What is Darier’s disease
Darier’s disease also known as Darier–White disease, is an inherited skin condition characterized by wart-like blemishes on the body 1. They usually first appear in late childhood or early adulthood and often occur on the scalp, forehead, upper arms, chest, back, knees, elbows, and/or behind the ear. The wart-like blemishes are usually yellowish in color, hard to the touch, mildly greasy, and can emit a strong odor. The most common sites for blemishes are the scalp, forehead, upper arms, chest, back, knees, elbows, and behind the ear. The mucous membranes can also be affected, with blemishes on the roof of the mouth (palate), tongue, inside of the cheek, gums, and throat. Other features of Darier disease include nail abnormalities, such as red and white streaks in the nails with an irregular texture, and small pits in the palms of the hands and soles of the feet.
The wart-like blemishes characteristic of Darier disease usually appear in late childhood to early adulthood. The severity of the disease varies over time; affected people experience flare-ups alternating with periods when they have fewer blemishes. The appearance of the blemishes is influenced by environmental factors. Most people with Darier disease will develop more blemishes during the summertime when they are exposed to heat and humidity. UV light; minor injury or friction, such as rubbing or scratching; and ingestion of certain medications can also cause an increase in blemishes.
On occasion, people with Darier’s disease may have neurological disorders such as mild intellectual disability, epilepsy, and depression. Learning and behavior difficulties have also been reported in people with Darier’s disease. Researchers do not know if these conditions, which are common in the general population, are associated with the genetic changes that cause Darier’s disease, or if they are coincidental. Some researchers believe that behavioral problems might be linked to the social stigma experienced by people with numerous skin blemishes.
Other features of Darier’s disease may include nail abnormalities, such as red and white streaks in the nails with an irregular texture; and small pits in the palms of the hands and soles of the feet. The severity of Darier’s disease varies over time. Some people have a more localized form of Darier’s disease known as the linear or segmental form. The linear or segmental form of Darier’s disease is characterized by blemishes on localized areas of the skin. The blemishes are not as widespread as they are in typical Darier disease. Some people with the linear form of this condition have the nail abnormalities that are seen in people with classic Darier disease, but these abnormalities occur only on one side of the body.
Darier’s disease is previously known as keratosis follicularis, but this is incorrect because the scaly papules do not arise from hair follicles 2. Darier disease is classified as a hereditary acantholytic dermatosis. Darier’s disease is not an infection and the blemishes are not contagious. Darier’s disease is caused by mutations in the ATP2A2 gene and is inherited in an autosomal dominant manner 3. However, not all people with a mutation in this gene will develop the disease. Darier’s disease treatment is not always needed but may include the use of moisturizers and sunscreen; staying cool; dermabrasion; and/or oral or topical retinoids 4.
The worldwide prevalence of Darier’s disease is unknown. The prevalence of Darier disease is estimated to be 1 in 30,000 people in Scotland, 1 in 36,000 people in northern England, and 1 in 100,000 people in Denmark. Darier’s disease affects men more frequently than women 5.
Figure 1. Darier’s disease
Footnote: Patient with typical signs of Darier’s disease. (Left) Lower back area. (Right) Frontal view of neck area.
[Source 6 ]Darier’s disease causes
Mutations in the ATP2A2 gene cause Darier’s disease. The ATP2A2 gene encodes a calcium pump in the endoplasmic reticulum called SERCA2 7. This enzyme acts as a pump that helps control the level of positively charged calcium atoms (calcium ions) inside cells, particularly in the endoplasmic reticulum and the sarcoplasmic reticulum. The endoplasmic reticulum is a structure inside the cell that is involved in protein processing and transport. The sarcoplasmic reticulum is a structure in muscle cells that assists with muscle contraction and relaxation by releasing and storing calcium ions. Calcium ions act as signals for a large number of activities that are important for the normal development and function of cells. SERCA2 allows calcium ions to pass into and out of the cell in response to cell signals.
Mutations in the ATP2A2 gene result in insufficient amounts of functional SERCA2 enzyme. A lack of SERCA2 enzyme reduces calcium levels in the endoplasmic reticulum, causing it to become dysfunctional. SERCA2 is expressed throughout the body; it is not clear why changes in this enzyme affect only the skin. Some researchers note that skin cells are the only cell types expressing SERCA2 that do not have a “back-up” enzyme for calcium transport. This dependence on the SERCA2 enzyme may make skin cells particularly vulnerable to changes in this enzyme.
The linear form of Darier disease is caused by ATP2A2 gene mutations that are acquired during a person’s lifetime and are present only in certain cells. These changes are called somatic mutations and are not inherited. There have been no known cases of people with the linear form of Darier disease passing it on to their children.
Darier’s disease inheritance pattern
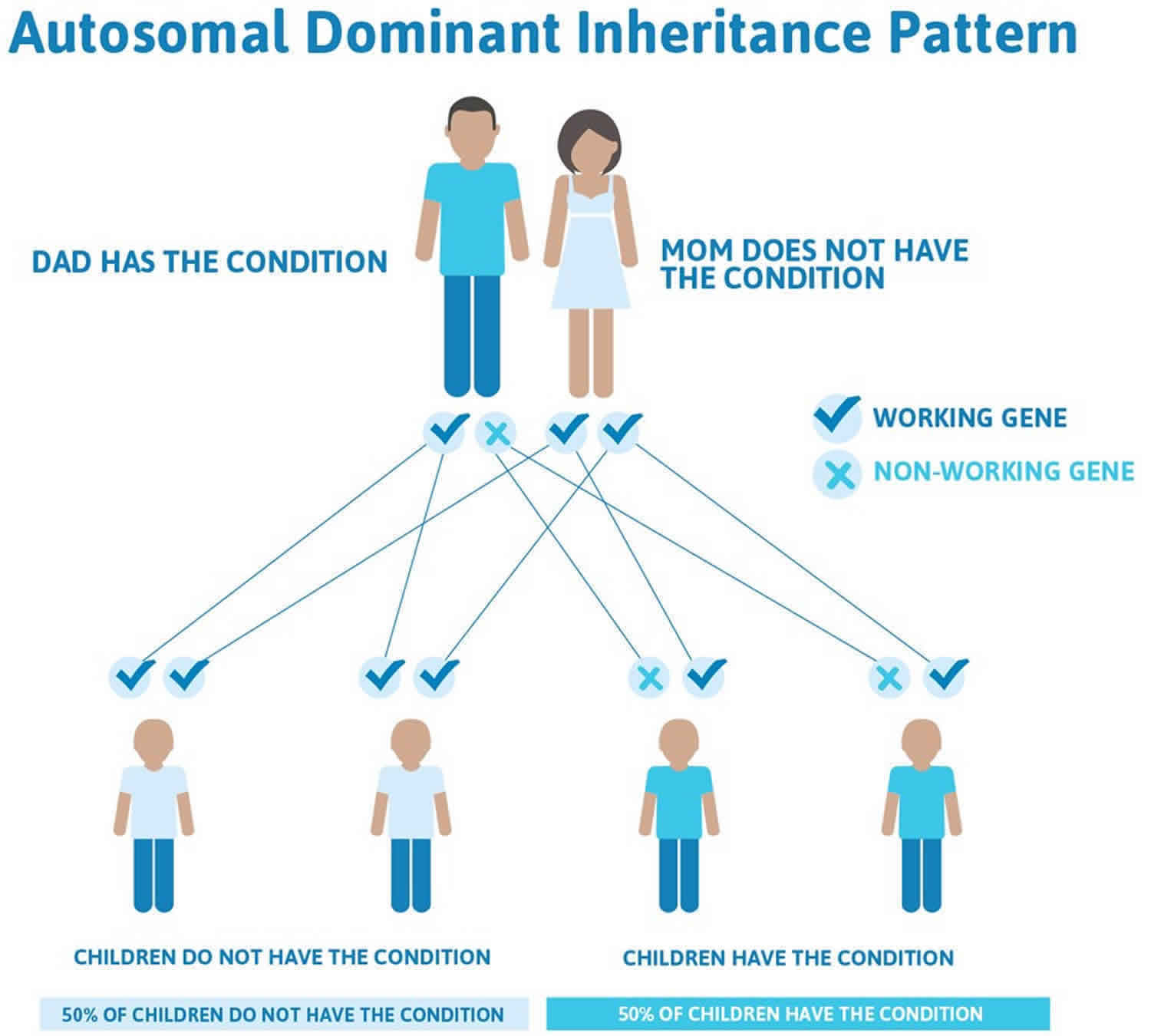
Darier’s disease is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder. The chance of a child inheriting the abnormal gene if one parent is affected is 1 in 2 (50%) but not all people with the abnormal gene will develop symptoms of the disease.
In some cases, an affected person inherits the mutation from one affected parent. Other cases may result from new mutations in the gene. These cases occur in people with no history of the disorder in their family.
The linear form of Darier disease is generally not inherited but arises from mutations in the body’s cells that occur after conception. These alterations are called somatic mutations.
Often autosomal dominant conditions can be seen in multiple generations within the family. If one looks back through their family history they notice their mother, grandfather, aunt/uncle, etc., all had the same condition. In cases where the autosomal dominant condition does run in the family, the chance for an affected person to have a child with the same condition is 50% regardless of whether it is a boy or a girl. These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
- When one parent has the abnormal gene, they will pass on either their normal gene or their abnormal gene to their child. Each of their children therefore has a 50% (1 in 2) chance of inheriting the changed gene and being affected by the condition.
- There is also a 50% (1 in 2) chance that a child will inherit the normal copy of the gene. If this happens the child will not be affected by the disorder and cannot pass it on to any of his or her children.
Figure 2 illustrates autosomal dominant inheritance. The example below shows what happens when dad has the condition, but the chances of having a child with the condition would be the same if mom had the condition.
Figure 2. Darier’s disease autosomal dominant inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Darier’s disease symptoms
The symptoms and signs of Darier’s disease vary markedly between individuals. Some have very subtle signs that are asymptomatic and found only on careful inspection. Others have extensive lesions which can cause considerable distress to the affected individual. In an affected person the severity of the disease can fluctuate over time.
The onset of skin changes is usually in adolescence and Darier’s disease is usually chronic.
The skin lesions are characterized by persistent, greasy, scaly papules. Affected sites include:
- Seborrheic areas of the face (scalp margins, forehead, ears, around the nostrils and sides of nose, eyebrows, and beard area)
- Scalp and neck
- Central chest and back
- Skin folds, such as armpits, groin, under the breasts and between the buttocks
The papules have a firm, harsh feel like coarse sandpaper and may be skin-colored, yellow-brown or brown in colour. If several of the small papules grow together they may form larger warty lesions which can become quite smelly within skin folds. There may be a heavily crusted rash similar to seborrheic dermatitis.
Most patients with Darier disease will have longitudinal broad stripes of white and reddish color on some or all fingernails. A V-shaped nick at the free edge of the nail as well as nail fragility is also very suggestive of Darier’s disease. These changes on the hands can also occur on the feet, albeit less commonly.
In 50% of patients with Darier disease, the oral mucosa is involved 5. The oral lesions consist of white or red firm papules. The papules may form crusts or ulcerations but are usually asymptomatic 5. Neurologic abnormalities such as epilepsy and intellectual disability have been described in association with Darier disease. Patients with Darier disease exhibit higher rates of depression and mood disorders 8.
Atypical presentations of Darier’s disease are common.
- Flat, freckle-like lesions
- Blistered papules
- Large, raised, warty lesions
- A linear pattern, with papules following the lines of embryonal development of the skin (segmental distribution)
Acne conglobata (cystic acne) is associated with Darier’s disease in some individuals.
Acrokeratosis verruciformis
Warty papules on the dorsum of hands are known as acrokeratosis verruciformis. Involvement of the hands is very common (approximately 95%). Lesions on the palms include punctate keratoses (80%), palmar pits (80%), and hemorrhagic macules (< 10%). Other signs may include:
- Small pits on the palms and soles
- Bleeding under the skin
A localized variant of Darier’s disease, in which papules on hands and feet are the main feature is called acrokeratosis verruciformis of Hopf.
Lesions affecting the mucous membranes
Mucous membranes are the red, moist linings of body surfaces (mouth, esophagus, rectum, vulva, vagina). Mucosal lesions are detected in approximately 15% of patients, and they appear as white papules with a central depression. Patients with Darier disease may uncommonly have a white cobblestone pattern of small papules affecting the mucous membranes most commonly found in the mouth, but they also may occur on the anogenital mucosa. Overgrowth of the gums may also occur. At times, oral lesions may affect the salivary glands and cause obstruction 9.
Most affected patients develop signs of Darier’s disease before the age of 30 years.
- Many have mild and unnoticed Darier’s disease.
- More severe disease may have a chronic relapsing-remitting pattern.
- The signs may clear up altogether.
Flare-ups may be caused by any of the following factors.
- Exposure to sunlight or heat.
- Topical corticosteroids
- Bacterial infection
- Herpes simplex infection – including severe Kaposi varicelliform eruption (see eczema herpeticum).
In most patients, general health remains good regardless of the severity of the disease.
How is Darier’s disease diagnosed?
Usually, Darier’s disease is diagnosed by its appearance and family history, but it is often is mistaken for other skin problems.
Diagnosis may require a skin biopsy. The histology is characteristic, known as focal acantholytic dyskeratosis associated with varying degrees of papillomatosis. The pathological features are similar to transient acantholytic dermatosis (Grover disease).
Darier’s disease treatment
Treatment of Darier’s disease is required only if there are troublesome symptoms. Mild disease can be managed with:
- Moisturizers
- Sun protection
- Careful selection of clothing to avoid heat and sweating
Localized Darier’s disease can be treated by:
- Topical retinoids
- Dermabrasion
Secondary bacterial infection (usually due to Staphylococcus aureus) should be treated with antibiotics. Herpes simplex is treated with aciclovir or valaciclovir.
Severe Darier’s disease is usually treated with oral retinoids, either acitretin or isotretinoin. Ciclosporin has been reported to be effective in a few patients.
The avoidance of triggers is paramount in preventing exacerbations of Darier disease. Triggers can include sunlight, heat, occlusive clothing, and friction.[1] Patients should avoid sun exposure, wear loose clothing, use sunscreen, and employ proper hygiene practices.
As Darier’s disease is inherited in an autosomal dominant fashion, patients should be offered genetic counseling.
Darier’s disease prognosis
Darier’s disease persists for life in a relapsing-remitting manner. Avoiding triggers and using the appropriate treatments can allow for at least partial control of Darier’s disease.
Patients with Darier’s disease experience itch (pruritus) and sometimes pain in the affected skin areas. Psychosocial consequences from the appearance and odor of the lesions also constitute the major morbidity of Darier’s disease. A serious complication associated with Darier’s disease is increased susceptibility to cutaneous bacterial and viral infections, in particular herpes simplex virus, human papillomavirus (HPV) 10 and poxvirus infections. Initial misdiagnosis of keratosis follicularis (Darier disease) may lead to undertreatment of such infections and may lead to fatal outcomes 11. However, overall, patients with Darier’s disease have a life expectancy similar to that of the general population.
Neuropsychiatric abnormalities such as epilepsy, mental impairment, schizophrenia, and mood disorders have been associated with Darier’s disease 12. Several national studies suggest that genetic variability within the ATP2A2 gene that causes Darier disease also confers susceptibility for a number of neuropsychiatric disorders 13, including bipolar disorder 14, intellectual disability, and subclinical impairments in cognitive ability 15.
References- Schmieder SJ, Rosario-Collazo JA. Keratosis Follicularis (Darier Disease) [Updated 2019 Mar 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519557
- Darier disease. https://www.dermnetnz.org/topics/darier-disease/
- Darier disease. https://ghr.nlm.nih.gov/condition/darier-disease
- Darier disease. https://www.dermnetnz.org/topics/darier-disease
- Suryawanshi H, Dhobley A, Sharma A, Kumar P. Darier disease: A rare genodermatosis. J Oral Maxillofac Pathol. 2017 May-Aug;21(2):321
- Beier, C., & Kaufmann, R. (1999). Efficacy of erbium:YAG laser ablation in Darier disease and Hailey-Hailey disease. Archives of dermatology, 135 4, 423-7
- Savignac M, Simon M, Edir A, Guibbal L, Hovnanian A. SERCA2 dysfunction in Darier disease causes endoplasmic reticulum stress and impaired cell-to-cell adhesion strength: rescue by Miglustat. J. Invest. Dermatol. 2014 Jul;134(7):1961-1970.
- Gordon-Smith K, Jones LA, Burge SM, Munro CS, Tavadia S, Craddock N. The neuropsychiatric phenotype in Darier disease. Br. J. Dermatol. 2010 Sep;163(3):515-22.
- Bernabé DG, Kawata LT, Beneti IM, Crivelini MM, Biasoli ER. Multiple white papules in the palate: oral manifestation of Darier’s disease. Clin Exp Dermatol. 2009 Oct. 34(7):e270-1.
- Matsumoto A, Gregory N, Rady PL, Tyring SK, Carlson JA. Brief Report: HPV-17 Infection in Darier Disease With Acrokeratosis Verrucosis of Hopf. Am J Dermatopathol. 2017 May. 39 (5):370-373.
- Okada E, Nagai Y, Motegi S, Tamura A, Ishikawa O. Fatal case of Darier’s disease with recurrent severe infections. Acta Derm Venereol. 2009. 89(4):408-9.
- Tang C, Chan M, Lee J, Hariram J. Darier’s disease and schizophrenia. East Asian Arch Psychiatry. 2010 Dec. 20(4):190-2.
- Dodiuk-Gad RP, Cohen-Barak E, Khayat M, Milo H, Amariglio-Diskin L, Danial-Faran N, et al. Darier disease in Israel: combined evaluation of genetic and neuropsychiatric aspects. Br J Dermatol. 2016 Mar. 174 (3):562-8.
- Cederlöf M, Bergen SE, Långström N, Larsson H, Boman M, Craddock N, et al. The association between Darier disease, bipolar disorder, and schizophrenia revisited: a population-based family study. Bipolar Disord. 2015 May. 17 (3):340-4.
- Cederlöf M, Karlsson R, Larsson H, Almqvist C, Magnusson PK, Nordlind K, et al. Intellectual disability and cognitive ability in Darier disease: Swedish nation-wide study. Br J Dermatol. 2015 Jul. 173 (1):155-8.