What is fibromatosis
Fibromatosis refers to a group of conditions characterized by overgrowths of skin and connective tissue tumors called fibromas. These fibromas are usually benign (non-cancerous). Fibromatosis can be classified by a person’s age or by the location of the fibromas. The cause of fibromatosis is often unknown, and treatment depends on the individual disease 1.
There appear to be many different ways to classify fibromatosis. One classification system used is based on age (i.e.: juvenile vs adult fibromatoses) and localization (ie, superficial vs deep fibromatoses).
Whilst most fibromatoses are benign tumors and do not metastasize (spread to other parts of the body), the desmoid tumors although they do not metastasize like malignant cancers can be locally aggressive. They can grow quickly into large tumors that can obstruct vital structures such as major blood vessels, nerves and organs.
Juvenile fibromatosis
- Congenital generalized fibromatosis (infantile myofibromatosis): Congenital fibromatosis (infantile myofibromatosis) is characterized by single or multiple benign tumours that appear to be derived from connective tissue and smooth muscle cells. These tumours may involve the skin and underlying tissues, bones, and/or certain internal organs. They are present at birth or develop within the first few weeks of life. Lesions usually resolve spontaneously, however severe or widespread involvement of internal organs may cause potentially life-threatening complications.
- Aponeurotic fibroma
- Infantile digital fibromatosis: Infantile digital fibromatosis (or fibroma) presents as single or multiple gelatinous or firm pinkish nodules on the fingers or toes of an infant. Similar lesions are occasionally diagnosed elsewhere on the hands, feet, arms or elsewhere on the body. In one-third of cases, they are present at birth. They are rare and are seen in both males and females. Although infantile digital fibromatosis may grow to a size of 2cm, they are harmless and do not usually cause any symptoms unless they rub on the neighboring toe or footwear. The cause of infantile digital fibromatosis is unknown.
- Aggressive infantile fibromatosis
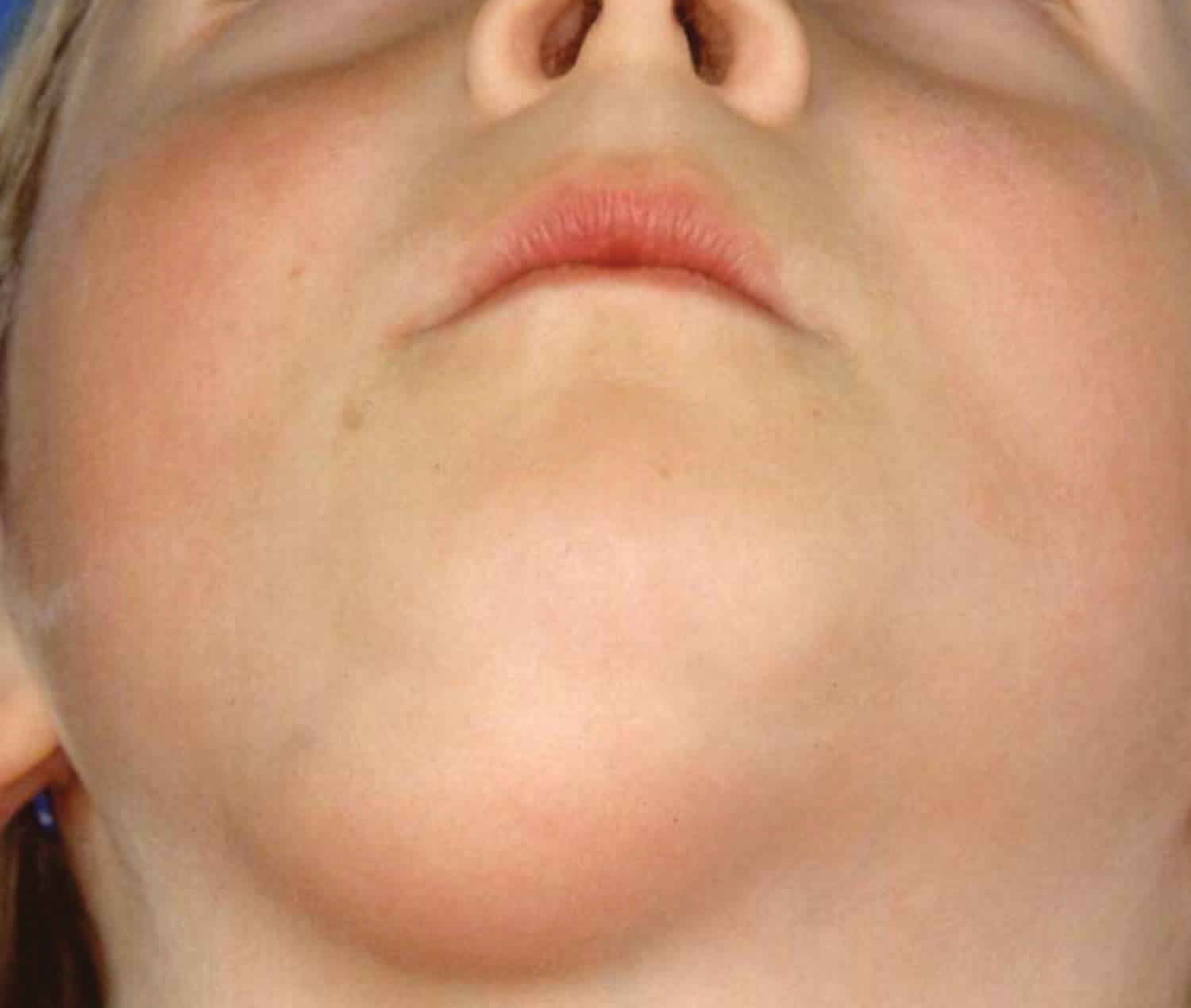
- Fibromatosis colli
- Dermatofibrosis lenticularis (Buschke-Ollendorf syndrome)
Adult fibromatosis
Superficial (fascial) fibromatoses
- Palmar (Dupuytren contracture) and plantar (Ledderhose disease) fibromatosis
- Penile fibromatosis (Peyronie disease)
- Knuckle pads
- Dermatofibroma
- Nodular fasciitis
- Elastofibroma
- Fibrous papule of the face
Deep (musculoaponeurotic) fibromatoses
- Desmoid tumors (aggressive fibromatoses)
- Extra-abdominal fibromatosis
- Abdominal fibromatosis
- Intra-abdominal fibromatosis (eg, pelvic fibromatosis)
Plantar fibromatosis
The term plantar fibromatosis is used for different conditions, as follows: (1) a relatively common plantar equivalent of Dupuytren palmar contracture most commonly termed Ledderhose disease, (2) but also referred to as morbus Ledderhose, a more uncommon plantar superficial fibromatosis that unlike deep fibromatosis (eg, abdominal, extra-abdominal, and visceral fibromatosis), generally has a less aggressive and recurrent tendency; and (3) an extremely rare, benign cerebriform mesodermal hamartomatous proliferation that in a plantar location, appears to be a clinicopathologic marker of Proteus syndrome.
A plantar fibromatosis is a fibrous knot (nodule) that grows on in the arch of the foot on the bottom of the foot and usually appears in the second through sixth decade of life. It is embedded within the plantar fascia, a band of tissue that extends from the heel to the toes on the bottom of the foot. Symptoms consist of a painful mass on the bottom of the foot, roughly in the middle of the arch or instep, between the heel pad and the forefoot pad. The mass will cause a soft convexity in the contour of the bottom of the foot that may be painful with pressure or shoewear. A plantar fibroma can develop in one or both feet, is benign (nonmalignant) and usually will not go away or get smaller without treatment. It is usually slow growing and measures less than an inch in size. More invasive, rapid-growing and multi-planar fibromas are considered plantar fibromatosis. Both of them are benign tumors made up of cells found in ligaments. Definitive causes for this condition have not been clearly identified.
What causes plantar fibroma?
The cause is unknown but thought to have a genetic component. Trauma to the foot does not seem to be a factor.
Plantar fibromatosis signs and symptoms
The characteristic sign of a plantar fibroma is a noticeable lump in the arch that feels firm to the touch. This mass can remain the same size or get larger over time or additional fibromas may develop.
People who have a plantar fibroma may or may not have pain. When pain occurs, it is often caused by shoes pushing against the lump in the arch, although it can also arise when walking or standing barefoot.
Plantar fibromatosis diagnosis
There are a few conditions that can cause soft-tissue masses in the foot, including cysts, swollen tendons or tendon ruptures, nerve tumors (neurilemomas) or fat tumors. Foreign body reactions from previous penetrating trauma can also cause a mass in the bottom of the foot, as can an infection. A more serious synovial cell sarcoma, a malignancy, will usually show calcification on X-ray and a more worrisome appearance on MRI. Clinical exam, X-ray and sometimes an MRI may be needed for diagnosis.
To diagnose a plantar fibroma, the foot and ankle surgeon will examine the foot and press on the affected area. Sometimes this can produce pain that extends down to the toes. An MRI or biopsy may be performed to further evaluate the lump and aid in diagnosis.
Plantar fibromatosis treatment
Nonsurgical treatment may help relieve the pain of a plantar fibroma, although it will not make the mass disappear. The foot and ankle surgeon may select one or more of the following nonsurgical options:
- Steroid injections. Injecting corticosteroid medication into the mass may help shrink it and thereby relieve the pain that occurs when walking. This reduction may only be temporary and the fibroma could slowly return to its original size.
- Orthotic devices. If the fibroma is stable, meaning it is not changing in size, custom orthotic devices (shoe inserts) may relieve the pain by distributing the patient’s weight away from the fibroma.
- Physical therapy. The pain is sometimes treated through physical therapy methods that deliver anti-inflammatory medication into the fibroma without the need for injection.
If the mass increases in size or pain, the patient should be further evaluated.
Surgical treatment to remove the fibroma is considered if the patient continues to experience pain following nonsurgical approaches. Surgical removal of a plantar fibroma may result in a flattening of the arch or development of hammertoes. Orthotic devices may be prescribed to provide support to the foot. Due to the high incidence of recurrence with this condition, continued follow-up with the foot and ankle surgeon is recommended.
Plantar fibromatosis surgery
Surgery is done for symptomatic fibromas when conservative treatment fails to give adequate pain relief. The recurrence rate is low for fibromas and significantly higher for plantar fibromatosis and in revision cases. Risks of surgery include wound complications, injury to local structures such as the digital nerves, and recurrence.
Recovery may be hastened by elevation of the foot and diligent control of swelling to help prevent blood clot formation and delayed wound healing. You may need to take one to two weeks off work after surgery, if you can keep your foot elevated and stay on crutches, or longer if this is not possible. Return to unrestricted activity and shoewear is in the one- to two-month range.
Recurrence is rare for fibromas but more common in multiple lesions or if invasive lesions are encountered.
Potential complications include wound drainage or infection, a healed but painful wound, the return of a mass, and chronic neuritic pain, especially for an invasive lesion or in revision surgery.
Desmoid fibromatosis
A desmoid tumor is an abnormal growth that arises from connective tissue, which is the tissue that provides strength and flexibility to structures such as bones, ligaments, and muscles. Typically, a single tumor develops, although some people have multiple tumors. The tumors can occur anywhere in the body. Tumors that form in the abdominal wall are called abdominal desmoid tumors; those that arise from the tissue that connects the abdominal organs are called intra-abdominal desmoid tumors; and tumors found in other regions of the body are called extra-abdominal desmoid tumors. Extra-abdominal tumors occur most often in the shoulders, upper arms, and upper legs.
Desmoid tumors are fibrous, much like scar tissue. They are generally not considered cancerous (malignant) because they do not spread to other parts of the body (metastasize); however, they can aggressively invade the surrounding tissue and can be very difficult to remove surgically. These tumors often recur, even after apparently complete removal.
The most common symptom of desmoid tumors is pain. Other signs and symptoms, which are often caused by growth of the tumor into surrounding tissue, vary based on the size and location of the tumor. Intra-abdominal desmoid tumors can block the bowel, causing constipation. Extra-abdominal desmoid tumors can restrict the movement of affected joints and cause limping or difficulty moving the arms or legs.
Desmoid tumors are rare, affecting an estimated 1 to 2 per 500,000 people worldwide. In the United States, 900 to 1,500 new cases are diagnosed per year. Sporadic desmoid tumors are more common than those associated with familial adenomatous polyposis.
Desmoid tumors occur frequently in people with an inherited form of colon cancer called familial adenomatous polyposis (FAP). These individuals typically develop intra-abdominal desmoid tumors in addition to abnormal growths (called polyps) and cancerous tumors in the colon. Desmoid tumors that are not part of an inherited condition are described as sporadic.
What causes desmoid fibromatosis?
Mutations in the CTNNB1 gene or the APC gene cause desmoid tumors. CTNNB1 gene mutations account for around 85 percent of sporadic desmoid tumors. APC gene mutations cause desmoid tumors associated with familial adenomatous polyposis as well as 10 to 15 percent of sporadic desmoid tumors. Both genes are involved in an important cell signaling pathway that controls the growth and division (proliferation) of cells and the process by which cells mature to carry out specific functions (differentiation).
The CTNNB1 gene provides instructions for making a protein called beta-catenin. As part of the cell-signaling pathway, beta-catenin interacts with other proteins to control the activity (expression) of particular genes, which helps promote cell proliferation and differentiation. CTNNB1 gene mutations lead to an abnormally stable beta-catenin protein that is not broken down when it is no longer needed. The protein accumulates in cells, where it continues to function in an uncontrolled way.
The protein produced from the APC gene helps regulate levels of beta-catenin in the cell. When beta-catenin is no longer needed, the APC protein attaches (binds) to it, which signals for it to be broken down. Mutations in the APC gene that cause desmoid tumors lead to a short APC protein that is unable to interact with beta-catenin. As a result, beta-catenin is not broken down and, instead, accumulates in cells. Excess beta-catenin, whether caused by CTNNB1 or APC gene mutations, promotes uncontrolled growth and division of cells, allowing the formation of desmoid tumors.
Most desmoid tumors are sporadic and are not inherited. Sporadic tumors result from gene mutations that occur during a person’s lifetime, called somatic mutations. A somatic mutation in one copy of the gene is sufficient to cause the disorder. Somatic mutations in either the CTNNB1 or the APC gene can cause sporadic desmoid tumors.
An inherited mutation in one copy of the APC gene causes familial adenomatous polyposis and predisposes affected individuals to develop desmoid tumors. The desmoid tumors occur when a somatic mutation occurs in the second copy of the APC gene. In these cases, the condition is sometimes called hereditary desmoid disease.
Desmoid fibromatosis treatment
Aggressive, wide surgical resection is the treatment of choice 2. Complete surgical excision of desmoid tumors is the most effective method of cure. This sometimes necessitates removal of most of an anterior compartment of a leg. Extensive cases may require excision plus adjuvant treatment including chemotherapy and repeat surgery 3. Positive margins (incomplete resections) after surgery reflect a high risk for recurrence 4. Surgery plus the administration of nonsteroidal anti-inflammatory medication, hormonal therapy, and cytotoxic chemotherapy is sometimes used, the latter being the most effective pharmacological approach 5. In selected patients, radical resection with intraoperative margin evaluation by frozen sections followed by immediate mesh reconstruction may be a safe and effective procedure providing definitive cure yet minimizing functional limitations 6.
Lesions involving the extremities and deep soft tissues of the trunk have a higher risk of recurrence, as do Gardner syndrome–associated lesions in other locations 7.
For tumors that are asymptomatic or nonprogressive, some prefer a wait-and-see approach 8.
In those patients who refuse surgery or are not surgical candidates, the options below may be considered.
Radiation therapy may be used as a treatment for recurrent disease or as primary therapy to avoid mutilating surgical resection. It may be used postoperatively, preoperatively, or as the sole treatment 9.
Pharmacologic therapy with antiestrogens and prostaglandin inhibitors may also be used. Pharmacologic agents result in objective response rates of approximately 40-50%; the duration of response is variable 10.
In cases of recurrent extra-abdominal desmoid tumors in which surgery is contraindicated or in cases of recurrence, a chemotherapeutic regimen of doxorubicin, dacarbazine, and carboplatin may be effective. Intra-abdominal desmoid tumors as a part of Gardner syndrome may respond to systemic doxorubicin, and ifosfamide can be useful for patients with complications from the tumor 11. Polychemotherapy has been used 12 and can be combined with targeted therapy with imatinib 13.
Expanded knowledge of familial adenomatosis polyposis–desmoid tumor molecular underpinnings may aid in the development of novel therapeutic strategies 14.
Magnetic resonance‒guided high-intensity focused ultrasound may prove a safe and effective option for selected desmoid tumors 15.
Systemic therapy is appropriate if a primary complete resection is not feasible or if there is relapse or progression after resection 16. There are a number of novel drug therapy candidates for desmoid tumors 17. Pazopanib, a potent tyrosine kinase inhibitor, represents a promising new therapy for desmoid tumors in adolescent and young adult patients 18.
Split-course radiotherapy in patients with desmoid tumors was well tolerated with good outcomes 19.
Long-Term Monitoring
After surgery, MRI may be useful for monitoring desmoid tumor recurrence.
What are the features of fibromatosis?
The following table lists the distinguishing features between superficial and deep fibromatoses.
Superficial fibromatoses
- Slow growing tumor
- Small size
- Arise from fascia or aponeurosis
- Less aggressive
Deep fibromatoses
- Rapidly growing pseudotumor
- Usually, they reach a large size
- Often involve deeper structures (muscles of the trunk and extremities)
What causes fibromatosis?
The cause of fibromatosis remains unclear. In some types of fibromatosis such as desmoid tumors, it is thought that the condition may be related to trauma, hormonal factors, or have a genetic association. Superficial fibromatoses such as palmar, plantar and penile fibromatosis have sometimes been linked to certain diseases such as diabetes, liver disease and hypertension.
Fibromatosis treatment
Management of fibromatosis depends on individual disease.
- Congenital generalized fibromatosis (infantile myofibromatosis)
- Aponeurotic fibroma
- Infantile digital fibromatosis: Eventually, many fibromatosis resorb and disappear by themselves over 2 to 3 years so that a conservative wait and see approach is best if they are not causing problems. If desired, they can be removed by a simple surgical procedure in which the lump is shaved off. However, many recur after surgery.
- Aggressive infantile fibromatosis
- Fibromatosis colli
- Dermatofibrosis lenticularis (Buschke-Ollendorf syndrome)
- Palmar (Dupuytren disease) and plantar (Ledderhose disease) fibromatosis
- Penile fibromatosis (Peyronie disease)
- Knuckle pads
- Dermatofibroma
- Nodular fasciitis
- Elastofibroma
- Fibrous papule of the nose or face
- Desmoid tumours (aggressive fibromatoses).
- Fibromatosis. https://www.dermnetnz.org/topics/fibromatosis/
- Soto-Miranda MA, Sandoval JA, Rao B, Neel M, Krasin M, Spunt S, et al. Surgical Treatment of Pediatric Desmoid Tumors. A 12-Year, Single-Center Experience. Ann Surg Oncol. 2013 Jul 10.
- Ramirez RN, Otsuka NY, Apel DM, Bowen RE. Desmoid tumor in the pediatric population: a report of two cases. J Pediatr Orthop B. 2009 May. 18(3):141-4
- Buitendijk S, van de Ven CP, Dumans TG, et al. Pediatric aggressive fibromatosis: a retrospective analysis of 13 patients and review of literature. Cancer. 2005 Sep 1. 104(5):1090-9.
- Inoue Y, Ishida H, Ueno H, Kobayashi H, Yamaguchi T, Konishi T, et al. The treatment of desmoid tumors associated with familial adenomatous polyposis: the results of a Japanese multicenter observational study. Surg Today. 2017 Mar 1.
- Bertani E, Chiappa A, Testori A, et al. Desmoid tumors of the anterior abdominal wall: results from a monocentric surgical experience and review of the literature. Ann Surg Oncol. 2009 Jun. 16(6):1642-9
- Cates JM, Stricker TP, Sturgeon D, Coffin CM. Desmoid-type fibromatosis-associated Gardner fibromas: prevalence and impact on local recurrence. Cancer Lett. 2014 Oct 28. 353(2):176-81.
- Oudot C, Defachelles AS, Minard-Colin V, Olschwang S, Fourcade L, Helfre S, et al. [Desmoid tumors in children: current strategy]. Bull Cancer. 2013 May. 100(5):518-28.
- El-Haddad M, El-Sebaie M, Ahmad R, et al. Treatment of aggressive fibromatosis: the experience of a single institution. Clin Oncol (R Coll Radiol). 2009 Dec. 21(10):775-80.
- Mendenhall WM, Zlotecki RA, Morris CG, Hochwald SN, Scarborough MT. Aggressive fibromatosis. Am J Clin Oncol. 2005 Apr. 28(2):211-5.
- Bhama PK, Chugh R, Baker LH, Doherty GM. Gardner’s syndrome in a 40-year-old woman: successful treatment of locally aggressive desmoid tumors with cytotoxic chemotherapy. World J Surg Oncol. 2006 Dec 17. 4:96.
- Constantinidou A, Jones RL, Scurr M, Al-Muderis O, Judson I. Advanced aggressive fibromatosis: Effective palliation with chemotherapy. Acta Oncol. 2010 Aug 30.
- Knechtel G, Stoeger H, Szkandera J, Dorr K, Beham A, Samonigg H. Desmoid tumor treated with polychemotherapy followed by imatinib: a case report and review of the literature. Case Rep Oncol. 2010 Aug 6. 3(2):287-93.
- Colombo C, Foo WC, Whiting D, Young ED, Lusby K, Pollock RE, et al. FAP-related desmoid tumors: a series of 44 patients evaluated in a cancer referral center. Histol Histopathol. 2012 May. 27(5):641-9.
- Avedian RS, Bitton R, Gold G, Butts-Pauly K, Ghanouni P. Is MR-guided High-intensity Focused Ultrasound a Feasible Treatment Modality for Desmoid Tumors?. Clin Orthop Relat Res. 2016 Mar. 474 (3):697-704.
- Sparber-Sauer M, Seitz G, von Kalle T, Vokuhl C, Leuschner I, Scheer M, et al. Systemic therapy of aggressive fibromatosis in children and adolescents: Report of the Cooperative Weichteilsarkom Studiengruppe (CWS). Pediatr Blood Cancer. 2018 Jan 5.
- Mercier KA, Al-Jazrawe M, Poon R, Acuff Z, Alman B. A Metabolomics Pilot Study on Desmoid Tumors and Novel Drug Candidates. Sci Rep. 2018 Jan 12. 8 (1):584.
- Agresta L, Kim H, Turpin BK, Nagarajan R, Plemmons A, Szabo S, et al. Pazopanib therapy for desmoid tumors in adolescent and young adult patients. Pediatr Blood Cancer. 2018 Jan 31.
- Luo J, Jin K, Qian S, Ma X, Pan Z, Yao W, et al. Single institution experience of split course radiotherapy in patients with desmoid tumors. Onco Targets Ther. 2019. 12:1741-1748.