What is calcium pantothenate
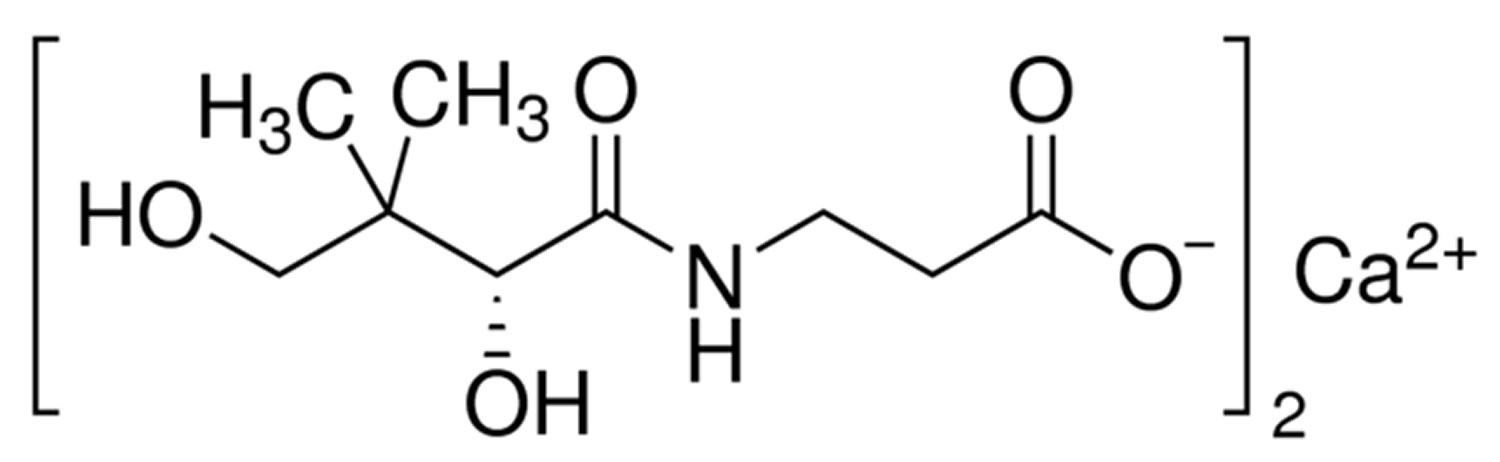
Calcium pantothenate is the calcium salt of the water-soluble vitamin B5 (pantothenic acid), ubiquitously found in plants and animal tissues with antioxidant property. Vitamin B5 (pantothenic acid) is an essential nutrient that is naturally present in some foods, added to others, and available as a dietary supplement. The main function of this water-soluble B vitamin is in the synthesis of coenzyme A (CoA) and acyl carrier protein 1. Pentothenate is a component of coenzyme A (CoA) and a part of the vitamin B2 complex. Calcium pantothenate is a butyryl-beta-alanine that can also be viewed as pantoic acid complexed with beta alanine. Calcium pantothenate is used in the synthesis of coenzyme A (CoA) and protects cells against peroxidative damage by increasing the level of glutathione. Coenzyme A (CoA) may act as an acyl group carrier to form acetyl-CoA and other related compounds; this is a way to transport carbon atoms within the cell 2. Coenzyme A (CoA) is important in energy metabolism for pyruvate to enter the tricarboxylic acid cycle (Kreb cycle) as acetyl-CoA, and for α-ketoglutarate to be transformed to succinyl-CoA in the cycle 3. Coenzyme A (CoA) is essential for fatty acid synthesis and degradation, transfer of acetyl and acyl groups, and a multitude of other anabolic and catabolic processes 4. Acyl carrier protein’s main role is in fatty acid synthesis 5. Vitamin B5 (pantothenic acid) is a growth factor and is essential for various metabolic functions, including the metabolism of carbohydrates, proteins, and fatty acids. This vitamin is also involved in the synthesis of cholesterol, lipids, neurotransmitters, steroid hormones, and hemoglobin.
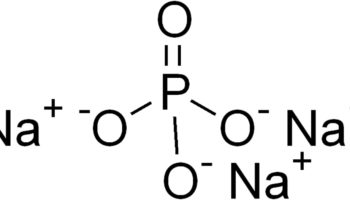
Figure 1. Calcium pantothenate formula
Vitamin B5 is commercially available as D-pantothenic acid, as well as dexpanthenol and calcium pantothenate, which are chemicals made in the lab from D-pantothenic acid.
Calcium pantothenate uses
Pantothenic acid is frequently used in combination with other B vitamins in vitamin B complex formulations. Vitamin B complex generally includes vitamin B1 (thiamine), vitamin B2 (riboflavin), vitamin B3 (niacin/niacinamide), vitamin B5 (pantothenic acid), vitamin B6 (pyridoxine), vitamin B12 (cyanocobalamin), and folic acid. However, some products do not contain all of these ingredients and some may include others, such as biotin, para-aminobenzoic acid (PABA), choline bitartrate, and inositol.
Pantothenic acid has a long list of uses, although there isn’t enough scientific evidence to determine whether it is effective for most of these uses. People take pantothenic acid for treating dietary deficiencies, acne, alcoholism, allergies, baldness, asthma, attention deficit-hyperactivity disorder (ADHD), autism, burning feet syndrome, yeast infections, heart failure, carpal tunnel syndrome, breathing problems, celiac disease, colitis, pink eye (conjunctivitis), seizures, and bladder infections. It is also taken by mouth for dandruff, depression, diabetic nerve pain, enhancing immune function, improving athletic performance, tongue infections, gray hair, headache, hyperactivity, low blood sugar, trouble sleeping (insomnia), irritability, low blood pressure, multiple sclerosis, muscular dystrophy, leg cramps associated with pregnancy or alcoholism, general nerve pain, and obesity.
Pantothenic acid is also taken by mouth for osteoarthritis, rheumatoid arthritis, Parkinson’s disease, premenstrual syndrome (PMS), enlarged prostate, protection against mental and physical stress and anxiety, reducing side effects of thyroid therapy for people with decreased function of the thyroid gland, reducing signs of aging, reducing the risk of getting a cold or other infection, delayed growth, shingles, skin disorders, stimulating adrenal glands, sore mouth (stomatitis), chronic fatigue syndrome, toxicity related to medications such as salicylates or streptomycin, dizziness, constipation, and wound healing. It is also used following surgery to improve movement in the intestines and to reduce sore throat.
People apply dexpanthenol, which is made from pantothenic acid, to the skin for itching, promoting healing of mild eczemas and other skin conditions, insect stings, bites, poison ivy, diaper rash, and acne. It is also applied topically for preventing and treating skin reactions to radiation therapy. It is also applie to reduce skin reactions to radiotherapy treatment, for dry eyes and eye trauma, and for sprains.
Dexpanthenol is given with a needle in to the vein or muscle to improve intestinal movement (intestinal peristalsis), possibly following surgery of the gut, for abdominal bloating (distension) due to reduced intestinal function, and for gas following surgery or pregnancy.
A nasal spray containing dexpanthenol is used to reduce the feeling of having a stuffed nose (nasal obstruction) and to reduce a runny nose (nasal discharge).
Dietary supplements
Pantothenic acid is available in dietary supplements containing only pantothenic acid, in combination with other B-complex vitamins, and in some multivitamin/multimineral products 6. Some supplements contain pantethine (a dimeric form of pantetheine) or more commonly, calcium pantothenate 6. No studies have compared the relative bioavailability of pantothenic acid from these different forms. The amount of pantothenic acid in dietary supplements typically ranges from about 10 mg in multivitamin/multimineral products to up to 1,000 mg in supplements of B-complex vitamins or pantothenic acid alone 6.
Recommended Intakes
Intake recommendations for pantothenic acid and other nutrients are provided in the Dietary Reference Intakes (DRIs) developed by the Food and Nutrition Board at the National Academies of Sciences, Engineering, and Medicine 7. DRI is the general term for a set of reference values used for planning and assessing nutrient intakes of healthy people. These values, which vary by age and sex, include:
- Recommended Dietary Allowance (RDA): Average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy individuals; often used to plan nutritionally adequate diets for individuals.
- Adequate Intake (AI): Intake at this level is assumed to ensure nutritional adequacy; established when evidence is insufficient to develop an RDA.
- Estimated Average Requirement (EAR): Average daily level of intake estimated to meet the requirements of 50% of healthy individuals; usually used to assess the nutrient intakes of groups of people and to plan nutritionally adequate diets for them; can also be used to assess the nutrient intakes of individuals.
- Tolerable Upper Intake Level (UL): Maximum daily intake unlikely to cause adverse health effects.
When the Food and Nutrition Board at the National Academies of Sciences, Engineering, and Medicine 7 evaluated the available data, it found the data insufficient to derive an EAR for pantothenic acid. Consequently, the Food and Nutrition Board at the National Academies of Sciences, Engineering, and Medicine established Adequate Intakes (AIs) for all ages based on usual pantothenic acid intakes in healthy populations 7. Table 1 lists the current Adequate Intakes (AIs) for pantothenic acid 7.
Table 1: Adequate Intakes (AIs) for Pantothenic Acid
| Age | Male | Female | Pregnancy | Lactation |
|---|---|---|---|---|
| Birth to 6 months | 1.8 mg | 1.7 mg | ||
| 7–12 months | 1.8 mg | 1.7 mg | ||
| 1–3 years | 2 mg | 2 mg | ||
| 4–8 years | 3 mg | 3 mg | ||
| 9–13 years | 4 mg | 4 mg | ||
| 14–18 years | 5 mg | 5 mg | 6 mg | 7 mg |
| 19+ years | 5 mg | 5 mg | 6 mg | 7 mg |
Few data on pantothenic acid intakes in the United States are available. However, a typical mixed diet in the United States provides an estimated daily intake of about 6 mg, suggesting that most people in the United States consume adequate amounts 8. Some intake information is available from other Western populations. For example, a 1996–1997 study in New Brunswick, Canada, found average daily pantothenic acid intakes of 4.0 mg in women and 5.5 mg in men 9.
Sources of Pantothenic Acid
Food
Almost all plant- and animal-based foods contain pantothenic acid in varying amounts. Some of the richest dietary sources are beef, chicken, organ meats, whole grains, and some vegetables 10. Pantothenic acid is added to various foods, including some breakfast cereals and beverages (such as energy drinks) 10. Limited data indicate that the body absorbs 40%–61% (or half, on average) of pantothenic acid from foods 11.
Edible animal and plant tissues contain relatively high concentrations of pantothenic acid. Food processing, however, can cause significant losses of this compound (20% to almost 80%) 12.
Several food sources of pantothenic acid are listed in Table 2.
Table 2: Selected Food Sources of Pantothenic Acid
| Food | Milligrams (mg) per serving | Percent DV* |
|---|---|---|
| Breakfast cereals, fortified with 100% of the DV | 10 | 100 |
| Beef liver, boiled, 3 ounces | 8.3 | 83 |
| Shitake mushrooms, cooked, ½ cup pieces | 2.6 | 26 |
| Sunflower seeds, ¼ cup | 2.4 | 24 |
| Chicken, breast meat, skinless, roasted, 3 ounces | 1.3 | 13 |
| Tuna, fresh, bluefin, cooked, 3 ounces | 1.2 | 12 |
| Avocados, raw, ½ avocado | 1.0 | 10 |
| Milk, 2% milkfat, 1 cup | 0.9 | 9 |
| Mushrooms, white, stir fried, ½ cup sliced | 0.8 | 8 |
| Potatoes, russet, flesh and skin, baked, 1 medium | 0.7 | 7 |
| Egg, hard boiled, 1 large | 0.7 | 7 |
| Greek yogurt, vanilla, nonfat, 5.3-ounce container | 0.6 | 6 |
| Ground beef, 85% lean meat, broiled, 3 ounces | 0.6 | 6 |
| Peanuts, roasted in oil, ¼ cup | 0.5 | 5 |
| Broccoli, boiled, ½ cup | 0.5 | 5 |
| Whole-wheat pita, 1 large | 0.5 | 5 |
| Chickpeas, canned, ½ cup | 0.4 | 4 |
| Rice, brown, medium grain, cooked, ½ cup | 0.4 | 4 |
| Oats, regular and quick, cooked with water, ½ cup | 0.4 | 4 |
| Cheese, cheddar, 1.5 ounces | 0.2 | 2 |
| Carrots, chopped, raw, ½ cup | 0.2 | 2 |
| Cabbage, boiled, ½ cup | 0.1 | 1 |
| Clementine, raw, 1 clementine | 0.1 | 1 |
| Tomatoes, raw, chopped or sliced, ½ cup | 0.1 | 1 |
| Cherry tomatoes, raw, ½ cup | 0 | 0 |
| Apple, raw, slices, ½ cup | 0 | 0 |
Notes:
*DV = Daily Value. DVs were developed by the U.S. Food and Drug Administration (FDA) to help consumers compare the nutrient contents of products within the context of a total diet. The DV for the values in Table 2 is 10 mg for adults and children age 4 years and older. This value, however, decreases to 5 mg when the updated Nutrition and Supplement Facts labels are implemented 13. The updated labels must appear on food products and dietary supplements beginning in January 2020, but they can be used now 14. The FDA does not require food labels to list pantothenic acid content unless a food has been fortified with this nutrient. Foods providing 20% or more of the DV are considered to be high sources of a nutrient.
The U.S. Department of Agriculture’s (USDA’s) National Nutrient Database for Standard Reference 15 lists the nutrient content of many foods and provides a comprehensive list of foods containing pantothenic acid arranged by pantothenic acid content 16 and by food name 17.
[Source: United States Department of Agriculture Agricultural Research Service. 15]A wide variety of plant and animal foods contain pantothenic acid 12. About 85% of dietary pantothenic acid is in the form of coenzyme A (CoA) or phosphopantetheine 4. These forms are converted to pantothenic acid by digestive enzymes (nucleosidases, peptidases, and phosphorylases) in the intestinal lumen and intestinal cells. Pantothenic acid is absorbed in the intestine and delivered directly into the bloodstream by active transport (and possibly simple diffusion at higher doses) 4. Pantetheine, the dephosphorylated form of phosphopantetheine, however, is first taken up by intestinal cells and converted to pantothenic acid before being delivered into the bloodstream 18. The intestinal flora also produces pantothenic acid, but its contribution to the total amount of pantothenic acid that the body absorbs is not known 4. Red blood cells carry pantothenic acid throughout the body 4. Most pantothenic acid in tissues is in the form of CoA, but smaller amounts are present as acyl carrier protein or free pantothenic acid 4.
Pantothenic acid status is not routinely measured in healthy people. Microbiologic growth assays, animal bioassays, and radioimmunoassays can be used to measure pantothenic concentrations in blood, urine, and tissue, but urinary concentrations are the most reliable indicators because of their close relationship with dietary intake 12. With a typical American diet, the urinary excretion rate for pantothenic acid is about 2.6 mg/day 19. Excretion of less than 1 mg pantothenic acid per day suggests deficiency 1. Like urinary concentrations, whole-blood concentrations of pantothenic acid correlate with pantothenic acid intake, but measuring pantothenic acid in whole blood requires enzyme pretreatment to release free pantothenic acid from CoA 1. Normal blood concentrations of pantothenic acid range from 1.6 to 2.7 mcmol/L, and blood concentrations below 1 mcmol/L are considered low and suggest deficiency 1. Unlike whole-blood concentrations, plasma levels of pantothenic acid do not correlate well with changes in intake or status 1.
Calcium pantothenate benefits
Pantothenic acid is important for our bodies to properly use carbohydrates, proteins, and lipids and for healthy skin.
Effective for pantothenic acid deficiency. Taking pantothenic acid by mouth prevents and treats pantothenic acid deficiency.
Possibly ineffective for skin reactions from radiation therapy. Applying dexpanthenol, a chemical similar to pantothenic acid, to areas of irritated skin does not seem to reduce skin reactions caused by radiation therapy.
Insufficient evidence to rate effectiveness for:
- Athletic performance. Some research suggests that taking pantothenic acid in combination with pantethine and thiamine does not improve muscular strength or endurance in well-trained athletes.
- Attention deficit-hyperactivity disorder (ADHD). There is conflicting evidence regarding the usefulness of pantothenic acid in combination with large doses of other vitamins for the treatment of ADHD.
- Constipation. Early research suggests that taking dexpanthenol, a chemical similar to pantothenic acid, by mouth daily or receiving dexpanthenol shots can help treat constipation.
- Eye trauma. Early research shows that applying drops containing dexpanthenol, a chemical similar to pantothenic acid, reduces eye pain and discomfort after surgery to the retinal. But applying dexpanthenol ointment doesn’t seem to help improve wound healing after surgery to the cornea.
- Osteoarthritis. Early research suggests that pantothenic acid (given as calcium pantothenate) does not reduce symptoms of osteoarthritis.
- Recovery of the bowels after surgery. Taking pantothenic acid or dexpanthenol, a chemical similar to pantothenic acid, does not seem to improve bowel function after gallbladder removal.
- Sore throat after surgery. Taking dexpanthenol, a chemical similar to pantothenic acid, by mouth might reduce sore throat symptoms after surgery.
- Rheumatoid arthritis. Early research suggests that pantothenic acid (given as calcium pantothenate) does not reduce the symptoms of arthritis in people with rheumatoid arthritis.
- Nasal dryness. Early research suggests that using a specific spray (Nasicur) that contains dexpanthenol, a chemical similar to pantothenic acid, helps relieve nasal dryness.
- Sinus infection. Early research suggests that using a nasal spray containing dexpanthenol, a chemical similar to pantothenic acid, after sinus surgery reduces discharge from the nose, but not other symptoms.
- Skin irritation. Applying dexpanthenol, a chemical similar to pantothenic acid, does not seem to prevent skin irritation caused by a certain chemical in soap. But it might help treat this type of skin irritation.
- Alcoholism.
- Allergies.
- Asthma.
- Carpal tunnel syndrome.
- Colitis.
- Convulsions.
- Dandruff.
- Diabetic problems.
- Enhancing immune function.
- Eye infections (conjunctivitis).
- Hair loss.
- Headache.
- Heart problems.
- Hyperactivity.
- Inability to sleep (insomnia).
- Irritability.
- Kidney disorders.
- Low blood pressure.
- Lung disorders.
- Multiple sclerosis.
- Muscle cramps.
- Muscular dystrophy.
- Other conditions.
More evidence is needed to rate the effectiveness of pantothenic acid for these uses.
Hyperlipidemia
Because of pantothenic acid’s role in triglyceride synthesis and lipoprotein metabolism, experts have hypothesized that pantothenic acid supplementation might reduce lipid levels in patients with hyperlipidemia 20.
Several clinical trials have shown that the form of pantothenic acid known as pantethine reduces lipid levels when taken in large amounts 21, but pantothenic acid itself does not appear to have the same effects 1. A 2005 review 21 included 28 small clinical trials (average sample size of 22 participants) that examined the effect of pantethine supplements (median daily dose of 900 mg for an average of 12.7 weeks) on serum lipid levels in a total of 646 adults with hyperlipidemia. On average, the supplements were associated with triglyceride declines of 14.2% at 1 month and 32.9% at 4 months. The corresponding declines in total cholesterol were 8.7% and 15.1%, and for low-density lipoprotein (LDL) “bad” cholesterol were 10.4% and 20.1%. The corresponding increases in high-density lipoprotein (HDL) “good” cholesterol were 6.1% and 8.4%.
A few additional clinical trials have assessed pantethine’s effects on lipid levels since the publication of the 2005 review. A double-blind trial in China 22 randomly assigned 216 adults with hypertriglyceridemia (204–576 mg/dl) to supplementation with 400 U/day CoA or 600 mg/day pantethine. All participants also received dietary counseling. Triglyceride levels dropped by a significant 16.5% with pantethine compared with baseline after 8 weeks. Concentrations of total cholesterol and non–HDL cholesterol also declined modestly but significantly from baseline. However, these declines might have been due, at least in part, to the dietary counseling that the participants received.
Two randomized, blinded, placebo-controlled studies by the same research group in a total of 152 adults with low to moderate cardiovascular disease risk found that 600 mg/day pantethine for 8 weeks followed by 900 mg/day for 8 weeks plus a therapeutic lifestyle change diet resulted in small but significant reductions in total cholesterol, LDL cholesterol, and non-HDL cholesterol compared with placebo after 16 weeks 23, 20. Increasing the amount of pantethine from 600 to 900 mg/day did not increase the magnitude of reduction in the lipid measures.
Additional studies are needed to determine whether pantethine supplementation has a beneficial effect on hyperlipidemia independently of, and together with, eating a heart-healthy diet. Research is also needed to determine the mechanisms of pantethine’s effects on lipid levels.
Pantothenic Acid Deficiency
Because some pantothenic acid is present in almost all foods, deficiency is rare except in people with severe malnutrition 12. When someone has a pantothenic acid deficiency, it is usually accompanied by deficiencies in other nutrients, making it difficult to identify the effects that are specific to pantothenic acid deficiency 12. The only individuals known to have developed pantothenic acid deficiency were fed diets containing virtually no pantothenic acid or were taking a pantothenic acid metabolic antagonist 24.
On the basis of the experiences of prisoners of war in World War II and studies of diets lacking pantothenic acid in conjunction with administration of an antagonist of pantothenic acid metabolism, a deficiency is associated with numbness and burning of the hands and feet, headache, fatigue, irritability, restlessness, disturbed sleep, and gastrointestinal disturbances with anorexia 12.
Groups at Risk of Pantothenic Acid Inadequacy
The following group is most likely to have inadequate pantothenic acid status.
People with a pantothenate kinase-associated neurodegeneration 2 mutation (PANK2)
Pantothenic acid kinase is an enzyme that is essential for CoA and phosphopantetheine production. It is the principle enzyme associated with the metabolic pathway that is responsible for CoA synthesis. Mutations in the pantothenate kinase 2 (PANK2) gene cause a rare, inherited disorder, pantothenate kinase-associated neurodegeneration (PKAN). PKAN is a type of neurodegeneration associated with brain iron accumulation 10. A large number of PANK2 mutations reduce the activity of pantothenate kinase 2, potentially decreasing the conversion of pantothenic acid to CoA and thus reducing CoA levels 5.
The manifestations of PKAN can include dystonia (contractions of opposing groups of muscles), spasticity, and pigmentary retinopathy 10. Its progression is rapid and leads to significant disability and loss of function 25. Treatment focuses primarily on reducing symptoms 26. Whether pantothenate supplementation is beneficial in PKAN is not known, but some anecdotal reports indicate that supplements can reduce symptoms in some patients with atypical PKAN 27.
Calcium pantothenate side effects
Health risks from excessive pantothenic acid: the Food and Nutrition Board at the National Academies of Sciences, Engineering, and Medicine 7 was unable to establish Tolerable Upper Intake Levels (ULs) [Maximum daily intake unlikely to cause adverse health effects] for pantothenic acid because there are no reports of pantothenic acid toxicity in humans at high intakes. Some individuals taking large doses of pantothenic acid supplements (e.g., 10 g/day) develop mild diarrhea and gastrointestinal distress, but the mechanism for this effect is not known 28.
Are there safety concerns?
Pantothenic acid is LIKELY SAFE for most people when taken by mouth in appropriate amounts. The recommended amount for adults is 5 mg per day. Even larger amounts (up to 10 grams) seem to be safe for some people. But taking larger amounts increases the chance of having side effects such as diarrhea.
Dexpanthenol, a derivative of pantothenic acid, is POSSIBLY SAFE when applied to the skin, used as a nasal spray, or injected as a shot into the muscle appropriately, short-term.
Special precautions and warnings
Pregnancy and breast-feeding: Pantothenic acid is LIKELY SAFE when taken by mouth in recommended amounts of 6 mg per day during pregnancy and 7 mg per day during breast-feeding. However, it is not known if taking more than this amount is safe. Avoid using larger amounts of pantothenic acid.
- Children:Dexpanthenol, a derivative of pantothenic acid, is POSSIBLY SAFE for children when applied to the skin.
- Hemophila: Do not take dexpanthenol, a derivative of pantothenic acid, if you have hemophila. It might increase the risk of bleeding.
- Stomach blockage: Do not receive injections of dexpanthenol, a derivative of pantothenic acid, if you have a gastrointestinal blockage.
- Ulcerative colitis: Use enemas containing dexpanthenol, a derivative of pantothenic acid, cautiously if you have ulcerative colitis.
Are there interactions with medications?
It is not known if this product interacts with any medicines.
Before taking this product, talk with your health professional if you take any medications.
Are there interactions with herbs and supplements?
- Royal jelly: Royal jelly contains significant amounts of pantothenic acid. The effects of taking royal jelly and pantothenic acid supplements together aren’t known.
Are there interactions with foods?
There are no known interactions with foods.
What dose is used?
The following doses have been studied in scientific research:
By MOUTH:
As a dietary supplement to prevent deficiency: 5-10 mg of pantothenic acid (vitamin B5).
Dietary Reference Intakes (DRI) are based on adequate intakes (AI) for pantothenic acid (vitamin B5) and are as follows: Infants 0-6 months, 1.7 mg; infants 7-12 months, 1.8 mg; children 1-3 years, 2 mg; children 4-8 years, 3 mg; children 9-13 years, 4 mg; men and women 14 years and older, 5 mg; pregnant women, 6 mg; and breastfeeding women, 7 mg.
What is d calcium pantothenate
Calcium D-pantothenate is also called calcium Dextro-Pantothenic acid, D-Pantothenic acid hemicalcium salt, Vitamin B5 or (R)-(+)-N-(2,4-Dihydroxy-3,3-dimethyl-1-oxobutyl)-β-alanine hemicalcium salt with chemical formula HOCH2C(CH3)2CH(OH)CONHCH2CH2CO2 ·1/2Ca 29.
Figure 2. Calcium d pantothenate
References- Miller JW, Rucker RB. Pantothenic acid. In: Erdman JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. 10th ed. Washington, DC: Wiley-Blackwell; 2012:375-90.
- Voet, D., Voet, J.G., Pratt, C.W. (2006). Fundamentals of Biochemistry: Life at the Molecular Level, 2nd ed. Hoboken, NJ: John Wiley & Sons, Inc.
- Gropper, S. S, Smith, J. L., Groff, J. L. (2009). Advanced nutrition and human metabolism. Belmont, CA: Wadsworth, Cengage learning.
- Trumbo PR. Pantothenic acid. In: Ross AC, Caballero B, Cousins RJ, et al., eds. Modern Nutrition in Health and Disease. 11th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2014:351-7
- Sweetman L. Pantothenic acid. In: Coates PM, Betz JM, Blackman MR, et al., eds. Encyclopedia of Dietary Supplements. 2nd ed. London and New York: Informa Healthcare; 2010:604-11
- National Institutes of Health. Dietary Supplement Label Database. http://www.dsld.nlm.nih.gov/dsld/
- Institute of Medicine. Food and Nutrition Board. Dietary Reference Intakes: Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: National Academy Press; 1998.
- Iyenga GV, Wolfe WR, Tanner JT, et al. Content of minor and trace elements, and organic nutrients in representative mixed total diet composites from the USA. Sci Total Environ 2000;256:215-26 https://www.ncbi.nlm.nih.gov/pubmed/10902848
- Provincial Epidemiology Service, New Brunswick Department of Health and Wellness. New Brunswick nutrition survey; 1997.
- Trumbo PR. Pantothenic acid. In: Ross AC, Caballero B, Cousins RJ, et al., eds. Modern Nutrition in Health and Disease. 11th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2014:351-7.
- Tarr JB, Tamura T, Stokstad EL. Availability of vitamin B6 and pantothenate in an average American diet in man. Am J Clin Nutr 1981;34:1328-37.
- Miller JW, Rucker RB. Pantothenic acid. In: Erdman JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. 10th ed. Washington, DC: Wiley-Blackwell; 2012:375-90
- U.S. Food and Drug Administration. Food Labeling: Revision of the Nutrition and Supplement Facts Labels. https://www.federalregister.gov/documents/2016/05/27/2016-11867/food-labeling-revision-of-the-nutrition-and-supplement-facts-labels
- U.S. Food and Drug Administration. Food Labeling: Revision of the Nutrition and Supplement Facts Labels and Serving Sizes of Foods That Can Reasonably Be Consumed at One Eating Occasion. https://www.federalregister.gov/documents/2017/10/02/2017-21019/food-labeling-revision-of-the-nutrition-and-supplement-facts-labels-and-serving-sizes-of-foods-that
- U.S. Department of Agriculture, Agricultural Research Service. USDA Food Composition Databases. https://ndb.nal.usda.gov/ndb/
- https://ndb.nal.usda.gov/ndb/nutrients/report/nutrientsfrm?max=25&offset=0&totCount=0&nutrient1=410&nutrient2=&nutrient3=&subset=0&sort=c&measureby=m
- https://ndb.nal.usda.gov/ndb/nutrients/report/nutrientsfrm?max=25&offset=0&totCount=0&nutrient1=410&nutrient2=&nutrient3=&subset=0&sort=f&measureby=m
- Sweetman L. Pantothenic acid. In: Coates PM, Betz JM, Blackman MR, et al., eds. Encyclopedia of Dietary Supplements. 2nd ed. London and New York: Informa Healthcare; 2010:604-11.
- Tarr JB, Tamura T, Stokstad EL. Availability of vitamin B6 and pantothenate in an average American diet in man. Am J Clin Nutr 1981;34:1328-37 https://www.ncbi.nlm.nih.gov/pubmed/7258123
- Rumberger JA, Napolitano J, Azumano I, et al. Pantethine, a derivative of vitamin B(5) used as a nutritional supplement, favorably alters low-density lipoprotein cholesterol metabolism in low- to moderate-cardiovascular risk North American subjects: a triple-blinded placebo and diet-controlled investigation. Nutr Res 2011;31:608-15 https://www.ncbi.nlm.nih.gov/pubmed/21925346
- McRae MP. Treatment of hyperlipoproteinemia with pantethine: A review and analysis of efficacy and tolerability. Nutrition Research 2005;25:319-33.
- Chen YQ, Zhao SP, Zhao YH. Efficacy and tolerability of coenzyme A vs pantethine for the treatment of patients with hyperlipidemia: A randomized, double-blind, multicenter study. J Clin Lipidol 2015;9:692-7 https://www.ncbi.nlm.nih.gov/pubmed/26350816
- Evans M, Rumberger JA, Azumano I, et al. Pantethine, a derivative of vitamin B5, favorably alters total, LDL and non-HDL cholesterol in low to moderate cardiovascular risk subjects eligible for statin therapy: a triple-blinded placebo and diet-controlled investigation. Vasc Health Risk Manag 2014;10:89-100. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3942300/
- Institute of Medicine. Food and Nutrition Board. Dietary Reference Intakes: Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: National Academy Press; 1998
- Hayflick SJ. Defective pantothenate metabolism and neurodegeneration. Biochem Soc Trans 2014;42:1063-8 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5906047/
- Gregory A, Hayflick SJ. Pantothenate Kinase-Associated Neurodegeneration. In: Adam MP, Ardinger HH, Pagon RA, et al., eds. GeneReviews. Seattle, WA: University of Washington, Seattle; 2017.
- Kurian MA, Hayflick SJ. Pantothenate kinase-associated neurodegeneration (PKAN) and PLA2G6-associated neurodegeneration (PLAN): review of two major neurodegeneration with brain iron accumulation (NBIA) phenotypes. Int Rev Neurobiol 2013;110:49-71 https://www.ncbi.nlm.nih.gov/pubmed/24209433
- Chawla J, Kvarnberg D. Hydrosoluble vitamins. Handb Clin Neurol 2014;120:891-914. https://www.ncbi.nlm.nih.gov/pubmed/24365359
- Calcium D-pantothenate https://pubchem.ncbi.nlm.nih.gov/compound/25021359