Fibular hemimelia
Fibular hemimelia is a birth defect where part or all of the fibular bone is partially or completely missing in the lower leg. This shortens the affected leg; there is also usually a lower leg deformity or bow and an abnormally positioned foot with missing toes. Although most of the limb abnormalities are concentrated in the lower leg and foot, the entire lower extremity (from the hip to the toes) is affected by this condition. The most inclusive medical term for this condition is post-axial hypoplasia of the lower limb. This means that one side of the limb bud (post-axial side – small toe side) was altered resulting in an abnormal growth pattern.
Children with fibular hemimelia have five main problems with their affected limb:
- limb length discrepancy
- foot and ankle deformities and deficiencies
- tibial deformity
- genu valgum or “knock-knee” (where the knees angle in and touch each other when the legs are straightened)
- knee instability
Fibular hemimelia is a congenital deficiency where part or all of the fibular bone is hypoplastic, dysplastic or aplastic associated with hypoplasia and dysplasia of the tibia and hypoplasia, dysplasia and aplasia of parts of the foot 1. Fibular hemimelia signs and symptoms have a wide spectrum of pathology, ranging from mild to severe limb length discrepancy, ankle/foot deformities with or without subtalar coalition, midfoot coalitions and absent rays. Knee ligament deficiencies and knee valgus deformity as well as associated femoral hypoplasia, dysplasia and partial aplasia are common. It is therefore part of the same spectrum of deficiency as congenital femoral deficiency. These are commonly referred to as postaxial deficiencies and are distinct in their pattern from preaxial deficiencies such as tibial hemimelia.
Fibular hemimelia is a very rare disorder, occurring in only 1 in 40,000 births. To put this into perspective, the United States of America usually averages about 4,000,000 live births per year. This results in 100 live births with fibular hemimelia per year in the United States. Bilateral fibular hemimelia (affecting both legs) is even rarer.
It is currently unknown why fibular hemimelia occurs. Research has demonstrated that if the genes guiding the formation of the limb are activated in an abnormal order, fibular hemimelia can occur. Other studies have demonstrated that isolated mutations of genes in the forming limb bud can lead to fibular hemimelia. Although genetic abnormalities are linked to fibular hemimelia, the condition is not heritable. The gene mutations and abnormalities are occurring only in the forming limb and not anywhere else, and thus cannot be transmitted to the next generation.
Furthermore, the vast majority of children born with this condition have no family history of other birth defects. Neither the parents of the child with fibular hemimelia nor the child themselves have any increased risk of producing additional children with this or other birth defects.
Children with fibular hemimelia present with three major complaints:
- Limb length discrepancy
- Foot and ankle deformities
- Knee deformity
Treatment in general depends upon the function of the hip, knee, and ankle joints, as well as the current and final projected limb length differences. Most children with fibular hemimelia will have projected differences at skeletal maturity > 2 inches. In fact, many children have final differences projected at 4-6 inches. The difference in leg lengths generally increases in proportion to the child’s overall growth so the final discrepancy can be predicted. This difference will often need to be treated because differences greater than ¾” may lead to painful problems in the future.
There is very little role for nonsurgical options for the ultimate treatment of fibular hemimelia, unless the ankle joint is essentially normal and the projected final difference between the limbs is less than ¾”. However, there are nonsurgical treatments needed for every child with fibular hemimelia.
- Physical Therapy: For every child with fibular hemimelia, physical therapy will be a necessity, whether it is to learn how to walk with a prosthesis or how to keep the knee and ankle limber during a limb lengthening surgery.
- Orthoses/Shoe lifts: Many children that are undergoing limb lengthening will need orthotics and shoe lifts to help “even out” the limb lengths during childhood. Internal shoe lifts can be made up to ½”. Lifts greater than ½” need to be placed outside of shoes, because the heel will not fit in the shoe otherwise. In addition, the child may need a brace such as a supramalleolar orthosis (SMO) or ankle foot orthosis (AFO). Supramalleolar orthosis provides side to side ankle support, while ankle foot orthosis provides more support to the bottom of the ankle. Your physician will prescribe the appropriate brace for your child.
- Prosthetic Fitting: If limb ablation is ultimately the decision made to treat a child with fibular hemimelia, then they will need long term care with a prosthetist. A pediatric prosthetist with experience working with children after amputations for fibular hemimelia is certainly preferable. Prosthetic technology continues to advance at a rapid rate. In addition, as the child ages, the prosthetic options also increase over time.
In general, the goal for children with differences in limb lengths is to have two limbs nearly equal in length and as functional and pain-free as possible by the time a child is fully grown. To achieve this goal, first the surgeon must examine the child for the function of his/her surrounding joints, and then calculate an estimated final projected difference. Based on this information, the decision then is made between the orthopaedic surgeon and the family whether a limb lengthening and reconstruction is the best option for treatment, or possibly a limb ablation (amputation) and prosthetic fitting. If limb reconstruction is chosen, your doctor will walk you through a “life plan” that discusses the surgical procedures recommended for your child and the anticipated timing of these surgeries.
The decision for limb ablation (amputation) versus reconstruction is obviously a very critical decision and should be discussed thoroughly with an orthopedic surgeon familiar at managing these limb length differences. The greater the projected difference, the more limb lengthening surgeries are needed to even out the limbs. In addition, most of the time, for the limbs that are very short initially in comparison to the other side, the joint may be more abnormal, and even if they can be “fixed” they may be painful and not as functional as a prosthesis. Again, there are many, many factors that weigh in to this decision, and consultation with a limb deformity specialist is recommended.
Surgical treatment:
- Limb Ablation – If the decision is made to amputate the limb in a growing children, amputations are typically made through a joint rather than through a bone itself. The two most common types of amputations are either a Symes or a Boyd amputation through the ankle joint. Both of these preserve the heel pad to provide a good surface to interface with the prosthetic. Once the child heals from the amputation surgery, he/she is fitted for a prosthesis. The surgery can be performed as young as 10 months, right before the child is pulling up to stand. If needed, the surgery can be delayed as well, especially if a family needs more time making this decision.
- Epiphysiodesis surgery – An epiphysiodesis is a surgery performed to stop the growth on the longer leg. This procedure “shortens” the longer leg. It is typically recommended for projected limb length differences between 2-5 cm (3/4”-2”), while lengthening is preferred for differences of greater than 2”. In this procedure, the growth area (physis) is drilled surgically. The growth area is made of cartilage, and after the surgery, the cartilage hole heals itself, but fills in with bone. Once bone fills up this hole, the bone can no longer grow. Some surgeons also use metal implants as a part of this procedure. The surgeon may also recommend epiphysiodesis as part of the “life plan”. For example, if a child has a projected 12 cm limb length difference, the surgeon may recommend 2 separate 5 cm limb lengthenings, and then an epiphysiodesis of the longer (normal) side when there is 2 cm left of growth to make up the remainder of the difference.
- Limb lengthening and reconstruction
- Ankle reconstruction: The term “superankle” was first coined by Dr. Dror Paley in 1996 1. The surgery itself has been modified from time to time since then. Nonetheless, the superankle surgery refers to an ankle joint reconstruction performed prior to limb lengthening. Prior to any limb lengthening, whether it is for fibular hemimelia, femoral deficiency, etc., the joints need to be in as normal of a position as possible. Specific to fibular hemimelia, as mentioned above, the ankle joints are often abnormal. Many have contractures that point the foot down and out (equinus and eversion), and many times there is a tarsal coalition in which two of the foot bones (typically the calcaneus and talus bones) are stuck together. During this ankle reconstruction surgery, the gastrocnemius muscle and peroneal muscles are often lengthened, the tarsal coalition is released, and many times, the bottom portion of the ankle joint is realigned (known as a supramalleolar osteotomy). Lastly, a portion of the anlage (the cartilaginous remnant of the fibula bone) is also removed. After the surgery, the surgeon may place a child in a cast and allow the ankle to heal. Some surgeons will place an external fixator on at this time and begin the limb lengthening process. There are pluses and minuses to each method, and further details should be discussed with the surgeon.
- Limb lengthening with external fixator.
- Limb lengthening with internal lengthening nail.
What are the chances that a second child in the same family will have fibular hemimelia?
The chances of a second child having fibular hemimelia are the same as the first, 1 in 40,000. Since this genetic mutation is spontaneous, there is no increased risk of having a second child with fibular hemimelia.
What are the chances that a person with fibular hemimelia will have a child with fibular hemimelia?
A person with fibular hemimelia has a 1 in 40,000 chance of having a child with fibular hemimelia. Since this genetic mutation is spontaneous, there is no increased risk of fibular hemimelia being passed down to the next generation.
Will a child with fibular hemimelia learn to walk?
The children do just fine and nothing stops them from walking. Even with a severe foot and ankle deformity and a leg length discrepancy, a child will adapt and walk usually between 12 and 16 months of age. If weight bearing on the affected limb appears to be placing forces across the foot and ankle that push the foot into a more deformed position, then a small lower leg brace will be used as mentioned above. This is a temporary problem due to the fact that the initial reconstruction is performed at the age of 18 to 24 months.
Fibular hemimelia types
Fibular hemimelia is not one condition where all of the cases have the same amount of deformity or deficiency or limb length discrepancy. Consequently, to facilitate the physicians’ recommendation of a specific treatment, fibular hemimelia is classified into different groups according to degree of severity. There are numerous classifications of fibular hemimelia 2, with the majority of these limited by the fact that they were developed at a time when surgical reconstruction for fibular hemimelia was unsuccessful and when amputation was the primary or only consideration for treatment. Therefore, the different groups of fibular hemimelia that have been described in the various classifications do not relate to the different types of treatment that are currently available. Most are only descriptive and recommend Syme’s amputation independent of the type of fibular hemimelia. The most commonly used classification is that of Achterman and Kalamchi 3, which describes the amount of fibular deficiency. Experts now know that the amount of leg length discrepancy and foot deformity, which are the two biggest problems in fibular hemimelia, do not correlate to the amount of fibula that is missing. The best prognostic factor is the foot deformity itself. Therefore, a classification based on the foot deficiency is needed. Birch et al. 4 classified fibular hemimelia according to the number of rays of the foot and recommended amputation for most cases with less than three rays.
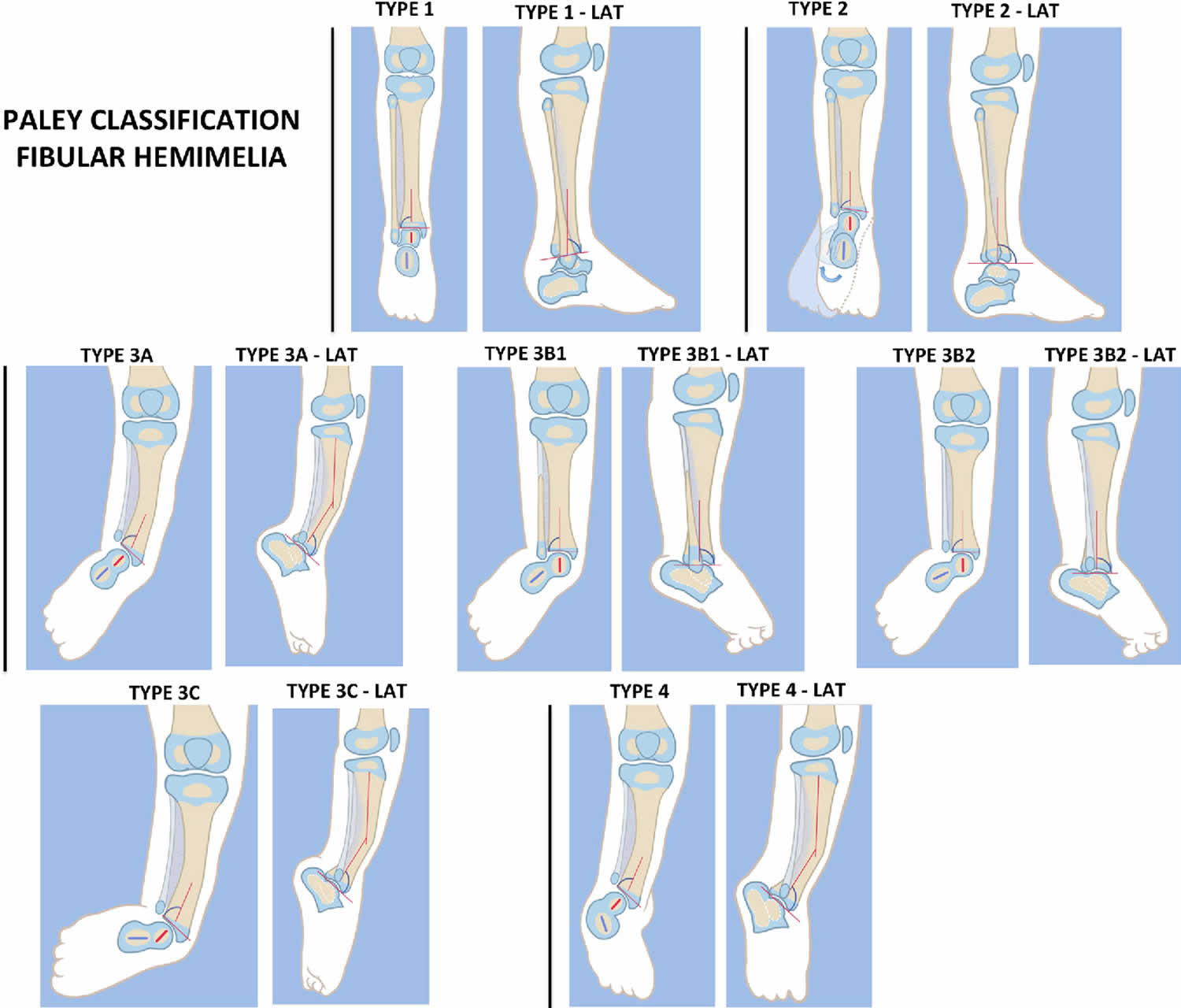
The Paley classification (Figure 2) is the first classification of fibular hemimelia to be designed with reconstructive surgery options in mind 2. It is based on the patho-anatomy and deformities of the ankle and subtalar joint. Each Paley classification type has a different surgical treatment; it is independent of the number of rays or the leg length discrepancy. The Paley classification of fibular hemimelia describes of four types of fibular hemimelia, with type 3 subdivided into three subtypes, as shown in the following list.
- Type 1 Stable ankle. In many cases the ankle of type 1 cases appears completely normal, and the fibula is only slightly shorter at its upper end compared to the opposite side. There are some type 1 cases with complete fibular aplasia. The predicted leg length discrepancy in type 1 cases is typically less than 5 cm (2 in.).
- Type 2 Dynamic valgus. The foot in these cases can be brought into a plantigrade position. There is no fixed equino-valgus. Most feet have a ball and socket ankle joint with a fibula that is relatively short compared to the tibia at the level of the ankle joint. The normal fibula has its distal physis at the level of the ankle mortise. When the fibula is short distally, its distal physis is proximal to the ankle joint. While the foot can be placed plantigrade, the ankle naturally rolls outwards, and the patient stands and walks in valgus. There is often limited dorsiflexion in this group but not fixed equinus.
- Type 3 Fixed equino-valgus. There is a fixed deformity of equino-valgus. In some cases the foot can be brought out of equinus with obligatory valgus. When the heel is held out of valgus in a neutral position, there is a fixed equinus deformity. This fixed equino-valgus can be divided into three groups:
- Type 3A Ankle type. The fixed equino-valgus deformity is due to a malorientation of the ankle joint (distal tibial epiphysis is in procurvatum-valgus; the LDTA is decreased and ADTA is increased).
- Type 3B Subtalar type. There is a malunited subtalar coalition. The calcaneus is located lateral to the talus and is often tilted into valgus relative to the body of the talus. If there is a fibula with distal fibular physis and lateral malleolus present (3B1), it is proximally migrated and articulates with the dorsal surface of the calcaneus. The same deformity can occur without a fibula (3B2).
- Type 3c Combined subtalar and ankle type. Both distal tibial malorientation and malunited subtalar coalition are present.
- Type 4 Fixed equino-varus. The only difference between type 3B or 3C and type 4 is that the subtalar coalition is malunited in varus in the former. In most of these cases the distal tibia is also maloriented into procurvatum and valgus. This type can be misdiagnosed as a clubfoot. It its resistant to Ponsetti casting as well as clubfoot releases of the subtalar joint since there is a subtalar coalition.
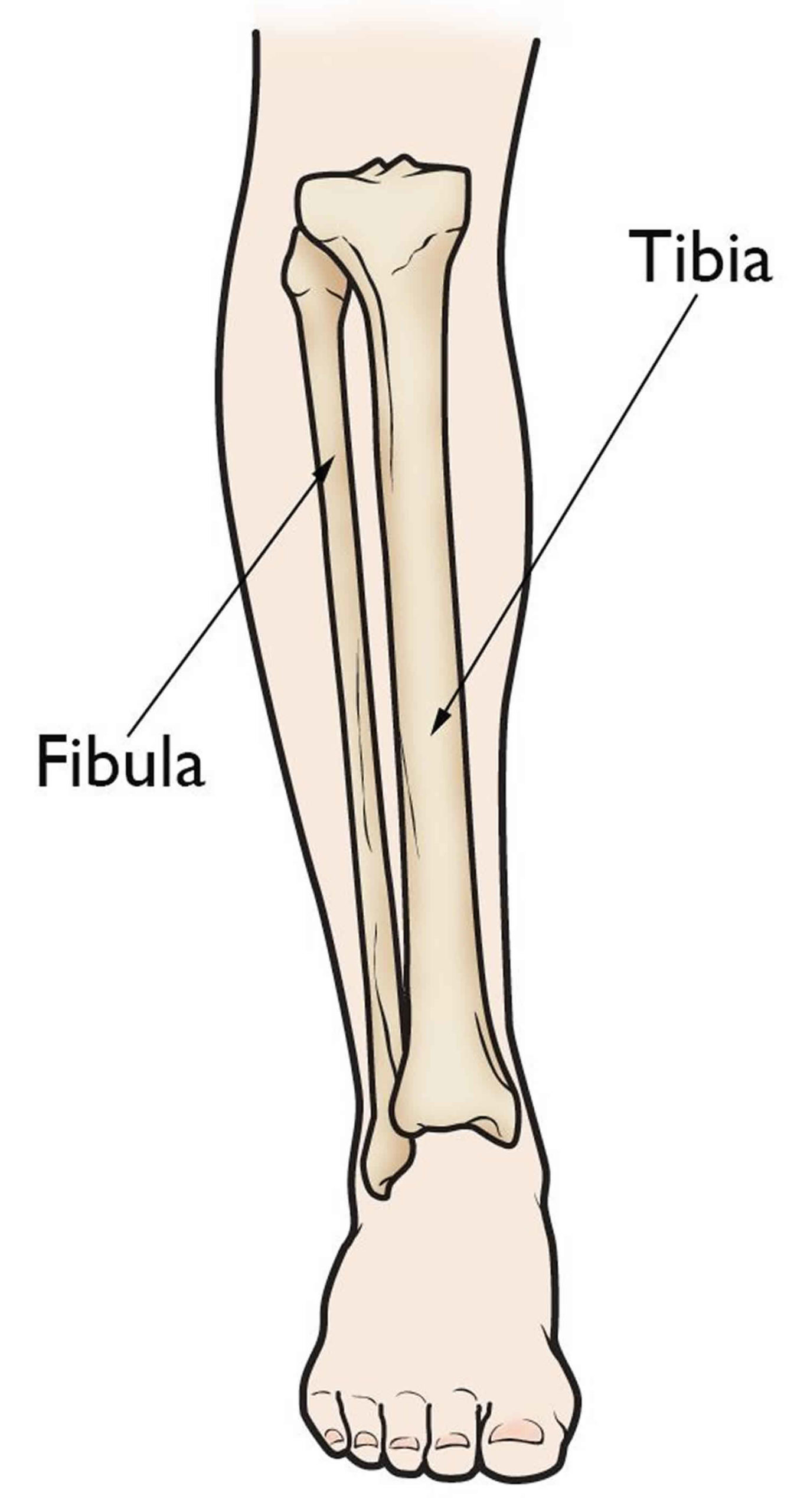
Figure 1. Normal leg bones
Footnote: Fibular hemimelia is a partial or total absence of the fibula, which is the smaller bone in your lower leg.
Figure 2. Fibular hemimelia types
Footnote: Paley classification of fibular hemimelia. Type 1 Stable ankle, Type 2 dynamic valgus ankle, Type 3 fixed equinovalgus ankle, 3A Ankle type, 3B subtalar type, 3C combined ankle/subtalar, Type 4 fixed equino-varus ankle. LAT = lateral.
[Source 1 ]Fibular hemimelia causes
The exact cause of fibular hemimelia remains unknown and in most cases it is usually not an inheritable condition, with the vast majority of children born with this condition having no family history of other birth defects 1. A spontaneous genetic error occurs during limb bud development. This growth abnormality occurs during the development of the lower limb bud at six to eight weeks after conception. This “blue print” error resides only in the cells of the limb bud of the developing fetus, not in any reproductive cells from the parents.
The exception to this is when fibular hemimelia is associated with deficiency in more than one limb; for example, bilateral fibular hemimelia is often an autosomal dominant condition. When multiple limbs are affected by a limb deficiency, one can often assume that this was either an autosomal-dominant gene disorder (inherited or new mutation) or related to a teratologic agent (drug, radiation, virus, etc.). Fibular hemimelia has been reproduced in a mouse model 5, suggesting that in most cases it may be a somatic gene mutation, although this theory has not been confirmed.
Fibular hemimelia signs and symptoms
Many children with fibular hemimelia can be diagnosed at birth or soon thereafter. Fibular hemimelia does not cause pain. The difference in limb lengths is often noticeable at birth.
The severity of fibular hemimelia has a wide spectrum. For example, one child may have a predicted 5-cm (2-inch) mild leg length discrepancy, five toes/rays present on the foot, and mild instability of the ankle. However, another child might have a predicted leg length discrepancy of 30 cm (12 inches), two or three toes present on the foot, and a very stiff ankle joint. Usually patients with a more severe form of fibular hemimelia will have more effects in the hip joint, femur and knee joint.
The most obvious effects of fibular hemimelia are limb shortening, lower leg deformity or bow, and an abnormally positioned foot with missing toes. However, there are other effects that are more subtle and do not become obvious until later in life. The hip joint can be mildly dysplastic, meaning the cup of the hip joint is shallow. There usually is a difference in length between the normal femur (thigh bone) and the femur with fibular hemimelia. This length difference can be minimal or very significant. The femur usually has an outward twist termed external femoral torsion, which can result in an out-toeing gait. The knee is always unstable to some degree due to the absence or abnormality of the ligaments inside the knee joint. The tibia (shin bone) is always shorter on the affected side with an abnormally positioned ankle and/or foot. The tibia usually has a dimple on the front side of the leg marking the bow or deformity in the tibia.
The fibula (small bone in the lower leg) can be partially or totally absent. When the fibula is totally absent on the X-rays, there is always a fibrous remnant connected to the calcaneus (heel bone) that is very tight and contracted. This fibrous fibula remnant is termed the fibular anlage. This tight band of tissue causes the foot and ankle to rotate outwards and the lower leg to grow in a valgus (knocked knee) direction. The foot’s toe down position (equinus contracture) is caused by the malalignment (misdirection) of the ankle joint and the tight heel cord/calf muscle. The ankle joint not only points down, but it also points in an outward direction. This is termed ankle valgus. When severe ankle valgus is present, this gives the appearance that the patient is walking on the inner side of the ankle. The ankle position is a combination of the above stated factors that are all related to fibular hemimelia.
The foot in fibular hemimelia is affected in various ways. The most obvious is the absence of the lateral digits or rays. The number of digits present on the foot with fibular hemimelia is extremely variable. Some patients retain all five digits whereas others might have only two digits. There is a common misconception among pediatric orthopedic doctors that the number of toes determines the functionality of the foot. The International Center for Limb Lengthening doctors strongly disagree with this thought process. Every foot with fibular hemimelia is unique and must be examined carefully to determine the functionality. Simply counting existing toes does not allow anyone to predict the function of the foot in the future.
Another foot anomaly that is very consistent in fibular hemimelia is called tarsal coalition. A tarsal coalition is when some of the bones in the foot are not separated. In fibular hemimelia, the ankle bone (talus) is usually fused or coalesced to the heel bone (calcaneus). This results in the absence of the subtalar joint. The subtalar joint is the joint between the ankle bone and heel bone that allows the foot and ankle to rock side to side. In response to the bones in the foot being fused, the ankle joint will form into a ball-in-socket type of configuration instead of the normal hinge joint.
The ball-in-socket configuration allows for all of the normal ankle motion of toe up (dorsiflexion) and toe down (plantar flexion) along with the side to side rocking motion (eversion and inversion) to come from one joint instead of two joints in a normal ankle. The benefit of this ball-in-socket adaptation is to allow all “normal” motion that a normal ankle would possess. The disadvantage of this ball-in-socket ankle joint is the potential for the foot and ankle to angle outward giving a “squashed” foot/ankle appearance that is termed dynamic ankle valgus. Dynamic means that the deformity appears when the joint is stressed by weight bearing. Ankle valgus means a “knocked knee” appearance of the ankle.
The tarsal coalition (fusion of the foot bones) in patients with fibular hemimelia creates a second issue besides the ball-in-socket adaptation of the ankle joint. The ankle bone (talus) and heel bone (calcaneus) are usually fused in an abnormal position with the heel bone (calcaneus) lying next to the ankle bone (talus) instead of underneath the ankle bone. This awkward position of the ankle and heel bones exaggerates the pushed out appearance of the foot.
In the same way that the number of digits varies among patients, the amount of motion at the ankle joint is also variable. Some patients will have normal motion at the ankle while others will have very stiff and immobile ankle joints. Once again, many orthopedists will decide the foot and ankle cannot be reconstructed due to stiffness in the ankle joint. The International Center for Limb Lengthening doctors strongly disagree. A foot and stiff ankle joint that has correct alignment is a very stable and functional limb. During the reconstruction and lengthening, the amount of ankle motion that a patient starts with is approximately the same ankle motion that the limb will have at the end of reconstruction.
Limb length discrepancy
Unilateral fibular hemimelia leads to a limb length discrepancy due to inhibition of growth of the tibia and foot. In addition, many children with fibular hemimelia have some femoral growth inhibition (congenital femoral deficiency). The foot grows shorter in height, contributing to limb length discrepancy, but it is also shorter in length. This limb length discrepancy follows a Shapiro 1a curve, meaning its growth inhibition remains constant 6. This characteristic makes the leg length discrepancy of fibular hemimelia predictable using the Anderson and Green 7, Moseley straight line graph 8, Amstutz method 9 or Paley Multiplier method 10. The limb length discrepancy with fibular hemimelia ranges from very mild to very severe inhibition, ranging at maturity of the patient from 2 to 25 cm in the absence of femoral deficiency discrepancy. With combined inhibition of the femur and tibia the magnitude of leg length discrepancy at maturity can be >30 cm.
Foot and ankle deformities
Foot and ankle deformities have been the most challenging and disabling problems with fibular hemimelia. Fibular hemimelia foot deformity has many components. At the ankle there is a dysplasia of the distal tibia and of the talus, which ranges from mild valgus of the distal tibia to severe dysplasia with flat malformed, maloriented joint surfaces. The distal tibial physis is more affected then the proximal tibial physis, with the former being often wedge shaped. The joint surface of the distal tibia ranges from a normal plafond with a 90° lateral distal tibial angle (LDTA) and 80° anterior distal tibial angle (ADTA) to a valgus plafond with an lateral distal tibial angle of <90° and an anterior distal tibial angle of >80° (procurvatum). The distal tibial articular surface is often concave in the frontal plane as part of a ball and socket ankle joint. The talus too ranges in its articular shape from normal to ball shaped in the frontal plane and from round to nearly flat in the sagittal plane. The talar neck may be very short and have little concave offset. The ankle joint function with fibular hemimelia may range from: normal range of motion, stable, no valgus instability, and no deformity; to, limited arc of motion, unstable with valgus instability, and fixed equino-valgus or varus deformity. Part of this deformity and instability is related to the fibular deficiency and part to the subtalar pathology. The fibula normally contributes to the lateral stability of the ankle. If the fibula is absent or deficient, then the ankle will sublux or roll into valgus. The subtalar joint pathology ranges from a normal subtalar joint to a subtalar joint with subtalar coalition. This subtalar coalition usually involves the posterior facet and is often malunited into equino-valgus. In a small minority of cases the subtalar coalition is malunited into equino-varus (clubfoot type). The combination of a malunited coalition, with valgus ankle joint instability, with a maloriented distal tibia produces a very significant magnitude of equino-valgus deformity of the foot and ankle. This foot malorientation is also associated with contractures of the tendo-Achilles and peroneal tendons. A further tether into equino-valgus may come from the fibular remnant referred to as the anlage. This anlage may be fibrous or both fibrous and cartilaginous. In some cases there is coalition of the cartilaginous fibular anlage to the calcaneus. Much of this patho-anatomy can be well visualized using magnetic resonance imaging (MRI).
Beyond the hindfoot deformities there can be deformities of the midfoot. When midfoot deformity is present it is most commonly abductus and rockerbottom. Most midfoot deformities are most commonly related to coalition between the cuboid and calcaneus. Talo-navicular joint coalition can also be present. One or more rays may be missing, making the foot narrower. Absence or weakness of the peroneus longus may lead to overpull of the tibialis anterior and elevation of the first metatarsal with compensatory flexion of the first metatarsophalangeal joint (dorsal bunion). A bracket first metatarsal or a bracket conjoined first and second metatarsal with hallux varus is not uncommon. Syndactaly between some or all of the toes is also common.
Tibial deformity
There is often a mild to severe diaphyseal tibial deformity of the valgus-procurvatum. A skin dimple is usually present over the apex of this angulation. The fibular anlage is located like the string of a bow in a straight line opposite the concavity of this deformity. This thick fibro-cartilagenous remnant may contribute to this angulation by tethering the growth of the tibia on its posterior-lateral side.
Knee joint deformities
The knee joint frequently has a valgus deformity. This valgus is related both to the distal femur and the proximal tibia. The lateral epiphysis of the proximal tibia may be delayed in its ossification compared to the normal opposite side.
Knee instability
Many patients with fibular hemimelia have hypoplasia or aplasia of the anterior and or posterior cruciate ligaments. The tibia may be subluxed anteriorly relative to the femur. The ligament deficiency and subluxation are often not symptomatic at a young age, but these become a bigger problem when the child becomes taller and heavier. Patients with anterior subluxation may have associated a rounded posterior aspect of the proximal tibial epiphysis. Whether this is primary (congenital) or secondary (developmental) is unclear.
Fibular hemimelia diagnosis
Fibular hemimelia diagnosis is based on clinical examination and X-rays.
Physical examination
The major physical hallmarks of fibular hemimelia are the following:
- Limb length difference
- Possible absence of toes
- Abnormal ankle joint
On exam, the lower leg (knee to ankle) is smaller and thinner. There is often a curve in the lower leg, and sometimes there is an associated dimple on the skin. Often, the thigh is shorter in length as well. The knee joint often has no anterior cruciate ligament (ACL), and so it will feel “loose” on exam. The ankle joint may be stiff, and it may be pointed down and out (everted). There may be absent toes on the outer portion of the foot as well.
Imaging studies
The orthopaedic surgeon will likely x-rays from hips to ankles. On these x-rays, the doctor can measure the difference in limb length, the crookedness of the limb, and evaluate for abnormalities in the foot and ankle. Radiographs are repeated often as the child grows. When the child is younger, it is possible that the surgeon may recommend an MRI of the ankle joint, and possibly the knee joint. There are times when bones in the foot and ankle are “stuck together” (known as a tarsal coalition), and prior to reconstructive surgery, the doctor may want a better look at this joint.
Fibular hemimelia treatment
A child with fibular hemimelia is usually seen in the first year of life. At the initial visit, X-rays are obtained to evaluate the exact configuration of the skeletal anatomy of the lower legs and to determine the amount of discrepancy in length between the legs. The current leg length discrepancy is used to predict the final leg length discrepancy at the end of growth. This predicted leg length discrepancy will allow the doctor to create a general treatment plan. Also, the predicted amount of limb lengthening required determines the number of surgical procedures required.
The initial clinical exam identifies the shape and position of the foot and ankle. Also, the range of motion and stability of the hip, knee, and ankle are assessed and recorded. At this point, our doctors look for a concurrent congenital femoral deficiency and hip joint shallowing in the X-rays. Clinically, the doctor assesses the stability and range of motion of the knee joint. The hip and knee are always involved to some degree in fibular hemimelia. If the involvement of the hip and knee are severe, then the overall reconstruction plan is altered by planning either concurrent hip/knee reconstruction or sequential reconstruction. Most commonly, the significantly involved hip and knee would be addressed first between the ages of 18 and 24 months (superhip/superknee procedure). The ankle reconstruction (superankle procedure) would then occur 6 to 12 months after the hip and knee reconstruction.
However, if the growth abnormality is mainly concentrated in the lower leg, then the superankle reconstruction is performed with or without concurrent lengthening between the ages of 18 and 24 months. The decision to lengthen during the first reconstructive surgery is determined by the amount of ankle motion present. If the ankle is inherently stiff, then a 5-cm (2-inch) lengthening is performed at the same surgical setting. If the ankle is very mobile, then the initial surgery concentrates on positioning the foot and ankle in a stable or corrected position while concurrently correcting the bowing in the lower leg. The mobile ankle scenario falls into a two-stage initial reconstruction plan. The second stage would be a 5-cm (2-inch) lengthening of the tibia performed 6 to 12 months after the first surgery.
The number of subsequent lengthenings is determined by the overall predicted lengthening goal. The subsequent lengthenings are performed at intervals of 4 to 6 years apart for a total of up to three lengthenings for the most severe types of fibular hemimelia. The first lengthening usually achieves a 5-cm (2-inch) gain in length. Subsequent lengthenings can achieve between 5 and 7 cm (2 and 2.8 inches) of length.
Fibular hemimelia treatment goals
The goals of treatment are to create a lower limb with a stable hip, knee, and ankle that is equal in length to the opposite lower limb. Also, all deformities in the lower limb are corrected during the treatment. The crucial goal in fibular hemimelia is the reconstruction of the ankle and foot. Contrary to many doctors’ opinions, the amount of length needed does not predict the success of reconstruction or the ability to reconstruct the lower limb. In the same way, the number of toes or rays of the foot does not predict the success of reconstruction or the function of the foot. Most doctors use predicted leg length discrepancy or the number toes on the foot to determine whether to recommend amputation/ablation and prosthetic reconstruction.
The success of reconstruction treatment is mainly determined by the foot and ankle reconstruction. This success is not determined by the final ankle motion. The goal is to create a stable ankle and a foot in a normal plantigrade (foot flat) position. This is achieved with the superankle procedure that will be explained in great detail below.
The amount of final ankle motion is usually predetermined by the amount of motion already present at the ankle joint. If a patient presents with a very stiff and deformed ankle, the goal is to achieve a plantigrade (foot flat) position with a stiff but stable ankle. The misconception is that a stiff ankle is a failure of reconstruction. Our doctors believe a stiff ankle in the correct position is a good and functional base for a plantigrade foot. On the other hand, if a patient has a deformed foot and ankle with good ankle motion, then the reconstruction is tailored to both correct the foot and ankle position and maintain ankle motion.
The amount of leg length difference predicted to occur by the end of growth does not determine whether a successful reconstruction is possible. There is no set limit to the amount of overall lengthening that can be performed. However, the overall lengthening amount does determine how many treatments or lengthenings will be needed to equalize the leg lengths at maturity. For example, if a 2-year-old boy has a 2.5-cm (1-in) leg length discrepancy, his predicted leg length difference at maturity would be 6.5 cm (2.6 in) when calculated using the Multiplier method. This amount of lengthening could be accomplished with one lengthening procedure.
On the other hand, a 2-year-old girl with a 6-cm (2.4-in) leg length difference would be predicted to have a 14.5 cm (5.7 in) difference at the end of growth. This amount of difference would require two lengthenings to accomplish about 11 to 12 cm (4.3 to 4.7 in) of lengthening. The remaining 2.5 to 3.5 cm ( .98 in to 1.4 in) of difference can be corrected either by a smaller third lengthening at the end of growth or a slowing down procedure of the long leg at the age of about 10 or 11 years. These types of strategies will be explained in greater detail below. The main point is that the total amount of length needed does not determine whether the reconstruction can be performed, but rather how many interventions or surgical procedures will be needed to successfully complete the reconstruction.
Step 1: Predicting leg length discrepancy and determining the number of lengthening surgeries
The first step is measuring the leg length discrepancy using standing radiographs of both lower limbs, with the short leg on a lift of known amount 11. The total leg length discrepancy at skeletal maturity and the separate bone segment (femur, tibia, foot height) discrepancy at maturity can be calculated using the multiplier method for limb length discrepancy prediction 12. The multiplier method has been validated for accuracy in the prediction of congenital limb length discrepancy, including for fibular hemimelia 13. It is now possible to do this method using smart phone apps [App name 1: Paley Growth (OS1 only); App name 2: Multiplier (OS1 and Android)]. Once the predicted leg length discrepancy at skeletal maturity has been calculated, a determination of the number of limb length equalization procedures can be made.
Under the age of 4 years it is safe to lengthen up to 5.0 cm in the tibia; lengthening of >5.0 cm can lead to growth inhibition in young children 14. Subsequent lengthenings can be performed preferably 4 years apart as needed to achieve limb length equalization at skeletal maturity. Lengthenings performed at an older age can safely achieve up to 8.0 cm of lengthening. Therefore, one lengthening by age 4 years and one at age 8 years would achieve a total lengthening of 13 cm (5.1 in.) (5.0 + 8.0 cm). One lengthening by age 4 years plus one at age 8 years and one at age 12 years would achieve a total lengthening of 21.0 cm (8.25 in.) (5 + 8 + 8 cm). If additional equalization is required, epiphysiodesis of the opposite proximal tibia can always be considered. Epiphysiodesis is typically performed at a specific age calculated with the Paley multiplier formulae and is usually recommended for up to 5.0 cm (2 in.) of limb length equalization. Therefore, leg length equalization up to 26.0 cm can be achieved with three lengthenings (21 cm) plus an epiphysiodesis (5 cm). This treatment covers the majority of cases with limb length discrepancy due to fibular hemimelia. It is rarely ever necessary to perform more than three limb lengthening procedures to equalize limb length discrepancy due to fibular hemimelia. Cases that present with discrepancies of >25.0 cm usually have some shortening in the femur, which can be treated with simultaneous or independent lengthening of the femur. This treatment will be discussed in a later section.
Step 2: Determining the Paley type of fibular hemimelia
The next step is to determine what type of fibular hemimelia. This distinction is based on the clinical exam of the foot and ankle. If there is a fixed equino-valgus foot deformity, then it is a type 3. If there is a fixed equino-varus foot deformity, then it is a type 4. If the ankle deformity is dynamic, then it is a type 2. If there is no foot deformity and the ankle is stable, then it is a type 1. An MRI is not necessary to separate types 1, 2, 3 and 4; these types can be determined by clinical and radiographic examination. An MRI examination is helpful to subdivide the type 3 fibular hemimelia into subtypes a, b or c.
Step 3: Determining the surgical procedures required
Most patients with type 1 fibular hemimelia do not require any foot surgery; rather, treatment consists of lengthening the tibia and fibula with no foot fixation. Most patients with type 2 will require a shortening realignment osteotomy of the distal tibia to correct the valgus and stabilize the ankle. This procedure is called the SHORDT (‘shortening osteotomy realignment distal tibia’). After the SHORDT, or together with it, the tibia can be lengthened. Types 3 and 4 fibular hemimelia have fixed deformities that should be corrected early to allow the patient to walk with the foot in a plantigrade position and to be able to wear a shoe properly. It is important to correct this deformity either before or at the time of tibial lengthening. Types 3 and 4 are treated by the SUPERankle procedures (SUPER being an acronym for ‘systematic utilitarian procedure for extremity reconstruction’). The SUPERankle procedure was developed in 1996 and is the most successful method to correct the fixed equino-valgus of type 3 fibular hemimelia or fixed equinovarus of type 4 fibular hemimelia. The SUPERankle procedure is performed in children between 18 and 24 months of age. It involves supramalleolar and/or subtalar osteotomies combined with soft tissue release. The SUPERankle procedure has been performed in infants as young as 12 months and in adults as old as 32 years. Lengthening is often combined with the SUPERankle procedure.
Fibular hemimelia surgery treatment plan
The surgical treatment of fibular hemimelia is designed to address all of the deformities and deficiencies and length discrepancies. The first step in this process is to create a reconstructive life plan individualized for each patient. This involves evaluating all of the surgical deformities and deficiencies, predicting the limb length discrepancy at maturity and then coming up with a surgical plan to correct these in the fewest number of surgeries spread out as much as possible throughout the child’s growing years, so that by skeletal maturity the child has achieved equal leg length, a functional plantigrade foot, excellent alignment of the hip, knee and ankle and, as needed, a stable knee joint.
Example of reconstructive life plan:
A 6-month-old boy presents with Paley type 3c fibular hemimelia. The predicted leg length discrepancy at skeletal maturity is 25.0 cm, with a valgus knee deformity. The reconstructive life plan would consist of:
- Surgery #1, at age 18 months, SUPERankle procedure combined with lengthening of 5.0 cm combined with hemiepiphysiodesis of distal femur for valgus knee correction.
- Surgery #2, at age 8 years, lengthening 7.0 cm of tibia.
- Surgery #3, at age 12 years, lengthening 8.0 cm of tibia.
- Surgery #4, at age 13 years, epiphysiodesis of the proximal tibia on long leg for correction of 5.0 cm.
Total leg length equalization = 25 cm (10 in.).
By the end of the first consultation, the child’s parents have a roadmap for the future. This allows them to plan their lives around the surgical plan. They leave the first consultation with a good understanding of what it would take to successfully correct the foot and leg deformities and to equalize the limb length discrepancy by skeletal maturity. They can now make an educated decision whether to reconstruct and lengthen their child’s leg with fibular hemimelia.
Fibular hemimelia surgery
After the initial reconstruction of the foot and ankle, the lower extremity can grow into a valgus or “knocked knee” position due to abnormal growth at the growth plates of either the distal femur or proximal tibia. The “knocked knee” deformity has also been attributed to the shape of the distal femur or the tethering effect of the residual scar-like fibular band called the fibular anlage. Genu valgus (knocked knee position) is treated by either straightening the bone during lengthening or performing hemiepiphysiodesis (guided growth).
Hemiepiphysiodesis is a minor procedure in which a small, two-hole plate is placed over the growth plate on the inner or outer aspect of the leg. This plate acts like a bracket that slows the growth on one side of the growth plate causing the bone to gradually turn as it grows, which corrects the knocked knee deformity. Once the leg is straight, the plate is removed. The placement and removal of the plate is performed during a brief outpatient surgery. The plates are called eight-Plates (manufactured by Orthofix) or Peanut Plates (manufactured by Biomet).
Sometimes a smaller revision surgery is required after the superankle procedure. After the initial correction of the foot and ankle with the superankle procedure, the foot can shift back to the outside. This gives the appearance that the child is walking on the inside ankle bone. This phenomenon can occur soon after the superankle procedure when the child returns to weight bearing or can gradually appear as the child continues to grow.
If the foot and ankle deformity returns soon after the initial procedure, then it means that an underlying bony deformity was either under corrected or unmasked by the initial reconstruction. One must understand that the initial reconstruction is a very complex set of procedures that is unique for each child. The deformity related to fibular hemimelia is the combination of contracted soft tissues and abnormally formed joints of the ankle and foot. This unmasked deformity or recurrence can be addressed with a smaller revision surgery that requires a bone cut in the distal tibia or between the ankle and heel bone. Usually the leg is placed in a cast for 4 to 6 weeks for healing and then the child is allowed to wear regular shoes.
The foot and ankle deformity that gradually reappears during early adolescence is addressed at the final surgical intervention, which usually occurs between 12 and 16 years of age. At the final surgical reconstruction, the leg lengths are equalized with a lengthening from the upper tibia and the foot/ankle position is corrected from the lower tibia. After this reconstruction is complete, the correction is permanent since the patient is nearing the end of growth.
SHortening Osteotomy Realignment Distal Tibia
The SHORDT (SHortening Osteotomy Realignment Distal Tibia) is a procedure that was designed by the Paley in 2014 to treat valgus instability of the ankle in patients who have a hypoplastic fibula where the growth plate of the distal fibula is present. Although in theory it could also be used for a fibular remnant lacking a distal physis, such remnants are so hypoplastic and have little growth potential that they are not likely to remain a successful lateral buttress.
Superankle procedure
The SUPERankle procedure achieves a stable plantigrade foot and ankle. It can be combined with lengthening, but it does not have to be. The superankle procedure is a comprehensive release of the contracted soft tissues around the ankle joint with osteotomies (bone cuts) of the distal tibia (shin bone) and hindfoot (ankle and heel bones). This procedure aligns the foot and ankle and corrects the patient’s downward and outward foot deformity (equinovalgus deformity). During the comprehensive release, the fibrous fibular anlage is removed and used to reinforce the lengthened heel cord (Achilles tendon). At the same time, a tibial osteotomy is performed to straighten the lower leg bow. The skin dimple marks the apex of the tibial deformity. This tibial bone cut can be used to straighten and lengthen the tibia. If the ankle joint is very stiff before reconstruction, then the superankle alignment procedure can be performed at the same time as the lengthening procedure. However, as stated above, if the ankle is very mobile, then the superankle alignment procedure is performed first followed by the first lengthening 6 to 12 months later. During this first lengthening procedure, the tibia can gain up to 5 cm (2 inches) of length.
If the superankle alignment procedure is performed without lengthening, then a simple Ilizarov external fixator is applied to support the leg. This type of external frame does not require adjustments. The patient is able to weight bear/walk in this frame.
If the patient is undergoing the superankle procedure and simultaneous lengthening, then a Taylor spatial frame external fixator is used. During the lengthening phase, the patient or parent adjusts the Taylor spatial frame on a daily basis to perform the lengthening and deformity correction. The patient is seen every two weeks for clinical and X-ray examination.
The lengthening phase of the treatment lasts for 2 to 3 months. Once lengthening is completed, the adjustments stop and the consolidation or healing phase begins. The consolidation phase can last from 2 to 4 months. During this period, the Taylor spatial frame remains on the leg and the patient will have X-rays taken once a month. These X-rays can be taken at another center that is close to the patient’s home and then sent to your child’s orthopedic surgeon for review. Clinic visits at your child’s orthopedic surgeon are not necessary during the consolidation phase unless issues or problems arise.
Tibial lengthening protocol for fibular hemimelia
One or multiple tibial lengthenings are performed when patients have a significant leg length discrepancy. The amount of length gained during a single lengthening treatment usually is determined by the new bone quality or the motion of the joints above and below the lengthening site. The amount of lengthening will be limited if the patient has poor bone quality or stiffness of the joints with loss of motion. In patients younger than 6 years of age, the maximum length gain during a single lengthening is 5 cm (2 inches). The total amount of lengthening in a younger patient is limited to avoid extreme pressures on the growth plate that can cause premature closure of the growth plate and loss of potential or “natural” growth. Older patients can acquire more length in a single treatment–between 6 and 7 cm (2.4 and 2.8 inches).
Typically the patient is admitted to the hospital on the day of the lengthening surgery. A circular external fixator is placed on the lower leg and foot of the involved side. The type of external fixator used is usually the Taylor spatial frame. The foot is always included in the Taylor spatial frame to ensure stability of the ankle joint and to maintain the proper foot position during the distraction or lengthening phase of the treatment. The tibia is cut through one or two small incisions after the Taylor spatial frame is applied. The Taylor spatial frame stabilizes the cut bones and maintains alignment.
After surgery, the patient stays at the hospital mainly for pain control and close observation of the neurovascular status of the limb. The initial hospitalization is usually 3 to 4 days. Postoperative pain is controlled with epidural analgesia or intravenous pain medicine on a patient control anesthesia machine. During the first two days of hospitalization, the pain control is fine-tuned with adjustments in the medicine doses or route of delivery. Also, physical therapy begins with gentle range of motion of the hip and knee on the involved side. The main goal in this part of physical therapy is to maintain full knee extension and to gain knee flexion to at least 60 to 70 degrees. The second aspect of physical therapy is to begin mobilization of the patient. This starts with simply sitting on the side of the bed or transferring to a wheelchair. Mobilization increases over the hospital stay to standing transfers and ambulation with a walker or crutches.
To lengthen the leg and correct the deformity, the patient or parent must adjust the struts on the Taylor spatial frame daily. During the first 5 to 7 days after surgery, the Taylor spatial frame is not adjusted. This allows the bone to recover from surgery and to begin to heal. After bone healing starts, the external fixator is activated and the lengthening begins. The lengthening phase is the time period where the Taylor spatial frame is adjusted on a daily basis by pulling the bone ends slowly apart (between 0.5 mm and 1.0 mm / day), which results in new bone formation. The lengthening phase lasts for 2 to 3 months depending on the amount of length needed. Younger patients can put as much weight as they can tolerate on the operated leg. Older and larger patients are kept at 50% weight bearing during the lengthening phase.
During hospitalization, a social worker will meet with the family to assess needs and to make arrangements for equipment (walker, wheelchair, etc.). Special transportation is also assessed, but it is rarely needed with the lower leg external fixation devices used for fibular hemimelia.
The patient is discharged from the hospital after the pain medications have been converted to an oral type of medicine, the patient is tolerating a regular diet with good fluid intake, the family is comfortable with the specifics on daily care, and the patient clears the physical therapy assessment for safe mobilization and transfers. Upon discharge, the family will have a supply of pain medication, antibiotic medication and dressings. Contact numbers are provided to the family so that questions and concerns can be addressed at any hour on any day during treatment.
After discharge, the outpatient portion of the lengthening treatment begins. This includes outpatient physical therapy five days a week as well as a daily exercise and stretching program. Doctor visits are necessary every two weeks. These follow-up examinations prevent major complications during this critical lengthening phase. Each doctor office visit includes a clinical examination of the operative leg and frame along with obtaining X-rays to assess the bone’s position and length gained.
Once the lengthening phase is completed and the planned length gained, the consolidation or healing phase begins. During the consolidation phase, the Taylor spatial frame remains in place for stabilization but no further adjustments are performed. Usually the consolidation phase lasts from 2 to 4 months, and patients are allowed full weight bearing. Office visits are not necessary unless concerns or problems arise. Instead, X-rays are obtained every 4 to 6 weeks in the patient’s hometown and mailed to the your orthopedic surgeon for review. The family is contacted via phone or e-mail to discuss the results of the X-rays and the next step in treatment.
Once the monthly X-rays show adequate healing of the new bone, the Taylor spatial frame removal surgery is scheduled in the following 2 to 4 weeks. This surgery is usually an outpatient procedure. After the Taylor spatial frame is removed, a long leg cast is applied for 2 to 4 weeks. The post-removal cast protects both the new bone and the pin holes left by the external fixator from potential fracture. Usually the patient may bear full weight in the post-removal cast.
Four weeks after Taylor spatial frame removal, the cast is removed and converted to a cast brace that may be weaned according to the patient’s comfort. A gradual return to normal activities occurs over the following 2 to 3 months. Contact sports to include soccer, lacrosse and football may be resumed 6 to 8 months after frame removal. Subsequent visits become annual or biannual office visits to assess the growth of the limb, recurrent limb length discrepancy, recurrent alignment problems and future reconstructive plans.
How is the lower extremity deformity and leg length discrepancy managed before or between reconstructive treatments?
Before a lengthening or reconstruction is performed, the lower leg is treated with a brace and a shoe lift as needed. The brace provides stability and the shoe lift provides additional length to the short limb. Usually a lower leg brace or ankle foot orthosis (AFO) is not needed before the initial reconstruction. Sometimes, if the deformity is severe and the leg length discrepancy is greater than 5 cm (2 inches), an AFO is used to support the foot and ankle during shoe wear.
Typically, after the initial foot and ankle reconstruction is completed, an AFO and appropriate-sized shoe lift are used temporarily. These assistive devices are usually discontinued after the patient has completed the postoperative physical therapy and the bone has healed.
In between surgical interventions, most legs do not require bracing. If a patient’s leg length discrepancy is greater than 2 cm (3/4 of an inch), a shoe lift can be used. Again, an AFO is used if the residual leg length discrepancy is greater than 5 cm (2 inches).
What is the strategy for shoe lifts?
A shoe lift is used if the leg length discrepancy is greater than 2 cm (3/4 of an inch). The height of the lift is calculated by subtracting 1 cm (0.4-in) from the total discrepancy. For example, a patient with a 4.5-cm (1.8-in) leg length discrepancy would be given a 3.5-cm (1.4-in) shoe lift. This 1-cm (0.4-in) reduction prevents the lift from catching on the ground and allows for better clearance of the shorter leg during walking.
The reason a patient with a leg length discrepancy wears a shoe lift is to prevent an ankle contracture in a toe-down direction (equinus contracture) and to improve the patient’s gait and posture. If a person with a significant leg length discrepancy does not use a shoe lift over the period of 15 to 20 years, the person may experience long-term problems such as back pain, hip joint arthritis, and knee joint arthritis. However, these long-term problems will not occur in young children if they do not use their lifts all the time.
Doctors usually recommend that the child use the prescribed lift on their most commonly used shoe (school shoe or play shoe). It is perfectly fine for a child to spend a significant portion of the day barefooted or not using a shoe lift as long as the ankle range of motion remains normal. This is especially important during the summer when sandals and flip flops are very popular.
The lift should not be used on athletic shoes or cleats. For sports, the feet should be shoed individually and the smaller fibular hemimelia foot should have a smaller, well-fitted shoe with no lift.
Knee valgus deformity
Most cases of fibular hemimelia have associated genu valgum secondary to distal femoral and/or proximal tibial valgus deformity. Valgus of the knee can negatively impact the foot. Since there is usually no subtalar joint present, genu valgum cannot be compensated by a mobile subtalar joint. The ankle joint, which is often a ball and socket type, cannot compensate for a valgus knee since it usually has valgus instability (dynamic valgus). After foot deformity correction with the SHORDT or SUPERankle procedure, knee valgus can promote recurrent ankle deformity. It is therefore important to identify and treat the knee valgus to improve the results of the foot correction and to help prevent recurrent ankle valgus. To objectively identify the level of the knee valgus, the lateral distal femoral angle (LDFA) and medial proximal tibia angle (MPTA) should both be measured off of the distal femoral joint line. In young children this line is difficult to see since most of the distal epiphysis is not ossified. It may be necessary to do a knee arthrogram to measure the lateral distal femoral angle and medial proximal tibia angle accurately. If the valgus is from the femur, hemiepiphysiodesis of the distal femur can be carried out using a screw-plate device at the time of the ankle surgery. If the deformity is from the tibia, and if tibial lengthening is carried out, then the deformity can be corrected through the lengthening osteotomy of the proximal tibia. If the tibia is not being lengthened a hemi-epiphysiodesis device can be applied to the proximal tibial physis.
Progressive genu valgum after lengthening is another cause of valgus in patients with fibular hemimelia. Paley et al. 12 found that 75% of patients younger than 12 years and all patients younger than 4 years developed this problem. The deformity recurs through the proximal tibia. The origin is unclear but follows a pattern similar to that seen with the Cozen phenomenon 15 after proximal tibial metaphyseal fractures. In fibular hemimelia, the progressive tibial valgus may be related to the lack of growth by the fibula or may be due to soft tissue tethers on the lateral side by the fibular anlage. It may also be related to the tendency for the proximal tibial epiphysis to ossify medially but not laterally, thereby creating an intra-articular component. Intentionally deforming the tibia into 10–15° of varus at the end of the lengthening compensates for the expected rebound valgus. Another approach is to insert a hemi-epiphysiodesis plate at the end of the lengthening. A similar valgus tendency is observed with progressive valgus deformity in children with fibular hemimelia after amputation 16. In contrast to the post lengthening tibial valgus, femoral valgus associated with fibular hemimelia is nonprogressive 17. Femoral valgus may contribute to valgus overload, which may be a factor for valgus rebound in the tibia. Distal femoral hemi-epiphysiodesis can be done at the time of the index lengthening procedure. Complete fibrous anlage resection may reduce the frequency and degree of rebound but has not eliminated the problem.
Growth inhibition has been reported after tibial lengthening for fibular hemimelia 18. Sharma et al. 18 concluded that this is related to complete fibular aplasia. Most of the cases presented by Sharma et al. were treated with double-level or combined femur and tibial lengthening without soft tissue release. Hope et al. 19, who used only single-level lengthening, could not demonstrate any growth inhibition. Sabharwal et al. 14 showed that growth inhibition occurred only if there had been a second tibial lengthening performed within a year of the first lengthening.
Knee ligament reconstruction
Most patients with fibular hemimelia have some knee ligament deficiency of the cruciate ligaments. If this instability is symptomatic or if the knee remains subluxed anteriorly in full extension, knee ligament reconstruction with the SUPERknee procedure 20 may be required together with the treatment of the ankle or at a separate time. Unlike femoral lengthening for congenital femoral deficiency, knee reconstruction or stabilization of the knee are not required in order to proceed with tibial lengthening.
Toe and metatarsal surgery
Many patients with fibular hemimelia are missing one or more toes. Some surgeons consider absence of two or more metatarsals an indication for amputation 4. As long as the foot is plantigrade, the foot in fibular hemimelia is very functional even with one, two, three or four rays.
Hallux varus, syndactaly and conjoint delta first metatarsals are the most common toe deformities associated with fibular hemimelia that benefit from surgical treatment of the toes. Syndactaly of the first to second toes is easily treated by release and skin grafting. Syndactaly between the middle toes does not need to be separated. Hallux varus is always associated with a short bracket (delta) first metatarsal. In most cases this is a conjoint metatarsal (fusion of first and second metatarsal) associated with syndactaly of the first and second toes. The treatment for this requires separation of the syndactaly combined with splitting of the conjoint metatarsal into two parts and reorienting of this osteotomy to realign the first metatarso-phalangeal joint surface.
Femoral lengthening
Femoral lengthening can be combined with the tibial lengthening at the same time or at a separate time to treat concomitant shortening of the femur. Simultaneous femur and tibia lengthening with external fixation is used when the femur and tibia shortening is of significant magnitude. In such cases, it is not unusual to perform the SUPERankle procedure with application of the external fixator for lengthening tibia and femur. A discussion of femoral lengthening is beyond the scope of this article, but for further information the reader is referred to published studies 20. If femoral lengthening is considered, it is factored into the surgical life plan discussed previously. Obviously, simultaneous femoral and tibial lengthening can yield much larger amounts of lengthening in one treatment than tibia lengthening alone. For example, simultaneous 5.0-cm femoral and 5.0-cm tibia lengthening together take a total of 5 months of external fixation, and isolated tibia lengthening of 5.0 cm also takes a total of 5 months of external fixation. Therefore, in the first example combined femoral and tibia lengthening achieve 10.0 cm (4 in.) of leg length equalization compared to only 5.0 cm (2 in.) when only the tibia is lengthened. While tibial lengthening alone requires daily physical therapy, combined femur and tibial lengthening mandates strict lengthening-specific physical therapy 21. There is no indication to do femoral lengthening in the absence of femoral discrepancy. The advent of internal lengthening methods makes femoral lengthening as a separate procedure much easier.
Physical therapy
Physical therapy is the most important aspect of the lengthening process. Without proper physical therapy, the lengthening goals will not be achieved and major complications will occur. Therefore, physical therapy requirements are very strict. The patient undergoing tibial lengthening must receive physical therapy 5 days per week while at the same time performing an exercise and stretching program at home. The physical therapy continues at this level of intensity for the duration of the distraction phase (2 to 3 months depending on the planned amount of lengthening). During this initial therapy, the parents are taught home exercises and stretching techniques that their child must perform every day. Also, the parents are able to observe the therapy sessions and the therapists’ techniques.
The physical therapy usually involves land and water therapy for patients undergoing lengthening. During the distraction phase, the ideal situation is to perform all physical therapy at the specialist center with experience in limb lengthening and limb reconstruction. Once the distraction phase is completed, the therapy requirements significantly decrease. At that point, the family may return home and their therapy transitions to a local therapist with guidance from the therapists at the specialist center. Even if the patient has returned home during the lengthening phase, the office visit for clinical and X-ray evaluation that occurs every 2 weeks is still mandatory.
If the family plans to return home immediately after the hospital stay, the patient must undergo at least one week of therapy at the specialist center. This is to allow the therapy team time to teach the family the lengthening stretches and prepare them for the transition to the local therapist. Again, the family choosing this strategy must still return every two weeks for the clinical and X-ray evaluations at the specialist center clinic. Doctors do not recommend this strategy due to the increased complication rate and the decreased overall length gain of the patients when compared with patients who have chosen to perform most of the therapy at the specialist center.
The relationship between the patient and the physical therapist is very important while the family is in the specialist center and becomes even more important when the family and patient return home. The therapists are the remote eyes and ears of the physician. During the daily therapy, if any concerns or complaints arise, the therapist notifies the surgeon immediately for a recommended solution or makes sure that the patient is seen in the office for a clinical check. After the patient returns home, the specialist center physical therapist will intermittently check on the patient’s progress and discuss the therapy with the local therapist. If there is a significant therapy issue, the individual therapist notifies the local therapist and provides additional instructions.
Recovery after surgery
Recovery depends upon the surgery performed.
- Epiphysiodesis: Recovery after this surgery is relatively easy. The child can go home the same day of the surgery and can typically bear full weight immediately after the surgery. After 2-3 weeks the child can typically return to full activities. Physical therapy is rarely needed.
- Limb lengthening with external fixator: This surgery is complex and the recovery extensive. The longer the lengthening, the longer the external fixator is in place, and therefore, the longer the recovery.
- Limb lengthening with internal lengthening nail: like the external fixator, lengthening with an internal lengthening nail is also an extensive process. However, for the most part, especially in older children, the nails are better accepted and less cumbersome.
Fibular hemimelia prognosis
Children who have fibular hemimelia live happy and fruitful lives, no matter whether they have a limb reconstruction or an ablation procedure. They can play sports, play with friends, and generally have normal intelligence and life expectancy. In order to optimize their leg function, they should be seen by an orthopaedic surgeon familiar with fibular hemimelia to discuss their treatment options.
References- Paley D. Surgical reconstruction for fibular hemimelia. J Child Orthop. 2016;10(6):557‐583. doi:10.1007/s11832-016-0790-0 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5145840
- Herzenberg JE, Shabtai L, Standard SC (2016) Fibular hemimelia: principles and techniques of management. In: Sabharwal Sanjeev (ed) Pediatric lower limb deformities. Springer, pp 427–454
- Achterman C, Kalamchi A. Congenital deficiency of the fibula. J Bone Joint Surg Br. 1979;61:133–157.
- Birch JG, Lincoln TL, Mack PW, Birch CM. Congenital fibular deficiency: a review of thirty years’ experience at one institution and a proposed classification system based on clinical deformity. J Bone Joint Surg Am. 2011;93(12):1144–1151. doi: 10.2106/JBJS.J.00683
- Barham G, Clarke NMP. Genetic regulation of embryological limb development with relation to congenital limb deformity in humans. J Child Orthop. 2008;2:1–9. doi: 10.1007/s11832-008-0076-2.
- Shapiro F. Developmental patterns in lower-extremity length discrepancies. J Bone Joint Surg Am. 1982;64:639–651. doi: 10.2106/00004623-198264050-00001
- Anderson M, Green WT, Messner MB. Growth and predictions of growth in the lower extremities. J Bone Joint Surg Am. 1963;45-A:1–14. doi: 10.2106/00004623-196345010-00001
- Moseley CF. A straight-line graph for leg-length discrepancies. J Bone Joint Surg Am. 1977;59-A:174–179. doi: 10.2106/00004623-197759020-00006
- Amstutz HC (1972) Natural history and treatment of congenital absence of the fibula. J Bone Joint Surg Am 54-A:1349
- Paley D, Bhave A, Herzenberg JE, Bowen JR. Multiplier method for predicting limb-length discrepancy. J Bone Joint Surg Am. 2000;82-A(10):1432–1446. doi: 10.2106/00004623-200010000-00010
- Paley D (2005) Length considerations. In: Principles of deformity correction, 1st edn, corrected 3rd printing. Springer, Berlin New York, pp 31–60
- Paley D (2005) Growth plate considerations. In: Principles of deformity correction, 1st edn, corrected 3rd printing. Springer, Berlin New York, pp 695–716
- Aguilar JA, Paley D, Paley J, Patel M, Santpure S, Bhave A, Herzenberg JE. Clinical validation of the multiplier method for predicting limb length at maturity: part I. J Pediatr Orthop. 2005;25:186–191. doi: 10.1097/01.bpo.0000150809.28171.12
- Sabharwal S, Paley D, Bhave A, Herzenberg JE. Growth patterns after lengthening of congenitally short lower limbs in young children. J Pediatr Orthop. 2000;20:137–145.
- Cozen L. Fracture of the proximal portion of the tibia in children followed by valgus deformity. Surg Gynecol Obstet. 1953;97:183–188.
- Davidson WH, Bohne WH. The Syme amputation in children. J Bone Joint Surg Am. 1975;57:905–909. doi: 10.2106/00004623-197557070-00005
- Boakes JL, Stevens PM, Moseley RF. Treatment of genu valgus deformity in congenital absence of the fibula. J Pediatr Orthop. 1991;11:721–724. doi: 10.1097/01241398-199111000-00004
- Sharma M, MacKenzie WG, Bowen JR. Severe tibial growth retardation in total fibular hemimelia after limb lengthening. J Pediatr Orthop. 1996;16:438–444. doi: 10.1097/01241398-199607000-00004
- Hope PG, Crawfurd EJ, Catterall A. Bone growth following lengthening for congenital shortening of the lower limb. J Pediatr Orthop. 1994;14:339–342. doi: 10.1097/01241398-199405000-00012
- Paley D, Chong DY, Prince DE (2016) Congenital femoral deficiency reconstruction and lengthening surgery. In: Sabharwal S (ed) Pediatric lower limb deformities. Springer, Heidelberg, pp 361–425
- Paley D, Guardo F (2014) Lengthening reconstruction surgery for congenital femoral deficiency. In: Kocoaglu M (ed) Advanced techniques in limb reconstruction surgery. Springer, Berlin, Heidelberg, pp 245–299