Discoid meniscus
Discoid meniscus is an abnormal meniscus that is thicker than normal and has a different shape and texture that usually affects the lateral meniscus of the knee 1. Healthy meniscus is shaped like crescent moons (in fact, “meniscus” comes from the Greek word for crescent). A discoid meniscus is thicker than normal, and often oval or disc-shaped. It is more prone to injury than a normally shaped meniscus. Usually a person with discoid meniscus has no complaints; however, discoid meniscus may present as pain, swelling, or a snapping sound heard from the affected knee. Strong suggestive findings on magnetic resonance imaging includes a thickened meniscal body seen on more than two contiguous sagittal slices.
Discoid meniscus is more likely to be injured than a normally shaped meniscus. There are people who will have a discoid meniscus and never experience an injury, but some people have problems because of it, usually during childhood. While a discoid meniscus is present from birth, injuries can occur with twisting motions to the knee, usually during pivoting motion or changes in direction while playing sports.
There is a greater incidence of discoid meniscus in Asian countries than in Western countries, and bilateral discoid menisci are also common 1. The discoid meniscus may be a congenital anomaly, and genetics or family history may play a role in the development of discoid menisci 1. After birth, no sudden change occurs in meniscal development 2.
Some authors have reported that magnetic resonance imaging (MRI) or arthroscopic evaluation reveals higher rates (79% to 97%) of bilateral discoid lateral meniscus in patients presenting with symptomatic unilateral discoid lateral meniscus 3.
People with discoid meniscus may go through their entire lives and never experience any problems. If a discoid meniscus does not cause pain or discomfort, no treatment is needed. Some people, however, will have knee problems related to the discoid meniscus. Symptoms often begin during childhood. When the discoid meniscus is causing pain, popping, or other problems a discoid meniscus is usually treated with surgery. The orthopedic surgeon will make a few small incisions around the knee and use a small camera and surgical instruments to treat the meniscus. These surgeries are done under anesthesia and patients are able to go home the same day.
After surgery, a knee brace or soft bandage is sometimes needed. A wheelchair or crutches may be useful for a short period of time. Physical therapy may be prescribed to regain mobility and strength following surgery.
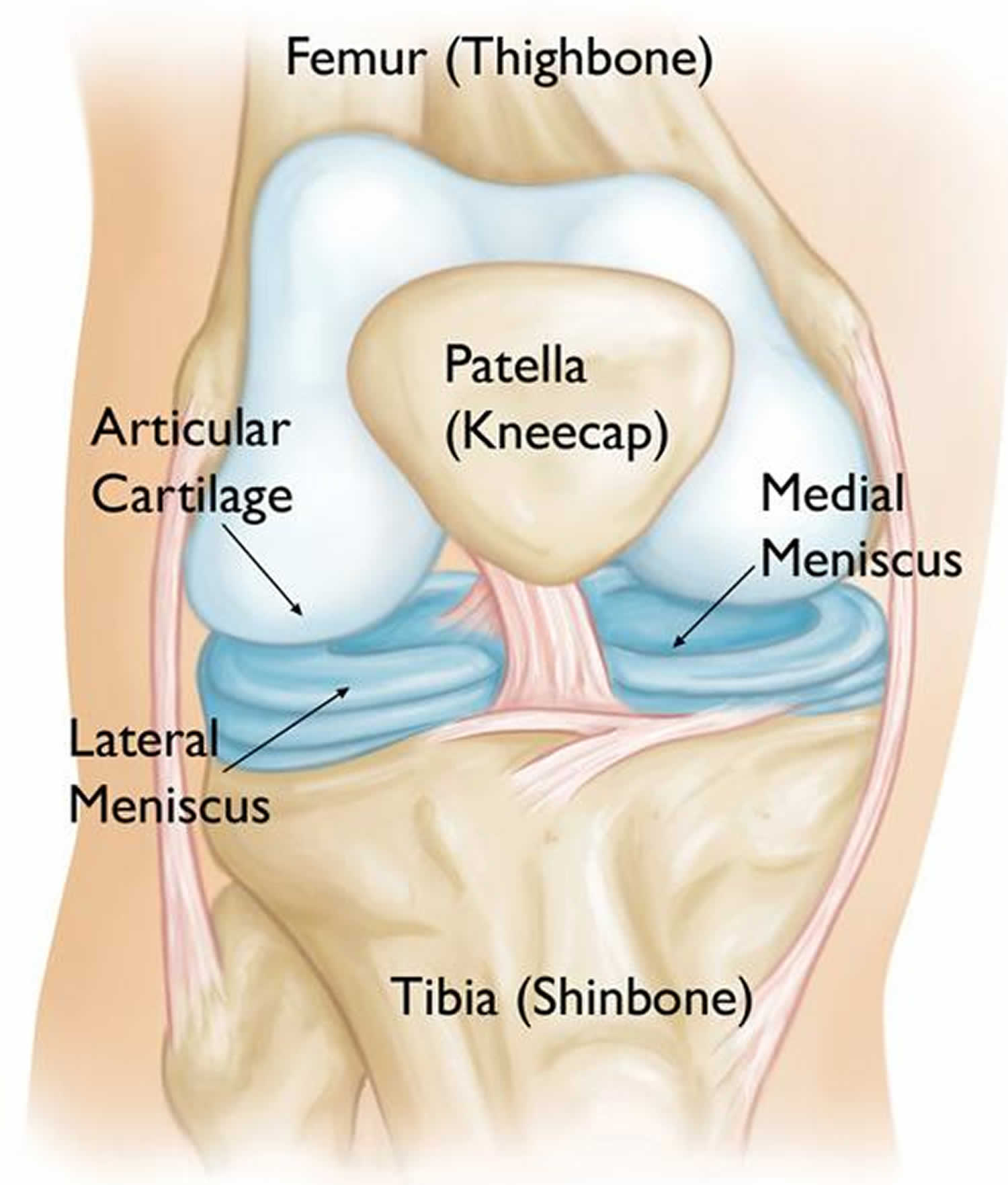
Meniscus anatomy
The menicus acts as a “shock absorber” between your femur (thighbone) and tibia (shinbone). It protects the thin articular cartilage that covers the ends of the bones and helps the knee to easily bend and straighten.
There are two menisci in the knee: the medial meniscus on the inside of the knee, and the lateral meniscus on the outside.
The menisci are attached to the femur bone by a strong tissue called the meniscofemoral ligament. This ligament also provides a blood supply to a small portion of the meniscus.
Figure 1. Meniscus anatomy
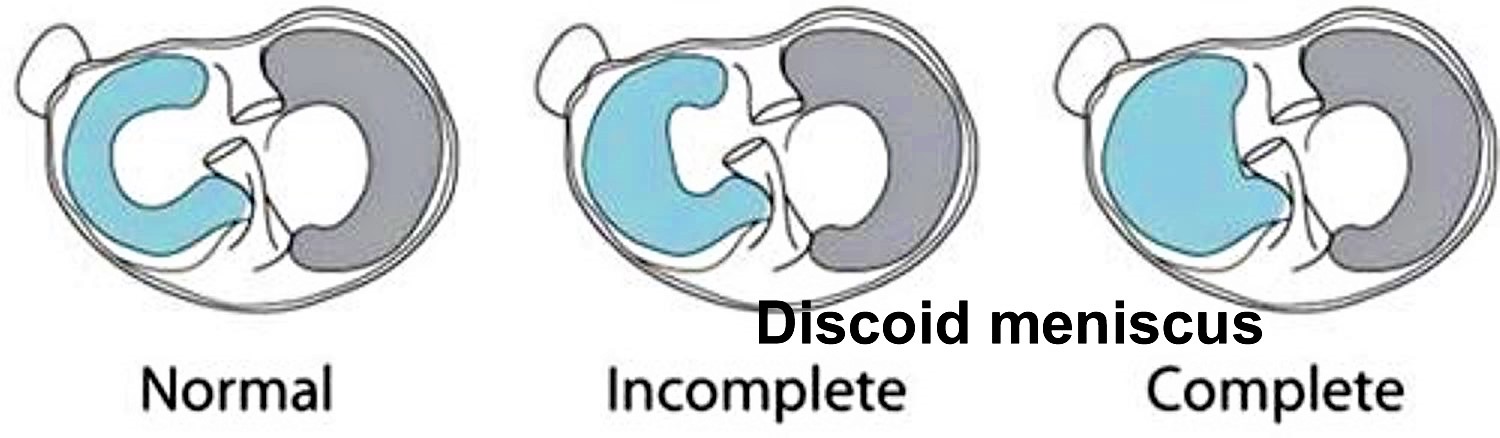
Discoid meniscus types
There are three types of discoid menisci 4:
- Incomplete. The incomplete type has a semilunar shape and normal posterior attachment, but it covers less than 80% of the lateral tibial plateau.
- Complete. The complete type is the disc-shaped meniscus that completely covers the lateral tibial plateau and has a normal posterior attachment.
- Hypermobile Wrisberg. The Wrisberg type is more normally shaped compared to the complete or incomplete type of discoid meniscus, but it lacks the usual posterior meniscal attachments (coronary ligament), and only the Wrisberg ligament connects the posterior horn of the lateral meniscus.
Each type presents its own unique pathophysiologic problems.
The Wrisberg type lacks an attachment to stabilize the posterior horn to the tibia 5. It may also be of normal shape rather than discoid. The only attachment of the posterior horn is to the Wrisberg or meniscofemoral ligament. The general configuration produces an unstable or hypermobile lateral meniscus.
Figure 2. Discoid meniscus
Footnote: Discoid meniscus most often affects the lateral meniscus, which is the on the outside of the knee joint. Cross-section views of incomplete and complete discoid menisci.
Discoid meniscus cause
The cause of discoid meniscus is not known. It is a congenital (present at birth) defect.
Smillie 6 suggested that the discoid meniscus is congenital. The discoid shape is an intermediate stage during fetal development, and final discoid morphology results from absorption failure of the central part of the menisci. However, the discoid shape has not yet been identified in anatomical studies on either human or animal embryos 7. The discoid meniscus may indeed be a congenital anomaly 8, and genetic or familial factors may play a role in the development of discoid menisci 9. Some authors have reported bilateral discoid menisci in identical female twins 10 or in a family of three brothers and sisters 11. The histology and ultrastructure of discoid meniscus is different from that of normal meniscus. The discoid meniscus is characterized by decreased collagen fibers and loss of normal collagen orientation, and intrameniscal mucoid degeneration is also common 12. Papadopoulos et al. 13 documented significant disorganization of the circular collagen network and a heterogeneous course of the circumferentially arranged collagen fibers in discoid meniscus structure. They also proposed that the discoid lesion is a structural rather than a morphological variant. In addition to structural abnormality, the increased thickness and abnormal vascularity of the discoid meniscus makes it prone to tearing 14. Morphological changes may also occur to compensate for an abnormally unstable meniscus during development 15. Recently, some authors have reported regeneration after partial meniscectomy of the discoid meniscus 16. This regeneration supports the possibility that the discoid meniscus arises through variant morphogenesis 17.
Discoid meniscus symptoms
Sometimes kids with a torn discoid meniscus will feel:
- Pain
- Stiffness or swelling
- Unable to fully straighten the knee
- Catching, popping, or locking of the knee
- Buckling or “giving out” of the knee
Individuals with a discoid meniscus can be asymptomatic 18. If there is a tear or instability, symptoms typically develop in discoid meniscus 19. However, a click or pain can develop even in the absence of a tear or instability 20. Symptoms of discoid meniscus include insidious popping or snapping without a traumatic origin, which is associated with pain, giving way, effusion, quadriceps atrophy, limited range of motion, and clicking or locking 21. Snapping knee syndrome, in which a clunk is heard at the end of flexion, is usually related to an unstable meniscus variant, such as the Wrisberg type 22. In very young children (range, 3 to 4 years), snapping is often asymptomatic, whereas older children (range, 8 to 10 years) more commonly experience pain with activity 23. In addition, the older child may present with more acute symptoms than younger children 19. The most common tear pattern of the discoid meniscus is a horizontal tear 24. Repetitive microtrauma to the abnormal collagen arrangement is thought to cause horizontal tears after mucoid degeneration 25.
Discoid meniscus injuries
A discoid meniscus is more prone to injury than a normal meniscus. The thick, abnormal shape of a discoid meniscus makes it more likely to get stuck in the knee or tear. If the meniscofemoral ligament attachment to the femur is also missing, the risk for injury is even greater. Injuries to the discoid meniscus often occur with twisting motions to the knee, such as during sports that require pivoting or fast changes in direction.
Once injured, even a normal meniscus is difficult to heal. This is because the meniscus lacks a strong blood supply and the nutrients that are essential to healing cannot reach the injured tissues.
In many cases of discoid meniscus, patients experience symptoms without there being any injury to the meniscus.
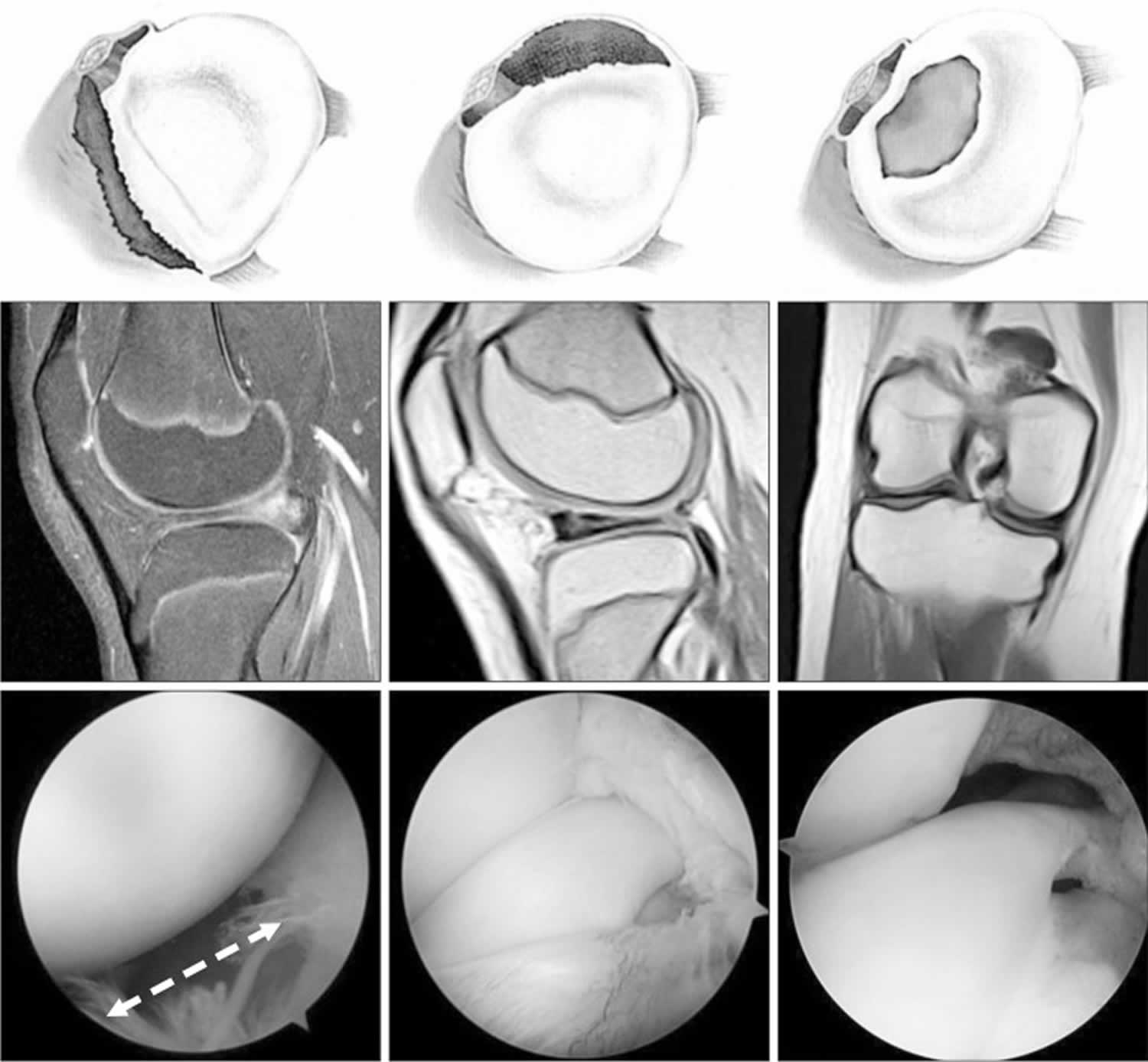
Figure 3. Discoid meniscus tear
Footnote: Magnetic resonance imaging findings and arthroscopic views of the discoid meniscus according to the corresponding tear pattern. A peripheral tear refers to a longitudinal tear in the meniscocapsular junction area, anterior horn (posterocentral shift, left column), and posterior horn (anterocentral shift, middle column). The white dotted arrow (bottom, left column) shows the wide gap between the anterolateral border of the meniscus and the joint capsule. Posterolateral corner loss refers to the absence of the posterolateral portion of the discoid meniscus due to degenerative tears around the popliteal hiatus (central shift).
[Source 1 ]Discoid meniscus diagnosis
After discussing your child’s medical history and any events that occurred before symptoms started, your doctor will examine your child’s knee.
Your child may or may not have tenderness where the bones meet.
To test for discoid meniscus, your doctor will twist your child’s knee with the knee bent and straightened. In many cases of discoid meniscus, there is a popping or clunking sensation. This can sometimes even be heard. In extreme cases, part of the meniscus will pop out of the knee joint and can be seen right under the skin.
Imaging tests
- X-rays. Although x-rays do not show tears of soft tissues like the meniscus, they can show whether there are other problems in the knee. In addition, because the discoid meniscus is so thick, the space between the femur and tibia on the lateral part of the knee may appear widened on an x-ray.
- Magnetic resonance imaging (MRI) scan. This study can create detailed images of the soft tissues of the knee joint and is the best imaging test for discoid meniscus. The MRI can show the abnormal shape of the discoid meniscus, as well as tears within the meniscus. However, the rare Wrisberg type of discoid meniscus cannot be tested with an MRI scan because the problem only occurs when the patient is moving. An MRI study involves lying still for 30-45 minutes. Many young patients require some sedation or anesthesia to complete the test.
Radiographs are often normal in patients with a discoid meniscus; however, they may reveal some radiologic features of discoid meniscus, such as widening of the lateral joint space, a squared-off appearance of the lateral femoral condyle, cupping of the lateral tibial plateau, elevation of the fibular head, and tibial eminence flattening 8. On MRI, a discoid meniscus can be diagnosed when the ratio of the minimal meniscal width to the maximal tibial width is more than 20% on the coronal image, and the ratio of sum of the width of both lateral horns to the maximal meniscal diameter on the sagittal image is more than 75% 26. Araki et al. 27 have proposed that the discoid meniscus is present when the meniscal width is over 15 mm on the coronal slice. Continuity of the meniscus between the anterior and posterior horns on three or more 5-mm thick consecutive sagittal slices demonstrates the presence of a discoid meniscus 28. An abnormal, thickened, bow-tie appearance of the meniscus is suggestive of discoid meniscus 19. In the Wrisberg variant, an MRI scan may show subtle anterior subluxation of the posterior horn of the lateral meniscus or high T2-weighted signal intensity, simulating a peripheral tear 29. However, some authors have reported low sensitivity in detecting the lateral discoid meniscus in children and have suggested that MRI does not provide enhanced diagnostic utility over clinical examination 30 because checking the stability of a discoid meniscus on an MRI scan is difficult, and some incomplete discoid menisci often look normal 31. Nonetheless, MRI is useful in detecting the presence of meniscus tear and a shift of the meniscus. This information can aid the surgeon in determining the appropriate surgical technique, such as saucerization or repair 32. Diagnostic arthroscopy may be needed to confirm the diagnosis of discoid meniscus in a symptomatic patient with instability or with the Wrisberg variant, showing a normal shape and MRI appearance 18. On physical examination, patients show joint line tenderness, effusion, joint line bulging, and even a positive McMurray test 33. The accuracy of physical examination ranges from 29% to 93% and varies according to the examiner’s experience and knowledge of this anomaly 34.
Discoid meniscus treatment
People with discoid meniscus may go through their entire lives and never experience any problems. If a discoid meniscus does not cause pain or discomfort, no treatment is needed. Some people, however, will have knee problems related to the discoid meniscus. Symptoms often begin during childhood. When the discoid meniscus is causing pain, popping, or other problems a discoid meniscus is usually treated with surgery. The orthopedic surgeon will make a few small incisions around the knee and use a small camera and surgical instruments to treat the meniscus. These surgeries are done under anesthesia and patients are able to go home the same day.
After surgery, a knee brace or soft bandage is sometimes needed. A wheelchair or crutches may be useful for a short period of time. Physical therapy may be prescribed to regain mobility and strength following surgery.
Discoid meniscus surgery
Knee arthroscopy is one of the most commonly performed orthopaedic surgical procedures. During knee arthroscopy, the surgeon makes a few small incisions around the knee and inserts a small camera, called an arthroscope, into the joint. The camera displays pictures on a television screen, and the surgeon uses these images to guide miniature surgical instruments.
Most arthroscopic surgeries are done on an outpatient basis. Patients usually go home a few hours after the procedure.
- Anesthesia. To prevent pain during the procedure, the patient is given anesthesia. There are different types of anesthesia: Local and regional types of anesthesia numb just parts of the body, and the patient remains awake. General anesthesia puts the patient to sleep. Most children are given general anesthesia for arthroscopic surgery.
Surgical procedure
Treatment will depend upon the type of discoid meniscus.
- Complete and incomplete discoid menisci with no tears are typically treated with saucerization, a procedure in which the meniscus is cut and re-shaped into a crescent.
- If the discoid meniscus is also torn, the surgeon may perform a saucerization and then trim away the torn portion. Some tears can be repaired with stitches, rather than removed.
- The hypermobile Wrisberg form of discoid meniscus is saucerized if necessary, then stabilized with stitches to sew the meniscus to the lining of the joint.
Discoid meniscus surgery recovery
Most patients return to normal daily activities after arthroscopy for a discoid meniscus. However, if the entire meniscus was removed, there is a risk for continued pain and, potentially, early arthritis.
Surgeons sometimes recommend that patients avoid sports that overstress the knee with cutting type movements. These include soccer, tennis, basketball, and football.
Rehabilitation
After surgery, your doctor may put your child’s knee in a brace or a soft bandage wrap. He or she may need to use crutches for a short period of time. Very young children may need a wheelchair for several weeks because they do not have the balance or strength to use crutches.
Once the initial healing is complete, your doctor may prescribe physical therapy exercises to restore strength and mobility. These may be done at home or with a physical therapist.
Discoid meniscus prognosis
In a retrospective study of 40 children with symptomatic lateral discoid meniscus, miniarthrotomy and arthroscopy were compared. Miniarthrotomy was found to provide slightly better results than arthroscopic resection with regard to functional outcome. The authors recommended miniarthrotomy for the resection of lateral discoid meniscus, particularly in young children with narrow joint spaces and for surgeons who are not familiar with arthroscopy in small joints 35.
Ahn et al 36 evaluated the long-term clinical and radiographic results of arthroscopic reshaping, with or without peripheral meniscus repair, in 38 children (48 knees; mean age, 9.9 years) with symptomatic discoid lateral meniscus. The surgical procedure performed was arthroscopic partial meniscectomy alone (22 knees), partial meniscectomy with repair (18 knees), or subtotal meniscectomy (8 knees). At a mean follow-up of 10.1 years, progression of degenerative changes was significantly greater in the group treated with subtotal meniscectomy than in either of the partial meniscectomy groups.
Lee et al 37 carried out a systematic review of 11 studies with more than 5 years of follow-up in which the clinical and radiologic outcomes of surgical treatment of discoid lateral meniscus (open or arthroscopic partial central meniscectomy, subtotal meniscectomy, total meniscectomy, or partial meniscectomy with repair) were evaluated. Most of the studies showed good clinical results. There was minimal progression of degenerative change and no findings of moderate or advanced degenerative changes. Possible risk factors for degenerative changes included greater age at the time of surgery, longer follow-up period, and subtotal or total meniscectomy.
In a meta-analysis aimed at comparing clinical and radiographic results between partial and total meniscectomy in patients with symptomatic discoid lateral meniscus, Lee et al 38 found that radiographic outcomes were better with partial meniscectomy with or without repair than with total meniscectomy but that clinical outcomes were comparable for the two procedures. These findings suggest that meniscal preservation may be a better option than total meniscectomy for symptomatic discoid lateral meniscus.
References- Kim JG, Han SW, Lee DH. Diagnosis and Treatment of Discoid Meniscus. Knee Surg Relat Res. 2016;28(4):255–262. doi:10.5792/ksrr.16.050 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5134787
- Clark CR, Ogden JA. Development of the menisci of the human knee joint. Morphological changes and their potential role in childhood meniscal injury. J Bone Joint Surg Am. 1983 Apr. 65 (4):538-47.
- Bae JH, Lim HC, Hwang DH, Song JK, Byun JS, Nha KW. Incidence of bilateral discoid lateral meniscus in an Asian population: an arthroscopic assessment of contralateral knees. Arthroscopy. 2012;28:936–41. doi: 10.1016/j.arthro.2011.12.003
- Watanabe M, Takeda S, Ikeuchi H. Atlas of arthroscopy. 3rd ed. Tokyo: Igaku-Shoin; 1979. pp. 75–130.
- Kim EY, Choi SH, Ahn JH, Kwon JW. Atypically thick and high location of the Wrisberg ligament in patients with a complete lateral discoid meniscus. Skeletal Radiol. 2008 Sep. 37 (9):827-33.
- Smillie IS. The congenital discoid meniscus. J Bone Joint Surg Br. 1948;30:671–82.
- Clark CR, Ogden JA. Development of the menisci of the human knee joint. Morphological changes and their potential role in childhood meniscal injury. J Bone Joint Surg Am. 1983;65:538–47. doi: 10.2106/00004623-198365040-00018
- Kramer DE, Micheli LJ. Meniscal tears and discoid meniscus in children: diagnosis and treatment. J Am Acad Orthop Surg. 2009;17:698–707. doi: 10.5435/00124635-200911000-00004
- Yaniv M, Blumberg N. The discoid meniscus. J Child Orthop. 2007;1:89–96. doi: 10.1007/s11832-007-0029-1.
- Gebhardt MC, Rosenthal RK. Bilateral lateral discoid meniscus in identical twins. J Bone Joint Surg Am. 1979;61:1110–1. doi: 10.2106/00004623-197961070-00027
- de Lambilly C, Pascarel X, Chauvet JF, Marle JL, Honton JL. External discoid menisci: apropos of a familial series of 6 cases. Rev Chir Orthop Reparatrice Appar Mot. 1991;77:359–61.
- Atay OA, Pekmezci M, Doral MN, Sargon MF, Ayvaz M, Johnson DL. Discoid meniscus: an ultrastructural study with transmission electron microscopy. Am J Sports Med. 2007;35:475–8. doi: 10.1177/0363546506294678.
- Papadopoulos A, Kirkos JM, Kapetanos GA. Histomorphologic study of discoid meniscus. Arthroscopy. 2009;25:262–8. doi: 10.1016/j.arthro.2008.10.006.
- Clark CR, Ogden JA. Development of the menisci of the human knee joint. Morphological changes and their potential role in childhood meniscal injury. J Bone Joint Surg Am. 1983;65:538–47. doi: 10.2106/00004623-198365040-00018.
- Kaplan EB. Discoid lateral meniscus of the knee joint; nature, mechanism, and operative treatment. J Bone Joint Surg Am. 1957;39:77–87. doi: 10.2106/00004623-195739010-00008.
- Stein MI, Gaskins RB, 3rd, Nalley CC, Nofsinger C. Regeneration of a discoid meniscus after arthroscopic saucerization. Am J Orthop (Belle Mead NJ) 2013;42:E5–8.
- Bisicchia S, Tudisco C. Re-growth of an incomplete discoid lateral meniscus after arthroscopic partial resection in an 11 year-old boy: a case report. BMC Musculoskelet Disord. 2013;14:285. doi: 10.1186/1471-2474-14-285.
- Kelly BT, Green DW. Discoid lateral meniscus in children. Curr Opin Pediatr. 2002;14:54–61. doi: 10.1097/00008480-200202000-00010
- Kushare I, Klingele K, Samora W. Discoid meniscus: diagnosis and management. Orthop Clin North Am. 2015;46:533–40. doi: 10.1016/j.ocl.2015.06.007
- Francavilla ML, Restrepo R, Zamora KW, Sarode V, Swirsky SM, Mintz D. Meniscal pathology in children: differences and similarities with the adult meniscus. Pediatr Radiol. 2014;44:910–25. doi: 10.1007/s00247-014-3022-0
- Mutlu S, Mutlu H, Mutlu B, Guler O, Duymus TM. Symptoms of discoid lateral menisci. J Orthop. 2014;11:180–2. doi: 10.1016/j.jor.2014.06.005
- Wong T, Wang CJ. Functional analysis on the treatment of torn discoid lateral meniscus. Knee. 2011;18:369–72. doi: 10.1016/j.knee.2010.07.002
- Dickhaut SC, DeLee JC. The discoid lateral-meniscus syndrome. J Bone Joint Surg Am. 1982;64:1068–73. doi: 10.2106/00004623-198264070-00018
- Bellisari G, Samora W, Klingele K. Meniscus tears in children. Sports Med Arthrosc. 2011;19:50–5. doi: 10.1097/JSA.0b013e318204d01a
- Smith CF, Van Dyk GE, Jurgutis J, Vangsness CT., Jr Cautious surgery for discoid menisci. Am J Knee Surg. 1999;12:25–8.
- Samoto N, Kozuma M, Tokuhisa T, Kobayashi K. Diagnosis of discoid lateral meniscus of the knee on MR imaging. Magn Reson Imaging. 2002;20:59–64. doi: 10.1016/S0730-725X(02)00473-3
- Araki Y, Ashikaga R, Fujii K, Ishida O, Hamada M, Ueda J, Tsukaguchi I. MR imaging of meniscal tears with discoid lateral meniscus. Eur J Radiol. 1998;27:153–60. doi: 10.1016/S0720-048X(97)00044-2
- Silverman JM, Mink JH, Deutsch AL. Discoid menisci of the knee: MR imaging appearance. Radiology. 1989;173:351–4. doi: 10.1148/radiology.173.2.2798867
- Singh K, Helms CA, Jacobs MT, Higgins LD. MRI appearance of Wrisberg variant of discoid lateral meniscus. AJR Am J Roentgenol. 2006;187:384–7. doi: 10.2214/AJR.04.1785
- Kocher MS, DiCanzio J, Zurakowski D, Micheli LJ. Diagnostic performance of clinical examination and selective magnetic resonance imaging in the evaluation of intraarticular knee disorders in children and adolescents. Am J Sports Med. 2001;29:292–6
- Hart ES, Kalra KP, Grottkau BE, Albright M, Shannon EG. Discoid lateral meniscus in children. Orthop Nurs. 2008;27:174–9. doi: 10.1097/01.NOR.0000320545.35858.04
- Ahn JH, Lee YS, Ha HC, Shim JS, Lim KS. A novel magnetic resonance imaging classification of discoid lateral meniscus based on peripheral attachment. Am J Sports Med. 2009;37:1564–9. doi: 10.1177/0363546509332502
- Fleissner PR, Eilert RE. Discoid lateral meniscus. Am J Knee Surg. 1999;12:125–31.
- Stanitski CL. Correlation of arthroscopic and clinical examinations with magnetic resonance imaging findings of injured knees in children and adolescents. Am J Sports Med. 1998;26:2–6.
- Krause FG, Haupt U, Ziebarth K, Slongo T. Mini-arthrotomy for lateral discoid menisci in children. J Pediatr Orthop. 2009 Mar. 29 (2):130-6.
- Ahn JH, Kim KI, Wang JH, Jeon JW, Cho YC, Lee SH. Long-term results of arthroscopic reshaping for symptomatic discoid lateral meniscus in children. Arthroscopy. 2015 May. 31 (5):867-73.
- Lee YS, Teo SH, Ahn JH, Lee OS, Lee SH, Lee JH. Systematic Review of the Long-term Surgical Outcomes of Discoid Lateral Meniscus. Arthroscopy. 2017 Oct. 33 (10):1884-1895.
- Lee DH, D’Lima DD, Lee SH. Clinical and radiographic results of partial versus total meniscectomy in patients with symptomatic discoid lateral meniscus: A systematic review and meta-analysis. Orthop Traumatol Surg Res. 2019 Jun. 105 (4):669-675.