What are diabetic foot problems
People with diabetes can get foot problems because there is too much blood sugar also called glucose, in the blood over a long period of time. The excess blood sugar cause nerve damage, also called diabetic neuropathy, that can cause tingling and pain, and can make you lose feeling in your feet. When you lose feeling in your feet, you may not feel a pebble inside your sock or a blister on your foot, which can lead to cuts and sores. Cuts and sores can become infected.
Diabetes also can also damage the blood vessels in your feet, which mean your feet do not get enough blood and oxygen. Not having enough blood flowing to your legs and feet can make it hard for a sore or an infection to heal. Sometimes, a bad infection never heals. The infection might lead to gangrene.
Gangrene and foot ulcers that do not get better with treatment can lead to an amputation of your toe, foot, or part of your leg. A surgeon may perform an amputation to prevent a bad infection from spreading to the rest of your body, and to save your life. Good foot care is very important to prevent serious infections and gangrene.
Although rare, nerve damage from diabetes can lead to changes in the shape of your feet, such as Charcot’s foot. Charcot’s foot may start with redness, warmth, and swelling. Later, bones in your feet and toes can shift or break, which can cause your feet to have an odd shape, such as a “rocker bottom.”
Figure 1. Charcot’s foot in diabetes
However, if you manage your diabetes well, most foot problems including amputations, can be prevented. You can also dramatically reduce your chances of foot problems by taking good care of your feet everyday and having them checked regularly by a podiatrist. Looking after your feet on a daily basis can be tough especially if you’ve lost any sensation in them. If this is the case, it’s a good idea to speak to your healthcare team as you may need help from a podiatrist.
Never ignore a problem with your feet. Foot problems can develop extremely quickly. Urgent treatment is vital. If you have any concerns about your feet contact your diabetes healthcare team. Know who to call at the first sign of any new foot problems and keep their numbers handy.
You can help avoid foot problems. First, control your blood sugar levels. Good foot hygiene is also crucial.
Tips to take care of your feet:
- Check your feet every day.
- Wash your feet every day.
- Keep the skin soft and smooth.
- Smooth corns and calluses gently.
- If you can see, reach, and feel your feet, trim your toenails regularly. Trim your toenails straight across. If you cannot, ask a foot doctor (podiatrist) to trim them for you.
- Wear shoes and socks at all times.
- Protect your feet from hot and cold.
- Keep the blood flowing to your feet.
- Get a foot check at every health care visit.
When should I see my health care provider about foot problems?
See your health care provider right away if you have:
- a cut, blister, or bruise on your foot that does not start to heal after a few days
- skin on your foot that becomes red, warm, or painful—signs of a possible infection
- a callus with dried blood inside of it,which often can be the first sign of a wound under the callus
- a foot infection that becomes black and smelly—signs you might have gangrene
Ask your provider to refer you to a foot doctor, or podiatrist, if needed.
Seek treatment from your doctor or podiatrist if blisters or injuries don’t heal quickly.
You should see your doctor urgently if:
- you notice breaks in the skin of your foot, or discharge seeping from the wound
- the skin over part or all of the foot changes color and becomes more red, blue, pale or dark
- you notice extra swelling in your feet where there was a blister or injury
- there is redness or swelling around an ulcer or in an area where you have previously been warned to seek immediate attention
Diabetic foot pain
Diabetes can cause nerve damage also called diabetic neuropathy, as a result of high blood glucose levels damaging the small blood vessels which supply the nerves. This prevents essential nutrients reaching the nerves. The nerve fibers are then damaged or disappear. About half of all people with diabetes have some form of nerve damage. Diabetic neuropathy is more common in those who have had the diabetes for a number of years and can lead to many kinds of problems.
If you keep your blood glucose levels on target, you may help prevent or delay nerve damage. If you already have nerve damage, this will help prevent or delay further damage. There are also other treatments that can help.
There are three different types of neuropathy:
- sensory neuropathy,
- autonomic neuropathy and
- motor neuropathy.
Sensory neuropathy
Sensory neuropathy occurs if the body’s sensory nerves become damaged. Sensory neuropathy affects your body’s sensory nerves that carry messages of touch, temperature, pain and other sensations from the skin, bones and muscles to your brain. Sensory neuropathy affects the nerves in the feet and the legs, but people can also develop this type of neuropathy in their arms and hands. Sensory neuropathy may also be called polyneuropathy as it affects a number of different nerve centers.
People with diabetes have an increased risk of neuropathy as high blood glucose levels over long periods of time can damage the nerves.
Diabetic foot pain symptoms
Sensory neuropathy starts from the extremities of your body such as your feet or hands and can develop to affect your legs and arms. The symptoms of sensory neuropathy will be present at the part of your body where the nerves are affected.
What does diabetic foot pain feel like:
- Tingling and numbness
- Loss of ability to feel pain
- Loss of ability to detect changes in temperature
- Loss of coordination – when you lose your joint position sense
- Burning or sharp shooting pains – these may be worse at night time.
People with sensory neuropathy may experience dysesthesia, which translates as abnormal sensation.
The symptoms of dysesthesia include:
- A burning feeling under the skin
- Extremely sensitive skin to the extent where clothes and bedding can cause intense pain
The main danger of sensory neuropathy for someone with diabetes is loss of feeling in the feet, especially if you don’t realize that this has happened. This is dangerous because you may not notice minor injuries caused by:
- Walking around barefoot
- Sharp objects in shoes
- Friction from badly fitting shoes
- Burns from radiators of hot water bottles.
If ignored, minor injuries may develop into infections or ulcers. People with diabetes are more likely to be admitted to hospital with a foot ulcer than with any other diabetes complication.
Charcot joint is a rare complication of people with diabetes who have severe neuropathy. It happens when an injury to the foot causes a broken bone, which may go unnoticed because of the existing neuropathy. The bone then heals abnormally, causing the foot to be come deformed and misshapen. Treatment includes immobilizing the foot in a below-kneeplaster cast and in some cases surgery. Non-weight bearing immobilization or below-knee cast duration of treatment will depend upon response and it is recommended to continue casting until the temperature differential between the active and non-affected foot is down to approximately 1.5°C 1. As for the foot ulcer, it is recommended that treatment in a cast be continued for up to 4 weeks after the temperature differential has settled. At present, there are no proven medical or pharmacological approaches other than casting that have been shown to improve outcome. The management of advanced Charcot joint with bone deformity requires reconstructive surgery 2.
Diabetic foot pain relief
People with diabetes experiencing sensory neuropathy should aim to keep their blood glucose levels under tight control to help prevent neuropathy from developing.
People with diabetes experiencing neuropathic pain may first be prescribed an oral painkiller called duloxetine. Alternatives to duloxetine include amitriptyline and pregabalin. People who do not respond to the aforementioned treatments may be prescribed tramadol.
A further alternative is to use topical lidocaine which is a local anaesthetic that may be prescribed as a cream, gel or spray.
Steps you can take to avoid neuropathy
- Keep your blood glucose levels within your target range.
- Have your feet checked at least once a year.
- Tell your diabetes healthcare team if you think you’re developing any signs of neuropathy.
- If you think you’ve lost sensation in your feet, protect them from injury and check them every day.
- And talk to your diabetes healthcare team.
Autonomic neuropathy
Autonomic neuropathy affects nerves that carry information to your organs and glands. They help to control some functions without you consciously directing them, such as stomach emptying, bowel control, heart beating and sexual organs working.
Damage to these nerves can result in:
- Gastroparesis – when food can’t move through the digestive system efficiently. Symptoms of this can include bloating, constipation or diarrhea
- Loss of bladder control, leading to incontinence
- Irregular heart beats
- Problems with sweating, either a reduced ability to sweat and intolerance to heat or sweating related to eating food (gustatory)
- Impotence (inability to keep an erection).
Motor neuropathy
Motor neuropathy affects the nerves which control movement. Damage to these nerves leads to weakness and wasting of the muscles that receive messages from the affected nerves. This can lead to problems such as:
- muscle weakness, which could cause falls or problems with tasks such as fastening buttons.
- muscle wasting, where muscle tissue is lost due to lack of activity
- muscle twitching and cramps.
Diabetic foot ulcer
Foot ulcers can occur in anyone, and refer to a patch of broken down skin usually on the lower leg or feet. When blood sugar levels are high or fluctuate regularly skin that would normally heal may not properly repair itself because of nerve damage. Even a mild injury can therefore start a foot ulcer.
Ulcers occur most often on the ball of the foot or on the bottom of the big toe. Ulcers on the sides of the foot are usually due to poorly fitting shoes. Remember, even though some ulcers do not hurt, every ulcer should be seen by your health care provider right away. Neglecting ulcers can result in infections, which in turn can lead to loss of a limb.
Diabetic foot ulcers affect many people with diabetes. Experts suggest that around 10 per cent of people with diabetes develop a foot ulcer at some point.
Foot ulcers can affect people with both type 1 and type 2 diabetes.
Diabetes influences foot ulcers in a number of ways, and it is important for people with diabetes to understand the potentially severe consequences of leaving a foot ulcer untreated.
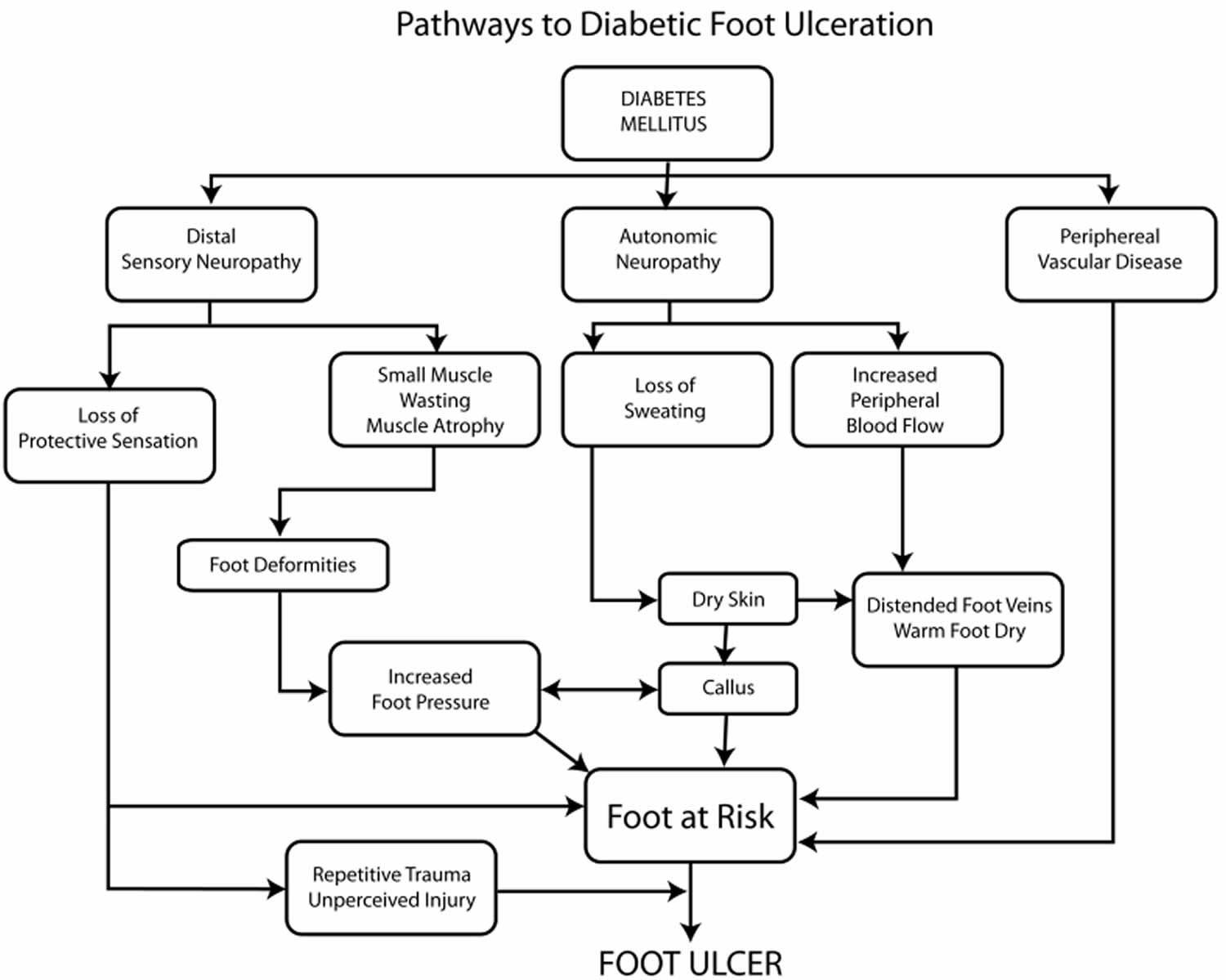
Figure 2. Pathways to diabetic foot ulceration
[Source 1 ]Why are people with diabetes more likely to get foot ulcers?
People with diabetes may have reduced nerve functioning due to peripheral diabetic neuropathy. This means that the nerves that usually carry pain sensation to the brain from the feet do not function as well and it is possible for damage to uccur to your foot without feeling it. Treading on something, wearing tight shoes, cuts, blisters and bruises can all develop into diabetes foot ulcers.
Narrowed arteries can also reduce blood flow to the feet amongst some people with diabetes and this can impair the foot’s ability to heal properly. When the foot cannot heal, a foot ulcer can develop.
What are the risk factors for diabetes foot ulcers?
The following can increase the likelihood of developing a foot ulcer:
- Neuropathy
- Poor blood circulation
- Insufficiently well controlled diabetes
- Wearing poor fitting footwear
- Walking barefoot
People who have diabetes for a longer period or manage their diabetes less effectively are more likely to develop foot ulcers. Smoking, not taking exercise, being overweight, having high cholesterol or blood pressure can all increase diabetes foot ulcer risk.
How serious are foot ulcers?
Unfortunately, for some people with diabetes, the end result of a foot ulcer can be amputation. Less serious foot ulcers can still take a long time to heal and be very uncomfortable during this time.
How can I avoid diabetes foot ulcers?
Avoiding diabetes foot ulcers is a matter of taking good care of the feet (see the Diabetes and Footcare guide).
Furthermore, people with diabetes should have their feet checked at least once a year by a doctor or healthcare professional. Recognising symptoms such as reduced feeling and acting on them immediately should help to avoid diabetes foot ulcers.
I have diabetes and I am worried that I have a foot ulcer, what should I do?
People with diabetes who are concerned that they may have a foot ulcer should speak to a doctor or podiatrist at once. These professionals should dress and protect the ulcer to avoid infection and help the skin heal.
Diabetic foot ulcer stages
Accurate and concise ulcer description and classification systems are required to improve multidisciplinary collaboration and communication, as well as for aiding treatment choices. For many years, the Meggitt-Wagner grading system was regarded as the gold standard 1. One problem with this system is that the ischemic status of the wound is not included. Thus a number of new classification systems for diabetic foot wounds have been proposed and validated over the last 20 years. One of the commonest used in the United States is the University of Texas Wound Classification System 3. This incorporates the Meggitt-Wagner grades but also enables the practitioner to stage the wound with respect to the presence or absence of infection and/or ischemia (Table 1). In a comparative prospective study across two centers, one in the UK and one in the US, the University of Texas Classification System was shown to be superior to the Meggitt-Wagner system at predicting outcomes 4. However, this study also showed that the traditional Meggitt-Wagner system was itself generally accurate in predicting outcomes.
Table 1. The University of Texas wound classification system
| GRADE | |||||
| STAGE | 0 | 1 | 2 | 3 | |
| A | Pre-ulcerative lesions No skin break | Superficial wound No penetration | Wound penetrating tendon or capsule | Wound penetrating bone or joint | |
| B | With infection | With infection | With infection | With infection | |
| C | With ischemia | With ischemia | With ischemia | With ischemia | |
| D | With infection and ischemia | With infection and ischemia | With infection ad ischemia | With infection and ischemia | |
Diabetic foot ulcer treatment
What your health care provider will do varies with your ulcer. Your health care provider may take x-rays of your foot to make sure the bone is not infected. The health care provider may clean out any dead and infected tissue. You may need to go into the hospital for this. Also, the health care provider may culture the wound to find out what type of infection you have, and which antibiotic will work best.
Treatment of superficial ulcers (involving only the top layers of skin) usually includes cleaning the ulcer and removing dead skin and tissue (debridement) by a health care provider. There are a number of debridement techniques available.
If the foot is infected, antibiotics are generally prescribed. The patient (or someone in his or her household) should clean the ulcer and apply a clean dressing twice daily. The patient should keep weight off the foot ulcer as much as possible, meaning that they should not walk with the affected foot. The foot should be elevated when sitting or lying down. The ulcer should be checked by a health care provider at least once per week to make sure that the ulcer is improving.
Ulcers that extend into the deeper layers of the foot, involving muscle and bone, usually require hospitalization. More extensive laboratory testing and x-rays may be done, and intravenous antibiotics are often necessary. Surgery may be necessary to remove infected bone or to place a cast on the foot to take pressure off the ulcer.
A neuropathic diabetic patient with a plantar ulcer will therefore walk on the ulcer as there is no warning symptom to inform him or her otherwise. Techniques for removing pressure include the use of casts (either removable or irremovable), boots, half shoes, sandals and felted foam dressings. The total contact cast is regarded as the gold standard. Studies that randomize patients to an irremovable total contact cast, a removable cast walker or other offloading devices invariably confirm that healing is fastest in the irremovable device 5. Although removable cast walkers and irremovable casts (such as the total contact cast) offload equally well in the gait laboratory, the irremovable device is always associated with more rapid healing in clinical practice. The problem is that patients with neuropathic foot ulcers have lost the sensory cue that tells them not to walk on their active ulcer. Studies suggest that patients are compliant with wearing the offloading removable cast walker during the day, but feel that home is safer and therefore tend to put slippers on, or even walk barefoot at home. A subsequent trial has confirmed that if the removable cast walker is rendered irremovable by wrapping with scotch cast for example, then the outcome is that there is no difference in healing rates between the total contact cast and the removable cast walker rendered irremovable 6. Most patients with simple neuropathic foot ulcers (University of Texas grades 1A, 2A, 1B, 2B) generally heal in less than three months although of course this does vary with ulcer size. There is no contraindication to casting neuropathic patients with mild foot infections (University of Texas grades 2A, 2B). It is recommended that after the wound is healed, offloading should continue for a further four weeks to enable the scar tissue to firm up.
Wound dressings are important to keep the ulcer clean, but the placement of a large dressing on a wound may lead the patient to a false sense of security by believing that dressing an ulcer is curative. Nothing could be further from the truth in the neuropathic ulcer. Unfortunately, there is little evidence from randomized controlled trials that any dressing is superior to another. Indeed Jeffcoate and colleagues 7 randomized patients to one of three dressings and could find no difference in outcome according to dressing used: the only difference was in cost. Thus, without an evidence-base, there is no indication to use some of the newer more expensive dressings.
If part of the toes or foot become severely damaged, causing areas of dead tissue (gangrene), partial or complete amputation may be required. Amputation is reserved for patients who do not heal despite aggressive treatment, or whose health is threatened by the gangrene. Untreated gangrene can be life threatening.
Some patients with severe foot ulcers and peripheral vascular disease (poor circulation) may require a procedure to restore blood flow to the foot. If your ulcer is not healing and your circulation is poor, your health care provider may need to refer you to a vascular surgeon.
Keeping off your feet is very important. Walking on an ulcer can make it get larger and force the infection deeper into your foot. Your health care provider may put a special shoe, brace, or cast on your foot to protect it.
After the foot ulcer heals, treat your foot carefully. Scar tissue under the healed wound will break down easily. You may need to wear special shoes after the ulcer is healed to protect this area and to prevent the ulcer from returning.
New treatments
Several experimental approaches are being evaluated for the treatment of diabetic foot complications. New options include synthetic wound dressings, skin grown in a laboratory, substances that stimulate healing and support the growth of infection-fighting cells, electrical stimulation, and exposure to elevated oxygen levels.
For people with diabetes, foot complications are an ever-present risk. However, it is possible to design a plan for keeping the feet as healthy as possible. It is important to learn as much as possible about diabetic foot care and to take an active role in medical decisions and care. While routine medical exams are important, everyday foot care plays the biggest role in preventing foot complications before they start.
Hyperbaric Oxygen in the Diabetic Foot
Hyperbaric oxygen has been promoted as an effective treatment in diabetic foot wounds over many years 8. However, early randomized clinical trials have been criticized because of the small numbers of patients enrolled, and methodological and reporting inadequacies. A well designed and blinded randomized clinical trial was conducted in Sweden some years ago suggesting the benefit of hyperbaric oxygen in chronic neuro-ischemic infected foot ulcers with no possibility of revascularization 9. More recently, there have been two negative studies including a large retrospective cohort trial 10 and a multi-center Canadian study that showed no benefits of hyperbaric oxygen whatsoever in any patient group 11. Thus, at present, the use of hyperbaric oxygen in any diabetic foot wound has few data to support its efficacy. A multi-centre trial is underway in the Netherlands which will be the largest trial ever performed for the use of hyperbaric oxygen in diabetic foot ulcers; results should be available by late 2017 12.
Negative Pressure Wound Therapy
The application of negative pressure wound therapy is believed to accelerate healing through reducing edema, removal of exudate, increased perfusion, self-proliferation and the formation of granulation tissue 13. Randomized clinical trials have suggested efficacy in rates of wound healing and reduced amputations, with the application of Negative Pressure Wound Therapy in both post-surgical and non-surgical chronic non-healing ulcers 14. A recent systematic review confirmed that there was some evidence to support the use of Negative Pressure Wound Therapy in post-operative wounds 15.
Diabetic foot infection
Foot wounds must not be ignored by those with diabetes as there are very serious consequences if foot wounds do not heal properly. A wound which does not heal properly and is left exposed may form a foot ulcer which further raises the risk of an infection occurring. Indeed, if a wound becomes infected, amputation is a very real prospect if medical attention is not received quickly, as a result of severe complications like gangrene.
Gangrene
Gangrene is a serious medical condition that comes in two type, known as “wet” and “dry” gangrene. They are caused by bacterial infections or pre-existing health-issues respectively. Unfortunately, diabetics are at risk of both types.
Gangrene is caused by a lack of blood flow to a certain part of the body, and so diabetes can cause “dry” gangrene by destroying blood vessels. Diabetics can also be at risk of the infections that destroy blood vessels or block off blood flow due to swelling because they have a weakened immune system.
The common signs of gangrene include:
- Redness in the affected area, which can then become brown or black
- Pain evolving into numbness
Dry gangrene and diabetes
Dry gangrene is the type of gangrene that can occur as a complication of a pre-existing health condition, including type 1 and type 2 diabetes.
As a result of damage to the blood vessels throughout the body due to prolonged hyperglycemia, it is possible for blood circulation to be cut off. Blood carries oxygen and nutrients to the tissue around the body and so without it, the tissue will eventually die.
This usually happens in the extremities first, in the toes, feet and fingers.
Wet gangrene and diabetes
Gangrene that is caused by an infection of some sort is known as wet gangrene. It occurs after an injury that gets infected, such as a burn or frostbite.
Swelling from the body fighting off an infection can cause a loss of blood circulation that can starve a section of the body of oxygen and nutrients and cause gangrene.
This type of gangrene is more of a threat to people with diabetes who have an impaired immune system as their bodies are less able to fight off bacteria, viruses and other types of infection.
Furthermore, gangrene infections can occur at the site of foot ulcers, which is a common complication of both type 2 and type 1 diabetes.
Wet gangrene is the more rapid of the two types and can lead to septic shock.
Treating gangrene
Extreme cases of gangrene may have to result in amputation, which is why it is important to be aware of the signs of gangrene so that it can be treated at an early stage.
Other methods of treating less severe cases include:
- Surgery – Gangrene can be treated via surgery by reconstructing the damaged blood vessels or bypassing them.
- Antibiotics – Antibiotic medication may be used to kill off the infection if it is caught early enough to avoid damage to the tissue.
- Hyperbaric oxygen therapy – Forcing oxygen into the damaged cells via a hyperbaric chamber and an oxygen hood over the damaged section stimulates healing and healthy cells.
- Maggot treatment – This has been proven to be very effective as maggots eat dead flesh and release bacteria killing secretions that help to fight the infection.
Diabetic foot infection symptoms
The following symptoms at the site of the wound may indicate that the foot has become infected:
- Swelling
- Reddening of white skin, darkening of brown or black skin
- You may experience increasing amount of pain
- Skin feels warm to the touch
- The appearance of pus
Infection may be accompanied by other symptoms including:
- Having a high temperature
- Swollen glands
- Feeling lethargic and unwell
If you notice these signs arrange to see your doctor or diabetic health team within a day and if this is not possible, visit your emergency department.
Diabetic foot infection treatment
Appropriate wound debridement and offloading together with antibiotics are important in the management of the infected neuropathic foot ulcer, although there are few data from randomized trials to guide the prescriber 16. There is however no evidence that clinically non-infected neuropathic ulcers warrant treatment with antibiotics. With respect to choice of antibiotic therapy, the 2012 Infectious Diseases Society of America Clinical Practice Guideline 17. Commonly used broad-spectrum antibiotics include Clindamycin, Cephalexin, Ciprofloxacin and the Amoxycillin – Clavulanate potassium. Oral antibiotics usually suffice for mild infections, whereas more severe infections including cellulitis and osteomyelitis require intravenous antibiotic usage initially. Care should also be taken to optimize blood sugar control, as hyperglycemia impairs leucocyte (a type of white blood cell) function.
The above statements on antibiotics refer to initial treatment: after starting with such broad spectrum antibiotics, when the results of cultured deep tissue specimens are available, antibiotic therapy should be targeted at the likely primary infective organisms. Finally, with respect to duration of antibiotics, there are no data available from randomized trials to help guide the practitioner. Antibiotics should be continued until clinical signs of infection have resolved, but there is no indication to continue antibiotics beyond this period of time and certainly no indication to continue until the wound has healed. A recent review by Lipsky 18 has identified the challenges facing us due to the increasing threat of multidrug-resistant pathogens.
Osteomyelitis
Although the treatment of osteomyelitis has traditionally been surgical, there is increasing evidence from case series and a randomized controlled trial, that osteomyelitis localized to one or two bones, such as digits, may successfully be treated with antibiotics alone 19. A randomized trial from Spain showed that antibiotics alone were not inferior to localized surgery 19. Again, with respect to duration of antibiotic therapy for osteomyelitis, there is no evidence-base to guide us though a recent trial suggests that six weeks’ antibiotic therapy for non-surgically treated diabetic foot osteomyelitis may be sufficient: traditionally, up to three months has been recommended 20.
Diabetic foot care
It’s especially important to look after your feet if you have diabetes. Here’s how to take care of your feet and advice on when to get professional help.
Diabetes can reduce the blood supply to your feet and cause a loss of feeling known as peripheral neuropathy. This can mean foot injuries don’t heal well and you may not notice if your foot is sore or injured. The risk of complications can be greatly reduced if you’re able to bring your blood sugar levels under control. Ensure that your blood pressure and cholesterol levels are also monitored and controlled with medication if needed.
10 simple steps to prevent diabetic foot problems
If you want a few pointers on looking after your feet, then take our simple steps to healthy feet:
- Get help to quit smoking. Smoking makes it harder for blood to travel around your body (like to your feet) so puts you at even greater risk of amputation. Your healthcare team can make it easier to quit.
- Manage your blood sugars, cholesterol and blood pressure. By lowering high amounts of sugar in your blood will help prevent nerve damage and can stop things getting worse. Ask your diabetes team about the different ways they can help.
- Check your feet every day. If you see any color changes, swelling, pain, cuts or bruises, build-up of hard skin, or anything unusual tell your diabetes team.
- Eat a healthy, balanced diet and stay active
- Watch out cutting your toenails. If your body can’t heal itself properly any kind of wound can increase the chances of a serious foot problem so cut your nails carefully. Don’t cut down the side of your nails to avoid ingrowing toenails.
- Make sure your footwear fits. Blisters can be dangerous for people with diabetes. If your shoes are too tight, too loose or rub you then don’t wear them. Even if they look great.
- Use moisturizing cream every day
- Don’t use blades or corn-removing plasters. These can damage your skin and cause more problems for your feet. If you have corns a healthcare professional should deal with them.
- Get expert advice
- Keep useful numbers handy
Foot care tips if you have diabetes:
- See a podiatrist at least once a year. Ask your doctor for a referral or find a local podiatrist.
- Keep your feet clean and free from infection.
- Wear shoes that fit well and don’t squeeze or rub. Ill-fitting shoes can cause corns and calluses, ulcers and nail problems.
- Never walk barefoot, especially in the garden or on the beach on holidays, to avoid cuts and try to avoid sitting with your legs crossed so you don’t constrict your blood circulation.
- Cut or file your toenails regularly.
- Get corns or hard skin treated by a podiatrist.
Stop smoking to protect your feet
- If you have diabetes, it’s important to try to stop smoking. Smoking impairs the blood circulation, particularly in people with diabetes. It can seriously worsen foot and leg problems.
Eat a healthy, balanced diet and keep active
You should also aim to eat a healthy, balanced diet and keep active if you have diabetes. This can help you to manage your diabetes and reduce the risk of getting problems with your feet and legs.
Check your feet every day
You may have foot problems, but feel no pain in your feet. Checking your feet each day will help you spot problems early before they get worse. A good way to remember is to check your feet each evening when you take off your shoes. Also check between your toes. If you have trouble bending over to see your feet, try using a mirror to see them, or ask someone else to look at your feet.
Diabetic foot exam
Look for problems such as:
- cuts, sores, or red spots
- swelling or fluid-filled blisters
- ingrown toenails, in which the edge of your nail grows into your skin
- corns or calluses, which are spots of rough skin caused by too much rubbing or pressure on the same spot
- plantar warts, which are flesh-colored growths on the bottom of the feet
- athlete’s foot (tinea pedis of fungal foot infection)
- warm spots
If you have certain foot problems that make it more likely you will develop a sore on your foot, your doctor may recommend taking the temperature of the skin on different parts of your feet. A “hot spot” can be the first sign that a blister or an ulcer is starting.
Cover a blister, cut, or sore with a bandage. Smooth corns and calluses as explained below.
Wash your feet every day
Wash your feet with soap in warm, not hot, water. Test the water to make sure it is not too hot. You can use a thermometer (90° to 95° F is safe) or your elbow to test the warmth of the water. Do not soak your feet because your skin will get too dry.
After washing and drying your feet, put talcum powder or cornstarch between your toes. Skin between the toes tends to stay moist. Powder will keep the skin dry to help prevent an infection.
Smooth corns and calluses gently
Thick patches of skin called corns or calluses can grow on the feet. If you have corns or calluses, talk with your foot doctor about the best way to care for these foot problems. If you have nerve damage, these patches can become ulcers.
If your doctor tells you to, use a pumice stone to smooth corns and calluses after bathing or showering. A pumice stone is a type of rock used to smooth the skin. Rub gently, only in one direction, to avoid tearing the skin.
DO NOT
- cut corns and calluses
- use corn plasters, which are medicated pads
- use liquid corn and callus removers
Cutting and over-the counter corn removal products can damage your skin and cause an infection.
To keep your skin smooth and soft, rub a thin coat of lotion, cream, or petroleum jelly on the tops and bottoms of your feet. Do not put lotion or cream between your toes because moistness might cause an infection.
Trim your toenails straight across
Trim your toenails, when needed, after you wash and dry your feet. Using toenail clippers, trim your toenails straight across. Do not cut into the corners of your toenail. Gently smooth each nail with an emery board or nonsharp nail file. Trimming this way helps prevent cutting your skin and keeps the nails from growing into your skin.
Have a podiatrist trim your toenails if:
- you cannot see, feel, or reach your feet
- your toenails are thick or yellowed
- your nails curve and grow into the skin
If you want to get a pedicure at a salon, you should bring your own nail tools to prevent getting an infection. You can ask your health care provider what other steps you can take at the salon to prevent infection.
Wear shoes and socks at all times
Wear shoes and socks at all times. Do not walk barefoot or in just socks – even when you are indoors. You could step on something and hurt your feet. You may not feel any pain and may not know that you hurt yourself.
Check the inside of your shoes before putting them on, to make sure the lining is smooth and free of pebbles or other objects.
Make sure you wear socks, stockings, or nylons with your shoes to keep from getting blisters and sores. Choose clean, lightly padded socks that fit well. Socks with no seams are best.
Wear shoes that fit well and protect your feet. Here are some tips for finding the right type of shoes:
- Walking shoes and athletic shoes are good for daily wear. They support your feet and allow them to “breathe.”
- Do not wear vinyl or plastic shoes, because they do not stretch or “breathe.”
- When buying shoes, make sure they feel good and have enough room for your toes. Buy shoes at the end of the day, when your feet are the largest, so that you can find the best fit.
- If you have a bunion, or hammertoes, which are toes that curl under your feet, you may need extra-wide or deep shoes.1 Do not wear shoes with pointed toes or high heels, because they put too much pressure on your toes.
- If your feet have changed shape, such as from Charcot’s foot, you may need special shoes or shoe inserts, called orthotics. You also may need inserts if you have bunions, hammertoes, or other foot problems.
When breaking in new shoes, only wear them for a few hours at first and then check your feet for areas of soreness.
Medicare Part B insurance and other health insurance programs may help pay for these special shoes or inserts. Ask your insurance plan if it covers your special shoes or inserts.
Protect your feet from hot and cold
If you have nerve damage from diabetes, you may burn your feet and not know you did. Take the following steps to protect your feet from heat:
- Wear shoes at the beach and on hot pavement.
- Put sunscreen on the tops of your feet to prevent sunburn.
- Keep your feet away from heaters and open fires.
- Do not put a hot water bottle or heating pad on your feet.
Wear socks in bed if your feet get cold. In the winter, wear lined, waterproof boots to keep your feet warm and dry.
Keep the blood flowing to your feet
Try the following tips to improve blood flow to your feet:
- Put your feet up when you are sitting.
- Wiggle your toes for a few minutes throughout the day. Move your ankles up and down and in and out to help blood flow in your feet and legs.
- Do not wear tight socks or elastic stockings. Do not try to hold up loose socks with rubber bands.
- Be more physically active. Choose activities that are easy on your feet, such as walking, dancing, yoga or stretching, swimming, or bike riding.
- Stop smoking.
Smoking can lower the amount of blood flow to your feet. If you smoke, ask your healthcare provider for help to stop.
Get a foot check at every health care visit
Ask your health care team to check your feet at each visit. Take off your shoes and socks when you’re in the exam room so they will remember to check your feet. At least once a year, get a thorough foot exam, including a check of the feeling and pulses in your feet.
Get a thorough foot exam at each health care visit if you have:
- changes in the shape of your feet
- loss of feeling in your feet
- peripheral artery disease
- had foot ulcers or an amputation in the past1
Ask your health care team to show you how to care for your feet.
References- Boulton AJM. The Diabetic Foot. [Updated 2016 Oct 26]. In: De Groot LJ, Chrousos G, Dungan K, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK409609
- Shen W, Wukich D. Orthopedic surgery and the diabetic Charcot foot. Med Clin North Am 2013; 97; 873-882.
- Armstrong DG, Lavery LA, Harkless LB. Validation of a diabetic wound classification system. The contribution of depth, infection, and ischemia to risk of amputation. Diabetes Care 1998; 21: 855-859.
- Oyibo S, Jude EB, Tarawneh I, et al. A comparison of two diabetic foot ulcer classification systems: the Wagner and the University of Texas wound classification system. Diabetes Care 2001; 24: 84-88.
- Boulton AJM. Diabetic neuropathy and foot complications. Handb Clin Neurol 2014; 126: 96-107.
- Katz IA, Harlan A, Miranda-Palma B, et al. A randomized trial of two irremovable offloading devices in the management of plantar neuropathic diabetic foot ulcers. Diabetes Care 2005; 28: 555-559.
- Jeffcoate WJ, Price PE, Phillips CJ, et al. Randomized controlled trial of the use of three dressing preparations in the management of chronic ulceration of the foot in diabetes. Health Technol Assess 2009; 13: 1-86.
- Markakis K, Bowling FL, Boulton AJM. The diabetic foot in 2015: an overview. Diabetes Metab Res Rev 2016; 32 (suppl 1): 169-178.
- Londahl M, Katzman P, Nilsson A, et al. Hyperbaric oxygen therapy facilitates healing of chronic foot ulcers in patients with diabetes. Diabetes Care 2010; 33: 998-1003.
- Margolis DJ, Gupta J, Hoffstad O, et al. Lack of effectiveness of hyperbaric oxygen therapy for the treatment of diabetic foot ulcer and the prevention of amputation: a cohort study. Diabetes Care 2013; 36: 1961-1966.
- Fedorko L, Bowen JM, Jones W, et al. Hyperbaric oxygen therapy does not reduce indications for amputation in patients with diabetes with non-healing ulcers of the lower limb: a prospective, double-blind, randomized controlled clinical trial. Diabetes Care 2016; 39; 392-399.
- Stoekenbroek RM, Santema TB, Koelemay MJ, et al. Is additional hyperbaric oxygen therapy cost-effective for treating ischemic diabetic ulcers? Study protocol for the Dutch DAMOCLES multicentre randomized clinical trial. J Diabetes 2015; 7: 125-132.
- Isaac AL, Armstrong DG. Negative pressure wound therapy and other new therapies for diabetic foot ulceration: the current state of play. Med Clin North Amer 2013; 97: 899-909.
- Blume PA, Walters J, Payne W, et al. Comparison of negative pressure wound therapy using vacuum-assisted closure with advanced moist wound therapy in the treatment of diabetic foot ulcers: a multicenter, randomized controlled trial. Diabetes Care 2008; 31: 631-636.
- Game FL, Apelqvist J, Attinger C, et al. Effectiveness of interventions to enhancehealing of chronic ulcers of the foot in diabetes: a systematic review. Diabetes Metab Res Rev 2016; 32 (suppl 1): 154-168.
- Lipsky BA, Aragón-Sánchez J, Diggle M, et al. IWGDF guidance on the diagnosis and management of foot infections in persons with diabetes. Diabetes Metab Res Rev 2016; 32 (suppl 1): 45-74.
- Lipsky BA, Berendt AR, Cornia PB, et al. 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis 2012; 54: e132-173
- Lipsky BA. Diabetic foot infections: current treatment and delaying the “post-antibiotic era”. Diabetes Metab Res Rev 2016; 32 (suppl 1): 246-253.
- Lázaro-Martinez JL, Aragón-Sánchez J, Garcia-Morales C. Antibiotics versus conservative surgery for treating diabetic foot osteomyelitis: a randomized comparative trial. Diabetes Care 2014; 37: 789-795.
- Tone A, Nguyen S, Devemy F, et al. Six-week versus twelve-week antibiotic therapy for non-surgically treated diabetic foot osteomyelitis: a multicentre open-label controlled randomized study. Diabetes Care 2015; 38: 302-307.