Eosinophilia myalgia syndrome
Eosinophilia-myalgia syndrome is a chronic multisystem disorder, characterized by peripheral eosinophilia, associated with muscle, nerve, fascia and skin involvement 1. According to the medical literature majority of the patients affected are caucasian females between 35–60 years old 2. Eosinophilia-myalgia syndrome was first described in 1989 in New Mexico, when approximately 1500 patients developed subacute onset of myalgias and peripheral eosinophilia 3. The patients then went on to have chronic muscle, fascia, nerve, and skin involvement. Eosinophilia myalgia syndrome also occurred in other parts of the world, including the United Kingdom, France, Israel, Japan (12 patients), western Germany (69 patients), and Canada (10 patients). Cohort studies performed during the epidemic estimated that the attack rate of eosinophilia myalgia syndrome among users of L-tryptophan was 0.5%-9%, depending on the product lot of the L-tryptophan ingested 3.
By July 1991, 31 deaths were attributed to eosinophilia myalgia syndrome. The mortality rate ranged from 2% in national surveillance data to 6% in some cohorts. Most deaths were the result of neurogenic complications such as ascending polyneuropathy, cardiopulmonary disease, or superimposed infection 4.
Of the patients with an acute presentation of eosinophilia myalgia syndrome, 34% required hospitalization for incapacitating myalgias, muscle cramps, or pulmonary involvement.
For the purpose of nationwide surveillance, the Centers for Disease Control and Prevention (CDC) defined eosinophilia myalgia syndrome as requiring the following criterias 5:
- Incapacitating myalgias
- Blood eosinophil count greater than 1000/µL
- No evidence of infection (ie, trichinosis) or neoplasm that could account for these findings
In 2001, new diagnostic criteria for eosinophilia myalgia syndrome were proposed that identified the following two patterns of presentation 5.
- Abrupt onset of peripheral eosinophilia, myalgia, and at least one of the following: rash, edema, pulmonary involvement, or neuropathy.
- One of the following occurring within 24 months of an acute illness: 1) fasciitis, neuropathy, and myalgia or muscle cramps OR 2) any three or more of: fasciitis, myopathy, neuropathy, or peripheral eosinophilia
Diagnosis with the new criteria requires exclusion of trichinosis, vasculitis, and infectious, allergic, neoplastic, or connective tissue disease that could explain the patient’s symptoms 5.
Toxoepidemiologic studies linked eosinophilia myalgia syndrome to dietary supplements containing L-tryptophan that had been manufactured using genetically engineered bacteria 6. The best characterized contaminant is 1,1-ethylidenebis (EBT), a tryptophan dimer.
Contamination with L-tryptophan may not be the only cause of eosinophilia myalgia syndrome. It is estimated that up to 14% of eosinophilia myalgia syndrome cases are not related to L-tryptophan 3. In these cases the symptoms are milder and the prognosis is better. Another similar entity is toxic oil syndrome that affected thousands of Spanish patients in 1981 and is associated with ingestion of adulterated rapeseed oil. The condition shares many clinical and histopatological features with eosinophilia myalgia syndrome. Biochemical data suggest that an impurity detected in L-tryptophan-3-(phenylamino)-alanine shares chemical properties with 3-(N-phenylamino)-1,2-propanediol, implicated in toxic oil syndrome epidemic. After the epidemic in late 1980s, the Food and Drug Administration (FDA) banned L-tryptophan containing products which were used as dietary supplements. The ban was lifted in 2005 and after that, only a few L-tryptophan-associated eosinophilia myalgia syndrome were reported 6.
There are no peer-reviewed guidelines for the standard of care of eosinophilia myalgia syndrome patients. Because of the variety and diversity of how eosinophilia myalgia syndrome manifests, patients are treated based on their individual symptoms and may be prescribed muscle relaxants, analgesics, and diuretics.
High doses of corticosteroids may help reduce inflammation, However, most researchers have concluded that this course of treatment does not reduce the severity or duration of eosinophilia myalgia syndrome symptoms 7.
In the acute phase, patients who have intense muscle pain and cramps may need to limit or avoid strenuous physical activity. Some patients have required hospitalization. In the chronic phase, patients who keep as physically active as possible seem to do better than others.
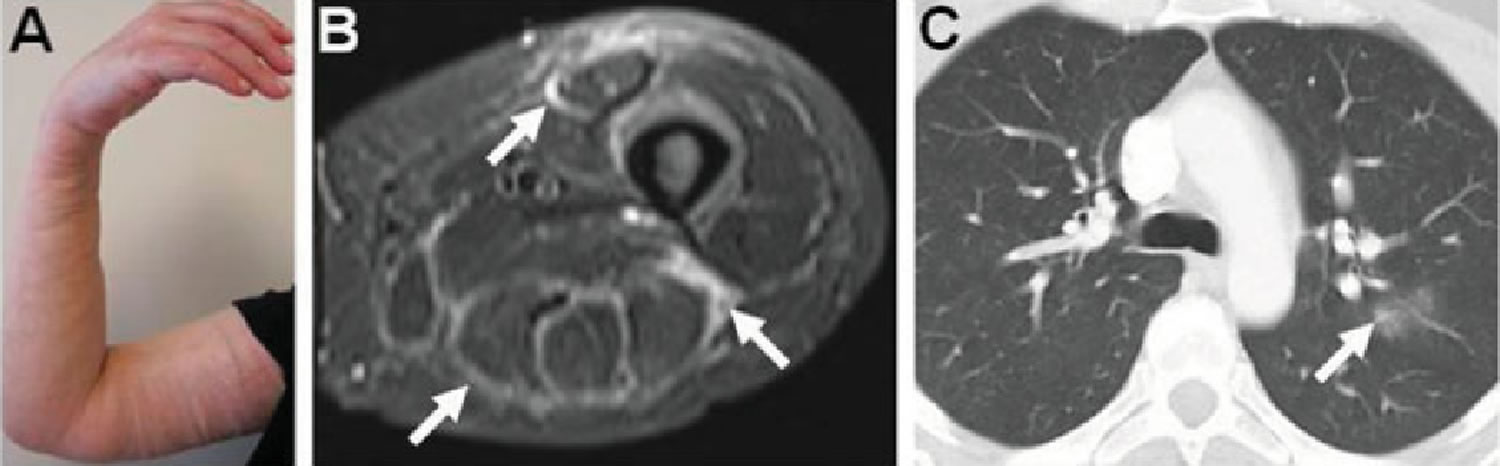
Figure 1. Eosinophilia–myalgia syndrome
Footnote: Clinical presentation of eosinophilia–myalgia syndrome. (A) Skin induration and edema were seen in the right arm; they were also present in the left upper and both lower extremities, with palpably thickened fascia. (B) Axial STIR sequence magnetic resonance images of the thigh revealed high signal intensity in the fascia surrounding the anterior and posterior compartment muscles (arrows). (C) High-resolution computed tomography of the chest showed ground-glass changes and air space opacity in the left lung (arrow).
[Source 8 ]Eosinophilia myalgia syndrome causes
Although no one cause of eosinophilia myalgia syndrome has been identified, most patients (97%) with this disease reported consuming L-tryptophan. The median exposure was 6 months, but this ranged from 2 weeks to 9 years. Doses vary from 500-11,500 mg per day, and the median dose patients consumed was 1250 mg. L-tryptophan is commonly used by patients with eosinophilia myalgia syndrome but also is taken for insomnia, depression, and premenstrual symptoms. One specific impurity identified in L-tryptophan was 1’1’-ethylidenebis[tryptophan] 3. But patients can develop eosinophilia myalgia syndrome without a history of drug or supplement use.
The exact pathogenesis of eosinophilia myalgia syndrome is still unknown. Pathohistological findings in eosinophilia myalgia syndrome are capillary endothelial cell hyperplasia, inflammatory cell infiltration (including monocytes, histiocytes, lymphocytes, macrophages and plasma cells), eosinophils in the nervous, muscle and connective tissue, along with increased fibrosis, mostly in the fascia, although fibrosis of the skin has also been described. In patients with eosinophilia myalgia syndrome, high levels of serum cytokines interleukin (IL)-2, IL-4, IL-5, interferon gamma and granulocyte-monocyte colony stimulating factor (GMCSF) have been reported. Increased deep dermis deposition of transforming growth factor beta (TGF-β) was described 6. A study involving subcutaneous quinolonic acid injections (an L-tryptophan metabolite) resulted in peripheral blood eosinophilia and subcutaneous lesions with increased TGF- β depositions resembling eosinophilic fasciitis 9. These data support a relationship between eosinophilia myalgia syndrome and eosinophilic fasciitis. As for imaging studies, chest radiographs may show acute inflitrates and pleural effusion and in some patients MRI findings of the brain showed inflammatory cerebrovascular
disease.
Eosinophilia myalgia syndrome symptoms
The symptoms of eosinophilia-myalgia syndrome vary greatly, but onset is typically acute or subacute and over the first 3-4 months most commonly consists of the following 3:
- Myalgias: Patients complain of generalized, severe, debilitating muscle pain and/or cramps. The shoulders, back, and legs are most commonly affected. Relapses after complete resolution are common. Weakness is an uncommon symptom early in the disease. Muscle cramps involving the leg and abdominal muscles occur early in the disease course and may persist for years
- Edema: Peripheral edema involving the extremities and face occur in more than half of patients, typically 3-4 weeks after disease onset.
- Arthralgias: Pain in large joints is common, but true arthritis is rare.
- Alopecia: Non-scarring scalp hair loss is observed frequently during the acute illness and gradually resolves.
- Rash: The types of rash seen in patients with eosinophilia myalgia syndrome include macules varying from small and purplish to large and brownish, urticaria, mucinous yellow plaques, dermatographism, serpiginous lesions, and erythematous plaques. Severe pruritus is prominent in some patients.
- Skin thickening: These findings occur in approximately one third of the patients. They resemble those seen in eosinophilic fasciitis, with skin thickening and subcutaneous induration affecting the forearms, arms, and legs. Patches of skin thickening resembling morphea are occasionally observed. In contrast with systemic sclerosis, digital skin thickening and Raynaud phenomenon are rare in patients with eosinophilia myalgia syndrome.
- Pulmonary symptoms: Nonproductive cough and/or dyspnea usually appear within 2-3 weeks after the onset of myalgias. They are self-limited in most patients.
- Neurological symptoms: These include parasthesias, numbness, or a burning sensations and affect up to one third of eosinophilia myalgia syndrome patients.
- Gastrointestinal symptoms: Rarely patients will complain of dysphagia, diarrhea, or dyspepsia.
The clinical manifestations of eosinophilia myalgia syndrome greatly vary. Typically, there is an abrupt onset of incapacitating myalgias, muscle cramps, dyspnea, peripheral edema, low-grade fever, fatigue, and skin rashes. These acute inflammatory symptoms resolve in 3-6 months, and variable degrees of neuropathy, myopathy, and skin thickening follow. Three to 4 years after the acute illness, patients report persistent chronic fatigue, intermittent myalgias, and muscle cramps, but no new manifestations appear after that time 10.
Initial symptoms of eosinophilia-myalgia syndrome may include the following:
- Acute pain
- Elevated eosinophil count in the blood
- Severe muscle cramping and/or pain
- Pain in muscle tissues
- Neuropathy (nerve malfunction resulting in numbness, weakness, burning pain and loss of reflexes)
- Joint pain
- Tremors
- Swelling of soft tissues
- Numbness, tingling, or burning sensations
- Tenderness and swelling of extremities • Patches of yellow or ivory colored rigid dry skin which become hard and slightly depressed
- Low grade fever
- Pulmonary disorders
- Rashes
- Weakness and severe fatigue
- Gastrointestinal disorders
- Cardiac arrhythmias
- Hair loss
- Cough
- Headache
The acute inflammatory symptoms just listed typically resolve after 3-6 months, but at 1 year patients with eosinophilia myalgia syndrome can have chronic symptoms that include the following 11:
- Subjective muscle weakness
- Spontaneous or activity-induced muscle cramps
- Muscle and joint pain and stiffness
- Short term memory loss, diminished concentration, communication problems
- Difficulty concentrating
- Difficulty communicating (eg, word finding and word substitution problems)
- Scleroderma-like skin changes
- Dyspnea on exertion
- Severe nerve pain
- Cardiomyopathy (disease of the heart muscle)
- Irreversible scarring of the liver
- Internal fibrosis (excessive growth of hard, fibrous tissue that replaces normal bone tissue in a single bone. Symptoms include pain and bone fracturing)
- High blood pressure
- Desmoid tumor (benign soft tissue tumors which intertwine extensively with the surrounding tissues)
- Malignant fibrous histiocytoma (a rare disorder in which histiocytes start to multiply and attack the person’s own tissue or organs resulting in tissue damage, fatigue and other symptoms) • Scleroderma-like syndrome (a fibrosing disease of connective tissue in the skin and sometimes also in other organs of the body)
- Fibromyalgia syndrome (chronically causes pain, stiffness, and tenderness of muscles, tendons, and joints without detectable inflammation)
- Chronic fatigue syndrome
- Post-traumatic stress disorder (a psychological disorder that develops in individuals who have had major traumatic experiences)
- Depression
- Vision and dental problems
- Sleeping disorders
Only about 10% of patients, out of 333 surveyed 4 years since symptom onset, reported a complete recovery 12.
Rashes occur most commonly over the face, neck, and extremities but truncal involvement is also seen. Examination of the skin in patients with eosinophilia-myalgia syndrome (eosinophilia myalgia syndrome) may reveal the following:
- Macules varying from small and purplish to large and brownish
- Mucinous yellow plaques
- Serpiginous lesions
- Erythematous plaques
Later in the disease course, the skin may appear scleroderma-like with a woody, peau d’orange appearance similar to eosinophilic fasciitis.
Examination of the muscles will rarely reveal objective weakness early in the disease course, although later in the illness this may be present.
Cardiopulmonary and abdominal examinations are generally normal, but hepatomegaly or findings of interstitial pneumonitis and/or a pleural effusion (i.e. pulmonary crackles, dullness to percussion, etc) may be present.
Extremities and facial exam may show edema. Joint examination may reveal tender joints, but synovitis and effusions are absent.
Neurologic findings are typically sensory abnormalities in a stocking-glove distribution, but reports of ascending paralysis, facial palsy, and encephalitis have been reported 3.
Eosinophilia myalgia syndrome complications
Serious and life-threatening complications (eg, ascending polyneuropathy, cardiomyopathy, myocarditis, myocardial infarction, encephalopathy, stroke, thrombocytopenia) have been reported, but they occur only rarely 3.
Eosinophilia myalgia syndrome test
Given the myriad different ways eosinophilia-myalgia syndrome can present, the initial workup should be directed at identifying other possible causes. Lab tests should including a complete blood count, electrolytes, kidney function, liver function, and inflammatory markers. Other studies (eg, antinuclear antibody [ANA], anti-neutrophil cytoplasmic antibodies [ANCA] should be ordered based on the clinical presentation.
Findings may include the following 3:
- Leukocytosis can be mild to severe
- Peripheral eosinophil count greater than 1000/µL, oftentimes much higher
- Abnormal liver function study (LFT) results are common, and mild-to-moderate elevation of transaminase levels is observed in approximately 40% of patients.
- An elevated serum creatinine kinase level is uncommon, affecting only approximately 10% of patients with eosinophilia myalgia syndrome.Elevated aldolase levels are common and occur in approximately half of patients.
- Mild-to-moderate elevation of the erythrocyte sedimentation rate (ESR) is observed in one third of patients.
- Antinuclear antibodies with a speckled pattern in low titer are observed in approximately half of patients. The significance of this is uncertain.
Other tests such as pulmonary function tests (PFTs), echocardiography, and electrophysiologic studies may be performed based on the patient’s symptoms. Again, none of these are diagnostic of eosinophilia myalgia syndrome. Findings include the following 3:
- Pulmonary function tests reveal a slightly decreased diffusion capacity in up to half of patients with eosinophilia myalgia syndrome but no evidence of restrictive or obstructive lung disease.
- Electrophysiologic studies demonstrate myopathic and neuropathic changes of varying degrees. Nerve conduction studies show mixed demyelination and a pattern of axonal degeneration.
- Echocardiography typically shows normal left ventricular function and normal estimated pulmonary artery pressure, but pulmonary arterial hypertension is occasionally detected.
Because of the varying skin rashes and muscle symptoms eosinophilia myalgia syndrome can cause, biopsy of skin, muscle, or full thickness (epidermis to muscle) biopsy may be required to rule out other diagnoses 3.
No consistent findings are observed in biopsy specimens from patients with eosinophilia myalgia syndrome; therefore, histopathologic findings are helpful but not diagnostic.
Muscle biopsy commonly reveals inflammatory infiltrates, frequently perivascular, in the endomysium and perimysium. The inflammatory cells are predominantly lymphocytes and acid phosphatase–reactive histiocytes, with rare eosinophils. In some instances, microangiopathy is present. Generalized type II myofiber atrophy and denervation atrophy are common, but myofiber necrosis and degeneration are infrequent.
Skin/fascia biopsy findings generally reveal a normal epidermis. The dermis may be normal or may have perivascular infiltrates of monocytes, eosinophils, and lymphocytes without fibrinoid necrosis. These findings differ from those in patients with scleroderma, who have more collagen deposition in the dermis.
Nerve biopsy of affected nerves shows a combination of demyelination and axonal degeneration, with epineural, perineural, and perivascular cellular infiltrates 13.
Eosinophilia myalgia syndrome treatment
The first and most important step is to discontinue the L-tryptophan or other possible offending agent(s). No medication has been shown to alter the course of eosinophilia myalgia syndrome, but high-dose steroids (eg, equivalent of prednisone 60 mg/day) may be helpful in acutely ill patients. However, the response to corticosteroids is not as dramatic as in patients with other causes of eosinophilia like eosinophilic fasciitis. Other care should be directed symptomatically 3.
Patients should avoid all herbal supplements and other over-the-counter medication unless further information about the pathophysiology of eosinophilia myalgia syndrome is elucidated 3.
Chronic symptoms such as muscle pain, spasm, weakness, neuropathy, and skin disease are treated symptomatically.
Activity may exacerbate the myalgias or muscle cramps. During the acute illness, patient may require bed rest if their symptoms are intense. Over the long term, strenuous activity should be avoided only if it causes symptoms to recur.
Because symptoms of eosinophilia myalgia syndrome tend to be prolonged, sometimes persisting for years, intermittent treatment with muscle relaxants and analgesics may be required.
Eosinophilia myalgia syndrome prognosis
Most patients (90%) continue to have some symptoms 3-4 years after the acute presentation. These are likely due to permanent tissue damage that occurred in the acute phase of the disease. Persistent muscle pain, fatigue, and muscle spasm were the most common residual complaints. Subjective memory loss and word-finding difficulties were also reported in this series. These symptoms were not responsive to any therapeutic intervention. Patients who had severe disease at onset with internal organ involvement, neurologic findings, and skin thickening tended to have a worse prognosis 3.
References- Holland SM, Gallin JI. Disorders of Granulocytes and Monocytes. In: Fauci AS et al. [ed.] Harrison’s Principles of Internal Medicine, ed. 17. New York, McGraw-Hill Companies, 2008:383
- Gotlib J. Eosinophilic disorders: Molecular pathogenesis, new classification and mofern therapy. Best practice & Reasearch Clinical Haematology. 2006;19(3):535-569.
- Eosinophilia-Myalgia Syndrome. https://emedicine.medscape.com/article/329614-overview
- Rieber N, Belohradsky BH. AHR activation by tryptophan–pathogenic hallmark of Th17-mediated inflammation in eosinophilic fasciitis, eosinophilia-myalgia-syndrome and toxic oil syndrome?. Immunol Lett. 2010 Feb 16. 128 (2):154-5.
- Hertzman PA, Clauw DJ, Duffy J, Medsger TA Jr, Feinstein AR. Rigorous new approach to constructing a gold standard for validating new diagnostic criteria, as exemplified by the eosinophilia-myalgia syndrome. Arch Intern Med. 2001 Oct 22. 161(19):2301-6.
- Allen J.A., Paterson A., Sufit R., et al. Post-epidemic eosinophilia-myalgia syndrome associated with L-tryptopan. Arthritis & Rheumatism. 2011; 63 (11) 3633-3639.
- Allen JA, Varga J. Eosinophilia-myalgia syndrome, eosinophilic fasciitis, and related fasciitis disorders. Katirji B, et al. Neuromuscular Disorders in Clinical Practice. New York: Springer Science+Business Media; 2014. 1561-73.
- Allen JA, Peterson A, Sufit R, et al. Post-epidemic eosinophilia-myalgia syndrome associated with L-tryptophan. Arthritis Rheum. 2011;63(11):3633–3639. doi:10.1002/art.30514 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3848710
- Noakes R, Spelman L, Williamsom R. Is the L-tryptophan metabolite quinolonic acid responsable for eosinophilic fasciitis? Clin Exp Med. 2006; 6:60-64.
- Martin RW, Duffy J, Engel AG, et al. The clinical spectrum of the eosinophilia-myalgia syndrome associated with L-tryptophan ingestion. Clinical features in 20 patients and aspects of pathophysiology. Ann Intern Med. 1990 Jul 15. 113(2):124-34.
- Eosinophilia-Myalgia Syndrome. https://apfed.org/about-ead/eosinophilia-myalgia-syndrome/
- Clauw DJ, Pincus T. The eosinophilia-myalgia syndrome: what we know, what we think we know, and what we need to know. J Rheumatol Suppl. 1996 Oct. 46:2-6.
- Haseler LJ, Sibbitt WL Jr, Sibbitt RR, Hart BL. Neurologic, MR imaging, and MR spectroscopic findings in eosinophilia myalgia syndrome. AJNR Am J Neuroradiol. 1998 Oct. 19(9):1687-94.