Blood sugar regulation
Many foods break down into blood sugar (glucose), which is used for energy to fuel your brain, heart, and muscles. Blood sugar either comes from the food you eat or is made by your liver. When you eat, your body breaks down carbohydrates from foods — such as bread, rice, pasta, vegetables, fruit and milk products — into various sugar molecules, including glucose, a monosaccharide.
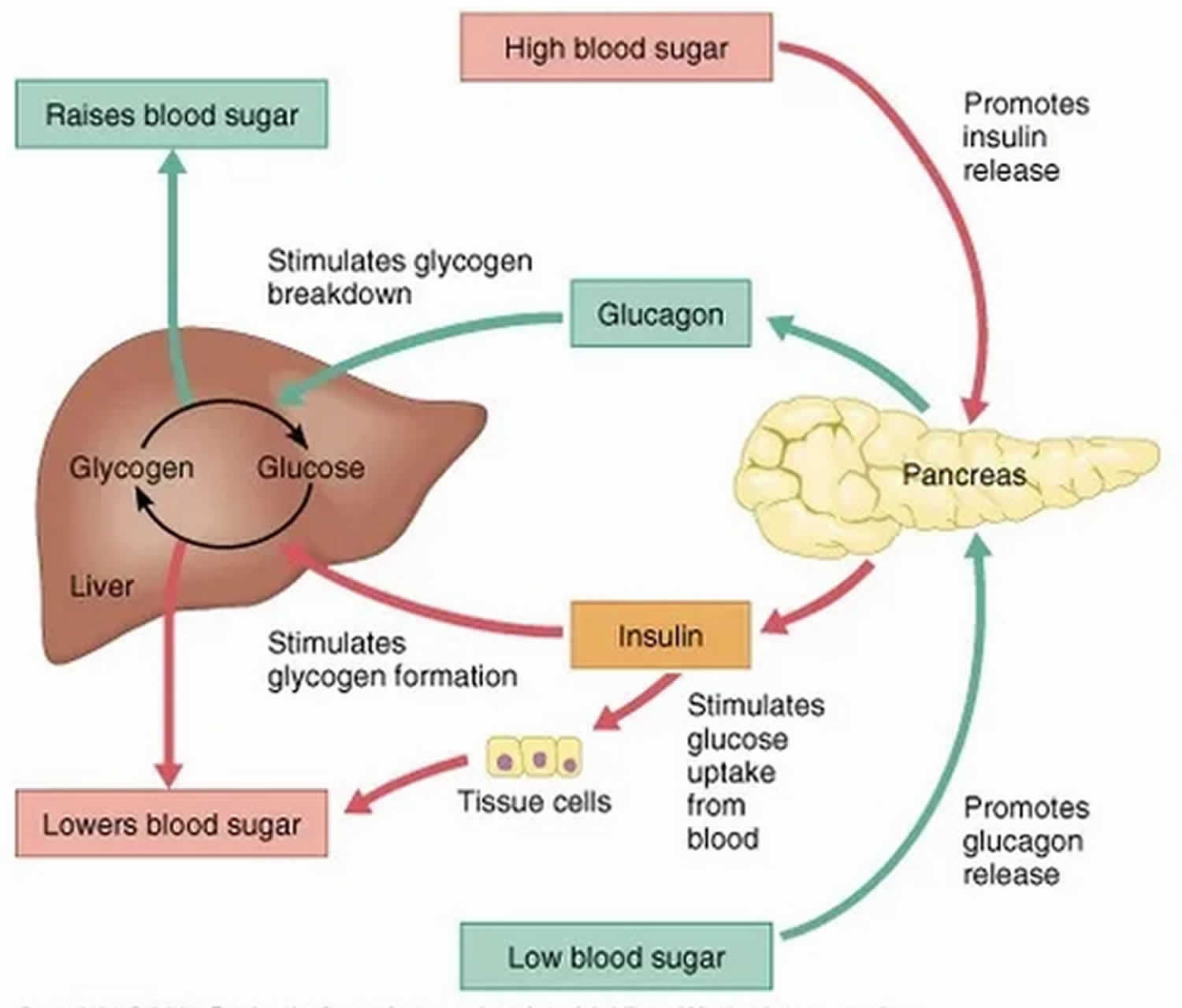
Glucose is the main energy source for your body, but it can’t enter the cells of most of your tissues without the help of insulin, a hormone secreted by your pancreas. When glucose levels rise, certain cells (beta cells) in your pancreas release insulin. This allows glucose to enter the cells and provide the fuel your cells need to function properly. Any extra glucose is stored in your liver and muscles in the form of glycogen.
If you haven’t eaten for several hours and your blood sugar level drops, another hormone from your pancreas called glucagon signals your liver to break down the stored glycogen and release glucose back into your bloodstream. This keeps your blood sugar level within a normal range until you eat again.
Aside from your liver breaking down glycogen into glucose, your body also has the ability to manufacture glucose. This process occurs primarily in your liver, but also in your kidneys.
How can I track my blood sugar?
There are two ways to keep track of your blood sugar levels:
- using a blood glucose meter to measure your blood sugar level at that moment
- getting an A1C at least twice a year to find out your average blood sugar for the past 2 to 3 months
What can make your blood sugar rise?
- Too much food, like a meal or snack with more carbohydrates than usual
- Not being active
- Not enough insulin or oral diabetes medications
- Side effects from other medications, such as steroids, anti-psychotic medications
- Illness – your body releases hormones to fight the illness, and those hormones raise blood sugar levels
- Stress, which can produce hormones that raise blood sugar levels
- Short- or long-term pain, like pain from a sunburn – your body releases hormones that raise sugar levels
- Menstrual periods, which cause changes in hormone levels
- Dehydration
What can make your blood sugar fall?
- Not enough food, like a meal or snack with fewer carbohydrates than usual, missing a meal or snack
- Alcohol, especially on an empty stomach
- Too much insulin or oral diabetes medications
- Side effects from other medications
- More physical activity or exercise than usual – physical activity makes your body more sensitive to insulin and can lower blood sugar.
How the liver regulates blood glucose levels
During absorption and digestion, the carbohydrates in the food you eat are reduced to their simplest form, glucose.
Excess glucose is then removed from the blood, with the majority of it being converted into glycogen, the storage form of glucose, by the liver’s hepatic cells via a process called glycogenesis.
When blood glucose concentration declines, the liver initiates glycogenolysis. The liver cells reconvert their glycogen stores into glucose, and continually release them into the blood until levels approach normal range.
However, when blood glucose levels fall during a long fast, the body’s glycogen stores dwindle and additional sources of blood sugar are required.
To help make up this shortfall, the liver, along with the kidneys, uses amino acids, lactic acid and glycerol to produce glucose. This process is known as gluconeogenesis.
The liver may also convert other sugars such as sucrose, fructose, and galactose into glucose if your body’s glucose needs not being met by your diet.
Ketones are alternative fuels that are produced by the liver from fats when sugar is in short supply.
When your body’s glycogen storage runs low, the body starts conserving the sugar supplies for the organs that always require sugar, including the brai, red blood cells and parts of the kidney. To supplement the limited sugar supply, the liver makes ketones in a process called ketogenesis.
Ketones are burned as fuel by muscle and other organs in the body, and the sugar is saved for the organs that need it.
Like glucose, the production of ketones in the liver is controlled by the hormone glucagon.
Hormones that regulates blood sugar
There are many hormones involved with glucose homeostasis. Hormones that are essential to regulate glucose level are the hormones insulin, which is the main regulator of sugar in your blood and glucagon. The main actions that insulin has are to allow glucose to enter cells to be used as energy and to maintain the amount of glucose found in the bloodstream within normal levels. Glucagon is produced to maintain glucose levels in the bloodstream when fasting and to raise very low glucose levels. Glucagon hormone increases blood glucose through increased glycogenolysis and gluconeogenesis. The effects of glucagon are the opposite of the effects induced by insulin. The two hormones need to work in partnership with each other to keep blood glucose levels balanced.
The others hormones that regulate blood glucose levels are:
- Somatostatin: Somatostatin is a hormone produced by many tissues in the body, principally in the nervous and digestive systems. It regulates a wide variety of physiological functions and inhibits the secretion of other hormones, including growth hormone, thyroid stimulating hormone, cholecystokinin and insulin. Somatostatin also inhibits the activity of the gastrointestinal tract and the rapid reproduction of normal and tumor cells. Somatostatin may also act as a neurotransmitter in the nervous system. Somatostatin decreases blood glucose levels through local suppression of glucagon release and suppression of gastrin and pituitary tropic hormones. This hormone also decreases insulin release; however, its net effect is a decrease in blood glucose levels.
- Cortisol: Cortisol is a steroid hormone, one of the glucocorticoids, made in the cortex of the adrenal glands and then released into the blood, which transports it all round your body. Almost every cell contains receptors for cortisol and so cortisol can have lots of different actions depending on which sort of cells it is acting upon, including metabolism and the immune response. Cortisol also has a very important role in helping the body respond to stress. Cortisol increases blood glucose levels via the stimulation of gluconeogenesis and through antagonism of insulin.
- Epinephrine (adrenaline): Epinephrine or adrenaline is a hormone released from the adrenal glands and its major action, together with noradrenaline, is to prepare the body for ‘fight or flight’. Epinephrine increases blood glucose levels through glycogenolysis (glucose liberation from glycogen) and increased fatty acid release from adipose tissues, which can then be catabolized and enter gluconeogenesis.
- Thyroxine: Thyroxine is the main hormone secreted into the bloodstream by the thyroid gland. It plays vital roles in digestion, heart and muscle function, brain development and maintenance of bones. Thyroxine increases blood glucose levels through glycogenolysis and increased absorption in the intestine.
- Growth hormone (somatotropin): Growth hormone is a small protein made in part of the brain called the pituitary gland. It travels in the bloodstream to all tissues in the body to stimulate growth. Growth hormone promotes gluconeogenesis, inhibits liver uptake of glucose, stimulates thyroid hormone, inhibits insulin.
- Adrenocorticotropic hormone (ACTH): Adrenocorticotropic hormone (ACTH) is a hormone produced in the anterior, or front, pituitary gland in the brain. Adrenocorticotropic hormone (ACTH) stimulates cortisol release from adrenal glands, stimulates the release of fatty acids from adipose tissue which can then feed into gluconeogenesis.
Insulin
Insulin is a hormone which plays a key role in the regulation of blood glucose levels. Insulin regulates how your body uses and stores glucose and fat. Many of the body’s cells rely on insulin to take glucose from the blood for energy. A lack of insulin or an inability to adequately respond to insulin, can each lead to the development of the symptoms of diabetes.
In addition to its role in controlling blood sugar levels, insulin is also involved in the storage of fat.
Insulin is a hormone made by an organ located behind the stomach called the pancreas. There are specialized areas within the pancreas called islets of Langerhans (the term insulin comes from the Latin insula that means island). The islets of Langerhans are made up of different type of cells that make hormones, the commonest ones are the beta cells, which produce insulin.
The release of insulin is tightly regulated in healthy people in order to balance food intake and the metabolic needs of the body. This is a complex process and other hormones found in the gut and pancreas also contribute to this blood glucose regulation. When you eat food, glucose is absorbed from your gut into the bloodstream, raising blood glucose levels. This rise in blood glucose causes insulin to be released from the pancreas so glucose can move inside the cells and be used. As glucose moves inside the cells, the amount of glucose in the bloodstream returns to normal and insulin release slows down. Proteins in food and other hormones produced by the gut in response to food also stimulate insulin release. Hormones released in times of acute stress, such as epinephrine (adrenaline), stop the release of insulin, leading to higher blood glucose levels to help cope with the stressful event.
Insulin works in tandem with glucagon, another hormone produced by the pancreas. While insulin’s role is to lower blood sugar levels if needed, glucagon’s role is to raise blood sugar levels if they fall too low. Using this system, the body ensures that the blood glucose levels remain within set limits, which allows the body to function properly.
Insulin and blood glucose levels
Insulin helps control blood glucose levels by signaling the liver and muscle and fat cells to take in glucose from the blood. Insulin therefore helps cells to take in glucose to be used for energy.
If the body has sufficient energy, insulin signals the liver to take up glucose and store it as glycogen.
The liver can store up to around 5% of its mass as glycogen.
Some cells in the body can take glucose from the blood without insuli, but most cells do require insulin to be present.
Synthetic insulin
People with type 1 diabetes and a proportion of people with type 2 diabetes will need to take exogenous insulin (insulin that is not produced by one’s own body). Insulin is usually injected but can also be delivered by an insulin pump which continually infuses insulin through the day and night.
Synthetic insulin is made in laboratories and is the most commonly prescribed form of insulin for medication purposes. Non-synthetic animal insulin is also available in the US if preferred.
What happens if I have too much insulin?
If a person accidentally injects more insulin than required, e.g. because they expend more energy or eat less food than they anticipated, cells will take in too much glucose from the blood. This leads to abnormally low blood glucose levels (called hypoglycaemia). The body reacts to hypoglycaemia by releasing stored glucose from the liver in an attempt to bring the levels back to normal. Low glucose levels in the blood can make a person feel ill.
The body mounts an initial ‘fight back’ response to hypoglycaemia through a specialised set of of nerves called the sympathetic nervous system. This causes palpitations, sweating, hunger, anxiety, tremor and pale complexion that usually warn the person about the low blood glucose level so this can be treated. However, if the initial blood glucose level is too low or if it is not treated promptly and continues to drop, the brain will be affected too because it depends almost entirely on glucose as a source of energy to function properly. This can cause dizziness, confusion, fits and even coma in severe cases.
Some drugs used for people with type 2 diabetes, including sulphonylureas (e.g. gliclazide) and meglitinides (e.g. repaglinide), can also stimulate insulin production within the body and can also cause hypoglycaemia. The body responds in the same way as if excess insulin has been given by injection.
Furthermore, there is a rare tumour called an insulinoma that occurs with an incidence of 1-4 per million population. It is a tumour of the beta cells in the pancreas. Patients with this type of tumour present with symptoms of hypoglycaemia.
What happens if I have too little insulin?
People with diabetes have problems either making insulin, how that insulin works or both. The main two types of diabetes are type 1 and type 2 diabetes, although there are other more uncommon types.
People with type 1 diabetes produce very little or no insulin at all. This condition is caused when the beta cells that make insulin have been destroyed by antibodies (these are usually substances released by the body to fight against infections), hence they are unable to produce insulin. With too little insulin, the body can no longer move glucose from the blood into the cells, causing high blood glucose levels. If the glucose level is high enough, excess glucose spills into the urine. This drags extra water into the urine causing more frequent urination and thirst. This leads to dehydration, which can cause confusion. In addition, with too little insulin, the cells cannot take in glucose for energy and other sources of energy (such as fat and muscle) are needed to provide this energy. This makes the body tired and can cause weight loss. If this continues, patients can become very ill. This is because the body attempts to make new energy from fat and causes acids to be produced as waste products. Ultimately, this can lead to coma and death if medical attention is not sought. People with type 1 diabetes will need to inject insulin in order to survive.
Type 2 diabetes can be caused by two main factors and its severity will depend on how advanced it is. Firstly, the patient’s beta cells may have problems manufacturing insulin, so although some insulin is produced, it is not enough for the body’s needs. Secondly, the available insulin doesn’t work properly because the areas in the cell where insulin acts, called insulin receptors, become insensitive and stop responding to the insulin in the bloodstream. These receptors appear to malfunction more in people who carry excessive amount of weight. Some people with type 2 diabetes might initially experience very few symptoms and the raised blood glucose is only picked up when a routine blood test is arranged for another reason; other people might experience symptoms similar to those seen in patients with type 1 diabetes (thirst, frequent urination, dehydration, hunger, fatigue and weight loss). Some patients with type 2 diabetes can control their symptoms by improving their diet and/or losing weight, some will need tablets, and others will need to inject insulin to improve blood glucose levels. See the article on diabetes mellitus for more information.
Insulin and type 1 diabetes
In type 1 diabetes, the body produces insufficient insulin to regulate blood glucose levels.
Without the presence of insuli, many of the body’s cells cannot take glucose from the blood and therefore the body uses other sources of energy.
Ketones are produced by the liver as an alternative source of energy, however, high levels of the ketones can lead to a dangerous condition called ketoacidosis (diabetic ketoacidosis or DKA).
People with type 1 diabetes will need to inject insulin to compensate for their body’s lack of insulin.
Insulin and type 2 diabetes
Type 2 diabetes is characterized by the body not responding effectively to insulin. This is termed insulin resistance. As a result the body is less able to take up glucose from the blood. In the earlier stages of type 2 diabetes, the body responds by producing more insulin than it would normally need to.
If type 2 diabetes develops over a number of years, the extra demands on the pancreas to produce insulin can lead to a loss of insulin producing cells (known as pancreatic beta cells) as they wear out.
Depending on their level of insulin resistance, people with type 2 diabetes may also need to take insulin injections to manage their blood sugar levels.
Insulin and fat storage
As well as being involved in the regulation of blood glucose, insulin is also involved in how fat is used by the body. When the liver is has taken up its capacity of glycogen, insulin signals fat cells to take up glucose to be stored as triglycerides.
An additional effect of insulin is in inhibiting the breakdown of fats.
Glucagon
Glucagon is a hormone that is involved in controlling blood sugar (glucose) levels. Glucagon is a hormone that is produced by the alpha cells, found in the islets of Langerhans, in the pancreas, from where it is released into the bloodstream. The glucagon-secreting alpha cells surround the insulin-secreting beta cells, which reflects the close relationship between the two hormones. Glucagon plays an active role in allowing your body to regulate the utilization of glucose and fats.
Glucagon’s role in the body is to prevent blood glucose levels dropping too low. To do this, it acts on the liver in several ways:
- Glucagon stimulates the conversion of stored glycogen (stored in the liver) to glucose, which can be released into the bloodstream. This process is called glycogenolysis.
- Glucagon promotes the conversion of amino acids into glucose. This process is called gluconeogenesis.
- Glucagon reduces glucose consumption by the liver so that as much glucose as possible can be secreted into the bloodstream to maintain blood glucose levels.
Glucagon also acts on adipose tissue to stimulate the breakdown of stored fat (triglycerides) into fatty acids into the bloodstream for use as fuel by cells.
Glucagon is released in response to low blood glucose levels and to events whereby the body needs additional glucose, such as in response to vigorous exercise.
Glucagon and blood glucose levels
Glucagon serves to keep blood glucose levels high enough for the body to function well.
When blood glucose levels are low, glucagon is released and signals the liver to release glucose into the blood.
Glucagon secretion in response to meals varies depending on what you eat:
- In response to a carbohydrate based meal, glucagon levels in the blood fall to prevent blood glucose rising too high.
- In response to a high protein meal, glucagon levels in the blood rise.
How is glucagon controlled?
Glucagon works along with the hormone insulin to control blood sugar levels and keep them within set levels. Glucagon is released to stop blood sugar levels dropping too low (hypoglycemia), while insulin is released to stop blood sugar levels rising too high (hyperglycemia).
The release of glucagon is stimulated by low blood glucose, protein-rich meals and adrenaline (another important hormone for combating low glucose). The release of glucagon is prevented by raised blood glucose and carbohydrate in meals, detected by cells in the pancreas.
In the longer-term, glucagon is crucial to the body’s response to lack of food. For example, it encourages the use of stored fat for energy in order to preserve the limited supply of glucose.
What happens if I have too much glucagon?
A rare tumor of the pancreas called a glucagonoma can secrete excessive quantities of glucagon. This can cause diabetes mellitus, weight loss, thrombosis, venous thrombosis and a characteristic skin rash.
What happens if I have too little glucagon?
Unusual cases of deficiency of glucagon secretion have been reported in babies. This results in severely low blood glucose which cannot be controlled without administering glucagon.
Glucagon in diabetes
In people with diabetes, glucagon’s presence can raise blood glucose levels too high.
The reason for this is either because not enough insulin is present or as is the case in type 2 diabetes, the body is less able to respond to insulin.
In type 1 diabetes , high levels of circulating insulin can inhibit the release of glucagon in response to hypoglycemia.
Medications which affect glucagon secretion
A number of medications have been developed to help modify the release of glucagon in type 2 diabetes.
Two different classes of diabetes drugs, DPP-4 inhibitors and incretin mimetics, act in response to the presence of meals to stimulate the increase of insulin and to inhibit the release of glucagon.
Glucagon injections
Glucagon can be administered by injection in response to severe episodes of hypoglycemia. Glucagon is useful for people treating their diabetes with insulin. Glucagon can be given by injection to restore blood glucose lowered by insulin (even in unconscious patients). It can increase glucose release from glycogen stores more than insulin can suppress it. The effect of glucagon is limited, so it is very important to eat a carbohydrate meal once the person has recovered enough to eat safely.