What is a colposcopy
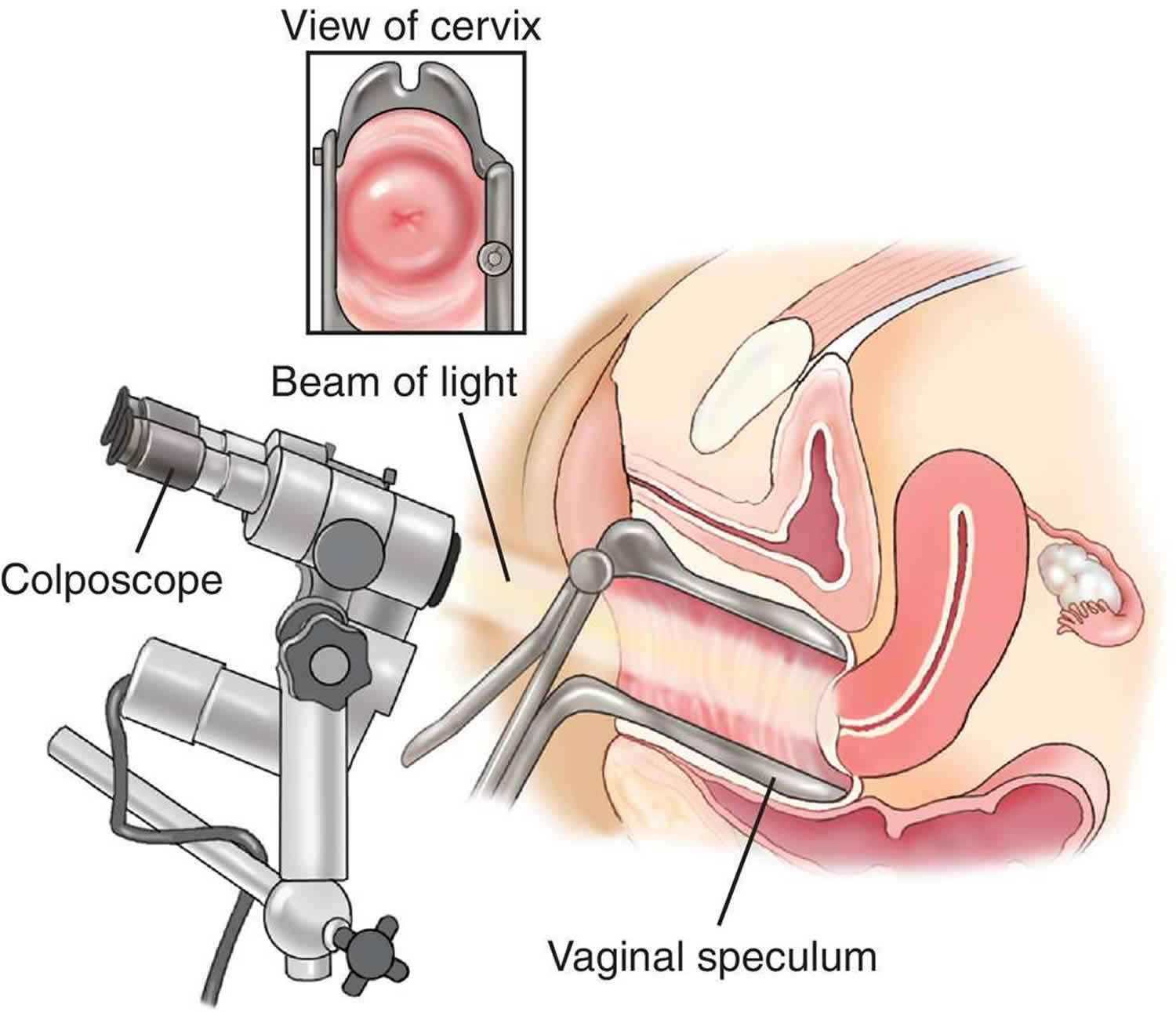
A colposcopy is a minor procedure in which a special microscope is used to examine the surface of the cervix for abnormalities. Gynecologists use colposcope, which looks like a pair of binoculars with a bright light that allows them a greatly magnified view of the surface of the vagina and cervix. If an area needs further investigation, your gynecologist can remove a tiny piece of tissue and send it to a laboratory for a biopsy. Colposcopy is often done if cervical screening (Pap smear test) finds abnormal cells in your cervix. During a colposcopy, a small amount of tissue might be removed and sent to a laboratory for testing. A colposcopy can confirm whether cells in your cervix are abnormal and determine whether you need treatment to remove them.
A colposcopy is usually done to assess the health of a woman’s cervix, which is the neck of the womb, and to see whether there are abnormal cells or growths (see Figures 1 to 7). These abnormal cells in your cervix aren’t harmful and often go away on their own, but sometimes there’s a risk they could eventually turn into cervical cancer if not treated.
Although the colposcopy procedure is usually not painful, the cervical biopsy can cause discomfort, cramping, bleeding, or even pain in some women.
When a colposcopy may be needed
You may be referred for a colposcopy within a few weeks of cervical screening (Pap smear test) if:
- some of the cells in your Pap smear screening test sample are abnormal
- the nurse or doctor who carried out the screening test thought your cervix didn’t look as healthy as it should
- it wasn’t possible to give you a clear result after several Pap smear screening tests
- unusual or unexplained bleeding, such as after intercourse
- an abnormal lump or growth on your cervix or vagina
A colposcopy can also be used to find out the cause of problems such as unusual vaginal bleeding (for example, bleeding after sex).
The colposcopy procedure can help diagnose conditions such as:
- cervical cancer or precancer
- benign growths such as polyps
- inflammation of the cervix
- genital warts.
Try not to worry if you’ve been referred for a colposcopy. It’s very unlikely you have cancer and any abnormal cells won’t get worse while you’re waiting for your appointment.
Colposcopy procedure
How to prepare for a colposcopy
Ask your gynecologist to explain the benefits and risks of a colposcopy. Let them know if you are pregnant.
The colposcopy procedure is usually done when you are not menstruating. For 24 to 48 hours before your colposcopy procedure, you should also not:
- wear tampons
- have sex
- use vaginal medicines, lubricants or creams
- douche
A colposcopy is safe during pregnancy, but a biopsy (removing a tissue sample) and any treatment will usually be delayed until a few months after giving birth.
Bring a panty liner – as you may have some light bleeding or discharge afterwards.
You can eat and drink as normal.
What happens during a colposcopy
A colposcopy will most likely be done in your gynecologist’s rooms or a clinic. Colposcopy takes about 15-30 minutes and you can go home soon afterwards.
You can bring a friend, partner or family member with you to the gynecologist’s rooms or a clinic if you think it will help you feel more at ease.
You might feel awkward and uncomfortable, but colposcopy is not usually painful. You won’t need an anesthetic for the colposcopy, but you might be offered a local anesthetic if the biopsy is in a sensitive area.
A colposcopy is carried out by a specialist called a colposcopist. This may be a doctor (gynecologist) or a specially trained nurse.
During the colposcopy procedure:
- you undress from the waist down (a loose skirt may not need to be removed) and lie down in a special type of chair with padded supports for your legs
- a device called a speculum is inserted into your vagina and gently opened similar to having a cervical screening test (Pap smear test)
- a microscope with a light is used to look at your cervix – this stays about 30cm (12 inches) outside your vagina and allows the colposcopist to see the cells on your cervix
- special liquids, weak solution of acetic acid (similar to vinegar) or an iodine solution, are applied to your cervix to highlight any abnormal areas – you may feel a mild tingling or burning sensation when these are applied. Schiller’s iodine test using an iodine solution – normal tissue on the outside of the cervix stains dark brown when iodine is applied. However, cervical abnormalities may not stain with iodine which helps the colposcopist to locate any areas of abnormal cells. This test may be used following acetic acid colposcopy and is often used before treatment.
- a small sample of tissue (a biopsy) may be removed for closer examination in a laboratory – this shouldn’t be painful, but you may feel a slight pinch or stinging sensation
Most colposcopists use a combination of the acetic acid and Schiller’s iodine tests. If there is an abnormality the colposcopist should be able to estimate whether or not treatment will be needed according to:
- How white the tissue goes after using acetic acid
- How quickly the tissue turns white
- How smooth or irregular the surface is
- The different patterns of the blood vessels (mosaic and punctation) under the surface of the cervix.
If it’s obvious that you have abnormal cells in your cervix, you may be offered treatment to remove the cells immediately. Otherwise, you’ll need to wait until you get your biopsy result.
The small sample of tissue (a biopsy) is sent to a lab to be looked at under a microscope. A biopsy is the best way to tell for certain whether an abnormal area is a pre-cancer, a true cancer, or neither.
Taking a biopsy
To be sure of the diagnosis, a biopsy is often required – this means taking a sample of tissue from the cervix. Depending on the results of this biopsy the colposcopist will decide whether you need treatment.
There are two types of biopsy that could be offered.
- A diagnostic or punch biopsy, which is a small biopsy that often doesn’t require local analgesia (anesthetic). Two or three punch biopsies may be taken at the first visit.
- The second type of biopsy is a loop excision, which is slightly larger and does require local anesthetic. This type of biopsy is usually a treatment biopsy and under certain circumstances can be performed at the first visit in some clinics.
If the colposcopist can immediately tell that you will need treatment this can be done during the same visit – in this case all of the abnormal area is removed and this constitutes the biopsy. Other more invasive types of treatment require a separate appointment.
Figure 1. Colposcopy
Figure 2. Colposcopy procedure
After a colposcopy
After a colposcopy without a biopsy, you can carry on normal activities right away, including work and driving, immediately – although some women prefer to rest until the next day.
If you have also had tissue removed for a biopsy, then you could have cramps for a day or so. If so, acetaminophen (paracetamol) can help. It is normal to have a slight vaginal discharge or light bleeding for around 3 to 6 days.
After a colposcopy biopsy, you will be asked to avoid sexual intercourse and heavy exercise, and not use tampons, medications, lubricants or creams for a couple of days. You can shower, but don’t have a bath or a swim.
Depending on what the colposcopy biopsy shows, you might need treatment, such as freezing abnormal cervical cells with cryosurgery. If the results are unclear, you might need to have more tests. Often no further action is required.
There is a very small risk of infection or heavy bleeding after colposcopy. You should contact your doctor if you have:
- a high temperature
- a bad-smelling vaginal discharge
- severe pelvic pain
- heavy bleeding that lasts longer than 5 days
What is a punch biopsy?
A punch biopsy is when a small sample of the cervix is taken at the time of a colposcopy examination, usually after the application of solutions to the cervix (used to highlight the abnormal area or areas). More than one punch biopsy may be taken. It is purely for diagnostic purposes. The biopsy is sent to the histopathology department who will report on the type of abnormality present. Some women do not feel anything when a punch biopsy is taken while others experience a little discomfort (tenderness or an ache) during and/or after the biopsy. You may experience a small amount of bleeding and/or discharge for a few days following a punch biopsy. You may get cramps like a period pain.
How long will it take for me to get the results of the biopsy taken at colposcopy?
Your colposcopist will often write to you with your results. It may take four to eight weeks for you to get the letter with your results. If the colposcopist is concerned that you may have cancer, then a telephone call or a clinic visit may be offered within two to three weeks.
Is it possible to see if I have cancer during colposcopy?
Not necessarily – it will depend on the size, position and appearance of any abnormality seen. If there are any highly suspicious areas seen at colposcopy, then a biopsy may be recommended.
What is a cervix
The cervix is part of the lower end of the uterus. The lumen (internal cavity) of the uterus communicates with the vagina by way of a narrow passage through the cervix called the cervical canal.
Cervix function
The cervical canal contains cervical glands that secrete mucus, thought to prevent the spread of microorganisms from the vagina into the uterus. Near the time of ovulation, the mucus becomes thinner than usual and allows easier passage for sperm.
The cervix has two different parts and is covered with two different types of cells.
- The part of the cervix closest to the body of the uterus is called the endocervix and is covered with glandular cells.
- The part next to the vagina is the exocervix (or ectocervix) and is covered in squamous cells.
These two cell types meet at a place called the transformation zone. The exact location of the transformation zone changes as you get older and if you give birth.
The cervix and superior part of the vagina are supported by cardinal (lateral cervical) ligaments extending to the pelvic wall.
Figure 3. Cervix position
Figure 4. Cervix location

Colposcopy results
After a colposcopy, your doctor or nurse will often be able to tell you what they’ve found straight away.
If they take a colposcopy biopsy (remove a small sample of tissue to be examined in a laboratory), you may need to wait up to four to eight weeks to receive your result by post.
When your biopsy is analyzed in the laboratory, they will be looking for different changes in the cells.
The changes they review are:
- The cell nucleus – irregular size, shape and colour of the cell nucleus (the part of the cell that contains the DNA) is the first indication of an abnormality
- The maturity of the cells – a normal cell will grow from an immature to mature cell. Cells that are abnormal can often still grow into mature cervical cells, which will still function in a similar way to normal cells. If the abnormal cells are still able to mature it indicates a low grade abnormality (e.g.,. cervical intra-epithelial neoplasia 1 [CIN 1])). New cells that grow with increased abnormalities may no longer be able to function normally and may remain as immature abnormal cells. The more immature the abnormal cells there are, the higher the grade of abnormality (e.g., CIN2 and CIN3). Immature abnormal cells have a greater potential to develop into cancerous cells than mature abnormal cells
- The thickness of abnormal cells in the lining of the cervix – the grading for cervical intra-epithelial neoplasia (CIN) cells comes from the thickness of immature abnormal cells within the ectocervix.
Normal result
About 4 in every 10 women who have a colposcopy have a normal result.
This means no abnormal cells were found in your cervix during the colposcopy and/or biopsy and you don’t need any immediate treatment.
You’ll be advised to continue with cervical screening as usual, in case abnormal cells develop later on.
Depending on your age, you’ll be invited for a cervical screening appointment in three or five years.
Abnormal result
If your biopsy comes back positive it is because you have abnormal cells or cervical intraepithelial neoplasia (CIN), you will have both abnormal mature cells and variable quantities of immature abnormal cells. Abnormal cells may develop into cancer of the cervix, so the quantity of these cells within the ectocervix is important. The grading of cervical intraepithelial neoplasia (CIN) is established according to the amount of immature cells within the sample taken and all the results below mean that you have cervical abnormalities.
About 6 in every 10 women have abnormal cells in their cervix – known as cervical intra-epithelial neoplasia (CIN) or cervical glandular intra-epithelial neoplasia (CGIN).
- This isn’t cancer, but there’s a risk it could turn into cancer if untreated.
Abnormal cells may be detected while a colposcopy is carried out, but a biopsy will be needed to determine what the risk of these becoming cancerous is and whether treatment is needed.
Grading of cervical intra-epithelial neoplasia (CIN) means that if you have:
- CIN1: the lining of the cervix has fully normal cells at the surface and the lower third has immature abnormal cells
- CIN2: the lining of the cervix has normal cells at the surface and the lower two-thirds have abnormal cells
- CIN3: the lining of the cervix has abnormal cells throughout its entire thickness.
High grade changes (also called moderate or severe dyskaryosis, or CIN2 or 3) or abnormal glandular cells (also known as glandular dyskaryosis) will usually require treatment to remove the abnormal areas. You will be asked to attend colposcopy to investigate further.
The different types of abnormal biopsy result and what they mean are as follows:
- CIN 1 – it’s unlikely the cells will become cancerous and they may go away on their own; no treatment is needed and you’ll be invited for a cervical screening test in 12 months to check they’ve gone
- CIN 2 – there’s a moderate chance the cells will become cancerous and treatment to remove them is usually recommended
- CIN 3 – there’s a high chance the cells will become cancerous and treatment to remove them is recommended
- Cervical Glandular Intra-epithelial Neoplasia (CGIN) – there’s a high chance the cells will become cancerous and treatment to remove them is recommended
Your colposcopy biopsy letter may also mention the word koilocytosis or koilocytotic atypia. This just means that some of the cells in your colposcopy biopsy show specific changes that are commonly caused by human papilloma virus (HPV) infections. Koilocytosis is sometimes referred to as a calling card for human papilloma virus (HPV). It is often seen in biopsy samples that also have abnormal cell growth (sometimes called dysplasia). It is the abnormal cell growth that will be watched and treated if necessary, as it is these cells that may become precancerous or cancerous if left untreated.
Having cervical abnormalities does not mean that you have or will get cancer. It just means that the laboratory has detected some changes to your cells that are abnormal and, if they are not treated, they may develop into cervical cancer in the future.
In rare cases, a colposcopy and biopsy will find cervical cancer. If this happens, you’ll be referred to a team of specialists to discuss treatment.
Abnormal cervical cells: CIN and CGIN
The cervix is covered with a layer of skin-like cells on its outer surface called the ectocervix. There are also glandular cells, usually lining the inside of the cervical canal, called the endocervix. These cells produce mucus. The skin-like cells of the ectocervix can become cancerous, leading to a squamous cell cervical cancer. The glandular cells of the endocervix can also become cancerous, leading to an adenocarcinoma of the cervix. Changes to these different areas are categorised differently: cervical intraepithelial neoplasia (CIN) is the name given to cellular changes to the ectocervix and Cervical Glandular Intra-epithelial Neoplasia (CGIN) represent abnormal changes to the endocervix.
Treatment for cervical intraepithelial neoplasia (CIN) depends on the degree of abnormality of the cells (see abnormal cells table). Cervical Glandular Intra-epithelial Neoplasia (CGIN) is not as common as CIN, but it is treated similarly. There is no good evidence that CGIN is more ‘aggressive’ than cervical intraepithelial neoplasia (CIN). Cervical Glandular Intra-epithelial Neoplasia (CGIN) is harder to pick up during screening and since the cellular changes are inside the cervical canal they can be marginally more difficult to treat.
If your cervical screening result shows abnormal cells you may be asked to attend a colposcopy appointment. Remember testing positive for cervical intraepithelial neoplasia (CIN) or cervical glandular intra-epithelial neoplasia (CGIN) means that you have abnormal cervical cells that may lead to cancer if untreated, but cervical intraepithelial neoplasia (CIN) and cervical glandular intra-epithelial neoplasia (CGIN) are not in themselves cancerous. Treatment for abnormal cellular changes is usually very successful.
Figure 5. Cervical epithelium
Figure 6. Cervical Transformation Zone
Figure 7. Cervical Transformation Zone
Figure 8. Cervical cells
Table 1. Understanding colposcopy biopsy test results
I’ve received an abnormal screening result, what happens next?
This will depend on the abnormality. Usually low grade squamous dyskaryosis will not require treatment; instead it will be closely monitored, either with a repeat screening in six months or with referral to a colposcopy clinic (this depends on the country you live in). High grade squamous dyskaryosis will require further investigation at a colposcopy clinic and may require treatment.
Some clinics and hospitals have a longer waiting list for treatments than others. If you are concerned about the timing of your appointment (short or long) do speak to your doctor.
I’m pregnant and just found out that I have an abnormal screening result, what do I do?
You should seek advice from your doctor. They will often ask you to undergo a colposcopy examination to properly assess the change on the cervix so that they can advise you with regard to any treatment that may be required. A colposcopy examination will not cause any risk to the pregnancy. If you are asked to attend a colposcopy examination do remember to tell your colposcopist that you are pregnant just in case they are not aware.
If I have high risk HPV, will my body ever clear it?
In research studies, most people with a healthy immune system who test positive for a high risk genital human papillomavirus (HPV) infection do eventually clear the infection (test negative), often within a year or two 1. Unfortunately, because human papillomavirus (HPV) is symptomless (making it difficult to identify and study in healthy individuals) and since an infection can persist in some cases over many years and may result in recurrent abnormalities (though this is rare) it hard to give a solid ‘yes’ or ‘no’ answer to this question. However, it does seem that your body will eventually clear the infection and the high risk human papillomavirus (HPV) will not always be active.
My colposcopy results showed that I have CIN, do I have cervical cancer?
No. If your results show you have cervical intraepithelial neoplasia (CIN) this means that you have abnormal/precancerous changes to cells in your cervix. These changes are not cancerous, but without treatment these cells could change into cancerous cells.
If cervical abnormalities are not cancer, why do I have to have treatment?
Although cervical abnormalities are not a cancer, the reason treatment is offered is to reduce the risk of a cancer developing in the future. Cervical abnormalities are changes to the cells on the surface of the cervix caused by high risk HPV. Without treatment there is a chance that, over time, these changes could turn into cancer. Research has shown that changes in abnormalities do not usually escalate quickly and it can take between 10 to 15 years for a cancer to develop.
What are the symptoms of cervical abnormalities (CIN or CGIN)?
Cervical abnormalities do not cause symptoms – no pain, no discharge and no bleeding. This is why it is important for you to attend your cervical screening (smear test) appointment when invited or to see your doctor if you experience any or all of the symptoms of cervical cancer.
How are abnormal cervical cells treated?
If your cervical screening result is abnormal you may be required to attend an outpatient colposcopy clinic where your cervix can be examined more closely. It is important to remember that abnormal cells can be treated. Treatment is usually given as an outpatient. Cervical abnormalities (CIN and CGIN) are largely treated in the same way.
Treatment can be dependent on:
- The grade and size of the abnormality diagnosed
- Your choice of treatment options
- Your colposcopists preference and recommendations
- Your age.
The main treatments (if advised) are either to eradicate the abnormal cells or remove the area of abnormality, and 95–98% of women are cured after one treatment. Between 2 and 5% of women do have recurrence of abnormalities, which will require further treatment 1.
The main treatments for CIN2, CIN3 and CGIN are:
- Removal of abnormal area, using either large loop excision of the transformation zone LEEP (Loop Electrosurgical Excisional Procedure) also called LLETZ (Large Loop Excision of the Transformation Zone), SWETZ, NETZ, cone biopsy, laser therapy or, very occasionally, a hysterectomy (usually only if you have other gynaecological problems)
- Eradication of the abnormal area with using cryotherapy (a cold treatment), laser therapy orcold coagulation (hot treatments).
If you have any concerns or experience any side effects, either physical or emotional, after your treatment that are worrying you or affecting your quality of life, please raise them with your colposcopy team or doctor.
What happens if I have an obvious abnormality at colposcopy or a positive biopsy result?
This will depend on the grade of abnormality. If the colposcopy or biopsy show CIN1, then treatment is rarely required, instead you will be monitored in either colposcopy or back at your doctor clinic. However, if CIN2 or CIN3 is identified then treatment may be required. In the US, the most common form of treatment is called LEEP (Loop Electrosurgical Excisional Procedure) also called LLETZ (Large Loop Excision of the Transformation Zone).
Treatments
If a colposcopy finds abnormal cells in your cervix, treatment to remove these cells may be recommended.
There’s sometimes a risk these cells could become cancerous if left untreated. Removing them means they won’t be able to turn into cancer.
The aim of treatment is to remove the abnormal cells while minimizing damage to healthy tissue. Usually an area about the size of a fingertip is removed.
For women requiring treatment, this treatment has been shown to reduce the risk of cervical cancer by 95%. However, even after treatment you will have a slightly greater risk of developing cervical cancer than women who have not had cervical abnormalities. It is, therefore, very important that you continue to attend regular check-ups, even after your treatment. Studies have found that the vast majority of women who have been treated for cervical abnormalities do not develop cervical cancer, even up to eight years after treatment 2, 3, 4.
When treatment is carried out
Treatment to remove abnormal cells from your cervix can be done at the same time as a colposcopy if it’s obvious that some of the cells in your cervix are abnormal.
But sometimes treatment can’t be done on the same day.
For example, you may need to wait until you get your biopsy result a few weeks later if it’s not immediately clear whether you have abnormal cells in your cervix.
Types of treatment
The treatment you will be offered depends on the type of abnormal cells you have in your cervix (the grade of CIN and/or the presence of CGIN) and how advanced the changes are. Your colposcopist will advise you on the specific treatment you will require during your colposcopy appointment. CIN1 is usually not treated, as these changes often return to normal given time and are not precancerous.
There are several ways abnormal cells can be removed from the cervix. Some of the main treatments are outlined below.
LEEP procedure
The most common treatment is LEEP (Loop Electrosurgical Excisional Procedure) also called LLETZ (Large Loop Excision of the Transformation Zone). LEEP (Loop Electrosurgical Excisional Procedure) is also called loop diathermy, loop cone, loop biopsy or loop excision.
LEEP procedure:
- involves removing the abnormal cells using a thin wire loop that’s heated with an electric current
- can be carried out at the same time as a colposcopy
- is usually done while you’re awake – local anesthetic is injected into your cervix to numb it during the treatment
- doesn’t usually need an overnight stay in hospital
Figure 8. LEEP procedure (LLETZ procedure)
Figure 9. LEEP cone biopsy
How do I prepare for LEEP?
- Your healthcare provider will explain the procedure and you can ask questions.
- You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully and ask questions if something is not clear.
- Generally, no preparation, such as fasting or sedation, is needed.
- If you are pregnant or think you may be, tell your healthcare provider.
- Tell your healthcare provider if you are sensitive to or are allergic to any medicines, latex, tape, iodine, and anesthesia.
- Tell your healthcare provider of all medicines (prescribed and over-the-counter) and herbal supplements that you are taking.
- Tell your healthcare provider if you have a history of bleeding disorders or if you are taking any blood-thinning medicines (anticoagulants), aspirin, or other medicines that affect blood clotting. You may be told to stop these medicines before the procedure.
- Your healthcare provider will tell you not to use tampons, vaginal creams or medicine, douching, or having sex before the procedure.
- LEEP is usually done when you are not having your menstrual period.
- Your healthcare provider may recommend that you take a pain reliever 30 minutes before the procedure.
- You may want to bring a sanitary napkin to wear home after the procedure.
- Follow any other instructions your provider gives you to get ready.
How is LEEP performed?
LEEP may be done in a healthcare provider’s office, on an outpatient basis, or as part of your stay in a hospital. Procedures may vary depending on your condition and your healthcare provider’s practices.
A LEEP should be done when you are not having your menstrual period to give a better view of the cervix. In most cases, LEEP is done in a health care professional’s office. The procedure only takes a few minutes.
During the LEEP procedure you will lie on your back and place your legs in stirrups. The health care professional then will insert a speculum into your vagina in the same way as for a pelvic exam. Local anesthesia will be used to prevent pain. It is given through a needle attached to a syringe. You may feel a slight sting, then a dull ache or cramp. The loop is inserted into the vagina to the cervix. There are different sizes and shapes of loops that can be used. You may feel faint during the procedure. If you feel faint, tell your health care professional immediately.
After the LEEP procedure, a special paste may be applied to your cervix to stop any bleeding. Electrocautery also may be used to control bleeding. The tissue that is removed will be studied in a lab to confirm the diagnosis.
Generally, LEEP follows this process:
- You will be asked to undress completely or from the waist down and put on a hospital gown.
- You will be instructed to empty your bladder before the procedure.
- You will lie on an exam table, with your feet and legs supported as for a pelvic exam.
- Your healthcare provider will insert an instrument called a speculum into your vagina to spread the walls of the vagina apart to expose the cervix.
- Often, the healthcare provider will use a colposcope, an instrument with a special lens similar to a microscope, to magnify the tissues. The colposcope will be placed at the opening of your vagina but does not enter your vagina.
- Your healthcare provider will look through the colposcope to locate any areas for treatment on the cervix or in the vagina. Photographs with the colposcope or sketches of the areas on your cervix may be made for your healthcare record.
- Your cervix may be cleaned and soaked with a vinegar solution, also called acetic acid solution. This helps make the abnormal tissues turn white and become more visible. You may feel a mild burning sensation. An iodine solution is sometimes used to coat the cervix, called the Schiller test.
- The healthcare provider will numb the area using a small needle to inject medicine.
- A type of forceps, called a tenaculum, may be used to hold the cervix steady for the procedure. You may feel some cramping when the tenaculum is applied.
- You will hear humming and/or blowing sounds from the equipment.
- The LEEP wire will be inserted through the speculum and passed through the abnormal tissues. One or more passes may be needed. You may feel pressure or a slight cramping.
- Some women feel faint during the procedure. Tell your healthcare provider or the nurse if you have this feeling.
- It is very important that you lie still during the procedure.
- The amount and location of tissue removed depends on the whether LEEP is being used as a diagnostic tool, or to remove abnormal tissue. LEEP wires come in different sizes and shapes.
- The electrical current will seal the blood vessels, so usually there is very little bleeding. Any bleeding from the LEEP site may be treated with a paste-like topical medicine.
- The tissue will be sent to a lab for further testing.
LEEP procedure side effects and risks
Some possible complications of LEEP procedure may include:
- Infection
- Bleeding
- Changes or scarring in the cervix from removal of tissue
- Trouble getting pregnant
- Potential for preterm birth or having a low birth weight baby
- Incomplete removal of the abnormal cells
If you are allergic to or sensitive to medications, iodine, or latex, tell your healthcare provider.
If you are pregnant or think you could be, tell your healthcare provider.
There may be other risks depending on your condition. Be sure to discuss any concerns with your healthcare provider before the procedure.
The most common risk in the first 3 weeks after a LEEP is heavy bleeding. If you have heavy bleeding, contact your health care professional. You may need to have more of the paste applied to the cervix to stop it.
LEEP has been associated with an increased risk of future pregnancy problems. Although most women have no problems, there is a small increase in the risk of premature births and having a low birth weight baby. In rare cases, the cervix is narrowed after the procedure. This narrowing may cause problems with menstruation.
There may be other risks depending on your condition. Be sure to discuss any concerns with your healthcare provider before the procedure.
Certain factors or conditions may interfere with LEEP. These factors include:
- Menstruation
- Acute pelvic inflammatory disease (PID)
- Acute inflammation of the cervix
LEEP procedure recovery
After LEEP, you may rest for a few minutes after the procedure before going home.
After the LEEP procedure, you may have:
- a watery, pinkish discharge
- mild cramping
- a brownish-black discharge (from the paste used)
You may want to wear a sanitary pad for bleeding. It is normal to have some mild cramping, spotting, and dark or black-colored discharge for several days. The dark discharge is from the medicine applied to your cervix to control bleeding.
It will take a few weeks for your cervix to heal. While your cervix heals, you should not place anything in the vagina, you may be instructed not to douche, use tampons, or have sex for 4 weeks after LEEP, or for a period of time recommended by your healthcare provider. Your health care professional will tell you when it is safe to do so.
You may also have other limits on your activity, including no strenuous activity or heavy lifting.
Take a pain reliever for cramping or soreness as directed by your healthcare provider. Aspirin or certain other pain medicines may increase the chance of bleeding. Be sure to take only recommended medicines.
Your healthcare provider will tell you when to return for further treatment or care. Generally, women who have had LEEP will need more frequent Pap tests.
You should contact your health care professional if you have any of the following problems:
- Heavy bleeding (more than your normal period)
- Bleeding with clots
- Severe abdominal pain
- Foul-smelling drainage from your vagina
- Fever and/or chills
Your healthcare provider may give you other instructions after the procedure, depending on your particular situation.
Will I need follow-up visits?
After the LEEP procedure, you will need to see your health care professional for follow-up visits. You will have cervical cancer screening to be sure that all of the abnormal cells are gone and that they have not returned. If you have another abnormal screening test result, you may need more treatment.
You can help protect the health of your cervix by following these guidelines:
- Have regular pelvic exams and cervical cancer screening.
- Stop smoking—smoking increases your risk of cancer of the cervix.
- Limit your number of sexual partners and use condoms to reduce your risk of sexually transmitted infections (STIs).
LEEP procedure on pregnancy outcomes
Retrospective, case-control observations conclude that overly aggressive use of diagnostic excisional procedures may produce long-term adverse obstetric outcomes 5, 6, 7. Cold knife conization and LEEP are associated with a small increase in the risk of preterm labor and low birth weight 5, 7. The risk of preterm delivery increases if the depth of LEEP or laser conization is more than 10 mm 5. The value of cervical length measurements during pregnancy for predicting preterm labor in women with a history of cervical intraepithelial neoplasia (CIN) treatments is unknown 7. Laser vaporization and cryotherapy did not affect outcomes, supporting the theory that ablation removes less tissue than excision 7. According to absolute risks, previous treatment with LEEP would result in two perinatal deaths per 1,000 pregnancies 6. The small absolute risk of preterm labor following cervical excisional procedures must be balanced with the risk of untreated cervical intraepithelial neoplasia 3 (CIN 3) 7. None of the treatments affected fertility 5.
Recent research has looked at the risk of preterm labour (giving birth before 37 weeks of pregnancy) for women who have LEEP (Loop Electrosurgical Excisional Procedure) or large loop excision of the transformation zone (LLETZ) 8, 9. This has been found to be linked to how deep the excision (area of tissue that is remove) is, which depends on how large the area of abnormalities is. The research shows that if the LEEP (Loop Electrosurgical Excisional Procedure) excision is less than 10 mm deep, the risk of preterm labor is not significantly higher 8, 9.
However, excisions that are deeper than 10 mm or repeated LEEP procedures may significantly increase the risk of preterm labour, depending on the individual 9. This is because deeper excisions remove more of the cervix, which reduces its ability to perform its function during pregnancy – which is to help keep the foetus in the uterus until birth. Each woman’s cervix is different; some are shorter than others, which means that there are no set rules about the effect LEEP treatment might have on future pregnancy.
If you are currently pregnant or are thinking about getting pregnant in the future, and have concerns about a previous LEEP, please raise this with your care team. They will be able to offer advice and reassure you. If you have had a deep excision, or have had repeated LEEP procedures they wish to put a stitch, called a cervical stich, in your remaining cervix to support it during any future pregnancies.
Chances of cervical cancer after LEEP
The goals of excisional treatment are complete removal of the lesion and the transformation zone, resulting in interpretable margins 10. There are conflicting reports as to whether margin status predicts the risk of recurrent disease 11. Treatment failure can occur in women with clear or involved margins 12. Women with clear margins show a pooled prevalence of high-grade residual disease of 3% vs. 18% in women with involved or uncertain margins 10.
Most women with involved margins will not develop persistent or recurrent disease 11. Based on the lack of definitive data showing that margin status independently predicts residual disease, it is preferred that women with CIN 2/3 and positive endocervical margins undergo cytologic and endocervical sampling four to six months after treatment, rather than immediate retreatment 11. If a decision is made to retreat, repeat excision or hysterectomy is acceptable 11.
Human papillomavirus DNA testing
Human papillomavirus (HPV) DNA testing appears to be more sensitive than colposcopy or cytology for detecting treatment failures for cervical intraepithelial neoplasia (CIN) 2/3 13. One systematic review showed a sensitivity of nearly 77% for cytology and nearly 91% for human papillomavirus (HPV) DNA testing 14. In another systematic review of women who had successful treatment, 84% had negative human papillomavirus (HPV) DNA testing following LEEP 15. Women who tested negative for human papillomavirus (HPV) had no recurrent disease during a two-year follow-up period 16.
According to the American Society for Colposcopy and Cervical Pathology 11 and the American College of Obstetricians and Gynecologists 17, human papillomavirus (HPV) DNA testing is an acceptable option for post-LEEP management of CIN 2/3. HPV DNA testing and cytology (co-testing) should be performed posttreatment at 12 and 24 months 11. If either test result is positive, colposcopy with endocervical sampling is recommended 11. Women who have negative co-testing results twice can repeat co-testing in three years and return to routine screening if results are negative 11. The risk of neoplastic invasion has been reported as late as two decades after treatment 18, 19. The American Society for Colposcopy and Cervical Pathology recommends a 20-year period of routine follow-up screening 11.
Cone biopsy
A cone biopsy is done less often than LEEP/LLETZ. A cone of tissue is cut away from your cervix to remove all the abnormal cells. In cone biopsy procedure the doctor removes a similar sized or slightly larger piece of the cervix than with a LEEP biopsy. There is not much variation in the size of a cone biopsy, so if only a small area needs removing it will probably be done using a LEEP. A cone biopsy allows for the cells at the edges of the specimen to be seen clearly through a microscope ensuring that all of the biopsy can be examined by a histopathologist (an expert in studying diseases by looking at cells).
A cone biopsy is usually carried out under a general anesthetic, which is where you are asleep (very few cone biopsies are performed under local anesthetic). A vaginal pack will sometimes be put in place in theater while you are under anesthetic. This is like a long bandage that puts pressure on the biopsy site and so helps stop any bleeding (a bit like putting pressure on a cut to stop it bleeding). It will be removed before you go home. Not all health gynae-oncologists use vaginal packs, so please discuss this with your medical team if you have any questions. It is advisable to have some painkillers at home (such as you would take for period pains) as some women experience a deep ache and/or tenderness in their pelvis. It is not unusual to feel tired for a few days or even a week or so following a general anesthetic.
A cone biopsy:
- is a minor operation to cut out a cone-shaped piece of tissue containing the abnormal cells
- only tends to be used if a large area of tissue needs to be removed
- can’t be done at the same time as a colposcopy
- is usually done under general anesthetic (where you’re asleep)
- may require an overnight stay in hospital
Cone biopsy side effects/complications
The side effects that you may have after a cone biopsy are very similar to those that you may have after a LEEP and include some bleeding and discharge for about three to four weeks. The amount and color of any bleeding/discharge, as well as when/if they begin will vary from woman to woman. The blood can be red or brown and it can vary in heaviness from light spotting to slightly heavier bleeding. Sometimes the discharge can be yellowy in color, and it can be heavy or watery. Some women find that their next monthly period comes slightly earlier than normal and it may be slightly heavier, which is thought to be caused by the increased blood supply around this area. The bleeding/discharge may begin straight after treatment or a few days to a week later.
These symptoms are very normal following a cone biopsy and in order to help avoid any possible infections it is recommended that you only use sanitary towels, and avoid tampons, sex and swimming, until any discharge has stopped and any bleeding has settled.
However, if you are having particularly heavy bleeding (e.g.,. your sanitary towels are soaking every hour) or discharge that smells really offensive and/or you feel unwell (either of which could be a sign of infection) you should contact a health care professional as soon as possible. This could be your colposcopy clinic or your doctor, or any other health care professional you feel comfortable talking to about this. There will be a specialist nurse in your colposcopy clinic who will be able to address any queries you have.
Straight wire excision of the transformation zone (SWETZ) or needlepoint excision of the transformation zone (NETZ)
Similar to a cone biopsy these procedures remove a piece of tissue but they use a straight wire or needle diathermy with electricity running through them to cut and seal the tissue, like a LEEP treatment. The procedures are done in a clinic with local anesthetic (like a LEEP) or under general anaesthetic (like a cone biopsy). These treatments are usually done if the abnormal cells are inside the cervical canal or if you have glandular abnormal cells.
Other treatments
Abnormal cells in the cervix can also be treated with:
- Cryotherapy – the abnormal cells are frozen and destroyed (this is only used to treat minor cell changes e.g. treat CIN1)
- Laser treatment – a laser is used to pinpoint and destroy abnormal cells on your cervix. If necessary, a laser can also be used to remove a small piece of the cervix itself. This is called laser excision or laser cone biopsy.
- Cold coagulation – despite the name of this treatment this procedure involves applying a hot probe to the cervix, which, like a laser, destroys the abnormal cells. This treatment can also be called thermocoagulation. A local anaesthetic is given before any of the treatments described above except for larger cone biopsies, which may require a general anesthetic.
- Hysterectomy (removal of the womb) – this will only be considered if abnormal cells on your cervix have been found more than once, if they’re severely abnormal, you’re past childbearing age, or you don’t want to have more children
Is laser treatment also used to remove abnormal cells from the cervix? Why is LEEP treatment now more popular?
Before the introduction of the LEEP treatment in the early 1990’s, laser treatment was the preferred method to remove pre-cancerous cells from the cervix. After confirming the presence of CIN with a small punch biopsy, a laser beam (high-energy light) was used to vaporise the abnormal area, or the laser beam was used to cut a cone of tissue out, similar to the LEEP procedure. Tissue healing after laser treatment was very good.
However, laser treatment has now largely been replaced by LEEP. The equipment for LEEP is much cheaper to buy, use and easier to maintain than laser generators; however, it is the safety aspects of sending the tissue of the transformation zone for pathological analysis after a LEEP procedure to ensure that a small, invasive cancer has not been missed which attracts gynaecologists to favour LEEP over small biopsies/lasers.
What side effects should I expect after a LEEP procedure?
You can usually expect some bleeding and discharge for about three to four weeks after treatment. In order to help avoid any possible infections it is recommended that you only use sanitary towels during this time, avoiding tampons and sex, until any bleeding and discharge has settled. Every woman’s experience is different, so the amount and color of any bleeding/discharge can vary a lot depending on how quickly the woman heals, the size of the area treated and treatment method used. Some women start to get bleeding or discharge from the day the treatment is performed and for other women this is very slight or absent during the first week or so.
After treatment, a soft healing scab forms on the cervix. Over time this slowly dissolves away, which is what often causes the discharge and some bleeding. This can vary a lot from woman to women. The bleeding experienced can be red or brown in color and it can vary in heaviness from light spotting to slightly heavier bleeding. Sometimes the discharge can be a yellowy color, and it can be heavy or watery. Some women find that their next monthly period comes slightly earlier than normal and it may be slightly heavier. This is thought to be caused by the increased blood supply around this area.
All of the above symptoms are very normal after a LEEP procedure. However, if the bleeding seems particularly heavy (e.g. your sanitary towels are soaking every hour) or if the discharge smells really offensive and/or you feel unwell (which could be a sign of infection) you should contact a health care professional.
After treatment
You can often go home to rest soon after the treatment is finished. Most women feel well enough to return to work and most normal activities the next day.
You’ll usually be advised to avoid:
- driving for at least 24 hours if you had a general anesthetic – you can drive straight away if a local anesthetic was used
- using tampons for four weeks (use sanitary pads instead)
- having sex for four weeks
- exercising, including swimming, for at least two weeks, or while there’s still any bleeding or discharge
You’ll also be advised to have another cervical screening test six months after treatment, to check for abnormal cells and the human papilloma virus (HPV).
If HPV isn’t found, you won’t need to be screened again for another three years. But if HPV or significant cell changes are found, you’ll be referred for another colposcopy.
It is extremely important that you attend your follow-up appointment as advised by your local service. Six months after your treatment you will be called back to have a repeat cervical screening test – this can be done at your doctor surgery or in a cervical screening clinic at the hospital where you had your treatment (your colposcopy department will advise you).
Approximately 18–20% of women will test positive for a high risk HPV infection after treatment, as it takes some women longer to clear HPV than others, but only between 5 and 15% of women continue to have cervical abnormalities after treatment. Occasionally second and third treatments are required. It is very important that you attend treatment if further treatment is advised 20.
Test of cure
In most parts of the US an HPV test is included as part of the screening test after treatment. This HPV test is referred to as a ‘test of cure’. These follow-up tests help to identify if the treatment has been successful, the abnormal cervical cells have been removed and the area is now back to normal.
Test of cure is available across all US countries. It uses HPV testing to identify if a woman has been successfully cured after treatment for abnormal cervical cells. It tests for high risk HPV, which can cause cervical cancer. Test of cure will only be given to women who have undergone treatment for cervical abnormalities. The test is used in combination with cervical screening cytology (looking at the cells under the microscope).
If high risk HPV is not found (negative test result) and your screening test comes back negative (that means the cells appear normal under the microscope), then you have been successfully treated by removing the abnormal cells and you will be returned to your regular screening schedules. You do not need to have another cervical screening test for three or five years depending on your age or upon your country’s screening programme. The HPV test helps to confirm that there is no longer a higher than average risk of developing further cervical abnormalities.
The test of cure will be done six months after the treatment for CGIN. If it is negative for high risk HPV and there are no abnormalities seen under the microscope (negative cytology) then the test of cure will be redone again in another 12 months (18 months after the treatment was done). If this test is negative for high risk HPV and cytology then you will be returned to your regular screening program.
If a high risk HPV infection is found for either CIN or CGIN (HPV positive), or the screening test shows an abnormality you will again be referred to colposcopy for further investigation. If this happens please try not to be alarmed, it is better to get things checked out. Occasionally cervical abnormalities are not fully removed at the first treatment. This is because the treatment needs to balance removing all of the area of abnormal cells as well as saving as much of the normal cervix as possible. This is important because the cervix plays a vital role in pregnancy. If there are still abnormal cells left at follow-up, further treatments can always be done to remove them.
Using both a cervical screening test and the HPV test of cure provides a more effective way of assessing the success of treatment than a cervical screening test alone would. Many women who come back to the colposcopy clinic do not need further treatment.
There is also a small chance that cervical abnormalities may come back in the future. It is therefore really important to keep going for your cervical screening when invited, so that you can have further treatment if necessary.
Remember if you have been found positive for abnormal cervical cells this is unlikely to be cervical cancer. Treatment for abnormal cervical cells is usually very effective and it is estimated that early detection and treatment can prevent up to 75% of cervical cancers from developing 21.
Treatment risks and side effects
Bleeding (at the time of treatment or in the two to three weeks afterwards) or infection (more often 10–14 days after) can occur after treatment for abnormal cells of the cervix. You may experience vaginal discharge or bleeding like the end of a period for two to three weeks after your treatment. However this does vary a lot, for example a few women will have no bleeding at all and some will be bleeding for up to six weeks. After your treatment you may feel some pain, this is because the local anaesthetic used during your treatment will wear off after two to three hours. This pain often feels like cramps that you can have during your period. Some women notice pain more the day after the treatment. Sometimes periods can be irregular or more painful for two to three months after treatment. Always contact your GP or colposcopist if you are experiencing any problems after treatment. There is no reason to put up with discomfort that can easily be treated.
If you are working you might be advised to take a day or two off from work (your colposcopist will let you know if this is necessary). You might need some pain relief after your treatment, the clinic where you had treatment can advise you on this.
Generally, a single, straightforward treatment to the cervix is very unlikely to adversely affect your fertility or your ability to have a normal pregnancy.
In most women, one treatment is enough to completely treat their cervical abnormalites. But between 5 and 15% of women will still be affected by CIN or CGIN after their first treatment.
Common side effects of treatment include:
- mild pain, similar to period pain – this should pass in a few hours and can be relieved with paracetamol or ibuprofen
- light vaginal bleeding and brown, watery vaginal discharge – this may last up to four weeks
There’s also a small risk of more serious complications, such as:
- an infection – this can cause heavy or persistent bleeding, smelly vaginal discharge and persistent tummy pain; see your doctor if you have these symptoms
- a slightly increased risk of premature birth (before the 37th week of pregnancy) in future pregnancies – this is more likely if you need repeated treatments or a lot of tissue needs to be removed
In most cases, the benefit of treatment will outweigh these risks. Talk to your doctor or nurse if you have any concerns or would like to know more about the potential risks of treatment.
References- Safaeian M et al., 2008. Determinants of incidence and clearance of high-risk HPV infections in rural Rakai, Uganda. Cancer Epidemiology, Biomarkers & Prevention 17 (6), 1300–1307.
- Soutter WP et al., 1997. Invasive cervical cancer after conservative therapy for cervical intraepithelial neoplasia. The Lancet 349(9057), 978–998.
- Soutter WP et al., 2006. Long-term risk of invasive cervical cancer after treatment of squamous cervical intraepithelial neoplasia. International Journal of Cancer 118(8), 2048–2055.
- TOMBOLA Group, 2009. Biopsy and selective recall compared with immediate large loop excision in management of women with low grade abnormal cervical cytology referred for colposcopy: multicentre randomised controlled trial. British Medical Journal 339, b2548.
- Kyrgiou M, Koliopoulos G, Martin-Hirsch P, Arbyn M, Prendiville W, Paraskevaidis E. Obstetric outcomes after conservative treatment for intraepithelial or early invasive cervical lesions: systematic review and meta-analysis. Lancet. 2006;367(9509):489–498.
- Arbyn M, Kyrgiou M, Simoens C, et al. Perinatal mortality and other severe adverse pregnancy outcomes associated with treatment of cervical intraepithelial neoplasia: meta-analysis. BMJ. 2008;337:a1284.
- Bevis KS, Biggio JR. Cervical conization and the risk of preterm delivery. Am J Obstet Gynecol. 2011;205(1):19–27.
- Castanon A et al., 2012. Risk of preterm birth after treatment for cervical intraepithelial neoplasia among women attending colposcopy in England: retrospective-prospective cohort study. British Medical Journal 345, e5174.
- Castanon A et al, 2014. Risk of preterm delivery with increasing depth of excision for cervical intraepithelial neoplasia in England: nested case-control study. British Medical Journal 349, g6223.
- Ghaem-Maghami S, Sagi S, Majeed G, Soutter WP. Incomplete excision of cervical intraepithelial neoplasia and risk of treatment failure: a meta-analysis. Lancet Oncol. 2007;8(11):985–993.
- Massad LS, Einstein MH, Huh WK, et al.; 2012 ASCCP Consensus Guidelines Conference. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis. 2013;17(5 suppl 1):S1–S27.
- Paraskevaidis E, Lolis ED, Koliopoulos G, Alamanos Y, Fotiou S, Kitchener HC. Cervical intraepithelial neoplasia outcomes after large loop excision with clear margins. Obstet Gynecol. 2000;95(6 pt 1):828–831.
- Arbyn M, Paraskevaidis E, Martin-Hirsch P, Prendiville W, Dillner J. Clinical utility of HPV-DNA detection: triage of minor cervical lesions, follow-up of women treated for high-grade CIN: an update of pooled evidence. Gynecol Oncol. 2005;99(3 suppl 1):S7–S11.
- Chan BK, Melnikow J, Slee CA, Arellanes R, Sawaya GF. Posttreatment human papillomavirus testing for recurrent cervical intraepithelial neoplasia: a systematic review. Am J Obstet Gynecol. 2009;200(4):422. e1–e9.
- Paraskevaidis E, Arbyn M, Sotiriadis A, et al. The role of HPV DNA testing in the follow-up period after treatment for CIN: a systematic review of the literature. Cancer Treat Rev. 2004;30(2):205–211.
- Kreimer AR, Guido RS, Solomon D, et al. Human papillomavirus testing following loop electrosurgical excision procedure identifies women at risk for posttreatment cervical intraepithelial neoplasia grade 2 or 3 disease. Cancer Epidemiol Biomarkers Prev. 2006;15(5):908–914.
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin number 66, September 2005. Management of abnormal cervical cytology and histology. Obstet Gynecol. 2005;106(3):645–664.
- Soutter WP, Sasieni P, Panoskaltsis T. Long-term risk of invasive cervical cancer after treatment of squamous cervical intraepithelial neoplasia. Int J Cancer. 2006;118(8):2048–2055.
- Kalliala I, Anttila A, Pukkala E, Nieminen P. Risk of cervical and other cancers after treatment of cervical intraepithelial neoplasia: retrospective cohort study. BMJ. 2005;331(7526):1183–1185.
- Kitchener HC et al., 2008. HPV testing as an adjunct to cytology in the follow-up of women treated for cervical intraepithelial neoplasia. BJOG: An International Journal of Obstetrics & Gynaecology 115(8), 1001–1007.
- Peto et al., 2004. The cervical cancer epidemic that screening has prevented in the UK. Lancet 35, 249–256.