Erythroplakia
Erythroplakia is Greek for “flat red area”, is defined as a red patch or red flat area or slightly raised or worn away red area that results when the lining of the mouth thins that cannot be accounted for by any specific disease entity or condition 1. The area appears red because the underlying capillaries are more visible. Oral erythroplakia is the rarer form of oral pre-malignant lesion and has been identified as the one with the highest malignant transformation rates 2.
Erythroplakia may appear as a bright red, smooth lesions often with a well-defined margins adjacent to normal looking mucosa and are usually asymptomatic. The soft palate, the floor of mouth, the ventral surface of tongue and the retro-molar area are the most common sites of involvement.
On the other hand leukoplakia is a flat white spot that may develop when the moist lining of the mouth (oral mucosa) is irritated for a long period. Leukoplakia is defined by the World Health Organization as a white lesion of the oral mucosa that cannot be scraped off and cannot be attributed to another definable lesion 3. The irritated spot appears white because it has a thickened layer of keratin—the same material that covers the skin and normally is less abundant in the lining of the mouth.
Erythroplakia is more common among middle aged to elderly persons and, especially among men. Erythroplakia is far less common than leukoplakia 4.
Erythroplakia is a much more ominous predictor of oral cancer than leukoplakia, with much greater probability (91%) of showing signs of dysplasia or malignancy at the time of diagnosis 5.
Erythroplakia exists on a continuum both in appearance and behavior with leukoplakia and mixed erythroleukoplakia (a lesion that is both white and red) 6.
Premalignant squamous lesions of the oral cavity are areas of altered epithelium that are at an increased risk for progression to oral squamous cell carcinoma (SCC) 3. A number of studies have reported that oral squamous cell carcinoma are frequently preceded by or associated with leukoplakia or erythroplakia 7. Furthermore, it has been shown that leukoplakia and erythroplakia are frequently seen adjacent to some oral squamous cell carcinoma 8. The most common potentially malignant disorders include leukoplakia, erythroplakia, lichen planus, and submucous fibrosis. Not to be ignored, however, is the fact that up to 50% of oral squamous cell carcinomas cases arise from clinically normal mucosa 9.
Regular examinations of your mouth and teeth are the key for early detection. Your dentist is qualified to perform a thorough soft tissue and head and neck exam to detect any problems in your mouth. Erythroplakia can develop without any pain or symptoms and usually doesn’t develop over a large area. The most common high risk sites for this lesion are the lateral border or underside of the tongue, the floor of the mouth, and the back of the throat. Any suspicious areas should be examined closely with instruments, gauze, and palpation as these flat, velvety red lesions will often bleed when scraped or palpated 10. The cheeks, lips, gums and the roof of the mouth will also be examined for abnormalities.
If a suspicious red lesion is identified, a biopsy is the next step. This can be done in your dentist’s office or an oral surgeon’s office using local anesthesia to remove tissue from the area. The tissue sample will be sent to a pathology lab for diagnosis, though the results may take several days. If the results indicate cancer, you will be referred to specialists for treatment that will include complete removal of the lesion as well as surrounding tissue. If the biopsy reveals dysplasia or a precancerous patch, removal or excision may still be recommended, or at the very least, close monitoring and frequent checks of the area will be necessary.
Treatment options for erythroplakia may include:
- careful watching (active surveillance) and frequent follow-up
- surgery
- cryosurgery
- laser surgery
Because erythroplakia can develop into cancer, people with erythroplakia should avoid known risk factors, such as using tobacco and drinking alcohol.
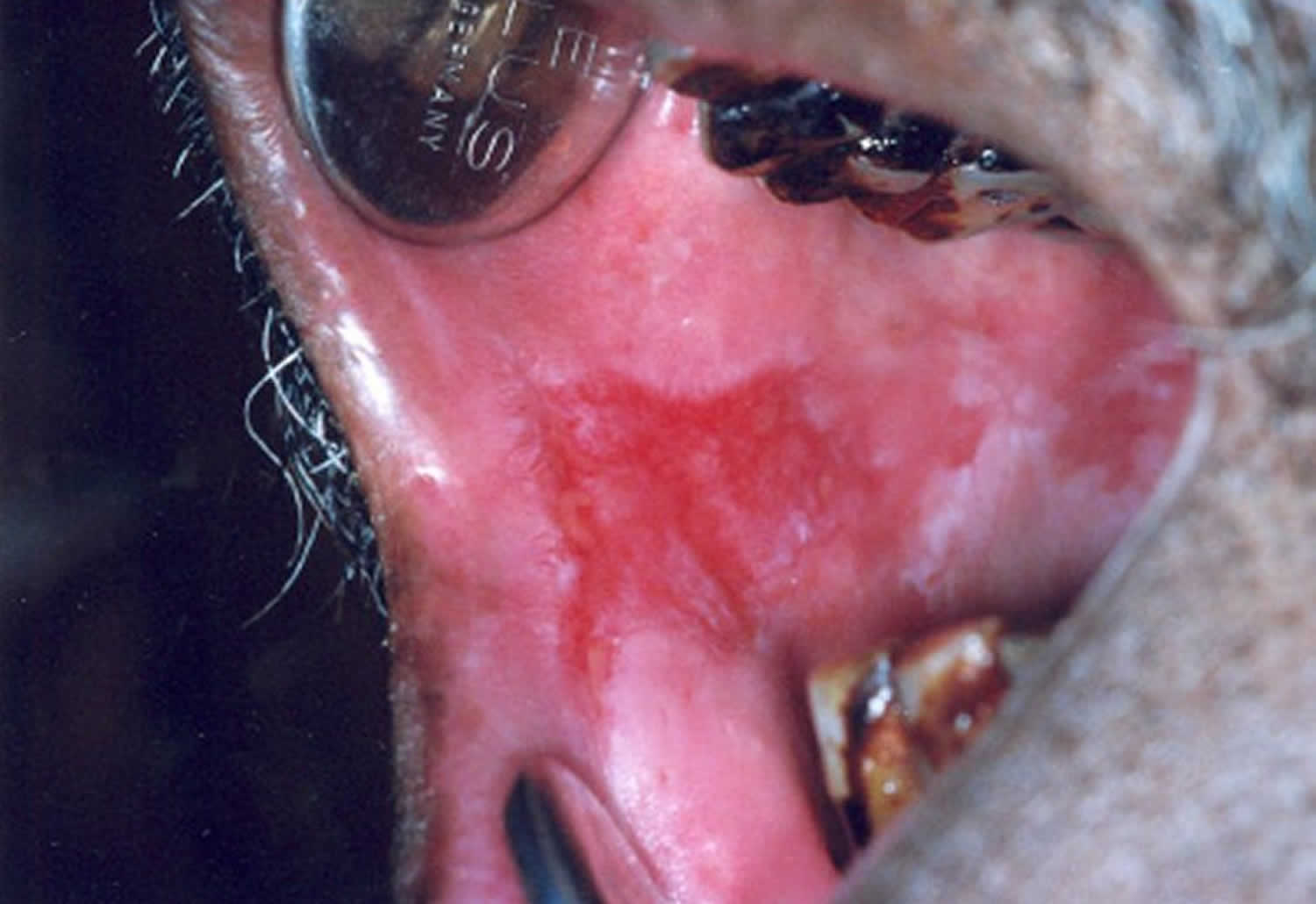
Figure 1. Erythroplakia
Footnote: Erythroplakia. Note the red velvety lesion involving the posterior aspect of the right side of the hard palate. Note the raised irregular area along the anterolateral aspect of the lesion which is clinically suspicious of malignant transformation.
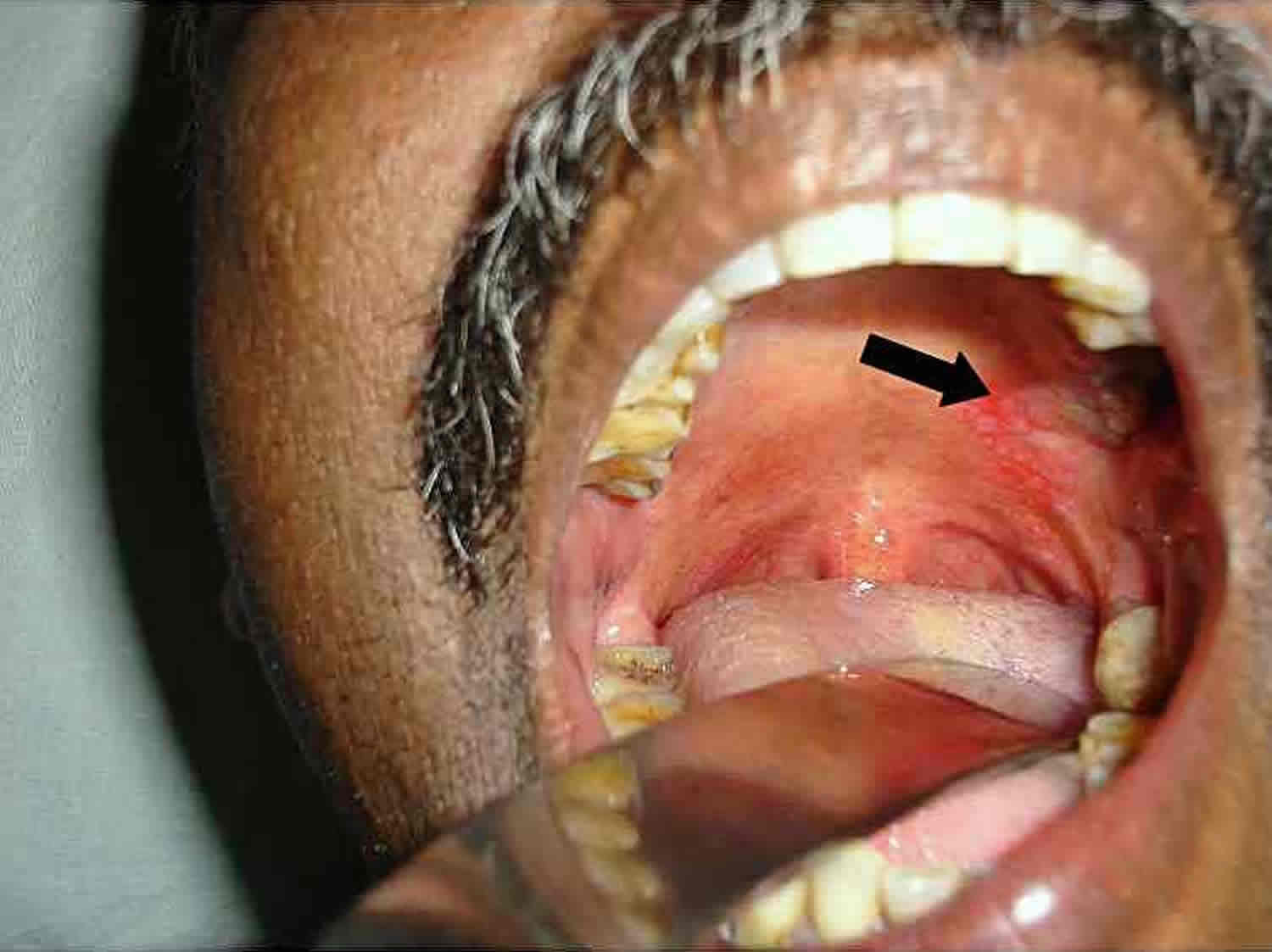
Figure 2. Erythroplakia roof of mouth
Footnote: Erythroplakia. A 53-year-old heavy smoker with 2×3 cm erythematous lesion (arrow) on the left side of the posterior aspect of the hard palate.
Figure 3. Erythroplakia on the tongue
Footnote: Oral submucous fibrosis with erythroplakia of the tongue.
Figure 4. Erythroplakia gums
Footnote: Erythroplakia. Note the red patch on the right buccal mucosa with white areas posteriorly.
People with a mouth growth that does not go away in a week or two should see their doctor or dentist when convenient. Warning signs suggest a higher risk of cancer, and although evaluation is not urgent, people with warning signs (particularly those who use tobacco) should not put off being evaluated.
Because oral cancer often causes no symptoms early on, it is important for people to have a yearly examination of the mouth. Such an examination can be done during an annual dental check-up.
Erythroplakia causes
Erythroplakia can be caused by unhealthy habits (like chewing tobacco, smoking and poor diet), long-term trauma to oral tissues, or simply from aging. Poorly fitting dentures that rub against the tongue or the inside of the cheeks can also cause these changes. But sometimes, there’s no clear cause. Dysplasia will often go away if the cause is removed. No one is exempt from developing this condition but it can be prevented or at least in its earliest form, eradicated before it develops into oral cancer. Since the risk of cancer increases with age and in the presence of certain risk factors, most cases are identified in heavy drinkers and smokers over 40, according to the American Family Physician 11.
Risk factors for developing erythroplakia
The following risk factors increase your chance of developing erythroplakia:
- smoking heavily
- chewing tobacco
- excessive alcohol use
Erythroplakia symptoms
Erythroplakia is usually asymptomatic, although some patients may complain of a sore, burning or metallic sensation. The development of pain or soreness may be associated with a malignant change.
Clinically, erythroplakia may appear as a red, velvet-like lesion or may have white patches on or peripheral to the lesion (speckled leukoplakia), which has a high risk of carcinoma 11. The boundaries of these lesions may be poorly defined; many are irregular, with a blending of inflamed and normal mucosa.
Erythroplakia is more frequently associated with epithelial dysplasia or oral squamous cell carcinoma. Most suspicious erythroplakias are found in patients considered to be at high risk for oral cancer, such as heavy smokers and drinkers 40 years and older. Approximately 90 percent of early carcinomas are predominantly red or have a red component. In high-risk patients, the red, velvety lesion appears long before any ulceration, bleeding, induration, dysfunction, pain or lymphadenopathy arises.
Erythroplakia diagnosis
Doctors first ask questions about the person’s symptoms and medical history. Doctors then do a physical examination. What they find during the history and physical examination can help suggest a cause of the mouth growth.
Doctors ask people about how long the growth has been present, whether it is painful, and whether there was any injury to the area (for example, biting a cheek or scraping by a sharp tooth edge or dental restoration). Other things they ask about include:
- The amount and duration of use of alcohol and tobacco
- Risk factors for thrush (caused by the fungus Candida albicans), including use of antibiotics and a history of diabetes or HIV infection
- Whether the person has lost weight or been feeling generally ill
The physical examination focuses on the mouth and neck. Doctors look carefully at all areas of the mouth and throat, including under the tongue. They feel the sides of the neck for swollen glands (lymph nodes), which indicate possible cancer or chronic infection.
Biopsy is mandatory for any persistent red lesion without an obvious cause. Biopsy is necessary to make sure a growth is noncancerous. Treatment depends on the results of a histologic examination.
Histological examination of clinically diagnosed erythroplakia often shows severe epithelial dysplasia, carcinoma in-situ or micro-invasive cancer 12.
Erythroplakia treatment
In view of the high malignant potential of erythroplakia, doctors advise surgical excision, including laser and histological examination as a mandatory procedure whenever an erythroplakia is clinically diagnosed 13. All erythroplakias should be viewed with extreme clinical suspicion for malignancy, as they are more likely to harbor histological foci of severe dysplasia, carcinoma in-situ (CIS) or invasive cancer. However, even after surgical excision, the recurrences and development of malignancy at the same site are high 14. In view of this, long-term follow-up is essential even after surgical removal.
Other management of oral erythroplakia focuses on the prevention of malignant transformation and early detection of occult malignancy. Persons with erythroplakia should be advised to stop tobacco and alcohol habits, and should be encouraged to take a diet rich in vegetables and fruits.
References- Wright JM. A review and update of oral precancerous lesions. Tex Dent J. 1998;115:15–9.
- Villa A, Villa C, Abati S. Oral cancer and oral erythroplakia: an update and implication for clinicians. Aust Dent J. 2011;56:253–6. doi: 10.1111/j.1834-7819.2011.01337.x
- Gale N, Pilch BZ, Sidransky D, et al. Epithelial precursor lesions. In: Barnes L, Eveson JW, Reichart P, Sidranksy D, eds. World Health Organization Classification of Tumours. Pathology and Genetics of Head and Neck Tumors. Lyon, France: IARC Press; 2005. 177-9.
- Premalignant Lesions. https://oralcancerfoundation.org/cdc/premalignant-lesions
- Shafer WG, Waldron CA. Erythroplakia of the oral cavity. Cancer 1975;36:1021-8.
- Leukoplakia and Erythroplakia – Premalignant Squamous Lesions of the Oral Cavity. https://emedicine.medscape.com/article/1840467-overview
- Yang SW, Lee YS, Chang LC, Hwang CC, Luo CM, Chen TA. Clinical characteristics of narrow-band imaging of oral erythroplakia and its correlation with pathology. BMC Cancer. 2015;15:406. Published 2015 May 15. doi:10.1186/s12885-015-1422-7 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4434519
- Lapthanasupkul P, Poomsawat S, Punyasingh J. A clinicopathologic study of oral leukoplakia and erythroplakia in a Thai population. Quintessence Int. 2007;38:e448–55.
- Speight PM. Update on oral epithelial dysplasia and progression to cancer. Head Neck Pathol. 2007 Sep. 1 (1):61-6.
- What Are Oral Cavity and Oropharyngeal Cancers? https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/about/what-is-oral-cavity-cancer.html
- Assessing Oral Malignancies. Am Fam Physician. 2002 Apr 1;65(7):1379-1385. https://www.aafp.org/afp/2002/0401/p1379.html
- A digital manual for the early diagnosis of oral neoplasia. https://screening.iarc.fr/atlasoral_list.php?cat=A3&lang=1
- Reichart PA, Philipsen HP. Oral erythroplakia–a review. Oral Oncol. 2005;41(6):551–561. doi:10.1016/j.oraloncology.2004.12.003
- Vedtofte P, Holmstrup P, Hjørting-Hansen E, Pindborg JJ. Surgical treatment of premalignant lesions of the oral mucosa. Int J Oral Maxillofac Surg. 1987;16(6):656–664. doi:10.1016/s0901-5027(87)80049-8