Best probiotics for women
Probiotics are supplements or foods that contain live microorganisms (in most cases, bacteria but also include yeasts) that are similar to beneficial microorganisms found in the human gut and may be beneficial to health 1. The International Scientific Association for Probiotics and Prebiotics defines “probiotics” as “live microorganisms that, when administered in adequate amounts, confer a health benefit on the host” 2. In addition, products containing dead microorganisms and those made by microorganisms (such as proteins, polysaccharides, nucleotides, and peptides) are, by definition, not probiotics. Most probiotics in use today are derived either from fermented foods or from the microbes colonizing a healthy human. The human gastrointestinal tract is colonized by many microorganisms, including bacteria, archaea, viruses, fungi, and protozoa. The activity and composition of these microorganisms (collectively known as the gut microbiota, microbiome or intestinal microflora) can affect human health and disease. Priobiotics are thought to alter the microflora of the host and the live microorganisms are believed to provide health benefits when consumed 3. Products sold as probiotics include foods (such as yogurt), dietary supplements, and products that aren’t used orally, such as such as suppositories and skin creams. Although people often think of them as harmful “germs,” many microorganisms help your bodies to function properly. For example, normal intestinal bacteria digest food, destroy disease-causing microorganisms and produce vitamins. Large numbers of microorganisms live on and in our bodies. In fact, microorganisms in the human body outnumber human cells by 100 to 1. Many of the microorganisms in probiotic products are the same as or similar to the ones in your bodies 4. Although a great deal of research has been done on probiotics, much remains to be learned, because not all foods and dietary supplements labeled as “probiotics” on the market have proven health benefits 5.
Probiotics should not be confused with prebiotics. The term “prebiotics” refers to nondigestible carbohydrates that act as food for probiotics. Prebiotics are typically complex carbohydrates such as inulin and other fructo-oligosaccharides that microorganisms in the gastrointestinal tract use as metabolic fuel 6. Commonly known prebiotics are: oligofructose, inulin, galacto-oligosaccharides, lactulose and breast milk oligosaccharides. Lactulose is a synthetic disaccharide used as a drug for the treatment of constipation and hepatic encephalopathy. The prebiotic oligofructose is found naturally in many foods, such as wheat, onions, bananas, honey, garlic, and leeks. Oligofructose can also be isolated from chicory root or synthesized enzymatically from sucrose. Fermentation of oligofructose in the colon results in a large number of physiologic effects, including 7:
- Increasing the numbers of bifidobacteria in the colon
- Increasing calcium absorption
- Increasing fecal weight
- Shortening gastrointestinal transit time
- Possibly lowering blood lipid levels
The increase in colonic bifidobacteria has been assumed to benefit human health by producing compounds to inhibit potential pathogens, by reducing blood ammonia levels, and by producing vitamins and digestive enzymes 7.
The term “synbiotics” refers to products that combine both prebiotic sugars and probiotic organisms. Fermented dairy products, such as yogurt and kefir, are considered synbiotic because they contain live bacteria and the fuel they need to thrive. Probiotics are found in foods such as yogurt, while prebiotics are found in whole grains, bananas, onions, garlic, honey and artichokes. In addition, probiotics and prebiotics are added to some foods and available as dietary supplements. Probiotics in dietary supplements are measured in colony forming units (CFU), which indicate the number of viable cells. Amounts may be written on product labels as, for example, 1 x 109 for 1 billion CFU or 1 x 1010 for 10 billion CFU. Many probiotic supplements contain 1 to 10 billion CFU per dose, but some products contain up to 50 billion CFU or more. However, higher CFU counts do not necessarily improve the product’s health effects.
The term probiotic —meaning “for life”— is currently used to name ingested live microorganisms associated with benefits for humans and animals. The term came into more common use after 1980. The introduction of the concept is generally attributed to Elie Metchnikoff (a Russian scientist, Nobel laureate, and professor at the Pasteur Institute in Paris), who postulated that yogurt-consuming Bulgarian peasants lived longer lives because of this custom 1. He suggested in 1907 that “the dependence of the intestinal microbes on the food makes it possible to adopt measures to modify the flora in our bodies and to replace the harmful microbes by useful microbes”. Data from the 2012 National Health Interview Survey show that about four million U.S. adults had used probiotics or prebiotics in the past 30 days. Other than vitamins and minerals, probiotics or prebiotics were the third most commonly used dietary supplement. Their use quadrupled between 2007 and 2012. The survey also showed that 300,000 children ages 4 to 17 had used probiotics or prebiotics in the prior 30 days 4.
Although there are numerous claimed benefits of using commercial probiotics, such as reduction of gastrointestinal discomfort or strengthening of the immune system, such claims are not backed by scientific evidence. And it is important to be aware that the U.S. Food and Drug Administration (FDA) has not approved any health claims for probiotics.
Although more research is needed, there’s encouraging evidence that probiotics may help:
- Treat diarrhea, especially following treatment with certain antibiotics (e.g., prevention of antibiotic-associated diarrhea including diarrhea caused by Clostridium difficile)
- Prevent and treat vaginal yeast infections and urinary tract infections
- Treat irritable bowel syndrome (IBS)
- Treat inflammatory bowel disease
- Speed treatment of certain intestinal infections
- Prevent or reduce the severity of common colds and flu
- Allergic disorders such as atopic dermatitis (eczema) and allergic rhinitis (hay fever)
- Tooth decay, periodontal disease, and other oral health problems
- Colic in infants
- Liver disease
- Prevention of necrotizing enterocolitis in very low birth weight infants.
A great deal of research has been done on probiotics, but much remains to be learned about whether they’re helpful and safe for various health conditions.
You don’t necessarily need probiotics — a type of “good” bacteria — to be healthy. However, these microorganisms may help with digestion and offer protection from harmful bacteria, just as the existing “good” bacteria in your body already do.
Probiotics are generally considered safe but caution is advised in immunologically vulnerable populations. A systematic review by the Agency for Healthcare Research and Quality of 387 studies with a total of 24,615 participants did not find a significant increase in the number of adverse events in individuals treated with short-term probiotics (less than one month) based on 121 randomized controlled trials, or in the number of adverse-event incidents reported in probiotic vs. control groups based on 208 randomized controlled trials.45 The long-term effects of probiotics are largely unknown, and additional randomized trials are needed to address this question 8. This study found no significant increase in the risk of adverse events for children (35 randomized controlled trials), adults (40 randomized controlled trials), or older persons (four randomized controlled trials) 8. However, a systematic review of 17 studies including 1,530 patients with cancer found five cases of probiotic-related bacteremia/fungemia/positive blood culture 9.
What types of bacteria are in probiotics?
Probiotics may contain a variety of microorganisms. Probiotics are identified by their specific strain, which includes the genus, the species, the subspecies (if applicable), and an alphanumeric strain designation 10. The seven core genera of microbial organisms most often used in probiotic products are Lactobacillus, Bifidobacterium, Saccharomyces, Streptococcus, Enterococcus, Escherichia, and Bacillus. Table 1 shows examples of the nomenclature used for several commercial strains of probiotic organisms.
The most common are bacteria that belong to groups called Lactobacillus and Bifidobacterium. Each of these two broad groups includes many types of bacteria. Other bacteria may also be used as probiotics, and so may yeasts such as Saccharomyces boulardii 4.
Different types of probiotics may have different effects. For example, if a specific kind of Lactobacillus helps prevent an illness, that doesn’t necessarily mean that another kind of Lactobacillus or any of the Bifidobacterium probiotics would do the same thing.
Table 1. Nomenclature for sample commercial strains of probiotics
| Genus | Species | Subspecies | Strain Designation | Strain Nickname |
| Lactobacillus | rhamnosus | none | GG | LGG |
| Bifidobacterium | animalis | lactis | DN-173 010 | Bifidus regularis |
| Bifidobacterium | longum | longum | 35624 | Bifantis |
What are sources of probiotics?
Fermented or cultured dairy products are a major source of probiotics 11. Other sources of probiotics include:
- miso
- tempeh
- soy beverages
- buttermilk
- fermented milk.
The bacteria either occur naturally in these foods or have been added during preparation. Probiotics are also available as dietary supplements in capsule, tablet or powder-form.
Food sources of probiotics
Fermented foods are made through the growth and metabolic activity of a variety of live microbial cultures. Many of these foods are rich sources of live and potentially beneficial microbes. Some fermented foods, such as sourdough bread and most commercial pickles, are processed after they are fermented and do not contain live cultures in the form in which they are consumed. Many commercial yogurts, another type of fermented food, contain probiotic microorganisms, such as Lactobacillus bulgaricus and Streptococcus thermophilus.
The live microorganisms used to make many fermented foods, including yogurt, typically survive well in the product throughout its shelf life. However, they usually do not survive transit through the stomach and might not resist degradation in the small intestine by hydrolytic enzymes and bile salts and, therefore, might not reach the distal gut 12. However, legitimate probiotic strains contained in yogurt or other foods do survive intestinal transit.
Fermented foods that contain live cultures but do not typically contain proven probiotic microorganisms include many cheeses, kimchi (a Korean fermented cabbage dish), kombucha (a fermented tea), sauerkraut (fermented cabbage), miso (a fermented soybean-based paste), pickles, and raw unfiltered apple cider vinegar made from fermented apple sugars 12.
Certain unfermented foods, such as milks, juices, smoothies, cereals, nutrition bars, and infant and toddler formulas, have added microorganisms. Whether these foods are truly probiotics depends on the microorganism levels they contain when they are eaten, whether they survive intestinal transit, and whether their specific species and strains have health effects.
Dietary supplements
Probiotics are also available as dietary supplements (in capsules, powders, liquids, and other forms) containing a wide variety of strains and doses. These products often contain mixed cultures of live microorganisms rather than single strains. The effects of many commercial products containing “probiotics” have not been examined in research studies, and it is difficult for people not familiar with probiotic research to determine which products are backed by evidence. However, some organizations have systematically reviewed the available evidence and developed recommendations on specific probiotics—including appropriate product, dose, and formulation—to use for preventing or treating various health conditions 13.
Probiotics in dietary supplements are measured in colony forming units (CFU), which indicate the number of viable cells. Amounts may be written on product labels as, for example, 1 x 109 for 1 billion CFU or 1 x 1010 for 10 billion CFU. Many probiotic supplements contain 1 to 10 billion CFU per dose, but some products contain up to 50 billion CFU or more. However, higher CFU counts do not necessarily improve the product’s health effects.
Current labeling regulations only require manufacturers to list the total weight of the microorganisms on probiotic products’ Supplement Facts labels; this cellular mass can consist of both live and dead microorganisms and, therefore, has no relationship with the number of viable microorganisms in the product 14. Manufacturers may now voluntarily list the CFUs in a product in addition to total microorganism weight on the Supplement Facts label. Because probiotics must be consumed alive to have health benefits and they can die during their shelf life, users should look for products labeled with the number of CFU at the end of the product’s shelf life, not at the time of manufacture.
How might probiotics work?
There is a relationship between disease, health, the immune system, and changes in the microbiota 15. Probiotics may have a variety of effects in the body, and different probiotics may act in different ways.
Proposed mechanisms of probiotics:
- Help your body maintain a healthy community of microorganisms or help your body’s community of microorganisms return to a healthy condition after being disturbed
- Produce substances that have desirable effects
- Influence your body’s immune response.
- Block the adhesion of pathogenic bacteria to the intestinal epithelium; produce inhibitory agents 16
- Enhance the intestinal immune response 17
- Maintain normal levels of short-chain fatty acids 18
- Modulate immune system function, such as suppression of intestinal proinflammatory cytokines 19
- Repair intestinal permeability 19
- Suppress the growth of pathogenic bacteria by directly binding to gram-negative bacteria 20
- Upregulate intestinal electrolyte absorption 17
Probiotics for vaginal health
Bacterial vaginosis also known as BV, results from overgrowth of one of several anaerobic bacteria called Gardnerella vaginalis that are naturally found in your vagina 21, 22. Generally, a healthy adult vaginal microbiome predominantly consists of Lactobacillus spp. and other microbes at lower abundances such as Peptostreptococcus spp., Bacteroides spp. and Enterobacteriaceae 23. Usually, “good” bacteria (Lactobacilli) outnumber “bad” bacteria (Gardnerella vaginalis, Atopobium, Mobiluncus, Prevotella, Bacteroides, Anaerococcus, Peptostreptococcus, Sneathia, Leptotrichia, Mycoplasma hominis and members of the class Clostridia, among others) 24. Normally, bacteria belonging mostly to the Lactobacillus family live harmlessly in your vagina and produce lactic acid, acetic acid, bacteriocin, and hydrogen peroxide (H2O2), that keep your vagina mildly acidic (maintain the vaginal pH around 4.5 or less), which is toxic to a range of potentially harmful bacteria and Candida albicans and inhibits their growth 25 and are thus considered protective against vulvovaginal candidiasis and bacterial vaginosis 26. But if there are too many anaerobic bacteria, they upset the natural balance of microorganisms in your vagina and cause bacterial vaginosis. In bacterial vaginosis, Lactobacillus bacteria are replaced by other types of bacteria that normally are present in smaller concentrations in the vagina. Scientists do not fully understand the reason for this change. Risk factors that seem to increase the likelihood of bacterial vaginosis include a history of multiple sex partners, unprotected sex, a sexual relationship with a new partner, cigarette smoking, vaginal douching and the use of the intrauterine contraceptive device (IUD). Although most of these risk factors are related to sexual activity, women who have never had vaginal intercourse can also develop bacterial vaginosis. Women in their reproductive years are most likely to get bacterial vaginosis, but it can affect women of any age.
Bacterial vaginosis doesn’t generally cause complications. Sometimes, having bacterial vaginosis may lead to:
- Increased risk for endometritis and salpingitis
- Sexually transmitted infections (STIs). Having bacterial vaginosis makes women more susceptible to sexually transmitted infections, such as human immunodeficiency virus (HIV), herpes simplex virus (HSV), chlamydia or gonorrhea. If you have HIV, bacterial vaginosis increases the odds that you’ll pass the virus on to your partner.
- Increased risk of infection after gynecologic surgery. Having bacterial vaginosis may increase the risk of developing a post-surgical infection after procedures such as hysterectomy or dilation and curettage (D&C).
- Adverse outcomes in pregnancy including premature labor, premature deliveries, premature rupture of membranes (PROM), low birth weight babies and postpartum endometritis.
- Pelvic inflammatory disease (PID). Bacterial vaginosis can sometimes cause PID, an infection of the uterus and the fallopian tubes, which can make it difficult or impossible for you to have children.
- Neonatal meningitis
Bacterial vaginosis has been associated with increased risk for acquisition of human immunodeficiency virus (HIV) 27 and other sexually transmitted infections 28, urinary tract infections 29, post-surgical complications 30, infertility 31, pregnancy losses 32, preterm birth 33, intrauterine infections 34, intraamniotic infections 35, as well as cervical infections, dysplasia, and cancer 36.
In about half of all cases of bacterial vaginosis, there are no noticeable symptoms 37. When they do occur, symptoms usually include a white or grey watery vaginal discharge, an unpleasant or ‘fishy’ vaginal odor and mild irritation around your vagina. Sometimes these symptoms come and go, or are more noticeable during menstrual periods.
Your doctor can make a diagnosis of bacterial vaginosis by taking a swab of vaginal discharge, and having it examined under a microscope looking for “clue cells,” vaginal cells covered with bacteria that are a sign of bacterial vaginosis 38. Your doctor may also check the acidity of your vagina by placing a pH test strip in your vagina. A vaginal pH of 4.5 or higher is a sign of bacterial vaginosis 39.
Bacterial vaginosis doesn’t necessarily have to be treated if there are no symptoms. It has even been reported that up to 30% of cases of bacterial vaginosis may even resolve on its own without treatment 21. However, if you are pregnant, it’s important you seek treatment because you can be at risk of complications such as miscarriage and premature delivery.
To treat bacterial vaginosis, your doctor may prescribe one of the following medications:
- Metronidazole (Flagyl, Metrogel-Vaginal, others). This medicine may be taken as a pill by mouth (orally). Metronidazole is also available as a topical gel that you insert into your vagina. To reduce the risk of stomach upset, abdominal pain or nausea while using this medication, avoid alcohol during treatment and for at least one day after completing treatment — check the instructions on the product.
- Clindamycin (Cleocin, Clindesse, others). This medicine is available as a cream that you insert into your vagina. Clindamycin cream may weaken latex condoms during treatment and for at least three days after you stop using the cream.
- Tinidazole (Tindamax). This medication is taken orally. Tinidazole has the same potential for stomach upset and nausea as oral metronidazole does, so avoid alcohol during treatment and for at least three days after completing treatment.
- Secnidazole (Solosec). This is an antibiotic you take orally in one dose. The medication comes as a packet of granules that you sprinkle onto a soft food, such as applesauce, pudding or yogurt. You eat the mixture within 30 minutes, being careful not to crunch or chew the granules.
It’s generally not necessary to treat an infected woman’s male sexual partner, but bacterial vaginosis can spread between female sexual partners. Female partners should seek testing and may need treatment. It’s especially important for pregnant women with symptoms to be treated to help decrease the risk of premature delivery or low birth weight.
Take your medicine or use the cream or gel for as long as your doctor prescribes it — even if your symptoms go away. Stopping treatment early may increase the risk of recurrence.
If you have had bacterial vaginosis, there are some things you can do to help prevent further episodes. In particular, avoid smoking, douching or using perfumed talcs or deodorants around your vagina.
While current research shows there may be some benefit to probiotic therapy, more research is needed on the subject. The commonly believed beneficial effect of probiotics supplementation for the treatment of bacterial vaginosis has been assessed in various meta-analysis 40, 41, 42. Evidence suggests that restoration of the vaginal microbiota and/or modulation of the local mucosal immune response can be achieved via supplementation with probiotics, which can be administered orally as a probiotic food supplement, intra-vaginally as vaginal suppositories, or applied topically as a gel 43. A 2009 Cochrane review 42 showed promising results derived from the use of oral and vaginal probiotics combined with metronidazole or used alone. In 2013, a systematic review 41 supported the potential beneficial effect of probiotics for the treatment of bacterial vaginosis. Huang et al. 41 included in their analysis twelve randomized controlled trials published between 1992 and 2012; probiotics were adopted either orally (n = 8) or vaginally (n = 4), with follow-up periods ranging from 4 weeks to 6 months. The pooled result showed that probiotics supplementation was able to significantly improve the cure rate in adult bacterial vaginosis patients 41. Subgroup analyses failed to demonstrate a beneficial effect of probiotics supplementation in terms of long-term (> 1 month) follow-up and a substantial heterogeneity was shown across different study designs (Buggio, L., Somigliana, E., Borghi, A., & Vercellini, P. (2019). Probiotics and vaginal microecology: fact or fancy?. BMC women’s health, 19(1), 25. https://doi.org/10.1186/s12905-019-0723-4()). Finally, in a recent meta-analysis 40, the authors compared the use of metronidazole alone with the combination of this antibiotic plus probiotics. Five randomized controlled trials including a total of 1186 participants were selected. An overall risk ratio of 0.98 was observed for the cure rate achieved with combined therapy over metronidazole alone on bacterial vaginosis 40.
The effectiveness of orally administered capsules containing probiotics (Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-1) was evaluated in a randomized, double-blind, multicentric, placebo-controlled trial including 544 women older than 18 years of age diagnosed with vaginal infection 44. The test group (395 women) and placebo group (149 women) received either two probiotic capsules (each containing >109 CFU of each Lactobacillus strain) or two placebo capsules per day for 6 weeks. Women underwent two gynecological examinations after 6 and 12 weeks of the study. Differences between groups were significant at forty-four days after the initial visit; the vaginal microbiota was restored in 243 women in the probiotic group compared to 40 women in the placebo group 44. After the additional 6 weeks of follow-up, normal vaginal microbiota was still present in more than half of the women in the probiotic group compared to only about one-fifth of those in the placebo group 44.
Gille et al. 43 studied the effect of an oral probiotic food supplement in maintaining or restoring the normal vaginal microbiota during pregnancy. Three hundred and twenty women with less than 12 completed weeks of pregnancy participated in the study. Patients consumed a probiotic capsule containing Lactobacillus rhamnosus GR-1® and Lactobacillus reuteri RC-14® (1 × 109 CFU of each strain per capsule) daily 43. The results showed that oral probiotics may be suitable for implementation in antenatal care but had no effect on vaginal health during mid-gestation.
Recently, Laue et al. 45 evaluated the effect of yoghurt containing Lactobacillus strains on bacterial vaginosis in a single-center, double-blind, placebo-controlled, randomized clinical trial with two parallel arms. The strains were isolated from healthy pregnant women and selected for acidification capacity, H2O2 production, glycogen utilization, bile salt tolerance, and pathogen inhibition. Thirty-six female volunteers were selected at reproductive age (≥ 18 years) with stable menstrual cycles or postmenopausal women diagnosed with bacterial vaginosis. The test group (18 patients) received yoghurt (125 g/daily) containing live strains of Lactobacillus crispatus, Lactobacillus gasseri, Lactobacillus rhamnosus, and Lactobacillus jensenii and the placebo group (18 patients) received chemically acidified milk (125 g/daily) without bacterial strains 45. Patients were treated with oral metronidazole for 7 days (2 × 500 mg/daily). Starting with the treatment, women consumed twice daily either yoghurt or placebo for 4 weeks. After 4 weeks of intervention, 0 of 17 had bacterial vaginosis in the test group vs. 6 of 17 in the placebo group. Additional intake of yoghurt containing these Lactobacillus strains improved the recovery rate, bacterial vaginosis symptoms, and vaginal microbial pattern 45.
Handalishy et al. 46 compared the efficacy of vaginally administered probiotic vaginal tampons with oral metronidazole for the treatment of bacterial vaginosis. This single blinded, randomized clinical trial included healthy women diagnosed with bacterial vaginosis. The patients, aged 20–40 years, were randomly assigned to two groups (antibiotic and probiotic groups). The antibiotic group (16 patients) received oral metronidazole (500 mg twice daily for 7 days), while the probiotic group (15 patients) used lactobacilli-impregnated vaginal tampons for 5 days during menstruation. The probiotic group had significantly lower incidence of discharge than metronidazole group and higher cure rate than metronidazole group, but this difference was not significant 46.
Verdenelli et al. 47 evaluated the effect of probiotic suppositories, SYNBIO® gin, on vaginal health. The study included 35 apparently healthy women (aged 18–48 years), who were instructed to receive daily for 7 days the probiotic suppositories SYNBIO® gin, containing at least 109 CFU of viable lactobacilli, a combination of Lactobacillus rhamnosus IMC 501® and Lactobacillus paracasei IMC 502® 47. Women were examined three times during the study. The results revealed the presence of the two strain of Lactobacilli originating from SYNBIO® gin in 100% of women at visit 2 and 34% at visit 3. In addition, the probiotic suppositories were well-tolerated and had no adverse effects, and no significant changes were registered for pH between visits. The SYNBIO® gin product is safe for daily use in healthy women and it could be useful to restore and maintain a normal vaginal microbiota 47.
Coste et al. 48 evaluated the efficacy and safety of an intravaginal prebiotic gel in the balance recovery of the vaginal flora in women previously treated for bacterial vaginosis. The double-blind, parallel placebo-controlled, randomized clinical trial included 42 premenopausal, nonpregnant women aged 18–50 years. Patients confirmed with bacterial vaginosis received oral antibiotic treatment with metronidazole during 7 days. Then, the test group (20 patients) were randomized to receive the APP-14 gel inside a small tube containing 7 mL of product with the glucooligosaccharides-alpha prebiotic (6%, equivalent to a minimum of 300 mg of oligosaccharide) and the Trifolium pratense extract (2%) 48. Meanwhile, the control group (22 patients) received placebo gel without the active ingredients. The intravaginal-gel was self-administered once a day for 16 consecutive days. The results showed that after the antibiotic treatment there was no significant difference between the groups and the normal vaginal flora was not completely restored. After 8 days of treatment, all women who received prebiotic treatment had normal vaginal flora, while 33% of women in the control group did not completely restore normal vaginal flora. After 16 days treatment, all women treated with the prebiotic gel maintained normal vaginal flora, whereas in the placebo group 24% had not completely restored vaginal flora 48.
Table 2. Role of probiotics in International guidelines for the treatment of vulvovaginal infections
| Guidelines | Role of probiotics |
| European (IUSTI/WHO) guideline, 2011 49 | Potential role of vaginal probiotics in the management of recurrent bacterial vaginosis |
| Faculty of Sexual & Reproductive Healthcare, Royal College of Obstetricians and Gynaecologists (RCOG), 2012 50 | Recurrent bacterial vaginosis: There is currently insufficient evidence to recommend the use of probiotics either before, during or after antibiotic treatment as a means of reducing recurrence. Recurrent vulvovaginal candidiasis: Non-conventional management regimens such as dietary changes, use of probiotics, tea tree oil and not wearing tight clothing have been studied. There is currently insufficient evidence to support their recommendation in treatment. |
| German Society for Gynecology and Obstetrics, 2015 51 | Probiotics have shown encouraging, but controversial results and require further investigation |
| Society of Obstetrician and Gynaecologyst of Canada (SOGC), 2015 52 | Current evidence of the efficacy of alternative therapies for bacterial vaginosis (probiotics, vitamin C) is limited. |
| Centers for Disease Control and Prevention (CDC), 2015 53 | Overall, no studies support the addition of any available lactobacillus formulations or probiotic as an adjunctive or replacement therapy in women with bacterial vaginosis. Further research efforts to determine the role of these regimens in bacterial vaginosis treatment and prevention are ongoing |
Footnote: IUSTI/WHO = International Union against Sexually Transmitted Infection and the World Health Organization
Can bacterial vaginosis be prevented or avoided?
You may not be able to prevent bacterial vaginosis. But you can try to reduce your risk of getting bacterial vaginosis. To reduce your risk, you should:
- Use condoms. Condoms can help prevent the spread of bacterial vaginosis.
- Keep sex toys clean. Do not share sex toys with other people. Always clean them after use.
- Limit your number of sexual partners. Monogamy (having sex with only one partner) is the one of the best ways to prevent bacterial vaginosis.
- Do not douche. Your vagina doesn’t require cleansing other than normal bathing. This can cause an imbalance in vaginal bacteria. Douching won’t clear up a vaginal infection.
- Minimize vaginal irritation. Use mild, nondeodorant soaps and unscented tampons or pads.
- See your doctor. If you feel you have symptoms of bacterial vaginosis, tell your doctor.
Bacterial vaginosis recurrence
Some women suffer from chronic (recurring) bacterial vaginosis. It’s common for bacterial vaginosis to recur within three to 12 months, despite treatment. Medicine can clear up the infection, but it returns again after a few weeks. Some women report that bacterial vaginosis returns after their period each month. Or it can return after they have sex. Researchers are exploring treatments for recurrent bacterial vaginosis.
Talk to your doctor if you have chronic bacterial vaginosis. One option may be extended-use metronidazole therapy. Your doctor may also suggest certain lifestyle changes that can help, like taking probiotics.
Is there a cure for bacterial vaginosis?
Yes, bacterial vaginosis is usually curable with prescription antibiotics that can help readjust the balance of bacteria in your vagina 54. Although some over-the-counter vaginal medications are sold, these are not effective for curing bacterial vaginosis. Currently, only prescribed antibiotics are effective.
Recommended regimens for bacterial vaginosis 54:
- Metronidazole 500 mg orally 2 times/day for 7 days
OR - Metronidazole gel 0.75% one full applicator (5 g) intravaginally, once daily for 5 days
OR - Clindamycin cream 2% one full applicator (5 g) intravaginally at bedtime for 7 days
Alternative regimens for bacterial vaginosis 54:
- Clindamycin 300 mg orally 2 times/day for 7 days
OR - Clindamycin ovules 100 mg intravaginally once at bedtime for 3 days*
OR - Secnidazole 2 g oral granules in a single dose†
OR - Tinidazole 2 g orally once daily for 2 days
OR - Tinidazole 1 g orally once daily for 5 days
Note:* Clindamycin ovules use an oleaginous base that might weaken latex or rubber products (e.g., condoms and diaphragms). Use of such products within 72 hours after treatment with clindamycin ovules is not recommended.
† Oral granules should be sprinkled onto unsweetened applesauce, yogurt, or pudding before ingestion. A glass of water can be taken after administration to aid in swallowing.
With bacterial vaginosis, there is a risk of relapsing if the entire course of antibiotics is not finished 55. Therefore, it is important to finish all of the pills in a bacterial vaginosis prescription.
Although bacterial vaginosis can be cured, it does carry certain risks. Women with bacterial vaginosis are at a higher risk for:
- Delivering an infant preterm (before 37 weeks of pregnancy)
- Delivering an infant with a low birth weight (generally, 5.5 pounds or less)
- More easily contracting certain sexually transmitted diseases (STDs), including gonorrhea, herpes, and HIV/AIDS
- More easily infecting a partner with certain STDs, including HIV/AIDS
- Developing pelvic inflammatory disease
What happens if bacterial vaginosis don’t get treated?
Bacterial vaginosis can cause some serious health risks, including:
- Increasing your chance of getting HIV if you have sex with someone who is infected with HIV;
- If you are HIV positive, increasing your chance of passing HIV to your sex partner;
- Making it more likely that you will deliver your baby too early if you have bacterial vaginosis while pregnant;
- Increasing your chance of getting other Sexually Transmitted Diseases (STDs), such as chlamydia and gonorrhea. These bacteria can sometimes cause pelvic inflammatory disease (PID), which can make it difficult or impossible for you to have children.
Probiotics for vulvovaginal candidiasis
Vulvovaginal candidiasis is also called vaginal candidiasis, vaginal thrush or vaginal yeast infection, is a common fungal infection caused by the Candida species of fungus. The fungus Candida albicans is responsible for most vaginal yeast infections. Vulvovaginal candidiasis causes irritation, discharge and intense itchiness of the vagina and the vulva — the tissues at the vaginal opening. Vaginal thrush can affect women of any age, although it is more common in women between the ages of 15 and 50 years old. Many women experience at least two episodes in their lifetimes. Vaginal candidiasis is unusual in girls who have not yet begun their periods and in older women after menopause. Candida is usually found in the vagina and is harmless, but when the fungus multiplies it can cause irritation and swelling both in the vagina and vulva. Vulvovaginal candidiasis is easily treated and can be prevented. Medications can effectively treat vaginal yeast infections. Yeast infections caused by other types of Candida fungus can be more difficult to treat, and generally need more-aggressive therapies. If you have recurrent yeast infections — four or more within a year — you may need a longer treatment course and a maintenance plan.
Your vagina naturally contains a balanced mix of yeast, including candida, and bacteria. Certain bacteria (lactobacillus) act to prevent an overgrowth of yeast. But that balance can be disrupted. An overgrowth of Candida or penetration of the fungus into deeper vaginal cell layers causes the signs and symptoms of a yeast infection.
Scientists estimate that about 20% of women normally have Candida in the vagina without having any symptoms 56. Sometimes, Candida can multiply and cause an infection if the environment inside the vagina changes in a way that encourages its growth. This can happen because of hormones, medicines, or changes in the immune system.
Overgrowth of yeast can result from:
- Antibiotic use, which causes an imbalance in natural vaginal flora
- Pregnancy
- Uncontrolled diabetes
- An impaired immune system
- Taking oral contraceptives or hormone therapy that increase estrogen levels
- Douche products
- Steroids
- Moisture and irritation of the vagina also seem to encourage yeast to grow.
Risk factors that increase your risk of developing a yeast infection include:
- Antibiotic use. Yeast infections are common in women who take antibiotics. Broad-spectrum antibiotics, which kill a range of bacteria, also kill healthy bacteria in your vagina, leading to overgrowth of yeast.
- Increased estrogen levels. Yeast infections are more common in women with higher estrogen levels — such as pregnant women or women taking high-dose estrogen birth control pills or estrogen hormone therapy.
- Uncontrolled diabetes. Women with poorly controlled blood sugar are at greater risk of yeast infections than women with well-controlled blood sugar.
- Impaired immune system. Women with lowered immunity — such as from corticosteroid therapy or HIV infection — are more likely to get yeast infections.
A vaginal yeast infection isn’t considered a sexually transmitted infection. But, there’s an increased risk of vaginal yeast infection at the time of first regular sexual activity. There’s also some evidence that infections may be linked to mouth to genital contact (oral-genital sex).
The most common symptoms of vaginal thrush are itchiness, irritation and redness in and around the vagina. A vaginal yeast infection symptoms can range from mild to moderate, and include:
- Itching and irritation in the vagina and vulva
- Pain and/or discomfort, especially during sexual intercourse
- A burning sensation when urinating
- Redness and swelling of the vulva
- Vaginal pain and soreness
- Vaginal rash
- Thick, white, odor-free vaginal discharge with a cottage cheese appearance
- Watery vaginal discharge
Up to 1 in 5 women with vaginal thrush do not experience noticeable symptoms.
You might have a complicated yeast infection if:
- You have severe signs and symptoms, such as extensive redness, swelling and itching that leads to tears, cracks or sores
- You have four or more yeast infections in a year
- Your infection is caused by a less typical type of fungus
- You’re pregnant
- You have uncontrolled diabetes
- Your immune system is weakened because of certain medications or conditions such as HIV infection
To diagnose vaginal yeast infection, your doctor may:
- Ask questions about your medical history. This might include gathering information about past vaginal infections or sexually transmitted infections.
- Perform a pelvic exam. Your doctor examines your external genitals for signs of infection. Next, your doctor places an instrument (speculum) into your vagina to hold the vaginal walls open to examine the vagina and cervix — the lower, narrower part of your uterus.
- Test vaginal secretions. Your doctor may send a sample of vaginal fluid for testing to determine the type of fungus causing the yeast infection. Identifying the fungus can help your doctor prescribe more effective treatment for recurrent yeast infections.
Vulvovaginal candidiasis can be diagnosed by visualization of yeast hyphae on potassium hydroxide preparation in a woman with typical symptoms 57. Vaginal yeast infection can also be diagnosed using antigen or DNA probe testing, with sensitivities of 77% to 97% and specificities of 77% to 99%, compared with culture as the diagnostic standard 58. Women with vulvovaginal candidiasis have a normal acidic vaginal pH.
Make an appointment with your doctor if:
- This is the first time you’ve had yeast infection symptoms
- You’re not sure whether you have a yeast infection
- Your symptoms aren’t relieved after treating with over-the-counter antifungal vaginal creams or suppositories
- You develop other symptoms
Vulvovaginal candidiasis treatment
Treatment for yeast infections depends on the severity and frequency of your infections. Vaginal candidiasis are usually treated with antifungal medicine you put in your vagina 59. This medicine may be a cream you insert with a special applicator. Or the medicine may be a suppository you put into your vagina and allow it to dissolve on its own. Medicine in a pill form to take by mouth is also available. Some medicine is available as a cream you can put on your vulva to help relieve itching.
For most infections, the treatment is an antifungal medicine applied inside the vagina or a single dose of fluconazole taken by mouth. Other treatments may be needed for infections that are more severe, that don’t get better, or that keep coming back after getting better. These treatments include more doses of fluconazole taken by mouth or other medicines applied inside the vagina, such as boric acid, nystatin, or flucytosine.
If you’ve had a yeast infection before and are having classic symptoms, you may want to treat the infection using over-the-counter (OTC) medicines. There are many brands available that offer creams (two brand names: Monistat and Vagisil) and suppositories (one brand name: NutraBlast).
Over-the-Counter (OTC) Intravaginal Agents 60:
- Clotrimazole 1% cream 5 g intravaginally daily for 7–14 days
OR - Clotrimazole 2% cream 5 g intravaginally daily for 3 days
OR - Miconazole 2% cream 5 g intravaginally daily for 7 days
OR - Miconazole 4% cream 5 g intravaginally daily for 3 days
OR - Miconazole 100 mg vaginal suppository, one suppository daily for 7 days
OR - Miconazole 200 mg vaginal suppository, one suppository for 3 days
OR - Miconazole 1,200 mg vaginal suppository, one suppository for 1 day
OR - Tioconazole 6.5% ointment 5 g intravaginally in a single application
Prescription intravaginal agents:
- Butoconazole 2% cream (single dose bioadhesive product), 5 g intravaginally in a single application
OR - Terconazole 0.4% cream 5 g intravaginally daily for 7 days
OR - Terconazole 0.8% cream 5 g intravaginally daily for 3 days
OR - Terconazole 80 mg vaginal suppository, one suppository daily for 3 days
Oral agent:
- Fluconazole (Diflucan) 150 mg orally in a single dose
For mild to moderate symptoms and infrequent yeast infections, your doctor might recommend:
- Short-course vaginal therapy. Taking an antifungal medication for three to seven days will usually clear a yeast infection. Antifungal medications — which are available as creams, ointments, tablets and suppositories — include miconazole (Monistat 3) and terconazole. Some of these medications are available over-the-counter and others by prescription only.
- Single-dose oral medication. Your doctor might prescribe a one-time, single oral dose of fluconazole (Diflucan). Oral medication isn’t recommended if you’re pregnant. To manage more-severe symptoms, you might take two single doses three days apart.
Short-course topical formulations (i.e., single dose and regimens of 1–3 days) effectively treat uncomplicated vulvovaginal candidiasis. The topically applied azole drugs are more effective than nystatin. Treatment with azoles results in relief of symptoms and negative cultures in 80%–90% of patients who complete therapy. See your doctor again if treatment doesn’t resolve your symptoms or if your symptoms return within two months.
Even women who have previously received a diagnosis of vulvovaginal candidiasis by a clinician are not necessarily more likely to be able to diagnose themselves; therefore, any woman whose symptoms persist after using an OTC preparation or who has a recurrence of symptoms within 2 months after treatment for vulvovaginal candidiasis should be clinically evaluated and tested.
If your symptoms are severe, or you have frequent yeast infections, your doctor might recommend:
- Long-course vaginal therapy. Your doctor might prescribe an antifungal medication taken daily for up to two weeks, followed by once a week for six months.
- Multidose oral medication. Your doctor might prescribe two or three doses of an antifungal medication to be taken by mouth instead of vaginal therapy. However, this therapy isn’t recommended for pregnant women.
- Azole resistant therapy. Your doctor might recommend boric acid, a capsule inserted into your vagina. This medication may be fatal if taken orally and is used only to treat candida fungus that is resistant to the usual antifungal agents.
Although it’s rare, you can transmit a yeast infection to your partner through sexual intercourse. Talk to your doctor about treatment options if your partner begins to develop symptoms of a yeast infection.
Management of sex partners
Uncomplicated vulvovaginal candidiasis is not usually acquired through sexual intercourse; thus, data do not support treatment of sex partners. A minority of male sex partners have balanitis, characterized by erythematous areas on the glans of the penis in conjunction with pruritus or irritation. These men benefit from treatment with topical antifungal agents to relieve symptoms.
Probiotics for vulvovaginal candidiasis
The effectiveness of probiotics for the treatment of vulvovaginal candidiasis in non-pregnant women was recently evaluated in a 2017 Cochrane systematic review 61. The studies included nonpregnant Chinese and Iranian women 16 to 50 years of age. A total of 10 randomized controlled trials (1656 participants) investigating the effect of probiotics used by the oral and vaginal route as a complementary therapy to conventional antifungal drugs were included 61. Probiotics slightly improved the short-term clinical and mycological cure rate and reduced the 1-month relapse rate 61. However, no important impact of probiotic use was observed on long-term clinical or mycological cure rate (3-month post-treatment evaluation). Adding probiotics (typically Lactobacillus species) to antifungal therapy for vulvovaginal candidiasis improves short-term cure rates by 14% and reduces one-month relapse rates by 66% 62. Given the low- or very low-quality of the considered studies, the authors emphasized the need for further and better designed randomized controlled trials with larger sample size, standardized methodology for probiotic preparation, and longer follow-up, in order to define also other outcomes that may matter to women, such as time to first relapse, need for repeated or prolonged treatments, patient satisfaction, and cost effectiveness.
Recurrent vulvovaginal candidiasis
Some women (about 5%) have recurrent yeast infections. Complicated vulvovaginal candidiasis is defined as recurrent vulvovalginal candidiasis (four or more episodes in one year) or severe infections, or infections that occur in a patient who is immunocompromised, such as someone with AIDS or poorly controlled diabetes mellitus. The pathogenesis of recurrent vulvovalginal candidiasis is poorly understood, and most women with recurrent vulvovalginal candidiasis have no apparent predisposing or underlying conditions. Candida glabrata and other nonalbicans Candida species are observed in 10%–20% of women with recurrent vulvovalginal candidiasis. Conventional antimycotic therapies are not as effective against these nonalbicans species as against Candida albicans. Culture is particularly important for the diagnosis and treatment of complicated vulvovaginal candidiasis, because patients are more likely to have an infection with nonalbicans strains of Candida, which may require different treatment 63, 64. Candidal species and anaerobes can be normal flora in asymptomatic women, so retesting (test of cure) is not recommended in the absence of symptoms.
Each individual episode of recurrent vulvovaginal candidiasis caused by Candida albicans responds well to short duration oral or topical azole therapy. However, to maintain clinical and mycologic control, some specialists recommend a longer duration of initial therapy (e.g., 7–14 days of topical therapy or a 100-mg, 150-mg, or 200-mg oral dose of fluconazole every third day for a total of 3 doses [day 1, 4, and 7]) to attempt mycologic remission before initiating a maintenance antifungal regimen.
Oral fluconazole (i.e., 100-mg, 150-mg, or 200-mg dose) weekly for 6 months is the first line maintenance regimen. If this regimen is not feasible, topical treatments used intermittently can also be considered. Suppressive maintenance therapies are effective in reducing recurrent vulvovaginal candidiasis. However, 30%–50% of women will have recurrent disease after maintenance therapy is discontinued. Symptomatic women who remain culture-positive despite maintenance therapy should be managed in consultation with a specialist.
Severe vulvovaginal candidiasis
Severe vulvovaginitis (i.e., extensive vulvar erythema, edema, excoriation, and fissure formation) is associated with lower clinical response rates in patients treated with short courses of topical or oral therapy. Either 7–14 days of topical azole or 150 mg of fluconazole in two sequential oral doses (second dose 72 hours after initial dose) is recommended.
Nonalbicans vulvovaginal candidiasis
Because at least 50% of women with positive cultures for nonalbicans Candida might be minimally symptomatic or have no symptoms and because successful treatment is often difficult, clinicians should make every effort to exclude other causes of vaginal symptoms in women with nonalbicans yeast 65. The optimal treatment of nonalbicans vulvovaginal candidiasis remains unknown. Options include longer duration of therapy (7–14 days) with a nonfluconazole azole regimen (oral or topical) as first-line therapy. If recurrence occurs, 600 mg of boric acid in a gelatin capsule is recommended, administered vaginally once daily for 2 weeks. This regimen has clinical and mycologic eradication rates of approximately 70% 66. If symptoms recur, referral to a specialist is advised.
Compromised host
Women with underlying immunodeficiency, those with poorly controlled diabetes or other immunocompromising conditions (e.g., HIV), and those receiving immunosuppression therapy (e.g., corticosteroid treatment) do not respond as well to short-term therapies. Efforts to correct modifiable conditions should be made, and more prolonged (i.e., 7–14 days) conventional treatment is necessary.
Pregnancy
Vulvovaginal candidiasis occurs frequently during pregnancy. Only topical azole therapies, applied for 7 days, are recommended for use among pregnant women.
HIV infection
Vaginal Candida colonization rates among women with HIV infection are higher than among seronegative women with similar demographic and risk behavior characteristics, and the colonization rates correlate with increasing severity of immunosuppression. Symptomatic vulvovaginal candidiasis is also more frequent in women with HIV infection and similarly correlates with severity of immunodeficiency. In addition, among women with HIV infection, systemic azole exposure is associated with the isolation of nonalbicans Candida species from the vagina.
On the basis of available data, therapy for uncomplicated and complicated vulvovaginal candidiasis in women with HIV infection should not differ from that for seronegative women. Although long-term prophylactic therapy with fluconazole at a dose of 200 mg weekly has been effective in reducing C. albicans colonization and symptomatic vulvovaginal candidiasis 67, this regimen is not recommended for women with HIV infection in the absence of complicated vulvovaginal candidiasis 68. Although vulvovaginal candidiasis is associated with increased HIV seroconversion in HIV-negative women and increased HIV cervicovaginal levels in women with HIV infection, the effect of treatment for vulvovaginal candidiasis on HIV acquisition and transmission remains unknown.
Management of sex partners
No data exist to support the treatment of sex partners of patients with complicated vulvovaginal candidiasis. Therefore, no recommendation can be made.
Can vulvovaginal candidiasis be prevented or avoided?
To reduce your risk of vaginal yeast infections, wear underwear that has a cotton crotch and doesn’t fit too tightly.
Here are some things you can do to help prevent a yeast infection:
- Avoid tight-fitting pantyhose
- Avoid douching, which removes some of the normal bacteria in the vagina that protect you from infection
- Avoid scented feminine products, including bubble bath, deodorant sanitary pads, tampons and hygiene sprays
- Avoid using colored or perfumed toilet paper
- Avoid hot tubs and very hot baths
- Avoid unnecessary antibiotic use, such as for colds or other viral infections
- Avoid staying in wet clothes, such as swimsuits and workout attire, for long periods of time
- Don’t wear tight-fitting clothing or clothing made out of synthetic material
- Wear cotton panties.
- Don’t wear pantyhose or leotards every day.
- Use your blow dryer on a low, cool setting to help dry your genital area after you bathe or shower and before getting dressed.
- Change out of wet swimsuits or other damp clothes as soon as you can.
Best probiotic for women’s gut health
Probiotics have been widely studied in a variety of gastrointestinal diseases, and one in five Americans takes probiotics for digestive problems 69. The most studied probiotics for human use belong to the Lactobacillus, Bifidobacterium and Saccharomyces species 70. Probiotics are not effective for acute pancreatitis or Crohn disease 71. A meta-analysis of six randomized controlled trials including 536 adults with severe acute pancreatitis showed that probiotics compared with control did not significantly affect pancreatic infection rate, total number of infections, operation rate, hospital length of stay, or mortality 72. Three Cochrane reviews found insufficient evidence for the effectiveness of probiotics in patients with Crohn disease for induction of remission, maintenance of remission, or prevention of postoperative recurrence 73, 74, 75, 76.
Table 3. Summary of gastrointestinal conditions that may benefit from probiotic use
| Clinical condition | Studied probiotic species | Studied products* | Third-party tested products | Comments |
| Antibiotic-associated diarrhea 77 | Bacillus clausii, coagulans | Align | Garden of Life Raw Probiotics Ultimate Care | Broad-spectrum combination products are likely to have the most benefit; consider 10 billion colony-forming units (CFUs) per day of each organism |
| Bifidobacterium animalis subsp lactis, bifidum, breve, longum, longum subsp infantis | Bio-K+ | Now Foods Probiotic-10 | ||
| Clostridium butyricum | Culturelle | Renew Life Ultimate Flora | ||
| Enterococcus faecium | DanActive | Sedona Labs iFlora Multi-Probiotics | ||
| Lactobacillus acidophilus, casei, casei subsp immunitas, delbrueckii subsp bulgaricus, paracasei, plantarum, reuteri, rhamnosus, rhamnosus GG, sporogenes | Florastor | |||
| Lactococcus lactis subsp diacetylactis | HOWARU Restore | |||
| Leuconostoc cremoris | MIYAIRI 588† | |||
| Saccharomyces boulardii, florentinus | VSL#3 | |||
| Streptococcus thermophilus | ||||
| Clostridium difficile–associated diarrhea 78 | Bifidobacterium animalis subsp lactis, breve, longum, longum subsp infantis | Align | Garden of Life Raw Probiotics Ultimate Care | — |
| Clostridium butyricum | Culturelle | Now Foods Probiotic-10 | ||
| Lactobacillus acidophilus, casei, delbrueckii subsp bulgaricus, paracasei, plantarum, rhamnosus GG | DanActive | Renew Life Ultimate Flora | ||
| Saccharomyces boulardii | Florastor | Sedona Labs iFlora Multi-Probiotics | ||
| Streptococcus thermophilus | MIYAIRI 588† | |||
| VSL#3 | ||||
| Helicobacter pylori 79 | Bifidobacterium animalis, breve | Bacid | Garden of Life Raw Probiotics Ultimate Care | Adjunct to antibiotics |
| Lactobacillus acidophilus, casei, delbrueckii subsp bulgaricus, gasseri, johnsonii, reuteri, rhamnosus, rhamnosus GG | Culturelle | Now Foods Probiotic-10 | ||
| Propionibacterium freudenreichii subsp shermanii (JS) | Lactinex | Renew Life Ultimate Flora | ||
| Streptococcus thermophilus | Sedona Labs iFlora Multi-Probiotics | |||
| Hepatic encephalopathy 80 | Bifidobacterium breve, longum, longum subsp infantis | Align | Garden of Life Raw Probiotics Ultimate Care | — |
| Escherichia coli (Nissle) | Mutaflor | Now Foods Probiotic-10 | ||
| Lactobacillus acidophilus, casei, delbrueckii subsp bulgaricus, paracasei, plantarum | VSL#3 | Renew Life Ultimate Flora | ||
| Leuconostoc mesenteroides | Sedona Labs iFlora Multi-Probiotics | |||
| Pediococcus pentosaceus | ||||
| Streptococcus thermophilus | ||||
| Ulcerative colitis 73 | Bifidobacterium animalis subsp lactis, breve, longum, longum subsp infantis | Activia | Garden of Life Raw Probiotics Ultimate Care | VSL#3 and similar high-dose multispecies products with several Bifidobacterium species are preferred |
| Escherichia coli (Nissle) | Align | Now Foods Probiotic-10 | ||
| Lactobacillus acidophilus, delbrueckii subsp bulgaricus, johnsonii, paracasei, plantarum, rhamnosus, rhamnosus GG | Bacid | Renew Life Ultimate Flora | ||
| Streptococcus thermophilus | Culturelle | Sedona Labs iFlora Multi-Probiotics | ||
| Mutaflor | ||||
| VSL#3 | ||||
| Irritable bowel syndrome (IBS) 81 | Bifidobacterium animalis subsp lactis, bifidum, breve, longum | Activia | Garden of Life Raw Probiotics Ultimate Care | — |
| Enterococcus faecalis | Align | Now Foods Probiotic-10 | ||
| Escherichia coli (Nissle) | Bacid | Renew Life Ultimate Flora | ||
| Lactobacillus acidophilus, delbrueckii subsp bulgaricus, lactis, paracasei, plantarum, rhamnosus, rhamnosus GG | Culturelle | Sedona Labs iFlora Multi-Probiotics | ||
| Propionibacterium freudenreichii subsp shermanii | USANA | |||
| Streptococcus thermophilus | VSL#3 | |||
| YoPlus | ||||
| Colic 82 | Lactobacillus reuteri ATCC 55730/DSM 17938 | — | Jarrow Formulas Baby’s Jarro-Dophilus plus FOS | — |
| Nature’s Way Primadophilus Reuteri | ||||
| Necrotizing enterocolitis 83 | Bacillus cereus, subtilis | Bacid | Florastor Kids | Products containing a variety of Bifidobacterium species are most beneficial |
| Bifidobacterium adolescentis, animalis subsp lactis, bifidum, breve, longum, longum subsp infantis | Culturelle | Nature’s Answer Probiotics for Kids | Dose approximately 3 billion CFUs per day of each organism for the first seven days of life; adult powdered products may be given at one-fourth dose in breast milk or formula 84 | |
| Enterococcus faecalis, faecium | Florajen | |||
| Lactobacillus acidophilus, casei, delbrueckii subsp bulgaricus, plantarum, reuteri, rhamnosus, rhamnosus GG, sporogenes | Florastor | |||
| Saccharomyces boulardii | ||||
| Streptococcus thermophilus |
Footnote:
*List is not comprehensive.
†Not available by this name in the United States.
Abbreviation: CFU = colony-forming unit
[Source 71 ]Table 4. Probiotic species shown to be effective for gastrointestinal conditions
| Acute infectious diarrhea | Acute pancreatitis | Antibiotic-associated diarrhea | Clostridium difficile–associated diarrhea | Clostridium difficile infection | Chemotherapy-associated diarrhea | Colic | Crohn disease | Functional abdominal pain | Functional constipation | Helicobacter pylori infection | Hepatic encephalopathy | Irritable bowel syndrome | NAFLD/NASH | Necrotizing enterocolitis | Radiation-associated diarrhea | Traveler’s diarrhea | Ulcerative colitis | |
| Bacillus cereus | • | |||||||||||||||||
| Bacillus coagulans | • | |||||||||||||||||
| Bacillus subtilis | • | • | ||||||||||||||||
| Bifidobacterium adolescentis | • | |||||||||||||||||
| Bifidobacterium animalis subsp lactis | • | • | • | • | • | • | • | • | • | • | • | • | ||||||
| Bifidobacterium bifidum | • | • | • | • | • | • | ||||||||||||
| Bifidobacterium breve | • | • | • | • | • | • | • | • | • | • | • | • | • | • | ||||
| Bifidobacterium longum | • | • | • | • | • | • | • | • | • | • | • | • | • | |||||
| Bifidobacterium longum subsp infantis | • | • | • | • | • | • | • | • | • | • | ||||||||
| Clostridium butyricum (MIYAIRI 588) | • | • | • | |||||||||||||||
| Enterococcus faecalis | • | • | • | |||||||||||||||
| Enterococcus faecium (SF68) | • | • | • | |||||||||||||||
| Escherichia coli (Nissle) | • | • | • | • | ||||||||||||||
| Lactobacillus acidophilus | • | • | • | • | • | • | • | • | • | • | • | • | • | • | ||||
| Lactobacillus casei | • | • | • | • | • | • | • | • | • | • | • | |||||||
| Lactobacillus casei subsp immunitas | • | |||||||||||||||||
| Lactobacillus delbrueckii subsp bulgaricus | • | • | • | • | • | • | • | • | • | • | • | • | • | |||||
| Lactobacillus fermentum | • | |||||||||||||||||
| Lactobacillus gasseri | • | |||||||||||||||||
| Lactobacillus johnsonii | • | • | • | |||||||||||||||
| Lactobacillus paracasei | • | • | • | • | • | • | • | • | • | • | ||||||||
| Lactobacillus plantarum | • | • | • | • | • | • | • | • | • | • | • | • | ||||||
| Lactobacillus reuteri | • | • | • | • | • | • | ||||||||||||
| Lactobacillus rhamnosus | • | • | • | • | • | • | • | • | ||||||||||
| Lactobacillus rhamnosus GG | • | • | • | • | • | • | • | • | • | • | • | • | • | |||||
| Lactobacillus sporogenes | • | • | • | |||||||||||||||
| Lactococcus cremoris | • | |||||||||||||||||
| Lactococcus lactis | • | |||||||||||||||||
| Lactococcus lactis subsp diacetylactis | • | • | • | |||||||||||||||
| Leuconostoc cremoris | • | • | ||||||||||||||||
| Leuconostoc mesenteroides | • | • | ||||||||||||||||
| Pediococcus pentosaceus | • | • | ||||||||||||||||
| Propionibacterium freudenreichii subsp shermanii | • | • | ||||||||||||||||
| Saccharomyces boulardii | • | • | • | • | • | • | • | |||||||||||
| Saccharomyces florentinus | • | |||||||||||||||||
| Streptococcus salivarius | • | |||||||||||||||||
| Streptococcus thermophilus | • | • | • | • | • | • | • | • | • | • | • | • | • | • | ||||
| VSL#3 | • | • | • | • | • | • | • | • | • |
Abbreviations: NAFLD = nonalcoholic fatty liver disease; NASH = nonalcoholic steatohepatitis.
[Source 71 ]Constipation
Constipation is a very common gastrointestinal problem among all ages and populations in the United States. Almost everyone gets constipated at some time in their life. About 16 out of 100 adults have symptoms of constipation. About 33 out of 100 adults ages 60 and older have symptoms of constipation 85. Constipation happens when your stool is hard and dry, making it difficult to pass.
Constipation is a condition in which you may have 86:
- fewer than three bowel movements a week
- stools that are hard, dry, or lumpy
- stools that are difficult or painful to pass
- a feeling that not all stool has passed
However, people can have different bowel movement patterns, and only you know what’s normal for you. Constipation may last for a short or long time.
Certain people are more likely to become constipated, including 87:
- women, especially during pregnancy or after giving birth
- older adults
- non-Caucasians
- people who eat little to no fiber
- people who take certain medicines or dietary supplements
- people with certain health problems, including functional gastrointestinal disorders
Constipation is not a disease, but may be a symptom of another medical problem.
Constipation is usually caused by:
- not eating enough fiber
- not drinking enough water or dehydration
- not exercising enough
- ignoring the urge to pass a stool when you need to
- being stressed
You can also get constipation when you:
- are pregnant
- are due to get your period
- use laxatives too much
- are taking certain medications and dietary supplements, such as:
- antacids that contain aluminum and calcium
- anticholinergics and antispasmodics
- anticonvulsants—used to prevent seizures
- calcium channel blockers
- diuretics
- iron supplements
- medicines used to treat Parkinson’s disease
- narcotic pain medicines
- some medicines used to treat depression
- don’t do enough exercise
- have a medical condition such as diabetes, Parkinson’s disease or multiple sclerosis
- have a problem with your digestive tract, such as irritable bowel syndrome (IBS), diverticulitis or hemorrhoids
- delayed emptying of the colon from pelvic floor disorders, especially in women, and colon surgery
- have emotional problems like anxiety, depression or grief
Certain health and nutrition problems can cause constipation:
- Celiac disease
- spinal cord or brain injuries
- conditions that affect your metabolism, such as diabetes
- conditions that affect your hormones, such as hypothyroidism (underactive thyroid)
- inflammation linked to diverticular disease or proctitis
- intestinal obstructions, including anorectal blockage and tumors
- anatomic problems of your digestive tract
Occasionally, constipation can be a sign of an underlying disease, such as bowel cancer. In such cases, there are likely to be other symptoms, such as a recent change in bowel habits, weight loss, anal bleeding or abdominal pain. If you have any of these symptoms, see your doctor. You should also see a doctor if your symptoms do not go away with self-care or you have a family history of colon or rectal cancer.
You should see a doctor right away if you have constipation and any of the following symptoms:
- bleeding from your rectum
- blood in your stool
- constant pain in your abdomen
- inability to pass gas
- vomiting
- fever
- lower back pain
- losing weight without trying
Doctors use your medical and family history, a physical exam, or medical tests to diagnose and find the cause of your constipation.
Your doctor may use one or more of the following lab tests to look for signs of certain diseases and conditions that may be causing your constipation:
- Blood tests can show signs of anemia, hypothyroidism, and celiac disease.
- Stool tests can show the presence of blood and signs of infection and inflammation.
- Urine tests can show signs of diseases such as diabetes.
Probiotics are effective for children and adults with constipation. Patients should start probiotics at the onset of symptoms and continue as symptoms persist. A meta-analysis of two trials including 165 adults with chronic idiopathic constipation reported a significant increase in the mean number of stools per week in patients treated with probiotics vs. placebo 88. An randomized controlled trial of 59 children with functional chronic intestinal constipation found significant improvements favoring Bifidobacterium-containing yogurt vs. standard yogurt for improving defecation frequency, pain with defecation, and abdominal pain 89.
You can most often treat your constipation at home by doing the following:
Change what you eat and drink
Changing what you eat and drink may make your stools softer and easier to pass. To help relieve your symptoms:
- eat more high-fiber foods
- drink plenty of water and other liquids if you eat more fiber or take a fiber supplement
Read about what you should eat and drink to help relieve constipation. Depending on your age and sex, adults should get 25 to 31 grams of fiber a day 90
Get regular physical activity
Getting regular physical activity may help relieve your symptoms.
Try bowel training
Your doctor may suggest that you try to train yourself to have a bowel movement at the same time each day to help you become more regular. For example, trying to have a bowel movement 15 to 45 minutes after breakfast may help, because eating helps your colon move stool.
Make sure you give yourself enough time to have a bowel movement, and use the bathroom as soon as you feel the need to go. Try to relax your muscles or put your feet on a footstool to make yourself more comfortable.
Stop taking certain medicines or dietary supplements
If you think certain medicines or dietary supplements are causing your constipation, talk with your doctor. He or she may change the dose or suggest a different medicine that does not cause constipation. Don’t change or stop any medicine or supplement without talking with a health care professional.
Take over-the-counter medicines
Your doctor may recommend using a laxative for a short time. He or she will tell you what type of laxative is best for you:
- fiber supplements (Citrucel, FiberCon, Metamucil)
- osmotic agents (Milk of Magnesia, Miralax)
- stool softeners (Colace, Docusate)
- lubricants, such as mineral oil (Fleet)
- stimulants (Correctol, Dulcolax)
You should only use stimulants if your constipation is severe or other treatments have not worked.
If you’ve been taking laxatives for a long time and can’t have a bowel movement without taking a laxative, talk with your doctor about how you can slowly stop using them. If you stop taking laxatives, over time, your colon should start moving stool normally.
How do doctors treat constipation?
If self-care treatments don’t work, your doctor may prescribe a medicine to treat your constipation. If you’re taking an over-the-counter or prescription medicine or supplement that can cause constipation, your doctor may suggest you stop taking it, change the dose, or switch to a different one. Talk with your doctor before changing or stopping any medicines.
Prescription medicines
Your doctor may prescribe one of the following medicines for constipation:
- lubiprostone: a medicine prescribed to increase fluid in your digestive tract, which can help reduce pain in your abdomen, make your stool softer, and increase how often you have bowel movements
- linaclotide or plecanatide: medicines that help make your bowel movements regular if you have irritable bowel syndrome with constipation or long-lasting constipation without a known cause
- prucalopride: a medicine that helps your colon move stool if you have long-lasting constipation without a known cause
Biofeedback therapy
If you have problems with the muscles that control bowel movements, your doctor may recommend biofeedback therapy to retrain your muscles. By using biofeedback therapy, you can change how you make your muscles work.
Surgery
Your doctor may recommend surgery to treat an anorectal blockage caused by rectal prolapse if other treatments don’t work. Your doctor may perform surgery to remove your colon if your colon muscles don’t work correctly. If your doctor recommends surgery, ask about the benefits and risks.
How can I prevent constipation?
You can help prevent constipation by doing some of the same things that treat constipation:
- get enough fiber in your diet
- drink plenty of water and other liquids. Staying hydrated is good for your overall health and can help you avoid getting constipated.
- get regular physical activity
- try to have a bowel movement at the same time every day
Good sources of fiber are:
- whole grains, such as whole wheat bread and pasta, oatmeal, and bran flake cereals
- legumes, such as lentils, black beans, kidney beans, soybeans, and chickpeas
- fruits, such as berries, apples with the skin on, oranges, and pears
- vegetables, such as carrots, broccoli, green peas, and collard greens
- nuts, such as almonds, peanuts, and pecans
To help prevent or relieve constipation, avoid foods with little to no fiber, such as:
- chips
- fast food
- meat
- prepared foods, such as some frozen meals and snack foods
- processed foods, such as hot dogs or some microwavable dinners.
Acute infectious diarrhea
Acute infectious diarrhea is also often referred to as gastroenteritis caused by a myriad of viruses, bacteria, and and less often, parasites 91. Clinically, acute infectious diarrhea is classified into two pathophysiologic syndromes, commonly referred to as noninflammatory diarrheal syndrome (mostly viral, milder disease) and inflammatory diarrheal syndrome (mostly invasive or with toxin-producing bacteria, more severe disease) 92. Table 5 compares noninflammatory and inflammatory acute infectious diarrhea 93.
Viral infections are the most common cause of acute diarrhea 94. Bacterial infections are more often associated with travel, comorbidities, and foodborne illness. When a specific organism is identified, the most common causes of acute diarrhea in the United States are Salmonella, Campylobacter, Shigella, and Shiga toxin–producing Escherichia coli (enterohemorrhagic E. coli) 95.
Table 5. Noninflammatory vs. Inflammatory Diarrheal Syndromes
| Factor | Noninflammatory | Inflammatory |
| Cause | Usually viral, but can be bacterial or parasitic | Generally invasive or toxin-producing bacteria |
| Pathophysiology | More likely to promote intestinal secretion without significant disruption in the intestinal mucosa | More likely to disrupt mucosal integrity, which may lead to tissue invasion and destruction |
| History and examination findings | Nausea, vomiting; normothermia; abdominal cramping; larger stool volume; nonbloody, watery stool | Fever, abdominal pain, tenesmus, smaller stool volume, bloody stool |
| Laboratory findings | Absence of fecal leukocytes | Presence of fecal leukocytes |
| Common pathogens | Enterotoxigenic Escherichia coli, Clostridium perfringens, Bacillus cereus, Staphylococcus aureus, Rotavirus, Norovirus, Giardia, Cryptosporidium, Vibrio cholerae | Salmonella (non-Typhi species), Shigella, Campylobacter, Shiga toxin–producing E. coli, enteroinvasive E. coli, Clostridium difficile, Entamoeba histolytica, Yersinia |
| Other | Generally milder disease | Generally more severe disease |
| Severe fluid loss can still occur, especially in malnourished patients |
Table 6. Clinical features of acute diarrhea caused by select pathogens
| Pathogen | Fever | Abdominal pain | Nausea, vomiting, or both | Fecal evidence of inflammation | Bloody stool | Heme-positive stools |
| Bacteria | ||||||
| Campylobacter | Common | Common | Occurs | Common | Occurs | Variable |
| Clostridium difficile | Occurs | Occurs | Not common | Common | Occurs | Occurs |
| Salmonella | Common | Common | Occurs | Common | Occurs | Variable |
| Shiga toxin–producing Escherichia coli | Not common | Common | Occurs | Not common | Common | Common |
| Shigella | Common | Common | Common | Common | Occurs | Variable |
| Vibrio | Variable | Variable | Variable | Variable | Variable | Variable |
| Yersinia | Common | Common | Occurs | Occurs | Occurs | Occurs |
| Parasite | ||||||
| Cryptosporidium | Variable | Variable | Occurs | None to mild | Not common | Not common |
| Cyclospora | Variable | Variable | Occurs | Not common | Not common | Not common |
| Entamoeba histolytica | Occurs | Occurs | Variable | Variable | Variable | Common |
| Giardia | Not common | Common | Occurs | Not common | Not common | Not common |
| Virus | ||||||
| Norovirus | Variable | Common | Common | Not common | Not common | Not common |
Table 7. Clues to the diagnosis of acute diarrhea
| History | Potential pathogen/etiology | ||
| Afebrile, abdominal pain with bloody diarrhea | Shiga toxin–producing Escherichia coli | ||
| Bloody stools | Salmonella, Shigella, Campylobacter, Shiga toxin–producing E. coli, Clostridium difficile, Entamoeba histolytica, Yersinia | ||
| Camping, consumption of untreated water | Giardia | ||
| Consumption of food commonly associated with foodborne illness | |||
| Fried rice | Bacillus cereus | ||
| Raw ground beef or seed sprouts | Shiga toxin–producing E. coli (e.g., E. coli O157:H7) | ||
| Raw milk | Salmonella, Campylobacter, Shiga toxin–producing E. coli, Listeria | ||
| Seafood, especially raw or undercooked shellfish | Vibrio cholerae, Vibrio parahaemolyticus | ||
| Undercooked beef, pork, or poultry | Staphylococcus aureus, Clostridium perfringens, Salmonella, Listeria (beef, pork, poultry), Shiga toxin–producing E. coli (beef and pork), B. cereus (beef and pork), Yersinia (beef and pork), Campylobacter (poultry) | ||
| Exposure to day care centers | Rotavirus, Cryptosporidium, Giardia, Shigella | ||
| Fecal-oral sexual contact | Shigella, Salmonella, Campylobacter, protozoal disease | ||
| Hospital admission | C. difficile, treatment adverse effect | ||
| Human immunodeficiency virus infection, immunosuppression | Cryptosporidium, Microsporida, Isospora, Cytomegalovirus, Mycobacterium aviumintracellulare complex, Listeria | ||
| Medical conditions associated with diarrhea | Endocrine: Hyperthyroidism, adrenocortical insufficiency, carcinoid tumors, medullary thyroid cancer | ||
| Gastrointestinal: Ulcerative colitis, Crohn disease, irritable bowel syndrome, celiac disease, lactose intolerance, ischemic colitis, colorectal cancer, short bowel syndrome, malabsorption, gastrinoma, VIPoma, bowel obstruction, constipation with overflow | |||
| Other: Appendicitis, diverticulitis, human immunodeficiency virus infection, systemic infections, amyloidosis, adnexitis | |||
| Medications or other therapies associated with diarrhea | Antibiotics (especially broad-spectrum), laxatives, antacids (magnesium- or calcium-based), chemotherapy, colchicine, pelvic radiation therapy | ||
| Less common: Proton pump inhibitors, mannitol, nonsteroidal anti-inflammatory drugs, angiotensin-converting enzyme inhibitors, cholesterol-lowering medications, lithium | |||
| Persistent diarrhea with weight loss | Giardia, Cryptosporidium, Cyclospora | ||
| Pregnancy | Listeria | ||
| Recent antibiotic use | C. difficile | ||
| Receptive anal intercourse, with or without rectal pain or proctitis | Herpes simplex virus infection, chlamydia, gonorrhea, syphilis | ||
| Rectal pain or proctitis | Campylobacter, Salmonella, Shigella, E. histolytica, C. difficile, Giardia | ||
| Rice-water stools | V. cholerae | ||
| Several persons with common food exposure have acute onset of symptoms | Food poisoning with preformed toxins | ||
| Onset of symptoms within 6 hours: Staphylococcus, B. cereus (typically causes vomiting) | |||
| Onset of symptoms within 8 to 16 hours: C. perfringens type A (typically causes diarrhea) | |||
| Travel to a developing country | Enterotoxigenic E. coli is most common | ||
| Many other pathogens (e.g., Shigella, Salmonella, E. histolytica, Giardia, Cryptosporidium, Cyclospora, enteric viruses) are possible because of poorly cleaned or cooked food, or fecal contamination of food or water | |||
Because most watery diarrhea is self-limited, testing is usually not indicated 99. The primary goal of the physical examination is to assess the patient’s degree of dehydration. Generally ill appearance, dry mucous membranes, delayed capillary refill time, increased heart rate, and abnormal orthostatic vital signs can be helpful in identifying more severe dehydration. Fever is more suggestive of inflammatory diarrhea. The abdominal examination is important to assess for pain and acute abdominal processes. A rectal examination may be helpful in assessing for blood, rectal tenderness, and stool consistency.
In general, specific diagnostic investigation can be reserved for patients with severe dehydration, more severe illness, persistent fever, bloody stool, or immunosuppression, and for cases of suspected nosocomial infection or outbreak.
- Occult blood testing: It is unclear how much fecal occult blood testing affects pretest probability. Nevertheless, it is a rapid and inexpensive test, and when tests are positive for fecal occult blood in conjunction with the presence of fecal leukocytes or lactoferrin, the diagnosis of inflammatory diarrhea is more common 100. Of note, fecal occult blood testing is 71% sensitive and 79% specific for inflammatory diarrhea in developed countries, but the sensitivity drops to 44% and specificity to 72% in developing countries 101.
- Fecal leukocytes and lactoferrin: Testing stool for leukocytes to screen for inflammatory diarrhea poses several challenges, including the handling of specimens and the standardization of laboratory processing and interpretation. There is a wide variability in sensitivity and specificity. Therefore, this testing has fallen out of favor 101. Lactoferrin is a marker for leukocytes that is released by damaged or deteriorating cells, and increases in the setting of bacterial infections 102. Commercially available immunoassay testing kits are a more precise and less variable method for specimen analysis compared with fecal leukocytes, with a sensitivity greater than 90% and a specificity greater than 70% 103. Although there is some debate as to whether fecal lactoferrin is clearly superior to fecal leukocytes, the speed and simplicity of lactoferrin testing make it the preferred method to screen for the presence of leukocytes when indicated 104.
- Stool cultures: The indiscriminate use of stool cultures in the evaluation of acute diarrhea is inefficient (results are positive in only 1.6% to 5.6% of cases) 96 and expensive, with an estimated cost of $900 to $1,200 per positive stool culture 105. Obtaining cultures only in patients with screening tests positive for leukocytes decreases the cost to $150 per positive culture 106. Obtaining cultures only in patients with grossly bloody stools increases the yield for positive culture results to greater than 30% 107. Although there is no consensus on which patients need a culture, it is reasonable to perform a stool culture if the patient has grossly bloody stool, severe dehydration, signs of inflammatory disease, symptoms lasting more than three to seven days, or immunosuppression 108. Cultures are often obtained for traveler’s diarrhea; however, empiric treatment is also an option 109. In the hospital setting, cultures should be reserved for the reasons listed above or if diarrhea begins more than three days after admission and there has been a nosocomial outbreak, the patient has human immunodeficiency virus infection or neutropenia, or the patient is older than 65 years with significant comorbidity (e.g., end-stage liver, renal, or pulmonary disease; leukemia hemiparesis caused by cardiovascular accident; inflammatory bowel disease) 110.
- Clostridium difficile toxins testing: Testing for Clostridium difficile toxins A and B is recommended for patients who develop unexplained diarrhea after three days of hospitalization; the test will be positive in 15% to 20% of these patients 110. Furthermore, the risk of contracting Clostridium difficile infection increases by seven to 10 times throughout any period of antibiotic treatment and for the first month after antibiotic discontinuation, and this risk is still three times higher in the second and third months after antibiotic discontinuation 111. Therefore, testing for Clostridium difficile toxins is also suggested in patients who develop unexplained diarrhea while using antibiotics or within three months of discontinuing antibiotics. C. difficile testing can be considered in certain populations with significant comorbidities, including older persons and those who are immunocompromised.
- Ova and parasites: Routine analysis for ova and parasites in patients with acute diarrhea is not cost-effective, especially in developed countries 112. Indications for ova and parasite testing include persistent diarrhea lasting more than seven days, especially if associated with infants in day care or travel to mountainous regions; diarrhea in persons with AIDS or men who have sex with men; community waterborne outbreaks; or bloody diarrhea with few fecal leukocytes 109. The benefit of sending multiple samples to increase the test yield is debatable.
- Endoscopy: The role of endoscopy in the diagnosis and management of acute diarrhea is limited. Endoscopic evaluation may be considered if the diagnosis is unclear after routine blood and stool tests, if empiric therapy is ineffective, or if symptoms persist 113. Specifically, lower endoscopy with colonic biopsy and culture can be helpful in patients with diarrhea and suspected tuberculosis or diffuse colitis (as in C. difficile colitis) and in determining noninfectious causes of acute diarrhea, such as inflammatory bowel disease, ischemic colitis, enteropathy related to nonsteroidal anti-inflammatory drug use, and cancer 114.
Acute infectious diarrhea treatment
The first step to treating acute diarrhea is rehydration, preferably oral rehydration 96. Fluids and electrolytes are lost during acute diarrhea, and replenishment is important, especially in young children or adults with chronic medical illness. In adult who are otherwise healthy, severe dehydration resulting from acute diarrhea is unusual unless vomiting is prolonged. Nonetheless, replacement of fluid losses remains an adjunct to other therapy and helps the patient feel better more quickly. Travelers should remember to use only beverages that are sealed, treated with chlorine, boiled, or are otherwise known to be purified.
For severe fluid loss, replacement is best accomplished with oral rehydration solution (ORS) prepared from packaged oral rehydration salts, such as those provided by the World Health Organization. An oral rehydration solution (ORS) must contain a mixture of salt and glucose in combination with water to best use the intestine’s sodium-glucose coupled cellular transport mechanism. ORS is widely available at stores and pharmacies in most developing countries. ORS is prepared by adding 1 packet to the indicated volume of boiled or treated water—generally 1 liter. Travelers may find most ORS formulations to be relatively unpalatable due to their saltiness. In mild cases, rehydration can be maintained with any palatable liquid (including sports drinks), although overly sweet drinks, such as sodas, can cause osmotic diarrhea if consumed in quantity.
In 2002, the World Health Organization endorsed an ORS with reduced osmolarity (250 mOsm per L or less compared with the prior standard of 311 mOsm per L). The reduced osmolarity ORS decreases stool outputs, episodes of emesis, and the need for intravenous rehydration 115, without increasing hyponatremia, compared with the standard ORS 116. A reduced osmolarity ORS can be roughly duplicated by mixing 1/2 teaspoon of salt, 6 teaspoons of sugar, and 1 liter of water. If oral rehydration is not feasible, intravenous rehydration may be necessary.
Feeding
Early refeeding decreases intestinal permeability caused by infections, reduces illness duration, and improves nutritional outcomes 117. This is particularly important in developing countries where underlying preexisting malnutrition is often a factor. Although the BRAT diet (bananas, rice, applesauce, and toast) and the avoidance of dairy are commonly recommended, supporting data for these interventions are limited. Instructing patients to refrain from eating solid food for 24 hours also does not appear useful 118.
Antidiarrheal medications
The antimotility agent loperamide (Imodium) may reduce the duration of diarrhea by as much as one day and increase the likelihood of clinical cure at 24 and 48 hours when given with antibiotics for traveler’s diarrhea 119. A loperamide/simethicone combination has demonstrated faster and more complete relief of acute nonspecific diarrhea and gas-related discomfort compared with either medication alone 120.
Loperamide may cause dangerous prolongation of illness in patients with some forms of bloody or inflammatory diarrhea and, therefore, should be restricted to patients with nonbloody stool 121. The antisecretory drug bismuth subsalicylate (Pepto-Bismol) is a safe alternative in patients with fever and inflammatory diarrhea. There is inadequate evidence to recommend the use of the absorbents kaolin/pectin, activated charcoal, or attapulgite (no longer available in the United States). The antisecretory drug racecadotril, widely used in Europe but unavailable in the United States, appears to be more tolerable and as effective as loperamide 122.
Antibiotic therapy
Because acute diarrhea is most often self-limited and caused by viruses, routine antibiotic use is not recommended for most adults with nonsevere, watery diarrhea. Additionally, the overuse of antibiotics can lead to resistance (e.g., Campylobacter), harmful eradication of normal flora, prolongation of illness (e.g., superinfection with C. difficile), prolongation of carrier state (e.g., delayed excretion of Salmonella), induction of Shiga toxins (e.g., from Shiga toxin–producing E. coli), and increased cost.
However, when used appropriately, antibiotics are effective for shigellosis, campylobacteriosis, C. difficile, traveler’s diarrhea, and protozoal infections. Antibiotic treatment of traveler’s diarrhea (usually a quinolone) is associated with decreased severity of illness and a two-or three-day reduction in duration of illness 123. If the patient’s clinical presentation suggests the possibility of Shiga toxin–producing E. coli (e.g., bloody diarrhea, history of eating seed sprouts or rare ground beef, proximity to an outbreak), antibiotic use should be avoided because it may increase the risk of hemolytic uremic syndrome 124. Conservative management without antibiotic treatment is less successful for diarrhea lasting more than 10 to 14 days, and testing and treatment for protozoal infections should be considered 96. Antibiotics may be considered in patients who are older than 65 years, immunocompromised, severely ill, or septic. Table 8 summarizes antibiotic therapy for acute diarrhea 125, 97.
Table 8. Summary of antibiotic therapy for acute diarrhea
| Organism | Therapy effectiveness | Preferred medication | Alternative medications | Comments |
| Bacterial | ||||
| Campylobacter | Proven in dysentery and sepsis, possibly effective in enteritis | Azithromycin (Zithromax), 500 mg once per day for 3 to 5 days | Erythromycin, 500 mg four times per day for 3 to 5 days | Consider prolonged treatment if the patient is immunocompromised |
| Ciprofloxacin (Cipro), 500 mg twice per day for 5 to7 days | ||||
| Clostridium difficile | Proven | Metronidazole (Flagyl), 500 mg three times per day for 10 days | Vancomycin, 125 mg four times per day for 10 days | If an antimicrobial agent is causing the diarrhea, it should be discontinued if possible |
| Enteropathogenic/enteroinvasive Escherichia coli | Possible | Ciprofloxacin, 500 mg twice per day for 3 days | TMP/SMX DS, 160/800 mg twice per day for 3 days | — |
| Enterotoxigenic E. coli | Proven | Ciprofloxacin, 500 mg twice per day for 3 days | TMP/SMX DS, 160/800 mg twice per day for 3 days | Enterotoxigenic E. coli is the most common cause of traveler’s diarrhea |
| Azithromycin, 500 mg per day for 3 days | ||||
| Salmonella, non-Typhi species | Doubtful in enteritis; proven in severe infection, sepsis, or dysentery | — | Options for severe disease: Ciprofloxacin, 500 mg twice per day for 5 to 7 days | In addition to patients with severe disease, it is appropriate to treat patients younger than 12 months or older than 50 years, and patients with a prosthesis, valvular heart disease, severe atherosclerosis, malignancy, or uremia |
| TMP/SMX DS, 160/800 mg twice per day for 5 to 7 days | ||||
| Azithromycin, 500 mg per day for 5 to 7 days | Patients who are immunocompromised should be treated for 14 days | |||
| Shiga toxin–producing E. coli | Controversial | No treatment | No treatment | The role of antibiotics is unclear; they are generally avoided because of their association with hemolytic uremic syndrome |
| Antimotility agents should be avoided | ||||
| Shigella | Proven in dysentery | Ciprofloxacin, 500 mg twice per day for 3 days, or 2-g single dose | Azithromycin, 500 mg twice per day for 3 days | Use of TMP/SMX is limited because of resistance |
| TMP/SMX DS, 160/800 mg twice per day for 5 days | Patients who are immunocompromised should be treated for 7 to 10 days | |||
| Ceftriaxone (Rocephin), 2- to 4-g single dose | ||||
| Vibrio cholerae | Proven | Doxycycline, 300-mg single dose | Azithromycin, 1-g single dose | Doxycycline and tetracycline are not recommended in children because of possible tooth discoloration |
| Tetracycline, 500 mg four times per day for 3 days | ||||
| TMP/SMX DS, 160/800 mg twice per day for 3 days | ||||
| Yersinia | Not needed in mild disease or enteritis, proven in severe disease or bacteremia | — | Options for severe disease: | — |
| Doxycycline combined with an aminoglycoside | ||||
| TMP/SMX DS, 160/800 mg twice per day for 5 days | ||||
| Ciprofloxacin, 500 mg twice per day for 7 to 10 days | ||||
| Protozoal | ||||
| Cryptosporidium | Possible | Therapy may not be necessary in immunocompetent patients with mild disease or in patients with AIDS who have a CD4 cell count greater than 150 cells per mm3 | Option for severe disease: Nitazoxanide (Alinia), 500 mg twice per day for 3 days (may offer longer treatment for refractory cases in patients with AIDS) | Highly active antiretroviral therapy, which achieves immune reconstitution, is adequate to eradicate intestinal disease in patients with AIDS |
| Cyclospora or Isospora | Proven | TMP/SMX DS, 160/800 mg twice per day for 7 to 10 days | — | — |
| AIDS or immunosuppression: TMP/SMX DS, 160/800 mg twice to four times per day for 10 to 14 days, then three times weekly for maintenance | ||||
| Entamoeba histolytica | Proven | Metronidazole, 750 mg three times per day for 5 to 10 days, plus paromomycin, 25 to 35 mg per kg per day in 3 divided doses for 5 to 10 days | Tinidazole (Tindamax), 2 g per day for 3 days, plus paromomycin, 25 to 35 mg per kg per day in 3 divided doses for 5 to 10 days | If the patient has severe disease or extraintestinal infection, including hepatic abscess, serology will be positive |
| Giardia | Proven | Metronidazole, 250 to 750 mg three times per day for 7 to 10 days | Tinidazole, 2-g single dose | Relapses may occur |
| Microsporida | Proven | Albendazole (Albenza), 400 mg twice per day for 3 weeks | — | Highly active antiretroviral therapy, which achieves immune reconstitution, is adequate to eradicate intestinal disease in patients with AIDS |
Abbreviations: DS = double strength; TMP/SMX = trimethoprim/sulfamethoxazole
Probiotics for acute infectious diarrhea
Probiotics are effective for acute infectious diarrhea caused by bacteria, but there are inconsistent results for the effectiveness of probiotics for diarrhea caused by viruses. Probiotics are thought to work by stimulating the immune system and competing for binding sites on intestinal epithelial cells. A Cochrane review of 63 randomized controlled trials and quasi-randomized controlled trials included 8,014 infants, children, and adults with acute infectious diarrhea 126. The researchers found that probiotics significantly reduced the mean duration of diarrhea (25 fewer hours); decreased the risk of diarrhea lasting four or more days by 59%; and led to approximately one fewer stool on day 2 126. A meta-analysis of 17 randomized controlled trials in 2,102 children comparing probiotics vs. control for the treatment of acute diarrhea showed a significant reduction in the duration of diarrhea with probiotic use (20 fewer hours) 127. Another meta-analysis of eight randomized controlled trials involving 1,229 children found that Lactobacillus reuteri administration reduced the duration of diarrhea (25 fewer hours) and increased the cure rate on days 1 and 2 128. However, a randomized controlled trial of 646 children with acute watery diarrhea caused predominantly by rotavirus found no significant difference between the group that received Lactobacillus rhamnosus GG probiotics and the control group in the daily frequency of stools, duration of diarrhea, vomiting, or length of hospital stay 129. A meta-analysis of two randomized controlled trials in 201 children with diarrhea from rotavirus found a significant reduction in diarrhea in those treated with L. rhamnosus GG vs. placebo (two fewer days) 130.
For patients with acute infectious diarrhea, probiotics should be started at the onset of symptoms and, although there is no evidence to support length of treatment, scientists suggest continuing for one to two weeks following the resolution of symptoms. A meta-analysis of 12 randomized controlled trials with 5,171 participants found a 15% relative decrease in the risk of traveler’s diarrhea with probiotic use 131. For prevention of traveler’s diarrhea, probiotics should be started two days before travel and continued throughout the trip.
Although many species are generally categorized as probiotics, even closely related strains may have different clinical effects. Effects of strain-specific probiotics need to be verified in adult studies before a specific evidence-based recommendation can be made 99.
Zinc supplementation
Research in children suggests that zinc supplementation (20 mg per day for 10 days in children older than two months) may play a crucial role in treating and preventing acute diarrhea, particularly in developing countries. Studies demonstrate a decrease in the risk of dehydration, and in the duration and severity of the diarrheal episode by an estimated 20% to 40% 132. Additional research is needed to evaluate potential benefits of zinc supplementation in the adult population.
Best probiotic for women with IBS
Irritable bowel syndrome (IBS) is a common functional disorder that affects the large intestine and causes symptoms such as abdominal pain, bloating, cramping, constipation, and diarrhea. With IBS, you have these symptoms without any visible signs of damage or disease in your digestive tract. As many as one in five Americans have symptoms of IBS 133. Women are up to two times more likely than men to develop IBS 133. People younger than age 50 are more likely to develop IBS than people older than age 50 134. The cause of IBS isn’t well understood growing evidence suggests potential roles for intestinal microbiota in its pathophysiology and symptoms; IBS has also been linked to stress, large meals, certain foods, and alcohol 135. IBS is a functional gastrointestinal disorder. Functional gastrointestinal disorders, which doctors now call disorders of gut-brain interactions, are related to problems with how your brain and your gut work together 136. These problems can cause your gut to be more sensitive and change how the muscles in your bowel contract. If your gut is more sensitive, you may feel more abdominal pain and bloating. Changes in how the muscles in your bowel contract lead to diarrhea, constipation, or both.
According to this research, proinflammatory bacterial species, including Enterobacteriaceae, are abundant in patients with IBS, who typically also have a corresponding reduction in amounts of Lactobacillus and Bifidobacterium 137. Probiotic products commonly contain Lactobacillus and Bifidobacterium and, therefore, have the potential to restore some missing microbial functionality and, consequently, help manage IBS symptoms. Although probiotics are a promising and reasonable treatment option for IBS, the overall quality and quantity of evidence are relatively weak.
Several meta-analyses have assessed the role of probiotics in patients with IBS 138, 139, 140, 141, 142, 143. Most have found that probiotics have a positive, although modest, beneficial effect. For example, a meta-analysis of 23 randomized controlled trials in a total of 2,575 patients found that, overall, probiotics reduced the risk that IBS symptoms would persist or not improve by 21% 139. Probiotics are somewhat effective in children and adults with irritable bowel syndrome (IBS) and in children with functional abdominal pain 71. A guideline and meta-analysis of 23 trials involving 2,575 children and adults with IBS found that probiotics significantly improved global symptoms, bloating, and flatulence compared with placebo, but the quality of studies was low 144. A meta-analysis of 21 randomized controlled trials involving 1,639 adults with IBS found that probiotics significantly improved overall symptom response and quality of life compared with placebo 81. A meta-analysis of children with IBS or functional abdominal pain found that probiotics increased the likelihood of treatment success compared with placebo and decreased abdominal pain intensity; however, there was no effect on abdominal pain frequency 145.
A 2018 review of 53 studies (5,545 total participants) of probiotics for irritable bowel syndrome (IBS) concluded that probiotics may have beneficial effects on global IBS symptoms and abdominal pain, but it was not possible to draw definite conclusions about their effectiveness or to identify which species, strains, or combinations of probiotics are most likely to be helpful 138.
Various species and strains of probiotics had beneficial effects on global IBS symptoms, abdominal pain, bloating, and flatulence scores, but the quality of the studies was low. Some combinations of probiotics were superior to individual strains in this analysis, but no specific combination was superior to another. A second meta-analysis of 15 randomized- controlled trials in a total of 1,793 patients with IBS found that probiotics reduced overall symptoms and abdominal pain more than placebo after 8 to 10 weeks of therapy; in children, these supplements also improved mucosal barrier function 140.
A more recent systematic review included 35 randomized controlled trials of 16 single-strain and 19 multi-strain products in 3,406 adults with IBS 146. Of the studies that found a statistically significant reduction in global symptoms (14 of 29 trials) or a clinically meaningful reduction in abdominal pain (8 of 34 trials), most used multi-strain probiotic products. Furthermore, only trials of multi-strain products found a clinically meaningful improvement in quality of life 141, 142.
Whether different strains of probiotic bacteria have beneficial effects on IBS probably depends on the IBS symptom being evaluated 147. In a meta-analysis of 10 randomized controlled trials with a total of 877 adults treated with probiotics or placebo for 4 weeks to 6 months, pain scores improved significantly with administration of probiotics containing Bifidobacterium breve, Bifidobacterium longum, or Lactobacillus acidophilus species compared with placebo treatment 148. In contrast, Streptococcus salivarius ssp. thermophilus, Bifidobacterium animalis, Bifidobacterium infantis, Lactobacillus casei, Lactobacillus plantarum, Lactobacillus bulgaricus, and Saccharomyces boulardii had no significant effect. The abdominal distension scores improved with use of probiotics containing Bifidobacterium breve, Bifidobacterium infantis, Lactobacillus casei, or Lactobacillus plantarum species. Flatulence declined with use of all tested probiotics, but the studies showed no positive effect of probiotics on quality of life.
Overall, the available evidence indicates that probiotics might reduce some symptoms of IBS. However additional high-quality clinical trials are needed to confirm the specific strain, dose, and duration of treatment required as well as the type of IBS (such as with predominant diarrhea or constipation) that can be treated effectively with probiotics.
Patients should consider starting probiotics at the onset of symptoms and continue as needed for persistent symptoms.
How do doctors treat IBS?
Doctors may treat irritable bowel syndrome (IBS) by recommending changes in what you eat and other lifestyle changes, medicines, probiotics, and mental health therapies. You may have to try a few treatments to see what works best for you. Your doctor can help you find the right treatment plan.
Changes to what you eat and other lifestyle changes
Changes in what you eat may help treat your symptoms. Your doctor may recommend trying one of the following changes to help treat your symptoms of irritable bowel syndrome (IBS) 149:
- eat more fiber
- avoid gluten
- follow a special eating plan called the low FODMAP diet
Different changes may help different people with IBS. You may need to change what you eat for several weeks to see if your symptoms improve. Your doctor may also recommend talking with a dietitian.
Research suggests that other lifestyle changes may help IBS symptoms, including:
- increasing your physical activity
- reducing stressful life situations as much as possible
- getting enough sleep
Diet and nutrition for IBS
Eat more fiber
Dietary fiber, also known as roughage or bulk, is the part of a plant that your body doesn’t absorb during digestion. Fibre is the part of food that is not digested in the small intestine. Dietary fibre moves largely unchanged into the large intestine or colon where it is fermented by friendly bacteria that live there. Fiber may improve constipation in IBS because it makes stool soft and easier to pass. The 2015-2020 Dietary Guidelines for Americans recommends that adults should get 22 to 34 grams of fiber a day 90.
Recent research suggests that fiber should be categorized by its physical characteristics; how well it dissolves (solubility), how thick it is (viscosity) and how well it breaks down (fermentability). Some commonly known terms are described below:
- Soluble fiber including pectins and beta glucans is found in foods like oats, peas, beans, apples, citrus fruits, carrots, barley and psyllium. Soluble fiber dissolves in water to form a gel-like material. It can help lower blood cholesterol and glucose levels. Foods high in soluble fiber can help you feel full. They also help reduce constipation by speeding up the time it takes for feces (poop) to pass through your body. Soluble dietary fiber has been associated with lower postprandial glucose levels and increased insulin sensitivity in diabetic and healthy subjects; these effects were generally attributed to the viscous and/or gelling properties of soluble fiber 150. Soluble dietary fiber exerts physiological effects on the stomach and small intestine that modulate postprandial glycemic responses, including delaying gastric emptying 151, which accounts for ~35% of the variance in peak glucose concentrations following the ingestion of oral glucose 152, modulating gastrointestinal myoelectrical activity and delaying small bowel transit 153, 154, reducing glucose diffusion through the unstirred water layer 155, and reducing the accessibility of α-amylase to its substrates due to the increased viscosity of gut contents 156. Notably, the increased viscosity and gel-forming properties of soluble fiber are predominantly responsible for its glycemic effect, since the hypoglycemic effect can be reversed by the hydrolysis of guar gum or following ultra-high heating and homogenization 151. In addition, the intestinal absorption of carbohydrates was prolonged by soluble dietary fiber, which was partially due to altered incretin levels, including increased glucagon-like peptide 1 levels 156. In experimental clamp studies, soluble dietary fiber also influenced peripheral glucose uptake mechanisms 157, 158, including increasing skeletal muscle expression of the insulin-responsive glucose transporter type 4 (GLUT-4), which enhances skeletal muscle uptake, augments insulin sensitivity and normalizes blood glucose 158. In humans, various fatty acids stimulate the expression of peroxisome proliferator-activated receptor-γ, which increases adipocyte GLUT-4 levels 159. A more recent study to find out the health benefits of soluble fiber on type 2 diabetes 160. A total of 117 patients with type 2 diabetes between the ages of 40 and 70 were assessed. Patients were randomly assigned to one of two groups, and administered extra soluble dietary fiber (10 or 20 g/day), or to a control group (0 g/day) for one month. The 20 g/day soluble dietary fiber group exhibited significantly improved fasting blood glucose and low-density (LDL) lipoprotein “bad cholesterol” levels, as well as a significantly improved insulin resistance index. In addition, 10 and 20 g/day soluble dietary fiber significantly improved the waist and hip circumferences and levels of triglycerides and apolipoprotein A. The results of the present study suggested that increased and regular consumption of soluble dietary fiber led to significant improvements in blood glucose levels, insulin resistance and metabolic profiles 160.
- Insoluble fiber including cellulose is found in wheat bran and nuts. Insoluble fiber is a type of fibre that doesn’t dissolve in water. Because insoluble fiber absorbs water, it helps to soften the contents of your bowel, contributing to keep the bowels regular. Insoluble fiber promotes the movement of material through your digestive system and increases stool bulk, so it can be of benefit to those who struggle with constipation or irregular stools. Whole-wheat flour, wheat bran, nuts, beans and vegetables, such as cauliflower, green beans and potatoes, are good sources of insoluble fiber. Diverticulitis, an inflammation of the intestine, is one of the most common age-related disorders of the colon in Western society. Among male health professionals in a long-term follow-up study, eating dietary fiber, particularly insoluble fiber, was associated with about a 40 percent lower risk of diverticular disease 161.
- Resistant starch is a soluble fiber that is highly fermentable in the gut. While most starch is digested in the upper part of the gut, resistant starch resists digestion in the small intestine and so goes all the way to the large intestine 162. Once in the large intestine, good bacteria ferment resistant starch. This process produces short chain fatty acids (SCFAs) and gasses that help to keep the lining of the bowel healthy. Resistant starch is starch that is not easily absorbed. Different ways of cooking can create different amounts of resistant starch. For example, resistant starch is found in slightly undercooked (‘al dente’) pasta, cooked but cooled potatoes (including potato salad), cooked and cooled grains like rice, quinoa, barley and buckwheat, under-ripe bananas, beans, lentils and a product called Hi-maize used in some breads and breakfast cereals. Freekeh, a Middle Eastern grain available in some supermarkets, is another good source. In general, foods that are less highly processed contain more resistant starch. An important benefit of resistant starch is that it ferments, which produces substances that help to keep the lining of the bowel healthy. Resistant starch has been classified into five basic “types” 163.
- Type 1 (resistant starch 1) is made up of starch granules surrounded by an indigestible plant matrix.
- Type 2 (resistant starch 2) occurs in its natural form such as in an uncooked potato and high amylose maize.
- Type 3 (resistant starch 3) are crystallized starches made by unique cooking and cooling processes.
- Type 4 (resistant starch 4) is a starch chemically modified by esterification, crosslinking, or transglycosylation and is not found in nature.
- Type 5 (resistant starch 5) is a starch consisting of amylose-lipid complex.
- Prebiotics are types of carbohydrate that only our gut bacteria can feed upon. Some examples are onions, garlic, asparagus and banana.
Research suggests that soluble fiber is more helpful in relieving IBS symptoms.
To help your body get used to more fiber, add foods with fiber to your diet a little at a time. Too much fiber at once can cause gas, which can trigger IBS symptoms. Adding fiber to your diet slowly, by 2 to 3 grams a day, may help prevent gas and bloating.
Avoid gluten
Your doctor may recommend avoiding foods that contain gluten—a protein found in wheat, barley, and rye—to see if your IBS symptoms improve. Foods that contain gluten include most cereal, grains, and pasta, and many processed foods. Some people with IBS have more symptoms after eating gluten, even though they do not have celiac disease.
Low FODMAP diet
Your doctor may recommend that you try a special diet—called the low FODMAP diet—to reduce or avoid certain foods that contain carbohydrates that are hard to digest. These carbohydrates are called FODMAPs.
Examples of foods that contain FODMAPs include 164:
- fruits such as apples, apricots, blackberries, cherries, mango, nectarines, pears, plums, and watermelon, or juice containing any of these fruits
- canned fruit in natural fruit juice, or large amounts of fruit juice or dried fruit
- vegetables such as artichokes, asparagus, beans, cabbage, cauliflower, garlic and garlic salts, lentils, mushrooms, onions, and sugar snap or snow peas
- dairy products such as milk, milk products, soft cheeses, yogurt, custard, and ice cream
- wheat and rye products
- honey and foods with high-fructose corn syrup
- products, including candy and gum, with sweeteners ending in “–ol,” such as sorbitol, mannitol, xylitol, and maltitol
Your doctor may suggest that you try the low FODMAP diet for a few weeks to see if it helps with your symptoms. If your symptoms improve, your doctor may recommend slowly adding foods that contain FODMAPs back into your diet. You may be able to eat some foods with FODMAPs without having IBS symptoms.
Medicines
Your doctor may recommend medicine to relieve your IBS symptoms.
To treat IBS with diarrhea, your doctor may recommend 149:
- loperamide
- rifaximin (Xifaxan), an antibiotic
- eluxadoline (Viberzi)
- alosetron (Lotronex), which is prescribed only to women and is prescribed with special warnings and precautions
To treat IBS with constipation, your doctor may recommend 149:
- fiber supplements (when increasing fiber in your diet doesn’t help)
- laxatives
- lubiprostone (Amitiza)
- linaclotide (Linzess)
- plecanatide (Trulance)
Other medicines may help treat pain in your abdomen, including 149:
- antispasmodics (medicines that help reduce muscle spasms)
- antidepressants , such as low doses of tricyclic antidepressants (TCAs) and selective serotonin reuptake inhibitors (SSRIs)
- coated peppermint oil capsules
Follow your doctor’s instructions when you use medicine to treat IBS. Talk with your doctor about possible side effects and what to do if you have them.
Mental health therapies
Your doctor may recommend mental health therapies to help improve your IBS symptoms. Therapies used to treat IBS include 149:
- cognitive behavioral therapy (CBT), which focuses on helping you change thought and behavior patterns to improve IBS symptoms
- gut-directed hypnotherapy, in which a therapist uses hypnosis—a trance-like state in which you are relaxed or focused—to help improve your IBS symptoms
- relaxation training, which can help you relax your muscles or reduce stress
Best probiotic for women’s urinary tract health
Your urinary tract is your body’s drainage system for removing urine, which is made up of wastes and extra fluid. For normal urination to occur, all body parts in the urinary tract need to work together, and in the correct order. Your urinary tract includes two kidneys, two ureters, a bladder, and a urethra (see Figure 1).
- Kidneys. Two bean-shaped organs, each about the size of a fist. They are located just below your rib cage, one on each side of your spine. Every day, your kidneys filter about 120 to 150 quarts of blood to remove wastes and balance fluids. This process produces about 1 to 2 quarts of urine per day.
- Ureters. Thin tubes of muscle that connect your kidneys to your bladder and carry urine to the bladder.
- Bladder. A hollow, muscular, balloon-shaped organ that expands as it fills with urine. The bladder sits in your pelvis between your hip bones. A normal bladder acts like a reservoir. It can hold 1.5 to 2 cups of urine. Although you do not control how your kidneys function, you can control when to empty your bladder. Bladder emptying is known as urination.
- Urethra. A tube located at the bottom of the bladder that allows urine to exit the body during urination.
The urinary tract also includes two sets of muscles that work together as a sphincter, closing off the urethra to keep urine in the bladder between your trips to the bathroom.
- The internal sphincter muscles of the bladder neck and urethra stay closed until your brain sends signals to urinate.
- The external sphincter muscles surround the internal sphincter and provide extra pressure to keep the urethra closed. You can consciously squeeze the external sphincter and the pelvic floor muscles to keep urine from leaking out.
Figure 1. Female urinary tract system
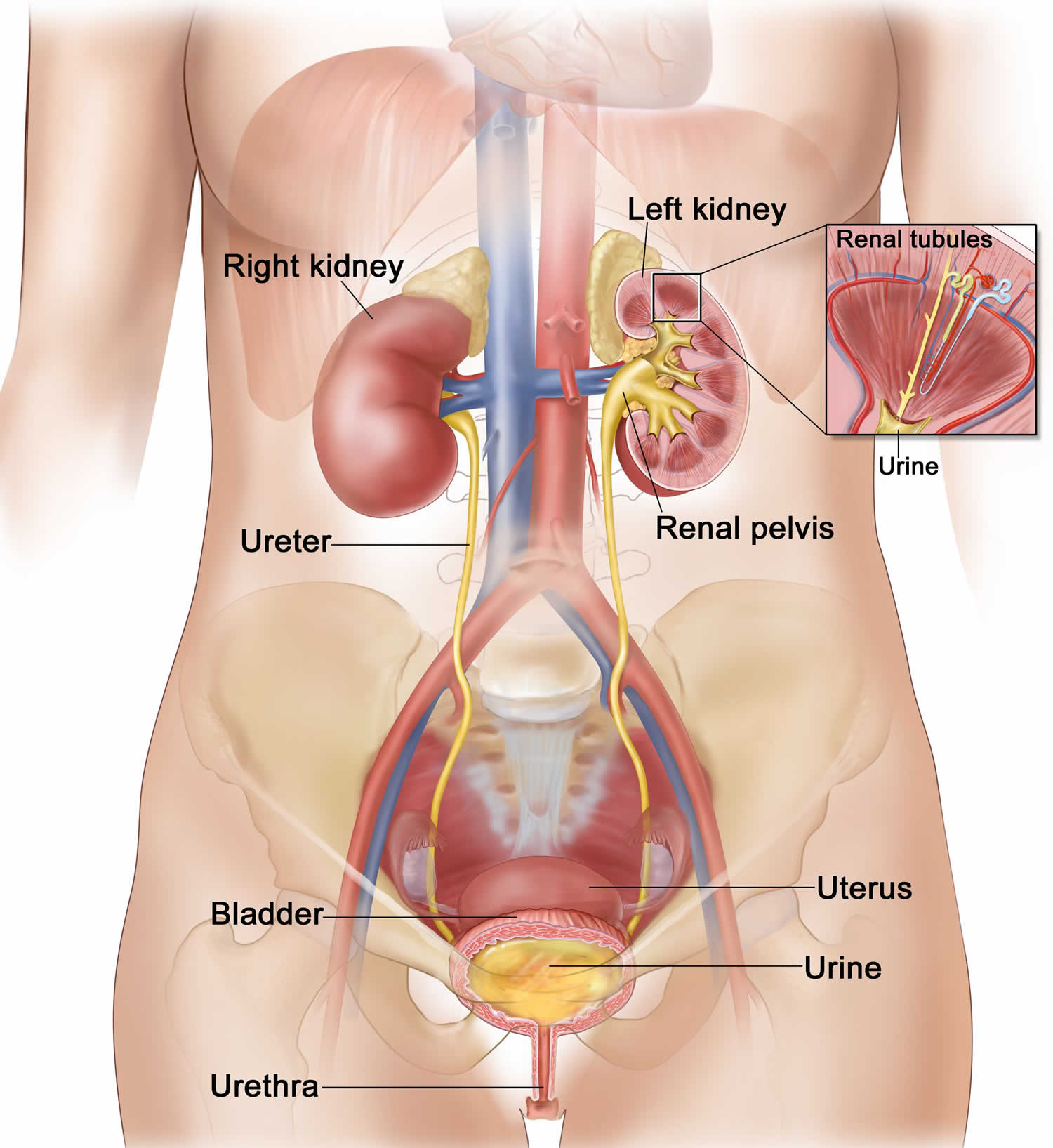
You can help keep your urinary tract healthy by following some of these basic tips.
- Drink enough fluids, especially water. If you’re healthy, try to drink six to eight 8-ounce glasses of fluid each day. You may need to drink more if you have kidney stones or bladder stones. At least half of your fluid intake should be water. You might need to drink less water if you have certain conditions, such as kidney failure or heart disease. Ask your health care professional how much fluid is healthy for you.
- Keep your bowels regular. Regular bowel movements are important to your bladder health. You can promote both bowel health and bladder health by making healthy food choices. You can keep your urinary tract healthy by sticking to an eating plan that includes lean proteins, whole grains, fiber-rich breads, nuts, colorful berries, fruits, and vegetables to promote regular bowel movements.
- Living a healthy lifestyle. Get regular physical activity, limit your alcohol intake, cut down on caffeinated food and drinks, and don’t smoke.
- Go whenever you need to. Often, people will hold their urine because it’s not a good time to go to the bathroom. However, holding in your urine for too long can weaken your bladder muscles and make it harder for your bladder to empty completely. Urine left in your bladder can allow bacteria to grow and makes you more likely to develop a urinary tract infection (UTI).
- Develop healthy bathroom habits. Take enough time to fully empty your bladder when urinating—don’t rush it. Urinate after sex to flush away bacteria that may have entered the urethra during sex. Clean the genital area before and after sex. If you’re a woman, wipe from front to back, especially after a bowel movement, to keep bacteria from getting into the urethra.
- Stay in tune with your body. Pay attention to how often you feel the urge to urinate. Take note if you need to urinate more often than usual, if your urine leaks, if it becomes more difficult for you to begin urinating, or if you feel you’re not able to completely empty your bladder. These changes may be early signs of different urinary tract problems. Talk with your health care professional if you notice any of these signs. You may be able to prevent a condition from becoming more severe if you get help early on.
- Do pelvic floor muscle exercises. Pelvic floor exercises, also called Kegel exercises, can keep your pelvic floor muscles strong and maintain healthy bladder and bowel function. Both men and women can benefit from pelvic floor muscle exercises.
Bladder Infection
A bladder infection is an illness caused by bacteria. Bladder infections are the most common type of urinary tract infection (UTI) 165. A urinary tract infection (UTI) is an infection in any part of your urinary system — your kidneys, ureters, bladder and urethra. Most infections involve the lower urinary tract — the bladder and the urethra. Bladder infections are common, especially among women. Research suggests that at least 40 to 60 percent of women develop a UTI during their lifetime, and most of these infections are bladder infections. One in 4 women is likely to have a repeat infection 165.
Your body has ways to defend against infection in the urinary tract. For example, urine normally flows from your kidneys, through the ureters to your bladder. Bacteria that enter your urinary tract are flushed out when you urinate. This one-way flow of urine helps to keep bacteria from infecting your urinary tract.
Women tend to get urinary tract infections more often than men because bacteria can reach the bladder more easily in women. The urethra (the opening to your urinary tract) is shorter in women than in men, so bacteria have a shorter distance to travel. The urethra is located near the rectum in women. Bacteria from the rectum can easily travel up the urethra and cause infections. Bacteria from the rectum is more likely to get into the urethra if you wipe from back to front (instead of front to back) after a bowel movement. Be sure to teach children how to wipe correctly.
Having sex may also cause urinary tract infections in women because bacteria can be pushed into the urethra. Using a diaphragm can lead to infections because diaphragms push against the urethra and make it harder to completely empty your bladder. The urine that stays in the bladder is more likely to grow bacteria and cause infections.
Frequent urinary tract infections may be caused by changes in the bacteria in the vagina. Antibacterial vaginal douches, spermicides, and certain oral antibiotics may cause changes in vaginal bacteria. Avoid using these items, if possible. Menopause can also cause changes in vaginal bacteria that increase your risk for urinary tract infection. Taking estrogen usually corrects this problem but may not be for everyone.
Sometimes bacteria can grow in your urinary tract but you won’t have any symptoms. This is called asymptomatic bacteriuria. Your doctor can test to find out if you have this. Asymptomatic bacteriuria should be treated in pregnant women, but does not need to be treated in most other women.
Sometimes a urinary tract infection (UTI) can damage the kidneys, therefore, it’s important to seek treatment right away if you think you have a UTI.
Possible signs of a urinary tract infection include the following:
- A burning sensation or pain when you urinate
- Feeling like you need to urinate more often than usual
- Feeling the urge to urinate but not being able to
- Leaking a little urine
- Cloudy, dark, smelly or bloody urine
There are many lifestyle choices that can help you prevent urinary tract infections (UTIs). These are some of the things you can do to protect yourself from them:
- Drink plenty of water to flush out bacteria. For some people, drinking cranberry juice may also help prevent urinary tract infections. However, if you’re taking warfarin, check with your doctor before using cranberry juice to prevent urinary tract infections. Your doctor may need to adjust your warfarin dose or you may need to have more frequent blood tests.
- Don’t hold your urine. Urinate when you feel like you need to. Some children don’t go to the bathroom often enough. If your child does this, teach him or her to go to the bathroom several times each day.
- Wipe from front to back after bowel movements.
- Urinate after having sex to help wash away bacteria.
- Use enough lubrication during sex. Try using a small amount of lubricant (such as K-Y Jelly) before sex if you’re a little dry.
- If you get urinary tract infections often, you may want to avoid using a diaphragm as a birth control method. Ask your doctor about other birth control choices.
Urinary tract infections (UTIs) are treated with antibiotics prescribed by your doctor. Currently, a second or third generation cephalosporin and amoxicillin-clavulanate are drugs of choice in the treatment of acute uncomplicated UTI 166. If you are a healthy adult woman who is not pregnant, a few days of antibiotic pills will usually cure your urinary tract infection. If you are pregnant, your doctor will prescribe a medicine that is safe for you and the baby. Usually, symptoms of the infection go away 1 to 2 days after you start taking the medicine. It’s important that you follow your doctor’s instructions for taking the medicine, even if you start to feel better. Skipping pills could make the treatment less effective.
Your doctor may also suggest a medicine to numb your urinary tract and make you feel better while the antibiotic starts to work. The medicine makes your urine turn bright orange, so don’t be alarmed by the color when you urinate.
If the antibiotic treatment isn’t working, your symptoms will stay the same, get worse, or you will develop new symptoms. Call your doctor if you have a fever (higher than 100.5 F degrees), chills, lower stomach pain, nausea, and vomiting. You should also call your doctor if, after taking antibiotic for 3 days, you still have a burning feeling when you urinate. If you are pregnant, you should also call your doctor if you have any contractions.
A meta-analysis evaluating the efficacy of Lactobacillus found that probiotic strains of Lactobacillus are safe and effective in preventing recurrent urinary tract infections in adult women. However, more randomized clinical trials are required before providing a definitive recommendation since only 127 patients contributed data to this meta-analysis 167.
A 2015 Cochrane Review evaluated the potential therapeutic advantage of probiotics in a meta-analysis to prevent urinary tract infections in susceptible patients in terms of morbidity and mortality compared to a placebo and other prophylactic interventions 168. The meta-analysis showed no significant reduction in the risk of recurrent symptomatic bacterial UTIs between patients treated with probiotics and a placebo 168. Furthermore, risk reduction of recurrent symptomatic bacterial urinary tract infections was insignificant between probiotic and antibiotic-treated patients (1 study, 223 participants) 168. However, a benefit cannot be excluded as the data were few and derived from small studies with poor methodological reporting.
In a recent meta-analysis, three double-blind randomized clinical trials evaluated the effect of oral administration of a mixture of four Lactobacillus strains (L. crispatus LbV 88 (DSM 22566), L. gasseri LbV 150N (DSM 22583), L. jensenii LbV 116 (DSM 22567), and L. rhamnosus LbV96 (DSM 22560) on vaginal dysbiosis. Selected clinical trials included 60 male-to-female transsexual women with neovagina, 36 women with bacterial vaginosis, and 22 postmenopausal breast cancer patients receiving chemotherapy. The meta-analysis showed that oral intake of a probiotic product containing Lactobacillus strains either as yoghurt or in capsule form may improve the microbial pattern in different forms of vaginal dysbiosis 169.
Best menopause probiotic
Menopause is when your monthly period stops permanently. Menopause is a natural biological process of a woman’s life. Menopause is sometimes called “the change of life.” Menopause does not happen all at once. As your body transitions to menopause over several years, you may have menopause symptoms and irregular periods. Most women become menopausal between 45 and 60 years of age — this marks the end of the reproductive stage of their life. The average age for menopause in the United States is 51 170. You have reached menopause when you have gone 12 months without having your period (including spotting). Menopause occurs naturally when a woman’s ovaries no longer have any eggs to release, and its symptoms are caused by a drop in the levels of the hormone estrogen. Some women experience early menopause due to health conditions, such as primary ovarian insufficiency (where ovaries stop working normally). Menopause can also occur after surgery to remove your ovaries or uterus, or cancer treatment. In the lead-up to natural menopause, hormone levels can swing from high to low as the body transitions (perimenopause). After menopause your ovaries make very low little of the hormones estrogen and progesterone. Low levels of estrogen and progesterone can raise your risk for certain health problems. Hormonal and metabolic changes in women undergoing menopause are also associated with increased body weight and visceral fat accumulation, which results in the prevalence of high abdominal obesity.
After menopause, your risk of certain medical conditions increases. Examples include:
- Heart and blood vessel (cardiovascular) disease. Before age 55, women have a lower risk of heart disease than men. Estrogen helps keep your blood vessels relaxed and open and helps your body maintain a healthy balance of good and bad cholesterol. Without estrogen, cholesterol may start building up on artery walls leading to the heart. Heart disease is the leading cause of death in women as well as in men. By age 70, women have about the same risk for heart disease as men of the same age. So it’s important to get regular exercise, eat a healthy diet and maintain a normal weight. Ask your doctor for advice on how to protect your heart, such as how to reduce your cholesterol or blood pressure if it’s too high.
- Stroke. Your risk for stroke doubles every decade after age 55 171. The lower levels of estrogen in your body may play a role in cholesterol build-up on artery walls leading to the brain.
- Osteoporosis. Having less estrogen after menopause causes you to lose bone mass much more quickly than you did before, which puts you at risk for osteoporosis. Osteoporosis causes bones to become brittle and weak, leading to an increased risk of fractures. During the first few years after menopause, you may lose bone density at a rapid rate, increasing your risk of osteoporosis. Postmenopausal women with osteoporosis are especially susceptible to fractures of their spine, hips and wrists. A recent large study found that women who have severe hot flashes and night sweats during the years around menopause usually have more bone loss and are at higher risk for hip fractures than women who do not have severe symptoms 172.
- Lead poisoning. Lead that you are exposed to over your lifetime gets stored in your bones. Because bone begins to break down much more quickly after menopause, that lead is more likely to be released into the blood. Older women can have blood lead levels 30% higher than before they reached menopause. This lead increases your risk for high blood pressure and atherosclerosis (sometimes called hardening of the arteries). This lead in your blood can also cause your kidneys to not work as well. It can also cause symptoms similar to dementia, affecting your memory and ability to think 173.
- Urinary incontinence. As the tissues of your vagina and urethra lose elasticity, you may experience frequent, sudden, strong urges to urinate, followed by an involuntary loss of urine (urge incontinence), or the loss of urine with coughing, laughing or lifting (stress incontinence). Lower estrogen levels may weaken the urethra. About half of postmenopausal women have trouble holding in their urine 174. You may have urinary tract infections more often. Strengthening pelvic floor muscles with Kegel exercises and using a topical vaginal estrogen may help relieve symptoms of incontinence. Hormone therapy may also be an effective treatment option for menopausal urinary tract and vaginal changes that can result in urinary incontinence.
- Sexual function. Vaginal dryness from decreased moisture production and loss of elasticity can cause discomfort and slight bleeding during sexual intercourse. Also, decreased sensation may reduce your desire for sexual activity (libido). Water-based vaginal moisturizers and lubricants may help. If a vaginal lubricant isn’t enough, many women benefit from the use of local vaginal estrogen treatment, available as a vaginal cream, tablet or ring.
- Weight gain. Many women gain weight during the menopausal transition and after menopause because metabolism slows. You may need to eat less and exercise more, just to maintain your current weight.
- Oral issues. Dry mouth and an increased risk for cavities are more common after menopause.
Probiotics promote the digestion of food, produce vitamins 175, or probiotic bacteria may protect from intestinal infections. The food sources for probiotics are yogurt and other fermented foods. The multi-strain probiotics also improve insulin resistance, endothelial dysfunction, and iron uptake 176.
Hormonal change is among the major physiological changes associated with menopause. Estrogen is the primary female sex hormone that dictates the secondary sex characteristics and affects the development and functioning of the female reproductive system 170. All estrogens are C18 steroids 177. In addition to estrogen’s indispensable role in the development of female reproductive tissues and organs—such as breasts, vagina, and uterus—estrogen is also involved in maintaining the function of these tissues and organs during puberty, adulthood, and pregnancy. Estradiol (E2) is almost always present in the body of women of reproductive age, whereas estriol (E3)—which is produced by the placenta—is primarily abundant during pregnancy and plays an important role in maintaining early-stage pregnancy 177. During pregnancy, the estriol (E3) levels increase up to 1000-fold, while the estrone and estradiol (E2) levels increase up to 100-fold. Thus, estriol (E3) can be measured in urine. Throughout the follicular phase of the menstrual cycle, the ovarian thecal cells produce androstenedione, which functions as a metabolic precursor to estrone and testosterone in the ovaries and peripheral tissues 178.
During a woman’s fertile life, the average level of total estrogen is 100–250 pg/mL 170. However, the concentration of estradiol (E2) in circulation declines up to 10 pg/mL postmenopause 179. This hormonal menopause is associated with menopausal syndromes, such as changes to the menstrual cycle, disturbances in sleep/mood, emotional changes, vasomotor symptoms (including hot flashes and night sweats), urogenital atrophy, muscle and joint aches, osteopenia and osteoporosis, psychiatric disorders, sexual dysfunction, skin lesions, cardiovascular diseases, cancer, metabolic disorders, and obesity 180. Women are at a higher risk of developing cardiovascular diseases after menopause due to estrogen deficiency and dysregulated lipid metabolism 181. Estrogens, especially estradiol (E2), exert a protective role in the cardiovascular system and are produced primarily in the ovaries via a process that uses low-density lipoprotein (LDL or “bad”) cholesterol (LDL-C) as a substrate. However, circulatory LDL-C cannot be utilized to synthesize estrogen during menopause, thereby resulting in decreased estrogen production. Therefore, menopause is associated with increased blood LDL-C (“bad” cholesterol) levels and enhanced cardiovascular disease risk 182.
Each woman experiences menopause differently. Many feel only minor discomfort, while others have more severe symptoms. Menopause symptoms are usually temporary, but sometimes last for several years.
Symptoms of menopause may begin suddenly and be very noticeable, or they may be very mild at first. Symptoms may happen most of the time once they begin, or they may happen only once in a while. Some women notice changes in many areas. Some menopausal symptoms, such as moodiness, are similar to symptoms of premenstrual syndrome (PMS). Others may be new to you. For example:
- Your menstrual periods may not come as regularly as before. They also might last longer or be shorter. You might skip some months. Periods might stop for a few months and then start up again.
- Your periods might be heavier or lighter than before.
- You might have hot flashes and problems sleeping.
- You might experience mood swings or be irritable.
- You might experience vaginal dryness. Sex may be uncomfortable or painful.
- You may have less interest in sex. It may take longer for you to get aroused.
Other possible changes are not as noticeable. For example, you might begin to lose bone density because you have less estrogen. This can lead to osteoporosis, a condition that causes bones to become weak and break easily. Changing estrogen levels can also raise cholesterol levels and increase your risk for heart disease and stroke.
Talk to your doctor about possible treatment for your menopause symptoms if they bother you.
There isn’t a specific test for menopause. Your doctor will help you determine if you are menopausal based on how frequent your periods are and what symptoms you are experiencing. Menopause is confirmed 12 months after your last period. Blood tests are unlikely to accurately predict menopause. But under certain circumstances, your doctor may recommend blood tests to check your level of:
- Follicle-stimulating hormone (FSH) and estrogen (estradiol), because your FSH levels increase and estradiol levels decrease as menopause occurs
- Thyroid-stimulating hormone (TSH), because an underactive thyroid (hypothyroidism) can cause symptoms similar to those of menopause
Over-the-counter home tests to check FSH levels in your urine are available. The tests could tell you whether you have elevated FSH levels and might be in perimenopause or menopause. But, since FSH levels rise and fall during the course of your menstrual cycle, home FSH tests can’t really tell you whether or not you’re definitely in a stage of menopause.
Management and treatment of menopausal symptoms depend on each individual woman, stage of life, relationships and general level of health and wellbeing. Healthy living, natural and complementary therapies, menopause hormone therapy (MHT) formerly called hormone replacement therapy (HRT) and some prescription medications can help relieve menopausal symptoms.
Always seek medical advice if you have bleeding from your vagina after menopause.
Seek medical advice if you are concerned about irregular cycles, heavy or abnormal bleeding, or symptoms that interfere with your daily life. Your doctor may also suggest other health checks such as a mammogram, pelvic examination or cervical screening.
Menopause treatment
Many women do not need treatment for their menopause symptoms. You may find that your symptoms go away by themselves. Or you may not find the symptoms uncomfortable. If you are bothered by your symptoms, talk to your doctor about ways to relieve them. You can work together to find a treatment that is right for you. Some women find that changing their eating habits and getting more physical activity can help. Others may need medicine to help relieve their symptoms.
Treatments may include:
- Hormone therapy also known as menopausal hormone therapy (MHT) or hormone replacement therapy (HRT). Menopausal hormone therapy involves replacing your hormones (estrogen and progesterone, and sometimes testosterone) to relieve menopausal symptoms. Estrogen therapy is the most effective treatment option for relieving menopausal hot flashes. Depending on your personal and family medical history, your doctor may recommend estrogen in the lowest dose and the shortest time frame needed to provide symptom relief for you. The FDA recommends that women take estrogen-only or estrogen plus progesterone menopausal hormone therapy at the lowest dose that works for the shortest time needed. If you still have your uterus, you’ll need progestin in addition to estrogen. Estrogen also helps prevent bone loss. Long-term use of hormone therapy may have some cardiovascular and breast cancer risks, but starting hormones around the time of menopause has shown benefits for some women. Talk to your doctor about the benefits and risks of hormone therapy and whether it’s a safe choice for you. The most recent and comprehensive reviews of menopausal hormone therapy show that many healthy women can safely use it for years to manage menopausal symptoms, but it’s important to first check with your doctor to see if menopausal hormone therapy is right for you. If you opt to start menopausal hormone therapy, take the lowest effective dose for only as long as you need to, and review with your doctor regularly whether to continue treatment.
- Research shows that 183:
- Menopausal hormone therapy may be an option for women up to age 59, but usually only within 10 years of menopause. Younger women and those closer to their final menstrual period are less likely to have the harmful side effects from menopausal hormone therapy.
- Menopausal hormone therapy reduces menopause symptoms, such as hot flashes, sleep problems, mood changes, and vaginal dryness.
- Hot flashes usually require higher doses of estrogen therapy that affect the whole body.
- Women with vaginal dryness or discomfort during sex may find relief with low doses of topical vaginal estrogen.
- Estrogen alone and estrogen plus progesterone raise the risk of stroke and blood clots in the legs and lungs. The risks are rare in women between 50 and 59.
- Menopausal hormone therapy is not appropriate if you have a history of oestrogen-dependent cancer, such as breast or uterine cancer.
- Other conditions that rule out menopausal hormone therapy include:
- undiagnosed vaginal bleeding
- untreated thickening of the uterine lining
- unmanaged high blood pressure
- current thrombosis (such as deep vein thrombosis, or DVT), or conditions that increase your risk of blood clots
- coronary heart disease, stroke or dementia
- Research shows that 183:
- Vaginal estrogen. To relieve vaginal dryness, estrogen can be administered directly to the vagina using a vaginal cream, tablet or ring. This treatment releases just a small amount of estrogen, which is absorbed by the vaginal tissues. It can help relieve vaginal dryness, discomfort with intercourse and some urinary symptoms.
- Low-dose antidepressants. Certain antidepressants related to the class of drugs called selective serotonin reuptake inhibitors (SSRIs) may decrease menopausal hot flashes. A low-dose antidepressant for management of hot flashes may be useful for women who can’t take estrogen for health reasons or for women who need an antidepressant for a mood disorder.
- Gabapentin (Gralise, Horizant, Neurontin). Gabapentin is approved to treat seizures, but it has also been shown to help reduce hot flashes. This drug is useful in women who can’t use estrogen therapy and in those who also have nighttime hot flashes.
- Clonidine (Catapres, Kapvay). Clonidine, a pill or patch typically used to treat high blood pressure, might provide some relief from hot flashes.
- Medications to prevent or treat osteoporosis. Depending on individual needs, doctors may recommend medication to prevent or treat osteoporosis. Several medications are available that help reduce bone loss and risk of fractures. Your doctor might prescribe vitamin D and calcium supplements to help strengthen bones.
Before deciding on any form of treatment, talk with your doctor about your options and the risks and benefits involved with each. Review your options yearly, as your needs and treatment options may change.
Lifestyle and home remedies
- Cool hot flashes. Dress in layers, have a cold glass of water or go somewhere cooler. Try to pinpoint what triggers your hot flashes. For many women, triggers may include hot beverages, caffeine, spicy foods, alcohol, stress, hot weather and even a warm room.
- Decrease vaginal discomfort. Try an over-the-counter, water-based vaginal lubricant (Astroglide, K-Y jelly, Sliquid, others) or a silicone-based lubricant or moisturizer (Replens, K-Y Liquibeads, Sliquid, others). You might consider choosing a product that doesn’t contain glycerin, which can cause burning or irritation if you’re sensitive to that chemical. Staying sexually active also helps with vaginal discomfort by increasing blood flow to the vagina.
- Get enough sleep. Avoid caffeine, which can make it hard to get to sleep, and avoid drinking too much alcohol, which can interrupt sleep. Exercise during the day, although not right before bedtime. If hot flashes disturb your sleep, you may need to find a way to manage them before you can get adequate rest.
- Practice relaxation techniques. Techniques such as deep breathing, paced breathing, guided imagery, massage and progressive muscle relaxation may help with menopausal symptoms. You can find a number of books and online offerings that show different relaxation exercises.
- Strengthen your pelvic floor. Pelvic floor muscle exercises, called Kegel exercises, can improve some forms of urinary incontinence.
- Eat a balanced diet. Include a variety of fruits, vegetables and whole grains. Limit saturated fats, oils and sugars. Ask your provider if you need calcium or vitamin D supplements to help meet daily requirements.
- Don’t smoke. Smoking increases your risk of heart disease, stroke, osteoporosis, cancer and a range of other health problems. It may also increase hot flashes and bring on earlier menopause.
- Exercise regularly. Get regular physical activity or exercise on most days to help protect against heart disease, diabetes, osteoporosis and other conditions associated with aging.
Alternative medicine
Some complementary and alternative treatments that have been or are being studied include:
- Plant estrogens (phytoestrogens). These estrogens occur naturally in certain foods. There are two main types of phytoestrogens — isoflavones and lignans. Isoflavones are found in soybeans, lentils, chickpeas and other legumes. Lignans occur in flaxseed, whole grains, and some fruits and vegetables. Whether the estrogens in these foods can relieve hot flashes and other menopausal symptoms remains to be proved, but most studies have found them ineffective. Isoflavones have some weak estrogen-like effects, so if you’ve had breast cancer, talk to your doctor before supplementing your diet with isoflavone pills. The herb sage is thought to contain compounds with estrogen-like effects, and there’s good evidence that it can effectively manage menopause symptoms. The herb and its oils should be avoided in people who have an allergy to sage, and in pregnant or breast-feeding women. Use carefully in people with high blood pressure or epilepsy.
- Bioidentical hormones. These hormones come from plant sources. The term “bioidentical” implies the hormones in the product are chemically identical to those your body produces. There are some commercially available bioidentical hormones approved by the Food and Drug Administration (FDA). But many preparations are compounded — mixed in a pharmacy according to a doctor’s prescription — and aren’t regulated by the FDA, so quality and risks could vary. There’s no scientific evidence that bioidentical hormones work any better than traditional hormone therapy in easing menopause symptoms. There’s also no evidence that they’re any less risky than traditional hormone therapy.
- Black cohosh. Black cohosh has been popular among many women with menopausal symptoms, such as hot flashes. The underground stems and root of black cohosh are used fresh or dried to make tea, capsules, pills, or liquid extracts. But there’s little evidence that black cohosh is effective, and the supplement can be harmful to the liver and may be unsafe for women with a history of breast cancer.
- Yoga. There’s no evidence to support the practice of yoga in reducing menopausal symptoms. But balance exercises such as yoga or tai chi can improve strength and coordination and may help prevent falls that could lead to broken bones. Check with your doctor before starting balance exercises. Consider taking a class to learn how to perform postures and proper breathing techniques.
- Acupuncture. Acupuncture may have some temporary benefit in helping to reduce hot flashes, but research hasn’t shown significant or consistent improvements. More research is needed.
- Hypnosis. Hypnotherapy may decrease the incidence of hot flashes by 74% for some menopausal women, according to research from the National Center for Complementary and Integrative Health at the U.S. National Institutes of Health 184. Hypnotherapy also helped improve sleep and decreased interference in daily life, according to the study.
You may have heard of or tried other dietary supplements, such as red clover, kava, dong quai, DHEA, evening primrose oil and wild yam (natural progesterone cream). Scientific evidence on effectiveness is lacking, and some of these products may be harmful.
Talk with your doctor before taking any herbal or dietary supplements for menopausal symptoms. The FDA does not regulate herbal products, and some can be dangerous or interact with other medications you take, putting your health at risk.
Probiotics for menopause belly and weight loss
To date, there is no conclusive evidence for the ability of probiotics to control body fat mass in humans 185. Despite a fair amount of promising clinical findings 186, 187, 188, 189, randomized controlled trials demonstrating beneficial probiotic effects in the primary statistical analysis of a well-powered study conducted according to Good Clinical Practice (GCP) are lacking. Only few studies on prebiotics have shown effects on weight management 190, 191. Furthermore, no clinical trials have explored probiotics and prebiotics alone and in combination to assess their potential synergistic benefits for metabolic health. Regarding the effectiveness of probiotics in weight control, the 2 meta-analysis, both published in 2015, show conflicting results: one shows that the intake of probiotics results in a significant weight loss and of the body Mass Index (BMI) reporting that the weight loss is more consistent if the assumption is performed for a time greater than 8 weeks and when taken multiple strains 192. The other meta-analysis instead shows that there is no efficiency in terms of weight and BMI reduction 193. In one randomized controlled trial 46 of 225 adults with overweight and obesity, a combination of Bifidobacterium animalis subsp. lactis 420 (B420) and polydextrose (12 g per day) resulted in a relative reduction in body fat mass of 4.5%, whereas the individual treatments had no effect 185. Changes in fat mass were most pronounced in the abdominal region, and were reflected by similar changes in waist circumference. Bifidobacterium animalis subsp. lactis 420 (B420) and polydextrose + B420 also significantly reduced food intake compared to placebo, whereas polydextrose alone had no effect on the measured outcomes 185. Based on the findings of a 2020 systematic review and meta-analysis of clinical trials, modulation of gut microbiota composition through probiotic supplementation might have modest effects on body weight and waist circumference 194.
References- National Center for Complementary and Integrative Health. Probiotics. https://nccih.nih.gov/health/probiotics
- Hill, C., Guarner, F., Reid, G. et al. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol 11, 506–514 (2014). https://doi.org/10.1038
- Clin Perinatol. 2013 Mar; 40(1): 11–25. Published online 2013 Jan 17. doi: 10.1016/j.clp.2012.12.002. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3575601/
- The National Institute of Health, Medline Plus. The Basics of Probiotics. https://medlineplus.gov/magazine/issues/winter16/articles/winter16pg22.html
- Probiotics. https://ods.od.nih.gov/factsheets/Probiotics-HealthProfessional
- Gibson GR, Hutkins R, Sanders ME, Prescott SL, Reimer RA, Salminen SJ, Scott K, Stanton C, Swanson KS, Cani PD, Verbeke K, Reid G. Expert consensus document: The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol. 2017 Aug;14(8):491-502. doi: 10.1038/nrgastro.2017.75
- Probiotics and prebiotics. https://www.worldgastroenterology.org/guidelines/global-guidelines/probiotics-and-prebiotics/probiotics-and-prebiotics-english
- Hempel S, et al. Safety of probiotics used to reduce risk and prevent or treat disease. Evid Rep Technol Assess (Full Rep). 2011;(200):1–645.
- Redman MG, Ward EJ, Phillips RS. The efficacy and safety of probiotics in people with cancer: a systematic review. Ann Oncol. 2014;25(10):1919–1929.
- World Gastroenterology Organisation Global Guidelines. Probiotics and prebiotics. 2017. https://www.worldgastroenterology.org/UserFiles/file/guidelines/probiotics-and-prebiotics-english-2017.pdf
- Harvard University. Harvard Health Publication. The Benefits of Probiotics Bacteria. http://www.health.harvard.edu/staying-healthy/the-benefits-of-probiotics
- Hogan DE, Ivanina EA, Robbins DH. Probiotics: a review for clinical use. Gastroenterology & Endoscopy News 2018:1-7.
- Szajewska H, Guarino A, Hojsak I, Indrio F, Kolacek S, Shamir R, Vandenplas Y, Weizman Z; European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. Use of probiotics for management of acute gastroenteritis: a position paper by the ESPGHAN Working Group for Probiotics and Prebiotics. J Pediatr Gastroenterol Nutr. 2014 Apr;58(4):531-9. doi: 10.1097/MPG.0000000000000320. Erratum in: J Pediatr Gastroenterol Nutr. 2016 Jan;62(1):188.
- Draft Guidance for Industry: Policy Regarding Quantitative Labeling of Dietary Supplements Containing Live Microbials. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/draft-guidance-industry-policy-regarding-quantitative-labeling-dietary-supplements-containing-live
- Logan AC, Jacka FN, Prescott SL. Immune-microbiota interactions: dysbiosis as a global health issue. Curr Allergy Asthma Rep. 2016;16(2):13.
- Jones RJ, et al. Isolation of lactic acid bacteria with inhibitory activity against pathogens and spoilage organisms associated with fresh meat. Food Microbiol. 2008;25(2):228-234.
- Paredes-Paredes M, Flores-Figueroa J, Dupont HL. Advances in the treatment of travelers’ diarrhea. Curr Gastroenterol Rep. 2011;13(5):402-407.
- Wullt M, et al. Lactobacillus plantarum 299v enhances the concentrations of fecal short-chain fatty acids in patients with recurrent Clostridium difficile–associated diarrhea. Dig Dis Sci . 2007;52(9):2082-2086.
- Dickinson B, Surawicz CM. Infectious diarrhea: an overview. Curr Gastroenterol Rep. 2014;16(8):399.
- Gedek BR. Adherence of Escherichia coli serogroup O 157 and the Salmonella typhimurium mutant DT 104 to the surface of Saccharomyces boulardii. Mycoses . 1999;42(4):261-264.
- Kairys N, Garg M. Gardnerella. [Updated 2021 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459350
- Gardnerella vaginalis as a Cause of Bacterial Vaginosis: Appraisal of the Evidence From in vivo Models. Front. Cell. Infect. Microbiol., 24 April 2020. https://doi.org/10.3389/fcimb.2020.00168
- Ceccarani, C., Foschi, C., Parolin, C., D’Antuono, A., Gaspari, V., Consolandi, C., Laghi, L., Camboni, T., Vitali, B., Severgnini, M., & Marangoni, A. (2019). Diversity of vaginal microbiome and metabolome during genital infections. Scientific reports, 9(1), 14095. https://doi.org/10.1038/s41598-019-50410-x
- Srinivasan, S., Hoffman, N. G., Morgan, M. T., Matsen, F. A., Fiedler, T. L., Hall, R. W., et al. (2012). Bacterial communities in women with bacterial vaginosis: high resolution phylogenetic analyses reveal relationships of microbiota to clinical criteria. PLoS ONE 7:e37818. doi: 10.1371/journal.pone.0037818
- Vallor A.C., Antonio M.A., Hawes S.E., Hillier S.L. Factors associated with acquisition of, or persistent colonization by, vaginal lactobacilli: Role of hydrogen peroxide production. J. Infect. Dis. 2001;184:1431–1436. doi: 10.1086/324445
- Ma, L., Su, J., Su, Y., Sun, W., & Zeng, Z. (2017). Probiotics administered intravaginally as a complementary therapy combined with antibiotics for the treatment of bacterial vaginosis: a systematic review protocol. BMJ open, 7(10), e019301. https://doi.org/10.1136/bmjopen-2017-019301
- Hartmann AA. Gardnerella vaginalis-Infektion. Klinik, Diagnostik und Therapie [Gardnerella vaginalis infection. Clinical aspects, diagnosis and therapy]. Urologe A. 1987 Sep;26(5):252-5. German.
- Van De Wijgert, J. H. H. M. (2017). The vaginal microbiome and sexually transmitted infections are interlinked: consequences for treatment and prevention. PLoS Med. 14:E1002478. doi: 10.1371/journal.pmed.1002478
- Hillebrand, L., Harmanli, O. H., Whiteman, V., and Khandelwal, M. (2002). Urinary tract infections in pregnant women with bacterial vaginosis. Am. J. Obstet. Gynecol. 186, 916–917. doi: 10.1067/mob.2002.123987
- Watts, D. H., Krohn, M. A., Hillier, S. L., and Eschenbach, D. A. (1990). Bacterial vaginosis as a risk factor for post-cesarean endometritis. Obstet. Gynecol. 75, 52–58.
- Spandorfer, S., Neuer, A., Paulo, G., Rosenwaks, Z., and Witkin, S. (2001). Relationship of abnormal vaginal flora, proinflammatory cytokines and idiopathic infertility in women undergoing IVF. J. Reprod. Med. 46, 806–10.
- Ralph, S. G., Rutherford, A. J., and Wilson, J. D. (1999). Influence of bacterial vaginosis on conception and miscarriage in the first trimester: cohort study. BMJ 319, 220–223. doi: 10.1136/bmj.319.7204.220
- Svare, J. A., Schmidt, H., Hansen, B. B., and Lose, G. (2006). Bacterial vaginosis in a cohort of Danish pregnant women: prevalence and relationship with preterm delivery, low birthweight and perinatal infections. BJOG 113, 1419–1425. doi: 10.1111/j.1471-0528.2006.01087.x
- Ádám, A., Pál, Z., Terhes, G., Szucs, M., Gabay, I. D., and Urbán, E. (2018). Culture- and PCR-based detection of BV associated microbiological profile of the removed IUDs and correlation with the time period of IUD in place and the presence of the symptoms of genital tract infection. Ann. Clin. Microbiol. Antimicrob 17:40. doi: 10.1186/s12941-018-0293-6
- Silver, H. M., Sperling, R. S., St Clair, P. J., and Gibbs, R. S. (1989). Evidence relating bacterial vaginosis to intraamniotic infection. Am. J. Obstet. Gynecol. 161, 808–12. doi: 10.1016/0002-9378(89)90406-7
- Brusselaers, N., Shrestha, S., van de Wijgert, J., and Verstraelen, H. (2019). Vaginal dysbiosis and the risk of human papillomavirus and cervical cancer: systematic review and meta-analysis. Am. J. Obstet. Gynecol. 221, 9–18.e8. doi: 10.1016/j.ajog.2018.12.011
- Kenyon CR, Osbak K. Recent progress in understanding the epidemiology of bacterial vaginosis. Curr Opin Obstet Gynecol. 2014 Dec;26(6):448-54. doi: 10.1097/GCO.0000000000000112
- Baruah, F. K., Sharma, A., Das, C., Hazarika, N. K., & Hussain, J. H. (2014). Role of Gardnerella vaginalis as an etiological agent of bacterial vaginosis. Iranian journal of microbiology, 6(6), 409–414. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4411427
- Hartmann AA, Elsner P. Gardnerella vaginalis-Infektion–eine weitere STD [Gardnerella vaginalis infection–another sexually transmitted disease]. Hautarzt. 1984 Oct;35(10):512-6. German.
- Tan H, Fu Y, Yang C, Ma J. Effects of metronidazole combined probiotics over metronidazole alone for the treatment of bacterial vaginosis: a meta-analysis of randomized clinical trials. Arch Gynecol Obstet. 2017;295:1331–1339. doi: 10.1007/s00404-017-4366-0
- Huang H, Song L, Zhao W. Effects of probiotics for the treatment of bacterial vaginosis in adult women: a meta-analysis of randomized clinical trials. Arch Gynecol Obstet. 2014 Jun;289(6):1225-34. doi: 10.1007/s00404-013-3117-0
- Oduyebo OO, Anorlu RI, Ogunsola FT. The effects of antimicrobial therapy on bacterial vaginosis in non-pregnant women. Cochrane Database Syst Rev. 2009 Jul 8;(3):CD006055. doi: 10.1002/14651858.CD006055.pub2
- Gille C, Böer B, Marschal M, Urschitz MS, Heinecke V, Hund V, Speidel S, Tarnow I, Mylonas I, Franz A, Engel C, Poets CF. Effect of probiotics on vaginal health in pregnancy. EFFPRO, a randomized controlled trial. Am J Obstet Gynecol. 2016 Nov;215(5):608.e1-608.e7. doi: 10.1016/j.ajog.2016.06.021
- Vujic G, Jajac Knez A, Despot Stefanovic V, Kuzmic Vrbanovic V. Efficacy of orally applied probiotic capsules for bacterial vaginosis and other vaginal infections: a double-blind, randomized, placebo-controlled study. Eur J Obstet Gynecol Reprod Biol. 2013 May;168(1):75-9. doi: 10.1016/j.ejogrb.2012.12.031
- Laue C, Papazova E, Liesegang A, Pannenbeckers A, Arendarski P, Linnerth B, Domig KJ, Kneifel W, Petricevic L, Schrezenmeir J. Effect of a yoghurt drink containing Lactobacillus strains on bacterial vaginosis in women – a double-blind, randomised, controlled clinical pilot trial. Benef Microbes. 2018 Jan 29;9(1):35-50. doi: 10.3920/BM2017.0018
- Handalishy II, Behery MA, Elkhouly M, et al. Comparative study between probiotic vaginal tampons and oral metronidazole in treatment of bacterial vaginosis. Al Azhar Assiut Med J. 2014;12(Suppl 2):185–203.
- Verdenelli, M.C., Cecchini, C., Coman, M.M. et al. Impact of Probiotic SYNBIO® Administered by Vaginal Suppositories in Promoting Vaginal Health of Apparently Healthy Women. Curr Microbiol 73, 483–490 (2016). https://doi.org/10.1007/s00284-016-1085-x
- Coste, I., Judlin, P., Lepargneur, J. P., & Bou-Antoun, S. (2012). Safety and efficacy of an intravaginal prebiotic gel in the prevention of recurrent bacterial vaginosis: a randomized double-blind study. Obstetrics and gynecology international, 2012, 147867. https://doi.org/10.1155/2012/147867
- Sherrard J, Donders G, White D, Jensen JS. European (IUSTI/WHO) guideline on the management of vaginal discharge. Int J STD AIDS. 2011;22:421–429. doi: 10.1258/ijsa.2011.011012
- Melvin L, Craic J, Abbott M, et al. Management of vaginal discharge in non-genitourinary medicine settings. Faculty of Sexual & repro- ductive Healthcare Clinical Guidance. 2012:1–28.
- Mendling W. Guideline: vulvovaginal candidosis (AWMF 015/072), S2k (excluding chronic mucocutaneous candidosis) Mycoses. 2015;58:1–15. doi: 10.1111/myc.12292
- Van Schalkwyk J, Yudin MH, Allen V, et al. Vulvovaginitis: screening for and management of trichomoniasis, vulvovaginal candidiasis, and bacterial vaginosis. J Obstet Gynaecol Can. 2015;37:266–274. doi: 10.1016/S1701-2163(15)30316-9
- Centers for Disease Control and Prevention. 2015 Sexually Transmitted Diseases Treatment Guidelines. https://www.cdc.gov/std/treatment-guidelines/STI-Guidelines-2021.pdf
- CDC’s Sexually Transmitted Infections (STI) Treatment Guidelines, 2021. MMWR July 23, 2021; Vol. 70; No. 4. https://www.cdc.gov/std/treatment-guidelines/STI-Guidelines-2021.pdf
- Bacterial Vaginosis – CDC Fact Sheet. https://www.cdc.gov/std/bv/STDFact-Bacterial-Vaginosis.htm
- Sobel JD. Vulvovaginal candidosis. Lancet. 2007 Jun 9;369(9577):1961-71. doi: 10.1016/S0140-6736(07)60917-9
- Hainer BL, Gibson MV. Vaginitis. Am Fam Physician. 2011;83(7):807–815.
- Dan M, Leshem Y, Yeshaya A. Performance of a rapid yeast test in detecting Candida spp. in the vagina. Diagn Microbiol Infect Dis. 2010;67(1):52–55.
- Pappas, P. G., Kauffman, C. A., Andes, D. R., Clancy, C. J., Marr, K. A., Ostrosky-Zeichner, L., Reboli, A. C., Schuster, M. G., Vazquez, J. A., Walsh, T. J., Zaoutis, T. E., & Sobel, J. D. (2016). Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America, 62(4), e1–e50. https://doi.org/10.1093/cid/civ933
- Vulvovaginal Candidiasis. 2015 Sexually Transmitted Diseases Treatment Guidelines. https://www.cdc.gov/std/tg2015/candidiasis.htm
- Xie, H. Y., Feng, D., Wei, D. M., Mei, L., Chen, H., Wang, X., & Fang, F. (2017). Probiotics for vulvovaginal candidiasis in non-pregnant women. The Cochrane database of systematic reviews, 11(11), CD010496. https://doi.org/10.1002/14651858.CD010496.pub2
- Probiotics to Augment Antifungal Treatment of Vulvovaginal Candidiasis. Am Fam Physician. 2020 Apr 1;101(7):432-433. https://www.aafp.org/afp/2020/0401/p432.html
- Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015 [published correction appears in MMWR Recomm Rep. 2015;64(33):924]. MMWR Recomm Rep. 2015;64(RR-03):1–137.
- van Schalkwyk J, Yudin MH; Infectious Disease Committee. Vulvovaginitis: screening for and management of trichomoniasis, vulvovaginal candidiasis, and bacterial vaginosis. J Obstet Gynaecol Can. 2015;37(3):266–274.
- Kennedy MA, Sobel JD. Vulvovaginal candidiasis caused by non-albicans Candida species: new insights. Curr Infect Dis Rep 2010;12:465–70.
- Sobel JD, Chaim W, Nagappan V, et al. Treatment of vaginitis caused by Candida glabrata: use of topical boric acid and flucytosine. Am J Obstet Gynecol 2003;189:1297–300.
- Vazquez JA, Peng G, Sobel JD, et al. Evolution of antifungal susceptibility among Candida species isolates recovered from human immunodeficiency virus-infected women receiving fluconazole prophylaxis. Clin Infect Dis 2001;33:1069–75.
- Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America.
- The scoop on probiotics. Consum Rep Health. 2015;27(8):9.
- Kligler B, Cohrssen A. Probiotics. Am Fam Physician. 2008;78(9):1073–1078.
- Probiotics for Gastrointestinal Conditions: A Summary of the Evidence. Am Fam Physician. 2017 Aug 1;96(3):170-178. https://www.aafp.org/afp/2017/0801/p170.html
- Gou S, Yang Z, Liu T, Wu H, Wang C. Use of probiotics in the treatment of severe acute pancreatitis: a systematic review and meta-analysis of randomized controlled trials. Crit Care. 2014;18(2):R57.
- Shen J, Zuo ZX, Mao AP. Effect of probiotics on inducing remission and maintaining therapy in ulcerative colitis, Crohn’s disease, and pouchitis: meta-analysis of randomized controlled trials [published correction appears in Inflamm Bowel Dis. 2014;20(12):2526–2528]. Inflamm Bowel Dis. 2014;20(1):21–35.
- Butterworth AD, et al. Probiotics for induction of remission in Crohn’s disease. Cochrane Database Syst Rev. 2008;(3):CD006634.
- Rolfe VE, et al. Probiotics for maintenance of remission in Crohn’s disease. Cochrane Database Syst Rev. 2006;(4):CD004826.
- Doherty G, Bennett G, Patil S, Cheifetz A, Moss AC. Interventions for prevention of post-operative recurrence of Crohn’s disease. Cochrane Database Syst Rev. 2009;(4):CD006873.
- Goldenberg JZ, et al. Probiotics for the prevention of pediatric antibiotic-associated diarrhea. Cochrane Database Syst Rev. 2015;(12):CD004827.
- Goldenberg JZ, Ma SS, Saxton JD, et al. Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children. Cochrane Database Syst Rev. 2013;5(5):CD006095.
- Lu C, Sang J, He H, et al. Probiotic supplementation does not improve eradication rate of Helicobacter pylori infection compared to placebo based on standard therapy: a meta-analysis. Sci Rep. 2016;6:23522.
- Dalal R, et al. Probiotics for people with hepatic encephalopathy. Cochrane Database Syst Rev. 2017;(2):CD008716.
- Zhang Y, Li L, Guo C, et al. Effects of probiotic type, dose and treatment duration on irritable bowel syndrome diagnosed by Rome III criteria: a meta-analysis. BMC Gastroenterol. 2016;16(1):62.
- Sung V, Collett S, de Gooyer T, Hiscock H, Tang M, Wake M. Probiotics to prevent or treat excessive infant crying: systematic review and meta-analysis. JAMA Pediatr. 2013;167(12):1150–1157.
- Olsen R, Greisen G, Schrøder M, Brok J. Prophylactic probiotics for pre-term infants: a systematic review and meta-analysis of observational studies. Neonatology. 2016;109(2):105–112.
- Deshpande GC, Rao SC, Keil AD, Patole SK. Evidence-based guidelines for use of probiotics in preterm neonates. BMC Med. 2011;9:92.
- American Gastroenterological Association, Bharucha AE, Dorn SD, Lembo A, Pressman A. American Gastroenterological Association medical position statement on constipation. Gastroenterology. 2013;144(1):211–217.
- Symptoms & Causes of Constipation. https://www.niddk.nih.gov/health-information/digestive-diseases/constipation/symptoms-causes
- Rose S, ed. Constipation: A Practical Approach to Diagnosis and Treatment. New York, NY: Springer Science and Business Media; 2014.
- Ford AC, Quigley EM, Lacy BE, et al. Efficacy of prebiotics, probiotics, and synbiotics in irritable bowel syndrome and chronic idiopathic constipation: systematic review and meta-analysis. Am J Gastroenterol. 2014;109(10):1547–1561.
- Guerra PV, Lima LN, Souza TC, et al. Pediatric functional constipation treatment with Bifidobacterium-containing yogurt: a crossover, double-blind, controlled trial. World J Gastroenterol. 2011;17(34):3916–3921.
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. 8th Edition. https://health.gov/sites/default/files/2019-09/2015-2020_Dietary_Guidelines.pdf
- Scallan E, Griffin PM, Angulo FJ, Tauxe RV, Hoekstra RM. Foodborne illness acquired in the United States–unspecified agents. Emerg Infect Dis. 2011 Jan;17(1):16-22. doi: 10.3201/eid1701.091101p2
- Turgeon DK, Fritsche TR. Laboratory approaches to infectious diarrhea. Gastroenterol Clin North Am. 2001;30(3):693–707.
- Aranda-Michel J, Giannella RA. Acute diarrhea: a practical review. Am J Med. 1999;106(6):670–676.
- Jones TF, Bulens SN, Gettner S, et al. Use of stool collection kits delivered to patients can improve confirmation of etiology in foodborne disease outbreaks. Clin Infect Dis. 2004;39(10):1454–1459.
- Centers for Disease Control and Prevention. Preliminary FoodNet data on the incidence of infection with pathogens transmitted commonly through food—10 states, 2009. MMWR Morb Mortal Wkly Rep. 2010;59(14):418–422.
- Guerrant RL, Van Gilder T, Steiner TS, et al.; Infectious Diseases Society of America. Practice guidelines for the management of infectious diarrhea. Clin Infect Dis. 2001;32(3):331–351.
- Thielman NM, Guerrant RL. Clinical practice. Acute infectious diarrhea. N Engl J Med. 2004;350(1):38–47.
- Acute Diarrhea in Adults. Am Fam Physician. 2014 Feb 1;89(3):180-189. https://www.aafp.org/afp/2014/0201/p180.html
- Farthing M, Salam MA, Lindberg G, et al.; World Gastroenterology Organisation. Acute diarrhea in adults and children: a global perspective. J Clin Gastroenterol. 2013;47(1):12–20.
- Guerrant RL, Shields DS, Thorson SM, Schorling JB, Gröschel DH. Evaluation and diagnosis of acute infectious diarrhea. Am J Med. 1985; 78(6B):91–98.
- Gill CJ, Lau J, Gorbach SL, Hamer DH. Diagnostic accuracy of stool assays for inflammatory bacterial gastroenteritis in developed and resource-poor countries. Clin Infect Dis. 2003;37(3):365–375.
- Chen CC, Chang CJ, Lin TY, Lai MW, Chao HC, Kong MS. Usefulness of fecal lactoferrin in predicting and monitoring the clinical severity of infectious diarrhea. World J Gastroenterol. 2011;17(37):4218–4224.
- Choi SW, Park CH, Silva TM, Zaenker EI, Guerrant RL. To culture or not to culture: fecal lactoferrin screening for inflammatory bacterial diarrhea. J Clin Microbiol. 1996;34(4):928–932.
- Hayakawa T, Jin CX, Ko SB, Kitagawa M, Ishiguro H. Lactoferrin in gastrointestinal disease. Intern Med. 2009;48(15):1251–1254.
- Guerrant RL, Wanke CA, Barrett LJ, Schwartzman JD. A cost effective and effective approach to the diagnosis and management of acute infectious diarrhea. Bull N Y Acad Med. 1987;63(6):484–499.
- Gangarosa RE, Glass RI, Lew JF, Boring JR. Hospitalizations involving gastroenteritis in the United States, 1985: the special burden of the disease among the elderly. Am J Epidemiol. 1992;135(3):281–290.
- Talan D, Moran GJ, Newdow M, et al.; EMERGEncy ID NET Study Group. Etiology of bloody diarrhea among patients presenting to United States emergency departments: prevalence of Escherichia coli O157:H7 and other enteropathogens. Clin Infect Dis. 2001;32(4):573–580.
- Manatsathit S, Dupont HL, Farthing M, et al.; Working Party of the Program Committee of the Bangkok World Congress of Gastroenterology 2002. Guideline for the management of acute diarrhea in adults. J Gastroenterol Hepatol. 2002;17(suppl):S54–S71.
- DuPont HL. Guidelines on acute infectious diarrhea in adults. The Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1997;92(11):1962–1975.
- Bauer TM, Lalvani A, Fehrenbach J, et al. Derivation and validation of guidelines for stool cultures for enteropathogenic bacteria other than Clostridium difficile in hospitalized adults. JAMA. 2001;285(3):313–319.
- Centers for Disease Control and Prevention. Vital signs: preventing Clostridium difficile infections. MMWR Morb Mortal Wkly Rep. 2012;61(9):157–162.
- Siegel DL, Edelstein PH, Nachamkin I. Inappropriate testing for diarrheal diseases in the hospital. JAMA. 1990;263(7):979–982.
- Shen B, Khan K, Ikenberry SO, et al.; ASGE Standards of Practice Committee. The role of endoscopy in the management of patients with diarrhea. Gastrointest Endosc. 2010;71(6):887–892.
- Bellaiche G, Le Pennec MP, Slama JL, et al. The value of rectosigmoidoscopy and the bacteriologic culture of colon biopsies in the etiologic diagnosis of acute diarrhea of adults. A prospective study of 65 patients [in French]. Ann Gastroenterol Hepatol (Paris). 1996;32(1):11–17.
- Hahn S, Kim Y, Garner P. Reduced osmolarity oral rehydration solution for treating dehydration due to diarrhoea in children: systematic review. BMJ. 2001;323(7304):81–85.
- Alam NH, Yunus M, Faruque AS, et al. Symptomatic hyponatremia during treatment of dehydrating diarrheal disease with reduced osmolarity oral rehydration solution. JAMA. 2006;296(5):567–573.
- Gadewar S, Fasano A. Current concepts in the evaluation, diagnosis and management of acute infectious diarrhea. Curr Opin Pharmacol. 2005;5(6):559–565.
- De Bruyn G. Diarrhea in adults (acute). Am Fam Physician. 2008;78(4):503–504.
- Riddle MS, Arnold S, Tribble DR. Effect of adjunctive loperamide in combination with antibiotics on treatment outcomes in traveler’s diarrhea: a systematic review and meta-analysis. Clin Infect Dis. 2008;47(8):1007–1014.
- Hanauer SB, DuPont HL, Cooper KM, Laudadio C. Randomized, double-blind, placebo-controlled clinical trial of loperamide plus simethicone versus loperamide alone and simethicone alone in the treatment of acute diarrhea with gas-related abdominal discomfort. Curr Med Res Opin. 2007;23(5):1033–1043.
- DuPont HL, Hornick RB. Adverse effect of lomotil therapy in shigellosis. JAMA. 1973;226(13):1525–1528.
- Matheson AJ, Noble S. Racecadotril. Drugs. 2000;59(4):829–835.
- De Bruyn G, Hahn S, Borwick A. Antibiotic treatment for travellers’ diarrhoea. Cochrane Database Syst Rev. 2000;(3):CD002242.
- Wong CS, Jelacic S, Habeeb RL, Watkins SL, Tarr PI. The risk of the hemolytic-uremic syndrome after antibiotic treatment of Escherichia coli O157:H7 infections. N Engl J Med. 2000;342(26):1930–1936.
- McMahan ZH, DuPont HL. Review article: the history of acute infectious diarrhoea management—from poorly focused empiricism to fluid therapy and modern pharmacotherapy. Aliment Pharmacol Ther. 2007;25(7):759–769.
- Allen SJ, et al. Probiotics for treating acute infectious diarrhoea. Cochrane Database Syst Rev. 2010;(11):CD003048.
- Feizizadeh S, Salehi-Abargouei A, Akbari V. Efficacy and safety of Saccharomyces boulardii for acute diarrhea. Pediatrics. 2014;134(1):e176–e191.
- Urbańska M, Gieruszczak-Białek D, Szajewska H. Systematic review with meta-analysis: Lactobacillus reuteri DSM 17938 for diarrhoeal diseases in children. Aliment Pharmacol Ther. 2016;43(10):1025–1034.
- Basu S, Chatterjee M, Ganguly S, Chandra PK. Efficacy of Lactobacillus rhamnosus GG in acute watery diarrhoea of Indian children: a randomised controlled trial. J Paediatr Child Health. 2007;43(12):837–842.
- Szajewska H, et al. Meta-analysis: Lactobacillus GG for treating acute gastroenteritis in children—updated analysis of randomised controlled trials. Aliment Pharmacol Ther. 2013;38(5):467–476.
- McFarland LV. Meta-analysis of probiotics for the prevention of traveler’s diarrhea. Travel Med Infect Dis. 2007;5(2):97–105.
- Bhutta ZA, Bird SM, Black RE, et al. Therapeutic effects of oral zinc in acute and persistent diarrhea in children in developing countries: pooled analysis of randomized controlled trials. Am J Clin Nutr. 2000;72(6):1516–1522.
- Chey WD, Kurlander J, Eswaran S. Irritable bowel syndrome: a clinical review. Journal of the American Medical Association. 2015;313(9):949–958.
- Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology. 2016;150(6):1393–1407.
- Staudacher HM, Whelan K. Altered gastrointestinal microbiota in irritable bowel syndrome and its modification by diet: probiotics, prebiotics and the low FODMAP diet. Proc Nutr Soc. 2016 Aug;75(3):306-18. doi: 10.1017/S0029665116000021
- Definition & Facts for Irritable Bowel Syndrome. https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome/definition-facts
- Zhuang X, Xiong L, Li L, Li M, Chen M. Alterations of gut microbiota in patients with irritable bowel syndrome: A systematic review and meta-analysis. J Gastroenterol Hepatol. 2017 Jan;32(1):28-38. doi: 10.1111/jgh.13471
- Ford, AC, Harris, LA, Lacy, BE, Quigley, EMM, Moayyedi, P. Systematic review with meta-analysis: the efficacy of prebiotics, probiotics, synbiotics and antibiotics in irritable bowel syndrome. Aliment Pharmacol Ther. 2018; 48: 1044– 1060. https://eprints.whiterose.ac.uk/165996/2/APT-1106-2018R2.pdf
- Ford AC, Quigley EM, Lacy BE, Lembo AJ, Saito YA, Schiller LR, Soffer EE, Spiegel BM, Moayyedi P. Efficacy of prebiotics, probiotics, and synbiotics in irritable bowel syndrome and chronic idiopathic constipation: systematic review and meta-analysis. Am J Gastroenterol. 2014 Oct;109(10):1547-61; quiz 1546, 1562. doi: 10.1038/ajg.2014.202
- Didari T, Mozaffari S, Nikfar S, Abdollahi M. Effectiveness of probiotics in irritable bowel syndrome: Updated systematic review with meta-analysis. World J Gastroenterol. 2015 Mar 14;21(10):3072-84. doi: 10.3748/wjg.v21.i10.3072
- Lorenzo-Zúñiga V, Llop E, Suárez C, Alvarez B, Abreu L, Espadaler J, Serra J. I.31, a new combination of probiotics, improves irritable bowel syndrome-related quality of life. World J Gastroenterol. 2014 Jul 14;20(26):8709-16. doi: 10.3748/wjg.v20.i26.8709
- Williams EA, Stimpson J, Wang D, Plummer S, Garaiova I, Barker ME, Corfe BM. Clinical trial: a multistrain probiotic preparation significantly reduces symptoms of irritable bowel syndrome in a double-blind placebo-controlled study. Aliment Pharmacol Ther. 2009 Jan;29(1):97-103. doi: 10.1111/j.1365-2036.2008.03848.x
- McKenzie YA, Bowyer RK, Leach H, Gulia P, Horobin J, O’Sullivan NA, Pettitt C, Reeves LB, Seamark L, Williams M, Thompson J, Lomer MC; (IBS Dietetic Guideline Review Group on behalf of Gastroenterology Specialist Group of the British Dietetic Association). British Dietetic Association systematic review and evidence-based practice guidelines for the dietary management of irritable bowel syndrome in adults (2016 update). J Hum Nutr Diet. 2016 Oct;29(5):549-75. doi: 10.1111/jhn.12385
- Ford AC, Moayyedi P, Lacy BE, et al.; Task Force on the Management of Functional Bowel Disorders. American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. Am J Gastroenterol. 2014;109(suppl 1):S2–S26.
- Korterink JJ, et al. Probiotics for childhood functional gastrointestinal disorders: a systematic review and meta-analysis. Acta Paediatr. 2014;103(4):365–372.
- McKenzie YA, Thompson J, Gulia P, Lomer MC; (IBS Dietetic Guideline Review Group on behalf of Gastroenterology Specialist Group of the British Dietetic Association). British Dietetic Association systematic review of systematic reviews and evidence-based practice guidelines for the use of probiotics in the management of irritable bowel syndrome in adults (2016 update). J Hum Nutr Diet. 2016 Oct;29(5):576-92. doi: 10.1111/jhn.12386
- Principi N, Cozzali R, Farinelli E, Brusaferro A, Esposito S. Gut dysbiosis and irritable bowel syndrome: The potential role of probiotics. J Infect. 2018 Feb;76(2):111-120. doi: 10.1016/j.jinf.2017.12.013
- Ortiz-Lucas M, Tobías A, Saz P, Sebastián JJ. Effect of probiotic species on irritable bowel syndrome symptoms: A bring up to date meta-analysis. Rev Esp Enferm Dig. 2013 Jan;105(1):19-36. doi: 10.4321/s1130-01082013000100005
- Treatment for Irritable Bowel Syndrome. https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome/treatment
- Therapeutic effects of psyllium in type 2 diabetic patients. Sierra M, García JJ, Fernández N, Diez MJ, Calle AP. Eur J Clin Nutr. 2002 Sep; 56(9):830-42. https://www.ncbi.nlm.nih.gov/pubmed/12209371/
- Dietary fibres, fibre analogues, and glucose tolerance: importance of viscosity. Jenkins DJ, Wolever TM, Leeds AR, Gassull MA, Haisman P, Dilawari J, Goff DV, Metz GL, Alberti KG. Br Med J. 1978 May 27; 1(6124):1392-4. https://www.ncbi.nlm.nih.gov/pubmed/647304/
- Gastric emptying in early noninsulin-dependent diabetes mellitus. Jones KL, Horowitz M, Carney BI, Wishart JM, Guha S, Green L. J Nucl Med. 1996 Oct; 37(10):1643-8. https://www.ncbi.nlm.nih.gov/pubmed/8862300/
- Action of guar gums on the viscosity of digestive contents and on the gastrointestinal motor function in pigs. Cherbut C, Albina E, Champ M, Doublier JL, Lecannu G. Digestion. 1990; 46(4):205-13. https://www.ncbi.nlm.nih.gov/pubmed/2178135/
- Effect of viscous fiber (guar) on postprandial motor activity in human small bowel. Schönfeld J, Evans DF, Wingate DL. Dig Dis Sci. 1997 Aug; 42(8):1613-7. https://www.ncbi.nlm.nih.gov/pubmed/9286225/
- Effect of gel-forming gums on the intestinal unstirred layer and sugar transport in vitro. Johnson IT, Gee JM. Gut. 1981 May; 22(5):398-403. https://www.ncbi.nlm.nih.gov/pubmed/7250752/
- Role of viscous guar gums in lowering the glycemic response after a solid meal. Leclère CJ, Champ M, Boillot J, Guille G, Lecannu G, Molis C, Bornet F, Krempf M, Delort-Laval J, Galmiche JP. Am J Clin Nutr. 1994 Apr; 59(4):914-21. https://www.ncbi.nlm.nih.gov/pubmed/7818627/
- Dietary guar gum improves insulin sensitivity in streptozotocin-induced diabetic rats. Cameron-Smith D, Habito R, Barnett M, Collier GR. J Nutr. 1997 Feb; 127(2):359-64. https://www.ncbi.nlm.nih.gov/pubmed/9039840/
- Soluble dietary fibre improves insulin sensitivity by increasing muscle GLUT-4 content in stroke-prone spontaneously hypertensive rats. Song YJ, Sawamura M, Ikeda K, Igawa S, Yamori Y. Clin Exp Pharmacol Physiol. 2000 Jan-Feb; 27(1-2):41-5. https://www.ncbi.nlm.nih.gov/pubmed/10696527/
- Troglitazone effects on gene expression in human skeletal muscle of type II diabetes involve up-regulation of peroxisome proliferator-activated receptor-gamma. Park KS, Ciaraldi TP, Lindgren K, Abrams-Carter L, Mudaliar S, Nikoulina SE, Tufari SR, Veerkamp JH, Vidal-Puig A, Henry RR. J Clin Endocrinol Metab. 1998 Aug; 83(8):2830-5. https://www.ncbi.nlm.nih.gov/pubmed/9709955/
- Chen C, Zeng Y, Xu J, et al. Therapeutic effects of soluble dietary fiber consumption on type 2 diabetes mellitus. Experimental and Therapeutic Medicine. 2016;12(2):1232-1242. doi:10.3892/etm.2016.3377. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4950069/
- Aldoori WH, Giovannucci EL, Rockett HR, Sampson L, Rimm EB, Willett WC. A prospective study of dietary fiber types and symptomatic diverticular disease in men. J Nutr. 1998;128:714-9. https://www.ncbi.nlm.nih.gov/pubmed/9521633
- Resistant starch: metabolic effects and potential health benefits. Higgins JA. J AOAC Int. 2004 May-Jun; 87(3):761-8. https://www.ncbi.nlm.nih.gov/pubmed/15287677/
- Birt DF, Boylston T, Hendrich S, et al. Resistant Starch: Promise for Improving Human Health. Advances in Nutrition. 2013;4(6):587-601. doi:10.3945/an.113.004325. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3823506/
- Eating, Diet, & Nutrition for Irritable Bowel Syndrome. https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome/eating-diet-nutrition
- Franco AV. Recurrent urinary tract infections. Best Practice & Research Clinical Obstetrics and Gynaecology. 2005;19:861–873.
- Leung, A., Wong, A., Leung, A., & Hon, K. L. (2019). Urinary Tract Infection in Children. Recent patents on inflammation & allergy drug discovery, 13(1), 2–18. https://doi.org/10.2174/1872213X13666181228154940
- Grin PM, Kowalewska PM, Alhazzan W, et al. Lactobacillus for preventing recurrent urinary tract infections in women: meta-analysis. Can J Urol Int. 2013;20:6607–6614.
- Schwenger EM, Tejani AM, Loewen PS. Probiotics for preventing urinary tract infections in adults and children. Cochrane Database Syst Rev. 2015 Dec 23;(12):CD008772. doi: 10.1002/14651858.CD008772.pub2
- de Vrese M, Laue C, Papazova E, Petricevic L, Schrezenmeir J. Impact of oral administration of four Lactobacillus strains on Nugent score – systematic review and meta-analysis. Benef Microbes. 2019 May 28;10(5):483-496. doi: 10.3920/BM2018.0129
- Ko, S. H., & Kim, H. S. (2020). Menopause-Associated Lipid Metabolic Disorders and Foods Beneficial for Postmenopausal Women. Nutrients, 12(1), 202. https://doi.org/10.3390/nu12010202
- Becker, R.C. (2005). Heart attack and stroke prevention in women . Circulation; 112: e273–e275. https://doi.org/10.1161/CIRCULATIONAHA.105.551341
- Crandall, C., Aragaki, A., Cauley, J., Manson, J., LeBlanc, E., Wallace, R., et al. (2015). Associations of Menopausal Vasomotor Symptoms with Fracture Incidence . Journal of Clinical Endocrinology and Metabolism; 100(2): 524–534.
- Jackson, L. W., Cromer, B. A., & Panneerselvamm, A. (2010). Association between bone turnover, micronutrient intake, and blood lead levels in pre- and postmenopausal women, NHANES 1999-2002. Environmental health perspectives, 118(11), 1590–1596. https://doi.org/10.1289/ehp.1002158
- Shifren, J.L., Gass, M.L.S., for the NAMS Recommendations for Clinical Care of Midlife Women Working Group. (2014). The North American Menopause Society Recommendations for Clinical Care of Midlife Women . Menopause; 21(10): 1038–1062. http://www.menopause.org/docs/default-source/2014/nams-recomm-for-clinical-care.pdf
- Hatti-Kaul R., Chen L., Dishisha T., Enshasy H.E. Lactic acid bacteria: From starter cultures to producers of chemicals. FEMS Microbiol. Lett. 2018;365 doi: 10.1093/femsle/fny213
- Szulinska M., Loniewski I., Skrypnik K. Multispecies Probiotic Supplementation Favorably Affects Vascular Function and Reduces Arterial Stiffness in Obese Postmenopausal Women-A 12-Week Placebo-Controlled and Randomized Clinical Study. Nutrients. 2018;10:1672. doi: 10.3390/nu10111672
- Patel S. Disruption of aromatase homeostasis as the cause of a multiplicity of ailments: A comprehensive review. J. Steroid Biochem. Mol. Biol. 2017;168:19–25. doi: 10.1016/j.jsbmb.2017.01.009
- Dewailly D., Robin G., Peigne M., Decanter C., Pigny P., Catteau-Jonard S. Interactions between androgens, FSH, anti-Mullerian hormone and estradiol during folliculogenesis in the human normal and polycystic ovary. Hum. Reprod. Update. 2016;22:709–724. doi: 10.1093/humupd/dmw027
- Cervellati C., Bergamini C.M. Oxidative damage and the pathogenesis of menopause related disturbances and diseases. Clin. Chem. Lab. Med. 2016;54:739–753. doi: 10.1515/cclm-2015-0807
- Lobo R.A., Davis S.R., De Villiers T.J., Gompel A., Henderson V.W., Hodis H.N., Lumsden M.A., Mack W.J., Shapiro S., Baber R.J. Prevention of diseases after menopause. Climacteric. 2014;17:540–556. doi: 10.3109/13697137.2014.933411
- Sobenin I.A., Myasoedova V.A., Orekhov A.N. Phytoestrogen-Rich Dietary Supplements in Anti-Atherosclerotic Therapy in Postmenopausal Women. Curr. Pharm. Des. 2016;22:152–163. doi: 10.2174/1381612822666151112150520
- Thaung Zaw J.J., Howe P.R.C., Wong R.H.X. Postmenopausal health interventions: Time to move on from the Women’s Health Initiative? Ageing Res. Rev. 2018;48:79–86. doi: 10.1016/j.arr.2018.10.005
- North American Menopause Society. (2014). The Experts Do Agree About Hormone Therapy. https://www.menopause.org/docs/for-women/expertsagree_consumer.pdf
- Elkins GR, Fisher WI, Johnson AK, Carpenter JS, Keith TZ. Clinical hypnosis in the treatment of postmenopausal hot flashes: a randomized controlled trial. Menopause. 2013 Mar;20(3):291-8. doi: 10.1097/gme.0b013e31826ce3ed
- Stenman, L. K., Lehtinen, M. J., Meland, N., Christensen, J. E., Yeung, N., Saarinen, M. T., Courtney, M., Burcelin, R., Lähdeaho, M. L., Linros, J., Apter, D., Scheinin, M., Kloster Smerud, H., Rissanen, A., & Lahtinen, S. (2016). Probiotic With or Without Fiber Controls Body Fat Mass, Associated With Serum Zonulin, in Overweight and Obese Adults-Randomized Controlled Trial. EBioMedicine, 13, 190–200. https://doi.org/10.1016/j.ebiom.2016.10.036
- Osterberg KL, Boutagy NE, McMillan RP, Stevens JR, Frisard MI, Kavanaugh JW, Davy BM, Davy KP, Hulver MW. Probiotic supplementation attenuates increases in body mass and fat mass during high-fat diet in healthy young adults. Obesity (Silver Spring). 2015 Dec;23(12):2364-70. doi: 10.1002/oby.21230
- Sanchez M, Darimont C, Drapeau V, Emady-Azar S, Lepage M, Rezzonico E, Ngom-Bru C, Berger B, Philippe L, Ammon-Zuffrey C, Leone P, Chevrier G, St-Amand E, Marette A, Doré J, Tremblay A. Effect of Lactobacillus rhamnosus CGMCC1.3724 supplementation on weight loss and maintenance in obese men and women. Br J Nutr. 2014 Apr 28;111(8):1507-19. doi: 10.1017/S0007114513003875
- Kadooka Y, Sato M, Imaizumi K, Ogawa A, Ikuyama K, Akai Y, Okano M, Kagoshima M, Tsuchida T. Regulation of abdominal adiposity by probiotics (Lactobacillus gasseri SBT2055) in adults with obese tendencies in a randomized controlled trial. Eur J Clin Nutr. 2010 Jun;64(6):636-43. doi: 10.1038/ejcn.2010.19
- Kadooka Y, Sato M, Ogawa A, Miyoshi M, Uenishi H, Ogawa H, Ikuyama K, Kagoshima M, Tsuchida T. Effect of Lactobacillus gasseri SBT2055 in fermented milk on abdominal adiposity in adults in a randomised controlled trial. Br J Nutr. 2013 Nov 14;110(9):1696-703. doi: 10.1017/S0007114513001037
- Li S, Guerin-Deremaux L, Pochat M, Wils D, Reifer C, Miller LE. NUTRIOSE dietary fiber supplementation improves insulin resistance and determinants of metabolic syndrome in overweight men: a double-blind, randomized, placebo-controlled study. Appl Physiol Nutr Metab. 2010 Dec;35(6):773-82. doi: 10.1139/H10-074
- Parnell, J. A., & Reimer, R. A. (2009). Weight loss during oligofructose supplementation is associated with decreased ghrelin and increased peptide YY in overweight and obese adults. The American journal of clinical nutrition, 89(6), 1751–1759. https://doi.org/10.3945/ajcn.2009.27465
- Zhang Q, Wu Y, Fei X. Effect of probiotics on body weight and body-mass index: A systematic review and meta-analysis of randomized, controlled trials. Int J Food Sci Nutr 2015; 67:571-80; https://doi.org/10.1080/09637486.2016.1181156
- Park S, Bae JH. Probiotics for weight loss: a systematic review and meta-analysis. Nutr Res. 2015 Jul;35(7):566-75. doi: 10.1016/j.nutres.2015.05.008
- Hadi A, Alizadeh K, Hajianfar H, Mohammadi H, Miraghajani M. Efficacy of synbiotic supplementation in obesity treatment: A systematic review and meta-analysis of clinical trials. Crit Rev Food Sci Nutr. 2020;60(4):584-596. doi: 10.1080/10408398.2018.1545218





