 22.
Table 1. Alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) content of selected foods
| Food | Grams per serving | ||
| ALA | DHA | EPA | |
| Flaxseed oil, 1 tbsp | 7.26 | ||
| Chia seeds, 1 ounce | 5.06 | ||
| English walnuts, 1 ounce | 2.57 | ||
| Flaxseed, whole, 1 tbsp | 2.35 | ||
| Salmon, Atlantic, farmed cooked, 3 ounces | 1.24 | 0.59 | |
| Salmon, Atlantic, wild, cooked, 3 ounces | 1.22 | 0.35 | |
| Herring, Atlantic, cooked, 3 ounces* | 0.94 | 0.77 | |
| Canola oil, 1 tbsp | 1.28 | ||
| Sardines, canned in tomato sauce, drained, 3 ounces* | 0.74 | 0.45 | |
| Mackerel, Atlantic, cooked, 3 ounces* | 0.59 | 0.43 | |
| Salmon, pink, canned, drained, 3 ounces* | 0.04 | 0.63 | 0.28 |
| Soybean oil, 1 tbsp | 0.92 | ||
| Trout, rainbow, wild, cooked, 3 ounces | 0.44 | 0.4 | |
| Black walnuts, 1 ounce | 0.76 | ||
| Mayonnaise, 1 tbsp | 0.74 | ||
| Oysters, eastern, wild, cooked, 3 ounces | 0.14 | 0.23 | 0.3 |
| Sea bass, cooked, 3 ounces* | 0.47 | 0.18 | |
| Edamame, frozen, prepared, ½ cup | 0.28 | ||
| Shrimp, cooked, 3 ounces* | 0.12 | 0.12 | |
| Refried beans, canned, vegetarian, ½ cup | 0.21 | ||
| Lobster, cooked, 3 ounces* | 0.04 | 0.07 | 0.1 |
| Tuna, light, canned in water, drained, 3 ounces* | 0.17 | 0.02 | |
| Tilapia, cooked, 3 ounces* | 0.04 | 0.11 | |
| Scallops, cooked, 3 ounces* | 0.09 | 0.06 | |
| Cod, Pacific, cooked, 3 ounces* | 0.1 | 0.04 | |
| Tuna, yellowfin, cooked 3 ounces* | 0.09 | 0.01 | |
| Kidney beans, canned ½ cup | 0.1 | ||
| Baked beans, canned, vegetarian, ½ cup | 0.07 | ||
| Ground beef, 85% lean, cooked, 3 ounces** | 0.04 | ||
| Bread, whole wheat, 1 slice | 0.04 | ||
| Egg, cooked, 1 egg | 0.03 | ||
| Chicken, breast, roasted, 3 ounces | 0.02 | 0.01 | |
| Milk, low-fat (1%), 1 cup | 0.01 | ||
Footnotes: *Except as noted, the U.S. Department of Agriculture (USDA) database does not specify whether fish are farmed or wild caught. **The USDA database does not specify whether beef is grass fed or grain fed.
Essential Fatty Acids
Essential Fatty Acids such as omega-3 oils are ‘essential’ because your body can’t make them and you have to obtain them from your food. Essential Fatty Acids are found in the skin of white fish but also in the flesh of oily fish such as fresh and tinned salmon, mackerel, sardines and fresh tuna. Advice for fish eaters is to have one portion of oily fish, and one portion of white fish per week.
Essential Fatty Acids can also be found in some plant oils such as flaxseed, rapeseed and soya but there is not as much in these oils as there is in fish and seafood.
Omega-3 fatty acids
Omega-3 fatty acids (omega-3s) are a type of polyunsaturated fat and have a carbon–carbon double bond located three carbons from the methyl end of the chain (see Figure 6). Omega-3 fatty acids, sometimes referred to as “n-3s,” are present in certain foods such as flaxseed and fish, as well as dietary supplements such as fish oil. Omega-3 fatty acids are especially beneficial to your health. Omega-3s play important roles in the body as components of the phospholipids that form the structures of cell membranes 19. There are different types of omega-3s: eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are found in fish and algae and have the most health benefits, while alpha-linolenic acid (ALA) comes from plants and is a less potent form of omega-3, although the body does convert ALA to EPA and DHA at low rates. Alpha-linolenic acid (ALA) contains 18 carbon atoms, whereas eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA) are considered “long-chain” omega-3s because EPA contains 20 carbons and DHA contains 22 30.
Docosahexaenoic acid (DHA), in particular, is especially high in the retina, brain, and sperm 22. In addition to their structural role in cell membranes, omega-3s (along with omega-6s) provide energy for the body and are used to form eicosanoids. Eicosanoids are signaling molecules that have similar chemical structures to the fatty acids from which they are derived; they have wide-ranging functions in the body’s cardiovascular, pulmonary, immune, and endocrine systems 20. Higher concentrations of EPA and DHA than arachidonic acid tip the eicosanoid balance toward less inflammatory activity 31.
Research has shown that a diet rich in omega-3 fatty acids may help to:
- Prevent and reduce symptoms of depression, ADHD, and bipolar disorder.
- Protect against memory loss and dementia.
- Reduce the risk of heart disease, stroke, and cancer.
- Ease arthritis, joint pain, and inflammatory skin conditions.
- Support a healthy pregnancy.
- Battle fatigue, sharpen your memory, and balance your mood.
Fish the best source of omega-3 (high in EPA and DHA):
- Anchovies
- Herring
- Salmon
- Mackerel
- Sardines
- Trout
- Tuna
- Mussels
- Oysters
- Halibut
Vegetarian sources of omega-3s (high in ALA):
- Algae such as seaweed (high in EPA and DHA)
- Eggs (small amounts of DHA)
- Flaxseeds and flaxseed oil
- Chia seeds
- Canola and soybean oil
- Walnuts
- Mayonnaise
- Edamame
- Beans (refried, kidney, etc.)
- Brussels sprouts
- Kale
- Spinach
Fish is a good source of protein and omega-3 fatty acids, which are good for your heart. Research has shown that omega-3 fatty acids can reduce your risk of heart disease and stroke. A 2020 Cochrane review 32 of 86 randomized controlled trials published between 1968 and 2019 found that 0.5 g/day to more than 5 g/day omega-3 fatty acids for 12 to 88 months in a total of 162,796 participants reduced serum triglyceride levels by about 15% and slightly decreased rates of cardiovascular mortality and coronary heart disease events. However, the omega-3 fatty acids supplements did not affect all-cause mortality, cardiovascular events, stroke, or arrhythmia. The authors of several earlier meta-analyses and systematic reviews, as well as a 2016 report from the Agency for Healthcare Research and Quality, concluded that omega-3 fatty acids supplements do not appear to significantly reduce the risk of most cardiovascular events 33. Many of these analyses 34, however, but not all 35, did find that omega-3s reduce the risk of cardiac death.
The American Heart Association recommends eating 2 servings of fish (particularly fatty fish) per week. A serving is 3.5 ounce (100 g) cooked, or about ¾ cup of flaked fish. Fatty fish like salmon, mackerel, herring, lake trout, sardines and albacore tuna are high in omega-3 fatty acids. For people with existing coronary heart disease, such as a recent heart attack (myocardial infarction), the American Heart Association recommends approximately 1 gram/day EPA plus DHA, preferably from oily fish; however, supplements could also be considered under the direction of a physician 36. The American Heart Association does not recommend omega-3 supplements for people who do not have a high cardiovascular disease risk.
While omega-3s are best obtained through food, there are many omega-3 and fish oil supplements available. A typical fish oil supplement provides about 1,000 mg fish oil, containing 180 mg EPA and 120 mg DHA, but doses vary widely 37. If you need to substantially lower your triglycerides, your doctor may recommend prescription fish oil, which has been concentrated to contain about 900 mg of EPA plus DHA per capsule. Cod liver oil supplements provide vitamin A and vitamin D in addition to omega-3s. For strict vegetarians or vegans, as well as obtaining ALA from food sources, look for capsules containing DHA and EPA extracted from algae, the original source of omega-3s for fish. Although seafood contains varying levels of methyl mercury (a toxic heavy metal) 38, omega-3 supplements have not been found to contain this contaminant because it is removed during processing and purification 39.
Some types of fish may contain high levels of mercury, PCBs (polychlorinated biphenyls), dioxins and other environmental contaminants. Levels of these substances are generally highest in older, larger, predatory fish and marine mammals.
The benefits and risks of eating fish vary depending on a person’s stage of life.
Children and pregnant women are advised by the U.S. Food and Drug Administration (FDA) to:
- Avoid eating those fish with the potential for the highest level of mercury contamination (such as shark, swordfish, king mackerel or tilefish).
- Eat a variety of fish and shellfish that are lower in mercury (such as canned light tuna, salmon, pollock, catfish).
- Check local advisories about the safety of fish caught by family and friends in local lakes, rivers and coastal areas.
For middle-aged and older men and postmenopausal women, the benefits far outweigh the potential risks when the amount of fish eaten is within the recommendations established by the FDA and Environmental Protection Agency.
Eating a variety of fish will help minimize any potentially adverse effects due to environmental pollutants. Five of the most commonly eaten fish or shellfish that are low in mercury are shrimp, canned light tuna, salmon, pollock, and catfish. Avoid eating shark, swordfish, king Mackerel, or tilefish because they contain high levels of mercury.
Cholesterol
Dietary fat plays a major role in your cholesterol levels. Cholesterol is a type of fat, a wax-like substance that your body needs to function properly that comes from foods such as eggs and is also found in your blood mostly made by your body in your liver. In and of itself, cholesterol isn’t bad. But when you get too much of it, it can have a negative impact on your health. The 2 main types of cholesterol are:
- “Good” cholesterol or HDL (high-density lipoprotein) cholesterol. “Good” HDL cholesterol has a positive effect by taking cholesterol from parts of the body where there’s too much of it to the liver, where it’s disposed of.
- “Bad” cholesterol or LDL (low-density lipoprotein) cholesterol.
High levels of LDL cholesterol (low-density lipoprotein or “bad” cholesterol) can increase your risk of heart disease. The key is to keep your LDL levels low and HDL high, which may protect against heart disease and stroke. High levels of LDL cholesterol (low-density lipoprotein or “bad” cholesterol) can clog arteries and low HDL (high-density lipoprotein or “good” cholesterol) can be a marker for increased cardiovascular risk. However, eating foods that contain any type of cholesterol won’t actually raise your body’s cholesterol levels. Rather than the amount of cholesterol you eat, the biggest influence on your cholesterol levels is the type of fats you consume. Eating saturated or trans fats is far more likely to give you high cholesterol. So instead of counting cholesterol, it’s important to focus on replacing bad fats with good fats.
LDL (bad) cholesterol
LDL (low-density lipoprotein) cholesterol is considered the “bad” cholesterol, because it contributes to fatty buildups in arteries (atherosclerosis). This narrows the arteries and increases the risk for heart attack, stroke and peripheral artery disease. Your body naturally produces all the LDL cholesterol you need. Eating foods containing saturated fats and trans fats causes your body to produce even more LDL — raising the level of “bad” cholesterol in your blood.
HDL (good) cholesterol
HDL (high-density lipoprotein) cholesterol can be thought of as the “good” cholesterol because a healthy level may protect against heart attack and stroke. HDL carries LDL (bad) cholesterol away from the arteries and back to the liver, where the LDL is broken down and passed from the body. But HDL cholesterol doesn’t completely eliminate LDL cholesterol. Only one-third to one-fourth of blood cholesterol is carried by HDL.
Trans fats
Avoid trans fat. Trans fats also known as trans fatty acids or “partially hydrogenated oils”, are created in an industrial process that adds hydrogen to liquid vegetable oils to make them more solid, so they ‘behave’ like a saturated fat. There are two broad types of trans fats found in foods: naturally-occurring and artificial trans fats. Naturally-occurring trans fats are produced in the gut of some animals and foods made from these animals (e.g., milk and meat products) may contain small quantities of these fats. Artificial trans fats (or trans fatty acids) are created in an industrial process that adds hydrogen to liquid vegetable oils to make them more solid.
Trans fats increase the levels of ‘bad’ LDL cholesterol and decreases the levels of ‘good’ HDL cholesterol in your body, which increases your risk of developing heart disease and stroke. Trans fats is also associated with a higher risk of developing type 2 diabetes. Trans fats can be found in many foods such as in butter, margarine (in small amounts), deep-fried and processed foods like doughnuts, cakes and pastries. Baked goods, such as pastries, pizza dough, frozen pizza, pie crust, cookies, biscuits, and crackers also can contain trans fats.
Since 2006, the FDA has required trans fat content to be listed on the Nutrition Facts panel of packaged foods. In recent years, many major national fast-food chains and casual-dining restaurant chains have announced they will no longer use trans fats to fry or deep-fry foods.
The American Heart Association recommends that adults who would benefit from lowering LDL cholesterol eliminate trans fat from their diet.
To find the amount of trans fats in a particular packaged food, look at the Nutrition Facts panel. Companies must list any measurable amount of trans fat (0.5 grams or more per serving) in a separate line in the “Total Fat” section of the panel, directly beneath the line for “Saturated Fat.” This means if a food package states 0 grams of trans fats, it might still have some trans fats if the amount per serving is less than 0.5 g. You can also spot trans fats by reading ingredient lists and looking for the ingredients referred to as “partially hydrogenated oils.”
Salt
Salt or sodium is a mineral that’s essential for life. Table salt is a combination of two minerals — about 40% sodium and 60% chloride. Salt or sodium is regulated by your kidneys, and it helps control your body’s fluid balance. It also helps send nerve impulses and affects muscle function. High levels of salt in your diet can increase blood pressure. High blood pressure is known as the “silent killer” because its symptoms are not always obvious. It’s one of the major risk factors for heart disease, the No. 1 killer worldwide. Ninety percent of American adults are expected to develop high blood pressure over their lifetimes. Because high blood pressure is an important risk factor for stroke, and strokes are detrimental to cognitive health, excessive salt intake is harmful for your brain health. There is a well-established relationship between consuming high levels of sodium and risk of stroke. In Japan, a public health education intervention in the 1960s showed the effectiveness of dietary interventions to reduce sodium intake. A 50% reduction in salt in the diet was associated with an 85% reduction in mortality caused by stroke.
Most of the salt that you eat is added to processed foods. More than 70% of the sodium you consume comes from packaged, prepared and restaurant foods. The rest of the sodium in the diet occurs naturally in food (about 15 percent) or is added when we’re cooking food or sitting down to eat (about 11 percent). Current recommendations from the Dietary Guidelines for Americans are to limit sodium intake to 2,300 milligrams (mg) a day, which amounts to about one teaspoon of salt. The American Heart Association recommends an ideal limit of no more than 1,500 mg per day for most adults. On average, Americans eat more than 3,400 milligrams of sodium each day — much more than the American Heart Association and other health organizations recommend. Because the average American eats so much excess sodium, even cutting back by 1,000 milligrams a day can significantly improve blood pressure and heart health. One estimate suggested that if the U.S. population dropped its sodium intake to 1,500 mg/day (1/2 teaspoon salt), overall blood pressure could decrease by 25.6%, with an estimated $26.2 billion in health care savings. Another estimate projected that achieving this goal would reduce cardiovascular disease deaths by anywhere from 500,000 to nearly 1.2 million over the next decade.
Here are the approximate amounts of sodium in a given amount of salt:
- 1/4 teaspoon salt = 575 mg sodium
- 1/2 teaspoon salt = 1,150 mg sodium
- 3/4 teaspoon salt = 1,725 mg sodium
- 1 teaspoon salt = 2,300 mg sodium
The body needs only a small amount of sodium (less than 500 milligrams per day) to function properly. That’s a mere smidgen — the amount in less than ¼ teaspoon. Very few people come close to eating less than that amount. Plus, healthy kidneys are great at retaining the sodium that your body needs.
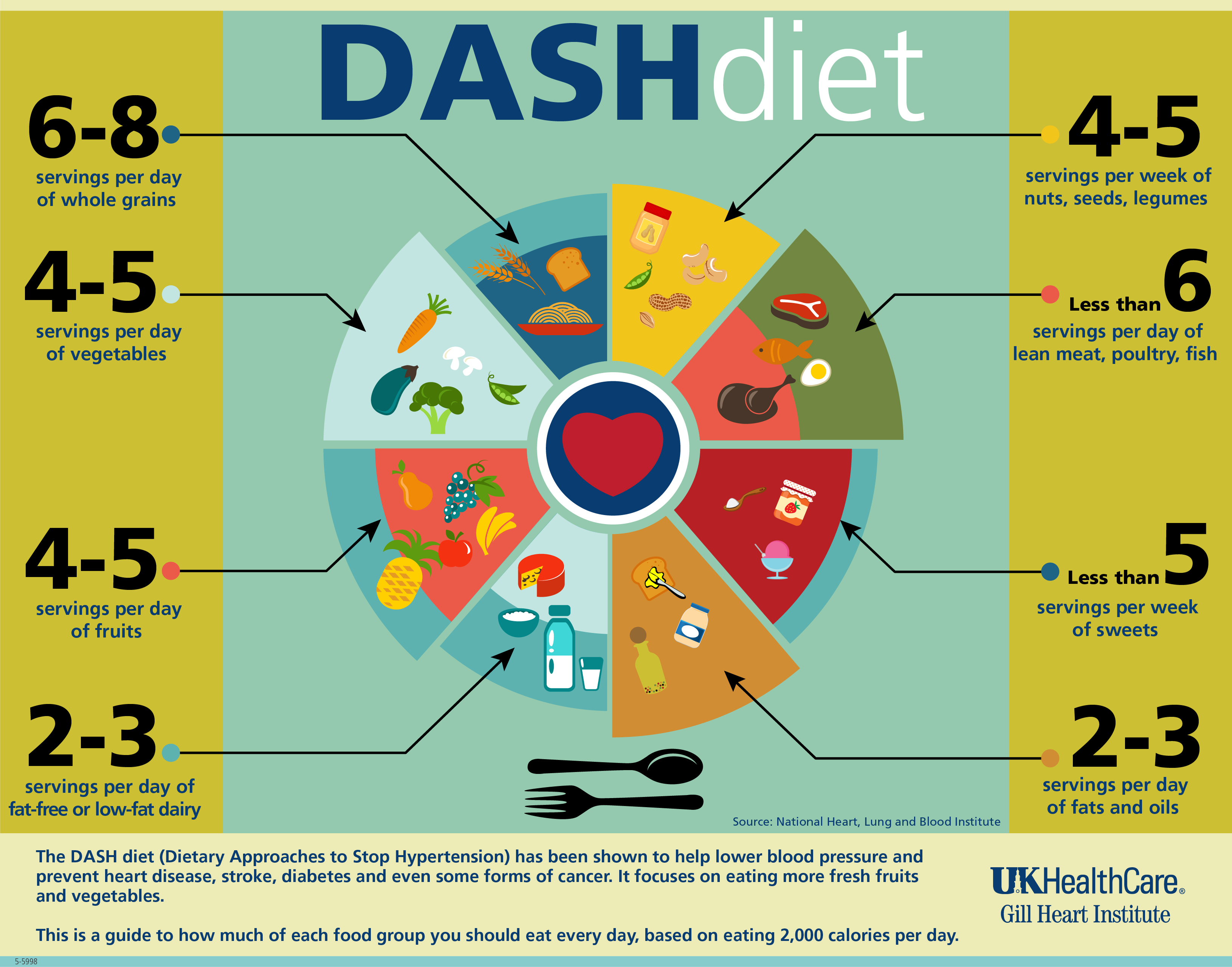
Best heart healthy diet
The typical, contemporary Western diet (high in salt, sugar, excess calories, and saturated fats) is not good for the heart. Eating a heart-healthy diet benefits both your body and your heart. In general, best diet for your heart and arteries is lower in saturated fats. Research in the area of the relationship between diet and your heart point to the benefits of two diets in particular: the DASH (Dietary Approaches to Stop Hypertension) diet and the Mediterranean diet. A plant-based diet that is rich in a variety of fruits and vegetables, particularly green-leafy vegetables and berries, is associated with better heart health. Specific foods (such as olive oil), and particular nutritional supplements (including phenolic compounds like curcumin and quercetin) that may also prove effective for Alzheimer’s disease prevention. These diets can help reduce heart disease and may also be able to reduce risk of dementia.
- Dietary Approaches to Stop Hypertension (DASH) diet
- The DASH diet aims to reduce blood pressure by:
- Eating foods that are low in saturated fat, total fat and cholesterol, and high in fruits, vegetables and low-fat dairy.
- Consuming whole grains, poultry, fish and nuts.
- Decreasing your intake of saturated fats, red meats, sweets, sugared beverages and sodium.
- The DASH diet aims to reduce blood pressure by:
- Mediterranean diet
- The Mediterranean diet incorporates different principles of healthy eating that are typically found in the areas bordering the Mediterranean Sea.
- Focusing on fruit, vegetables, nuts and grains.
- Replacing butter with healthy fats, like olive oil.
- Limiting red meat.
- Using herbs to flavor food rather than salt.
- Eating fish and poultry at least twice a week.
- The Mediterranean diet incorporates different principles of healthy eating that are typically found in the areas bordering the Mediterranean Sea.
Mediterranean diet
“Mediterranean diet” is a generic term based on the traditional eating habits in the countries bordering the Mediterranean Sea 40. There’s not one standard Mediterranean diet. At least 16 countries border the Mediterranean. Eating styles vary among these countries and even among regions within each country because of differences in culture, ethnic background, religion, economy, geography and agricultural production 41. However, there are some common factors. Mediterranean diet is low in saturated fat and high in fiber 42.
A Mediterranean-style diet typically includes:
- plenty of fruits, vegetables, bread and other grains, potatoes, beans, nuts and seeds are eaten daily and make up the majority of food consumed;
- olive oil as a primary fat source, may account for up to 40% of daily calories; and
- small portions of cheese or yogurt are usually eaten each day, along with a serving of fish, poultry, or eggs.
Fish and poultry are more common than red meat in the Mediterranean diet. The Mediterranean diet also centers on minimally processed, plant-based foods. Wine may be consumed in low to moderate amounts, usually with meals. Fruit is a common dessert instead of sweets.
Main meals consumed daily should be a combination of three elements: cereals, vegetables and fruits, and a small quantity of legumes, beans or other (though not in every meal). Cereals in the form of bread, pasta, rice, couscous or bulgur (cracked wheat) should be consumed as one–two servings per meal, preferably using whole or partly refined grains. Vegetable consumption should amount to two or more servings per day, in raw form for at least one of the two main meals (lunch and dinner). Fruit should be considered as the primary form of dessert, with one–two servings per meal. Consuming a variety of colors of both vegetables and fruit is strongly recommended to help ensure intake of a broad range of micronutrients and phytochemicals. The less these foods are cooked, the higher the retention of vitamins and the lower use of fuel, thus minimizing environmental impact.
The Mediterranean Diet is associated with a lower incidence of mortality from all-causes 43 and is also related to lower incidence of cardiovascular diseases 44, type 2 diabetes 45, certain types of cancer 46, and neurodegenerative diseases 47. The Mediterranean diet is now recognized as one of the most healthy food patterns in the world.
Year after year, the Mediterranean diet comes out on top in the U.S. News and World Report annual ranking of best diets. The Mediterranean diet is also touted as one of the healthiest by many health organizations and dietitians 48.
A Mediterranean-style diet is a healthy dietary pattern that:
- emphasizes vegetables, fruits, whole grains, beans and legumes;
- includes low-fat or fat-free dairy products, fish, poultry, non-tropical vegetable oils and nuts; and
- limits added sugars, sugary beverages, sodium, highly processed foods, refined carbohydrates, saturated fats, and fatty or processed meats.
This style of eating can play a big role in preventing heart disease and stroke and reducing risk factors such as obesity, diabetes, high cholesterol and high blood pressure. There is some evidence that a Mediterranean diet rich in virgin olive oil may help the body remove excess cholesterol from arteries and keep blood vessels open.
The Mediterranean Diet is characterized by 49:
- An abundance of plant food (fruit, vegetables, breads, cereals, potatoes, beans, nuts, and seeds);
- Minimally processed, seasonally fresh, locally grown foods;
- Desserts comprised typically of fresh fruit daily and occasional sweets containing refined sugars or honey;
- Olive oil (high in polyunsaturated fat) as the principal source of fat;
- Daily dairy products (mainly cheese and yogurt) in low to moderate amounts;
- Fish and poultry in low to moderate amounts;
- Up to four eggs weekly;
- Red meat rarely; and
- Wine in low to moderate amounts with meals.
Here are some things you can do to switch from a traditional Western-style diet to a more Mediterranean way of eating.
- Dip bread in a mix of olive oil and fresh herbs instead of using butter.
- Add avocado slices to your sandwich instead of bacon.
- Have fish for lunch or dinner instead of red meat. Brush it with olive oil, and broil or grill it.
- Sprinkle your salad with seeds or nuts instead of cheese.
- Cook with olive or canola oil instead of butter or oils that are high in saturated fat.
- Choose whole-grain bread, pasta, rice, and flour instead of foods made with white flour.
- Add ground flaxseed to cereal, low-fat yogurt, and soups.
- Cut back on meat in meals. Instead of having pasta with meat sauce, try pasta tossed with olive oil and topped with pine nuts and a sprinkle of Parmesan cheese.
- Dip raw vegetables in a vinaigrette dressing or hummus instead of dips made from mayonnaise or sour cream.
- Have a piece of fruit for dessert instead of a piece of cake.
- Use herbs and spices instead of salt to add flavor to foods.

DASH diet
DASH stands for Dietary Approaches to Stop Hypertension is similar to a Mediterranean-type diet 50. DASH diet is an eating plan that is based on research studies sponsored by the National Heart, Lung, and Blood Institute 51. The DASH diet is a lifelong approach to healthy eating that’s designed to help treat or prevent high blood pressure (hypertension). The DASH diet encourages you to reduce the sodium in your diet and eat a variety of foods rich in nutrients that help lower blood pressure, such as potassium, calcium and magnesium and eating foods that are low in saturated fat, total fat, and cholesterol, and high in fruits, vegetables, and low fat dairy foods 52.
DASH Diet is a flexible and balanced eating plan that helps you create a heart-healthy eating style for life.
The DASH diet eating plan requires no special foods and has no hard-to-follow recipes. It simply calls for a certain number of daily servings from various food groups to provide your daily and weekly nutritional goals. The Dietary Approaches to Stop Hypertension (DASH) diet recommends 53:
- Grains and grain products: 7–8 servings per day, more than half of which are whole-grain foods
- Fruits: 4–5 servings per day
- Vegetables: 4–5 servings per day
- Low-fat or non-fat dairy foods: 2–3 servings per day
- Lean meats, fish, poultry: 6 or less servings or fewer per day
- Nuts, seeds, and legumes: 4–5 servings per week
- Added fats and oils: 2–3 servings per day
- Sweets: 5 or less servings per week
- Salt (sodium): 1,500 milligrams (mg) sodium lowers blood pressure even further than 2,300 mg sodium daily.
- Limiting foods that are high in saturated fat, such as fatty meats, full-fat dairy products, and tropical oils such as coconut, palm kernel and palm oils
- Limiting sugar-sweetened beverages and sweets.
The DASH diet eating plan includes vegetables, whole grains, poultry, fish, and nuts, and has low amounts of fats, red meats, sweets, and sugared beverages. It is also high in potassium, calcium and magnesium, as well as protein and fiber. The number of servings depends on the number of calories you’re allowed each day. Your calorie level depends on your age, sex, the amount of lean body mass (muscular, athletic, average or overweight), height and, especially, how active you are. Think of this as an energy balance system—if you want to maintain your current weight, you should take in only as many calories as you burn by being physically active. If you need to lose weight, eat fewer calories than you burn or increase your activity level to burn more calories than you eat.
The DASH dietary approach has been shown to lower blood pressure, but little has been published regarding weight loss 50. In fact, a systematic review and meta-analysis on observational prospective studies on the effects of Dietary Approaches to Stop Hypertension (DASH)-style diet, showed that the DASH diet can significantly protect against cardiovascular diseases, coronary heart disease, stroke, and heart failure risk by 20%, 21%, 19% and 29%, respectively 54, 55.
Blood pressure is usually measured in millimeters of mercury (mmHg) and is recorded as two numbers—systolic pressure (as the heart beats) “over” diastolic pressure (as the heart relaxes between beats)—for example, 120/80 mmHg. Both numbers in a blood pressure test are important, but for people who are age 50 or older, systolic pressure gives the most accurate diagnosis of high blood pressure. Systolic pressure is the top number in a blood pressure reading. It is high if it is 140 mmHg or above 56.
High blood pressure is blood pressure higher than 140/90 mmHg and prehypertension is blood pressure between 120/80 and 139/89 mmHg. Prehypertension means that you don’t have high blood pressure now, but are likely to develop it in the future unless you adopt the healthy lifestyle. High blood pressure is dangerous because it makes your heart work too hard, hardens the walls of your arteries, and can cause the brain to hemorrhage or the kidneys to function poorly or not at all. If not controlled, high blood pressure can lead to heart and kidney disease, stroke and blindness.
Being overweight or obese increases your risk of developing high blood pressure. In fact, your blood pressure rises as your body weight increases. Losing even 10 pounds can lower your blood pressure and losing weight has the biggest effect on those who are overweight and already have hypertension. Overweight and obesity are also risk factors for heart disease. And being overweight or obese increases your chances of developing high blood cholesterol and diabetes—two
more risk factors for heart disease.
The original DASH trial 57 consisted of 459 subjects with systolic blood pressures <160 mm Hg and diastolic blood pressures between 80 and 95 mm Hg. For three weeks, all participants were fed a control diet low in fruits, vegetables, and dairy products, and with a fat content typical of an American diet (37% of daily caloric intake). During the following eight weeks, the participants were randomized to one of three diets: the control diet, a diet rich in fruits and vegetables, or the DASH Diet.
The DASH Diet was not low in sodium (salt), but still reduced blood pressure. A meta-analysis of 56 randomized, controlled trials that included over 3,500 participants did not support universal sodium restriction, but instead only recommended dietary sodium restriction in the elderly 58.
The DASH Diet reduced systolic blood pressure by 5.5 mm Hg and diastolic blood pressure by 3.3 mm Hg, as compared with controls. Subgroup analysis showed that African Americans and those with hypertension had the greatest reduction in blood pressure 57 . The DASH diet results might be applied to a larger group due to the heterogeneous population: half of the participants were women, 60% were African American, and 37% had household incomes of <$30,000 per year. One limitation of applying the DASH Diet to the general population is that the study was carried out in a very controlled setting, where all the meals were prepared for the subjects, and thus no comments may be made regarding attrition rates for the diet.
By following the DASH diet, you may be able to reduce your blood pressure by a few points in just two weeks. Over time, your systolic blood pressure could drop by eight to 14 points, which can make a significant difference in your health risks.
Salt or sodium is a mineral that’s essential for life. Table salt is a combination of two minerals — about 40% sodium and 60% chloride. Salt or sodium is regulated by your kidneys, and it helps control your body’s fluid balance. It also helps send nerve impulses and affects muscle function. High levels of salt in your diet can increase blood pressure. High blood pressure is known as the “silent killer” because its symptoms are not always obvious. It’s one of the major risk factors for heart disease, the No. 1 killer worldwide. Ninety percent of American adults are expected to develop high blood pressure over their lifetimes. Because high blood pressure is an important risk factor for stroke, and strokes are detrimental to cognitive health, excessive salt intake is harmful for your brain health. Most of the salt that you eat is added to processed foods. More than 70% of the sodium you consume comes from packaged, prepared and restaurant foods. The rest of the sodium in the diet occurs naturally in food (about 15 percent) or is added when we’re cooking food or sitting down to eat (about 11 percent). The American Heart Association recommends no more than 2,300 milligrams (mg) a day and moving toward an ideal limit of no more than 1,500 mg per day for most adults. On average, Americans eat more than 3,400 milligrams of sodium each day — much more than the American Heart Association and other health organizations recommend. Because the average American eats so much excess sodium, even cutting back by 1,000 milligrams a day can significantly improve blood pressure and heart health. One estimate suggested that if the U.S. population dropped its sodium intake to 1,500 mg/day (1/2 teaspoon salt), overall blood pressure could decrease by 25.6%, with an estimated $26.2 billion in health care savings. Another estimate projected that achieving this goal would reduce cardiovascular disease deaths by anywhere from 500,000 to nearly 1.2 million over the next decade.
Here are the approximate amounts of sodium in a given amount of salt:
- 1/4 teaspoon salt = 575 mg sodium
- 1/2 teaspoon salt = 1,150 mg sodium
- 3/4 teaspoon salt = 1,725 mg sodium
- 1 teaspoon salt = 2,300 mg sodium
The body needs only a small amount of sodium (less than 500 milligrams per day) to function properly. That’s a mere smidgen — the amount in less than ¼ teaspoon. Very few people come close to eating less than that amount. Plus, healthy kidneys are great at retaining the sodium that your body needs.
Table 2. Daily Nutrient Goals Used in the DASH Studies (for a 2,100 Calorie Eating Plan)
| Total fat: 27% of calories | Sodium: 2,300 mg* |
| Saturated fat: 6% of calories | Potassium: 4,700 mg |
| Protein: 18% of calories | Calcium: 1,250 mg |
| Carbohydrate: 55% of calories | Magnesium: 500 mg |
| Cholesterol: 150 mg | Fiber: 30 g |
Footnote: 1,500 mg sodium* was a lower goal tested and found to be even better for lowering blood pressure. It was particularly effective for middle-aged and older individuals, African Americans, and those who already had high blood pressure. The American Heart Association recommends no more than 2,300 milligrams (mg) a day and moving toward an ideal limit of no more than 1,500 mg per day for most adults. On average, Americans eat more than 3,400 milligrams of sodium each day — much more than the American Heart Association and other health organizations recommend. Because the average American eats so much excess sodium, even cutting back by 1,000 milligrams a day can significantly improve blood pressure and heart health.
Abbreviations: g = grams; mg = milligrams
[Source 59 ]How to lower your cholesterol
Cholesterol is a waxy, fat-like substance that’s found in all the cells in your body. Cholesterol is produced by your body and also found in some foods. Your body needs some cholesterol to make hormones, vitamin D and substances that help you digest foods. Cholesterol comes from two sources. Your liver makes all the cholesterol you need. Cholesterol is also found in foods from animal sources, such as egg yolks, meat, and cheese, which is called dietary cholesterol.
There are different types of cholesterol:
- HDL stands for high-density lipoprotein or HDL-C (high-density lipoprotein cholesterol). HDL is sometimes called “good cholesterol” because it carries harmful cholesterol from other parts of your body including your arteries back to your liver. Your liver then removes the cholesterol from your body and helps protect you from heart attack and stroke. A healthy HDL-cholesterol level may protect against heart attack and stroke. Your doctor will evaluate your HDL and other cholesterol levels and other factors to assess your risk for heart attack or stroke. People with high blood triglycerides usually also have lower levels of HDL. Genetic factors, Type 2 diabetes, smoking, being overweight and being sedentary can all lower HDL cholesterol. Women tend to have higher levels of HDL cholesterol than men do, but this can change after menopause.
- LDL stands for low-density lipoprotein or LDL-C (low-density lipoprotein cholesterol). LDL is sometimes called “bad cholesterol” because a high LDL level leads to the buildup of plaque in your arteries. Low-density lipoprotein (LDL or ‘bad’) cholesterol can join with fats and other substances to build up in the inner walls of your arteries. The arteries can become clogged and narrow, and blood flow is reduced. Since LDL is the bad kind of cholesterol, a low LDL level is considered good for your heart health. A diet high in saturated and trans fat is unhealthy because it tends to raise LDL cholesterol levels.
- VLDL stands for very low-density lipoprotein or VLDL-C (very low-density lipoprotein cholesterol). Some people also call VLDL a “bad cholesterol” because it too contributes to the buildup of plaque in your arteries. But VLDL and LDL are different; VLDL mainly carries triglycerides and LDL mainly carries cholesterol. VLDL particles are released into the blood by the liver and circulate in the bloodstream, ultimately being converted into LDL as they lose triglyceride, having carried it to other parts of the body. According to the National Heart, Lung and Blood Institute’s National Cholesterol Education Program Guidelines ATP III, there is growing evidence that VLDL plays an important role in atherogenesis, in which plaques form on the interior walls of arteries, narrowing these passageways and restricting blood flow, which can lead to heart disease and increase the risk of stroke. Currently, direct measurement of VLDL cholesterol requires specialized testing. However, since VLDL-C contains most of the circulating triglyceride (if a person is fasting) and since the composition of the different particles is relatively constant, it is possible to estimate the amount of VLDL-C based on the triglyceride value. To estimate VLDL-C, divide the triglyceride value by 5 if the value is in mg/dL or divide by 2.2 if the value is in mmol/L. In most cases, this formula provides a good estimate of VLDL-C. However, this formula becomes less accurate with increased triglyceride levels when, for example, a person has not fasted before having blood drawn. The calculation is not valid when the triglyceride level is greater than 400 mg/dl (4.5 mmol/L) because other lipoproteins are usually present. In this situation, VLDL-C may be measured directly using specialized testing.
- Triglycerides. Triglycerides are the most common type of fat in your blood. Triglycerides come from food, and your body also makes them. When you eat, your body converts calories it doesn’t need into triglycerides, which are stored in fat cells. High triglyceride levels are associated with several factors, including being overweight, eating too many sweets or drinking too much alcohol, smoking, being sedentary, or having diabetes with elevated blood sugar levels. Normal triglyceride levels vary by age and sex. People with high triglycerides often have a high total cholesterol level, including a high LDL (bad) cholesterol level and a low HDL (good) cholesterol level. Many people with metabolic syndrome or diabetes also have high triglyceride levels. Factors that can contribute to elevated triglyceride levels:
- Overweight or obesity
- Insulin resistance or metabolic syndrome
- Diabetes mellitus, especially with poor glucose control
- Alcohol consumption, especially in excess
- Excess sugar intake, especially from processed foods
- High saturated fat intake
- Hypothyroidism
- Chronic kidney disease
- Physical inactivity
- Pregnancy (especially in the third trimester)
- Inflammatory diseases (such as rheumatoid arthritis, systemic lupus erythematosus
- Some medications may also increase triglycerides.
You can find out the levels of these in your blood and also your total cholesterol level with a cholesterol or lipid profile blood test. If you are concerned about your cholesterol level, talk to your doctor.
Table 3. Desirable Cholesterol Levels
| Desirable Cholesterol Levels | |
|---|---|
| Total cholesterol | Less than 200 milligrams per deciliter of blood (mg/dL) or 5.18 mmol/L |
| LDL (“bad” cholesterol) | Less than 100 mg/dL (2.59 mmol/L) |
| HDL (“good” cholesterol) | 60 mg/dL (1.55 mmol/L) or higher |
| Triglycerides | Less than 150 mg/dL (1.70 mmol/L) |
Footnotes:
Total blood (or serum) cholesterol is a composite of different measurements. Your total blood cholesterol is calculated by adding your HDL and LDL cholesterol levels, plus 20% of your triglyceride level.
Triglycerides are the most common type of fat in your blood. Triglycerides come from food, and your body also makes them. When you eat, your body converts calories it doesn’t need into triglycerides, which are stored in fat cells. High triglyceride levels are associated with several factors, including being overweight, eating too many sweets or drinking too much alcohol, smoking, being sedentary, or having diabetes with elevated blood sugar levels.
“Normal ranges” are less important than your overall cardiovascular risk. Like HDL and LDL cholesterol levels, your total blood cholesterol level should be considered in context with your other known risk factors.
Your doctor can recommend treatment approaches accordingly.
[Source 60 ]The most common cause of high cholesterol is an unhealthy lifestyle. An unhealthy lifestyle makes your body produce more LDL cholesterol than it needs. This can include:
- Unhealthy eating habits or unhealthy diet, such as eating lots of bad fats. One type, saturated fat, is found in some meats, dairy products, chocolate, baked goods, and deep-fried and processed foods. Another type, trans fat, is in some fried and processed foods. Eating these fats can raise your LDL (bad) cholesterol.
- Lack of physical activity, with lots of sitting and little exercise. This lowers your HDL (good) cholesterol.
- Smoking or exposure to tobacco smoke, which lowers HDL cholesterol, especially in women. It also raises your LDL cholesterol.
- Being overweight or obese.
Genetics may also cause people to have high cholesterol. For example, some people inherit genes from their mother, father or even grandparents that cause them to have too much cholesterol. This is called familial hypercholesterolemia (FH). The severity of familial hypercholesterolemia is related to the duration and degree of LDL cholesterol in the blood. Familial hypercholesterolemia is dangerous because it can cause premature atherosclerotic heart disease. Other medical conditions and certain medicines may also cause high cholesterol. If you have a family history of familial hypercholesterolemia or problems related to high cholesterol, get your levels checked.
Factors that can increase your risk of bad cholesterol include:
- Poor diet. Eating saturated fat, found in animal products, and trans fats, found in some commercially baked cookies and crackers and microwave popcorn, can raise your cholesterol level. Foods that are high in cholesterol, such as red meat and full-fat dairy products, will also increase your cholesterol.
- Age. Your cholesterol levels tend to rise as you get older. For instance, as you age, your liver becomes less able to remove LDL cholesterol. Even though it is less common, younger people, including children and teens, can also have high cholesterol.
- Heredity. High blood cholesterol can run in families.
- Weight. Being overweight or having obesity raises your cholesterol level. Having a body mass index (BMI) of 30 or greater puts you at risk of high cholesterol.
- Race. Certain races may have an increased risk of high cholesterol. For example, African Americans typically have higher HDL and LDL cholesterol levels than whites.
- Lack of exercise. Being physically inactive contributes to overweight and can raise LDL and lower HDL. Exercise helps boost your body’s HDL, or “good,” cholesterol while increasing the size of the particles that make up your LDL, or “bad,” cholesterol, which makes it less harmful.
- Smoking. Cigarette smoking damages the walls of your blood vessels, making them more prone to accumulate fatty deposits. Smoking might also lower your level of HDL, or “good,” cholesterol.
- Diabetes. High blood sugar contributes to higher levels of a dangerous cholesterol called very-low-density lipoprotein (VLDL) and lower HDL cholesterol. High blood sugar also damages the lining of your arteries.
You can lower your cholesterol through heart-healthy lifestyle changes. They include a heart-healthy eating plan, weight management, and regular physical activity.
If the lifestyle changes alone do not lower your cholesterol enough, you may also need to take medicines. There are several types of cholesterol-lowering drugs available, including statins. If you take medicines to lower your cholesterol, you still should continue with the lifestyle changes.
Some people with familial hypercholesterolemia (FH) may receive a treatment called lipoprotein apheresis. This treatment uses a filtering machine to remove LDL cholesterol from the blood. Then the machine returns the rest of the blood back to the person.
From a dietary standpoint, the best way to lower your cholesterol is reduce your intake of saturated fat and trans fat. The American Heart Association recommends limiting saturated fat to less than 6% of daily calories and minimizing the amount of trans fat you eat.
Reducing these fats means limiting your intake of red meat and dairy products made with whole milk. Choose skim milk, low-fat or fat-free dairy products instead. It also means limiting fried food and cooking with healthy oils, such as vegetable oil.
A heart-healthy diet emphasizes fruits, vegetables, whole grains, poultry, fish, nuts and nontropical vegetable oils, while limiting red and processed meats, sodium and sugar-sweetened foods and beverages.
Many diets fit this general description. For example, the DASH (Dietary Approaches to Stop Hypertension) eating plan promoted by the National Heart, Lung, and Blood Institute as well as diets suggested by the U.S. Department of Agriculture and the American Heart Association are heart-healthy approaches. Such diets can be adapted based on your cultural and food preferences.
Low cholesterol diet
Diet can play an important role in lowering your cholesterol. To lower your cholesterol levels, follow these healthy diet tips.
You can lower cholesterol over time by eating fewer of the foods that cause high cholesterol and more of the foods that lower cholesterol. The DASH eating plan is one example. DASH stands for Dietary Approaches to Stop Hypertension. DASH diet is an eating plan that is based on research studies sponsored by the National Heart, Lung, and Blood Institute. Clinical studies have shown that DASH diet lowers high blood pressure and improves levels of cholesterol. This reduces your risk of getting heart disease. Other lifestyle changes can help lower your blood pressure. They include staying at a healthy weight, exercising, and not smoking.
The DASH eating plan:
- Emphasizes vegetables, fruits, and whole-grains
- Includes fat-free or low-fat dairy products, fish, poultry, beans, nuts, and vegetable oils
- Limits foods that are high in saturated fat. These foods include fatty meats, full-fat dairy products, and tropical oils such as coconut, palm kernel, and palm oils.
- Limits sugar-sweetened beverages and sweets
Another example of a heart-healthy diet is the Mediterranean diet. The Mediterranean diet is similar to other heart-healthy diets. It promotes foods such as fish, fruits, vegetables, beans, and whole grains. It does not include many meats, dairy products, or sweets. In other ways, the Mediterranean diet is different. For example, it allows for more calories from fats, like olive oil. The Mediterranean diet also allows for moderate intake of wine.
Studies show that the Mediterranean diet has many health benefits. These are greater when combined with exercise. The Mediterranean diet can help you lose or maintain weight. It also helps to manage your blood pressure, blood sugar, and cholesterol levels. In older adults, it can improve your brain function. Following the Mediterranean diet may also protect against some chronic diseases, such as:
- heart disease
- cancer
- type 2 diabetes
- Alzheimer’s disease
- Parkinson’s disease
You can integrate the Mediterranean diet into your lifestyle.
A heart-healthy diet limits some nutrients.
You should also limit both total fat and saturated fat. No more than 25 to 35 percent of your daily calories should come from dietary fats, and less than 7 percent of your daily calories should come from saturated fat. Depending upon how many calories you eat per day, here are the maximum amounts of fats that you should eat:
Table 4. Maximum amounts of total fat and saturated fat in your diet, based on calories
| Calories per Day | Total Fat | Saturated Fat |
| 1500 | 42-58 grams | 10 grams |
| 2000 | 56-78 grams | 13 grams |
| 2500 | 69-97 grams | 17 grams |
Saturated fat is a bad fat because it raises your LDL (bad cholesterol) level more than anything else in your diet. Saturated fat is usually solid at room and refrigerator temperatures. Saturated fat is found in some meats, dairy products, chocolate, baked goods, butter, lard, and coconut and palm oils and deep-fried and processed foods.
- Foods that are high in saturated fat include:
- meat pies
- sausages and fatty cuts of meat
- butter
- lard
- cream
- hard cheese
- cakes and biscuits
- foods that contain coconut or palm oil
Try to replace foods containing saturated fats with foods that are high in unsaturated fats, such as:
- avocados or olives
- oily fish (for example, mackerel and salmon)
- nuts (for example, almonds and cashews)
- seeds (for example, sunflower and pumpkin)
- vegetable oils and spreads (for example, sunflower, olive, corn, walnut and rapeseed oils)
Trans fat also known as trans fatty acids or “partially hydrogenated oils” is another bad fat; it can raise your LDL (bad cholesterol) and lower your HDL (good cholesterol). Trans fat is mostly in foods made with hydrogenated oils and fats, such as stick margarine, crackers, and french fries. Trans fats are created in an industrial process that adds hydrogen to liquid vegetable oils to make them more solid. Instead of these bad fats, try healthier fats, such as lean meat, nuts, and unsaturated oils like canola, olive, and safflower oils.
Limit foods with cholesterol. If you are trying to lower your cholesterol, you should have less than 200 mg a day of cholesterol. Cholesterol is in foods of animal origin, such as liver and other organ meats, egg yolks, shrimp, and whole milk dairy products. Choose reduced fat dairy foods such as milk (preferably unflavored), yogurt (preferably unflavored) and cheese. You can eat smaller amounts of eggs and lean poultry but limit red meat to 1-3 times a week.
Eat plenty of soluble fiber. Fiber comes from plants. Your body can’t really digest it or absorb it into your bloodstream—your body isn’t nourished by it. But it is vital for your good health. Foods high in soluble fiber help prevent your digestive tract from absorbing cholesterol. Furthermore, eating foods rich in fiber can help you feel full on fewer calories, which makes it a good food choice if you need to lose weight. These foods include:
- Whole-grain cereals such as oatmeal, oats and oat bran
- Fruits such as apples, bananas, oranges, pears, and prunes
- Legumes such as kidney beans, lentils, chickpeas, black-eyed peas, and lima beans
Eat lots of fruits and vegetables. A diet rich in fruits and vegetables can increase important cholesterol-lowering compounds in your diet. These compounds, called plant stanols or sterols, work like soluble fiber. Aim to eat at least five portions of fruit and vegetables each day.
Eat fish that are high in omega-3 fatty acids. Omega-3 fatty acids won’t lower your LDL level, but they may help raise your HDL level. They may also protect your heart from blood clots and inflammation and reduce your risk of heart attack. Fish that are a good source of omega-3 fatty acids include salmon, tuna (canned or fresh), and mackerel. Try to eat these fish two times a week. Omega-3 fats are also found in some plant sources, such as walnuts, canola and soybean oils, and flaxseed. In some studies, people who ate fish had a reduced death rate from heart disease. It is possible that this is related to the effects of omega-3 fats, which may help prevent blood clots from forming and inflammation from affecting artery walls. Omega-3 fats also may reduce the risk for heart rhythm problems and, at high doses, reduce triglyceride levels. Studies have suggested that omega-3 fats reduce the risk for heart attack and death from heart disease for those who already have heart disease. Based on what is now known, try to have about two fish meals every week.
Limit salt (sodium). You should try to limit the amount of sodium (salt) that you eat to no more than 2,300 milligrams (about 1 teaspoon of salt) a day. That includes all the sodium you eat, whether it was added in cooking or at the table, or already present in food products. Limiting salt won’t lower your cholesterol, but it can lower your risk of heart diseases by helping to lower your blood pressure. You can reduce your sodium by instead choosing low-salt and “no added salt” foods and seasonings at the table or while cooking. Flavor your foods with herbs and spices rather than salt, and avoid processed foods, prepackaged foods, sauces and canned foods as these contain a lot of salt too.
Avoid added sugar. Sweetened drinks, snacks, and sweet treats are the main source of added sugars in the United States. These include sodas, sweetened coffee and tea, energy drinks, cakes, pies, ice cream, candy, syrups, and jellies. Limit these types of foods and drinks.
Reading the Nutrition labels on foods you buy and eat can help you figure out how much fat, saturated fat, cholesterol, fiber, added sugar and sodium is in the foods that you buy.
Limit alcohol. Alcohol adds extra calories, which can lead to weight gain. Being overweight can raise your LDL level and lower your HDL level. Too much alcohol can also increase your risk of heart diseases because it can raise your blood pressure and triglyceride level. One drink is a glass of wine, beer, or a small amount of hard liquor, and the recommendation is that:
- Men should have no more than two drinks containing alcohol a day
- Women should have no more than one drink containing alcohol a day.
Reduce saturated fat in meat and poultry
The American Heart Association recommends a diet that emphasizes fish and poultry and limits red meat. The amount of saturated fat in meats can vary widely, depending on the cut and how it’s prepared.
Here are some ways to reduce the saturated fat in meat:
- Select lean cuts of meat with minimal visible fat. Lean beef cuts include the round, chuck, sirloin or loin. Lean pork cuts include the tenderloin or loin chop. Lean lamb cuts come from the leg, arm and loin.
- Buy “choice” or “select” grades rather than “prime.” Select lean or extra lean ground beef.
- Trim all visible fat from meat before cooking.
- Broil rather than pan-fry meats such as hamburger, lamb chops, pork chops and steak.
- Use a rack to drain off fat when broiling, roasting or baking. Instead of basting with drippings, keep meat moist with wine, fruit juices or a heart-healthy oil-based marinade.
- Cook a day ahead of time. Stews, boiled meat, soup stock or other dishes in which fat cooks into the liquid can be refrigerated. Later, remove the hardened fat from the top.
- When a recipe calls for browning the meat first, try browning it under the broiler instead of in a pan.
- Eat chicken and turkey rather than duck and goose, which are usually higher in fat. Choose white meat most often when eating poultry.
- Remove the skin from chicken or turkey before cooking. If your poultry dries out too much, first try basting with wine, fruit juices or a heart-healthy oil-based marinade. Or leave the skin on for cooking and then remove it before eating.
- Limit processed meats such as sausage, bologna, salami and hot dogs. Many processed meats – even those with “reduced fat” labels – are high in calories and saturated fat. Such foods are often high in sodium, too. Read labels carefully and eat processed meats only occasionally.
Eat more fish
Fish can be fatty or lean, but it’s still low in saturated fat. Eat at least 8 ounces of non-fried fish each week. Choose oily fish such as salmon, trout and herring, which are high in omega-3 fatty acids. Prepare fish baked, broiled, grilled or boiled rather than breaded and fried, and without added salt, saturated fat or trans fat. Non-fried fish and shellfish, such as shrimp, crab and lobster, are low in saturated fat and are a healthy alternative to many cuts of meat and poultry.
Research has shown the health benefits of eating seafood rich in omega-3 fatty acids, especially when it replaces less healthy proteins that are high in saturated fat and low in unsaturated fat. Including seafood high in omega-3 fatty acids as part of a heart-healthy diet can help reduce the risk of heart failure, coronary heart disease, cardiac arrest and the most common type of stroke (ischemic).
Eat less meat
Try meatless meals featuring vegetables or beans. For example, think eggplant lasagna, or instead of a burger, consider a big grilled portobello mushroom on a bun. Maybe substitute low-sodium beans for beans-n-franks. Or treat meat as a sparingly used ingredient, added mainly for flavor in casseroles, stews, low-sodium soups and spaghetti.
Eat more vegetables
A growing body of scientific evidence indicates that wholesome vegetarian diets offer distinct advantages compared to diets containing meat and other foods of animal origin. The benefits arise from lower intakes of saturated fat, cholesterol and animal protein as well as higher intakes of complex carbohydrates, dietary fiber, magnesium, folic acid, vitamin C and E, carotenoids and other phytochemicals.
Try cooking vegetables in a tiny bit of vegetable oil and add a little water during cooking, if needed. Or use a vegetable oil spray. Just one or two teaspoons of oil is enough for a package of plain frozen vegetables that serves four. Place the vegetables in a skillet with a tight cover and cook them over very low heat until done.
Add herbs and spices to make vegetables even tastier. It’s a healthier choice than opting for pre-packaged vegetables with heavy sauce or seasonings. For example, these combinations add subtle and surprising flavors:
- Rosemary with peas, cauliflower and squash
- Oregano with zucchini
- Dill with green beans
- Marjoram with Brussels sprouts, carrots and spinach
- Basil with tomatoes
Start with a small quantity of herbs and spices (1/8 to 1/2 teaspoon for a package of frozen vegetables), then let your family’s feedback be your guide. Chopped parsley and chives, sprinkled on just before serving, can also enhance the flavor of many vegetables.
Limiting saturated and trans fats
Here are some ways to lower your intake of saturated and trans fats:
- Maintain a diet that emphasizes fruits, vegetables, whole grains, low-fat dairy products, poultry, fish and nuts. Also limit red meat and sugar-sweetened foods and beverages.
- Opt for naturally occurring unhydrogenated vegetable oils such as canola, safflower, sunflower or olive oil.
- Look for processed foods made with unhydrogenated oil rather than saturated fat or hydrogenated (or partially hydrogenated) vegetable oils.
- Use soft margarine as a substitute for butter and choose soft margarines (liquid or tub varieties) over harder stick forms. Look for “0 g trans fat” on the Nutrition Facts label.
- Doughnuts, cookies, crackers, muffins, pies and cakes are examples of foods high in trans fat. Don’t eat them often.
- Limit commercially fried foods and baked goods made with shortening or partially hydrogenated vegetable oils. These foods are very high in fat, and it’s likely to be trans fat.
- Limit fried fast food. Commercial shortening and deep-frying fats are still made by hydrogenation and contain saturated and trans fats.
Consider using a food diary to keep track of what you eat. It’s a handy way to evaluate the healthy, not-so-healthy and unhealthy foods you’re making a part of your everyday diet.
Use liquid vegetable oils in place of solid fats
Liquid vegetable oils such as canola, safflower, sunflower, soybean and olive oil can often be used instead of solid fats, such as butter, lard or shortening. If you must use margarine, try the soft or liquid kind.
Use a little liquid oil to:
- Pan-fry fish and poultry.
- Sauté vegetables.
- Make cream sauces and soups using low-fat or fat-free milk.
- Add to whipped or scalloped potatoes using low-fat or fat-free milk.
- Brown rice for Spanish, curried or stir-fried rice.
- Cook dehydrated potatoes and other prepared foods that call for fat to be added.
- Make pancakes or waffles.
Puree fruits and veggies for baking
Pureed fruits or vegetables can be used in place of oil in muffin, cookie, cake and snack bar recipes to give your treats an extra healthy boost. For many recipes, use the specified amount of puree instead of oil. Check the mix’s package or your cookbook’s substitutions page for other conversions. You can:
- Use applesauce in spice muffins or oatmeal cookies.
- Include bananas in breads and muffins.
- Try zucchini in brownies.
Lower dairy fats
Low-fat (1%) or fat-free (skim) milk can be used in many recipes in place of whole milk or half-and-half. (Some dishes, such as puddings, may result in a softer set.)
When it comes to cheeses used in recipes, you can substitute low-fat, low-sodium cottage cheese, part-skim milk mozzarella (or ricotta) cheese, and other low-fat, low-sodium cheeses with little or no change in consistency.
Increase fiber and whole grains
Fiber is a substance found in plants. Dietary fiber, the kind you eat, is found in fruits, vegetables, and grains. Your body cannot digest fiber, so it passes through your intestines without being absorbed much.
Dietary fiber adds bulk to your diet. Because it makes you feel full faster and for longer, it can help you with weight loss efforts or to maintain a healthy weight.
High fiber diets can also help with constipation.
Slowly increase the amount of fiber in your diet. If you have bloating or gas, you have probably eaten too much and need to reduce the amount of fiber you eat for a few days. Drink plenty of fluids. When you increase fiber in your diet, you also need to get enough fluids. Not getting enough fluids may make constipation worse instead of better. Ask your health care provider or a dietitian how much fluid you should be getting each day.
The daily recommended intake (DRI) of fiber for adults 19 to 50 years old is 38 grams a day for men and 25 grams a day for women. To get more fiber into your diet, eat different types of foods, such as:
- Fruits
- Vegetables
- Whole grains
Vegetables, Legumes, and Nuts
Vegetables are a good source of fiber. Eat more:
- Lettuce, Swiss chard, raw carrots, and spinach
- Tender cooked vegetables, such as asparagus, beets, mushrooms, turnips, and pumpkin
- Baked potatoes and sweet potatoes with skin
- Broccoli, artichokes, squashes, and string beans
You can also get more fiber by eating:
- Legumes, such as lentils, black beans, split peas, kidney beans, lima beans, and chickpeas
- Nuts and seeds, such as sunflower seeds, almonds, pistachios, and pecans
Fruits
Fruits are another good source of fiber. Eat more:
- Apples and bananas
- Peaches and pears
- Tangerines, prunes, and berries
- Figs and other dried fruits
Grains
Grains are another important source of dietary fiber. Eat more:
- Hot cereals, such as oatmeal and farina
- Whole-grain breads
- Brown rice
- Popcorn
- High-fiber cereals, such as bran, shredded wheat, and puffed wheat
- Whole-wheat pastas
- Bran muffins
Consider these heart-smart choices:
- Toast and crush (or cube) fiber-rich whole-grain bread to make breadcrumbs, stuffing or croutons.
- Replace the breadcrumbs in your meatloaf with uncooked oatmeal.
- Serve whole fruit at breakfast in place of juice.
- Use brown rice instead of white rice and try whole grain pasta.
- Add lots of colorful veggies to your salad – carrots, broccoli and cauliflower are high in fiber and give your salad a delicious crunch.
Foods that lower cholesterol
Here are some foods to improve your cholesterol and protect your heart.
Oatmeal, oat bran and high-fiber foods
Oatmeal contains soluble fiber, which reduces your low-density lipoprotein (LDL) cholesterol, the “bad” cholesterol. Soluble fiber is also found in such foods as kidney beans, Brussels sprouts, apples and pears.
Soluble fiber can reduce the absorption of cholesterol into your bloodstream. Five to 10 grams or more of soluble fiber a day decreases your LDL cholesterol. One serving of a breakfast cereal with oatmeal or oat bran provides 3 to 4 grams of fiber. If you add fruit, such as a banana or berries, you’ll get even more fiber.
Fish and omega-3 fatty acids
Fatty fish has high levels of omega-3 fatty acids, which can reduce your triglycerides — a type of fat found in blood — as well as reduce your blood pressure and risk of developing blood clots. In people who have already had heart attacks, omega-3 fatty acids may reduce the risk of sudden death.
Omega-3 fatty acids don’t affect LDL cholesterol levels. But because of those acids’ other heart benefits, the American Heart Association recommends eating at least two servings of fish a week. Baking or grilling the fish avoids adding unhealthy fats.
The highest levels of omega-3 fatty acids are in:
- Mackerel
- Herring
- Tuna
- Salmon
- Trout
Foods such as walnuts, flaxseed and canola oil also have small amounts of omega-3 fatty acids.
Omega-3 and fish oil supplements are available. Talk to your doctor before taking any supplements.
Almonds and other nuts
Almonds, peanuts and other tree nuts can improve blood cholesterol. Walnuts are especially high in omega-3 fatty acids, the same heart-healthy fat found in oily fish, but are a lot easier to stash in your pocket or purse. A recent study concluded that a diet supplemented with walnuts can lower the risk of heart complications in people with history of a heart attack. All nuts are high in calories, so a handful added to a salad or eaten as a snack will do.
All nuts will go bad (rancid) in time so keep them in the fridge. The same goes for nut oils and nut butters in jars after you’ve opened them. Rancid nuts have an unpleasant smell and bitter taste.
Avocados
Avocados are a potent source of nutrients as well as monounsaturated fatty acids (MUFAs). Research suggests that adding an avocado a day to a heart-healthy diet can help improve LDL cholesterol levels in people who are overweight or obese.
People tend to be most familiar with avocados in guacamole, which usually is eaten with high-fat corn chips. Try adding avocado slices to salads and sandwiches or eating them as a side dish. Also try guacamole with raw cut vegetables, such as cucumber slices.
Replacing saturated fats, such as those found in meats, with MUFAs are part of what makes the Mediterranean diet heart healthy.
Olive oil
Try using olive oil in place of other fats in your diet. You can saute vegetables in olive oil, add it to a marinade or mix it with vinegar as a salad dressing. You can also use olive oil as a substitute for butter when basting meat or as a dip for bread.
Foods with added plant sterols or stanols
There is evidence that foods that contain certain added ingredients, such as plant sterols and stanols, can reduce levels of cholesterol in the blood. Sterols and stanols are substances found in plants that help block the absorption of cholesterol. Plant sterols and stanols are found in nuts, seeds and legumes, vegetable oils, breads and cereals, and fruits and vegetables. You need to eat 2 to 3 grams a day of plant sterols and stanols to assist in reducing high cholesterol. Eating more is not harmful, but you won’t get any additional benefits.
Foods that have been fortified with sterols or stanols are available.
Margarines, low-fat milks, low-fat yogurts and breakfast cereals, lower fat cheese, processed cheese and orange juice with added plant sterols can help reduce LDL cholesterol. Adding 2 grams of sterol to your diet every day can lower your LDL cholesterol by 5 to 15 percent. People who do not have high cholesterol should not eat these products regularly, particularly children and pregnant or breastfeeding women.
If you do eat foods that are designed to lower cholesterol, read the label carefully to avoid eating too much.
You should not eat foods fortified with plant sterols as a substitute for medication. You can use plant sterol-enriched foods while taking cholesterol medication, but check with your doctor first.
However, it’s not clear whether food with plant sterols or stanols reduces your risk of heart attack or stroke — although experts assume that foods that reduce cholesterol do reduce the risk. Plant sterols or stanols don’t appear to affect levels of triglycerides or of high-density lipoprotein (HDL) cholesterol, the “good” cholesterol.
Whey protein
Whey protein, which is found in dairy products, may account for many of the health benefits attributed to dairy. Studies have shown that whey protein given as a supplement lowers both LDL and total cholesterol as well as blood pressure. You can find whey protein powders in health food stores and some grocery stores.
References- WHO. Diet, nutrition and the prevention of chronic diseases. Report of a Joint FAO, WHO Expert Consultation. WHO Technical Report Series. Geneva: World Helath Organization; 2003.
- Aune D, Giovannucci E, Boffetta P, Fadnes LT, Keum N, Norat T, Greenwood DC, Riboli E, Vatten LJ, Tonstad S. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality—a systematic review and dose-response meta-analysis of prospective studies. Int J Epidemiol. 2017;46(3):1029–1056. doi: 10.1093/ije/dyw319
- Davis B.A., Prall B.C. The challenges of incorporation of omega-3 fatty acids into ration components and their prevalence in garrison feeding. Military medicine. 2014;179:162–167. doi: 10.7205/MILMED-D-14-00172
- Bailes J.E., Patel V. The potential for DHA to mitigate mild traumatic brain injury. Mil. Med. 2014;179:112–116. doi: 10.7205/MILMED-D-14-00139
- Michael I McBurney, Nathan L Tintle, Ramachandran S Vasan, Aleix Sala-Vila, William S Harris, Using an erythrocyte fatty acid fingerprint to predict risk of all-cause mortality: the Framingham Offspring Cohort, The American Journal of Clinical Nutrition, 2021;, nqab195, https://doi.org/10.1093/ajcn/nqab195
- Fish and Omega-3 Fatty Acids. https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/fats/fish-and-omega-3-fatty-acids
- Devore, E. E., Kang, J. H., Breteler, M. M., & Grodstein, F. (2012). Dietary intakes of berries and flavonoids in relation to cognitive decline. Annals of neurology, 72(1), 135–143. https://doi.org/10.1002/ana.23594
- Mink PJ, Scrafford CG, Barraj LM, Harnack L, Hong CP, Nettleton JA, Jacobs DR., Jr Flavonoid intake and cardiovascular disease mortality: a prospective study in postmenopausal women. Am J Clin Nutr. 2007;85(3):895–909. doi: 10.1093/ajcn/85.3.895
- Lichtenstein AH, Appel LJ, Vadiveloo M, Hu FB, Kris-Etherton PM, Rebholz CM, Sacks FM, Thorndike AN, Van Horn L, Wylie-Rosett J; American Heart Association Council on Lifestyle and Cardiometabolic Health; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; and Stroke Council. 2021 Dietary Guidance to Improve Cardiovascular Health: A Scientific Statement From the American Heart Association. Circulation. 2021 Nov 2:CIR0000000000001031. https://doi.org/10.1161/CIR.0000000000001031
- Scientific Report of the 2020 Dietary Guidelines Advisory Committee. https://www.dietaryguidelines.gov/2020-advisory-committee-report
- https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2015-2020. https://health.gov/sites/default/files/2019-09/2015-2020_Dietary_Guidelines.pdf
- J Sports Sci Med. 2004 Sep; 3(3): 118–130. International Society of Sports Nutrition Symposium, June 18-19, 2005, Las Vegas NV, USA – Symposium – Macronutrient Utilization During Exercise: Implications For Performance And Supplementation. Protein – Which is Best ? https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3905294
- The National Kidney Disease Education Program. Protein – tips for people with chronic kidney disease. https://www.niddk.nih.gov/health-information/health-communication-programs/nkdep/a-z/nutrition-protein/Documents/nutrition-protein-508.pdf
- Agriculture, U.D.o., USDA Nutrient Database for Standard Reference, Release 14. 2005.
- The Vegetarian Society. Protein. https://www.vegsoc.org/facts/protein
- The Skinny on Fats. https://www.heart.org/en/health-topics/cholesterol/prevention-and-treatment-of-high-cholesterol-hyperlipidemia/the-skinny-on-fats
- Jakobsen, M.U., et al., Intake of carbohydrates compared with intake of saturated fatty acids and risk of myocardial infarction: importance of the glycemic index. Am J Clin Nutr, 2010. 91(6): p. 1764-8.
- Institute of Medicine, Food and Nutrition Board. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids (macronutrients). Washington, DC: National Academy Press; 2005.
- Jones PJH, Rideout T. Lipids, sterols, and their metabolites. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, eds. Modern Nutrition in Health and Disease. 11th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2014.
- Jones PJH, Papamandjaris AA. Lipids: cellular metabolism. In: Erdman JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. 10th ed. Washington, DC: Wiley-Blackwell; 2012:132-48.
- Harris WS. Omega-3 fatty acids. In: Coates PM, Betz JM, Blackman MR, et al., eds. Encyclopedia of Dietary Supplements. 2nd ed. London and New York: Informa Healthcare; 2010:577-86.
- Simopoulos AP. The importance of the omega-6/omega-3 fatty acid ratio in cardiovascular disease and other chronic diseases. Exp Biol Med (Maywood). 2008 Jun;233(6):674-88. doi: 10.3181/0711-MR-311
- Wang C, Chung M, Lichtenstein A, Balk E, Kupelnick B, DeVine D, et al. Effects of omega-3 fatty acids on cardiovascular disease. Summary, evidence report/technology assessment no. 94. (Prepared by the Tufts New England Medical Center Evidence-based Practice Center, Boston, MA.) AHRQ Publication No. 04-E009-1. Agency for Healthcare Research and Quality, 2004. https://archive.ahrq.gov/downloads/pub/evidence/pdf/o3cardio/o3cardio.pdf
- Harris WS, Davidson MH. RE: Plasma phospholipid fatty acids and prostate cancer risk in the SELECT trial. J Natl Cancer Inst. 2014 Apr;106(4):dju019. doi: 10.1093/jnci/dju019
- Brasky TM, Darke AK, Song X, Tangen CM, Goodman PJ, Thompson IM, Meyskens FL Jr, Goodman GE, Minasian LM, Parnes HL, Klein EA, Kristal AR. Plasma phospholipid fatty acids and prostate cancer risk in the SELECT trial. J Natl Cancer Inst. 2013 Aug 7;105(15):1132-41. doi: 10.1093/jnci/djt174
- Harris WS. Are n-3 fatty acids still cardioprotective? Curr Opin Clin Nutr Metab Care. 2013 Mar;16(2):141-9. doi: 10.1097/MCO.0b013e32835bf380
- Agency for Healthcare Research and Quality. Omega-3 fatty acids and cardiovascular disease – 2015. https://effectivehealthcare.ahrq.gov/products/fatty-acids-cardiovascular-disease/research-protocol
- Harris WS. The omega-3 index as a risk factor for coronary heart disease. Am J Clin Nutr. 2008 Jun;87(6):1997S-2002S. doi: 10.1093/ajcn/87.6.1997S
- Metcalf RG, Cleland LG, Gibson RA, Roberts-Thomson KC, Edwards JR, Sanders P, Stuklis R, James MJ, Young GD. Relation between blood and atrial fatty acids in patients undergoing cardiac bypass surgery. Am J Clin Nutr. 2010 Mar;91(3):528-34. doi: 10.3945/ajcn.2009.28302
- James M, Proudman S, Cleland L. Fish oil and rheumatoid arthritis: past, present and future. Proc Nutr Soc. 2010 Aug;69(3):316-23. doi: 10.1017/S0029665110001564
- Abdelhamid AS, Brown TJ, Brainard JS, Biswas P, Thorpe GC, Moore HJ, Deane KH, Summerbell CD, Worthington HV, Song F, Hooper L. Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2020 Feb 29;3(2):CD003177. doi: 10.1002/14651858.CD003177.pub5
- Weylandt KH, Serini S, Chen YQ, Su HM, Lim K, Cittadini A, Calviello G. Omega-3 Polyunsaturated Fatty Acids: The Way Forward in Times of Mixed Evidence. Biomed Res Int. 2015;2015:143109. doi: 10.1155/2015/143109
- Casula M, Soranna D, Catapano AL, Corrao G. Long-term effect of high dose omega-3 fatty acid supplementation for secondary prevention of cardiovascular outcomes: A meta-analysis of randomized, placebo controlled trials [corrected]. Atheroscler Suppl. 2013 Aug;14(2):243-51. doi: 10.1016/S1567-5688(13)70005-9. Erratum in: Atheroscler Suppl. 2014 Mar;233(1):122.
- Agency for Healthcare Research and Quality. Omega-3 fatty acids and cardiovascular disease: an updated systematic review. 2016. https://effectivehealthcare.ahrq.gov/products/fatty-acids-cardiovascular-disease/research
- Siscovick DS, Barringer TA, Fretts AM, Wu JH, Lichtenstein AH, Costello RB, Kris-Etherton PM, Jacobson TA, Engler MB, Alger HM, Appel LJ, Mozaffarian D; American Heart Association Nutrition Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Epidemiology and Prevention; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; and Council on Clinical Cardiology. Omega-3 Polyunsaturated Fatty Acid (Fish Oil) Supplementation and the Prevention of Clinical Cardiovascular Disease: A Science Advisory From the American Heart Association. Circulation. 2017 Apr 11;135(15):e867-e884. doi: 10.1161/CIR.0000000000000482
- National Institutes of Health. Dietary Supplement Label Database. 2015.
- U.S. Food and Drug Administration. Fish: what pregnant women and parents should know. 2014. https://www.fda.gov/food/consumers/advice-about-eating-fish
- ConsumerLab.com. Product review: fish oil and omega-3 fatty acid supplements review (including krill, algae, calamari, green-lipped mussel oil). 2021. https://www.consumerlab.com/reviews/fish-oil-supplements-review/omega3
- Altomare, R., Cacciabaudo, F., Damiano, G., Palumbo, V. D., Gioviale, M. C., Bellavia, M., Tomasello, G., & Lo Monte, A. I. (2013). The mediterranean diet: a history of health. Iranian journal of public health, 42(5), 449–457. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3684452
- Castro-Quezada, I., Román-Viñas, B., & Serra-Majem, L. (2014). The Mediterranean diet and nutritional adequacy: a review. Nutrients, 6(1), 231–248. https://doi.org/10.3390/nu6010231
- Serra-Majem, L., Tomaino, L., Dernini, S., Berry, E. M., Lairon, D., Ngo de la Cruz, J., Bach-Faig, A., Donini, L. M., Medina, F. X., Belahsen, R., Piscopo, S., Capone, R., Aranceta-Bartrina, J., La Vecchia, C., & Trichopoulou, A. (2020). Updating the Mediterranean Diet Pyramid towards Sustainability: Focus on Environmental Concerns. International journal of environmental research and public health, 17(23), 8758. https://doi.org/10.3390/ijerph17238758
- Sofi F., Macchi C., Abbate R., Gensini G.F., Casini A. Mediterranean diet and health. Biofactors. 2013;39:335–342. doi: 10.1002/biof.1096
- Estruch R., Ros E., Salas-Salvadó J., Covas M.I., Corella D., Arós F., Gómez-Gracia E., Ruiz-Gutiérrez V., Fiol M., Lapetra J., et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013;368:1279–1290. doi: 10.1056/NEJMoa1200303
- Mitrou P.N., Kipnis V., Thiébaut A.C., Reedy J., Subar A.F., Wirfält E., Flood A., Mouw T., Hollenbeck A.R., Leitzmann M.F., et al. Mediterranean dietary pattern and prediction of all-cause mortality in a US population: Results from the NIH-AARP Diet and Health Study. Arch. Intern. Med. 2007;167:2461–2468. doi: 10.1001/archinte.167.22.2461
- Couto E., Boffetta P., Lagiou P., Ferrari P., Buckland G., Overvad K., Dahm C.C., Tjønneland A., Olsen A., Clavel-Chapelon F., et al. Mediterranean dietary pattern and cancer risk in the EPIC cohort. Br. J. Cancer. 2011;104:1493–1499. doi: 10.1038/bjc.2011.106
- Sofi F., Abbate R., Gensini G.F., Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. Am. J. Clin. Nutr. 2010;92:1189–1196. doi: 10.3945/ajcn.2010.29673
- Widmer, R. J., Flammer, A. J., Lerman, L. O., & Lerman, A. (2015). The Mediterranean diet, its components, and cardiovascular disease. The American journal of medicine, 128(3), 229–238. https://doi.org/10.1016/j.amjmed.2014.10.014
- F.B. Hu. The Mediterranean Diet and mortality—olive oil and beyond. N Engl J Med, 348 (2003), pp. 2595-2596
- Journal of the American College of Cardiology Volume 45, Issue 9, 3 May 2005, Pages 1379-1387. Diets and Cardiovascular Disease: An Evidence-Based Assessment. http://www.sciencedirect.com/science/article/pii/S0735109705003670
- National Institutes of Health. National Heart, Blood and Lung Institute. Description of the DASH Eating Plan. https://www.nhlbi.nih.gov/health/health-topics/topics/dash
- National Institutes of Health. National Heart, Blood and Lung Institute. Your Guide To Lowering Your Blood Pressure With DASH. https://www.nhlbi.nih.gov/files/docs/public/heart/dash_brief.pdf
- Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER 3rd, Simons-Morton DG, Karanja N, Lin PH; DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001 Jan 4;344(1):3-10. doi: 10.1056/NEJM200101043440101
- Salehi-Abargouei A, Maghsoudi Z, Shirani F, Azadbakht L. Nutrition. 2013 Apr;29(4):611-8. doi: 10.1016/j.nut.2012.12.018. Effects of Dietary Approaches to Stop Hypertension (DASH)-style diet on fatal or nonfatal cardiovascular diseases–incidence: a systematic review and meta-analysis on observational prospective studies. http://www.nutritionjrnl.com/article/S0899-9007(13)00007-5/fulltext
- Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008 Apr 14;168(7):713-20. PMID: 18413553. http://jamanetwork.com/journals/jamainternalmedicine/fullarticle/414155
- National Institutes of Health. National Heart, Blood and Lung Institute. Your Guide to Lowering Blood Pressure. https://www.nhlbi.nih.gov/files/docs/public/heart/hbp_low.pdf
- L.J. Appel, T.J. Moore, E. Obarzenek, et al.A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med, 336 (1997), pp. 1117-1124
- J.P. Midgley, A.G. Matthew, C.M. Greenwood, A.G. Logan. Effect of reduced dietary sodium on blood pressure: a meta-analysis of randomized controlled trials. JAMA, 275 (1996), pp. 1590-1597
- National Institutes of Health. National Heart, Blood and Lung Institute. Your Guide to Lowering Blood Pressure with DASH. https://www.nhlbi.nih.gov/files/docs/public/heart/new_dash.pdf
- National Cholesterol Education Program. Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. https://www.nhlbi.nih.gov/files/docs/guidelines/atp3xsum.pdf