Cuboid syndrome
Cuboid syndrome is a cause of lateral midoot pain, believed to result from abnormal articulation of the cuboid with the calcaneus (calcaneocuboid joint) 1. Cuboid syndrome presents with lateral foot pain and swelling, often diffuse and similar to an ankle (ligament) sprain 2. Pain is often aggravated by weightbearing and side-to-side movements 1.
Cuboid syndrome often presents with swelling, lateral proximal foot pain, and antalgic gait 3. There are no reliable imaging modalities for identifying cuboid syndrome, and diagnosis is often made on the basis of history, mechanism of injury, and clinical examination.
Cuboid syndrome has been reported as difficult to recognize and is often misdiagnosed or improperly managed 4. According to several authors, cuboid syndrome may result from a plantar flexion/inversion ankle sprain and may be a source of pain 5. It is reported that up to 4% of all athletes with foot problems present with a cuboid syndrome 6. It appears that the occurrence of cuboid syndrome in professional ballet dancers may be higher, accounting for up to 17% of reported foot and ankle injuries in this population 4.
Midtarsal adduction (stressing the midtarsal joint by superior-inferior manipulation of the midfoot against a stabilized hindfoot) and supination tests (inversion and plantar flexion of midfoot against stabilized hindfoot) tend to reproduce the symptoms 1.
Currently, there are no definitive diagnostic tests for cuboid syndrome. Case reports suggest that cuboid syndrome often responds favorably to manipulation and/or external support 1.
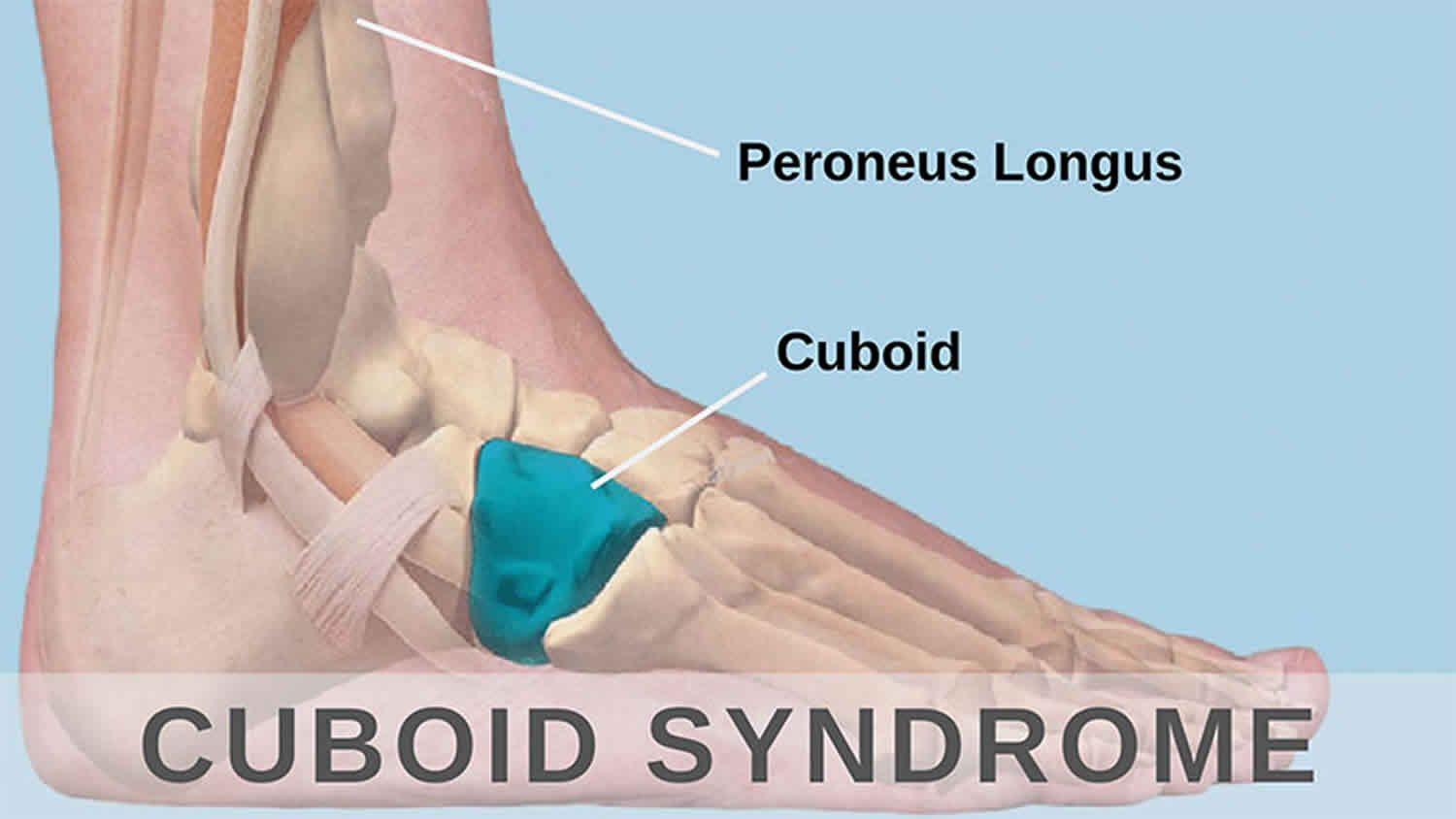
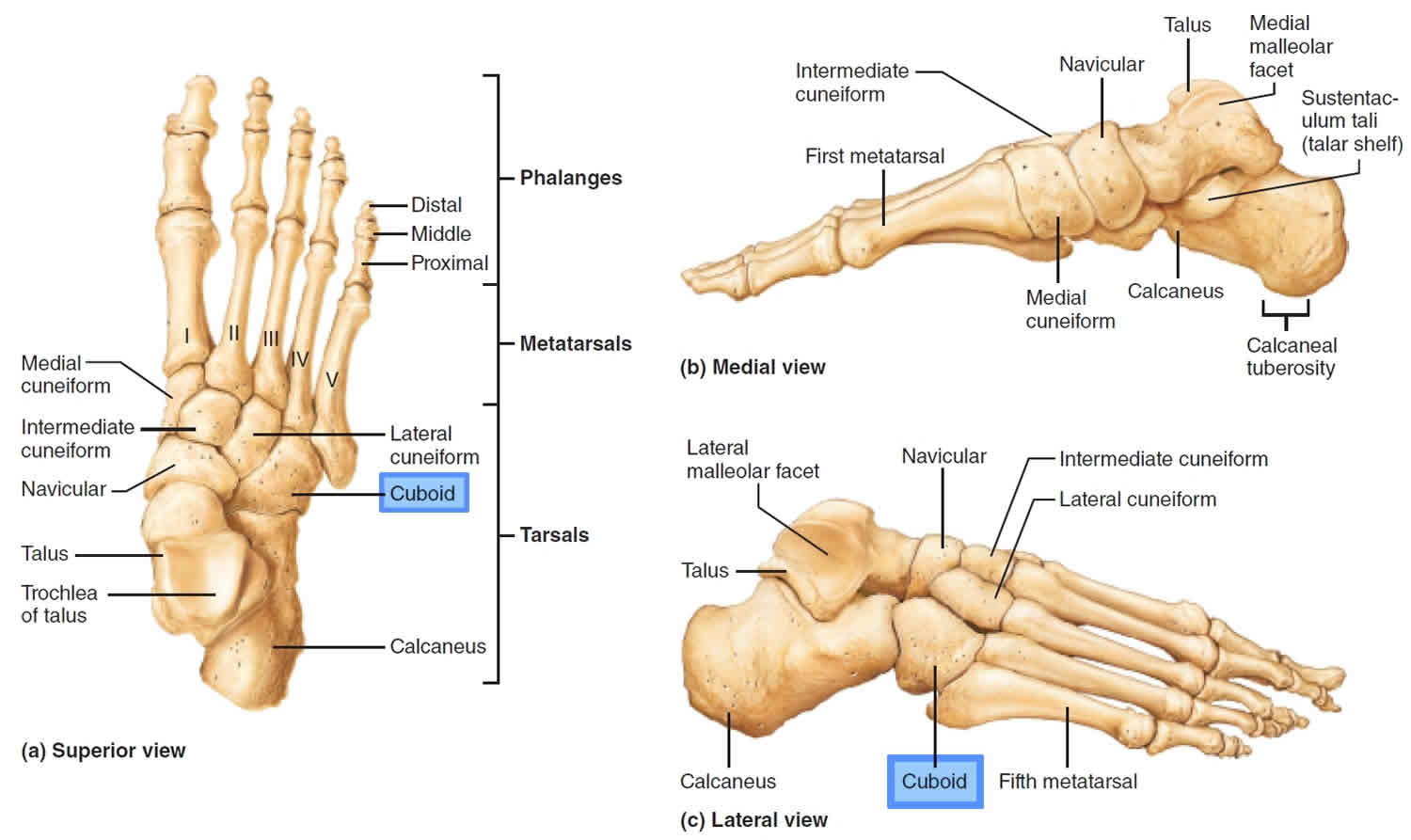
Cuboid anatomy
The cuboid bone (Greek for “cube” bone) is located in the lateral midfoot, articulates posteriorly with the calcaneus, the fourth and fifth metatarsals anteriorly, and the navicular and lateral cuneiform medially, the tendon of the fibularis longus muscle lies in a prominent groove on the anterior plantar surface, which passes obliquely forward across the bone from lateral to medial.
Figure 1. Cuboid bone
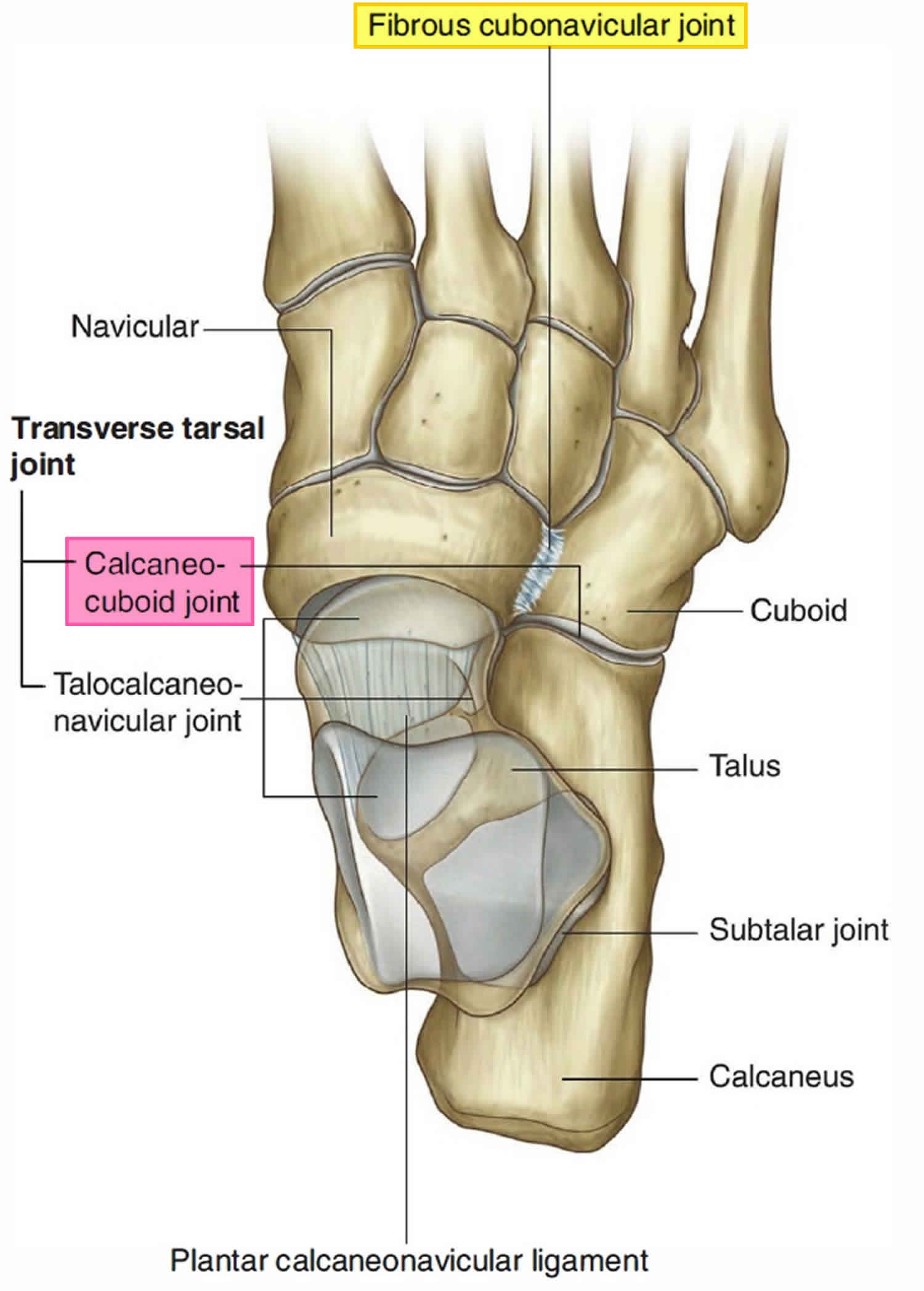
Figure 2. Calcaneocuboid joint
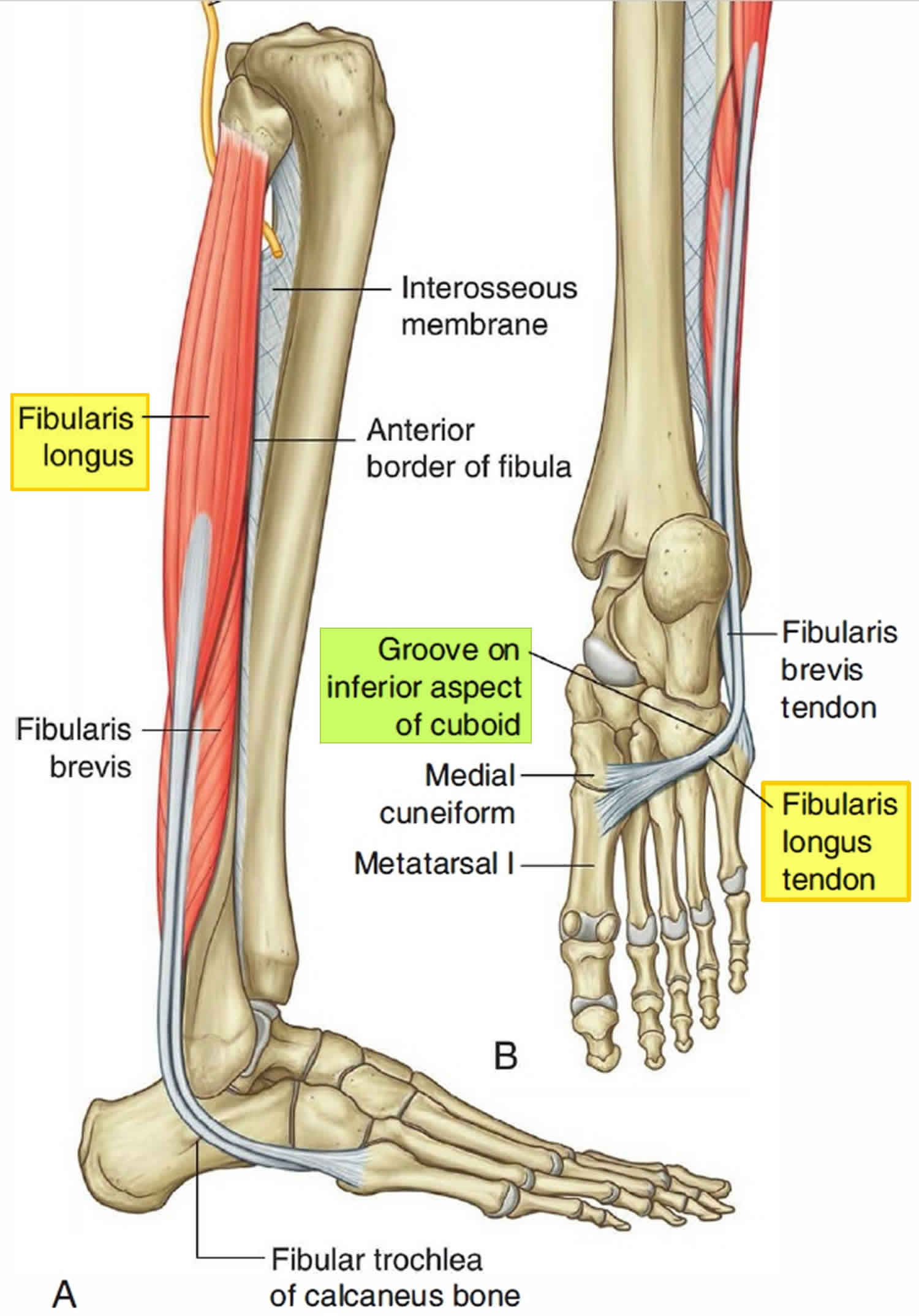
Figure 3. Peroneus longus tendon (fibularis longus tendon)
Calcaneocuboid joint function is dependent on midtarsal joint mechanics, since the navicular and cuboid bones move essentially in tandem during gait 7. The mechanics of the calcaneocuboid joint are highly variable 8. The principal movement at the calcaneocuboid joint is medial/lateral rotation about an anterior/posterior axis with the calcaneal process acting as a pivot 9. The rotation has been described as pronation/supination and obvolution/involution 9. Inversion/eversion is used herein.
The cuboid rotates as much as 25° during inversion/eversion about an axis that passes from posteroinferior to anterosuperior at an angle of roughly 52° (range, 43°-72°) with respect to the ground 9. In addition to inversion/eversion, there is some evidence that posterior-anterior distraction of the calcaneocuboid joint also occurs during the gait cycle 9.
The calcaneocuboid joint is intrinsically stable due to the congruence of its articular surfaces and reinforcement from ligaments and tendon attachments (Figure 2) 10. The calcaneocuboid joint appears to be maximally congruent radiographically when the calcaneus is placed in a vertical position 11. The dorsal and plantar cuboideonavicular and cuboideometatarsal ligaments and wedge-shaped fibroadipose labra within the calcaneocuboid joint and cuboid-metatarsal joints contribute to stability 12.
The peroneus longus tendon also known as fibularis longus tendon, which forms a sling around the lateral and plantar aspects of the cuboid before inserting on the plantar aspect of the lateral first metatarsal base and medial cuneiform, also assists with calcaneocuboid joint stabilization (Figure 3) 13. The cuboid is a pulley for the peroneus longus tendon; muscle contraction from midstance through the late propulsive phase exerts an eversion torque on the cuboid 14. Eversion of the cuboid via the peroneus longus tendon is thought to facilitate load transfer across the forefoot from lateral to medial as stance progresses 15.
Although the normal mechanics of the midtarsal joints are not fully understood, the midtarsal joints (talonavicular and calcaneocuboid) are thought to play a vital role in the transition of the foot from a mobile adapter during weight acceptance to a rigid lever during push-off and in rearfoot-to-forefoot load transfer during propulsion 16. Load transfer should occur from the lateral-to-medial forefoot to facilitate an effective “windlass effect” when the metatarsophalangeal joints extend 15. During early stance when the calcaneus is everted, the forefoot tends to flex and extend more; during push-off, the calcaneus is inverted, and the forefoot is more rigid 16. This phenomenon is attributed to the orientation of the talonavicular and calcaneocuboid joint axes 17, which become parallel during calcaneal eversion, increasing motion in these joints and in the forefoot in general 17. Conversely, calcaneal inversion during push-off causes the midtarsal joint axes to diverge, which reduces mobility in the midtarsal joint and the forefoot. Forefoot flexion/extension may increase when the calcaneus everts, even though cuboid and navicular mobility decrease 16.
Cuboid syndrome causes
Although the precise pathomechanic mechanisms are debated, cuboid syndrome is believed to be secondary to repeated or forceful eversion of the cuboid relative to the calcaneus, resulting in disruption of the calcaneocuboid joint 1. Fibroadipose synovial folds (or labra) within the calcaneocuboid joint may play a role in the cause of cuboid syndrome, but this is highly speculative.
The mechanism of the peroneus longus is implicated as a contributing factor, as the tendon wraps around the cuboid and is responsible for cuboid eversion. The peroneus is thought to aid in load transfer from lateral to medial forefoot during normal stride 1.
Injury to the calcaneocuboid joint may co-occur during an ankle ligament sprain, which may be a cause of persistent pain surpassing typical sprain symptoms 2.
Cuboid syndrome symptoms
The symptoms of cuboid syndrome resemble those of a ligament sprain 1. Pain is often diffuse along the lateral foot between the calcaneocuboid joint and the fourth and/or fifth cuboid-metatarsal joints and may radiate throughout the foot 18. A slight sulcus over the dorsum of the cuboid and/or a slight prominence or fullness on the plantar surface may be present with subluxation along with erythema, edema, and/or ecchymosis 19.
Tenderness may be present along the peroneus longus tendon, the cuboid groove, the dorsolateral and/or plantar cuboid 19 or the origin of the extensor digitorum brevis muscle 20. Ankle and/or foot active and passive range of motion may be decreased due to pain.31,34 Resisted ankle/foot eversion or inversion may elicit pain 18.
Antalgic gait is common with cuboid syndrome, with pain and/or weakness most pronounced during push-off or with side-to-side movements 19. Hopping may elicit symptoms 21, which increase with weightbearing and decrease with rest 22.
Cuboid syndrome diagnosis
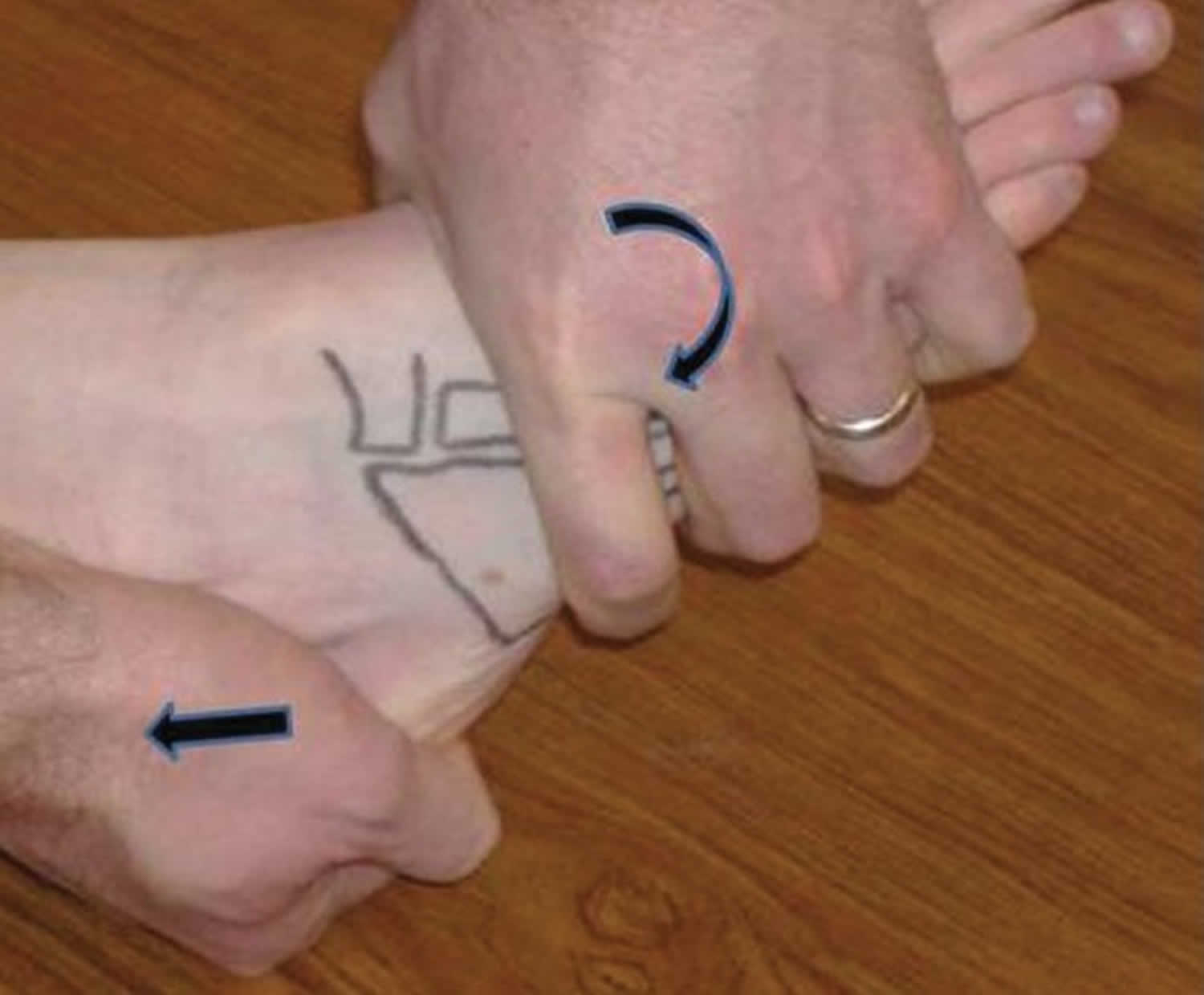
Although there are no definitive validated diagnostic tests for cuboid syndrome, two clinical maneuvers have been described—the midtarsal adduction test and the midtarsal supination test 18. During the adduction test, the midtarsal joint is manipulated passively in the transverse plane (about a superior-inferior axis) while the calcaneus is stabilized (Figure 4). This maneuver compresses the medial aspect of the calcaneocuboid joint and distracts the lateral side. The supination test is similar by adding inversion (frontal plane) and plantar flexion (sagittal plane) (Figure 5) 18.
Pain may also be elicited when the cuboid is passively translated dorsally or plantarly (Figure 6) 23. This motion is decreased when the cuboid is “locked.” The diagnostic accuracy of these maneuvers has not been determined.
Figure 4. Midtarsal adduction test
Figure 5. Midtarsal supination test
Figure 6. Dorsal-plantar cuboid shear test
Cuboid syndrome test
Imaging
Radiography, computerized tomography (CT scan), and magnetic resonance imaging (MRI) have not improved the diagnosis of cuboid syndrome 23, in part because nonpathologic variations in lateral foot anatomy are common 20. Aberrations in midtarsal joint alignment that produce symptoms in weightbearing may also be undetectable with radiography if foot radiographs are obtained nonweightbearing 24. Plain radiographs can rule out fractures or other significant bony abnormalities and help establish a differential diagnosis.
Differential diagnosis
Because of the difficulty in diagnosing cuboid syndrome, the differential diagnosis of lateral foot pain should include fracture or dislocation of the cuboid, calcaneus, or fourth or fifth metatarsals, calcaneonavicular coalition, peroneal or extensor digitorum brevis tendinopathy, plantar fasciitis, sinus tarsi syndrome, meniscoid of the ankle, gout, tarsitis, Lisfranc injury, compression neuropathy of the sural nerve, lateral plantar nerve entrapment, and anterolateral ankle impingement 25. Approximately 90% of tarsal coalitions occur either at the calcaneonavicular joint or the talocalcaneal joint 26. Isolated fractures of the cuboid are rare 27 as are cuboid dislocations, with only 13 reported cases in the literature.
Cuboid syndrome may be misdiagnosed as a lateral ankle sprain or overlooked when it develops in conjunction with a lateral ankle injury 18. Persistent pain in the calcaneocuboid joint region after lateral ankle symptoms have subsided should raise suspicion of cuboid syndrome 18.
Cuboid syndrome treatment
Multiple sources have recommended manipulation of the cuboid 1, as the initial treatment for cuboid syndrome unless contraindicated (ie, bone disease, inflammatory arthritis, gout, neural or vascular compromise, or fracture) 28. Two techniques have been described—the cuboid whip (Figure 7) 29 and the cuboid squeeze (Figure 8) 23. For the cuboid whip, the clinician cups the dorsum of the patient’s forefoot, placing thumbs on the plantomedial aspect of the cuboid. The patient’s knee is flexed 70° to 90° while the ankle is placed in 0° dorsiflexion 29. With the patient’s leg relaxed, the clinician abruptly “whips” the foot into inversion and plantarflexion while delivering a low-amplitude, high-velocity thrust (via the thumbs) to the cuboid (Figure 7). A “pop” or shift may be heard and/or felt by the clinician and/or patient during the thrust 23. During the cuboid squeeze, the clinician slowly stretches the ankle into maximal plantarflexion and the foot and toes into maximal flexion. When the clinician feels the dorsal soft tissues relax, the cuboid is “squeezed” (ie, forced dorsal) with the thumbs (Figure 8). The cuboid squeeze may not be appropriate for patients who have a coincident lateral ankle sprain, because the ankle is maximally plantarflexed before the manipulation. Manipulation of the cuboid should be attempted only when edema and ecchymosis have significantly diminished and when the injured ankle capsule and ligaments have healed adequately to tolerate the stress of manipulation.
Figure 7. Cuboid whip manipulation
Figure 8. Cuboid squeeze technique
Heel raise tolerance and/or reduced discomfort with passive dorsal-plantar cuboid gliding may be evidence of improvement after manipulation. Patients who experience partial or incomplete symptom resolution may benefit from additional manipulations. There appears to be an association between the duration of symptoms and the number of manipulations required for complete symptom resolution 18. Some patients experience mild discomfort after the manipulation and may benefit from cryotherapy, nonthermal ultrasound, pain-modulating electrical stimulation, or therapeutic massage 18. Patients should be advised to avoid vigorous weightbearing activities (eg, running) for several days after manipulation 23.
Following successful manipulation, recurrence may be prevented by employing taping, orthoses, and/or cuboid padding 23. Various taping techniques have been suggested, with a common goal of supporting the medial longitudinal arch 30. Padding to support the plantar cuboid is commonly recommended for cuboid syndrome 19. The dimensions, thickness, and placement of the pad beneath the medial aspect of the cuboid are adjusted to prevent eversion of the cuboid (felt with a thickness of 1/8 or 1/4 in. [3-6 mm]) 31. A lateral wedge under the calcaneus may also help reduce pain with weightbearing.
Patients who do not experience relief after manipulation should be reexamined and other diagnoses considered, including isolated sprain of the lateral midfoot ligaments. Immobilization of the foot/ankle, coupled with crutch/cane unloading, is advisable. Orthoses may reduce excessive pronation 20 and may prevent a recurrence of cuboid syndrome 19. Stretching the gastrocnemius, soleus, hamstring, and/or peroneus longus and strengthening the intrinsic and extrinsic foot muscles may help prevent recurrence of cuboid syndrome 19.
References- Durall CJ. Examination and treatment of cuboid syndrome: a literature review. Sports Health. 2011;3(6):514–519. doi:10.1177/1941738111405965 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3445231
- Recognizing Cuboid Syndrome. Curr Sports Med Rep. 2018 Jan;17(1):6. doi: 10.1249/JSR.0000000000000437. https://journals.lww.com/acsm-csmr/fulltext/2018/01000/Recognizing_Cuboid_Syndrome.4.aspx
- Jennings J, Davies GJ. Treatment of cuboid syndrome secondary to lateral ankle sprains: a case series. J. Orthop. Sports Phys. Ther. 2005; 35:409–15.
- Marshall P, Hamilton WG. Cuboid subluxation in ballet dancers. Am J Sports Med. 1992;20:169-175.
- Treatment of Cuboid Syndrome Secondary to Lateral Ankle Sprains: A Case Series. J Orthop Sports Phys Ther Volume 35, Number 7; July 2005 https://www.jospt.org/doi/pdf/10.2519/jospt.2005.35.7.409
- Newell SG, Woodle A. Cuboid syndrome. Phys Sports Med. 1981;9:71-76.
- Hardy RH. Observations on the structure and properties of the plantar calcaneo-navicular ligament in man. J Anat. 1951;85(2):135-139
- Nester CJ, Findlow AH. Clinical and experimental models of the midtarsal joint: proposed terms of reference and associated terminology. J Am Podiatr Med Assoc. 2006;96(1):24-31
- Greiner TM, Ball KA. The calcaneocuboid joint moves with three degrees of freedom. J Foot Ankle Res. 2008;1(suppl 1):O39
- Smith JS, Flemister AS. Complete cuboid dislocation in a professional baseball player. Am J Sports Med. 2006;34(1):2-3
- Hlavac HF. Differences in x-ray findings with varied positioning of the foot. J Am Podiatry Assoc. 1967;57(10):465-471
- Dorn-Lange NV, Nauck T, Lohrer H, Arentz S, Konerding MA. Morphology of the dorsal and lateral calcaneocuboid ligaments. Foot Ankle Int. 2008;29(9):942-949
- Sutherland DH. The evolution of clinical gait analysis, part I: kinesiological EMG. Gait Posture. 2001;14:61-70
- Johnson CH, Christensen JC. Biomechanics of the first ray: part I. The effects of peroneus longus function: a three-dimensional kinematic study on a cadaver model. J Foot Ankle Surg. 1999;38(5):313-321
- Bojsen-Moller F. Calcaneocuboid joint and stability of the longitudinal arch of the foot at high and low gear push off. J Anat. 1979;129:165-176
- Suckel A, Muller O, Langenstein P, Herberts T, Reize P, Wulker N. Chopart’s joint load during gait in vitro study of 10 cadaver specimen in a dynamic model. Gait Posture. 2008;27:216-222
- Elftman H. The transverse tarsal joint and its control. Clin Orthop. 1960;16:41-45
- Jennings J, Davies GJ. Treatment of cuboid syndrome secondary to lateral ankle sprains a case series. J Orthop Sports Phys Ther. 2005;35(7):409-415
- MacIntyre J, Joy E. The athletic woman foot and ankle injuries in dance. Clin Sports Med. 2000;1(2):351-368
- Blakeslee TJ, Morris JL. Cuboid syndrome and the significance of midtarsal joint stability. J Am Podiatr Med Assoc. 1987;77(12):638-642
- Marshall P, Hamilton WG. Cuboid subluxation in ballet dancers. Am J Sports Med. 1992;20(2)169-17
- Omey ML, Micheli LJ. Foot and ankle problems in the young athlete. Foot Ankle. 1999;31(7):S470-S486
- Marshall P, Hamilton WG. Cuboid subluxation in ballet dancers. Am J Sports Med. 1992;20(2)169-175
- Gamble FO, Yale I. Clinical Foot Roentgenology. Baltimore, MD: Lippincott Williams & Wilkins; 1975
- Main BJ, Jowett RL. Injuries of the midtarsal joint. J Bone Joint Surg Br. 1975;57:89
- Leerar PJ. Differential diagnosis of tarsal coalition versus cuboid syndrome in and adolescent athlete. J Orthop Sports Phys Ther. 2001;31(12):702-707
- Miller SR, Handzel C. Isolated cuboid fracture: a rare occurrence. J Am Podiatr Med Assoc. 2001;91(2):85-88
- Caselli MA, Pantelaras N. How to treat cuboid syndrome in an athlete. Podiatry Today. 2004;17(10):76-80
- Newell SG, Woodle A. Cuboid syndrome. Phys Sports Med. 1981;9(4):71-76
- Mooney M, Maffey-Ward L. Cuboid plantar and dorsal subluxations assessment and treatment. J Orthop Sports Phys Ther. 1994;20(4):220-226
- White SC. Padding and taping techniques. In: Valmassy RL, editor. , ed. Clinical Biomechanics of the Lower Extremities. St Louis, MO: Mosby-Year Book Inc; 1996:367-390