What is carotid endarterectomy
Carotid endarterectomy is a type of surgery used to remove plaque from inside a carotid artery in your neck. Carotid endarterectomy surgery is done to restore normal blood flow to the brain to prevent a stroke if you already have symptoms of reduced blood flow. Carotid endarterectomy also may be performed preventively if a diagnostic test such as carotid ultrasound shows significant blockage that is likely to trigger a stroke. Carotid endarterectomy is not a cure. Your arteries can become blocked again if your underlying condition, such as high blood cholesterol, is not controlled and causes new plaque buildup.
Carotid endarterectomy is the third most common kind of cardiovascular surgery in the United States.
During the carotid artery endarterectomy, the surgeon peels the plaque away from the carotid artery. Once the plaque is removed from the carotid artery, more oxygen-rich blood can flow through the artery to the brain, reducing the risk of stroke.
Your doctor may want you to have a carotid endarterectomy if a carotid artery is narrowed 70% or more and if the narrowing may have caused:
- A transient ischemic attack (TIA) or “mini stroke.” TIAs are episodes of dizziness, tingling, numbness, blurred vision, confusion, or paralysis that can last anywhere from a few minutes to a couple of hours.
- A stroke marked by loss of vision, persistent weakness, or paralysis.
Your doctor may also recommend the operation if you have not had a transient ischemic attack (TIA) or stroke, but your carotid arteries are narrowed 80% or more.
Patients with mild blockages of 50% or less usually do not need the carotid endarterectomy surgery, unless they have some of the symptoms mentioned above.
Carotid endarterectomy can prevent a future stroke and help ease the symptoms of transient ischemic attacks (TIAs). Studies have shown that a carotid endarterectomy works better than medicines alone in preventing a stroke in people with blockages in the carotid arteries.
But a carotid endarterectomy may not be suitable for everyone, because the carotid endarterectomy surgery can be risky for patients whose overall health is poor. Patients may not be candidates for carotid endarterectomy if they have:
- TIAs that are a result of narrowed blood vessels in the back of the head and not the carotid arteries.
- Severe coronary artery disease.
- High blood pressure that is not controlled by medicines.
- Severe hardening of the arteries (atherosclerosis) in many places in the body.
- Heart failure.
- Kidney failure.
Carotid endarterectomy is done in a hospital. You may have general anesthesia and will not be awake or feel pain during the surgery. Your surgeon instead may decide to use local anesthesia to numb only the part of your body being worked on so that he or she can check your brain’s reaction to the decreased blood flow during surgery. You also will be given medicine to relax you during the surgery. Your vital signs will be monitored during surgery. You will lie on your back on an operating table with your head turned to one side. Your surgeon will make an incision, or cut, on your neck to expose the blocked section of the carotid artery. Your surgeon will cut into the affected artery and remove the plaque through this cut. A temporary flexible tube may be inserted so blood can flow around the blocked area as the plaque is cleared. After removing the plaque from your artery, the surgeon will close the artery and neck incisions with stitches.
After carotid endarterectomy surgery, you will recover in the hospital for one to two days. Your neck may hurt for a few days, and you may find it hard to swallow. Your doctor may prescribe medicine to prevent clots and suggest steps to keep your carotid arteries healthy.
Carotid endarterectomy is fairly safe when performed by experienced surgeons. However, serious complications such as clotting, stroke, or death may occur. Taking anticlotting medicines before and after surgery can reduce this risk. Other complications may include a reaction to anesthesia, short-term nerve injury that causes temporary numbness in your face or tongue, bleeding, infection, high blood pressure, heart attack, and seizure. The risk of complications is higher in women, older people, those with certain conditions such as chronic kidney disease or diabetes, and those with other serious medical conditions.
Carotid endarterectomy anatomy
Within the superior mediastinum, the arch of the aorta can be found at the level of the sternal angle. Three large vessels originate from the aorta. This includes the brachiocephalic trunk, the left common carotid artery, and left subclavian artery. On the right side, the common carotid artery stems off as the first branch the brachiocephalic trunk. Both the left and right common carotids will bifurcate into an internal and external carotid artery. This division occurs around the fourth cervical vertebrae (C4) along the superior border of the thyroid cartilage. There is a deep cervical fascia that forms the carotid sheath. This surrounds the carotid arteries, internal jugular vein, and vagus nerve. They are found medially to the sternocleidomastoid muscle. The internal carotid artery will continue into the skull to form part of the Circle of Willis and supply blood to the brain and eyes. Branches of the external carotid artery supply blood to the neck and face.
The left and right common carotid arteries diverge into the internal and external carotid arteries. The external carotid artery courses upward on the side of the head, giving off branches to structures in the neck, face, jaw, scalp, and base of the skull. The internal carotid artery begins lateral to the external carotid artery, then extends medially to follow a deep course upward along the pharynx to the base of the skull. Entering the cranial cavity, it provides the major blood supply to the brain. Near the base of each internal carotid artery is an enlargement called a carotid sinus. Like the aortic arch, these structures contain baroreceptors
that control blood pressure.
External carotid artery via its branches supply blood, oxygen and nutrients to your:
- Larynx and thyroid gland
- Tongue and salivary glands
- Pharynx, palate, chin, lips, and nose
- Posterior scalp, meninges, and neck muscles
- Ear and lateral scalp
- Teeth, jaw, cheek, and eyelids
- Parotid salivary gland and surface of the face and scalp
Internal carotid artery via its branches supply blood, oxygen and nutrients to your:
- Eye and eye muscles
- Choroid plexus and brain
- Frontal lobes of the brain
- Parietal lobes of brain
Figure 1. Carotid artery anatomy
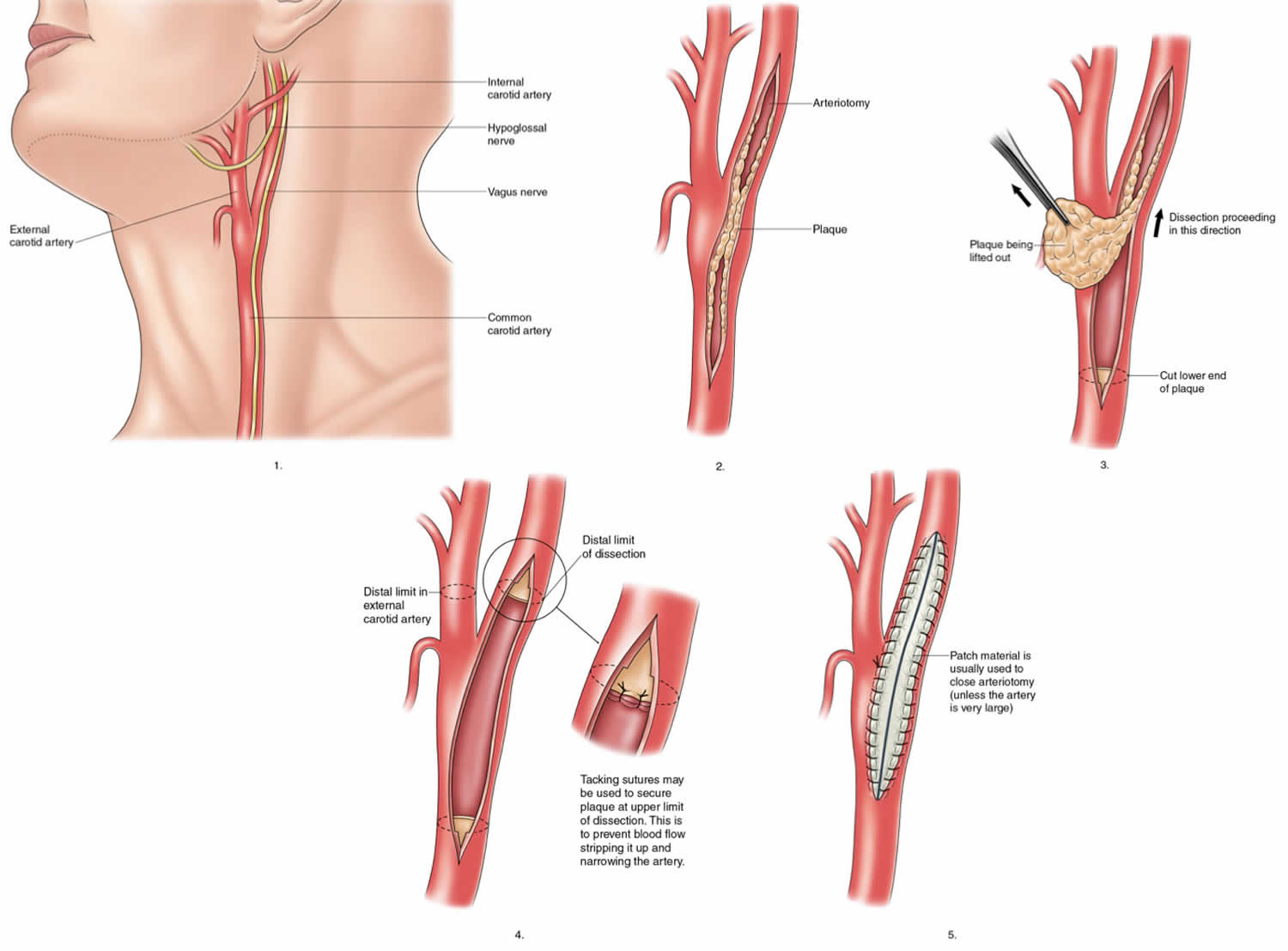
Figure 2. Carotid endarterectomy
Carotid endarterectomy indications
Doctors may recommend carotid endarterectomy if you have a severe narrowing in your carotid artery. There are several other factors that will be considered other than the degree of blockage in the artery. You may or may not be experiencing symptoms. Your doctor will evaluate your condition and determine whether you’re a candidate for carotid endarterectomy.
If carotid endarterectomy isn’t the best option for you, you might have a procedure called carotid angioplasty and stenting instead of carotid endarterectomy. In this procedure, doctors thread a long hollow tube (catheter) with a small balloon attached through a blood vessel in your neck to the narrowed artery. The balloon is then inflated to widen the artery. A metal mesh tube (stent) is often inserted to decrease the chance of the artery narrowing again.
Carotid artery disease (also called cerebrovascular disease) affects the vessels leading to the brain. Like the heart, the brain’s cells need a constant supply of oxygen-rich blood. This blood supply is delivered to the brain by the 2 large carotid arteries in the front of your neck and by 2 smaller vertebral arteries at the back of your neck. The right and left vertebral arteries come together at the base of the brain to form what is called the basilar artery. A stroke may occur when the carotid arteries become blocked and the brain does not get enough oxygen.
Carotid artery disease increases the risk of stroke in 3 ways:
- By fatty deposits called plaque severely narrowing the carotid arteries.
- By a blood clot becoming wedged in a carotid artery already narrowed by plaque.
- By plaque or a clot breaking off from the carotid arteries and blocking a smaller artery in the brain (a cerebral artery).
In 1987 the North American Symptomatic Carotid Endarterectomy Trials (NASCET) began. Patients with moderate carotid stenosis (less than 70%) and severe carotid stenosis (greater than 70%) were randomly assigned to treatment groups, which included antithrombotic medication for a majority of patients. The study found that the benefit of surgery was great for those who had severe carotid stenosis, and patients with less than 50% stenosis were found to have no benefit. Patients who have 50% or more narrowing of the carotid artery and history of ipsilateral stroke or TIA are recommended to have carotid endarterectomy surgery. Symptoms of TIA can include amaurosis fugax, a painless temporary loss of vision in one or both eyes, hemiparesis, and speech loss episode.
Asymptomatic patients with 70% or more narrowing, also are encouraged to undertake the surgery. In the Asymptomatic Carotid Artery Stenosis (ACAS) trials for endarterectomy, it was shown that after the procedure there is a significant 5-year reduction in stroke risk in asymptomatic patients. As medical therapy has improved since the 1980s, the CREST-2 trial is currently underway. The trial will provide data about best medical therapy versus surgery in patients with asymptomatic, high grade internal carotid stenosis.
It is possible to screen asymptomatic patients with the use of carotid duplex ultrasonography. It can assess the degree of carotid stenosis. The severity of the obstruction correlates to carotid velocity. Inaccuracies can be shown if there are blood vessel kinks and bends which may cause elevated velocities. Although it is a great tool for detecting hemodynamically significant stenosis, it has relatively low specificity for those patients with 50% to 60% stenosis. Other forms of screening include computed tomography angiography, and contrast-enhanced magnetic resonance angiography. They help to assess other variables that can impact an individuals risk including plaque morphology, intracranial collateralization, and brain perfusion. Computed tomography angiography or contrast-enhanced magnetic resonance angiography information can be used alongside carotid duplex ultrasonography to help put into perspective a patient’s need for surgery 1.
For patients with symptomatic carotid occlusion (50-99%), if carotid endarterectomy was done within 2 weeks of symptoms, the number needed to treat for preventing one stroke is 5. The number needed to treat increases to 125 if it has done more than 2 weeks of symptoms or stroke onset. Carotid endarterectomy is beneficial if the symptoms are non-disabling, no tandem stenoses, high-grade stenosis. Carotid endarterectomy surgery can be deferred if the stroke is too big, contralateral carotid occlusion, hemodynamic instability, and contralateral laryngeal palsy is a relative contraindication. There is more myocardial infarction associated with carotid artery endarterectomy 2.
Carotid artery stenting is preferred in symptomatic carotid occlusion (50-99%) with multiple comorbidities, tracheostomy, patients with prior neck radiation or dissection. Usually, there is an increased risk of stroke after the carotid artery stenting. Due to the advancement of the stents and technique, carotid artery stenting is comparable to carotid artery endarterectomy in most instances. CREST-2 study is ongoing and will shed more light in this important area 2.
Carotid endarterectomy contraindications
Symptomatic patients who are very ill and unable to undergo surgery may be candidates for carotid angioplasty and stenting (carotid artery stenting). The stent, a small, flexible, mesh-like tube is inserted into the artery under local anesthesia. The tube is then expanded to move plaque deposit out of the way and allow for more blood flow through the area. It was found from the Carotid Revascularization Endarterectomy Versus Stenting Trials (CREST) that carotid endarterectomy and carotid artery stenting did not yield significant differences when considering postoperative complications like restenosis, myocardial infarction, periprocedural stroke, ipsilateral stroke, and/or death. However, differences in the risk of stroke or death were higher in patients that underwent carotid artery stenting. Other considerations for stenting is if the patient is at high risk for general anesthesia complications.
Patients who have undergone neck radiotherapy, inducing stenosis, are at higher risk of developing temporary cranial nerve injury during endarterectomy, and late cerebrovascular events and restenosis following angioplasty and stenting. Endarterectomy is more challenging because these patients tend to have more diffuse plaques, as well as adhesions, scar tissue, and wound complications if prior radical neck dissection is done.
Women are at higher risk of developing complications because they have smaller carotid arteries. A study using multivariate regression compared the diameters of the common and internal carotid arteries in men and women based on age, weight, height, body mass index (BMI), neck circumference, body surface area, neck length, and blood pressure. Even with controlling for confounding variables such as blood pressure, body size, neck size, and age, women were found to have smaller arteries and a slightly smaller left common carotid when compared to the right. Women with asymptomatic carotid stenosis may benefit less from carotid endarterectomy surgery and could experience early complications from the surgery.
Carotid endarterectomy preparation
A patient undergoing carotid endarterectomy should be on antiplatelet therapy (unless contraindicated) before the surgery.
Before surgery, you may have to have an electrocardiogram (ECG or EKG) [no link], blood tests, urine tests, and a chest x-ray to give your surgeon the latest information about your health.
If you smoke, your doctor will want you to stop at least 2 weeks before your surgery. Smoking before surgery can lead to problems with blood clotting and breathing.
The night before surgery, you will be asked to bathe to reduce the amount of germs on your skin. A medicine (anesthetic) will make you sleep during the operation. This is called “anesthesia.” Because anesthesia is safest on an empty stomach, you will be asked not to eat or drink after midnight the night before surgery. If you do eat or drink anything after midnight, it is important that you tell your anesthesiologist and surgeon.
You will get complete instructions from your cardiologist and surgeon about the procedure, but here are some basics you can expect as a patient.
How is a carotid endarterectomy performed?
Most patients are admitted to the hospital the day before surgery or, in some cases, on the morning of carotid endarterectomy surgery.
Small metal disks called electrodes will be attached to your chest. These electrodes are connected to an electrocardiogram machine, which will monitor your heart’s rhythm and electrical activity. You will receive a local anesthetic to numb the area where a plastic tube (called a line) will be inserted in an artery in your wrist. An intravenous (IV) line will be inserted in your vein. The IV line will give you the anesthesia during the operation. You will be given something to help you relax (a mild tranquilizer) before you are taken into the operating room.
During carotid endarterectomy:
- You receive general anesthesia. You are asleep and pain free. Some hospitals use local anesthesia instead. Only the part of your body being worked on is numbed with medicine so that you do not feel pain. You are also given a medicine to help you relax.
- After you are completely asleep, a tube will be inserted down your windpipe and connected to a machine called a respirator, which will take over your breathing. Another tube will be inserted through your nose and down your throat, into your stomach. This tube will stop liquid and air from collecting in your stomach, so you will not feel sick and bloated when you wake up. A thin tube called a catheter will be inserted into your bladder to collect any urine produced during the operation.
- You lie on your back on an operating table with your head turned to one side. The side your blocked carotid artery is on faces up.
- The surgeon will make a cut (called an incision) on your neck over your carotid artery. The surgeon places a flexible tube called a shunt into the artery above and below the blockage. The shunt lets blood flow around the blocked area to nourish your brain.
- Your carotid artery is opened. The surgeon removes the plaque inside the artery.
- When all of the plaque is removed, the shunt is removed, and the incision in the artery is closed by stitching a patch of fabric (Dacron) or vein into the incision.
- Blood now flows through the artery to your brain.
- Your heart activity will be monitored closely during surgery.
A carotid endarterectomy can also be done by a technique that does not require blood flow to be rerouted. In this procedure, the surgeon stops the blood flow just long enough to peel the blockage away from the artery.
The carotid endarterectomy surgery takes about 2 hours. After the carotid endarterectomy procedure, your doctor may do a test to confirm that the carotid artery has been opened.
Carotid endarterectomy technique
There are two main surgical techniques for carotid endarterectomy: the classical/conventional method and the eversion method.
Classical/Conventional Method
The surgeon makes an incision alongside the medial aspect of the sternocleidomastoid muscle, cutting through fat, the platysma muscle, and eventually reaching the carotid sheath. After carefully removing part of the sheath, the carotid arteries are exposed. The internal carotid artery is clamped down to temporarily stop blood flow. The surgeon will open a long the length of the internal carotid artery, as much needed to find the plaque. Before removing the plaque, the clamps are taken off the artery, and a flexible tube is placed to shunt blood around the endarterectomy site. After the blockage is removed, the artery is sewn closed with a patch that will widen the vessel. There are different options for patches, including the patient’s vein, bovine patch, or artificial patch (Dacron). After the patch is sewn on, it is important to confirm satisfactory blood flow with ultrasound Doppler or angiography.
Eversion Method
With the eversion method, the internal carotid artery is cut obliquely at the base where it originates from the bifurcation of the common carotid artery. It is shortened and partially everted. The plaque is divided and removed. Sutures then close the artery. The benefits of this include no need for patch closure, the operation time and carotid clamping time is also reduced.
Carotid endarterectomy risks
Risks of anesthesia are:
- Allergic reactions to medicines
- Breathing problems
Risks of carotid surgery are:
- Blood clots or bleeding in the brain
- Brain damage
- Heart attack
- More blockage of the carotid artery over time
- Seizures
- Stroke
- Swelling near your airway (the tube you breathe through)
- Infection
Carotid endarterectomy complications
Complications during and after carotid endarterectomy surgery are dependent on various factors, such as surgeon skill and technique, patient’s risk factors, management before or after surgery.
Complications of carotid endarterectomy include:
Major complications
- Myocardial Infarction
- Hyperperfusion syndrome
- Nerve Injury, particularly the cranial nerves; hypoglossal, vagus, glossopharyngeal, trigeminal, and facial nerves
- Perioperative stroke
- Death
Minor complications
- Restenosis
- Transient ischemic attack
- Bleeding
- Cervical hematoma
- Infection
Carotid endarterectomy recovery
You can expect to stay in the hospital for about 1 to 3 days, including 1 day in the Intensive Care Unit (ICU). During that time in the hospital, you will need to lie flat and not move your head too much. You may have a drain in your neck that goes into your incision. It will drain fluid that builds up in the area. It will be removed within a day.
You may find that your neck aches, and this may last for up to 2 weeks. Try to avoid physically demanding activities for about 1 week. It may take as long as 2 weeks before you are totally healed.
Life after carotid endarterectomy
After a carotid endarterectomy, you should limit the fat and cholesterol in your diet. Your doctor may want you to start an exercise program. Other lifestyle changes include quitting smoking, limiting how much alcohol you drink, and controlling your blood pressure and cholesterol levels.
References- Babić S, Tanasković S, Nešković M, Gajin P, Nenezić D, Stevanović P, Aleksić N, Ševković M, Ilijevski N, Matić P, Popov P, Vučurević G, Unić-Stojanović D, Radak D. Surgical Treatment of Proximal Segmental Occlusion of the Internal Carotid Artery. Surg Res Pract. 2019;2019:2976091
- DaCosta M, Tadi P, Surowiec SM. Carotid Endarterectomy. [Updated 2019 Mar 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470582