Cervical kyphosis
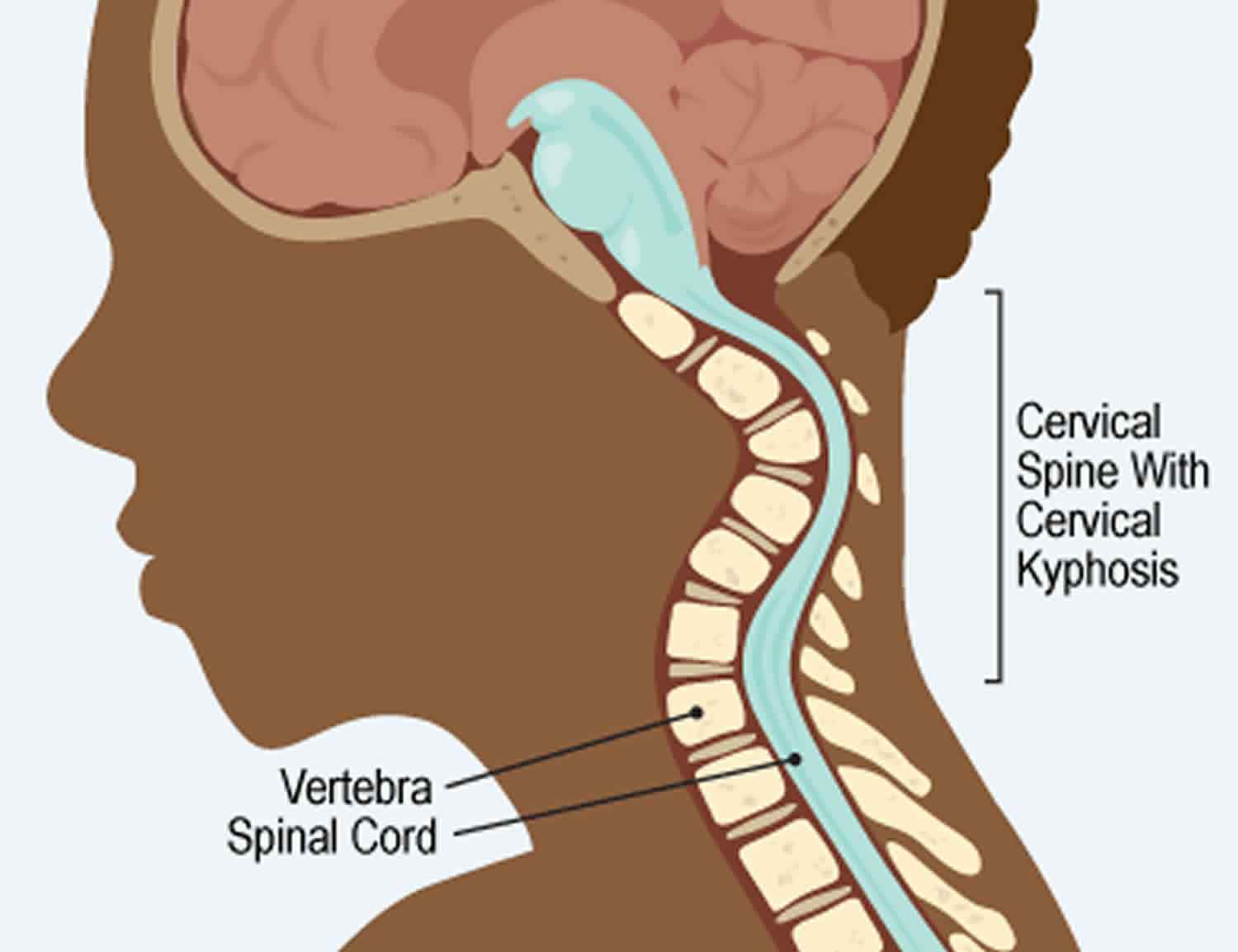
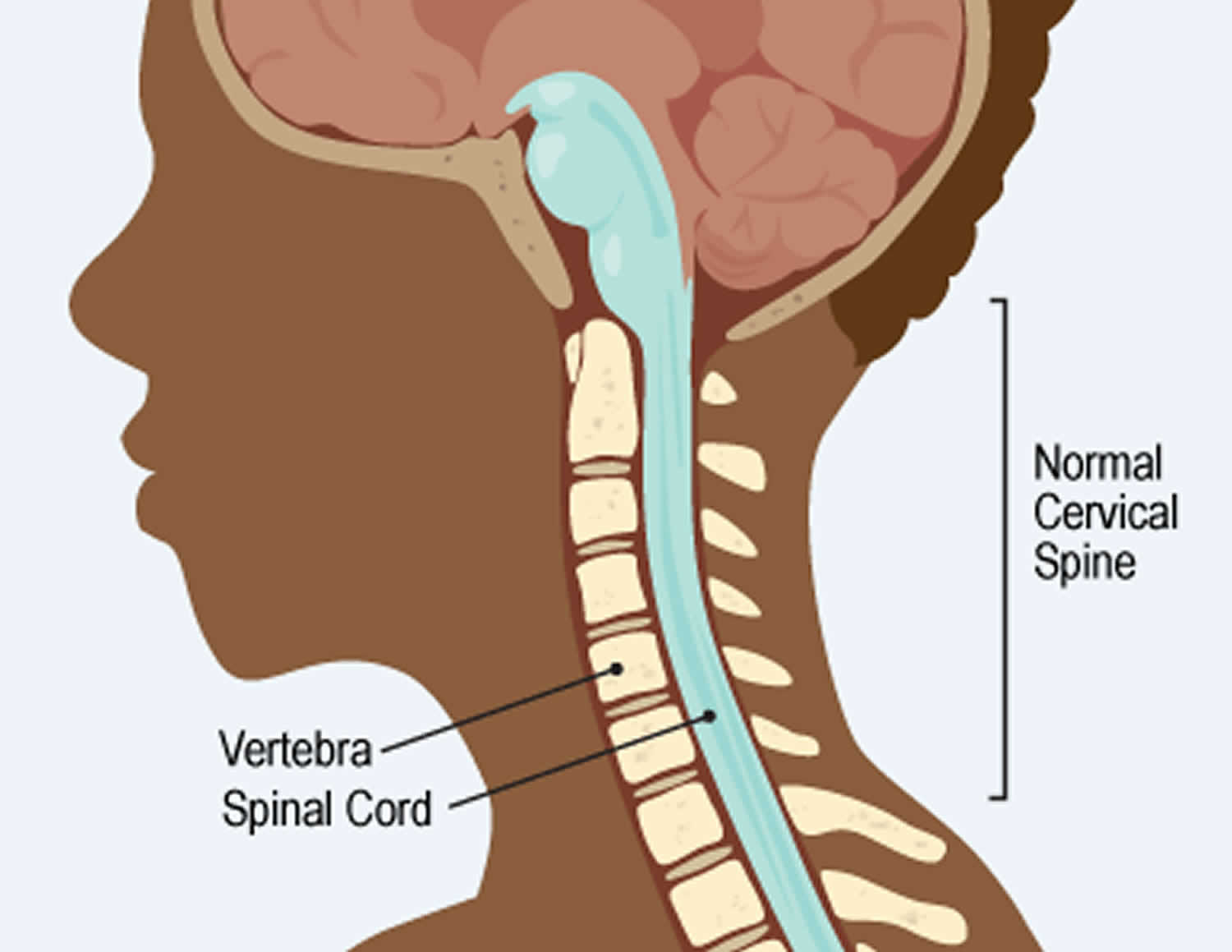
Cervical kyphosis is when the cervical spine (the neck) curves in the opposite direction than normal 1. Cervical kyphosis can be either regional or global, and has been shown to be associated with reduced quality of life 2. Cervical kyphosis can lead to problems 3. However, most cervical kyphosis isn’t serious. But if the curve is severe, bones in the spine called vertebrae might pinch the spinal cord. This can damage the spinal cord.
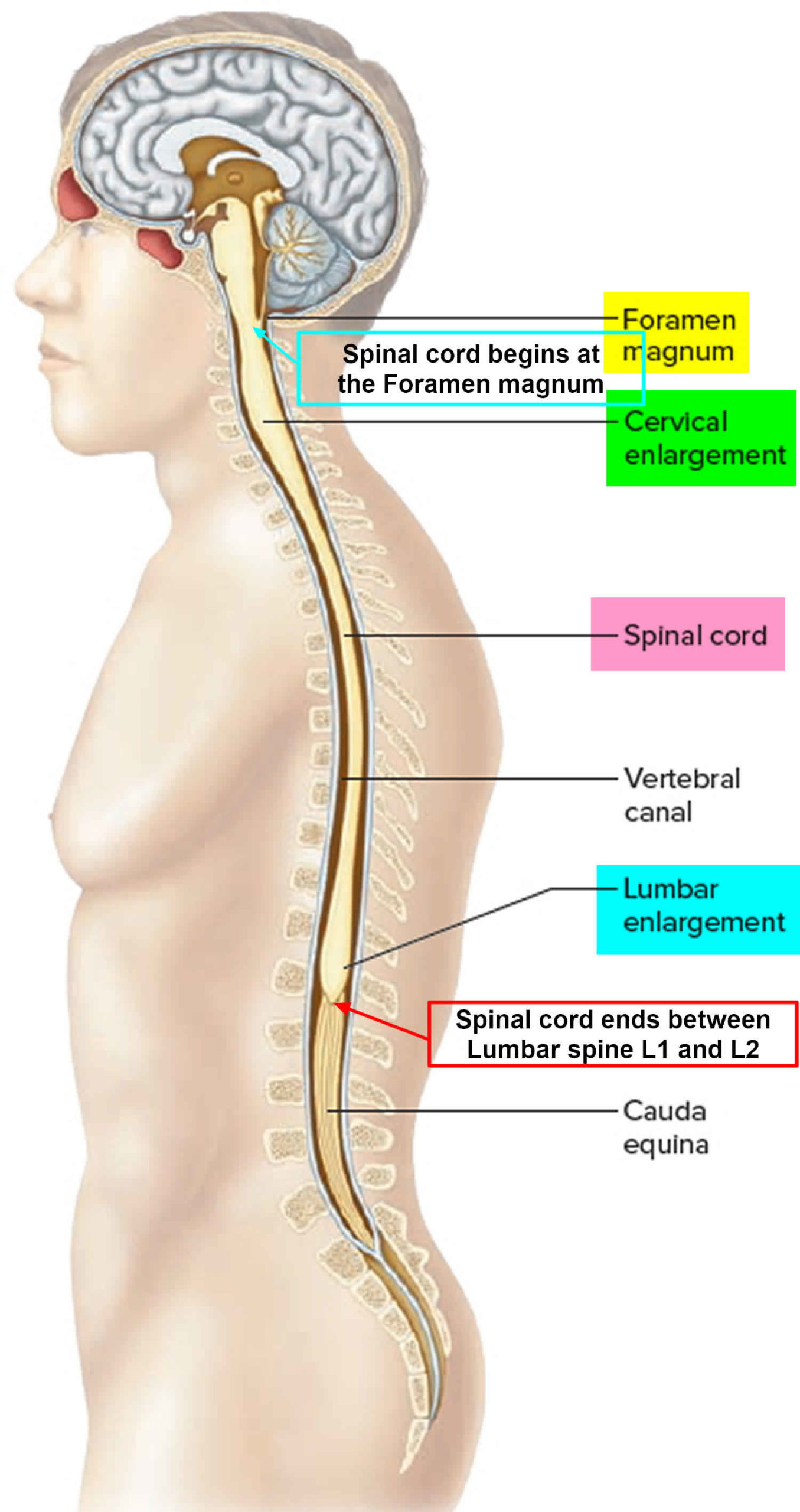
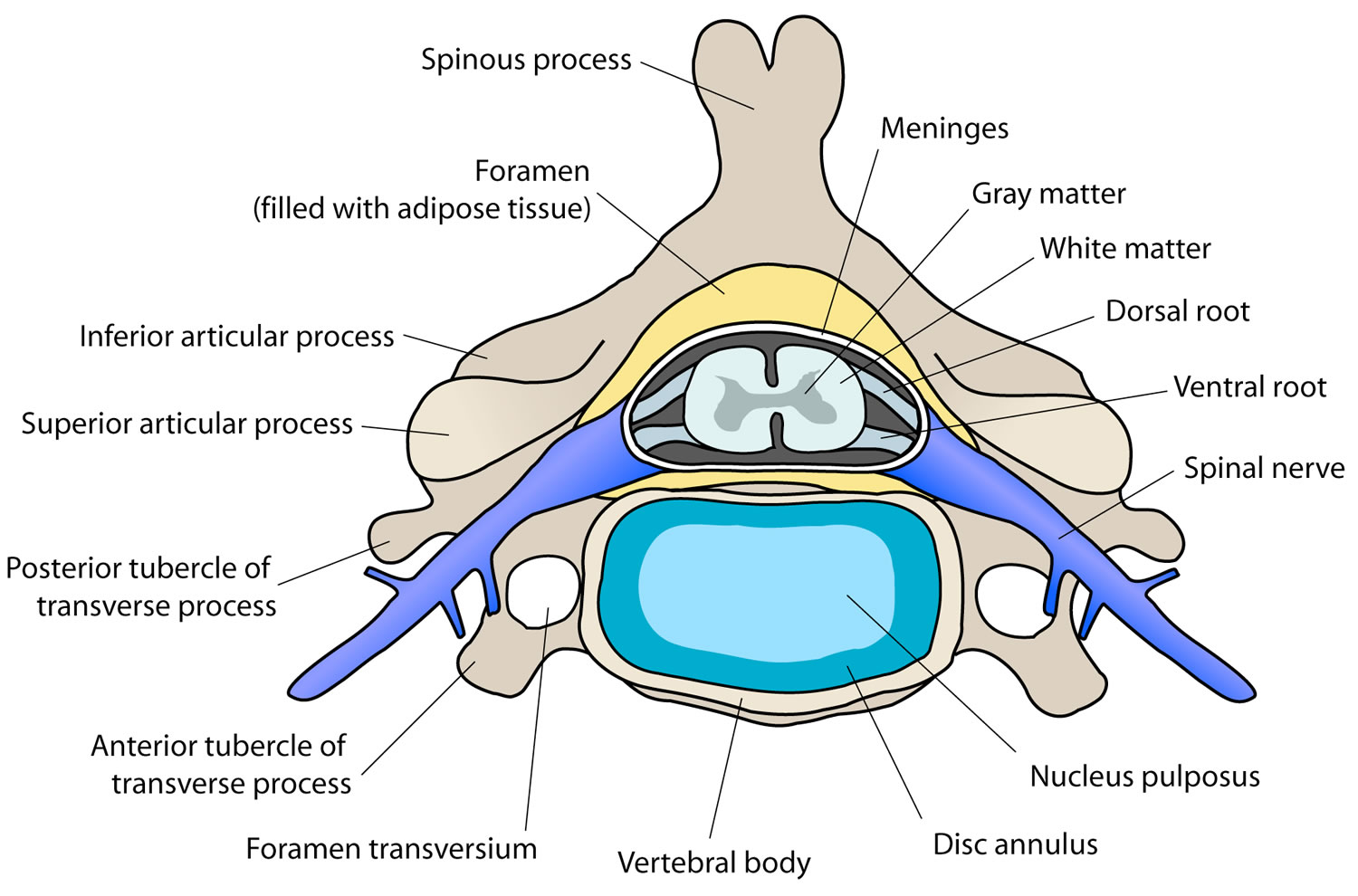
The spinal cord is the body’s central communication system (see Figure 3 below). It’s a tube of nerves that runs inside the spine. The nerves branch out to every part of the body. They send messages between the brain and the rest of the body. If damage is very bad, the nerves can’t send important signals like telling the lungs to breathe or blood to move around the body.
Cervical kyphosis isn’t common. It can happen to any child, but kids who have it often have another health problem too.
Parents can’t stop cervical kyphosis from happening. But they can help kids get the best care.
It’s important to diagnose spine problems early. If kids don’t get treatment, some may end up with spinal cord damage that can’t be fixed.
Here are tips for avoiding problems:
- See a doctor if your child has trouble with head movements or neck pain. Neck trouble needs to be checked out to be sure it’s not something serious.
- Go to all medical appointments if your child has cervical kyphosis. Even a small curve can get bigger as a child grows. The care team will want to keep watching for possible problems.
- If your child had surgery, ask the care team when you should bring your child for follow-up visits. The will check your child to be sure the kyphosis does not come back.
The care team is a resource — for you and your child. They can answer questions and help your child get the best treatment. So reach out for help and answers when you need to.
Managing cervical kyphosis is challenging for the spinal surgeon, and setting realistic surgical goals and meticulous preoperative planning can achieve the optimal clinical outcomes, while managing the condition 1.
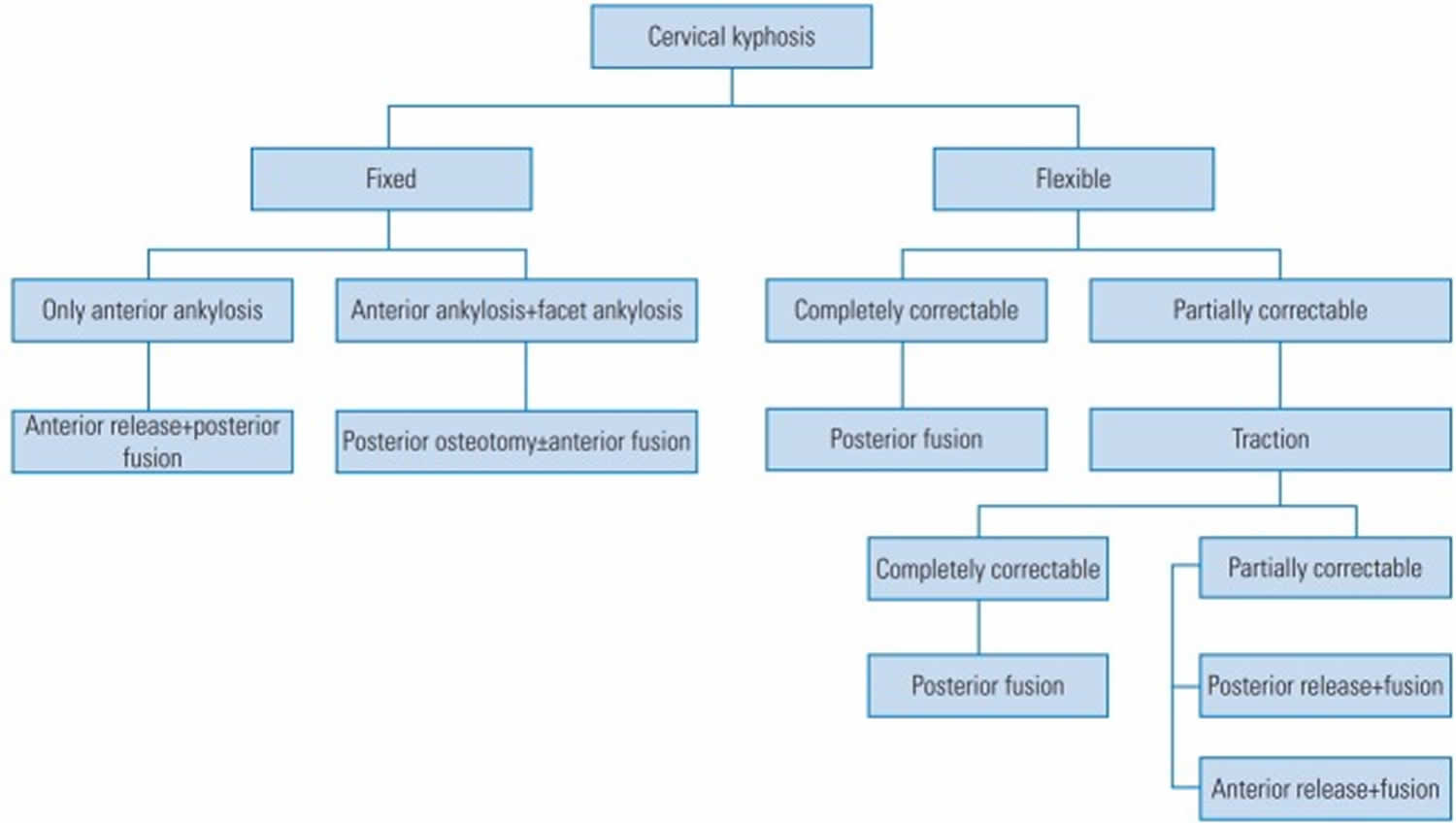
Surgical treatment of this challenging pathology is a daunting task and focuses on neural decompression, and improvement in alignment and stabilization of the cervical spine 1. Flexible deformities are preferably managed by posterior stabilization provided the alignment of cervical spine is restored optimally. Fixed deformities are treated using skeletal traction for a brief period before deciding the surgical approach. An anterior approach is preferable in short segment cervical kyphosis with anterior compression of spinal cord requiring one to two-level corpectomy. A circumferential approach has the advantage of rigid fixation and restoration of posterior tension band. Though radical, it reduces the chances of instrumentation failure, graft extrusion, and pseudoarthrosis. As the benefits of this approach outweigh the potential complications, the morbidity of circumferential cervical spine surgeries is decreased by use of proper techniques and experience 1.
Figure 1. Cervical kyphosis
Figure 2. Normal cervical spine
Figure 3. Spinal cord
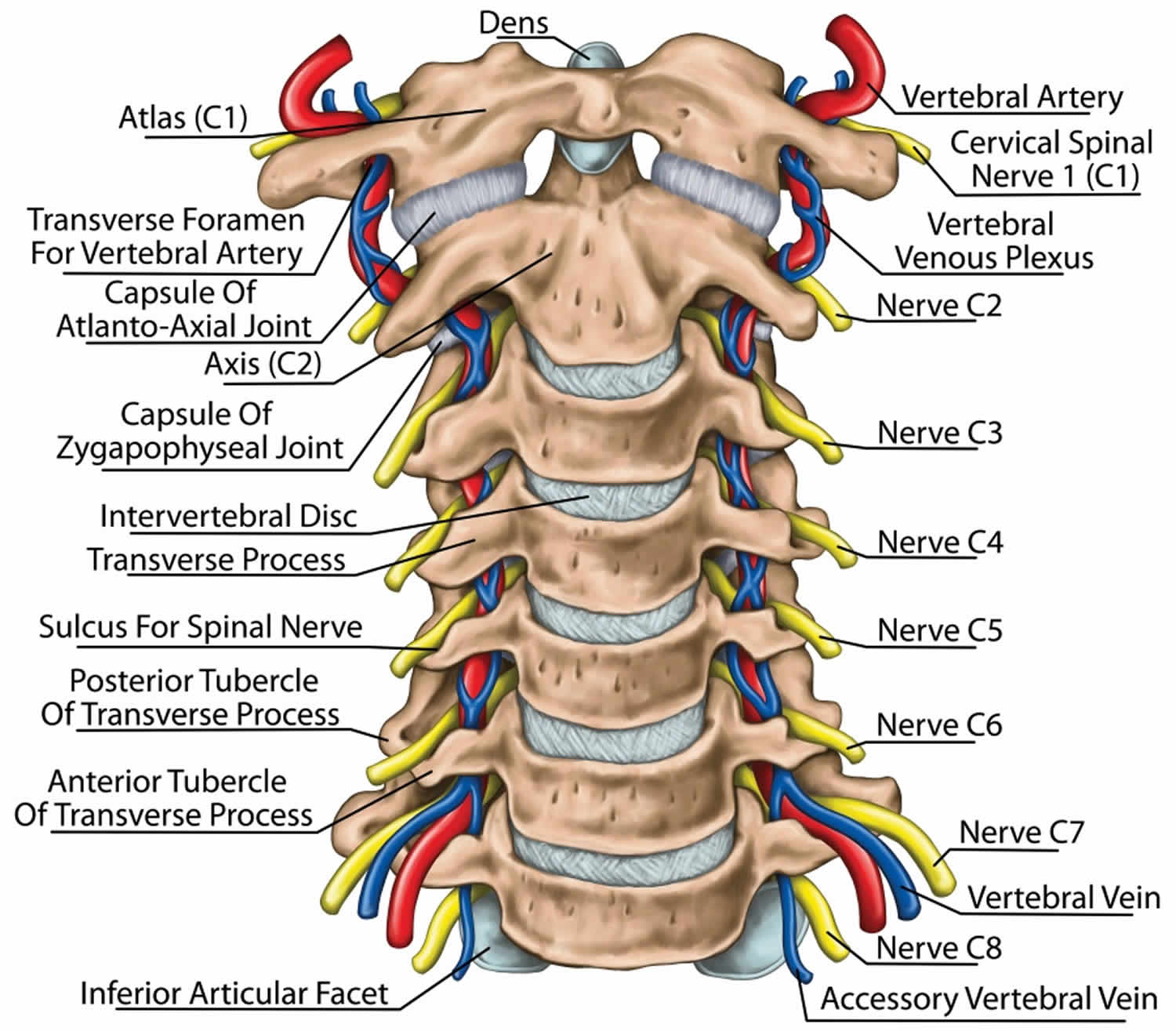
Figure 4. Cervical spine
Figure 5. Cervical spine anatomy
Figure 6. Cervical kyphosis treatment algorithm
[Source 1 ]Cervical kyphosis causes
Kids can get cervical kyphosis in three ways:
1. They are born with it.
- This is called congenital cervical kyphosis. No one knows what causes it. Doctors do know that it has nothing to do with anything a mom did when she was pregnant.
2. Something goes wrong in the body.
- This is called acquired cervical kyphosis. Lots of different things can cause it, such as:
- injury to the bones of the spine or the ligaments around them
- infection
- tumors
- surgery
- radiation therapy for cancer
3. They have another condition that causes them to get kyphosis.
For example:
- skeletal dysplasia
- spina bifida
- osteogenesis imperfecta
- neurofibromatosis type 1
Cervical kyphosis signs and symptoms
Here are some things parents may notice when a child has cervical kyphosis:
- an unusual curve in the child’s neck
- the child has trouble looking up or turning his or her head
- the child has neck pain
If the curve is sharp enough to pinch the spinal cord, kids might have these problems:
- pain, tingling, loss of feeling, or weakness
- be unable to move their arms or legs
- trouble peeing or pooping
- accidents because they can’t control when they pee or poop (called incontinence)
Cervical kyphosis diagnosis
If you think your child has a neck problem, make an appointment with your pediatrician. The doctor, nurse, or physician assistant will ask about what’s going on. They will order tests like X-rays.
If the pediatrician thinks your child needs specialized help, he or she will send you to a specialist. Specialists who treat kids with kyphosis are:
- neurologists (experts in the nervous system)
- neurosurgeons (doctors who operate on the brain and spinal cord)
- orthopedists (experts in bones, muscles, and joints)
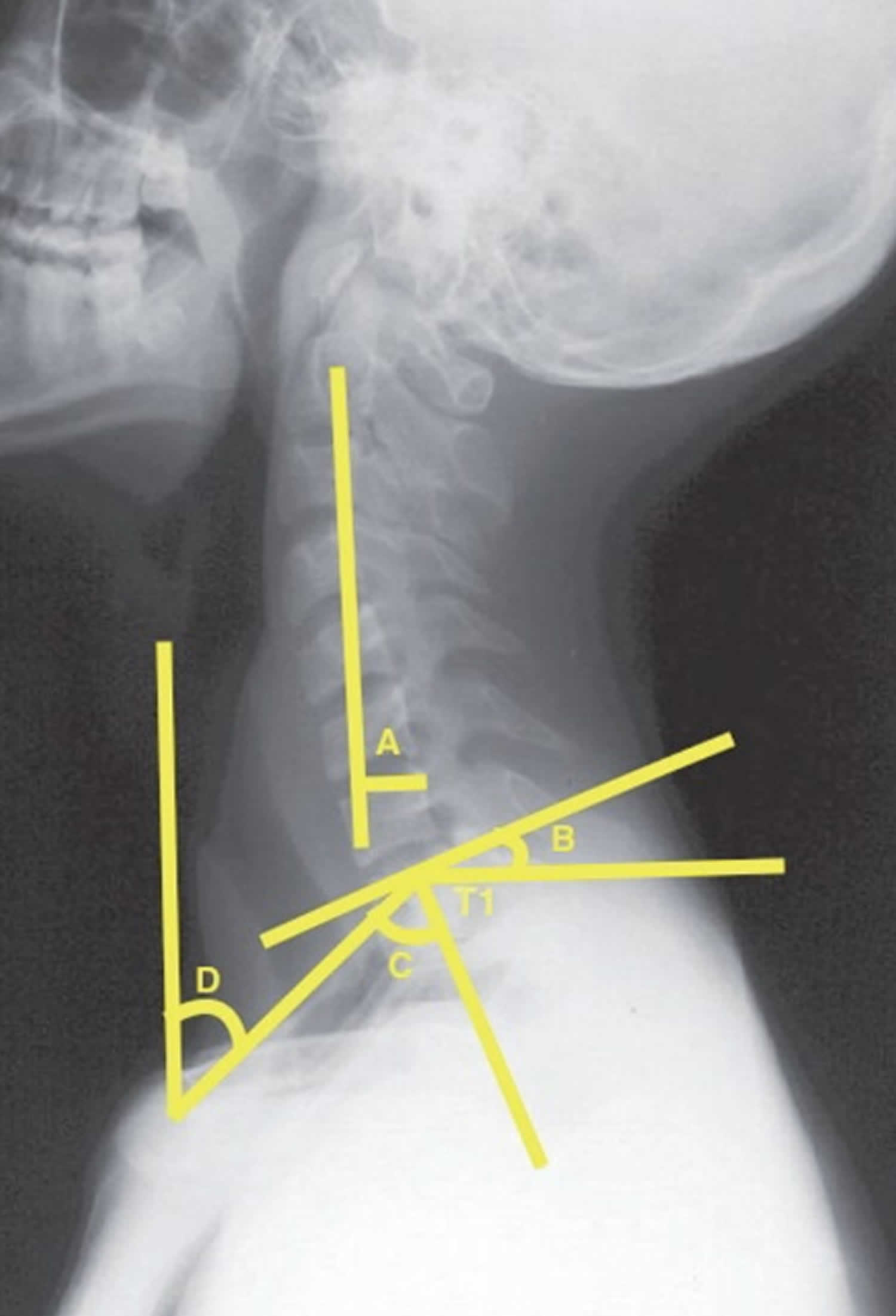
Radiographic evaluation
Preoperative planning for surgical treatment of the cervical spine begins with assessing the plain and dynamic radiographs of the cervical spine. Various parameters used to assess cervical spine include cervical lordosis (CL), chin to brow vertical angle (CBVA), C2–C7 sagittal vertical axis (C2–C7 SVA), T1 slope (T1S), neck tilt, and thoracic inlet angle (TIA) 4. Figure 7 shows these parameters measured using plain X-ray. Advanced radiological investigations such as computed tomography (CT) myelogram and/or magnetic resonance imaging (MRI) are useful to determine the compression of the spinal cord. MRI also aids the assessment of the intervertebral discs, presence of scar tissue, and posttraumatic integrity of the posterior ligamentous complex.
Figure 7. Cervical kyphosis preoperative planning
Footnote: Parameters measured using plain X-ray. a: C2–C7 sagittal vertical axis; b: T1 slope; c: thoracic inlet angle; and d: neck tilt.
[Source 1 ]Cervical kyphosis treatment
Cervical kyphosis treatment depends on the child’s age and how bad the curve is. Here are some of the things doctors use:
- Bracing. Children may wear a neck brace to treat cervical kyphosis.
- Physical therapy. Physical therapists work with kids to help improve flexibility and posture and reduce pain.
- Pain management. If kids have pain, doctors and nurses prescribe medicines and other pain management techniques.
- Surgery. Kids need surgery when a curve puts pressure on the spinal cord in a way that may cause nerve damage. Kids who also have diseases that make their bones weak or slow to heal may need more than one operation.
Preoperative planning
The first step in appropriate preoperative planning is to understand the underlying cause and the magnitude of the deformity. It is imperative to know that cervical kyphosis in the subaxial spine is associated with compensatory hyperlordosis at the cervico–occipital junction 1. This is important in planning cranio–cervical fusion 1.
The main goals of cervical kyphosis surgery are 5:
- To restore subaxial cervical lordosis to 15°, thus improving the spinal alignment and balance;
- To decompress the spinal cord and nerve roots;
- To restore C2–C7 sagittal vertical axis to <40 mm;
- To restore the horizontal gaze of vision;
- To attempt to normalize the T1 slope; and
- To achieve good fusion to reduce neck pain.
The type of approach (anterior, posterior, or combined) is decided using MRI and/or CT myelogram, depending upon the severity and location of the neurological compression. It is also useful to determine the extent of adequate neurological decompression 5. The most important and critical factor to determine the type of surgery (anterior, posterior, or combined) is the flexibility of the deformity 6. Dynamic radiographs help to determine the ability of deformity correction by altering the position, while a CT scan provides additional information about bony ankylosis at disc space and facet joints.
Cervical kyphosis surgery
Surgical planning involves calculating the amount of correction required for the radiographic parameters. Although there is no ‘normal’ range described, the current literature recommends that T1 slope to C2–C7 lordosis should be <15°, C2–C7 sagittal vertical axis should be <40 mm, and an acceptable chin to brow vertical angle is −10 to +20 7.
The magnitude of kyphosis, location of the compression, flexibility of the deformity, presence and location of the bony ankyloses, and history of previous surgery/laminectomy determines the specific surgical approach. Broadly, cervical kyphosis can be classified as fixed or flexible. Flexible deformities usually require realignment surgery, whereas more complex, fixed deformities require surgical correction using a combined (anterior+posterior) approach or osteotomies.
Anterior approach
An anterior approach is preferred in patients with a fixed deformity. Anterior techniques rely on restoring segmental lordosis, thus it is crucial to evaluate facet ankylosis using CT. Kyphosis correction with an anterior fusion, and with or without instrumentation, has been described in the literature 8.
In a retrospective analysis of 14 patients who underwent anterior corpectomy with strut grafting and without instrumentation, Zdeblick and Bohlman 9 reported that at the average follow-up period of 27.9 months, Nurick scores improved from 3.6 (preoperative) to 1.3 (postoperative). No patient had neurological deterioration. The mean preoperative kyphosis was 45°, mean postoperative kyphosis was 13°, and mean kyphosis correction was 32°. The authors reported an average loss of 4° correction at follow-up. Three patients had their bone grafts dislodged in the immediate postoperative period despite immobilization using a halo vest.
In another retrospective study, Zdeblick et al. 10 reported the functional outcome of anterior corpectomy and strut grafting in patients with failed anterior cervical diskectomy and fusion and kyphosis (n=8). Revision surgery was performed with an average duration of 32 months from the index procedure. The average kyphosis correction was 30°. Seven out of eight patients had excellent or good functional outcome; however, poor outcome was reported in one patient. This patient had pseudoarthrosis and recurrence of myelopathy, and underwent revision surgery.
In a series of 18 patients, Riew et al. 8 analyzed 18 patients with postlaminectomy cervical kyphosis that were treated with anterior cervical corpectomy and fusion. The mean kyphosis correction at final follow-up was 6°. Eight out of 18 patients had demonstrated kyphosis correction. The authors also reported an increment in kyphosis by 10° due to the subsidence of strut graft. The major focus of this study was to study the complications associated with this procedure. The authors reported a complication rate of >50% related to surgery alone, including failure of fusion, dislodging or subsidence of the graft, and an increment in kyphosis. They also reported that the halo vest provided insufficient immobilization and was not adequate to prevent complications related to the strut graft.
Following further advances in instrumentation systems, anterior cervical decompression and fusion with plate reconstruction was described as the only anterior procedure for the treatment of cervical kyphosis. Herman and Sonntag 11 retrospectively analyzed 20 patients undergoing anterior cervical corpectomy with fusion and plate fixation for treatment of postlaminectomy kyphosis. The mean preoperative kyphosis was 38°. At a mean follow-up of 28 months, all patients showed an evidence of solid fusion with a mean postop kyphosis of 16°. A mean deformity correction of 20° was achieved with intraoperative traction. The majority of complications in this study were not related to surgical technique, and only one (5%) patient had implant-related complications (screw pulled out).
In a case series of four patients of postlaminectomy kyphosis treated with anterior decompression and fusion with platting, Gulmen and Zileli 12 reported good clinical outcome in three patients, and around 20° of mean improvement in kyphosis. One of the four patients died 20 days after surgery due to respiratory complications.
Ferch et al. 13 retrospectively studied 28 patients undergoing anterior decompression with instrumented fusion for cervical kyphosis. A total of 93% (26/28) of patients were available for analysis. The average follow-up period was 25 months. The mean preoperative local and regional kyphosis was 12 and 10, respectively, and the average local and regional kyphosis correction was 14 and 11, respectively. At final follow-up, the modified Japanese Orthopedic Association (mJOA) scores improved in 11 patients, whereas it remained stable in 15 patients. Deterioration of the mJOA score was reported in one patient. Neck pain scores remained unchanged in the preoperative and postoperative periods.
Steinmetz et al. 14 proposed hybrid surgery for postlaminectomy cervical kyphosis correction. This technique combined corpectomy and discectomy with anterior cervical plate fixation. In a retrospective study of 10 patients, the authors reported improvement in all patients, and three patients reported complete resolution of symptoms. The average preoperative kyphosis was 13.2°, while that at final follow-up was −8.4°. A mean cervical kyphosis correction of 21.6° was observed. However, one limitation of this study was the low duration of follow-up. Three patients experienced complications; one had postoperative dysphagia and two suffered hoarseness of the voice.
In a retrospective study of prospectively collected data, Park et al. 15 analyzed 23 patients undergoing anterior reconstruction surgery using a hybrid technique and plate fixation for postlaminectomy kyphosis. The average follow-up was 44.5 months. The mean preoperative kyphosis was 20.9°, while that at the final follow-up was −9.6°, with mean cervical kyphosis correction 30.5° for cervical kyphosis. There was significant improvement in the neck disability index, Visual Analog Scale (VAS) scores, and Nurick grades. All patients showed improved neurology, while nine patients had complete resolution of symptoms. The authors concluded that augmentation of fusion with the plate decreased the graft-related complications 15. However, posterior instrumented fusion to the construct was added in patients undergoing corpectomy at more than three levels. Almost 13% of patients in this series showed graft-related complications.
Posterior approach
A posterior-only approach is less commonly implicated in the management of cervical kyphosis. It is commonly used in conjunction with an anterior approach for circumferential fusion, and is indicated in flexible deformities, when kyphosis correction is achieved by positioning of head or traction, and whenever there is no anterior compression 16. Abumi et al. 16 retrospectively analyzed 30 patients undergoing cervical kyphosis correction with the use of cervical pedicle screws. Of these patients, 17 had flexible kyphosis and were managed with an entirely posterior procedure. The mean preoperative kyphosis was 28.4° that improved to 5.1° at final follow-up. All patients had fusion at the final follow-up. Transient nerve root complications related to placement of the pedicle screw was reported in two patients.
Lateral mass screws are the preferred modality of fixation owing to a low complication rate compared with that of pedicle screws. However, biomechanically, they are inferior to pedicle screws. In a systemic review, Coe et al. 17 found lateral mass screws provided an adequate fusion rate and an acceptable deformity correction. Gerling et al. 18 studied nine patients with dropped head deformity and flexible kyphosis due to cervical myopathy who underwent deformity correction and posterior instrumented arthrodesis. The mean follow-up duration was 6 years. Four patients had primary cervical myopathy, while the other 5 patients had secondary cervical myopathy due to radiotherapy. Outcome measures were reported using Odom’s criteria, VAS scores for neck pain, and patient satisfaction ratings. All patients showed improvement in Visual Analog Scale (VAS) scores at the final follow-up. Seven patients had an excellent outcome, while two patients had a fair outcome as reported by Odom’s criteria and patient reported measures. Though 11 complications were reported, none of the patients had neurological deterioration.
Combined approach
White and Panjabi 19 proposed the idea that corpectomy in patients with postlaminectomy kyphosis further destabilizes the spine. The right and left elements of the vertebrae are only connected by soft tissue that has significantly less resistance to torsion and axial forces. An anterior graft in the absence of posterior elements bears the entire axial load, which may not be prevented by halo vest immobilization alone. Therefore, there is an increased risk of graft dislodgement or subsidence. The authors strongly recommended the addition of posterior instrumented fusion in patients undergoing anterior corpectomy and fusion for postlaminectomy kyphosis 19.
Posterior osteotomy
Patients with rigid cervical kyphosis along with ankylosed facet joints require the use of posterior-based osteotomies for deformity correction. Although Mason et al. 20 first described posterior-based open wedge osteotomy for the treatment of cervical kyphosis, many modifications of this procedure were described for treatment of cervical kyphosis in ankylosing spondylitis. MacMaster 21 reported 15 patients with ankylosing spondylitis with severe cervical kyphosis managed by extension osteotomy at C7–T1. After osteotomy, kyphosis correction was achieved by extension of the head using spinal cord monitoring. Halo traction or internal fixation was used postoperatively to maintain the kyphosis correction. The mean cervical kyphosis was 23°, and was corrected to a mean lordosis of 31°, providing a mean kyphosis correction of 54°. However, internal fixation (Luque rods and wiring) was used in only three patients. Four patients in this series had subluxation at the osteotomy site. As this procedure was dependent on lengthening the anterior column, it was associated with a high rate of morbidity.
1) Pedicle subtraction osteotomy
Pedicle subtraction osteotomy is a posterior closing wedge osteotomy involving resection of a wedge of the vertebral body along with superior and inferior articular processes and lamina 22. It is most commonly performed at C7 owing to the anatomy of the vertebral artery as well as the wide diameter of spinal canal at C7–T1 23.
Deviren et al. 23 analyzed 11 patients that underwent pedicle subtraction osteotomy at the cervicothoracic junction for cervicothoracic sagittal imbalance. Then patients underwent pedicle subtraction osteotomy at C7, whereas one patient underwent T1 pedicle subtraction osteotomy. Outcome measures were reported using the Neck Disability Index (NDI) scores, the 36-item Short-Form Health Survey (SF-36) scores, and the VAS scores for neck pain in nine out of the 11 patients that were followed for a mean duration of 23 months. The mean kyphosis correction was 19°, and mean chin to brow vertical angle correction was 36.7°. There was significant improvement in NDI, VAS, and SF-36 scores in all patients. None of the patients had any neurological complications.
2) Circumferential osteotomy
Abumi et al. 16 reported on 13 patients with fixed and rigid cervical kyphosis who were managed using combined anterior and posterior procedures. The mean preoperative kyphosis was 30.8°, and the mean cervical kyphosis at final follow-up was 0.5°. All patients had complete fusion at final follow-up. The authors concluded that circumferential osteotomies along with posterior shortening procedures with the use of pedicle screw instrumentation provided the best cervical kyphosis correction with bony fusion 16. Mummaneni et al. 24 retrospectively analyzed 30 patients with cervical kyphosis undergoing circumferential procedures. Anterior procedures included discectomies and corpectomies/osteotomies at one or more levels, while posterior procedures included decompression and/or osteotomies with lateral mass or pedicle screw fixation. A total of 27 patients were available for analysis at mean a follow-up period of 2.6 years. Ishihara kyphosis indices improved from a preoperative mean of −17.7 to a postoperative mean of +11.4. Furthermore, the mJOA scores improved from 10.5 to 15, while the Nurick scores improved from 3.2 to 1.3. The fusion rate was reported to be 95%. This study had significant complication rates; 33% of patients had major and minor complications, while there were four deaths. None of the patients had neurological worsening. The authors concluded that circumferential reconstruction is efficacious in treating cervical kyphosis adequately. O’Shaughnessy et al. 25 analyzed 16 patients who underwent anterior and posterior reconstruction for fixed cervical kyphosis. The mean follow-up period was 4.5 years. The C2–C7 Cobb angle improved from a preoperative mean of +38° to a mean of −10° at final follow-up, yielding a mean kyphosis correction of 48°. The mean Nurick scores improved from 2.4 prior to surgery to 1.5 at final follow-up. Excellent and good outcomes were reported in 38% and 50% of patients, respectively, as per Odom’s criteria, while the fair and poor outcome groups contained 6% of the patients each. All patients had good bony fusion and maintenance of correction at final follow-up. Nottmeier et al. 26 retrospectively reviewed 41 patients undergoing circumferential reconstruction for rigid cervical kyphosis. Patients were followed for mean period of 19 months. The mean preoperative kyphosis of 18° improved to 4° of lordosis at final follow-up, resulting in a mean kyphosis correction of 22°. There was no loss of correction in any patient, while a fusion rate of 97.5% was obtained. Two patients had neurological complications (one quadriparesis and one transient C8 radiculopathy). Ogihara and Kunogi 27 reported three patients undergoing single stage anterior and posterior fusion surgery for cervical kyphotic deformity correction using an intervertebral cage and lateral mass screws. All patients were followed up for a minimum period of 61 months and showed improved symptoms following surgery. All three patients had complete fusion and maintenance of correction at final follow-up. The authors concluded that the combination of anterior cages and lateral mass screws was considered a safe and effective procedure for the cervical kyphosis correction. Shah et al. 28 reported a case of neurofibromatosis with buckling kyphosis of cervical spine. The patient was treated with circumferential osteotomy in a staged procedure. In the first stage, anterior cervical corpectomy with soft tissue release was performed. In the second stage, posterior fusion was carried out using lateral mass screws.
References- Gadia A, Shah K, Nene A. Cervical Kyphosis. Asian Spine J. 2019;13(1):163–172. doi:10.31616/asj.2018.0086 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6365778
- Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery. 2012;71:662–9.
- Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine. 2013;19:141–59.
- Lee SH, Kim KT, Seo EM, Suk KS, Kwack YH, Son ES. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech. 2012;25:E41–7.
- Savage JW, Schroeder GD, Hsu WK, Patel AA. Cervical deformity: pre-operative evaluation and surgical treatment options. Semin Spine Surg. 2014;26:172–9.
- Ames CP, Smith JS, Scheer JK, et al. A standardized nomenclature for cervical spine soft-tissue release and osteotomy for deformity correction: clinical article. J Neurosurg Spine. 2013;19:269–78.
- Song K, Su X, Zhang Y, et al. Optimal chin-brow vertical angle for sagittal visual fields in ankylosing spondylitis kyphosis. Eur Spine J. 2016;25:2596–604.
- Riew KD, Hilibrand AS, Palumbo MA, Bohlman HH. Anterior cervical corpectomy in patients previously managed with a laminectomy: short-term complications. J Bone Joint Surg Am. 1999;81:950–7.
- Zdeblick TA, Bohlman HH. Cervical kyphosis and myelopathy: treatment by anterior corpectomy and strut-grafting. J Bone Joint Surg Am. 1989;71:170–82.
- Zdeblick TA, Hughes SS, Riew KD, Bohlman HH. Failed anterior cervical discectomy and arthrodesis: analysis and treatment of thirty-five patients. J Bone Joint Surg Am. 1997;79:523–32.
- Herman JM, Sonntag VK. Cervical corpectomy and plate fixation for postlaminectomy kyphosis. J Neurosurg. 1994;80:963–70.
- Gulmen V, Zileli M. Surgical treatment of postlaminectomy cer vical kyphosis. Turk Neurosurg. 2000;10:28–35.
- Ferch RD, Shad A, Cadoux-Hudson TA, Teddy PJ. Anterior correction of cervical kyphotic deformity: effects on myelopathy, neck pain, and sagittal alignment. J Neurosurg. 2004;100(1 Suppl Spine):13–9.
- Steinmetz MP, Kager CD, Benzel EC. Ventral correction of postsurgical cervical kyphosis. J Neurosurg. 2003;98(1 Suppl):1–7.
- Park Y, Riew KD, Cho W. The long-term results of anterior surgical reconstruction in patients with postlaminectomy cervical kyphosis. Spine J. 2010;10:380–7.
- Abumi K, Shono Y, Taneichi H, Ito M, Kaneda K. Correction of cervical kyphosis using pedicle screw fixation systems. Spine (Phila Pa 1976) 1999;24:2389–96.
- Coe JD, Vaccaro AR, Dailey AT, et al. Lateral mass screw fixation in the cervical spine: a systematic literature review. J Bone Joint Surg Am. 2013;95:2136–43.
- Gerling MC, Bohlman HH. Dropped head deformity due to cervical myopathy: surgical treatment outcomes and complications spanning twenty years. Spine (Phila Pa 1976) 2008;33:E739–45.
- White AA 3rd, Panjabi MM. Biomechanical considerations in the surgical management of cervical spondylotic myelopathy. Spine (Phila Pa 1976) 1988;13:856–60.
- Mason C, Cozen L, Adelstein L. Surgical correction of flexion deformity of the cervical spine. Calif Med. 1953;79:244–6.
- McMaster MJ. Osteotomy of the cervical spine in ankylosing spondylitis. J Bone Joint Surg Br. 1997;79:197–203.
- Wollowick AL, Kelly MP, Riew KD. Pedicle subtraction osteotomy in the cervical spine. Spine (Phila Pa 1976) 2012;37:E342–8.
- Deviren V, Scheer JK, Ames CP. Technique of cervicothoracic junction pedicle subtraction osteotomy for cervical sagittal imbalance: report of 11 cases. J Neurosurg Spine. 2011;15:174–81.
- Mummaneni PV, Dhall SS, Rodts GE, Haid RW. Circumferential fusion for cervical kyphotic deformity. J Neurosurg Spine. 2008;9:515–21.
- O’Shaughnessy BA, Liu JC, Hsieh PC, Koski TR, Ganju A, Ondra SL. Surgical treatment of fixed cervical kyphosis with myelopathy. Spine (Phila Pa 1976) 2008;33:771–8.
- Nottmeier EW, Deen HG, Patel N, Birch B. Cervical kyphotic deformity correction using 360-degree reconstruction. J Spinal Disord Tech. 2009;22:385–91.
- Ogihara S, Kunogi J. Single-stage anterior and posterior fusion surgery for correction of cervical kyphotic deformity using intervertebral cages and cervical lateral mass screws: postoperative changes in total spine sagittal alignment in three cases with a minimum follow-up of five years. Neurol Med Chir (Tokyo) 2015;55:599–604.
- Shah KC, Gadia A, Nagad P, Bhojraj S, Nene A. buckling collapse of midcervical spine secondary to neurofibromatosis. World Neurosurg. 2018;114:228–9.