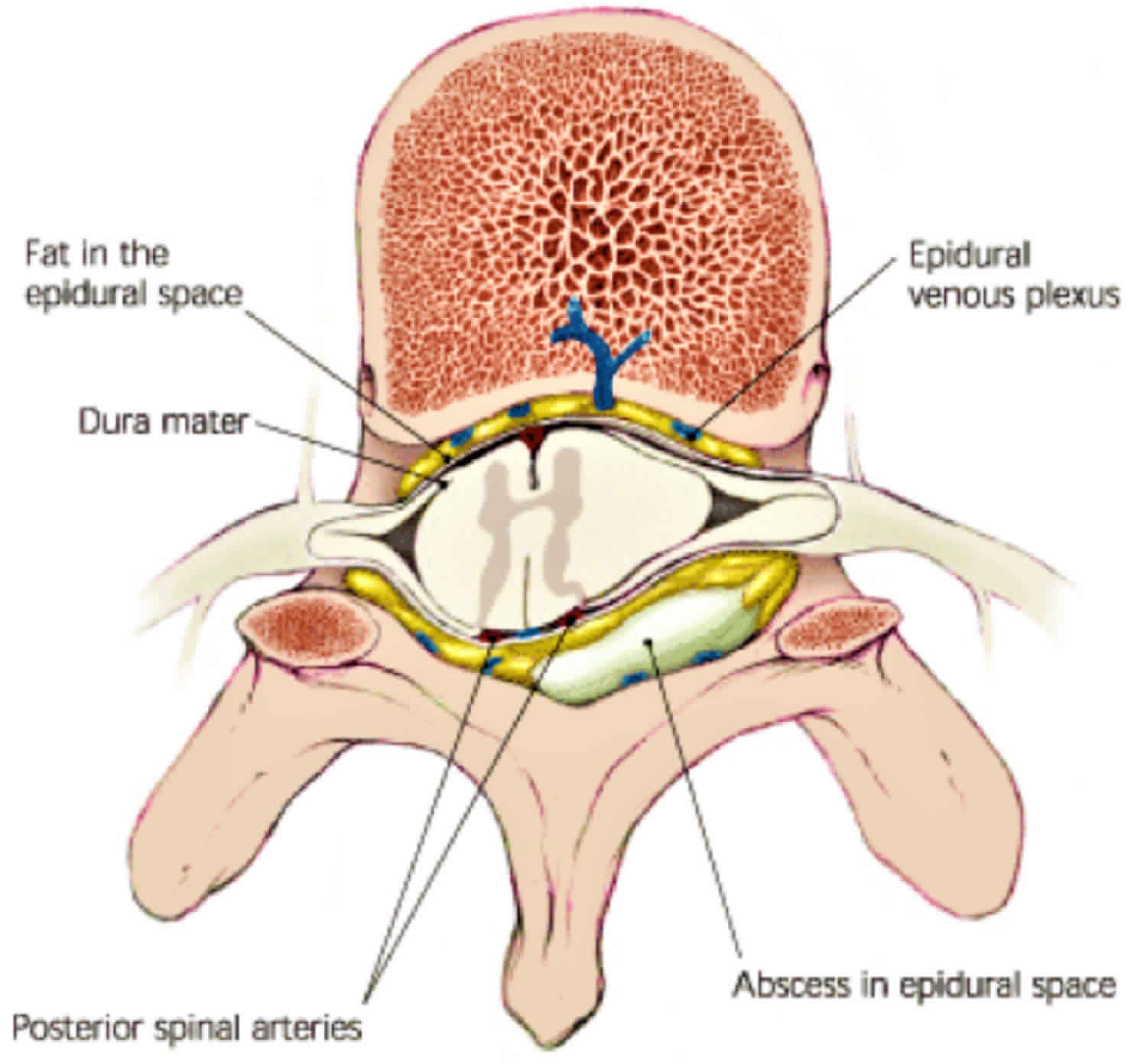
Spinal epidural abscess
Epidural abscess also known as spinal epidural abscess, is a rare severe suppurative infection of the epidural space that leads to devastating neurological deficits and may be fatal 1. Epidural abscess is defined as an inflammation that involves a collection of pus between the dura (the outer membrane that covers the brain and spinal cord) and the bones of the skull or spine 2. Epidural abscess can cause injury to the spinal cord by direct compression 3 or secondary to local ischemia 4. Spinal cord injury may be prevented if surgical and medical interventions are implemented early.
Risk factors for epidural abscess include intravenous drug abuse, diabetes mellitus, old age, and renal disease 5. However, no definitive cause can be identified in 20% of patients 6. The annual incidence of spinal epidural abscess has risen in the past 2-3 decades from 0.2-1 cases per 10,000 hospital admissions to 2.5-5.1 per 10,000 admissions 7. The rising incidence of spinal epidural abscess has been attributed to the increasing prevalence of injection drug use, as well as to an increased performance of invasive spinal procedures.
Epidural abscess is usually located in the thoracic and lumbar parts of the vertebral column and injures the spinal cord by direct compression or local ischemia. Most abscesses occur posteriorly. An anterior location is often associated with vertebral osteomyelitis or a psoas abscess 8. The thoracic and lumbar areas are the most likely sites of involvement, with the cervical spine accounting for approximately 20% of cases 9. Spread to multiple vertebral levels is common and occurs as the abscess extends up and down the spinal dural sheath. In some cases, this process involves most or all of the spine.
The clinical presentation of epidural abscess includes the “classic triad” of back pain, fever, and neurological dysfunction 10. However, these nonspecific features can lead to a high rate of misdiagnosis 11. Spinal epidural abscess may lead to paralysis or even death; thus, prognosis of these patients remains unfavorable. 15% of patients with spinal epidural abscess show a poor prognosis (rate of development of paralysis = 8% and death rate = 7%) 12. Therefore accurate diagnosis and prompt treatment are important to treat patients with epidural abscess.
Spinal epidural abscess diagnosis is difficult, because clinical symptoms are not specific and can mimic many benign conditions. The gold standard in the diagnostic evaluation is magnetic resonance imaging (MRI) with gadolinium enhancement, which determines the location and extent of the epidural abscess. Increased awareness of the epidural abscess is essential for rapid recognition and immediate implementation of treatment.
Conventionally, epidural abscess is diagnosed based on clinical symptoms, laboratory tests, imaging studies, and invasive diagnostic tests. Among these modalities, gadolinium-enhanced magnetic resonance imaging (MRI) shows 90% sensitivity and specificity and is the gold standard to diagnose epidural abscess 13. Computed tomography (CT) is rarely performed because of its lower sensitivity, particularly in patients with early-stage epidural abscess. CT is performed only if MRI is unavailable 14. Furthermore, other methods can be used to improve the diagnostic rate. Unfortunately, the misdiagnosis rate of epidural abscess remains significantly high (≥50%) 15. Previous studies have reported several treatment options including antibiotic therapy and surgical intervention. However, the optimal treatment for epidural abscess remains unclear 10.
Figure 1. Spinal epidural abscess MRI
Footnote: Preoperative magnetic resonance imaging (MRI) scan of the thoracic spine obtained in a 22-year-old woman shows a fluid collection between the 6th and 12th thoracic vertebral levels on sagittal T1-weighted and T2-weighted images.
[Source 10 ]Epidural abscess causes
Ten to thirty percent of spinal epidural abscesses result from direct extension of local infection, usually vertebral osteomyelitis, psoas abscess, or contiguous soft-tissue infection 7.
About half are due to hematogenous seeding. The most likely source is a soft-tissue process, but anything capable of causing bacteremia can result in spinal epidural abscess (endocarditis, urinary tract infection, respiratory tract infections, intravenous drug use, vascular access devices). Hematogenous seeding of the spinal epidural abscess can result in multilevel noncontiguous spinal epidural abscess.
Fifteen to twenty-seven percent of spinal epidural abscesses are due to invasive procedures or instrumentation. Spinal surgery, epidural anesthesia, steroid and pain-relieving injections, and placement of pain pumps are all associated with spinal epidural abscess. Short-term epidural anesthesia is much less risky than a catheter left in place for days or permanently implanted. Rates of infection after intraoperative epidural block are about 1 in 2,000, while longer-duration (days) epidural pain catheter placement may be associated with rates of infection as high as 4.3%. Simple epidural injections rarely cause infection; the risk has been estimated at 1 in 10,000 to 1 in 60,000 injections.
In some cases (up to 30% in some series), the source of the spinal epidural abscess is not identified.
Staphylococcus aureus infection causes most cases of spinal epidural abscess. This is followed in frequency by streptococcal and Enterobacteriaceae infections. Coagulase-negative staphylococcal infections are observed almost exclusively in the context of recent spinal instrumentation or other medical procedures. The most common organisms that cause spinal epidural abscess include the following 16:
- Staphylococcus aureus (60%; up to 25% may be methicillin-resistant S aureus [MRSA]) 7
- Enteric gram-negative bacilli, especially Escherichia coli (10%);their incidence is rising in some series
- Coagulase-negative staphylococci (3-5%), primarily involving spinal instrumentation or epidural anesthesia/injections
- Bacteroides species and other anaerobes (2%)
- Pseudomonas species (2%)
- Streptococci, including Streptococcus viridans, group B streptococci, and pneumococcus (10%)
- Mycobacteria, usually Mycobacterium tuberculosis (< 1% in Western countries but much more common in developing countries). Do not forget to send acid-fast bacilli (AFB) stains and cultures.
- Less-common organisms -Acinetobacter,enterococci, Actinomyces species, Nocardia species, Brucella species, and fungi, including Candida, Coccidioides, Aspergillus, Blastomyces, and Sporothrix species
- Exserohilum rostratum was a common cause in 2012 due to the use of contaminated methylprednisolone injections
- Polymicrobial (possibly 5%-10%)
- Unknown (6%-10%).
In intracranial epidural abscess, upper-respiratory bacterial pathogens predominate in sinus-associated disease, whereas nosocomial pathogens are of concern in cases that develop after craniotomy. The most common causative organisms include the following:
- Staphylococci, both coagulase-positive and coagulase-negative
- Streptococci, including anaerobic and microaerophilic species
- Aerobic gram-negative bacilli
- Propionibacterium acnes
- Other anaerobes
- Can be polymicrobial
Mechanism of injury
Direct compression of the cord is clearly a major factor 17.
Vascular occlusion due septic thrombophlebitis and/or vasculitis is also a factor
The exact mechanism of injury remains controversial.
Risk factors for spinal epidural abscess
The most common risk factor for spinal epidural abscess is diabetes mellitus, followed by spinal trauma (may be remote) or surgery, intravenous drug abuse, alcoholism, renal insufficiency, immunosuppression (including infection, steroid use, cirrhosis, and malignancy), central lines, implantable devices (eg, pacemakers), pregnancy, and spinal/epidural anesthesia or injections 8.
Intravenous drug use seems to represent an increasing risk factor in many series.
Risk factors for intracranial epidural abscess include prior craniotomy, head injury, sinusitis, otitis media, and mastoiditis 18.
Epidural abscess symptoms
Most symptoms of a spinal epidural abscess are due to enlargement of the abscess and surrounding inflammation, which can lead to tissue compression and spinal cord ischemia. Onset of symptoms usually occurs within hours to days but may be more chronic in nature, presenting with weeks to months of symptoms. The microbiology often dictates the pace of progression 17.
Back or neck pain is the most common symptom in individuals with spinal epidural abscess, occurring in 70%-100% of cases 19.
The classic diagnostic triad of fever, spinal pain, and neurological deficits is present in only 10-15% of cases at first physician contact and must not be relied on for diagnosis. Significant back or neck pain coupled neurologic deficits, Staphylococcus aureus bacteremia, recent surgery/injections, or unexplained elevated C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) should prompt an MRI without delay to facilitate diagnosis 20.
Findings associated with spinal epidural abscess from multiple studies include the following 17:
- Fever (range, 13%-95%; median, 32%) (However, note that many patients with spinal epidural abscess are afebrile.)
- Spinal tenderness (range, 17%-98%; median, 58%)
- Weakness of the extremities (range, 26%-87%; median, 40%)
- Sensory abnormalities (range, 13%-45%; median, 36%)
- Paralysis (range, 5%-39%; median, 27%)
- Reflex abnormalities (up to 40% of cases) (Early hyperreflexia may give way to diminished or absent reflexes.)
- Respiratory compromise (with cervical lesions)
If left untreated, the progression of symptoms is usually sequential and forms the basis for the staging of spinal epidural abscess: (1) back pain; (2) radicular irritation; (3) motor weakness, sphincter dysfunction, sensory changes; and, finally, (4) paralysis. Note that this progression may occur very rapidly, and some symptoms may be skipped.
The patient’s neurological status at the time of diagnosis is the most accurate predictor of outcome and prognosis.
Intracranial epidural abscess
The symptoms of intracranial epidural abscess are generally more acute but may be difficult to discern from the inciting process (eg, sinusitis, postoperative infection). When intracranial epidural abscess is combined with a subdural empyema, as is often the case, the course is compressed 18.
Signs and symptoms are due to both infection and the slowly expanding intracranial mass. Fever, headache, malaise, lethargy, nausea, and vomiting may be present. Intracranial epidural abscesses due to sinus infections can cause purulent drainage from the nose or ear.
Patients without a history of recent cranial manipulation who develop intracranial epidural abscess present with encephalopathy and focal neurological deficits. Most patients who have undergone craniotomy (67%) tend to be afebrile at presentation, and their neurological deficits are often less severe and less acute, with more than 90% showing evidence of wound infection.
Findings associated with intracranial epidural abscess include the following 18:
- Fever (However, fewer than half of patients are febrile, so this symptom is unreliable.)
- Headache (50%-73%)
- Altered mental status (44%-50%)
- Sinus tenderness (32%-90%)
- Focal neurological deficits
- Evidence of wound infection (>90% of patients who have undergone craniotomy)
- Seizure (4%-63%)
Epidural abscess complications
Death or permanent neurologic sequelae occur in a substantial proportion of patients with epidural abscess, especially those who present with major neurological deficits or sepsis. In a large 2017 series, 7% died and 8% were left paralyzed 7.
Epidural abscess diagnosis
A combination of various modalities including clinical symptoms (thorough history taking), laboratory tests, and imaging studies are important to improve the diagnostic rate of spinal epidural abscess. Among these modalities, gadolinium-enhanced MRI shows 90% sensitivity and specificity and is the gold standard to diagnose epidural abscess 13. Hypointense spinal cord signals on T1-weighted imaging and hyperintense signals on T2WI characterize epidural abscess 21. However, diagnosis of multifocal epidural abscess can be challenging and may easily be missed. Therefore, whole spine imaging is important 22. Radiography and CT can accurately diagnose bone lesions, which can serve as indicators of other conditions, such as spinal fractures and spinal tuberculosis.
Lumbar puncture is generally not indicated in spinal epidural abscess and carries the risk of spreading the bacteria into the subarachnoid space, with consequent meningitis. Lumbar puncture is contraindicated in intracranial epidural abscess because of the high risk of cerebellar tonsillar herniation due to increased intracranial pressure. When obtained in spinal epidural abscess, lumbar puncture usually reveals a nonspecific parameningeal infection picture, with elevated protein levels, normal or slightly depressed glucose levels, and modest pleocytosis. Results may also be normal or indicative of frank bacterial meningitis. Culture results may be positive in up to 25% of cases, but almost all of these patients have positive blood cultures 8.
CT-guided needle aspiration may be used to obtain material for analysis.
Routine tests
The CBC count may reveal leukocytosis, left shift, thrombocytopenia, and anemia. Only about two thirds of patients who present with spinal epidural abscess have leukocytosis at the time of initial evaluation.
The erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are almost invariably elevated; this is a nonspecific finding. Sendi et al 13 reported leukocytosis in 60% to 80% and ESR >20 mm/h in >95% of cases of epidural abscess, which may be useful diagnostic indicators of epidural abscess.
Always obtain blood cultures, as they are positive in 60% of cases 7.
Abscess fluid/operative material
Perform Gram staining and routine aerobic and anaerobic cultures on aspirated or surgically obtained abscess fluid.
Special stains and cultures for mycobacteria and fungi are indicated.
Consider Brucella cultures and serologies when this is a possibility; alert laboratory personnel that Brucella may be involved so they can take precautions.
Epidural abscess staging
A staging system for the progression of spinal epidural abscess exists and may be of some diagnostic value, but it must be stressed that not all patients move sequentially through the stages, and that deterioration may be rapid 17.
- Back pain, tenderness, and fever
- Radicular pain, reflex abnormalities
- Sensory abnormalities, motor weakness, bowel and bladder problems
- Paralysis, which rapidly becomes permanent without surgical intervention
Epidural abscess treatment
A combined medical-surgical approach, with emergent surgical decompression and drainage of purulent material, has been the standard approach to spinal epidural abscess. Antibiotic-based therapy, sometimes combined with CT-directed needle aspiration, has traditionally been used only in patients who are determined to be at prohibitively high risk of surgery or who have a fixed paralysis that lasts more than 48-72 hours and that is presumed to be irreversible.
Optimal treatment for epidural abscess remains controversial, and there is lack of consensus regarding the efficacy of conservative (systemic antibiotic therapy) vs surgical management (laminectomy) 10. In recent years, wider use of antibiotic-based, nonsurgical therapy for spinal epidural abscess has been advocated 23, condemned 24 and cautiously discussed 25. Conflicting reports are available in the literature in this context. Pathak et al 26 reported a case of a 13-year-old boy who presented with paraparesis, as well as bladder and bowel involvement and showed an excellent response to 6-week antibiotic therapy with only minimal residual gait disturbance. However, Arko et al 27 reported that exclusive antibiotic use fails in patients with risk factors, including white blood cell counts >12 × 109 cells/L and severe neurological involvement. Epstein NE et al 28 reported failure rates of 41% to 42.5% associated with nonoperative treatment (including a 22% risk of permanent paralysis and 3–25% risk of mortality). These authors proposed surgical intervention to avoid these risks. Furthermore, a 5-year prospective study performed by Khursheed et al 29 showed that delayed surgical management (>36 hours after symptom onset) was associated with a poor prognosis. Therefore, they recommend prompt surgical intervention in such cases. Other researchers have reported similar findings 30.
If medical therapy is to be used as initial therapy for spinal epidural abscess and surgery held in reserve, a number of caveats apply, as follows:
- The patient should have no neurological deficits. Patients with deficits experience better outcomes with prompt surgery 31.
- A culture-proven microbiological diagnosis should be available (from blood culture or aspiration). MRSA seems to be associated with higher failure rates than MSSA; be extremely cautious when contemplating medical therapy for MRSA epidural infections 32.
- Stringent follow-up by both the primary team and neurosurgeons must be available and emergent surgery available, if needed.
- The physicians caring for the patient must be aware that rapid deterioration may occur at any time (the first 72 hours being most risky) and that even prompt rescue surgery may leave the patient with a neurological deficit that might have been avoided with surgery at first diagnosis. Failure rates with medical management in one recent study were 41%, with some these failures termed “catastrophic” 25. Other studies have found failure rates of 17%-38%. Cavalier follow-up of medically managed patients with epidural abscess can be disastrous; repeat MRI scanning and/or surgical re-evaluation must be available and performed on an emergent basis when the clinical picture changes.
- Risk factors for failure of medical therapy include any neurological deficit, sensory changes, diabetes, malignancy, bacteremia, age older than 65 years, and MRSA as the causative organism 33. Patients with multiple risk factors for failure of medical therapy should have the traditional combined medical/surgical approach, with the surgery performed soon after diagnosis.
- A follow-up MRI is necessary within 2-4 weeks to evaluate for improvement with medical therapy.
Empirical antibiotic therapy should include coverage of gram-positive cocci, particularly staphylococci (including MRSA), and gram-negative bacilli. Vancomycin has been the standard agent for gram-positive infections, although linezolid, daptomycin, ceftaroline, or tigecycline could be considered. The third- and fourth-generation cephalosporins and meropenem offer excellent gram-positive (except MRSA) and gram-negative coverage in addition to CNS penetration.
Pending cultures, a combination of agents (vancomycin plus cefepime or similar) is needed. Additional coverage may be needed if some of the less-common etiologic agents are suspected. Always tailor coverage once culture data are available; for example, nafcillin is a much better drug for MSSA infections than vancomycin. Note that failures due to the development of resistance have occurred when daptomycin alone was used for MRSA spinal epidural abscess 34. Experience with ceftaroline for these infections is extremely limited, but this maybe a useful second-line MRSA agent 35. especially when combined with vancomycin or daptomycin.
Intracranial epidural abscess
A combined medical-surgical approach is used for intracranial epidural abscess. Prompt decompression is used to manage intracranial epidural abscess, as it is uniformly considered a neurosurgical emergency. A craniotomy is usually performed. Empiric antibiotic therapy is similar to that described for spinal epidural abscess; since many of these infections result from prior interventions, the possibility of more-resistant nosocomial organisms must be considered. Vancomycin plus cefepime or meropenem would be good starting choices, with metronidazole added to the cefepime if anaerobes are a major concern.
Long-term monitoring
Follow-up MRI should be obtained if any clinical deterioration is noted in patients with an intracranial epidural abscess or spinal epidural abscess. Follow-up MRI at 2-4 weeks should be performed in patients with spinal epidural abscess undergoing exclusively medical treatment to ensure the abscess has improved. It is unclear whether surgically treated patients with spinal epidural abscess who are doing well require follow-up MRI, as the MRI findings often correlate poorly with the clinical course 36.
Follow-up with the neurosurgeon is needed.
Follow-up with an infectious diseases specialist is advised to monitor intravenous antibiotics.
Epidural abscess prognosis
The degree of neurologic recovery after surgery correlates with the duration and initial severity of the neurologic defect.
Spinal epidural abscess carries a mortality rate of 2%-20%; intracranial epidural abscess, about 10% (see Mortality). Eight percent of survivors were left paralyzed in one large 2017 series 7.
A worse outcome has been observed in patients with the following 17:
- Multiple medical problems
- Prior spinal surgery
- Prior cervical or thoracic abscess location
- Thrombocytopenia
- Leukocytosis (>14,000 white blood cell count/µL)
- Persistently elevated inflammatory markers
- Infection with methicillin-resistant staphylococci
- Significant degree of thecal sac compression
- Sepsis.
- Rosc-Bereza K, Arkuszewski M, Ciach-Wysocka E, Boczarska-Jedynak M. Spinal epidural abscess: common symptoms of an emergency condition. A case report. Neuroradiol J. 2013;26(4):464–468. doi:10.1177/197140091302600411 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4202809
- Epidural abscess. https://emedicine.medscape.com/article/232570-overview
- Khanna RK, Malik GM, Rock JP, et al. Spinal epidural abscess: evaluation of factors influencing outcome. Neurosurgery 1996;39:958–64.
- Heusner AP. Nontuberculous spinal epidural infections. N Engl J Med 1948;239:845–54.
- Shweikeh F, Saeed K, Bukavina L, et al. An institutional series and contemporary review of bacterial spinal epidural abscess: current status and future directions. Neurosurg Focus 2014;37:E9.
- Louis A, Fernandes CM. Spinal epidural abscess. Can J Emerg Med 2005;7:351–4.
- Vakili M, Crum-Cianflone NF. Spinal Epidural Abscess: A Series of 101 Cases. Am J Med. 2017 Dec. 130 (12):1458-1463.
- Darouiche RO. Spinal epidural abscess. N Engl J Med. 2006 Nov 9. 355(19):2012-20.
- Kabbara A, Rosenberg SK, Untal C. Methicillin-resistant Staphylococcus aureus epidural abscess after transforaminal epidural steroid injection. Pain Physician. 2004 Apr. 7(2):269-72.
- Yang X, Guo R, Lv X, et al. Challenges in diagnosis of spinal epidural abscess: A case report. Medicine (Baltimore). 2019;98(5):e14196. doi:10.1097/MD.0000000000014196 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6380696
- Alerhand S, Wood S, Long B, et al. The time-sensitive challenge of diagnosing spinal epidural abscess in the emergency department. Intern Emerg Med 2017;12:1179–83.
- Vakili M, Crum-Cianflone NF. Spinal epidural abscess: a series of 101 cases. Am J Med 2017;130:1458–63.
- Sendi P, Breqenzer T, Zimmerli W. Spinal epidural abscess in clinical practice. Q J Med 2008;101:1–2.
- Lury K, Smith JK, Castillo M. Imaging of spinal infections. Semin Roentgenol 2006;41:363–79.
- Hsieh PC, Liu JC, Wang MY. Introduction: vertebral osteomyelitis and spinal epidural abscess. Neurosurg Focus 2014;37:1 p preceding E1.
- Chiller TM, Roy M, Nguyen D, Guh A, Malani AN, Latham R. Clinical findings for fungal infections caused by methylprednisolone injections. N Engl J Med. 2013 Oct 24. 369(17):1610-9.
- Sendi P, Bregenzer T, Zimmerli W. Spinal epidural abscess in clinical practice. QJM. 2008 Jan. 101(1):1-12.
- Tunkel AR. Subdural empyema, epidural abscess, and suppurative intracranial thrombophlebitis. Mandell GL, Bennet JE, Dolin R. Mandell, Douglas, and Bennett’s Principles and Practices of Infectious Diseases. 8th ed. Philadelphia: Elsevier Saunders; 2015. 1177-85.
- Epidural Abscess Clinical Presentation. https://emedicine.medscape.com/article/232570-clinical
- Bond A, Manian FA. Spinal Epidural Abscess: A Review with Special Emphasis on Earlier Diagnosis. Biomed Res Int. 2016. 2016:1614328.
- Akalan N, Ozqen T. Infection as a cause of spinal cord compression: a review of 36 spinal epidural abscess cases. Acta Neurochir (Wien) 2000;142:17–23.
- Ju KL, Kim SD, Melikian R, et al. Predicting patients with concurrent non-contiguous spinal epidural abscess lesions. Spine J 2015;15:95–101.
- Avilucea FR, Patel AA. Epidural infection: Is it really an abscess?. Surg Neurol Int. 2012. 3(Suppl 5):S370-6.
- Pereira CE, Lynch JC. Spinal epidural abscess: an analysis of 24 cases. Surg Neurol. 2005. 63 Suppl 1:S26-9.
- Patel AR, Alton TB, Bransford RJ, Lee MJ, Bellabarba CB, Chapman JR. Spinal epidural abscesses: risk factors, medical versus surgical management, a retrospective review of 128 cases. Spine J. 2014 Feb 1. 14(2):326-30.
- Pathak A, Singh P, Gehlot P, et al. Spinal epidural abscess treated with antibiotics alone. BMJ Case Rep 2013;2013
- Arko L, Quach E, Nguyen V, et al. Medical and surgical management of spinal epidural abscess: a systematic review. Neurosurg Focus 2014;37:E4.
- Epstein NE. Timing and prognosis of surgery for spinal epidural abscess: a review. Surg Neurol Int 2015;6Suppl 19:S475–86.
- Khursheed N, Dar S, Ramzan A, et al. Spinal epidural abscess: report on 27 cases. Surg Neurol Int 2017;8:240.
- Patel AR, Alton TB, Bransford RJ, et al. Spinal epidural abscesses: risk factors, medical versus, surgical management, a retrospective review of 128 cases. Spine J 2014;14:326–30.
- Howie BA, Davidson IU, Tanenbaum JE, Pahuta MA, Buchholz AL, Steinmetz MP, et al. Thoracic Epidural Abscesses: A Systematic Review. Global Spine J. 2018 Dec. 8 (4 Suppl):68S-84S.
- Spernovasilis N, Demetriou S, Bachlitzanaki M, Gialamas I, Alpantaki K, Hamilos G, et al. Characteristics and predictors of outcome of spontaneous spinal epidural abscesses treated conservatively: A retrospective cohort study in a referral center. Clin Neurol Neurosurg. 2017 May. 156:11-17.
- Shah AA, Ogink PT, Nelson SB, Harris MB, Schwab JH. Nonoperative Management of Spinal Epidural Abscess: Development of a Predictive Algorithm for Failure. J Bone Joint Surg Am. 2018 Apr 4. 100 (7):546-555.
- Velazquez A, DeRyke CA, Goering R, Hoover V, Wallace MR. Daptomycin non-susceptible Staphylococcus aureus at a US medical centre. Clin Microbiol Infect. 2013 Dec. 19(12):1169-72.
- Ebot J, Freeman WD, Wharen R, Diaz MA, Libertin C. MRSA Spinal Epidural Abscess as a Neurosurgical and Infectious Disease Emergency with Unresolved Antimicrobial Solution. Case Rep Infect Dis. 2019. 2019:7413089.
- Kowalski TJ, Layton KF, Berbari EF, et al. Follow-up MR imaging in patients with pyogenic spine infections: lack of correlation with clinical features. AJNR Am J Neuroradiol. 2007 Apr. 28(4):693-9.