What are beta agonists
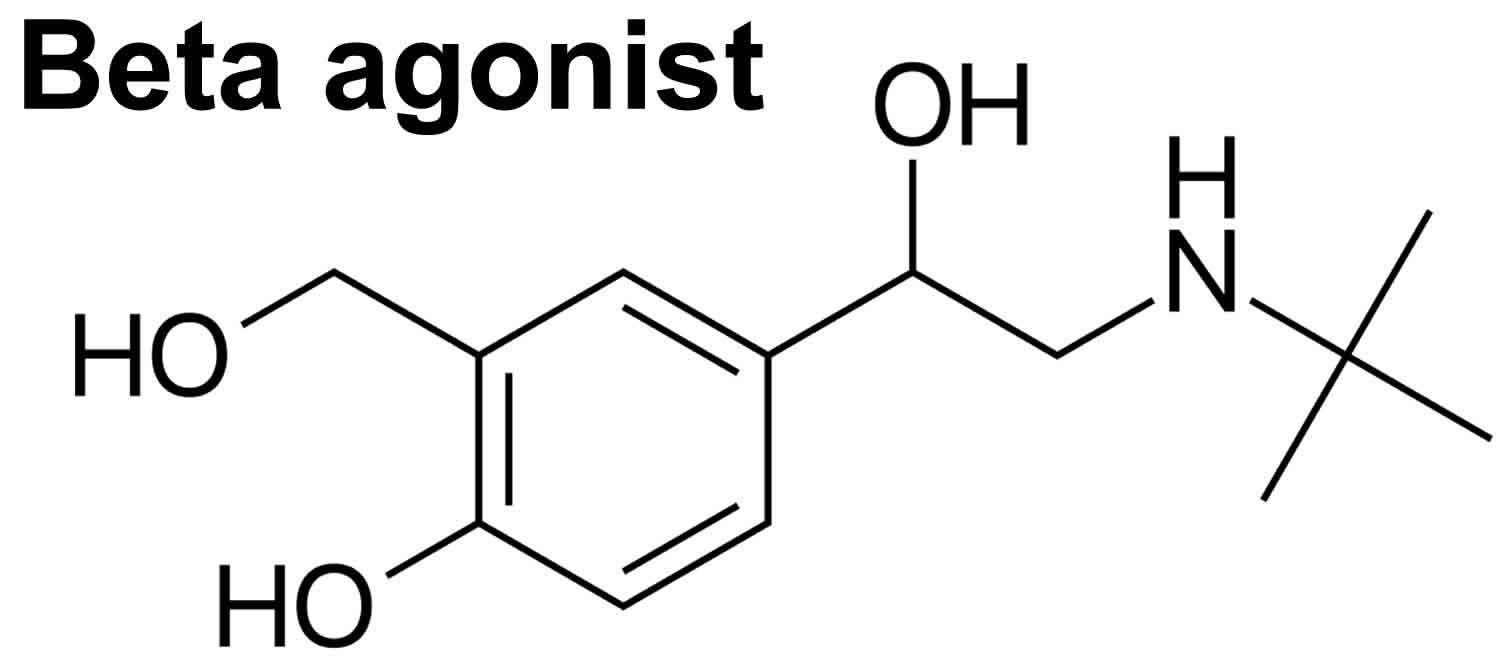
Beta-2 adrenergic agonists are a large group of drugs that mimic the actions of naturally occurring catecholamines such as norepinephrine (noradrenaline), epinephrine (adrenaline) and dopamine. Direct beta-agonists directly interact with the adrenergic receptors, whereas indirect beta-agonists typically stimulate the release of endogenous catecholamines (e.g., epinephrine, norepinephrine and dopamine).
The beta-2 adrenergic agonists act mainly on the smooth muscle of the blood vessels, bronchial tree, intestines and uterus. Beta-2 adrenergic agonists also act on the liver stimulating glycogenolysis and release of glucose from the liver and muscle (particularly if used in high doses). The beta-2 adrenergic agonists are used largely as bronchodilators in the management of asthma, both in control of acute symptomatic attacks as well as chronic, long term prevention and management. These agents are some of the most commonly prescribed drugs for asthma and are widely used and proven to be well tolerated and safe. When given in large doses or after intentional overdose, beta adrenergic agonists can cause liver injury. Most case reports of liver damage from these agents have been associated with their use in control of premature labor (for their effects on relaxation of uterine smooth muscle). The liver injury typically arises within a few days of starting high dose intravenous beta adrenergic agonists, is usually asymptomatic, not associated with jaundice, and rapidly reversed once the medication is stopped.
Major effects of beta agonist binding at adrenergic receptors:
- Beta-1 receptor: Increased cardiac chronotropic and inotropic effects 1. The key beta-1 selective drug is dobutamine 2. Dobutamine is indicated for the treatment of cardiogenic shock and heart failure 3
- Beta-2 receptor: Bronchodilators, such as albuterol and salmeterol. Bronchodilators are used for the treatment of obstructive lung disease, such as asthma 4.
- Beta-3 receptor: Increased lipolysis
Non-Selective Drugs
- Norepinephrine (noradrenaline): Norepinephrine binds to the alpha-1, alpha-2, and beta-1 receptors. Norepinephrine is used for the treatment of shock and hypotension.
- Epinephrine (adrenaline): Epinephrine binds to all of the adrenergic receptors (i.e., alpha-1, alpha-2, beta-1, beta-2, beta-3 receptors). Epinephrine is used for the treatment of cardiac arrest, anaphylaxis, and croup.
- Dopamine: Dopamine binds to the alpha-1, alpha 2, beta-1 receptors, and also the two dopamine receptors. Dopamine is used to treat hypotension, bradycardia, and cardiac arrest.
- Isoprenaline: Indicated for treating bradycardia and heart block.
Many of these medications, especially the non-selective ones, are used in the critical care and emergency setting. They are referred to as vasopressors. Side effects depend on the specific agent. However, changes in heart rate and blood pressure are the most common side effects.
Indirect acting adrenergic drugs increase norepinephrine and epinephrine through various mechanisms. Hence, their side effect profiles are similar to those seen with vasopressors.
Beta adrenergic agonists drugs
Commonly used beta adrenergic drugs include albuterol, bitolterol, metaproterenol, pirbuterol, salbutamol, salmeterol and terbutaline. These agents share structural similarity and are discussed together.
Beta 2 adrenergic agonist drugs:
- Albuterol
- Bitolterol,
- Formoterol (long acting beta agonist),
- Metaproterenol,
- Pirbuterol,
- Salbutamol,
- Salmeterol (long acting beta agonist),
- Terbutaline
The beta adrenergic agonists act on bronchial smooth muscle inducing bronchodilation and relieving bronchospasm in asthma and chronic obstructive pulmonary disease with asthmatic features.
The beta adrenergic agonists are potent bronchodilators that are widely used in the management of bronchial asthma. These agents act by engaging the beta-2 adrenergic receptors on smooth muscle of bronchial tissue, relieving bronchospasm and reducing airway resistance. They also act on smooth muscle of the vascular system, intestines and uterus.
Common forms of beta adrenergic agonists include albuterol, bitolterol, fenoterol, formoterol, levalbuterol, metaproterenol, salmeterol, pirbuterol and terbutaline, which all have similar mechanisms of action, chemical structure, side effects and efficacy, but somewhat different pharmacokinetics allowing for differences in dosing regimens and duration of action.
Most of these agents are administered by inhalation (alone or in combination with other bronchodilators or corticosteroids), with only albuterol and terbutaline being available in oral forms in the United States.
Albuterol (also known as salbutamol) is available in generic forms and under the brand names of Proventil and Ventolin as 2 and 4 mg tablets as well as in aerosol and syrup solutions. The recommended regimen of albuterol is 2 to 4 mg orally 3 to 4 times a day. Sustained release formulations are available for twice daily dosing (4 and 8 mg).
Salmeterol is available as an inhalation powder in generic forms and under the brand name of Serevent Diskus. The typical dosage is one inhalation (50 mcg) twice daily and it is recommended to be given with corticosteroids only. Systemic absorption is minimal.
Terbutaline is available in generic forms and under the brand name of Brethine in tablets of 2.5 and 5 mg, the usual adult dosage being 5 mg three times daily. These oral forms of beta adrenergic agonists are approved as means of prevention and reversal of bronchospasm and are used largely in the therapy of asthma. Terbutaline is also available in parenteral formulations for use in acute bronchospasm and has also been used as therapy of premature labor.
Short acting beta agonist
Albuterol
Albuterol is in a class of medications called bronchodilators. It works by relaxing and opening the air passages to the lungs to make breathing easier. Albuterol is used to prevent and treat wheezing, difficulty breathing, chest tightness, and coughing caused by lung diseases such as asthma and chronic obstructive pulmonary disease (COPD; a group of diseases that affect the lungs and airways).
Albuterol comes as a tablet, a syrup, and an extended-release (long-acting) tablet to take by mouth. The tablets and syrup are usually taken three or four times a day. The extended-release tablets are usually taken once every 12 hours. Take albuterol at around the same times every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take albuterol exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Swallow the extended-release tablets whole with plenty of water or other liquid. Do not split, chew, or crush them.
Your doctor may start you on a low dose of albuterol and gradually increase your dose.
Albuterol may help control your symptoms but will not cure your condition. Continue to take albuterol even if you feel well. Do not stop taking albuterol without talking to your doctor.
Call your doctor if your symptoms worsen or if you feel that albuterol no longer controls your symptoms.
Albuterol special precautions
Before taking albuterol:
- tell your doctor and pharmacist if you are allergic to albuterol, any other medications, or any of the ingredients in albuterol tablets, extended-release tablets, or capsules. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: beta blockers such as atenolol (Tenormin), labetalol (Normodyne), metoprolol (Lopressor, Toprol XL), nadolol (Corgard), and propranolol (Inderal); digoxin (Lanoxin); diuretics (‘water pills’); epinephrine (Epipen, Primatene Mist); other oral and inhaled medications for asthma and medications for colds. Also tell your doctor or pharmacist if you are taking the following medications or have stopped taking them within the past two weeks: antidepressants such as amitriptyline (Elavil), amoxapine (Asendin), clomipramine (Anafranil), desipramine (Norpramin), doxepin (Adapin, Sinequan), imipramine (Tofranil), nortriptyline (Aventyl, Pamelor), protriptyline (Vivactil), and trimipramine (Surmontil); and monoamine oxidase (MAO) inhibitors, including isocarboxazid (Marplan), phenelzine (Nardil), selegiline (Eldepryl, Emsam, Zelapar), and tranylcypromine (Parnate). Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have or have ever had an irregular heartbeat, heart disease, high blood pressure, hyperthyroidism (condition in which there is too much thyroid hormone in the body), diabetes, or seizures.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while taking albuterol, call your doctor.
- you should know that albuterol sometimes causes wheezing and difficulty breathing. If this happens, call your doctor right away. Do not use albuterol again unless your doctor tells you that you should.
Albuterol side effects
Albuterol may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- nervousness
- shakiness
- dizziness
- headache
- uncontrollable shaking of a part of the body
- muscle cramps
- excessive motion or activity
- sudden changes in mood
- nosebleed
- nausea
- increased or decreased appetite
- difficulty falling asleep or staying asleep
- pale skin
Some side effects can be serious. If you experience any of these symptoms, call your doctor immediately:
- fast, pounding, or irregular heartbeat
- chest pain
- fever
- blisters or rash
- hives
- itching
- swelling of the face, throat, tongue, lips, eyes, hands, feet, ankles, or lower legs
- increased difficulty breathing
- difficulty swallowing
- hoarseness
Albuterol may cause other side effects. Call your doctor if you have any unusual problems while taking albuterol.
Metaproterenol
Metaproterenol is used to prevent and treat wheezing, shortness of breath, coughing, and chest tightness caused by asthma, chronic bronchitis, emphysema, and other lung diseases. It relaxes and opens air passages in the lungs, making it easier to breathe.
Metaproterenol comes as tablets and syrup to take by mouth and as a solution to inhale by mouth. It usually is used by oral inhalation every 4 hours to relieve symptoms or 3 to 4 times a day to prevent symptoms or by mouth three or four times a day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Use metaproterenol exactly as directed. Do not use more or less of it or use it more often than prescribed by your doctor.
Metaproterenol controls symptoms of asthma and other lung diseases but does not cure them. Continue to use metaproterenol even if you feel well. Do not stop using metaproterenol without talking to your doctor.
Metaproterenol special precautions
Before using metaproterenol:
- tell your doctor and pharmacist if you are allergic to metaproterenol or any other drugs.
- tell your doctor and pharmacist what prescription medications you are taking, especially atenolol (Tenormin); carteolol (Cartrol); labetalol (Normodyne, Trandate); metoprolol (Lopressor); nadolol (Corgard); phenelzine (Nardil); propranolol (Inderal); sotalol (Betapace); theophylline (Theo-Dur); timolol (Blocadren); tranylcypromine (Parnate); other medications for asthma, heart disease, or depression.
- tell your doctor and pharmacist what nonprescription medications and vitamins you are taking, including ephedrine, phenylephrine, phenylpropanolamine, or pseudoephedrine. Many nonprescription products contain these drugs (e.g., diet pills and medications for colds and asthma), so check labels carefully. Do not take any of these medications without talking to your doctor (even if you never had a problem taking them before).
- tell your doctor if you have or have ever had irregular heartbeat, increased heart rate, glaucoma, heart disease, high blood pressure, an overactive thyroid gland, diabetes, or seizures.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while using metaproterenol, call your doctor.
if you are having surgery, including dental surgery, tell the doctor or dentist that you are using metaproterenol.
Metaproterenol side effects
Metaproterenol may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- tremor
- nervousness
- dizziness
- weakness
- headache
- nausea
If you experience any of the following symptoms, call your doctor immediately:
- increased difficulty breathing
- rapid or increased heart rate
- irregular heartbeat
- chest pain or discomfort
Metaproterenol may cause other side effects. Call your doctor if you have any unusual problems while taking metaproterenol.
Pirbuterol
Pirbuterol is used to prevent and treat wheezing, shortness of breath, coughing, and chest tightness caused by asthma, chronic bronchitis, emphysema, and other lung diseases. It works by relaxing and opening air passages in the lungs, making it easier to breathe.
Pirbuterol comes as an aerosol to inhale by mouth. It is usually taken as 1 to 2 puffs every 4 to 6 hours as needed to relieve symptoms or every 4 to 6 hours to prevent symptoms. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Use pirbuterol exactly as directed. Do not use more or less of it or use it more often than prescribed by your doctor. Do not use more than 12 puffs in 24 hours.
Pirbuterol controls symptoms of asthma and other lung diseases but does not cure them. Do not stop using pirbuterol without talking to your doctor.
Before you use the pirbuterol inhaler the first time, read the written instructions that come with it. Ask your doctor, pharmacist, or respiratory therapist to demonstrate the proper technique. Practice using the inhaler while in his or her presence.
The pirbuterol inhaler should be primed (tested) before you use it the first time and any time it has not been used for 48 hours. To prime the inhaler, follow these steps:
- Remove the mouthpiece cover by pulling down the lip on the back of the cover.
- Point the mouthpiece away from yourself and other people so that the priming sprays will go into the air.
- Push the lever up so it stays up.
- Push the white test fire slide on the bottom of the mouthpiece in the direction indicated by the arrow on the test fire slide. A priming spray will be released.
- To release a second priming spray, return the lever to its down position and repeat steps 2-4.
- After the second priming spray is released, return the lever to its down position.
To use the inhaler, follow these steps:
- Remove the mouthpiece cover by pulling down the lip on the back of the cover. Make sure there are no foreign objects in the mouthpiece.
- Hold the inhaler upright so that the arrows point up. Then raise the lever so that it snaps into place and stays up.
- Hold the inhaler around the middle and shake gently several times.
- Continue to hold the inhaler upright and exhale (breathe out) normally.
- Seal your lips tightly around the mouthpiece and inhale (breathe in) deeply through the mouthpiece with steady force. You will hear a click and feel a soft puff when the medicine is released. Do not stop when you hear and feel the puff; continue to take a full, deep breath.
- Take the inhaler away from you mouth, hold your breath for 10 seconds, then exhale slowly.
- Continue to hold the inhaler upright while lowering the lever. Lower the lever after each inhalation.
- If your doctor has told you to take more than one inhalation, wait 1 minute and then repeat steps 2-7.
- When you have finished using the inhaler, make sure the lever is down and replace the mouthpiece cover.
Pirbuterol special precautions
Before using pirbuterol:
- tell your doctor and pharmacist if you are allergic to pirbuterol or any other drugs.
- tell your doctor and pharmacist what prescription medications you are taking, especially atenolol (Tenormin); carteolol (Cartrol); labetalol (Normodyne, Trandate); metoprolol (Lopressor); nadolol (Corgard); phenelzine (Nardil); propranolol (Inderal); sotalol (Betapace); theophylline (Theo-Dur); timolol (Blocadren); tranylcypromine (Parnate); other medications for asthma, heart disease, or depression.
- tell your doctor and pharmacist what nonprescription medications and vitamins you are taking, including ephedrine, phenylephrine, phenylpropanolamine, or pseudoephedrine. Many nonprescription products contain these drugs (e.g., diet pills and medications for colds and asthma), so check labels carefully. Do not take any of these medications without talking to your doctor (even if you never had a problem taking them before).
- tell your doctor if you have or have ever had an irregular heartbeat, increased heart rate, glaucoma, heart disease, high blood pressure, an overactive thyroid gland, diabetes, or seizures.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while using pirbuterol, call your doctor.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are using pirbuterol.
Pirbuterol side effects
Pirbuterol may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- tremor
- nervousness
- dizziness
- weakness
- headache
- upset stomach
- diarrhea
- cough
- dry mouth
- throat irritation
If you experience any of the following symptoms, call your doctor immediately:
- increased difficulty breathing
- rapid or increased heartbeat
- irregular heartbeat
- chest pain or discomfort
Pirbuterol may cause other side effects. Call your doctor if you have any unusual problems while taking pirbuterol.
Terbutaline
Terbutaline is used to prevent and treat wheezing, shortness of breath, and chest tightness caused by asthma, chronic bronchitis, and emphysema. Terbutaline works by relaxing and opening the airways, making it easier to breathe.
Terbutaline comes as a tablet to take by mouth. The tablets are usually taken three times a day, once every six hours. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take terbutaline exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Each dose of terbutaline should control your symptoms for at least 6 hours after you take it. If you find that your symptoms return before it is time for your next dose, that terbutaline does not control your symptoms as well as it did at the beginning of your treatment, or that your symptoms are getting worse, call your doctor. These may be signs that your condition is worsening.
Terbutaline may control your symptoms but will not cure your condition. Continue to use terbutaline even if you feel well. Do not stop taking terbutaline without talking to your doctor.
Terbutaline should not be used to stop or prevent premature labor in pregnant women, especially in women who are not in a hospital. Terbutaline has caused serious side effects, including death, in pregnant women who took the medication for this purpose. Terbutaline has also caused serious side effects in newborns whose mothers took the medication to stop or prevent labor.
Terbutaline special precautions
Before taking terbutaline:
- tell your doctor and pharmacist if you are allergic to terbutaline, any other medications, or any of the ingredients in terbutaline tablets. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: beta blockers such as atenolol (Tenormin), carteolol (Cartrol), labetalol (Normodyne, Trandate), metoprolol (Lopressor), nadolol (Corgard), propanolol (Inderal), sotalol (Betapace), and timolol (Blocadren); certain diuretics ( ‘water pills’); other medications for asthma; and medications for colds, appetite control, and attention-deficit hyperactivity disorder. Also tell your doctor if you are taking any of the following medications or if you have stopped taking them in the past 2 weeks: tricyclic antidepressants including amitriptyline, amoxapine, clomipramine (Anafranil), desipramine (Norpramin), doxepin, imipramine (Tofranil), maprotiline, nortriptyline (Pamelor), protriptyline (Vivactil), and trimipramine (Surmontil) and monoamine oxidase inhibitors (MAOIs) including isocarboxazid (Marplan), phenelzine (Nardil), selegiline (Eldepryl, Emsam, Zelapar), and tranylcypromine (Parnate). Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have or have ever had an irregular heartbeat, heart disease, high blood pressure, an overactive thyroid gland, diabetes, or seizures.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while taking terbutaline, call your doctor.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking terbutaline.
Terbutaline side effects
Terbutaline may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- uncontrollable shaking of a part of the body
- nervousness
- dizziness
- drowsiness
- difficulty falling asleep or staying asleep
- weakness
- headache
- nausea
- sweating
- dry mouth
Some side effects can be serious. If you experience any of the following symptoms, call your doctor immediately:
- increased difficulty breathing
- tightening of the throat
- fast, pounding, or irregular heartbeat
- chest pain
- seizures
Terbutaline may cause other side effects. Call your doctor if you have any unusual problems while taking terbutaline.
Symptoms of terbutaline overdose may include:
- chest pain
- fast, pounding, or irregular heartbeat
- dizziness or fainting
- nervousness
- headache
- uncontrollable shaking of a part of the body
- excessive tiredness
- difficulty falling asleep or staying asleep
- weakness
- dry mouth
- seizures
Long acting beta agonist
Formoterol
Formoterol is in a class of medications called long-acting beta agonists. It works by relaxing and opening air passages in the lungs, making it easier to breathe. Formoterol oral inhalation is used for the maintenance treatment of wheezing, shortness of breath, and breathing difficulties caused by chronic obstructive pulmonary disease (COPD; a group of lung diseases that includes chronic bronchitis and emphysema) in adults.
Formoterol oral inhalation comes as a solution (liquid) to inhale by mouth using a nebulizer (machine that turns medication into a mist that can be inhaled). It is usually inhaled twice a day in the morning and the evening about 12 hours after you inhaled your last dose. Inhale formoterol at about the same times every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Use formoterol exactly as directed. Do not use more or less of it or use it more often than prescribed by your doctor.
Formoterol oral inhalation helps to prevent COPD attacks but will not stop an attack that has already started. Do not use formoterol during a sudden COPD attack. Your doctor will prescribe a short-acting inhaler to use during attacks.
Formoterol inhalation should not be used to treat COPD that is quickly getting worse. Call your doctor or get emergency medical help if your breathing problems worsen, if you have to use your short-acting inhaler to treat attacks of COPD more often, or if your short-acting inhaler does not relieve your symptoms.
Formoterol inhalation may help control your symptoms but will not cure your condition. Do not stop using formoterol without talking to your doctor. If you suddenly stop using formoterol, your symptoms may worsen.
To inhale the solution using a nebulizer, follow these steps:
- Remove one vial of formoterol inhalation solution from the foil pouch.
- Look at the liquid in the vial. It should be clear and colorless. Do not use the vial if the liquid is cloudy or discolored.
- Twist off the top of the vial and squeeze all of the liquid into the nebulizer reservoir. Do not mix other medications with formoterol in the reservoir.
- Connect the nebulizer reservoir to the mouthpiece or face mask.
- Connect the nebulizer to the compressor.
- Place the mouthpiece in your mouth or put on the face mask. Sit in an upright, comfortable position and turn on the compressor.
- Breathe in calmly, deeply, and evenly for about 9 minutes until mist stops forming in the nebulizer chamber.
- Dispose of the empty vial and its top safely, so that they are out of the reach of children.
Clean your nebulizer regularly. Follow the manufacturer’s directions carefully and ask your doctor or pharmacist if you have any questions about cleaning your nebulizer.
Do not mix the formoterol solution with other inhalation solutions in your nebulizer.
In a large clinical study, more people who used an asthma medication similar to formoterol experienced more severe episodes of asthma that needed to be treated in a hospital or caused death than patients who did not use the medication. Use of formoterol inhalation may increase the risk of serious asthma problems or death in people who have asthma. Formoterol inhalation is not approved by the Food and Drug Administration (FDA) to treat asthma. There is not enough information to tell whether formoterol inhalation increases the risk of death in people who have chronic obstructive pulmonary disease (COPD; a group of lung diseases, which includes chronic bronchitis and emphysema).
Talk to your doctor about the risks of using this medication.
Your doctor or pharmacist will give you the manufacturer’s patient information sheet (Medication Guide) when you begin treatment with formoterol and each time you refill your prescription. Read the information carefully and ask your doctor or pharmacist if you have any questions. You can also visit the Food and Drug Administration (FDA) website (https://www.fda.gov/Drugs/DrugSafety/ucm085729.htm) or the manufacturer’s website to obtain the Medication Guide.
Formoterol special precautions
Before using formoterol oral inhalation:
- tell your doctor and pharmacist if you are allergic to formoterol, any other medications, or any of the ingredients in formoterol nebulizer solution. Ask your pharmacist or check the Medication Guide for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: amiodarone (Nexterone, Pacerone); beta blockers such as atenolol (Tenormin), labetalol (Trandate), metoprolol (Lopressor, Toprol XL, others), nadolol (Corgard), propranolol (Inderal, Innopran), and sotalol (Betapace, Sorine); clonidine (Catapres); disopyramide (Norpace); diuretics (‘water pills’); dofetilide (Tikosyn); erythromycin (E.E.S, E-Mycin, Erythrocin);other long-acting beta agonists (LABAs) such as arformoterol (Brovana) or salmeterol (Serevent, in Advair, in Airduo); moxifloxacin (Avelox); pimozide (Orap); procainamide; quinidine (in Nuedexta);steroids such as dexamethasone, methylprednisolone (Medrol), and prednisone (Rayos); theophylline (Elixophyllin, Theo-24); and thioridazine. Also, tell your doctor if you are taking a tricyclic antidepressant such as amitriptyline, desipramine (Norpramin), clomipramine (Anafranil), imipramine (Tofranil), nortriptyline, or trimipramine (Surmontil) or a monoamine oxidase (MAO) inhibitor such as isocarboxazid (Marplan), linezolid (Zyvox), methylene blue, phenelzine (Nardil), selegiline (Eldepryl, Emsam, Zelapar), and tranylcypromine (Parnate). Many other medications may also interact with formoterol, so be sure to tell your doctor about all the medications you are taking, even those that do not appear on this list. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have or have ever had an irregular heartbeat; QT prolongation (an irregular heart rhythm that can lead to fainting, loss of consciousness, seizures, or sudden death); high blood pressure; seizures; diabetes; or heart, liver, or thyroid disease.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are using formoterol oral inhalation.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while using formoterol, call your doctor.
Formoterol side effects
Formoterol may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- nervousness
- headache
- uncontrollable shaking of a part of the body
- dry mouth
- muscle cramps
- nausea
- vomiting
- diarrhea
- extreme tiredness
- dizziness
- difficulty falling asleep or staying asleep
- stuffed or runny nose
- sore throat
Some side effects can be serious. If you experience any of the following symptoms, stop using formoterol inhalation and call your doctor immediately or get emergency medical treatment:
- coughing, wheezing, or chest tightness that begins soon after you inhale formoterol
- swelling of the face, throat, tongue, lips, eyes, hands, feet, ankles, or lower legs
- difficulty swallowing or breathing
- hives
- rash
- itching
- fast, pounding, or irregular heartbeat
- chest pain
- fainting
- seizures
Formoterol may cause other side effects. Call your doctor if you have any unusual problems while using formoterol.
Symptoms of formoterol overdose may include the following:
- chest pain
- fainting
- fast, pounding, or irregular heartbeat
- nervousness
- headache
- uncontrollable shaking of a part of the body
- seizures
- muscle cramps
- dry mouth
- nausea
- dizziness
- excessive tiredness
- difficulty falling asleep or staying asleep
- thirst
- trouble breathing
Salmeterol
Salmeterol is in a class of medications called long-acting beta agonists. It works by relaxing and opening air passages in the lungs, making it easier to breathe. Salmeterol is used to treat wheezing, shortness of breath, coughing, and chest tightness caused by asthma and chronic obstructive pulmonary disease (COPD; a group of lung diseases that includes chronic bronchitis and emphysema). It also is used to prevent bronchospasm (breathing difficulties) during exercise.
Salmeterol comes as a dry powder to inhale by mouth using a specially designed inhaler. When salmeterol is used to treat asthma or COPD, it is usually used twice a day, in the morning and evening, about 12 hours apart. Use salmeterol at around the same times every day. When salmeterol is used to prevent breathing difficulties during exercise, it is usually used at least 30 minutes before exercise, but not more often than once every 12 hours. If you are using salmeterol twice a day on a regular basis, do not use another dose before exercising. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Use salmeterol exactly as directed. Do not use more or less of it or use it more often than prescribed by your doctor.
Talk to your doctor about how you should take your other oral or inhaled medications for asthma during your treatment with salmeterol. If you were taking a corticosteroid (a type of medication used to prevent airway swelling in patients with asthma), you doctor will probably tell you to continue taking it just as you did before you began using salmeterol. If you were using a short acting beta agonist inhaler such as albuterol (Proventil, Ventolin) on a regular basis, your doctor will probably tell you to stop using it regularly, but to continue to use it to treat sudden attacks of asthma symptoms. Follow these directions carefully. Do not change the way you use any of your medications without talking to your doctor.
Do not use salmeterol during an attack of asthma or COPD. Your doctor will prescribe a short-acting inhaler to use during attacks.
Salmeterol controls the symptoms of asthma and other lung diseases but does not cure these conditions. Do not stop using salmeterol without talking to your doctor. If you suddenly stop using salmeterol, your symptoms may worsen.
Before you use the salmeterol inhaler the first time, ask your doctor, pharmacist, or respiratory therapist to show you how to use it. Practice using the inhaler while he or she watches.
To use the inhaler, follow these steps:
- If you will be using a new inhaler for the first time, remove it from the box and the foil wrapper. Fill in the blanks on the inhaler label with the date that you opened the pouch and the date 6 weeks later when you must replace the inhaler.
- Hold the inhaler in one hand, and put the thumb of your other hand on the thumbgrip. Push your thumb away from you as far as it will go until the mouthpiece appears and snaps into position.
- Hold the inhaler in a level, horizontal position with the mouthpiece toward you. Slide the lever away from you as far as it will go until it clicks.
- Every time the lever is pushed back, a dose is ready to inhale. You will see the number in the dose counter go down. Do not waste doses by closing or tilting the inhaler, playing with the lever, or advancing the lever more than once.
- Hold the inhaler level and away from your mouth, and breathe out as far as you comfortably can.
- Keep the inhaler in a level, flat position. Put the mouthpiece to your lips. Breathe in quickly and deeply though the inhaler, not through your nose.
- Remove the inhaler from your mouth, and hold your breath for 10 seconds or as long as you comfortably can. Breathe out slowly.
- You will probably taste or feel the salmeterol powder released by the inhaler. Even if you do not, do not inhale another dose. If you are not sure you are getting your dose of salmeterol, call your doctor or pharmacist.
- Put your thumb on the thumbgrip and slide it back toward you as far as it will go. The device will click shut.
Never exhale into the inhaler, take the inhaler apart, or wash the mouthpiece or any part of the inhaler. Keep the inhaler dry. Do not use the inhaler with a spacer.
In a large clinical study, more patients with asthma who used salmeterol experienced severe episodes of asthma that had to be treated in a hospital or caused death than patients with asthma who did not use salmeterol. If you have asthma, use of salmeterol may increase the chance that you will experience serious or fatal asthma problems.
Your doctor will only prescribe salmeterol if your asthma is so severe that two medications are needed to control it. You should never use salmeterol alone; you must always use it along with another asthma controller medication. Children and teenagers who need to be treated with salmeterol will probably be treated with a product that combines salmeterol and another medication in a single inhaler to make it easier for them to use both medications as prescribed.
Because of the risks of using salmeterol, you should only use salmeterol as long as it is needed to bring your asthma symptoms under control. Once your asthma is controlled, your doctor will probably tell you to stop using salmeterol but continue using the other asthma medication.
Do not use salmeterol if you have asthma that is quickly getting worse. Tell your doctor if you have had many severe asthma attacks or if you have ever been hospitalized because of asthma symptoms. If you have any of the following signs of worsening asthma, call your doctor immediately:
- your short-acting inhaler (inhaled medication such as albuterol [Proventil, Ventolin] that is used to treat sudden attacks of asthma symptoms) does not work as well as it did in the past
- you need to use more puffs than usual of your short-acting inhaler or use it more often
- you need to use four or more puffs per day of your short-acting inhaler for two or more days in a row
- you use more than one canister (200 inhalations) of your short-acting inhaler during an 8-week period
- your peak-flow meter (home device used to test breathing) results show your breathing problems are worsening
- you need to go to the emergency room for asthma treatment.
- your symptoms do not improve after you use salmeterol regularly for one week or your symptoms get worse at any time during your treatment
Talk to your doctor about the risks of using this medication.
Your doctor or pharmacist will give you the manufacturer’s patient information sheet (Medication Guide) when you begin treatment with salmeterol and each time you refill your prescription. Read the information carefully and ask your doctor or pharmacist if you have any questions. You can also visit the Food and Drug Administration (FDA) website (https://www.fda.gov/Drugs/DrugSafety/ucm085729.htm) or the manufacturer’s website to obtain the Medication Guide.
Salmeterol special precautions
Before using salmeterol:
tell your doctor and pharmacist if you are allergic to salmeterol, any other medications, milk protein, or any foods.
tell your doctor if you use another LABA such as fluticasone and salmeterol combination (Advair) or formoterol (Foradil). These medications should not be used with salmeterol. Your doctor will tell you which medication you should use and which medication you should stop using.
tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking. Be sure to mention any of the following: antifungals such as itraconazole (Sporanox) and ketoconazole (Nizoral); beta blockers such as atenolol (Tenormin), labetalol (Normodyne), metoprolol (Lopressor, Toprol XL), nadolol (Corgard), and propranolol (Inderal); clarithromycin (Biaxin); diuretics (‘water pills’); HIV protease inhibitors such as atazanavir (Reyataz), indinavir (Crixivan), nelfinavir (Viracept), ritonavir (Norvir), and saquinavir (Invirase); other medications for asthma or COPD; nefazodone; and telithromycin (Ketek). Also tell your doctor or pharmacist if you are taking the following medications or have stopped taking them within the past 2 weeks: antidepressants such as amitriptyline (Elavil), amoxapine (Asendin), clomipramine (Anafranil), desipramine (Norpramin), doxepin (Adapin, Sinequan), imipramine (Tofranil), nortriptyline (Aventyl, Pamelor), protriptyline (Vivactil), and trimipramine (Surmontil); and monoamine oxidase (MAO) inhibitors including isocarboxazid (Marplan), phenelzine (Nardil), selegiline (Eldepryl), and tranylcypromine (Parnate). Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
tell your doctor if you have or have ever had irregular heartbeat, high blood pressure, hyperthyroidism (overactive thyroid), diabetes, seizures, or liver or heart disease.
tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while using salmeterol, call your doctor.
Salmeterol side effects
Salmeterol may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- shaking of a part of your body that you cannot control
- headache
- nervousness
- dizziness
- cough
- stuffed nose
- runny nose
- ear pain
- pale skin
- muscle pain, stiffness, or cramps
- sore throat
- throat irritation
- flu-like symptoms
- nausea
- heartburn
- tooth pain
- dry mouth
- sores or white patches in the mouth
- red or irritated eyes
- difficulty falling asleep or staying asleep
- burning or tingling of the hands or feet
Some side effects can be serious. If you experience any of the following symptoms, call your doctor immediately:
- coughing, wheezing, or chest tightness that begins soon after you inhale salmeterol
- fast or pounding heartbeat
- chest pain
- rash
- hives
- swelling of the face, throat, tongue, lips, eyes, hands, feet, ankles, or lower legs
- hoarseness
- choking or difficulty swallowing
- loud, high-pitched breathing
Salmeterol may cause other side effects. Call your doctor if you have any unusual problems while you are taking salmeterol.
Symptoms of salmeterol overdose may include:
- seizures
- chest pain
- dizziness
- fainting
- blurred vision
- fast, pounding, or irregular heartbeat
- nervousness
- headache
- shaking of a part of your body that you cannot control
- muscle cramps or weakness
- dry mouth
- nausea
- dizziness
- excessive tiredness
- lack of energy
- difficulty falling asleep or staying asleep
Beta agonist side effects
Common side effects of the beta adrenergic agonists include dizziness, headache, nervousness, tachycardia, palpitations, nausea and diaphoresis, largely due to their beta adrenergic effects on other organs. Rare, potentially severe adverse events include cardiovascular events, paradoxical worsening of asthma and acute hypersensitivity reactions.
Selective binding to beta-1 receptors commonly causes tachycardia, palpitations, and hypertension. Tachyarrhythmias and anxiety can also be common. High doses may induce dangerous arrhythmias. An example of a selective beta-1 receptor agonist is dobutamine.
Beta-2 receptor agonists can cause tremor, tachycardia, palpitations, and anxiety. Common examples are the various bronchodilator drugs such as albuterol and salmeterol 5.
Non-selective binding to the adrenergic receptors can cause different side effects that vary based on the specific agent as well as the dosage. The common non-selective agonists are norepinephrine, epinephrine, and isoprenaline. Common side effects are tachycardia, hypertension, arrhythmias, palpitations, and anxiety. Norepinephrine is less likely to cause arrhythmias than some of the other pressor medications.
References- Wachter SB, Gilbert EM. Beta-adrenergic receptors, from their discovery and characterization through their manipulation to beneficial clinical application. Cardiology. 2012;122(2):104-12
- Farzam K, Lakhkar AD. Adrenergic Drugs. [Updated 2019 Mar 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534230
- Dubin A, Lattanzio B, Gatti L. The spectrum of cardiovascular effects of dobutamine – from healthy subjects to septic shock patients. Rev Bras Ter Intensiva. 2017 Oct-Dec;29(4):490-498.
- Matera MG, Rinaldi B, Page C, Rogliani P, Cazzola M. Pharmacokinetic considerations concerning the use of bronchodilators in the treatment of chronic obstructive pulmonary disease. Expert Opin Drug Metab Toxicol. 2018 Oct;14(10):1101-1111
- Almadhoun K, Sharma S. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Oct 27, 2018. Bronchodilators.