What is brachytherapy
Brachytherapy is an internal radiation therapy or radiotherapy in which radioactive material sealed in needles, seeds, wires, or catheters is placed directly into or near a tumor. Getting the implant placed is usually a painless procedure. Depending on your type of cancer and treatment plan, you might get a temporary or a permanent implant.
Brachytherapy or internal radiation therapy allows a higher dose of radiation in a smaller area than might be possible with external radiation treatment. Brachytherapy uses a radiation source that’s usually sealed in a small holder called an implant. Different types of implants may be called pellets, seeds, ribbons, wires, needles, capsules, balloons, or tubes. No matter which type of implant is used, it is placed in your body, very close to or inside the tumor. This way the radiation harms as few normal cells as possible.
- During intracavitary radiation, the radioactive source is placed in a body cavity (space), such as the rectum or uterus.
- With interstitial radiation, the implants are placed in or near the tumor, but not in a body cavity.
How your doctor places that radioactive material in your body depends on many factors, including the location and extent of the cancer, your overall health, and your treatment goals.
Some brachytherapy treatments are given using specialist applicators. The applicators are hollow tubes that the doctor puts into or as close to the area of cancer as possible.
There are different types of applicator for different areas of the body. You have the applicators inserted in the operating room. You either have a general anaesthetic or a spinal anaesthetic. A spinal anaesthetic means you have no feeling from below your waist.
One or more radioactive metal pellets travel out of the machine, into the applicators. The metal gives a dose of radiotherapy in the area of the cancer. You might have more than one treatment.
Some treatments use radioactive seeds. Using specialised needles, the doctor puts the seeds in the area of the cancer. The seeds stay there permanently. They are tiny and don’t cause any problems.
Placement may be inside a body cavity or in body tissue:
- Radiation placed inside a body cavity. During intracavity brachytherapy, a device containing radioactive material is placed in a body opening, such as the windpipe or the vagina. The device may be a tube or cylinder made to fit the specific body opening. Your radiation therapy team may place the brachytherapy device by hand or may use a computerized machine to help place the device.Imaging equipment, such as a CT scanner or ultrasound machine, may be used to ensure the device is placed in the most effective location.
- Radiation inserted into body tissue. During interstitial brachytherapy, devices containing radioactive material are placed within body tissue, such as within the breast or prostate. Devices that deliver interstitial radiation into the treatment area include wires, balloons and tiny seeds the size of grains of rice. A number of techniques are used for inserting the brachytherapy devices into body tissue. Your radiation therapy team may use needles or special applicators. These long, hollow tubes are loaded with the brachytherapy devices, such as seeds, and inserted into the tissue where the seeds are released. In some cases, narrow tubes (catheters) may be placed during surgery and later filled with radioactive material during brachytherapy sessions. CT scans, ultrasound or other imaging techniques may be used to guide the devices into place and to ensure they’re positioned in the most-effective locations.
Brachytherapy side effects
Side effects of brachytherapy are specific to the area being treated. Because brachytherapy focuses radiation in a small treatment area, only that area is affected.
You may experience tenderness and swelling in the treatment area. Ask your doctor what other side effects can be expected from your treatment.
Brachytherapy procedure
Before you begin brachytherapy, you may meet with a doctor who specializes in treating cancer with radiation (radiation oncologist). You may also undergo scans to help your doctor determine your treatment plan.
Procedures such as X-rays, computerized tomography (CT) or magnetic resonance imaging (MRI) may be performed before brachytherapy.
The brachytherapy implant procedure is usually done in a hospital operating room designed to keep the radiation inside the room. You’ll get anesthesia, which may be either general (where drugs are used to put you into a deep sleep so that you don’t feel pain) or local (where part of your body is numbed).
One or more radioactive implants is put into your body cavity or tissue with an applicator, usually a metal tube or a plastic tube called a catheter. Imaging tests (an x-ray, ultrasound, MRI, or CT scan) are usually used during the procedure to find the exact place the implant needs to go.
Before being placed, implants are kept in containers that hold the radiation inside so it can’t affect others. The health professionals handling the radioactive implants may wear special gear that protects them from exposure once the implants are taken out of the container.
HDR brachytherapy
HDR (high-dose-rate) brachytherapy is often an outpatient procedure, which means each treatment session is brief and doesn’t require that you be admitted to the hospital. High-dose-rate brachytherapy allows a person to be treated for only a few minutes up to 20 minutes at a time with a powerful radioactive source that’s put in the applicator. The source is removed after several minutes. This may be repeated over the course of a few days to weeks. The radioactive material is not left in your body. The applicator might be left in place between treatments, or it might be put in before each treatment.
You’ll lie in a comfortable position during high-dose-rate brachytherapy. Your radiation therapy team will position the radiation device. This may be a simple tube or tubes placed inside a body cavity or small needles inserted into the tumor.
The radioactive material is inserted into the brachytherapy device with the help of a computerized machine.
Your radiation therapy team will leave the room during your brachytherapy session. They’ll observe from a nearby room where they can see and hear you.
You shouldn’t feel any pain during brachytherapy, but if you feel uncomfortable or have any concerns, be sure to tell your caregivers.
Once the radioactive material is removed from your body, you won’t give off radiation or be radioactive. You aren’t a danger to other people, and you can go on with your usual activities.
Low-dose-rate brachytherapy
In low-dose-rate (LDR) brachytherapy, the implant gives off lower doses of radiation over a longer period – from several hours to several days.
Some implants are left in from 1 to a few days and then removed. You’ll probably have to stay in the hospital, sometimes in a special room, during treatment. For larger implants, you might have to stay in bed and lie still to keep it from moving.
Some smaller implants (such as the seeds or pellets) are left in place – they’re never taken out. Over the course of several weeks they stop giving off radiation. The seeds are about the size of rice grains and rarely cause problems. If your implants are to be left in, you may be able to go home the same day they’re put in.
Radioactive material is placed in your body by hand or by machine. Brachytherapy devices may be positioned during surgery, which may require anesthesia or sedation to help you remain still during the procedure and to reduce discomfort.
You’ll likely stay in a private room in the hospital during low-dose-rate brachytherapy. Because the radioactive material stays inside your body, there is a small chance it could harm other people. For this reason, visitors will be restricted.
Children and pregnant women shouldn’t visit you in the hospital. Others may visit briefly once a day or so. Your health care team will still give you the care you need, but may restrict the amount of time they spend in your room.
You shouldn’t feel pain during low-dose-rate brachytherapy. Keeping still and remaining in your hospital room for days may be uncomfortable. If you feel any discomfort, tell your health care team.
After a designated amount of time, the radioactive material is removed from your body. Once brachytherapy treatment is complete, you’re free to have visitors without restrictions.
Permanent brachytherapy
In some cases, such as with prostate cancer brachytherapy, radioactive material is placed in your body permanently.
The radioactive material is typically placed by hand with the guidance of an imaging test, such as ultrasound or CT. You may feel pain during the placement of radioactive material, but you shouldn’t feel any discomfort once it’s in place.
Your body will emit low doses of radiation from the area being treated at first. Usually the risk to others is minimal and may not require any restrictions about who can be near you.
In some cases, for a short period of time you may be asked to limit the length and frequency of visits with pregnant women or with children. The amount of radiation in your body will diminish with time, and restrictions will be discontinued.
How long do brachytherapy implants stay in place?
The length of time a brachytherapy implant is left in place depends on the type of brachytherapy you are getting. Some implants are permanent, while others are taken out after a few minutes or days. The type of implant you get will depend on the kind of cancer, where it is in your body, your general health, and other treatments you have had.
How will I feel during brachytherapy implant therapy?
You’re not likely to have a lot of pain or feel sick while implants are being put in. The drugs used while they’re being placed might make you feel drowsy, weak, or sick to your stomach, but these side effects don’t last long. If your brachytherapy implant is held in place by an applicator, you may have some discomfort in that area. Ask for medicine to help you relax or to relieve pain if needed. Be sure to tell your cancer care team if you have burning, sweating, or other symptoms.
What happens after a temporary brachytherapy implant is removed?
In most cases, anesthesia is not needed when the applicator and/or implant is removed. It’s usually done right in your hospital room. The treated area may be sore or tender for some time after treatment, but most people can return to normal activities quickly. Keep in mind that your body is recovering from radiation treatments, and you may need extra sleep or rest breaks over the next few days.
What happens to permanent brachytherapy implants?
The radioactive materials stop giving off radiation over time. It may take weeks or months. Talk to your cancer care team about how long it will take in your case. Once the radiation is gone, the implant(s) are no longer active. They usually stay in place and cause no harm, so there’s no need to take them out.
Will I be radioactive during or after internal radiation treatment?
With brachytherapy, your body may give off a small amount of radiation for a short time.
If you have a temporary implant, you’ll be asked to stay in the hospital and might have to limit visitors during treatment. You also may be asked to stay a certain distance away from them. Pregnant women and children might not be allowed to visit you. Once the implant is removed, your body will no longer give off radiation.
Over a few weeks to months, permanent implants will slowly stop giving off radiation. The radiation usually doesn’t travel much farther than the area being treated, so the chances that others could be exposed to radiation is very small. Still, your health care team might ask you to take certain precautions such as staying away from small children and pregnant women, especially right after you get the implants.
Brachytherapy for breast cancer
If you’ve been diagnosed with breast cancer, your cancer care team will discuss your treatment options with you. It’s important that you think carefully about each of your choices.
Some women with breast cancer will need radiation, often in addition to other treatments. The need for radiation depends on what type of surgery you had, whether your cancer has spread to the lymph nodes or somewhere else in your body, and in some cases, your age. Tumors that are large or involve the skin might also need radiation. You could have just one type of radiation, or a combination of different types.
Radiation therapy is treatment with high-energy rays (such as x-rays) or particles that destroy cancer cells. Two main types of radiation therapy can be used to treat breast cancer:
- External beam radiation: This is the most common type of radiation therapy for women with breast cancer. A machine outside the body focuses the radiation on the area affected by the cancer.
- Internal radiation (brachytherapy): For this treatment, a radioactive source is put inside the body for a short time.
Brachytherapy, also known as internal radiation, is another way to deliver radiation therapy. Instead of aiming radiation beams from outside the body, a device containing radioactive seeds or pellets is placed into the breast tissue for a short time in the area where the cancer had been removed.
When might radiation therapy be used for breast cancer?
Not all women with breast cancer need radiation therapy, but it may be used in several situations:
- After breast-conserving surgery, to help lower the chance that the cancer will come back in the breast or nearby lymph nodes.
- After a mastectomy, especially if the cancer was larger than 5 cm (about 2 inches), or if cancer is found in the lymph nodes.
- If cancer has spread to other parts of the body, such as the bones or brain.
For women who had breast-conserving surgery, brachytherapy can be used along with external beam radiation as a way to add an extra boost of radiation to the tumor site. It may also be used by itself (instead of radiation to the whole breast) as a form of accelerated partial breast irradiation. Tumor size, location, and other factors may limit who can get brachytherapy.
Types of brachytherapy for breast cancer
There are different types of brachytherapy:
- Interstitial brachytherapy: In this approach, several small, hollow tubes called catheters are inserted into the breast around the area where the cancer was removed and are left in place for several days. Radioactive pellets are inserted into the catheters for short periods of time each day and then removed. This method of brachytherapy has been around longer (and has more evidence to support it), but it is not used as much anymore.
- Intracavitary brachytherapy: This is the most common type of brachytherapy for women with breast cancer. A device is put into the space left from BCS and is left in place until treatment is complete. There are several different devices available (including MammoSite, SAVI, Axxent, and Contura), most of which require surgical training for proper placement . They all go into the breast as a small catheter (tube). The end of the device inside the breast is then expanded so that it stays securely in place for the entire treatment. The other end of the catheter sticks out of the breast. For each treatment, one or more sources of radiation (often pellets) are placed down through the tube and into the device for a short time and then removed. Treatments are typically given twice a day for 5 days as an outpatient. After the last treatment, the device is collapsed down again and removed.
Early studies of intracavitary brachytherapy as the only radiation after BCS have had promising results as far as having at least equal cancer control compared with standard whole breast radiation, but may have more complications including poor cosmetic results. Studies of this treatment are being done and more follow-up is needed.
Intracavitary brachytherapy for breast cancer side effects
As with external beam radiation, intracavitary brachytherapy can have side effects, including:
- Redness at the treatment site
- Bruising at the treatment site
- Breast pain
- Infection
- Damage to fatty tissue in the breast
- Weakness and fracture of the ribs in rare cases
- Fluid collecting in the breast (seroma)
Brachytherapy cervical cancer
If you’ve been diagnosed with cervical cancer, your cancer care team will talk with you about treatment options. In choosing your treatment plan, you and your cancer care team will also take into account your age, your overall health, and your personal preferences.
The stage of a cervical cancer is the most important factor in choosing treatment. But other factors can also affect your treatment options, including the exact location of the cancer within the cervix, the type of cancer (squamous cell or adenocarcinoma), your age and overall health, and whether you want to have children.
Radiation therapy uses high energy x-rays or radioactive particles to kill cancer cells. Radiation therapy may be used for cervical cancer:
- As a part of the main treatment. For some stages of cervical cancer, the preferred treatment is radiation alone or surgery followed by radiation. For other stages, radiation and chemo given together (called concurrent chemoradiation) is the preferred treatment. The chemo helps the radiation work better.
- To treat cervical cancer that has spread or that has come back after treatment. Radiation therapy may be used to treat cancers that have spread to other organs and tissues.
The two types of radiation therapy most often used to treat cervical cancer include:
- External beam radiation
- Brachytherapy
Brachytherapy used most often to treat cervical cancer is known as intracavitary brachytherapy. The radiation source is placed in a device in the vagina (and sometimes in the cervix). This is often used in addition to external beam radiation therapy as a part of the main treatment for cervical cancer.
There are two types of brachytherapy:
- Low-dose rate (LDR) brachytherapy is completed over a few days. During this time, the patient stays in bed in a private room in the hospital with instruments holding the radioactive material in place. While the radiation therapy is being given, the hospital staff will care for you, but also take precautions to lessen their own radiation exposure.
- High-dose rate (HDR) brachytherapy is done as an outpatient over several treatments (often at least a week apart). For each high-dose treatment, the radioactive material is inserted for a few minutes and then removed. The advantage of HDR treatment is that you do not have to stay in the hospital or stay still for long periods of time.
To treat cervical cancer in women who have had a hysterectomy, the radioactive material is placed in a tube in the vagina.
To treat a woman who still has a uterus, the radioactive material can be placed in a small metal tube (called a tandem) that goes in the uterus, along with small round metal holders (ovoids) placed near the cervix. This is sometimes called tandem and ovoid treatment. Another option is called tandem and ring. For this, a round holder (like a disc) is placed close to the uterus. The choice of which one to use depends on what type of brachytherapy is planned.
Brachytherapy for cervical cancer side effects
Since the radiation only travels a short distance with brachytherapy, the main effects of the radiation are on the cervix and the walls of the vagina. The most common side effect is irritation of the vagina. It may become red and sore, and there may be a discharge. The vulva may become irritated as well.
Brachytherapy can also cause many of the same side effects as external beam radiation therapy, such as fatigue, diarrhea, nausea, irritation of the bladder, and low blood counts. Often brachytherapy is given right after external beam radiation (before the side effects can go away), so it can be hard to know which type of treatment is causing the side effect.
Long-term side effects of radiation therapy
Vaginal stenosis: Both external beam radiation therapy and brachytherapy can cause scar tissue to form in the vagina. The scar tissue can make the vagina narrower (called vaginal stenosis), less able to stretch, or even shorter, which can make vaginal sex painful.
A woman can help prevent this problem by stretching the walls of her vagina several times a week, either by having sex or by using a vaginal dilator (a plastic or rubber tube used to stretch out the vagina).
Vaginal dryness: Vaginal dryness and painful sex can be long-term side effects from radiation (both brachytherapy and external beam radiation therapy). Estrogens used locally may help with vaginal dryness and changes to the vaginal lining, especially if radiation to the pelvis damaged the ovaries, causing early menopause. These hormones are typically applied into the vagina and absorbed into the genital area, rather than taken by mouth. They come in gel, cream, ring, and tablet forms.
Weakened bones: Radiation to the pelvis can weaken the bones, leading to fractures. Hip fractures are the most common, and might occur 2 to 4 years after radiation. Bone density tests are recommended to monitor the risk of fracture.
Swelling of the leg(s): If pelvic lymph nodes are treated with radiation, it can lead to fluid drainage problems in the leg. This can cause severe swelling in the leg, a condition called lymphedema. More information about lymphedema can be found in our section on Lymphedema
If you are having side effects from radiation treatment, discuss them with your cancer care team.
It is important to know that smoking increases the side effects from radiation and can make treatment less effective. If you smoke, you should stop.
Brachytherapy for prostate cancer
Depending on each case, treatment options for men with prostate cancer might include:
- Watchful waiting or active surveillance
- Surgery
- Radiation therapy
- Cryotherapy (cryosurgery)
- Hormone therapy
- Chemotherapy
- Vaccine treatment
- Bone-directed treatment
These treatments are generally used one at a time, although in some cases they may be combined.
When is radiation therapy used in prostate cancer?
Radiation may be used:
- As the first treatment for cancer that is still just in the prostate gland and is low grade. Cure rates for men with these types of cancers are about the same as those for men treated with radical prostatectomy.
- As part of the first treatment (along with hormone therapy) for cancers that have grown outside the prostate gland and into nearby tissues.
- If the cancer is not removed completely or comes back (recurs) in the area of the prostate after surgery.
- If the cancer is advanced, to help keep the cancer under control for as long as possible and to help prevent or relieve symptoms.
Types of radiation therapy
The 2 main types of radiation therapy used for prostate cancer are:
- External beam radiation
- Brachytherapy (internal radiation)
Radiopharmaceuticals are drugs that contain radioactive elements. They are injected into a vein and settle in areas of damaged bones (like those containing cancer spread). Once there, they give off radiation that kills cancer cells. These drugs can be used to treat prostate cancer that has spread to many bones. Unlike external beam radiation, these drugs can reach all the affected bones at the same time.
The radiopharmaceuticals that can be used to treat prostate cancer spread to bone include:
- Strontium-89 (Metastron)
- Samarium-153 (Quadramet)
- Radium-223 (Xofigo)
All of these drugs can help relieve pain caused by bone metastases. Radium-223 has also been shown to help men who have prostate cancer spread only to their bones (as opposed to spread to other organs such as the lungs) to live longer. For these men, radium-223 may be an early part of treatment.
The major side effect of these drugs is a decrease in blood cell counts, which could increase risks for infections or bleeding, especially if your counts are already low. Other side effects have also been seen, so ask your doctor what you can expect.
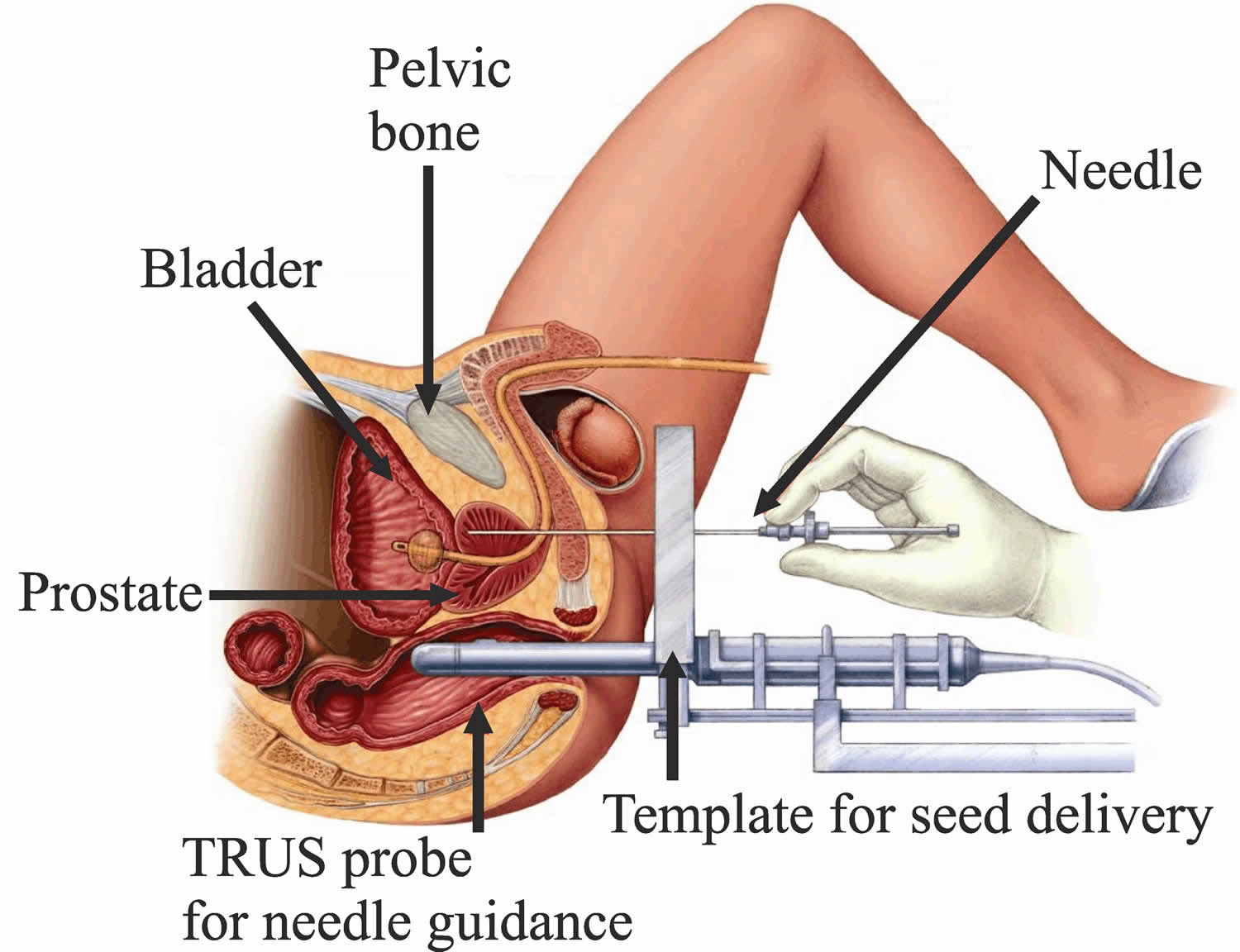
Brachytherapy (also called seed implantation or interstitial radiation therapy) uses small radioactive pellets, or “seeds,” each about the size of a grain of rice. These pellets are placed directly into your prostate.
- Brachytherapy alone is generally used only in men with early-stage prostate cancer that is relatively slow growing (low-grade).
- Brachytherapy combined with external radiation is sometimes an option for men who have a higher risk of the cancer growing outside the prostate.
The use of brachytherapy is also limited by some other factors. For men who have had a transurethral resection of the prostate (TURP) or for those who already have urinary problems, the risk of urinary side effects may be higher. Brachytherapy might not work as well in men with large prostate glands because it might not be possible to place the seeds into all of the correct locations. One way to get around this may be to get a few months of hormone therapy beforehand to shrink the prostate.
Imaging tests such as transrectal ultrasound, CT scans, or MRI are used to help guide the placement of the radioactive pellets. Special computer programs calculate the exact dose of radiation needed.
Types of prostate cancer brachytherapy
There are 2 types of prostate brachytherapy. Both are done in an operating room. You will get either spinal anesthesia (where the lower half of your body is numbed) or general anesthesia (where you are asleep), and you might need to stay in the hospital overnight.
Permanent (low dose rate, or LDR) brachytherapy
In this approach, pellets (seeds) of radioactive material (such as iodine-125 or palladium-103) are placed inside thin needles, which are inserted through the skin in the area between the scrotum and anus and into the prostate. The pellets are left in place as the needles are removed and give off low doses of radiation for weeks or months. Radiation from the seeds travels a very short distance, so the seeds can give off a large amount of radiation in a very small area. This limits the amount of damage to nearby healthy tissues.
Usually, around 100 seeds are placed, but this depends on the size of the prostate. Because the seeds are so small, they seldom cause discomfort, and are simply left in place after their radioactive material is used up.
You may also get external beam radiation along with brachytherapy, especially if there is a higher risk that your cancer has spread outside the prostate (for example, if you have a higher Gleason score).
Temporary (high dose rate, or HDR) brachytherapy
This technique is done less often. It uses higher doses of radiation that are left in place for a short time. Hollow needles are placed through the skin between the scrotum and anus and into the prostate. Soft nylon tubes (catheters) are placed in these needles. The needles are then removed but the catheters stay in place. Radioactive iridium-192 or cesium-137 is then placed in the catheters, usually for 5 to 15 minutes. Generally, about 3 brief treatments are given over 2 days, and the radioactive substance is removed each time. After the last treatment the catheters are removed. For about a week after treatment, you may have some pain or swelling in the area between your scrotum and rectum, and your urine may be reddish-brown.
These treatments are usually combined with external beam radiation given at a lower dose than if used by itself. The advantage of this approach is that most of the radiation is concentrated in the prostate itself, sparing nearby normal tissues.
Brachytherapy prostate cancer side effects
Radiation precautions: If you get permanent (low dose rate) brachytherapy, the seeds will give off small amounts of radiation for several weeks or months. Even though the radiation doesn’t travel far, your doctor may advise you to stay away from pregnant women and small children during this time. If you plan on traveling, you might want to get a doctor’s note regarding your treatment, as low levels of radiation can sometimes be picked up by detection systems at airports.
There’s also a small risk that some of the seeds might move (migrate). You may be asked to strain your urine for the first week or so to catch any seeds that might come out. You may be asked to take other precautions as well, such as wearing a condom during sex. Be sure to follow any instructions your doctor gives you. There have also been reports of the seeds moving through the bloodstream to other parts of the body, such as the lungs. As far as doctors can tell, this is uncommon and doesn’t seem to cause any ill effects.
These precautions aren’t needed after HDR brachytherapy, because the radiation doesn’t stay in the body after treatment.
Bowel problems: Brachytherapy can sometimes irritate the rectum and cause a condition called radiation proctitis. Bowel problems such as rectal pain, burning, and/or diarrhea (sometimes with bleeding) can occur, but serious long-term problems are uncommon.
Urinary problems: Severe urinary incontinence (trouble controlling urine) is not a common side effect. But some men have problems with frequent urination or other symptoms due to irritation of the urethra, the tube that drains urine from the bladder. This tends to be worse in the weeks after treatment and gets better over time. Rarely, the urethra may actually close off (known as a urethral stricture) and need to be opened with a catheter or surgery.
Erection problems: Some studies have found rates of erection problems to be lower after brachytherapy, but other studies have found that the rates were no lower than with external beam radiation or surgery. The younger you are and the better your sexual function before treatment, the more likely you will be to regain function after treatment.
Erection problems can often be helped by treatments such as those listed in the surgery section, including medicines.