What is cardiac arrest
Sudden cardiac arrest also called sudden cardiac death, is the sudden, unexpected loss of heart function, breathing and consciousness. Sudden cardiac arrest usually results from an electrical disturbance in your heart that disrupts its pumping action (ventricular arrhythmia), stopping blood flow to the rest of your body including your brain. Sudden cardiac arrest usually causes death if it’s not treated within minutes. Cardiac arrest occurs through three different mechanisms: (1) lethal arrhythmias [ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT)] leading to loss of cardiac output, (2) insufficient myocardial contraction to produce cardiac output [pulseless electrical activity] and (3) complete failure of the electrical conduction system of the heart (asystole) 1. The most common electrical sequence of events is ventricular tachycardia (VT) degenerating into ventricular fibrillation (VF) 2. As defined by the American Heart Association and the American College of Cardiology, “sudden cardiac arrest is the sudden cessation of cardiac activity so that the victim becomes unresponsive, with no normal breathing and no signs of circulation. If corrective measures are not taken rapidly, this condition progresses to sudden death. Cardiac arrest should be used to signify an event as described above, which is reversed, usually by cardiopulmonary resuscitation (CPR) and/or defibrillation or cardioversion, or cardiac pacing. Sudden cardiac death should not be used to describe events that are not fatal” 3.
Most people who have sudden cardiac arrest die from it, often within minutes. Sudden cardiac arrest should be treated right away with a defibrillator. Rapid treatment of sudden cardiac arrest with a defibrillator can be lifesaving. A defibrillator is a device that sends an electric shock to the heart to try to restore its normal rhythm.
Automated external defibrillators (AEDs) can be used by bystanders to save the lives of people who are having sudden cardiac arrest. These portable devices often are found in public places, such as shopping malls, golf courses, businesses, airports, airplanes, casinos, convention centers, hotels, sports venues, and schools.
But if someone is having sudden cardiac arrest and there is no defibrillator available, then cardiopulmonary resuscitation (CPR) should be performed until an ambulance or other help arrives. The chest compressions given during CPR move a small amount of blood to the heart and brain, “buying time” until a normal heartbeat can be restored. Patients with known heart problems who are at risk of sudden cardiac arrest should be under the care of a doctor.
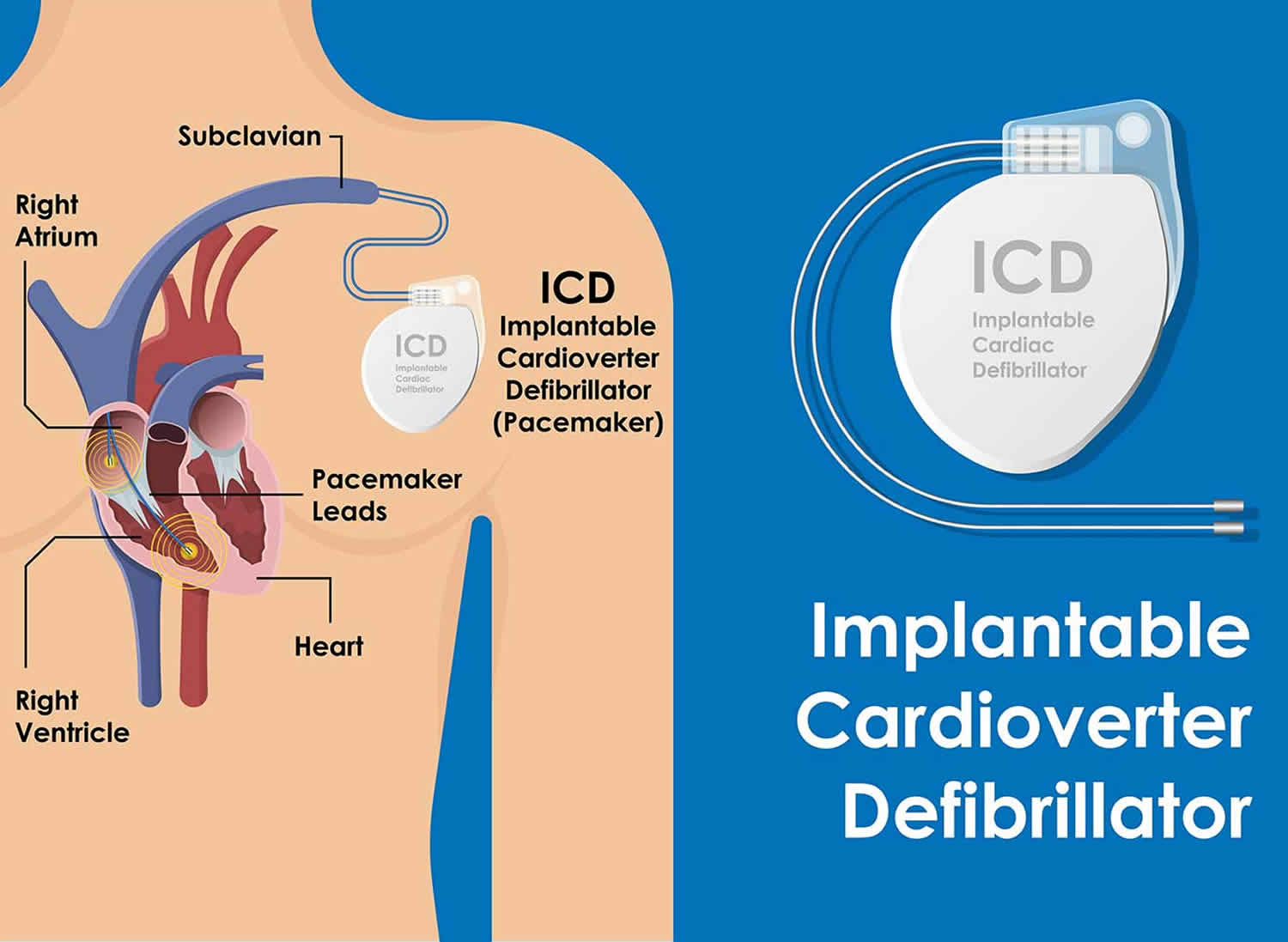
Patients who have already had sudden cardiac arrest are at greater risk of having it again. These patients may be treated with antiarrhythmic medicines or an implantable cardioverter defibrillator (ICD) to stop the arrhythmias that can lead to sudden cardiac arrest. An ICD is a device that applies electric impulses or, if needed, a shock to restore a normal heartbeat.
In some patients, balloon angioplasty or coronary artery bypass surgery may be performed to treat their coronary heart disease and prevent the heart damage that can lead to arrhythmias and sudden cardiac arrest.
Sudden cardiac arrest symptoms are immediate and drastic.
Signs and symptoms suggesting a person has gone into cardiac arrest include:
- Sudden collapse
- No pulse
- No breathing or is only gasping
- Loss of consciousness
- They don’t respond to any stimulation, such as being touched (no response to tapping on shoulders) or spoken to
If you think somebody has gone into cardiac arrest and you don’t have access to an automated external defibrillator (AED), you should perform chest compressions (CPR), as this can help restart the heart.
- Sudden cardiac arrest is a medical emergency. If not treated immediately, it causes sudden cardiac death!
- With fast, appropriate medical care, survival is possible.
Administering cardiopulmonary resuscitation (CPR), treating with a defibrillator — or even just compressions to the chest — can improve the chances of survival until emergency personnel arrive (watch the video below on how to perform a CPR). However, it’s best that you enrolled in a first aid course and learn how to do CPR properly from trained paramedics.
Sometimes other signs and symptoms precede sudden cardiac arrest. These may include fatigue, fainting, blackouts, dizziness, chest pain, shortness of breath, weakness, palpitations or vomiting. But sudden cardiac arrest often occurs with no warning.
- The time and mode of death are unexpected. Sudden cardiac arrest occurs instantly or shortly after symptoms appear.
Sudden cardiac arrest is different from a heart attack, which occurs when blood flow to a portion of the heart is blocked. However, a heart attack can sometimes trigger an electrical disturbance that leads to sudden cardiac arrest.
- Each year, more than 400,000 emergency medical services-assessed out-of-hospital cardiac arrests occur in the United States 4. Almost 95% of these people die within minutes.
- The incidence of out-of-hospital sudden cardiac arrest in industrial countries is reported to be between 35.7 and 128.3 cases per 100,000, with a mean of 62 cases per year 5. This translates into approximately 300,000 people in the United States and about the same number in Europe each year.
- Sudden cardiac arrest happens most often in adults in their mid 30s to mid 40s. It affects men twice as often as it affects women. It hardly ever affects children, unless they have an inherited problem that increases their risk.
- People with heart disease have a greater chance of sudden cardiac arrest, but it can happen in people who appear healthy and do not know they have any heart problems.
If you suspect the symptoms of a heart attack, dial your local emergency number immediately and ask for an ambulance.
Don’t worry if you have doubts. Paramedics would rather be called out to find an honest mistake has been made than be too late to save a person’s life.
Symptoms of a heart attack can include:
- chest pain – a sensation of pressure, tightness or squeezing in the center of your chest
- pain in other parts of the body – it can feel as if the pain is traveling from your chest to your arms (usually the left arm is affected, but it can affect both arms), jaw, neck, back and abdomen
- feeling lightheaded or dizzy
- sweating
- shortness of breath
- feeling sick (nausea) or being sick (vomiting)
- an overwhelming sense of anxiety (similar to having a panic attack)
- coughing or wheezing
Although the chest pain is often severe, some people may only experience minor pain, similar to indigestion. In some cases, there may not be any chest pain at all, especially in women, the elderly and people with diabetes.
It’s the overall pattern of symptoms that helps to determine whether you are having a heart attack.
If someone has had a heart attack, it’s important to rest while they wait for an ambulance, to avoid unnecessary strain on the heart.
If aspirin is easily available and the person who has had a heart attack isn’t allergic to it, slowly chew and then swallow an adult-sized tablet (300mg) while waiting for the ambulance.
The aspirin helps to thin the blood and restore the heart’s blood supply.
How to perform a Cardiopulmonary Resuscitation (CPR)
If the person’s breathing or heart stops, cardiopulmonary resuscitation (CPR) should be performed immediately.
Hands-only CPR
- Ensure the area is safe
- Check for hazards, such as electrical equipment or traffic.
To carry out a chest compression:
- Place the heel of your hand on the breastbone at the center of the person’s chest. Place your other hand on top of your first hand and interlock your fingers.
- Position yourself with your shoulders above your hands.
- Using your body weight (not just your arms), press straight down by 5-6cm (2-2.5 inches) on their chest.
- Keeping your hands on their chest, release the compression and allow the chest to return to its original position.
- Repeat these compressions at a rate of 100 to 120 times per minute until an ambulance arrives or you become exhausted.
When you call for an ambulance, telephone systems now exist that can give basic life-saving instructions, including advice about CPR. These are now common and are easily accessible with mobile phones.
Cardiopulmonary Resuscitation (CPR) with rescue breaths
If you’ve been trained in CPR, including rescue breaths, and feel confident using your skills, you should give chest compressions with rescue breaths. If you’re not completely confident, attempt hands-only CPR instead (see above).
Adults
- Place the heel of your hand on the center of the person’s chest, then place the other hand on top and press down by 5-6cm (2-2.5 inches) at a steady rate of 100 to 120 compressions per minute.
- After every 30 chest compressions, give two rescue breaths.
- Tilt the casualty’s head gently and lift the chin up with two fingers. Pinch the person’s nose. Seal your mouth over their mouth and blow steadily and firmly into their mouth for about one second. Check that their chest rises. Give two rescue breaths.
- Continue with cycles of 30 chest compressions and two rescue breaths until they begin to recover or emergency help arrives.
Children over one year old
- Open the child’s airway by placing one hand on the child’s forehead and gently tilting their head back and lifting the chin. Remove any visible obstructions from the mouth and nose.
- Pinch their nose. Seal your mouth over their mouth and blow steadily and firmly into their mouth, checking that their chest rises. Give five initial rescue breaths.
- Place the heel of one hand on the center of their chest and push down by 5cm (about two inches), which is approximately one-third of the chest diameter.
- The quality (depth) of chest compressions is very important. Use two hands if you can’t achieve a depth of 5cm using one hand.
- After every 30 chest compressions at a rate of 100 to 120 per minute, give two breaths.
- Continue with cycles of 30 chest compressions and two rescue breaths until they begin to recover or emergency help arrives.
Infants under one year old
- Open the infant’s airway by placing one hand on their forehead and gently tilting the head back and lifting the chin. Remove any visible obstructions from the mouth and nose.
- Place your mouth over the mouth and nose of the infant and blow steadily and firmly into their mouth, checking that their chest rises. Give five initial rescue breaths.
- Place two fingers in the middle of the chest and push down by 4cm (about 1.5 inches), which is approximately one-third of the chest diameter. The quality (depth) of chest compressions is very important. Use the heel of one hand if you can’t achieve a depth of 4cm using the tips of two fingers.
- After 30 chest compressions at a rate of 100 to 120 per minute, give two rescue breaths.
- Continue with cycles of 30 chest compressions and two rescue breaths until they begin to recover or emergency help arrives.
Cardiac arrest vs Heart attack
People often use the term “heart attack” mistakenly used to describe cardiac arrest. Heart attack and Sudden Cardiac Arrest are not the same.
While a heart attack may cause cardiac arrest and sudden death, the terms don’t mean the same thing. Heart attacks are caused by blood supply to the heart being suddenly interrupted due to a blockage in the coronary arteries that stops blood flow to the heart. A heart attack (or myocardial infarction) refers to death of heart muscle tissue due to the loss of blood supply, not necessarily resulting in the death of the heart attack patient.
Cardiac arrest is caused when the heart’s electrical system malfunctions. In cardiac arrest death results when the heart suddenly stops working properly. This may be caused by abnormal, or irregular, heart rhythms (called arrhythmias). Cardiac arrest, however, may happen after or during recovery from a heart attack.
People who have heart disease are at higher risk for cardiac arrest. However, sudden cardiac arrest can happen in people who appear healthy and have no known heart disease or other risk factors for sudden cardiac arrest.
Difference between heart attack and cardiac arrest
- A heart attack is when blood flow to the heart is blocked, and sudden cardiac arrest is when the heart malfunctions and suddenly stops beating unexpectedly.
- A heart attack is a “circulation” problem and sudden cardiac arrest is an “electrical” problem.
A common arrhythmia in cardiac arrest is ventricular fibrillation. This is when the heart’s lower chambers suddenly start beating chaotically and don’t pump blood. Death occurs within minutes after the heart stops. Cardiac arrest may be reversed if CPR (cardiopulmonary resuscitation) is performed and a defibrillator is used to shock the heart and restore a normal heart rhythm within a few minutes.
These two distinct heart conditions are linked. Sudden cardiac arrest can occur after a heart attack, or during recovery. Heart attacks increase the risk for sudden cardiac arrest. Most heart attacks do not lead to sudden cardiac arrest. But when sudden cardiac arrest occurs, heart attack is a common cause. Other heart conditions may also disrupt the heart’s rhythm and lead to sudden cardiac arrest. These include a thickened heart muscle (cardiomyopathy), heart failure, arrhythmias, particularly ventricular fibrillation, and long Q-T syndrome.
What is a heart attack?
A heart attack occurs when a blocked artery prevents oxygen-rich blood from reaching a section of the heart. If the blocked artery is not reopened quickly, the part of the heart normally nourished by that artery begins to die. Without treatment, the heart muscles will experience irreversible damage. The longer a person goes without treatment, the greater the damage. Symptoms of a heart attack may be immediate and intense. More often, though, symptoms start slowly and persist for hours, days or weeks before a heart attack. Unlike with sudden cardiac arrest, the heart usually does not stop beating during a heart attack. The heart attack symptoms in women can be different than men.
If a large portion of the heart is damaged in this way, the heart stops beating (known as a cardiac arrest), resulting in death.
Coronary heart disease (coronary artery disease) is the leading cause of heart attacks. Coronary heart disease (coronary artery disease) is a condition in which the coronary arteries (the major blood vessels that supply the heart with blood) get clogged up with deposits of cholesterol (atheroma). These deposits are called plaques.
Before a heart attack, one of the plaques ruptures (bursts), causing a blood clot to develop at the site of the rupture. The clot may block the supply of blood to the heart, triggering a heart attack.
Your risk of developing coronary artery disease is increased by:
- smoking
- a high-fat diet
- diabetes
- high cholesterol
- high blood pressure
- being overweight or obese.
What to do for Heart Attack
Even if you’re not sure it’s a heart attack, call your emergency response number. Every minute matters! It’s best to call emergency medical services (EMS) to get to the emergency room right away. Emergency medical services staff can begin treatment when they arrive — up to an hour sooner than if someone gets to the hospital by car. Emergency medical services staff are also trained to revive someone whose heart has stopped. Patients with chest pain who arrive by ambulance usually receive faster treatment at the hospital, too.
What is cardiac arrest?
Sudden cardiac arrest occurs suddenly and often without warning. It is triggered by an electrical malfunction in the heart that causes an irregular heartbeat (arrhythmia). With its pumping action disrupted, the heart cannot pump blood to the brain, lungs and other organs. Seconds later, a person loses consciousness and has no pulse. Death occurs within minutes if the victim does not receive treatment.
What to do in Sudden Cardiac Arrest
Cardiac arrest is reversible in most victims if it’s treated within a few minutes. Begin CPR immediately and continue until professional emergency medical services arrive. If two people are available to help, one should begin CPR immediately while the other calls the local emergency number and finds a defibrillator.
Cardiac arrest causes
Cardiac arrest may be caused by almost any known heart condition. Most cardiac arrests occur when the diseased heart’s electrical system malfunctions, producing an abnormal rhythm such as ventricular tachycardia (very fast heartbeat) or ventricular fibrillation (very chaotic heartbeat). During ventricular fibrillation, the ventricles (the heart’s lower chambers) don’t beat normally. Instead, they quiver very rapidly and irregularly. When this happens, the heart pumps little or no blood to the body. Ventricular fibrillation is fatal if not treated within a few minutes.
Some cardiac arrests are caused by extreme slowing of the heart’s rhythm also known as bradycardia. Sudden cardiac arrest also can occur if the heart muscle doesn’t respond to the heart’s electrical signals.
Certain diseases and conditions can cause heart electrical problems that lead to sudden cardiac arrest. Examples include ischemic heart disease, also called coronary heart disease or coronary artery disease; severe physical stress; certain inherited disorders; and structural changes in the heart.
All of these events are called life-threatening arrhythmias.
Heart conditions that can lead to sudden cardiac arrest
Sudden cardiac arrest can happen in people who have no known heart disease. However, a life-threatening arrhythmia usually develops in a person with a preexisting, possibly undiagnosed heart condition. Heart conditions include:
- Coronary artery disease or ischemic heart disease. Most cases of sudden cardiac arrest occur in people who have coronary artery disease, in which the arteries become clogged with cholesterol and other deposits, reducing blood flow to the heart, which results from a condition called atherosclerosis. Atherosclerosis is a condition where a waxy substance (plaque) forms inside the arteries that supply blood to your heart. If that plaque builds up in the arteries that supply blood to your heart, the blood flow slows or stops. This decreases the amount of oxygen that gets to the heart, which can lead to a heart attack. Any scarring or damage to the heart after a heart attack increases the risk of arrhythmia and sudden cardiac arrest.
- Heart attack. If a heart attack occurs, often as a result of severe coronary artery disease, it can trigger ventricular fibrillation and sudden cardiac arrest. Also, a heart attack can leave scar tissue in your heart. Electrical short circuits around the scar tissue can lead to abnormalities in your heart rhythm.
- Enlarged heart or thickened heart muscle (cardiomyopathy). This occurs primarily when your heart’s muscular walls stretch and enlarge or thicken (typically due to high blood pressure or valvular heart disease). Then your heart’s muscle is abnormal, a condition that often leads to arrhythmias and sudden cardiac arrest.
- Valvular heart disease. Leaking or narrowing of your heart valves can lead to stretching or thickening of your heart muscle. When the chambers become enlarged or weakened because of stress caused by a tight or leaking valve, there’s an increased risk of developing arrhythmia.
- Acute myocarditis (inflammation of the heart muscle).
- Heart defect present at birth (congenital heart disease). When sudden cardiac arrest occurs in children or adolescents, it can be due to congenital heart disease. Adults who’ve had corrective surgery for a congenital heart defect still have a higher risk of sudden cardiac arrest.
- Electrical problems in the heart. In some people, the problem is in the heart’s electrical system itself instead of a problem with the heart muscle or valves. These are called primary heart rhythm abnormalities and include conditions such as Brugada syndrome, Wolff-Parkinson-White syndrome and Long QT syndrome. These electrical abnormalities may cause sudden cardiac arrest in children and young people.
Some other causes of cardiac arrest include:
- Scarring from a prior heart attack or other causes: A heart that’s scarred or enlarged from any cause is prone to develop life-threatening ventricular arrhythmias. The first six months after a heart attack is a particularly high-risk period for sudden cardiac arrest in patients with atherosclerotic heart disease.
- Physical stress, which can cause the heart’s electrical system to stop working. In people who already have heart problems, intense physical activity or exercise can lead to sudden cardiac arrest because the release of the hormone adrenaline acts as a trigger for sudden cardiac arrest.
- Heart medications: Under certain conditions, various heart medications can set the stage for arrhythmias that cause sudden cardiac arrest. Paradoxically, antiarrhythmic drugs used to treat arrhythmias can sometimes produce lethal ventricular arrhythmias even at normally prescribed doses. This is called a “proarrhythmic” effect. Regardless of whether there’s organic heart disease, significant changes in blood levels of potassium and magnesium (from using diuretics, for example) also can cause life-threatening arrhythmias and cardiac arrest.
- Blood vessel abnormalities: Less often, inborn blood vessel abnormalities, particularly in the coronary arteries and aorta, may be present in young sudden death victims. Adrenaline released during intense physical or athletic activity often acts as a trigger for sudden cardiac arrest when these abnormalities are present.
- Recreational drug use: In people without organic heart disease, recreational drug use (like cocaine or amphetamines) is a cause of sudden cardiac arrest.
- A drug overdose
- Electrocution
- A severe hemorrhage (known as hypovolemic shock) – losing a large amount of blood
- Hypoxia – caused by a severe drop in oxygen levels.
Several research studies are under way to try to find the exact causes of sudden cardiac arrest and how to prevent them.
Ischemic heart disease
Ischemic heart disease is a disease in which a waxy substance called plaque builds up in the coronary arteries (also known as atherosclerosis). These arteries supply oxygen-rich blood to your heart muscle.
Plaque is made up of fat, cholesterol, calcium, and other substances found in the blood. Over time, plaque hardens and narrows your arteries. This limits the flow of oxygen-rich blood to your organs and other parts of your body. Plaque narrows the arteries and reduces blood flow to your heart muscle. Eventually, an area of plaque can rupture (break open). This may cause a blood clot to form on the plaque’s surface.
A blood clot can partly or fully block the flow of oxygen-rich blood to the portion of heart muscle fed by the artery. This causes a heart attack.
During a heart attack, some heart muscle cells die and are replaced with scar tissue. The scar tissue damages the heart’s electrical system. As a result, electrical signals may spread abnormally throughout the heart. These changes to the heart increase the risk of dangerous arrhythmias and sudden cardiac arrest.
Ischemic heart disease seems to cause most cases of sudden cardiac arrest in adults. Many of these adults, however, have no signs or symptoms of heart disease before having sudden cardiac arrest.
Physical stress
Certain types of physical stress can cause your heart’s electrical system to fail. Examples include:
- Intense physical activity. The hormone adrenaline is released during intense physical activity. This hormone can trigger sudden cardiac arrest in people who have heart problems.
- Very low blood levels of potassium or magnesium. These minerals play an important role in your heart’s electrical signaling.
- Major blood loss.
- Severe lack of oxygen.
Inherited disorders
A tendency to have arrhythmias runs in some families. This tendency is inherited, which means it’s passed from parents to children through the genes. Members of these families may be at higher risk for sudden cardiac arrest. An example of an inherited disorder that makes you more likely to have arrhythmias is long QT syndrome (LQTS). LQTS is a disorder of the heart’s electrical activity. Problems with tiny pores on the surface of heart muscle cells cause the disorder. Long QT syndrome (LQTS) can cause sudden, uncontrollable, dangerous heart rhythms.
People who inherit structural heart problems also may be at higher risk for sudden cardiac arrest. These types of problems often are the cause of sudden cardiac arrest in children.
Structural changes in the heart
Changes in the heart’s normal size or structure may affect its electrical system. Examples of such changes include an enlarged heart due to high blood pressure or advanced heart disease. Heart infections also may cause structural changes in the heart.
Risk factors for sudden cardiac arrest
Because sudden cardiac arrest is so often linked with coronary artery disease, the same factors that put you at risk of coronary artery disease can also put you at risk of sudden cardiac arrest.
The risk of sudden cardiac arrest increases:
- With age, the risk of sudden cardiac arrest increases with age
- If you are a man. Men are more likely than women to have sudden cardiac arrest.
- Some studies show that blacks—particularly those with underlying conditions such as diabetes, high blood pressure, heart failure, and chronic kidney disease or certain cardiac findings on tests such as an electrocardiogram—have a higher risk for sudden cardiac arrest.
Major risk factor
The major risk factor for sudden cardiac arrest is ischemic heart disease. Most people who have sudden cardiac arrest have some degree of ischemic heart disease; however, many people may not know that they have heart disease until sudden cardiac arrest occurs. Usually their heart disease is “silent”—that is, it has no signs or symptoms. Because of this, doctors and nurses have not detected it.
Many people who have sudden cardiac arrest also have silent or undiagnosed, heart attacks before sudden cardiac arrest happens. These people have no clear signs of heart attack, and they don’t even realize that they’ve had one.
Other risk factors for sudden cardiac arrest include:
- A personal history of arrhythmias
- A family history of coronary artery disease
- A personal or family history of sudden cardiac arrest or inherited disorders that make you prone to arrhythmias
- Smoking
- Drug or alcohol abuse
- Heart attack
- Heart failure
- High blood pressure
- High blood cholesterol
- Obesity
- Diabetes
- An inactive lifestyle
- Nutritional imbalance, such as low potassium or magnesium levels
- Obstructive sleep apnea
- Chronic kidney disease
Cardiac arrest prevention
Ways to prevent death due to sudden cardiac arrest differ depending on whether:
- You’ve already had sudden cardiac arrest
- You’ve never had sudden cardiac arrest but are at high risk for the condition
- You’ve never had sudden cardiac arrest and have no known risk factors for the condition
You can reduce your risk of sudden cardiac arrest by getting regular checkups, being screened for heart disease and living a heart-healthy lifestyle.
People who have survived sudden cardiac arrest
If you’ve already had sudden cardiac arrest, you’re at high risk of having it again. Research shows that an implantable cardioverter defibrillator (ICD) reduces the chances of dying from a second sudden cardiac arrest. An ICD is surgically placed under the skin in your chest or abdomen. The device has wires with electrodes on the ends that connect to your heart’s chambers. The implantable cardioverter defibrillator monitors your heartbeat.
If the ICD detects a dangerous heart rhythm, it gives an electric shock to restore the heart’s normal rhythm. Your doctor may give you medicine to limit irregular heartbeats that can trigger the ICD.
An ICD isn’t the same as a pacemaker. The devices are similar, but they have some differences. Pacemakers give off low-energy electrical pulses. They’re often used to treat less dangerous heart rhythms, such as those that occur in the upper chambers of the heart. Most new ICDs work as both pacemakers and ICDs.
Figure 1. Implantable cardioverter defibrillator (ICD)
Footnote: The illustration shows the location of an implantable cardioverter defibrillator in the upper chest. The electrodes are inserted into the heart through a vein.
People at high risk for a first sudden cardiac arrest
If you have severe ischemic heart disease, you’re at increased risk for sudden cardiac arrest. This is especially true if you’ve recently had a heart attack. Your doctor may prescribe a type of medicine called a beta blocker to help lower your risk for sudden cardiac arrest. Your doctor also may discuss beginning statin treatment if you have an elevated risk for developing heart disease or having a stroke.
Doctors usually prescribe statins for people who have:
- Diabetes
- Heart disease or had a prior stroke
- High LDL cholesterol (low-density lipoprotein or “bad” cholesterol) levels
Your doctor also may prescribe other medications to:
- Decrease your chance of having a heart attack or dying suddenly.
- Lower blood pressure.
- Prevent blood clots, which can lead to heart attack or stroke.
- Prevent or delay the need for a procedure or surgery, such as angioplasty or coronary artery bypass grafting.
- Reduce your heart’s workload and relieve heart disease symptoms.
Take all medicines regularly, as your doctor prescribes. Don’t change the amount of your medicine or skip a dose unless your doctor tells you to. You should still follow a heart-healthy lifestyle, even if you take medicines to treat your heart disease.
A heart-healthy lifestyle includes:
- Heart-healthy eating
- Aiming for a healthy weight
- Managing stress
- Physical activity
- Quitting smoking
Other treatments for coronary heart disease—such as percutaneous coronary intervention (also known as coronary angioplasty) or coronary artery bypass grafting—also may lower your risk for sudden cardiac arrest. Your doctor also may recommend an ICD if you’re at high risk for sudden cardiac arrest.
People who have no known risk factors for sudden cardiac arrest
Ischemic heart disease seems to be the cause of most sudden cardiac arrests in adults. Heart disease also is a major risk factor for angina (chest pain or discomfort) and heart attack, and it contributes to other heart problems.
Following a heart-healthy lifestyle can help you lower your risk for heart disease, sudden cardiac arrest, and other heart problems. A heart-healthy lifestyle includes:
- Heart-healthy eating
- Aiming for a healthy weight
- Managing stress
- Physical activity
- Quitting smoking
Cardiac arrest signs and symptoms
Cardiac arrest strikes immediately and without warning! Usually, the first sign of sudden cardiac arrest is loss of consciousness (fainting). At the same time, no heartbeat (or pulse) can be felt. Breathing may also stop at this time.
Some people may have a racing heartbeat or feel dizzy or light-headed just before they faint. Within an hour before sudden cardiac arrest, some people have chest pain, shortness of breath, nausea (feeling sick to the stomach), or vomiting.
Here are the signs of sudden cardiac arrest:
- Sudden loss of responsiveness (no response to tapping on shoulders).
- No response to tapping on shoulders.
- Does nothing when you ask if he’s OK.
- No normal breathing
- Victim is not breathing or is only gasping.
If you suspect someone is suffering from cardiac arrest:
- Tap and shout
- Check if the person responds. Tap him and shout, “Are you OK?” If he doesn’t move, speak, blink, or otherwise react, then he is not responding.
- Yell for help
- Tell someone to call your emergency response number and get an Automated External Defibrillator (if one is available).
- If you are alone with an adult who has these signs of cardiac arrest, call your local emergency number and get an Automated External Defibrillator (if one is available).
- Check breathing:
- If the person isn’t breathing or is only gasping, give CPR.
- Giving CPR: Push hard and fast
- Push down at least 2 inches at a rate of 100 to 120 pushes a minute in the center of the chest, allowing the chest to come back up to its normal position after each push.
- Use an Automated External Defibrillator as soon as it arrives by turning it on and following the prompt.
- Keep pushing until the person starts to breathe or move or someone with more advanced training takes over.
Cardiac arrest complications
When sudden cardiac arrest occurs, reduced blood flow to your brain causes unconsciousness. If your heart rhythm doesn’t rapidly return to normal, brain damage occurs and death results. Survivors of cardiac arrest might show signs of brain damage.
Sudden cardiac arrest diagnosis
Sudden cardiac arrest happens without warning and requires emergency treatment. Because sudden cardiac arrest happens quickly and without warning, it usually cannot be diagnosed when it is happening. Doctors rarely diagnose sudden cardiac arrest with medical tests as it’s happening. Instead, sudden cardiac arrest often is diagnosed after it happens. Doctors do this by ruling out other causes of a person’s sudden collapse.
If you’re at high risk for sudden cardiac arrest, your doctor may refer you to a cardiologist. This is a doctor who specializes in diagnosing and treating heart diseases and conditions. Your cardiologist will work with you to decide whether you need treatment to prevent sudden cardiac arrest.
Some cardiologists specialize in problems with the heart’s electrical system. These specialists are called cardiac electrophysiologists.
Diagnostic tests and procedures
Doctors use several tests to help detect risk factors that put people at risk for sudden cardiac arrest.
EKG (Electrocardiogram)
An EKG or ECG is a simple, painless test that detects and records the heart’s electrical activity. The test shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through each part of the heart.
An EKG can show evidence of heart damage due to ischemic heart disease. The test also can show signs of a previous or current heart attack.
Echocardiography (Echocardiogram)
Echocardiography or echo, is a painless test that uses sound waves to create pictures of your heart. The test shows the size and shape of your heart and how well your heart chambers and valves are working.
Echo also can identify areas of poor blood flow to the heart, areas of heart muscle that aren’t contracting normally, and previous injury to the heart muscle caused by poor blood flow.
There are several types of echo, including stress echo. This test is done both before and after a cardiac stress test. During this test, you exercise (or are given medicine if you’re unable to exercise) to make your heart work hard and beat fast.
Stress echo shows whether you have decreased blood flow to your heart (a sign of coronary artery disease).
MUGA test
A MUGA (multiple gated acquisition) test shows how well your heart is pumping blood. For this test, a small amount of radioactive substance is injected into a vein and travels to your heart. The substance releases energy, which special cameras outside of your body can detect. The cameras use the energy to create pictures of many parts of your heart.
Cardiac MRI
Cardiac MRI (magnetic resonance imaging) is a safe procedure that uses radio waves and magnets to create detailed pictures of your heart. The test creates still and moving pictures of your heart and major blood vessels. Doctors use cardiac MRI to get pictures of the beating heart and to look at the structure and function of the heart.
Cardiac catheterization
Cardiac catheterization is a procedure used to diagnose and treat certain heart conditions. During cardiac catheterization, a long thin flexible tube called a catheter is put into an artery or vein in your arm, groin (upper thigh), or neck and threaded through your blood vessels to your heart. Through the catheter, your doctor can do diagnostic tests and treatments on your heart. Some heart disease treatments, such as coronary angioplasty and coronary stenting, also are done using cardiac catheterization.
Sometimes dye is put into the catheter. The dye will flow through your bloodstream to your heart. The dye makes your coronary (heart) arteries visible on x-ray pictures. The dye can show whether plaque has narrowed or blocked any of your coronary arteries.
Usually, you’ll be awake during cardiac catheterization but be given medications to help you relax. Recovery time for a cardiac catheterization is quick, and there’s a low risk of complications.
Electrophysiology study
For an electrophysiology study, doctors use cardiac catheterization to record how your heart’s electrical system responds to certain medicines and electrical stimulation. This helps your doctor find where the heart’s electrical system is damaged.
Blood tests
Your doctor may recommend blood tests to check the levels of potassium, magnesium, and other chemicals in your blood. These chemicals play an important role in your heart’s electrical signaling.
Sudden cardiac arrest treatment
Sudden cardiac arrest is an emergency. A person having sudden cardiac arrest needs to be treated with a defibrillator right away. This device sends an electric shock to the heart. The electric shock can restore a normal rhythm to a heart that’s stopped beating. To work well, defibrillation must be done within minutes of sudden cardiac arrest. With every minute that passes, the chances of surviving sudden cardiac arrest drop rapidly.
Police, emergency medical technicians, and other first responders usually are trained and equipped to use a defibrillator. Call your local emergency services number right away if someone has signs or symptoms of sudden cardiac arrest. The sooner you call for help, the sooner lifesaving treatment can begin.
Automated External Defibrillators
Automated external defibrillators (AEDs) are special defibrillators that untrained bystanders can use. These portable devices often are found in public places, such as shopping malls, golf courses, businesses, airports, airplanes, casinos, convention centers, hotels, sports venues, and schools.
Automated external defibrillators are programmed to give an electric shock if they detect a dangerous arrhythmia, such as ventricular fibrillation. This prevents giving a shock to someone who may have fainted but isn’t having sudden cardiac arrest.
You should give cardiopulmonary resuscitation (CPR) to a person having sudden cardiac arrest until defibrillation can be done.
People who are at risk for sudden cardiac arrest may want to consider having an automated external defibrillator at home. A 2008 study by the National Heart, Lung, and Blood Institute and the National Institutes of Health found that automated external defibrillators in the home are safe and effective.
Some people feel that placing these devices in homes will save many lives because many sudden cardiac arrests occur at home. Others note that no evidence supports the idea that home-use automated external defibrillators save more lives. These people fear that people who have automated external defibrillators in their homes will delay calling for help during an emergency. They’re also concerned that people who have home-use automated external defibrillators will not properly maintain the devices or forget where they are.
When considering a home-use automated external defibrillator, talk with your doctor. He or she can help you decide whether having an automated external defibrillator in your home will benefit you.
Treatment in a hospital
If you survive sudden cardiac arrest, you’ll likely be admitted to a hospital for ongoing care and treatment. In the hospital, your medical team will closely watch your heart. They may give you medicines to try to reduce the risk of another sudden cardiac arrest.
While in the hospital, your medical team will try to find out what caused your sudden cardiac arrest. If you’re diagnosed with ischemic heart disease, you may have percutaneous coronary intervention, also known as coronary angioplasty, or coronary artery bypass grafting. These procedures help restore blood flow through narrowed or blocked coronary arteries.
Often, people who have sudden cardiac arrest get a device called an implantable cardioverter defibrillator (ICD). This small device is surgically placed under the skin in your chest or abdomen. An ICD uses electric pulses or shocks to help control dangerous arrhythmias.
Long-term treatment
After you recover, your doctor will discuss with you or your family what other tests might help determine the cause of the cardiac arrest. Your doctor will also discuss preventive treatment options with you to reduce your risk of another cardiac arrest.
Treatments might include:
- Drugs. Doctors use various anti-arrhythmic drugs for emergency or long-term treatment of arrhythmias or potential arrhythmia complications. A class of medications called beta blockers is commonly used in people at risk of sudden cardiac arrest. Other possible drugs that can be used to treat the condition that led to the arrhythmia include angiotensin-converting enzyme (ACE) inhibitors and calcium channel blockers.
- Implantable cardioverter-defibrillator (ICD). After your condition stabilizes, your doctor is likely to recommend an ICD, a battery-powered unit that’s put into your body near your left collarbone. One or more electrode-tipped wires from the ICD run through veins to your heart. The ICD constantly monitors your heart rhythm. If it detects a rhythm that’s too slow, it paces your heart as a pacemaker would. If it detects a dangerous heart rhythm change, it sends out low- or high-energy shocks to reset your heart to a normal rhythm.
- Coronary angioplasty. This procedure opens blocked coronary arteries, letting blood flow more freely to your heart, which might reduce your risk of serious arrhythmia. A long, thin tube is passed through an artery, usually in your leg, to a blocked artery in your heart. This catheter is equipped with a special balloon tip that briefly inflates to open the blocked artery. At the same time, a metal mesh stent might be inserted into the artery to keep it open long term, restoring blood flow to your heart. Coronary angioplasty can be done at the same time as a coronary catheterization, a procedure that doctors do to locate narrowed arteries to the heart.
- Coronary bypass surgery also called coronary artery bypass grafting (CABG), bypass surgery involves sewing veins or arteries in place at a site beyond a blocked or narrowed coronary artery, restoring blood flow to your heart. This can improve the blood supply to your heart and reduce the frequency of racing heartbeats.
- Radiofrequency catheter ablation. This procedure can be used to block a single abnormal electrical pathway. One or more catheters are threaded through your blood vessels to inside your heart. They’re positioned along electrical pathways identified by your doctor as causing your arrhythmia. Electrodes at the catheter tips are heated with radiofrequency energy. This destroys a small spot of heart tissue and creates an electrical block along the pathway that’s causing your arrhythmia to stop your arrhythmia.
- Corrective heart surgery. If you have a congenital heart deformity, a faulty valve or diseased heart muscle tissue due to cardiomyopathy, surgery to correct the abnormality might improve your heart rate and blood flow, reducing your risk of fatal arrhythmias.
Prognosis for Cardiac Arrest Survivors
The majority of cardiac arrest survivors have some degree of brain injury and impaired consciousness. Some remain in a persistent vegetative state. Determining the survivor’s prognosis and making the decision to treat or to withdraw care is complicated and based on many variables (many of which have not been thoroughly studied).
Factors before cardiac arrest:
- Age
- Ethnicity
- Poor health including diabetes, cancer, infection, kidney disease and stroke
Factors during cardiac arrest:
- Time between collapse and start of CPR/defibrillation
- Quality of CPR/defibrillation
- Whether survivor had any neurological function during or immediately after CPR
Factors after cardiac arrest and resuscitation:
- Neurological function: Generally, poor function equals poor prognosis but could be complicated by medical instability and treatments. Some patients suffer a stroke after a cardiac arrest.
- Neurophysiologic function: tests include somatosensory evoked potentials (SSEP) and electroencephalogram (EEG).
- Neuroimaging and monitoring: to determine structural brain injury — such as cranial CT, MRI, magnetic resonance spectroscopy, positron emission tomography (PET) — mostly to exclude hemorrhage or stroke.
- Biochemistry: from blood or cerebrospinal fluid
- Whether therapeutic hypothermia (intentionally lowering the patient’s body temperature) was used.
Changes after a cardiac arrest
Because of a lack of oxygen to the brain during a cardiac arrest, you might experience long-term effects to your brain. People who have a cardiac arrest often can’t remember what happened. This is because their brain was starved of oxygen at the time. This can cause them to have memory loss or personality changes. Afterwards they may have been put in an induced coma to help them recover. If you continue to feel anxious and you’re unable to cope, it’s important to speak to your family doctor.
Changes after a cardiac arrest can include:
- personality changes
- problems with memory
- fatigue
- dizziness or balance issues
- aphasia/dysphasia (problems with speech and language)
- myoclonus (involuntary movements)
- permanent brain injury.
It’s also common to feel low, angry, confused or a combination of lots of different emotions due to the shock of the experience. Speak to your doctor if you’re concerned about your mental health as they may be able to refer you to counseling or cognitive behavioral therapy (CBT).
References- Perkins GD, Ji C, Achana F, et al. Adrenaline to improve survival in out-of-hospital cardiac arrest: the PARAMEDIC2 RCT. Southampton (UK): NIHR Journals Library; 2021 Apr. (Health Technology Assessment, No. 25.25.) Chapter 1, Introduction. Available from: https://www.ncbi.nlm.nih.gov/books/NBK569521
- Huikuri HV, Castellanos A, Myerburg RJ. Sudden death due to cardiac arrhythmias. N Engl J Med. 2001;345 (20):1473–1482.
- Kuller LH. Sudden death–definition and epidemiologic considerations. Prog Cardiovasc Dis. 1980 Jul-Aug;23(1):1-12. doi: 10.1016/0033-0620(80)90002-x
- Centers for Disease Control and Prevention (CDC). State-specific mortality from sudden cardiac death–United States, 1999. MMWR Morb Mortal Wkly Rep. 2002 Feb 15;51(6):123-6.
- Becker LB, Smith DW, Rhodes KV. Incidence of cardiac arrest: a neglected factor in evaluating survival rates. Ann Emerg Med. 1993 Jan. 22 (1):86-91.