What is a CSF leak
A CSF leak is an escape of the cerebrospinal fluid (CSF) that surrounds your brain and spinal cord. CSF leaks have been traditionally classified as traumatic or non-traumatic 1. Non-traumatic CSF leak may be spontaneous in the absence of obvious cause, such as skull base abnormalities or bone erosion related to tumors or hydrocephalus 2. Spontaneous CSF leaks are sometimes referred to as high-pressure leaks when increased intracranial pressure contributes to the development of the CSF leak 2. Idiopathic intracranial hypertension is increasingly recognized as a cause of spontaneous CSF leak in the ear nose and throat and neurosurgical literature 3. Over the past 20 years, a few authors have suggested that so-called “primary spontaneous CSF leaks” might represent a form of idiopathic intracranial hypertension 2. As the obesity epidemic grows in the United States, rhinorrhea and otorrhea from spontaneous CSF leaks secondary to untreated idiopathic intracranial hypertension are increasing in prevalence 4. Some of these patients are asymptomatic or only have symptoms attributable to the CSF leak (such as fluid from the nose (rhinorrhea), fluid from the ear (otorrhea), CSF hypotension-related headaches, or bacterial meningitis) while the leak is active 5. Cerebrospinal fluid (CSF) from the nose (rhinorrhea) is a known entity resulting from congenital malformations, postinfectious hydrocephalus, and skull base erosion from intracranial tumors 6.
See your doctor if:
- You have a headache that gets worse when you sit up, especially if you have recently had a head injury, surgery, or childbirth involving epidural anesthesia.
- You have a moderate head injury, and then develop a headache that is worse when you sit up, or you have a thin, clear fluid draining from your nose or ear.
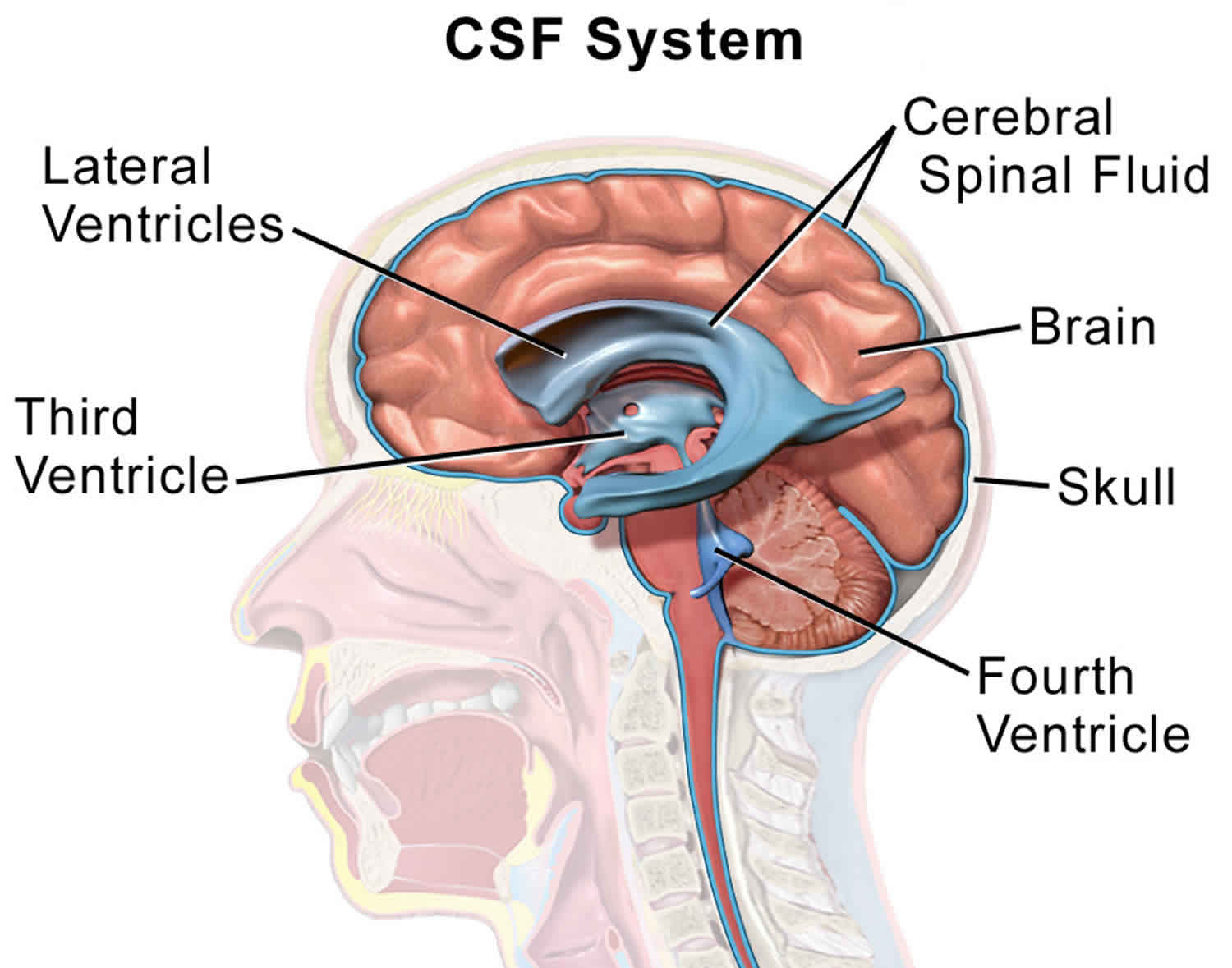
What is cerebrospinal fluid
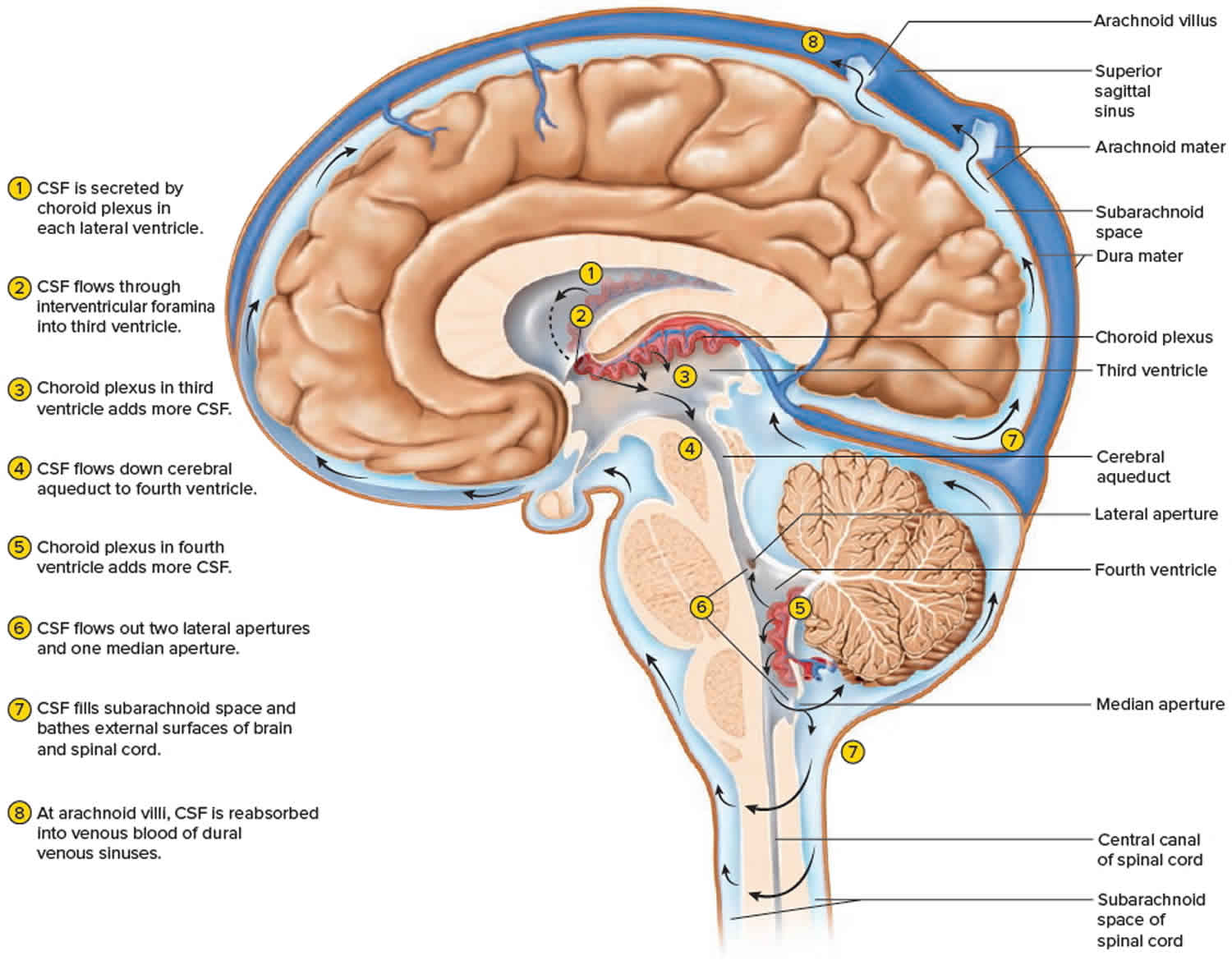
Cerebrospinal fluid is a clear, colorless liquid that fills the ventricles and canals of the brain and spinal cord (central nervous system) and bathes its external surface. The brain produces about 500 mL of cerebrospinal fluid per day, but the fluid is constantly reabsorbed at the same rate and only 100 to 160 mL is normally present at one time. About 40% of it is formed in the subarachnoid space external to the brain, 30% by the general ependymal lining of the brain ventricles, and 30% by the choroid plexuses. Cerebrospinal fluid production begins with the filtration of blood plasma through the capillaries of the brain. Ependymal cells modify the filtrate as it passes through them, so the cerebrospinal fluid has more sodium chloride than blood plasma, but less potassium, calcium, and glucose and very little protein.
Cerebrospinal fluid serves three functions for the brain:
- Buoyancy. Because the brain and cerebrospinal fluid are similar in density, the brain neither sinks nor floats in the cerebrospinal fluid. It hangs from delicate specialized fibroblasts of the arachnoid meninx. A human brain removed from the body weighs about 1.5 kg, but when suspended in cerebrospinal fluid its effective weight is only about 50 g. This buoyancy allows the brain to attain considerable size without being impaired by its own weight. If the brain rested heavily on the floor of the cranium, the pressure would kill the nervous tissue.
- Protection. Cerebrospinal fluid also protects the brain from striking the cranium when the head is jolted. If the jolt is severe, however, the brain still may strike the inside of the cranium or suffer shearing injury from contact with the angular surfaces of the cranial floor. This is one of the common findings in head injuries (concussions) from contact sports like NFL, rugby and boxing.
- Chemical stability. Cerebrospinal fluid rinses metabolic wastes from the nervous tissue and regulates its chemical environment. Slight changes in cerebrospinal fluid composition can cause malfunctions of the nervous system. For example, a high glycine concentration disrupts the control of body temperature and blood pressure, and a high pH causes dizziness and fainting.
Cerebrospinal fluid continually flows through and around the brain and spinal cord, driven partly by its own pressure, partly by the beating of ependymal cilia, and partly by rhythmic pulsations of the brain produced by each heartbeat. The cerebrospinal fluid of the lateral ventricles flows through the interventricular foramina into the third ventricle, then down the cerebral aqueduct to the fourth ventricle. The third and fourth ventricles and their choroid plexuses add more cerebrospinal fluid along the way. A small amount of cerebrospinal fluid fills the central canal of the spinal cord, but ultimately, all of it escapes through three pores in the fourth ventricle—a median aperture and two lateral apertures. These lead into the subarachnoid space on the brain and spinal cord surface. From here, cerebrospinal fluid is reabsorbed by arachnoid granulations, extensions of the arachnoid meninx shaped like little sprigs of cauliflower, protruding through the dura mater into the superior sagittal sinus. Cerebrospinal fluid penetrates the walls of the granulations and mixes with blood in the sinus.
Figure 1. Cerebrospinal fluid formation, absorption and circulation around and within the brain
CSF leak causes
Any tear or hole in the membrane that surrounds the brain and spinal cord (dura) can allow the fluid that surrounds those organs to leak. When it leaks out, the pressure around the brain and spinal cord drops.
Causes of CSF leakage through the dura include:
- Certain head, brain, or spinal surgeries
- Head injury
- Placement of tubes for epidural anesthesia or pain medicines
- Spinal tap (lumbar puncture)
Blunt trauma is the most common cause. Traumatic CSF leak is reported in approximately 10-30% of skull base fractures in adults. More than half of these present within 48 hours. The most common fracture sites leading to CSF leaks are the frontal sinus (30.8%), sphenoid sinus (11.4–30.8%), ethmoid (15.4–19.1%), cribriform plate (7.7%), frontoethmoid (7.7%), and sphenoethmoid (7.7%) 7.
Sometimes, no cause can be found. This is called a spontaneous CSF leak. Spontaneous CSF leaks, where the onset of symptoms comes out of the blue, were once considered rare, but are now known to be far more prevalent than first thought. Such CSF leaks are increasingly attributed to an underlying congenital disorder, such as Ehlers-Danlos Syndrome and other connective tissue diseases.
CSF leak symptoms
CSF leak symptoms may include:
- A headache that is worse when you sit up and improves when you lie down. It may be associated with light sensitivity, nausea, and neck stiffness.
- Drainage of CSF from the ear (rarely).
- Drainage of CSF from the nose (rarely).
Cerebrospinal fluid (CSF) from the ear (otorrhea) is the leakage of cerebrospinal fluid (CSF) though the ear. It is a rare but very serious condition that requires rapid intervention. Symptoms include leak of clear fluid through the ear, inflammation of the membranes that cover the brain (meningitis), hearing loss, and seizures.
CSF leak possible complications
CSF leak complications may occur if the cause of the CSF leak is due surgery or trauma. Infections after surgery or trauma can lead to meningitis and serious complications, such as swelling of the brain, and need to be treated right away.
CSF leak diagnosis
Where a CSF leak is suspected as a result of symptoms, establishing the location of the leak is generally the next step. While success can be had with some spontaneous spinal CSF leaks through high-volume blind blood patches without knowing the location of the leak (the success rate is thought to be around 40%), in many cases establishing precise location of the hole or tear can be critical to proper management and enables more directed treatment.
Your health care provider will perform a physical exam and ask about your symptoms. Tests may include:
- CT scan of the head with contrast dye
- CT myelogram of the spine
- MRI of the head or spine
- Radioisotope test of the CSF to track the leakage
- Beta-2-transferrin is a protein which is almost exclusively found in the cerebrospinal fluid. It is not found in blood, mucus or tears, which makes it a specific marker of cerebrospinal fluid. While cerebrospinal fluid from spinal leaks disperses within the body and cannot therefore be collected and tested, Beta-2-transferrin testing can be a successful, non-evasive test for confirming the presence of cranial CSF leaks. Where CSF is leaking significantly, it may be possible to collect it in a specimen bottle, however, in many cases, pledgets (small wads of absorbent material) are inserted into the nose and ears.
CSF leak tests
Nasal Endoscopy
Where a traumatic cranial CSF leak is suspected, nasal endoscopy is often performed. This procedure may narrow down the side/site of the leak and may occasionally identify active leaks, but findings are often non-specific. Signs of a leak can include glistening nasal mucosa. Although direct visualisation through endoscopy plays an important role in identifying cranial leak sites, imaging (particularly CT) of the skull base is critical to localisation, particularly traumatic leaks.
High-Resolution Computed Tomographic (CT) Scan
Multiple imaging studies have been used to localise cranial defects which can cause cranial leaks, but the most common is technique is high-resolution Computed Tomographic (HRCT) scanning. A HRCT scan uses 1- to 2-mm sections in both the coronal and axial planes with bone algorithm, resulting in localisation of the majority of skull base defects that can result in CSF leak.
HRCT technology can be used with most surgical image guidance systems. Due to the relative ease of obtaining this study and high degree of accuracy, this method is often used as the primary imaging modality for traumatic cranial CSF leaks. Plain CT scans may lead to false-positive results secondary to volume averaging, and their use is generally be limited. The use of intrathecal fluorescein in combination with HRCT allows for the identification of most cranial CSF leaks.
It is important to note that congenital or acquired thinning or absence of portions of the bony skull base may be identified and may not necessarily correspond to the site of CSF leak. HRCT scans may only have limited use in identifying CSF leaks located in the spinal region.
Computed Tomographic (CT) Myelography
CT Myelography, sometimes called CT Cisternography, involves the intrathecal administration (lumbar puncture) of radiopaque contrast (metrizamide, iohexol, or iopamidol) followed by CT scanning.
Studies have shown that approximately 80% of CSF leaks can be confirmed through this technology. Weaknesses include its invasive nature, which can limit its use particularly with young children, as well as its low sensitivity in small, intermittent or ‘slow’ leaks.
Positive findings usually reveal pooling of contrast in the frontal or sphenoid sinuses or outwith the dura mater, but may not necessarily locate the actual hole or tear.
Magnetic Resonance Imaging
Magnetic Resonance Imaging (MRI) is generally thought to be less effective than CT Myelography or MR Myelography at detecting the specific site of CSF leak, unless it stems from a sizable tear, but it does have a use in the diagnosis of Intracranial Hypotension through the disclosure of pockets of CSF outwith the dura, secondary conditions and symptoms.
While the symptoms of those diagnosed with Intracranial Hypotension worsen in the vertical position, studies have shown that MRI scans undertaken with patients sitting upright or standing generally show no discernable difference to those undertaken lying down[i]. MRI with fat suppression sequences is increasingly regarded as being the most appropriate MRI type for successfully disclosing CSF pockets outwith the dura.
MRI studies may show pachymeningeal enhancement (when the dura mater looks thick and inflamed) and the downward displacement of the cerebellar tonsils through the foramen magnum (known as an ‘Arnold-Chiari’ or simply ‘Chiari’ malformation) due to the decreased volume and buoyancy of CSF in which the brain floats. This is present in many, but not all, cases[ii].
Standard MRI scans may also show the engorgement of the cerebral dural venous sinuses, the cerebral ventricles may be reduced in size and the pituitary gland may appear enlarged. There may be apparent downward displacement of the optic chiasm and the upper cervical epidural veins may appear congested.
Spinal MRI scans for patients with a suspected CSF leak may show some irregularity of the thecal sac due to partial dural collapse. Extradural fluid collections are common in spinal cerebrospinal fluid (CSF) leak. Intense extradural contrast enhancement may be noted in congested epidural veins. One or more CSF fistulas may originate from spinal nerve root sleeves in the case of spontaneous spinal CSF leak.
A new MRI technique, using intrathecal gadolinium contrast, is becoming more common, although is still relatively uncommon in the UK. Introducing contrast into the CSF can increase the likelihood of an MRI scan disclosing the location of a leak, particularly if administered with a solution such as Elliot’s B to raise intracranial pressure. As is the case with CT Myelography and Radionuclide Cisternography, the procedure is considered fairly safe, but there are risks whenever foreign bodies are introduced into the cerebrospinal fluid.
It is important to note, however, that standard MRI imaging can present as completely normal and, for some doctors, are not the study of choice[iii] for the detection of a leak site. MRI imaging presenting as normal does not mean that a CSF leak is not present and that Intracranial Hypotension is not the correct diagnosis.
MR Myelography
Magnetic Resonance (MR) Myelography, sometimes called MR Cisternography, is a study of the spinal canal and subarachnoid space using high-resolution Magnetic Resonance Imaging (MRI) that has been shown[iv] to be accurate in localising CSF leaks for patients with spontaneous intracranial hypotension (SIH).
MR Myelography comprises a special MRI technique in which a sequence with heavy T2-weighting is used to provide high contrast between the ‘dark’ spinal cord and its nerves and the surrounding ‘bright’ cerebrospinal fluid, mimicking the results of Computed Tomographic (CT) Myelography. Fat suppression technology is normally used.
Studies have demonstrated[v] that heavily weighted MR Myelography can successfully detect abnormal cerebrospinal fluid (CSF) collections and CSF leakages, such as C1-2 extra-spinal collections, CSF along nerve root sleeves, and epidural fluid collections, with only with minor discrepancies compared with CT Myelography studies.
This is normally a non-invasive, non-contrasted and time-saving technique and is often considered as an alternative to invasive CT Myelography, before embarking on targeted epidural blood patches. However, intrathecal gadolinium can also be administered and can increase the likelihood of leak detection.
MR Myelography is proving to be a promising study for patients with SIH, with some studies suggesting sensitivity in the region of 85% to 92% in relation to cranial leaks, with 100% specificity, albeit lower for spinal leaks, but further large-scale validation studies are needed.
Digital Subtraction Myelography
Digital Subtraction Myelogram (DSM) is similar to CT myelogram and uses intrathecal contrast, however is performed under fluoroscopy. It also utilises the ability to digitally subtract a pre-contrast image in order to enhance the visibility of the contrast.
In a medical study carried out in 2012, featured in the American Journal of Roentgenology, eleven patients underwent digital subtraction myelography. All of the patients had previously undone MRI imaging which showed extradural fluid collection on average up to a length of 15.5 vertebral levels.
Digital subtraction myelography was used to successful locate the site of the CSF leak in nine of the 11 patients, and all of the dural tears disclosed were located in the thoracic spine between T3 and T11.
Digital subtraction myelography has been shown to be a valuable diagnostic tool for the localisation of rapid spinal CSF leaks and is increasingly considered in patients who are clinically suspected to have a dural tear that is accompanied by a longitudinally extensive extradural fluid collection on spinal MRI.
Radionuclide Cisternography
A variety of radioactive markers have been used with relatively good effect to detect CSF leaks, including radioactive iodine (131I)-labeled serum albumin, technetium (99mTc)-labeled serum albumin or diethylenetriamine penta-acetic acid (DTPA), and radioactive indium (111In)-labeled DTPA.
This technique is similar to intrathecal fluorescein and involves administration of the tracer via a lumbar puncture. Intranasal pledgets are normally placed in defined locations under endoscopic guidance and analysed for tracer uptake approximately 12 to 24 hours later. A scintillation camera is also used, but has poor resolution and difficulty precisely localising the leak.
Overpressure radionuclide cisternography increases the intrathecal pressure with a constant infusion to improve the sensitivity of radionuclide cisternography; however, this technique is not common place in the UK and through use in the USA has been shown to result in a high degree of false-positive findings, with sensitivities from 62% to 76%.
Intrathecal Fluorescein
Intrathecal agents can be used both to confirm the presence of, and to attempt to localise, CSF leaks. The agent is administered via lumbar puncture into the subarachnoid space (within which the cerebrospinal fluid circulates) and, as such, there are associated risks and complications can be serious.
Visible dyes, radiopaque dyes, and radioactive markers have been used with a positive results. Intrathecal fluorescein is currently the most common visible agent. Intrathecal fluorescein has been associated with multiple complications, including grand mal seizures and even death. However, in a study of 420 administrations low-dose (50 mg or less), intrathecal fluorescein was found to be useful in localising CSF fistulas and was deemed unlikely to be associated with adverse events, as most complications were dose-related.
The current recommended dilution is 0.1 mL of 10% intravenous fluorescein (not ophthalmic preparation) in 10 mL of the patient’s own CSF, which is infused slowly over 30 minutes. Patients should be extensively appraised of the risks by their doctor, as this use may be “off-label use”.
CSF leak treatment
Treatment for a CSF leak depends on the type and location of any hole or tear, as well as the underlying cause. Depending on the cause of the CSF leak, many symptoms improve on their own after a few days. Complete bed rest for several days is usually recommended. Drinking more fluids, especially drinks with caffeine, can help slow or stop the leak and may help with headache pain.
Some common treatments for a CSF leak include:
Conservative
- Bed rest
- Hydration (2-3 litres per day)
- IV Caffeine infusions
- Strong coffee or caffeine tablets
Headache may be treated with pain relievers and fluids. If the headache lasts longer than a week after a lumbar puncture, a procedure may be done to block the hole that may be leaking CSF fluid. This is called a blood patch, because a blood clot can be used to seal the leak. In most cases, this makes symptoms go away. In rare cases, surgery is needed to repair the tear in the dura and stop the headache.
If symptoms of infection (fever, chills, change in mental status) are present, they need to be treated with antibiotics.
Invasive treatment
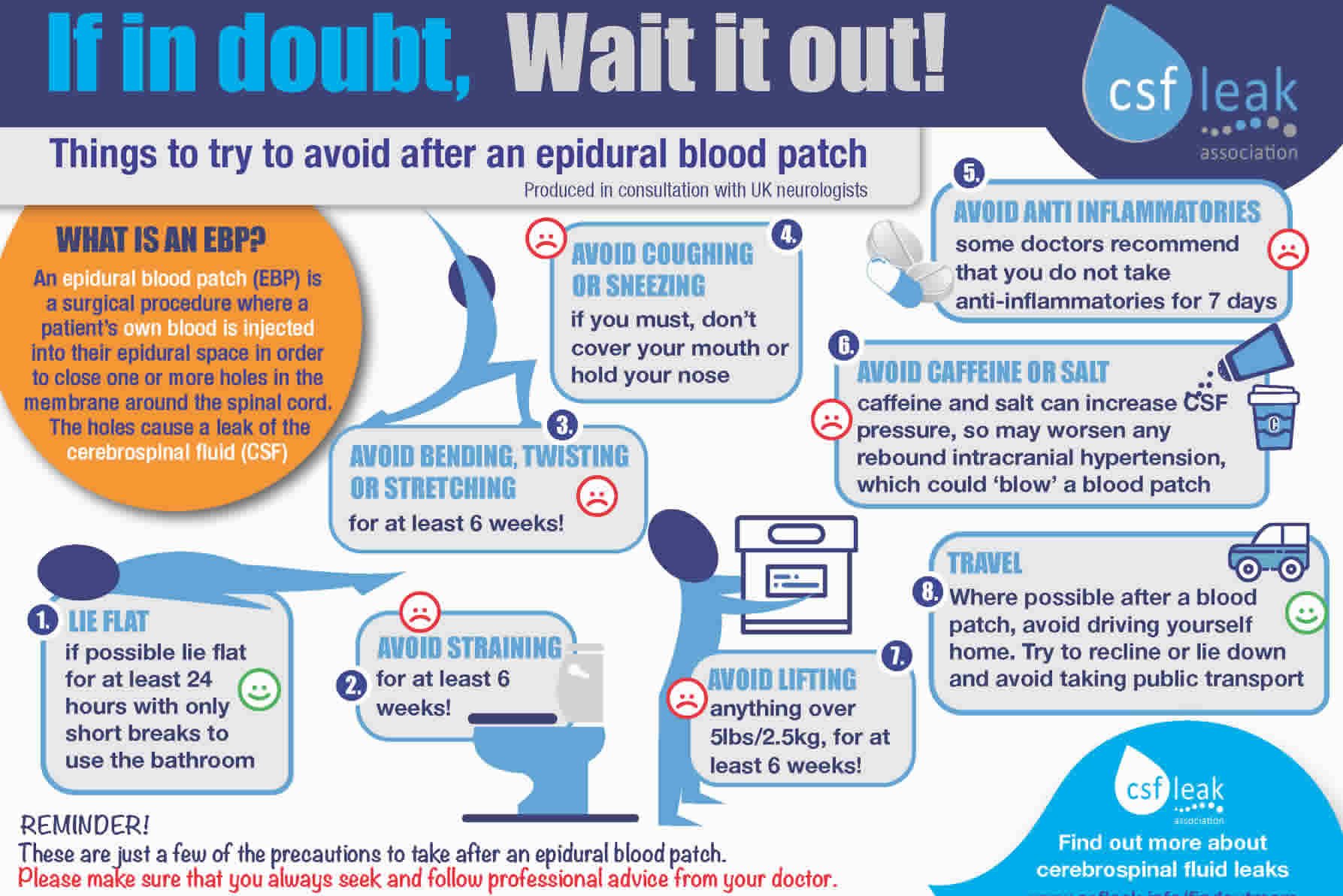
An epidural blood patch, where blood is drawn from the patient and immediately injected into the epidural space, is the most common invasive treatment for spinal leaks. Where the leak site is known, blood will be injected as close to it as possible. Where the leak site is not known, a high volume blood patch (typically 20ml) is injected into the lumbar spine (less commonly, the thoracic spine). Blood patches are generally thought to be relatively safe, but occasional reports of increased CSF pressure, persistent epidural fluid collections, nerve damage and infection have been reported.
Fibrin glue can be applied in much the same way as a blood patch to seal a known spinal CSF leak site. Fibrin glue is often used where a blood patch repeatedly fails. Occasionally, glue may be mixed with blood and injected as a combination patch, and this is sometimes used where the precise leak site is not known, but a relatively small area of the spine is suspected.
A surgical repair may be performed where a patient fails to respond to a blood patch or a blood patch fails, if the site of the leak has been identified. Surgical repairs can include suturing, the application of artificial dura patches and the use of aneurism clips. If the site is not known, but an area is suspect, exploratory surgery may sometimes be possible, with any discovered leak being repaired as above. Cranial leaks tend to require surgery as there a few less invasive treatment options.
General Precautions
If you have had a CSF leak and it has resolved on its own, or you’ve had a leak that required medical intervention, you must always seek advice from you doctor as to what post-leak or post-treatment precautions should be taken. However, sensible precautions to take in the aftermath of any of these circumstances may include:
- Avoiding bending, twisting, stretching and straining
- Avoiding lifting anything heavy (nothing over 2.5kg/5lbs)
- Avoiding coughing or sneezing with you nose/mouth closed
- Avoiding straining on the toilet, blowing up balloons or playing brass/wind instruments
- Avoiding/reducing things that may elevate the volume or pressure of the fluid around the brain, such as caffeine or salt (sodium)
- Avoiding walking on soft sand or snow
The timescale for sticking to these precautions should be determined by your doctor.
Post-Blood Patch Precautions
The most common intervention to resolve a spinal CSF leak that hasn’t resolved on its own is a blood patch.
It is important to note that there are no absolute right or wrongs when it comes to what you should/should not do following a blood patch, nor how long precautions should last. Guidance must always be sought from the doctor(s) responsible for your care.
Long term side effects of csf leak
Long term side effects of CSF leak is usually good depending on the cause. Most CSF leaking cases heal by themselves with no lasting symptoms.
If the CSF leak keeps coming back, high pressure of the CSF (intracranial hypertension) might be the cause and should be treated.
Rebound Intracranial Hypertension
Rebound intracranial hypertension (sometimes called ‘rebound high pressure’) can be a complication of epidural blood patching or surgery performed to resolve a CSF leak. It is characterized by increased intracranial pressure, resulting in potentially severe headache, nausea, and vomiting.
As a condition, it has only relatively recently begun to be recognized by doctors, however there are now a number of good medical papers documenting its existence and discussing ways to manage it. It is still not uncommon, however, for many neurologists and other specialists to be unaware of its existence.
References- Clark D, Bullock P, Hui T, et al. Benign intracranial hypertension: a cause of CSF rhinorrhoea. J Neurol Neurosurg Psych. 1994;57:847–849
- Yang Z, Wang B, Wang C, et al. Primary spontaneous cerebrospinal fluid rhinorrhea: a symptom of idiopathic intracranial hypertension? J Neurosurg. 2011;115:165–170
- Brainard L, Chen DA, Aziz KM, et al. Association of benign intracranial hypertension and spontaneous encephalocele with cerebrospinal fluid leak. Otol & Neurotol. 2012;33:1621–1624.
- Imaging of Cerebrospinal Fluid Rhinorrhea and Otorrhea. Reddy M, Baugnon K. Radiol Clin North Am. 2017 Jan;55(1):167-187. doi: 10.1016/j.rcl.2016.08.005. https://www.ncbi.nlm.nih.gov/pubmed/27890184
- Pérez MA, Bialer OY, Bruce BB, Newman NJ, Biousse V. Primary spontaneous cerebrospinal fluid leaks and idiopathic intracranial hypertension. J Neuroophthalmol. 2013;33(4):330-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4040082/
- Wang EW, Vandergrift WA, III, Schlosser RJ. Spontaneous CSF leaks. Otolaryngol Clin North Am 44:845–856, vii, 2011
- Oh JW, Kim SH, Whang K. Traumatic Cerebrospinal Fluid Leak: Diagnosis and Management. Korean J Neurotrauma. 2017 Oct. 13 (2):63-67.