What is clenbuterol
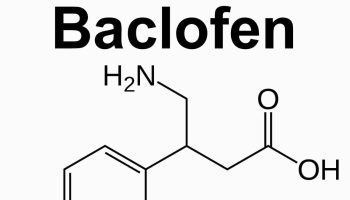
Clenbuterol is a substituted phenylaminoethanol and a long-acting beta-2 adrenergic agonist with sympathomimetic activity used to prevent asthma in humans, by inhibiting smooth muscle contraction and increasing epithelial mucus clearance, in some countries and its use in the United States is strictly restricted to farm animals (veterinary use only). Clenbuterol is NOT approved by the FDA for human use. Clenbuterol selectively binds to and activates beta-2 adrenergic receptors in bronchiolar smooth muscle, thereby causing stimulation of adenyl cyclase, the enzyme that catalyzes the conversion of adenosine triphosphate (ATP) to cyclic-3′,5′-adenosine monophosphate (cAMP). Increased intracellular cAMP levels cause relaxation of smooth muscle. In addition, clenbuterol also stimulates central nervous system (CNS), and causes an increase in blood pressure and heart rate due to both beta-2 and beta-1 adrenergic activities. This agent may also exert an anabolic or anti-catabolic effect due to as of yet unidentified mechanisms.
Clenbuterol, one of the selective β2-adrenergic agonists, is known to induce a specific protein anabolic effect in skeletal muscle 1. Because of this effect, clenbuterol has been extensively studied in animals, especially for its therapeutic potential in various diseases affecting muscle mass or weakness. Effects of β2-adrenergic agonist treatment on muscle mass have been demonstrated in the contexts of muscular dystrophy, disuse 2, ageing, denervation and amyotrophic lateral sclerosis in both animals and humans 1. In addition to the effect on muscle mass, chronic clenbuterol treatment induces a fiber-type transition from slow to fast twitch fibers in animal models 3. The phenotypic and metabolic changes induced by clenbuterol have raised questions about the impact of this treatment on muscle contractile function and ATPase activity. Previous studies have shown greater force-producing capacity in clenbuterol-treated muscle in both fast and slow twitch muscles 4. Nevertheless, when maximal tetanic contraction was corrected for muscle cross-sectional area, muscle force was unchanged and even altered in soleus muscle 5. These results suggest a potentially deleterious effect of chronic clenbuterol treatment on the skeletal muscle contractile machinery. Chronic clenbuterol treatment leads to hypertrophy but reduced specific force in slow twitch muscle 6. The beneficial anabolic effects of high-dose β2-agonists for treatment of sarcopenia, muscle weakness and muscular dystrophy seem counterbalanced, at least in part, by deleterious effects on muscle contractility, relaxation kinetics and Ca2+ handling 6. A preliminary study suggested that chronic clenbuterol treatment induces significant changes in the calcium (Ca2+) signals associated with excitation–contraction coupling in fast twitch skeletal muscles 7. However, the mechanisms responsible for the changes in clenbuterol-induced contractility are not well understood.
The World Anti-Doping Agency (WADA) Ruling on Clenbuterol 8
- Clenbuterol is a prohibited substance and there is no threshold under which this substance is not prohibited.
- At present there is no plan to introduce a threshold level for clenbuterol.
- It is possible that under certain circumstances the presence of a low level of clenbuterol in an athlete sample can be the result of food contamination. However, each case is different and all elements need to be taken into account.
- Under the World Anti-Doping Code, result management of cases foresees the opportunity for an athlete to explain how a prohibited substance entered his/her body.
Although traditionally used for treating bronchospasm, it became apparent that some β-agonists could increase skeletal muscle mass and decrease body fat. Clenbuterol has been shown to increase lean mass and lean/fat ratio as well as a significant increase in maximal strength. These so-called “repartitioning effects” proved desirable for the livestock industry trying to improve feed efficiency and meat quality 9.
Studying β-agonist effects on skeletal muscle has identified potential therapeutic applications for muscle wasting conditions such as sarcopenia, cancer cachexia, denervation, and neuromuscular diseases, aiming to attenuate (or potentially reverse) the muscle wasting and associated muscle weakness, and to enhance muscle growth and repair after injury. Sarcopenia is considered to be a primarily age‐dependent syndrome and was initially defined as the age‐related loss of skeletal muscle of the limbs 2 SD below the mean of a healthy young reference group, and has been associated with a range of adverse outcomes 10. In contrast to cachexia, sarcopenia and muscle wasting cannot be diagnosed by simply weighing the patients longitudinally to detect unintentional weight loss 11. Sarcopenia affects 5–13% of elderly persons aged 60–70 years and up to 50% of all octogenarians 12. Not surprisingly, β-agonists were soon being used by those engaged in competitive bodybuilding and by other athletes, especially those in strength- and power-related sports.
So far, there are only limited treatment options for sarcopenic patients, which include (resistance) exercise 13, nutritional strategies to increase intake of proteins and micronutrients 14 and finally, drug treatment, including compounds like testosterone 15, growth hormone and IGF‐1 16.
Resistance exercise is often used in combination with nutrition support, which increases muscle mass and muscle strength more than exercise alone 17. Supplementation of a low dose creatine in combination with resistance training improved lean mass in elderly over a period of 12 weeks 18. In a patient‐centered exercise approach in frail elderly and older adults with mobility limitations, physical activity was considered to improve effective quality of life and reduce frailty, while also being cost‐effective 19. An accelerometer‐determined physical activity showed an independent, dose‐response relationship with lean mass percentage and lower limb strength 20.
As a consequence of their muscle anabolic actions, the effects of β-agonist administration on skeletal muscle have been examined in a number of animal models (and in humans) in the hope of discovering therapeutic applications, particularly for muscle wasting conditions such as sarcopenia (age-related muscle wasting and associated weakness), cancer cachexia, sepsis, and other forms of metabolic stress, denervation, disuse, inactivity, unloading or microgravity, burns, human immunodeficiency virus (HIV)-acquired immunodeficiency syndrome, chronic kidney or heart failure, chronic obstructive pulmonary disease, muscular dystrophies, and other neuromuscular disorders. For many of these conditions, the anabolic properties of β-agonists may attenuate (or potentially reverse) the muscle wasting, muscle fiber atrophy, and associated muscle weakness. β-Agonists also have clinical significance for enhancing muscle repair and restoring muscle function after injury or following reconstructive surgery.
Despite their muscle anabolic properties, β-agonists have also been associated with some undesirable side effects, including increased heart rate (tachycardia) and muscle tremor, which have so far limited their therapeutic potential. The endurance and exercise duration decreased after clenbuterol 21. In fact, many athletes are not aware of the deleterious cardiovascular effects of chronic high-dose β-agonist administration and in many cases rely on anecdotal information about these compounds from nonscientific sources 9. Some undesirable cardiovascular side effects of -agonists have so far limited their therapeutic potential.
Other options to increase muscle mass include β2‐adrenergic agonists like salbutamol and formoterol. These compounds have beneficial effects on muscle mass, most likely via an induction of protein synthesis in myocytes and increased blood flow 22. Patients with chronic heart failure were prone to develop detrimental ventricular arrhythmias when treated with salbutamol 23. In contrast, in experimental cancer cachexia, formoterol has been shown to improve muscle mass, reduce progression of cachexia and improve survival, while also being cardio‐protective 24. Espindolol, the s‐enantiomer of pindolol, may be the more interesting compound to use. It is a beta‐1 receptor antagonist, a partial beta‐2 receptor agonist and also has 5‐HT1a receptor activities. In old rats, it has been shown to significantly increase muscle mass, while reducing fat mass without negative affecting cardiac function, making it an interesting compound to use in sarcopenic obesity 25. Also, it has shown very promising results in Phase IIa cancer cachexia study leading to an increase in muscle mass and hand grip strength 26.
A greater understanding of β-adrenergic signaling in skeletal muscle is important for identifying its role in muscle growth, development, and muscle regeneration and for identifying new therapeutic targets. Research is needed to understand how the β-adrenergic signaling pathway can be manipulated for the purposes of 1) attenuating the muscle wasting associated with many diseases and conditions and 2) enhancing muscle fiber growth and improving the functional repair of damaged and regenerating skeletal muscle after injury.
Use of Clenbuterol by Athletes for Performance Enhancement
β-Agonist (clenbuterol) usage is highest among bodybuilders for its muscle anabolic properties, but primarily for its lipolytic effects. The exact dosage of clenbuterol that results in the greatest improvements in muscle mass and reductions in body fat has not yet been identified. These criteria are especially important for bodybuilders before competitions where the maintenance of muscle mass is critical during periods of strict dieting. The dosages used by bodybuilders exceed that recommended for asthmatics for therapeutic purposes. Typically, the dose of clenbuterol used ranges from 50–100 or 80–140 μg/day taken over the course of the day, depending on the individual’s tolerance 27. The fact that clenbuterol is not approved by the United States Food and Drug Administration for use on humans means that little information is available in the scientific literature concerning its use and abuse by athletes 28.
To prevent receptor downregulation, clenbuterol is often used in two or three week “on and off” cycles. Comparing the doses that are effective in rats and translating these for use in humans is obviously difficult due to the differences in size, growth, and metabolism between the species. However, some authors have made interspecies comparisons based on metabolic measurements. For example, Maltin et al. 29 suggested that a dose of 10 μg/kg for the rat was equivalent to 1.0 μg/kg for humans, a dose considered to be safe 30. Even if a theoretical safe dosage of clenbuterol was prescribed for promoting muscle mass in humans, it is unlikely that this level would be adhered to by bodybuilders given that some of these athletes are notorious for taking anabolic steroids in excess of 26 times the therapeutic dose 31. Another confounding issue is the fact that many bodybuilders take more than one drug at any one time, and the supposed increases in muscle mass following clenbuterol administration are hard to gauge when, for example, it is taken in conjunction with either one or more anabolic steroids.
Traditionally, the use of anabolic steroids and growth hormone (GH) has dominated the world of performance-enhancing drugs. However, the use of β-agonists, particularly clenbuterol, for athletic and cosmetic purposes has been increasing steadily 32. The notoriety of clenbuterol emerged during the 1992 Summer Olympic Games in Barcelona, Spain, when two athletes tested positive for its use. Clenbuterol has a long half-life of ∼35 h 33, and subsequently, the drug will accumulate with repeated doses 34. It can be detected via hair and urine analysis; however, veterinary studies have shown that 97% of the drug will be removed from the body within ∼10–11 days 35.
Clenbuterol was banned by the International Olympic Committee on April 21, 1992. Regardless, many athletes still abuse this substance, with most not aware of its potentially lethal side effects when taken in excessive dosages. Sadly, the combination of clenbuterol use with diuretics, for example, has been thought to be responsible for the deaths of several prominent professional bodybuilders 36. There have been case reports describing myocardial infarction in young male body builders either only taking clenbuterol or a combination of clenbuterol and anabolic steroids 37, 38.
It is clear that athletes taking clenbuterol in excessive doses and for extended periods are at greater risk for cardiovascular events. Although many of the side effects (i.e., sweating, tachycardia, and tremor) will cease once the treatment is stopped, the question of whether the deleterious effects on the heart are reversible is more difficult to answer. Urhausen et al. 39 reported that even several years after discontinuation of anabolic steroid abuse, strength athletes still showed a slight concentric left ventricular hypertrophy compared with drug-free strength athletes. Evidence from animals treated chronically with a high dose of clenbuterol indicates that the deposition of noncontractile fibrotic material in the ventricular walls is likely to affect cardiac mechanics and impair exercise performance. Based on its deleterious and potentially lethal side effects, athletes would be advised not to experiment with these compounds for nonmedical use 40.
Adrenoceptors and the Sympathetic Nervous System
The sympathetic nervous system is comprised of two major chemical signaling molecules, the catecholamines adrenaline (epinephrine) and noradrenaline (norepinephrine). Adrenaline is produced and released from the adrenal glands, and noradrenaline is produced and released from nerve axons following stimulation with acetylcholine. Binding of one of these chemicals to an adrenergic receptor will elicit a response, depending on the receptor subtype bound.
To date, there are at least nine subtypes of adrenoceptors that have been cloned, including six α- and three β-subtypes, which are located in different proportions in numerous tissues throughout the body, with the β-adrenoceptor family predominating in skeletal muscle. Over the past 20 years there have been a multitude of studies demonstrating the growth-promoting actions of β-adrenoceptor stimulation in skeletal muscle 41. However, very little work has focused on the role of this pathway in normal muscle growth and development, muscle fiber regeneration after injury, or its involvement in pathological conditions where muscle wasting and weakness are indicated.
All adrenoceptors belong to the guanine nucleotide-binding G protein-coupled receptor (GPCR) family, the largest group of cell-surface receptors in mammals and which comprise >1% of the human genome 42. The most well-characterized family of guanine nucleotide-binding G protein-coupled receptors is the rhodopsin receptors, which include the dopaminergic, adenosine, histamine, α-, and β-adrenergic receptors 42. One of the defining features of the guanine nucleotide-binding G protein-coupled receptor superfamily is that all of the receptors couple to heterotrimeric guanine nucleotide-binding regulatory proteins (G proteins). These molecules received their name from the typical three subunit composition (designated “αβγ”).
β-Adrenoceptors
β-Adrenoceptors play a regulatory role in cardiovascular, respiratory, metabolic, and reproductive function. Therefore, it is not surprising that the β-adrenoceptor family is the most widely studied of all the adrenergic receptors. Three subtypes of β-adrenoceptors have been identified and cloned: β1-, β2-, and β3-adrenoceptors 43, each with a 65–70% homology in their amino acid composition 44. The β-adrenoceptor family was originally believed to signal predominantly via coupling with Gαs; however, more recent studies suggest that both β2- and β3-adrenoceptors are also capable of coupling to Gαi 45. The crystal structure of the β2-adrenoceptor has been described in two studies 46.
The most well-documented β-adrenoceptor signaling pathway involves the cAMP-protein kinase A (PKA) signaling pathway, which has been characterized in numerous cell types and tissue systems 47. In skeletal muscle, activation of this pathway is believed to be, at least in part, responsible for the anabolic response of skeletal muscle to β-adrenoceptor stimulation.
β-Adrenoceptor signaling in skeletal muscle
Much of our current knowledge of β-adrenoceptor signaling in skeletal muscle is based on work conducted in cardiac muscle 48. It is only recently that scientists have begun to appreciate the importance of this system in skeletal muscle growth, development, and repair after injury 49.
Skeletal Muscle β-Adrenoceptor Subtypes
Skeletal muscle contains a significant proportion of β-adrenoceptors, which are mostly of the β2-subtype, but there are ∼7–10% β1-adrenoceptors present 50 as well as a smaller population of α-adrenoceptors, usually found in higher proportions in slow-twitch muscles 51. Slow-twitch muscles, such as the soleus muscle, have a greater density of β-adrenoceptors than fast-twitch muscles, such as the extensor digitorum longus 52. Although the functional significance of this difference in β-adrenoceptor density is not yet fully understood, the response to β-agonist administration appears to be greater in fast- than in slow-twitch skeletal muscles 53.
Recently, a fourth β-adrenoceptor subtype (designated as a “putative” β4-adrenoceptor) was proposed to exist in the mouse 54 but was later reclassified as a novel β3-adrenoceptor isoform (designated as β3a- and β3b-adrenoceptors) 55. Both β3-adrenoceptors are believed to have stimulatory effects that are mediated through a Gαs pathway 56. The β3b-adrenoceptor is also believed to be coupled to a second pathway involving the inhibitory G protein, Gαi 57.
One of the most important characteristics of adrenoceptors is that a catecholamine can elicit very different responses depending on the adrenoceptor that it activates. This enables the adrenoceptors to be targeted specifically and to be manipulated by synthetically tailored agents. Many synthetic adrenoceptor agonists and antagonists have been developed for the treatment of (primarily) cardiovascular diseases. β-Adrenoceptors have been the main focus of most investigations regarding adrenergic receptors 58, and information gathered from this receptor has helped develop a family of β2-adrenoceptor agonists (β2-agonists) for clinical purposes 59.
G Protein Coupling in Skeletal Muscle
While β2-adrenoceptor-mediated signaling has been traditionally believed to involve selective coupling to Gαs to initiate downstream signaling via AC pathways, recent studies suggest that the β2-adrenoceptor may exhibit dual coupling to both Gαs and Gαi 60. This dual coupling mechanism has been described in numerous studies involving cardiac muscle 61, and more recently in skeletal muscle 62. In addition to the well-documented inhibition of AC activity, β2-adrenoceptor coupling to Gαi appears to activate Gαs independent pathways 63.
To further complicate skeletal muscle β2-adrenoceptor signaling, the Gβγ dimer has been found to initiate intracellular signaling pathways independent of the Gα subunit 64. Specifically, Gβγ activates the phosphoinositol 3-kinase (PI3K)-AKT signaling pathway 64. PI3K is thought to phosphorylate the membrane phospholipid phosphatidylinositol-4,5-bisphosphate (PIP2), generating phosphatidylinositol-3,4,5-trisphosphate (PIP3), and creating two lipid-binding sites on the cell membrane for the serine/threonine kinase AKT (also referred to as protein kinase B) and 3′-phosphoinositide-dependent protein kinase 1 (PDK). AKT is phosphorylated at the membrane by PDK, and once activated, AKT phosphorylates numerous proteins involved in protein synthesis, gene transcription, cell proliferation, and survival 65.
Clenbuterol side effects
Despite the clinical potential of manipulating the β-adrenergic signaling pathway, current approaches stimulating the pathway with β-agonists are not without side effects, and many of these less well-reported deleterious effects have important implications for the health of athletes taking these drugs for performance enhancement. Since the early 1990s, the use of β-agonists for the purpose of enhancing sporting performance has become increasingly prevalent. Despite the so-called desirable effects of increasing muscle bulk and decreasing body fat, many athletes are not aware of the deleterious effects of chronic high-dose β-agonist administration.
The side effects associated with long-term therapeutic use of β-agonists have been detailed 66, 67, 68. Excluding athletes, there are two groups of individuals exposed to β-agonists: patients being treated with the drugs and individuals who eat the meat of animals that have been treated with the drugs 69.
The most frequently reported side effects associated with the use of β-agonists include:
- nausea,
- headaches, and
- insomnia.
Excessive use of β-agonists can lead to symptoms such as muscle tremor, palpitations, muscle cramps, headache, and peripheral vasodilatation 36.
Clenbuterol administration has been linked to alterations in animal behavior including increased aggression in mice 70 and suppression of feeding following acute treatment in rats 71. Interestingly, data from Benelli et al. 72 indicated that clenbuterol negatively affects the copulatory behavior of sexually vigorous male rats, but improved that of sexually sluggish ones, providing evidence that central β-adrenoceptor activation can alter behaviors. Clenbuterol has been shown to produce effects on behavior similar to those seen after administration of clinically active antidepressant drugs, indicating that clenbuterol and related β2-agonists may have antidepressant activity 34.
Studies on the effects of chronic high-dose β-agonist administration on exercise performance have been conducted on animals. Ingalls et al. 73 subjected mice to a combination of 8 wk of treadmill running (3 sets of 3 min, 36–40 m/min, 10–17% grade, 30-s recovery, 4 days/wk) and clenbuterol treatment (1.6 mg/kg, 4 days/wk) and found that clenbuterol treatment decreased total work performance. Although clenbuterol increased muscle mass, it had antagonistic effects on running performance 73. Clenbuterol administration to rats altered the normal adaptations of skeletal muscle to endurance exercise training 74. Clenbuterol treatment (0.8 mg/kg for 8 wk) decreased glucose transporter (GLUT-4) content within the muscle and decreased citrate synthase activity 75. Other studies have shown that similar high-dose clenbuterol treatments can reduce citrate synthase activity in skeletal muscles 76 as well as decrease capillary density in the left ventricle and skeletal muscles of rats, thereby increasing the diffusion distances for oxygen in the heart and skeletal muscles 77.
Effects of β-Agonists on Cardiac Muscle Structure and Function
In addition to these potentially deleterious effects on skeletal muscle, chronic β-agonist administration has been found to have toxic effects on the heart 78. There are three β-adrenoceptors in the heart 79, so it is not surprising that adrenergic stimulation following systemic β-agonist administration can also have major effects on cardiac as well as skeletal muscle 80. Tachycardia (rapid heart beat) is one of the first indications that β-agonists such as clenbuterol are having an effect. Sudden death due to cardiac failure associated with clenbuterol administration has been reported in both humans 38 and rats during high-intensity swimming exercise 81. Chronic administration of β-agonists such as clenbuterol or salbutamol in rats almost invariably produces significant cardiac hypertrophy 82. Clenbuterol treatment in rats has also been shown to increase cortisol and corticosterone secretions and increase the size of the adrenal glands due to hyperplasia of adrenocortical cells 83.
Cardiac hypertrophy is commonly observed in rats and mice when treated chronically with high doses of β-agonists such as clenbuterol and fenoterol 84. In adult and aged rats treated daily with an intraperitoneal injection of fenoterol (1.4 mg/kg) for 4 weeks, cardiac hypertrophy was evident in both groups, and a decrease in cardiac function was observed in the adult rats 85. The cardiac hypertrophy in fenoterol-treated aged rats was associated with an increase in midventricular collagen deposition, whereas adult rats exhibited no change in collagen with treatment. Although previous studies found that β-agonist treatment could increase collagen content in the heart 81, the study by Gregorevic et al. 85 that employed a working heart preparation to evaluate cardiac function suggested that other mechanisms could be responsible for the detrimental effects of high-dose fenoterol treatment in adult rats. Furthermore, areas of apoptotic activity were observed in rat hearts after chronic high dose (5 mg/kg) clenbuterol administration 86 and it is possible that similar damage can contribute to a deterioration of cardiac muscle integrity, collagen infiltration, and impaired cardiac function.
Interestingly, acute periods of clenbuterol administration did not appear to affect cardiac function despite left ventricular hypertrophy 87. Similar findings of little or no change in cardiac function have been reported in rats treated with low doses (0.2–0.4 mg/kg body mass) of isoproterenol 88, although it has been suggested that in rats, the changes to the heart during isoproterenol-induced cardiac hypertrophy are not homogeneous and that myocardial mass, myocardial relaxation, left ventricular stiffness, and systolic function can differ between subgroups of animals 89.
On the contrary, rats administered high doses of clenbuterol (2 mg/kg) daily for several months showed significant cardiac hypertrophy, infiltration of collagen in the left ventricular walls 81, and impaired cardiac mechanics, including reductions in left ventricular pressure 90. Histological examination of the myocardium of dogs following chronic treatment with isoprenaline (in mg/kg doses) revealed severe necrosis 67, while congestion, interstitial edema, hypertrophy of muscle fibers, and myocardial necrosis were evident in rats given very large doses (between 17 and 150 mg/kg daily) of another β-agonist, salbutamol, for 1 mo 91. Severe myocardial lesions have been observed in the hearts of sheep given intravenous doses of either salbutamol, fenoterol, or isoprenaline (128 μg/kg at 15-min intervals), for 4 days 92, and isoproterenol treatment produced necrosis and an increase in collagen content in the hearts of rats 93 even when given in low doses 94.
It should also be noted that the β-agonist-induced increases in skeletal and cardiac mass have been utilized favorably in combination with left ventricular devices for treating end-stage cardiac failure to reverse or prevent the adverse effects of unloading-induced cardiac atrophy 95. The rationale is that increasing the frequency and durability of myocardial recovery could reduce or postpone the need for subsequent heart transplantation 96. It is proposed that the cardiac hypertrophy associated with β-agonist administration confers physiological benefits by attenuating myocyte atrophy associated with left ventricular assist devices. Left ventricular device support can restore β-adrenergic receptor signaling in patients with chronic heart failure 97. Birks et al. 98 treated 15 human patients who had undergone implantation of left ventricular assist devices with clenbuterol at an initial dose of 40 μg twice daily, then at a dose of 40 μg three times daily, and finally at a dose of 700 μg three times daily. The dose of clenbuterol was adjusted to maintain the patient’s resting heart rate at a level below 100 beats/min. After clenbuterol administration, no serious side effects were observed, but most patients developed a mild tremor, four developed muscle cramps, one developed diaphoresis, and although no new arrhythmias were evident, heart rate increased as expected following β-agonist administration 98. The authors acknowledged that the potential benefits of clenbuterol administration in cases of heart failure should be interpreted with caution, since adverse effects on the heart and the skeletal muscle have been reported in animal models 86.
Summary
The action of β-agonists on β-adrenoceptors in smooth muscle facilitates their life-saving role in the prevention and treatment of bronchospasm in asthma. On the other hand, most evidence obtained from rigorously controlled animal studies has found that chronic stimulation of the β-adrenoceptors in skeletal muscle can elicit anabolic effects. This knowledge has served as the basis for many of the potential therapeutic applications of β-agonists for skeletal muscle wasting disorders, including many neuromuscular diseases, aging, and several metabolic conditions that cause muscle catabolism. Although there is great promise that β-agonists can be used for treating these conditions, their clinical application has been limited by cardiovascular side effects, especially when β-agonists are administered chronically and at high doses. Newer generation β-agonists (such as formoterol) have been shown to elicit an anabolic response in skeletal muscle even at very low doses, and this has renewed enthusiasm for their clinical application, especially because they exhibit reduced effects on the heart and cardiovascular system compared with older generation β-agonists (such as fenoterol and clenbuterol). However, the potentially deleterious cardiovascular side effects of β-agonists have not been obviated completely, so it is important to refine their development. In so doing, it is hoped that beneficial effects of β-agonists can find application to these severe muscle-wasting conditions that impact not only on the ability to perform the tasks of daily living, or quality of life, but ultimately on life itself, since the maintenance of functional muscle mass is critical for survival. It is likely that a greater understanding of the β-adrenergic signaling pathway in skeletal muscle will reveal novel targets that will facilitate the development of new therapeutic strategies, ones that manipulate pathways that benefit skeletal muscle by increasing protein synthesis or reducing protein degradation, without simultaneously activating pathways that affect the cardiovascular system deleteriously.
Despite warnings to athletes about the potential side effects of using β-agonists for athletic performance or enhancing physical appearance, there is no doubt that these drugs will continue to be used either alone or in conjunction with other compounds. It is hoped that the wealth of evidence presented in this review regarding the effects of β-agonists on skeletal muscle (and on other tissues) might help to encourage athletes not using these drugs safely for the purpose they were originally intended (i.e., bronchospasm), to reconsider their actions. Although very promising, the therapeutic potential of β-agonists for muscle-wasting conditions will not be realized until all aspects relating to their safety can be established, especially for their chronic, long-term administration necessary for attenuating the loss of muscle size and strength in these severe muscle-wasting conditions.
References- Role of beta-adrenoceptor signaling in skeletal muscle: implications for muscle wasting and disease. Lynch GS, Ryall JG. Physiol Rev. 2008 Apr; 88(2):729-67. https://www.physiology.org/doi/full/10.1152/physrev.00028.2007
- Effects of beta(2)-agonist clenbuterol on biochemical and contractile properties of unloaded soleus fibers of rat. Ricart-Firinga C, Stevens L, Canu MH, Nemirovskaya TL, Mounier Y. Am J Physiol Cell Physiol. 2000 Mar; 278(3):C582-8. https://www.physiology.org/doi/full/10.1152/ajpcell.2000.278.3.C582
- Time course in calpain activity and autolysis in slow and fast skeletal muscle during clenbuterol treatment. Douillard A, Galbes O, Rossano B, Vernus B, Bonnieu A, Candau R, Py G. Can J Physiol Pharmacol. 2011 Feb; 89(2):117-25. https://www.ncbi.nlm.nih.gov/pubmed/21326343/
- Effects of clenbuterol on contractile and biochemical properties of skeletal muscle. Dodd SL, Powers SK, Vrabas IS, Criswell D, Stetson S, Hussain R. Med Sci Sports Exerc. 1996 Jun; 28(6):669-76. https://www.ncbi.nlm.nih.gov/pubmed/8784754/
- Clenbuterol and formoterol decrease force production in isolated intact mouse skeletal muscle fiber bundles through a beta2-adrenoceptor-independent mechanism. McCormick C, Alexandre L, Thompson J, Mutungi G. J Appl Physiol (1985). 2010 Dec; 109(6):1716-27. https://www.physiology.org/doi/full/10.1152/japplphysiol.00592.2010
- Py G, Ramonatxo C, Sirvent P, et al. Chronic clenbuterol treatment compromises force production without directly altering skeletal muscle contractile machinery. The Journal of Physiology. 2015;593(Pt 8):2071-2084. doi:10.1113/jphysiol.2014.287060. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4405760/
- Effects of chronic administration of clenbuterol on contractile properties and calcium homeostasis in rat extensor digitorum longus muscle. Sirvent P, Douillard A, Galbes O, Ramonatxo C, Py G, Candau R, Lacampagne A. PLoS One. 2014; 9(6):e100281. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4074032/
- https://www.wada-ama.org/en/content/what-is-prohibited/prohibited-at-all-times/non-approved-substances
- Role of β-Adrenoceptor Signaling in Skeletal Muscle: Implications for Muscle Wasting and Disease. Physiol Rev 88: 729–767, 2008 https://doi.org/10.1152/physrev.00028.2007 https://www.physiology.org/doi/full/10.1152/physrev.00028.2007
- Dodds RM, Granic A, Davies K, Kirkwood TB, Jagger C, Sayer AA. Prevalence and incidence of sarcopenia in the very old: findings from the Newcastle 85+ Study. J Cachexia Sarcopenia Muscle 2017; 8: 229–237.
- von Haehling S, Ebner N, Dos Santos MR, Springer J, Anker SD. Muscle wasting and cachexia in heart failure: mechanisms and therapies. Nat Rev Cardiol 2017; 14: 323–341
- Morley JE, Anker SD, von Haehling S. Prevalence, incidence, and clinical impact of sarcopenia: facts, numbers, and epidemiology‐update 2014. J Cachexia Sarcopenia Muscle 2014; 5: 253–259
- Landi F, Marzetti E, Martone AM, Bernabei R, Onder G. Exercise as a remedy for sarcopenia. Curr Opin Clin Nutr Metab Care 2014; 17: 25–31
- Bauer JM, Verlaan S, Bautmans I, Brandt K, Donini LM, Maggio M, McMurdo ME, Mets T, Seal C, Wijers SL, Ceda GP, De Vito G, Donders G, Drey M, Greig C, Holmback U, Narici M, McPhee J, Poggiogalle E, Power D, Scafoglieri A, Schultz R, Sieber CC, Cederholm T. Effects of a vitamin D and leucine‐enriched whey protein nutritional supplement on measures of sarcopenia in older adults, the PROVIDE study: a randomized, double‐blind, placebo‐controlled trial. J Am Med Dir Assoc 2015; 16: 740–747.
- Vitale G, Cesari M, Mari D. Aging of the endocrine system and its potential impact on sarcopenia. Eur J Intern Med 2016; 35: 10–15.
- Morley JE. Pharmacologic Options for the Treatment of Sarcopenia. Calcif Tissue Int 2016; 98: 319–333.
- Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE. SARC‐F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle 2016; 7: 28–36. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4799853/
- Pinto CL, Botelho PB, Carneiro JA, Mota JF. Impact of creatine supplementation in combination with resistance training on lean mass in the elderly. J Cachexia Sarcopenia Muscle 2016; 7: 413–421 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4864174/
- de Vries NM, Staal JB, van der Wees PJ, Adang EM, Akkermans R, Olde Rikkert MG, Nijhuis‐van der Sanden MW. Patient‐centred physical therapy is (cost‐) effective in increasing physical activity and reducing frailty in older adults with mobility problems: a randomized controlled trial with 6 months follow‐up. J Cachexia Sarcopenia Muscle 2016; 7: 422–435. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4864107/
- Foong YC, Chherawala N, Aitken D, Scott D, Winzenberg T, Jones G. Accelerometer‐determined physical activity, muscle mass, and leg strength in community‐dwelling older adults. J Cachexia Sarcopenia Muscle 2016; 7: 275–283 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4863829/
- Kamalakkannan G, Petrilli CM, George I, LaManca J, McLaughlin BT, Shane E, Mancini DM, Maybaum S. Clenbuterol increases lean muscle mass but not endurance in patients with chronic heart failure. J Heart Lung Transplant 2008; 27: 457–461. https://www.ncbi.nlm.nih.gov/pubmed/18374884
- Harrington D, Chua TP, Coats AJ. The effect of salbutamol on skeletal muscle in chronic heart failure. Int J Cardiol 2000; 73: 257–265. https://www.ncbi.nlm.nih.gov/pubmed/10841968
- Mettauer B, Rouleau JL, Burgess JH. Detrimental arrhythmogenic and sustained beneficial hemodynamic effects of oral salbutamol in patients with chronic congestive heart failure. Am Heart J 1985; 109: 840–847 https://www.ncbi.nlm.nih.gov/pubmed/3984838
- Toledo M, Springer J, Busquets S, Tschirner A, Lopez‐Soriano FJ, Anker SD, Argiles JM. Formoterol in the treatment of experimental cancer cachexia: effects on heart function. J Cachexia Sarcopenia Muscle 2014; 5: 315–320 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4248407/
- Potsch MS, Tschirner A, Palus S, von Haehling S, Doehner W, Beadle J, Coats AJ, Anker SD, Springer J. The anabolic catabolic transforming agent (ACTA) espindolol increases muscle mass and decreases fat mass in old rats. J Cachexia Sarcopenia Muscle 2014; 5: 149–158. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4053568/
- Stewart Coats AJ, Ho GF, Prabhash K, von Haehling S, Tilson J, Brown R, Beadle J, Anker SD. for, on behalf of the ACTONEsg. Espindolol for the treatment and prevention of cachexia in patients with stage III/IV non‐small cell lung cancer or colorectal cancer: a randomized, double‐blind, placebo‐controlled, international multicentre phase II study (the ACT‐ONE trial). J Cachexia Sarcopenia Muscle 2016; 7: 355–365. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4929828/
- Embleton P, Thorne G.MuscleMag Int 576-1998.
- Clarkson PM, Thompson HS.Sports Med 24: 366-1997.
- Maltin CA, Delday MI, Watson JS, Heys SD, Nevison IM, Ritchie IK, Gibson PH.Clin Sci 84: 651-1993. http://www.clinsci.org/content/84/6/651.long
- Duncan ND.Striated Muscle Adaptations Resulting From Exercise and Clenbuterol Administration. 1996.
- Brower KJ, Blow FC, Young JP, Hill EM.Br J Addict 86: 759-1991. https://deepblue.lib.umich.edu/bitstream/handle/2027.42/73678/j.1360-0443.1991.tb03101.x.pdf?sequence=1&isAllowed=y
- Delbeke FT, Desmet N, Debackere M.Int J Sports Med 16: 66-1995.
- Tschan M, Perruchoud A, Herzog H.Eur J Clin Pharmacol 15: 159-1979.
- Murugaiah KD, O’Donnell JM.Res Commun Mol Pathol Pharmacol 86: 311-1994.
- Harkins JD, Woods WE, Lehner AF, Fisher M, Tobin T.J Vet Pharmacol Ther 24: 7-2001.
- Prather ID, Brown DE, North P, Wilson JR.Med Sci Sports Exercise 27: 1118-1995. https://www.ncbi.nlm.nih.gov/pubmed/7476054
- Goldstein DR, Dobbs T, Krull B, Plumb VJ.South Med J 91: 780-1998. https://www.ncbi.nlm.nih.gov/pubmed/9715231
- Kierzkowska B, Stanczyk J, Kasprzak JD.Circ J 69: 1144-2005. https://www.jstage.jst.go.jp/article/circj/69/9/69_9_1144/_pdf/-char/en
- Urhausen A, Albers T, Kindermann W.Heart 90: 496-2004. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1768225/
- Anis AH, Lynd LD, Wang XH, King G, Spinelli JJ, Fitzgerald M, Bai T, Pare P.Cmaj 164: 625-2001. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC80815/
- Agbenyega ET, Morton RH, Hatton PA, Wareham AC.2Comp Biochem Physiol C Pharmacol Toxicol 111: 397-1995 https://www.ncbi.nlm.nih.gov/pubmed/8564781
- Fredriksson R, Lagerström MC, Lundin LG, Schiöth HB.Mol Pharmacol 63: 1256-2003.
- Dixon RAF, Kobilka BK, Strader DJ, Benovic JL, Dohlman HG, Frielle T, Bolanowski MA, Bennett CD, Rands E, Diehl RE, Mumford RA, Slater EE, Sigal IS, Caron MG, Lefkowitz RJ, Strader CD.Nature 321: 75-1986.
- Kobilka BK, Dixon RA, Frielle T, Dohlman HG, Bolanowski MA, Sigal IS, Yang-Feng TL, Francke U, Caron MG, Lefkowitz RJ.2Proc Natl Acad Sci USA 84: 46-1987.
- Gosmanov AR, Wong JA, Thomason DB.Am J Physiol Cell Physiol 283: C1025-2002.
- Cherezov V, Rosenbaum DM, Hanson MA, Rasmussen SG, Thian FS, Kobilka TS, Choi HJ, Kuhn P, Weis WI, Kobilka BK, Stevens RC.2Science 318: 1258-2007.
- Tasken K, Aandahl EM.Physiol Rev 84: 137-2004.
- Rockman HA, Koch WJ, Lefkowitz RJ.Nature 415: 206-2002.
- Beitzel F, Gregorevic P, Ryall JG, Plant DR, Sillence MN, Lynch GS.2J Appl Physiol 96: 1385-2004.
- Kim YS, Sainz RD, Molenaar P, Summers RJ.12Biochem Pharmacol 42: 1783-1991.
- Rattigan S, Appleby GJ, Edwards SJ, McKinstry WJ, Colquhoun EQ, Clark MG, Richter EA.Biochem Biophys Res Commun 136: 1071-1986.
- Martin WH 3rd, Murphree SS, Saffitz JE.Circ Res 64: 1096-1989.
- Ryall JG, Gregorevic P, Plant DR, Sillence MN, Lynch GS.2Am J Physiol Regul Integr Comp Physiol 283: R1386-2002.
- Kaumann AJ, Lynham JA.Br J Pharmacol 120: 1187-1997.
- Evans BA, Papaioannou M, Hamilton S, Summers RJ.3Br J Pharmacol 127: 1525-1999.
- Kaumann AJ, Engelhardt S, Hein L, Molenaar P, Lohse M.1214Naunyn-Schmiedebergs Arch Pharmacol 363: 87-2001.
- Hutchinson DS, Bengtsson T, Evans BA, Summers RJ.3a3bBr J Pharmacol 135: 1903-2002.
- O’Donnell SR.The Role of β Receptor Agonist Therapy in Asthma Mortality. 4-1993.
- Ball DI, Brittain RT, Coleman RA, Denyer LH, Jack D, Johnson M, Lunts LH, Nials AT, Sheldrick KE, Skidmore IF.2Br J Pharmacol 104: 665-1991.
- Xiao RP.2siSci STKE 2001: RE15-2001.
- Kilts JD, Gerhardt MA, Richardson MD, Sreeram G, Mackensen GB, Grocott HP, White WD, Davis RD, Newman MF, Reves JG, Schwinn DA, Kwatra MM.2siCirc Res 87: 705-2000
- Gosmanov AR, Wong JA, Thomason DB.Am J Physiol Cell Physiol 283: C1025-2002
- Communal C, Colucci WS, Singh K.iJ Biol Chem 275: 19395-2000.
- Yamamoto DL, Hutchinson DS, Bengtsson T.2Diabetologia 50: 158-2007.
- Bodine SC, Stitt TN, Gonzalez M, Kline WO, Stover GL, Bauerlein R, Zlotchenko E, Scrimgeour A, Lawrence JC, Glass DJ, Yancopoulos GD.Nat Cell Biol 3: 1014-2001.
- Burgess CD, Beasley R, Crane J, Pearce N.2Agonists in Asthma Treatment. 257-1997.
- Kendall MJ, Haffner CA.The Role of β Receptor Agonist Therapy in Asthma Mortality. 163-1993.
- Abramson MJ, Walters J, Walters EH.Am J Respir Med 2: 287-2003. https://www.ncbi.nlm.nih.gov/pubmed/14719995
- Baldi A, Bontempo V, Cheli F, Corino C, Polidori F.Zentralbl Veterinarmed A 41: 189-1994.
- Matsumoto K, Ojima K, Ohta H, Watanabe H.21Pharmacol Biochem Behav 49: 13-1994.
- Yamashita J, Onai T, York DA, Bray GA.Int J Obes Relat Metab Disord 18: 429-1994.
- Benelli A, Zanoli P, Bertolini A.Physiol Behav 47: 373-1990.
- Ingalls CP, Barnes WS, Smith SB.J Appl Physiol 80: 795-1996.
- Yaspelkis BB 3rd, Castle AL, Ding Z, Ivy JL.Acta Physiol Scand 165: 71-1999.
- Kuo CH, Ding Z, Ivy JL.Am J Physiol Endocrinol Metab 271: E847-1996.
- Torgan CE, Etgen GJ Jr, Brozinick JT Jr, Wilcox RE, Ivy JL.J Appl Physiol 75: 1471-1993.
- Suzuki J, Gao M, Xie Z, Koyama T.2Acta Physiol Scand 161: 317-1997.
- Au DH, Lemaitre RN, Curtis JR, Smith NL, Psaty BM.Am J Respir Crit Care Med 161: 827-2000.
- Kaumann AJ.Trends Pharmacol Sci 18: 70-1997.
- Deshaies Y, Willemot J, Leblanc J.Can J Physiol Pharmacol 59: 113-1981.
- Duncan ND, Williams DA, Lynch GS.Clin Sci 98: 339-2000.
- Cepero M, Perez-Pertejo Y, Cubria JC, Reguera R, Balana-Fouce R, Ordonez C, Ordonez Escudero D.Comp Biochem Physiol C Toxicol Pharmacol 126: 45-2000.
- Illera JC, Silvan G, Blass A, Martinez MM, Illera M.Analyst 123: 2521-1998.
- Jeppsson AB, Waldeck B, Widmark E.Acta Pharmacol Toxicol 58: 121-1986.
- Gregorevic P, Ryall JG, Plant DR, Sillence MN, Lynch GS.Am J Physiol Heart Circ Physiol 289: H344-2005.
- Burniston JG, Ng Y, Clark WA, Colyer J, Tan LB, Goldspink DF.J Appl Physiol 93: 1824-2002.
- Wong K, Boheler KR, Bishop J, Petrou M, Yacoub MH.Cardiovasc Res 37: 115-1998.
- Baldwin KM, Ernst SB, Mullin WJ, Schrader LF, Herrick RE.J Appl Physiol 52: 591-1982.
- Murad N, Tucci PJ.Clin Exp Pharmacol Physiol 27: 352-2000.
- Duncan ND, Lynch GS, Jones DL, Williams DA.Med Sci Sports Exercise 28: S167-1996.
- Libretto SE.Arch Toxicol 68: 213-1994.
- Pack RJ, Alley MR, Dallimore JA, Lapwood KR, Burgess C, Crane J.Int J Exp Pathol 75: 357-1994.
- Beznak M.Can J Biochem Physiol 40: 25-1962.
- Benjamin IJ, Jalil JE, Tan LB, Cho K, Weber KT, Clark WA.Circ Res 65: 657-1989.
- Petrou M, Clarke S, Morrison K, Bowles C, Dunn M, Yacoub M.Circulation 99: 713-1999.
- Yacoub MH.Eur Heart J 22: 534-2001. https://watermark.silverchair.com/534.pdf?token=AQECAHi208BE49Ooan9kkhW_Ercy7Dm3ZL_9Cf3qfKAc485ysgAAAakwggGlBgkqhkiG9w0BBwagggGWMIIBkgIBADCCAYsGCSqGSIb3DQEHATAeBglghkgBZQMEAS4wEQQMNu2oNnRnMpAkyxrtAgEQgIIBXGh9xf_LtaidJrOxEedw6QqDZxHu3ZYeVfQuQh4pAFlxuxwhr3xO2wSQvdHR0FLIFHtGT6ojACR6DRZJYsSg-siXIuGcBmzd1efJ6QU4jlloSalYTGMkpecPSGWn-hfaPtS_GZuL00PcU-PfuCECIn5U3HSt7_vjP52TKCmwhW-069k-UPUmHK1RKbhfQm2jClp1E_NStPI0ciYsXPGBzdo-h2Cuj496SokIxwDp2s1f8Fu1Yod0uFKPHsPpYEtvpBK5qy-OoNnP14lIFym_QI5Ownst4IzAzwkW9mSWOtJGDcGneOa0b4bEqgvvqXBvzVGKfHRwjY4byv9mzmRFtzA9uK3y7sNgtTyD7Wkbo1joPKT3IdVEqNfsQ7J_cOMpNEh12FA3LKX6GR6Ow9aJT31WF_F4rUR5aa4LFneMdxBBuE1psLq2GlhffJKMaULcYBYZ7hC4z7pUkIbB3Q
- Klotz S, Barbone A, Reiken S, Holmes JW, Naka Y, Oz MC, Marks AR, Burkhoff D.J Am Coll Cardiol 45: 668-2005.
- Birks EJ, Tansley PD, Hardy J, George RS, Bowles CT, Burke M, Banner NR, Khaghani A, Yacoub MH.N Engl J Med 355: 1873-2006.