Flutter valve
A flutter valve is a handheld Oscillating Positive Expiratory Pressure (PEP) device that is used as a type breathing therapy. A flutter valve helps to clear mucus from your lungs as well as make breathing easier and more comfortable. A flutter valve is a type of oscillatory Positive Expiratory Pressure (PEP) therapy that loosens secretions in the lungs and helps the patient to cough them up in order to clear the airways. The positive expiratory pressure (PEP) component encourages airflow behind secretions. The oscillations induce vibrations within the airway wall to displace secretions into the airway lumen and decrease the viscosity of tenacious secretions. The repeated accelerations of expiratory airflow favour movement of secretions from the peripheral to the central airways. The Acapella flutter valve causes both airway vibrations and positive expiratory pressure (PEP) therapy, so it essentially provides dual therapy for the patient. Acapella flutter valve is a triangularly shaped cylinder and is sometimes green or blue in color.
The flutter valve device has a steel ball that rests inside near the valve. As the patient breathes into the device, the ball rattles against the valve causing vibrations. These vibrations helps to loosen secretions form the patient’s airways.
Also, as the patient blow into the device, back pressure is created. This can ‘pop’ the alveoli in the lungs open, which helps to treat and prevent atelectasis (complete or partial collapse of a lung or a section (lobe) of a lung).
There are many flutter valve devices used to provide oscillating positive expiratory pressure (PEP):
- PARI O-PEP, Flutter, TurboForte, PEPE
- Acapella
- Bottle PEP
- Aerobika
- RC-Cornet
Types of Acapella Flutter Valves
There are several Acapella flutter valve devices that are available based on the patient’s expiratory flow:
- Acapella Green – The green model is more difficult. It is indicated for patients that can generate an expiratory flow of > 15 L/min.
- Acapella Blue – The blue model is less difficult and produces a lower amplitude of vibrations compared to Acapella Green or Acapella Choice. Acapella blue is indicated for patients that can generate an expiratory flow of < 15 L/min. For this reason, it may be more useful than other oscillating PEP devices, as it can be applied in those with lower expiratory flows, due to severe airflow obstruction or airway instability, age or size.
- Acapella Choice – used for flow rates of > 15L/min. It is able to be taken apart and thoroughly cleaned.
- Acapella Duet – It is able to be taken apart and thoroughly cleaned and has a dedicated nebulizer port
Clinical precautions for respiratory flutter valve therapy:
- Undrained pneumothorax or drained pneumothorax, due to risk of air leak
- Post-lung lobectomy or lung transplantation, due to the risk of pneumothorax or compromise to the anastomosis
- Hemodynamic instability or severe cardiovascular disease due to the application of positive pressure to the thorax, although with low pressure PEP, the risk is minimal compared to a cough
- Undrained empyema or lung abscess (due to the risk of sudden release of large volume of loculated fluid)
- Active hemoptysis due to the risk of inducing excessive bleeding with the technique
- Inability to tolerate due to increased work of breathing
- Sinusitis
- Middle ear infection, due to the risk of increased pressure within the Eustachian tubes during the technique
- Increased risk of early, uncontrolled coughing with patients with hyper-reactive airways
Figure 1. Acapella flutter valve mucus removal device
Flutter valve uses
People who are suffering from chronic bronchitis and cystic fibrosis, among other cardiopulmonary diseases, sometimes produce a large amount of mucus in their airway.
This, of course, is a problem that needs to be solved, as it can lead to other issues. Besides, having mucus in an individual’s lung is just not healthy. That’s where the little gadget known as an acapella flutter valve can come in handy.
Here are the indications for using acapella flutter valve:
- To prevent or reduce atelectasis (complete or partial collapse of a lung or a section (lobe) of a lung)
- To help the patient remove secretions and clear the airways
- To help reduce air trapping
- To maximize the delivery of aerosolized medications to patients receiving bronchial hygiene therapy.
There are no absolute contraindications for the use of a flutter valve. However, the following points need to be carefully assessed before a decision is taken to initiate this type of therapy:
- Untreated pneumothorax
- Hemoptysis
- Intracranial pressure > 20 mmHg
- Acute dyspnea
- Severe nausea
Hazards of using a flutter valve
While you may not think that blowing into a small plastic device is dangerous, there are definitely some hazards and complications that you must be aware. This is why it’s important to consult with your doctor before using a flutter valve.
With that said, please keep the following hazards in mind:
- Barotrauma in the lungs
- Increased intracranial pressure
- Decreased venous return to the heart
- Increased work of breathing
- Air swallowing that can lead to nausea or vomiting
How to use the flutter valve
For someone using a flutter valve for the first time, make sure the frequency adjustment dial is set counterclockwise to the lowest frequency-resistance setting. Now, sit in a chair by keeping your back straight. Keep your elbows resting comfortably on the table. Now, tilt your head slightly upward. This enhances the function of the diaphragm and the pelvic floor and minimises musculoskeletal stress.
This will help to keep the upper airway open wide. As a result, the air you exhale will be able to flow out smoothly.
Take a breath that is deeper than a normal inhalation. Make sure that your lips make a tight seal around the mouthpiece, then blow into the device with a forceful exhalation.
Typically, you should blow out about twice as fast as normal, but not as hard as you can.
Repeat this process for approximately 10 breaths.
After the final attempt, be sure to cough, in order to remove the secretions from the airways. You can even perform 2 to 3 “huff” coughs in order to increase secretion removal as needed.
Note: You must need to be able to exhale for at least three to four seconds while using the device. If you fail to maintain your exhalation for this advised length of time, then you need to turn the adjustment dial to increase the resistance.
This adjustment will help the patient exhale at a lower flow-rate by raising the total resistance of the vibrating orifice.
Oscillating PEP using the Acapella flutter device
Acapella flutter device is a flow-operated oscillatory device, which uses a counterweighted plug and magnet to create airflow oscillations. The frequency/resistance dial allows adjustments to the expiratory pressure and the frequency of oscillations. Acapella flutter device has the option of adjusting the flow pressure and frequency of the oscillations for each individual patient and may be used with a mouthpiece or mask or with a nebulizer in-situ. Compared to the Flutter valve device, the Acapella valve device produces more effective oscillations at lower airflows and a wider range of PEP.
Application of the Acapella flutter valve device has 2 components:
- Breathing (inhalation and slightly forced exhalation)
- Huffing/coughing
Breathing
The individual is instructed to inspire slowly to a volume slightly greater than tidal volume through the mouthpiece and perform an inspiratory breath hold for 2 to 3 seconds. Inspiration should be slow, with the inspiratory hold encouraging homogenous ventilation.
Following the breath hold, the individual is instructed to expire against a slight expiratory resistance through the Acapella valve device, at a slightly faster rate than normal. This is repeated consecutively for the prescribed number of breaths.
During expiration, the exhaled air passes through a cone, which is intermittently occluded by a counterweighted plug attached to a lever, to produce airflow oscillations. In addition, the proximity between the counterweighted plug and a magnet can be adjusted to alter the vibration frequency and amplitude and the positive expiratory pressure, with 5 settings available. The frequency of oscillations generally range between 11 and 15 Hz.
Optimal oscillation frequency and flow are those which give reinforcement of airway resonance/vibration in the lower chest and upper abdominal region. Individuals are generally taught to recognize this tactile feedback and use this to adapt their technique.
Forced Expiration Technique
Cycles of breaths are followed by the forced expiration technique (FET), then coughing to further mobilize secretions.
Prescription
Acapella flutter device therapy can be performed in either an upright seated position or a gravity assisted drainage position.
A typical cycle of oscillating PEP with an Acapella flutter device consists of:
- The number of breaths through the device may vary from 6 to 10. This will depend on the individual’s sputum volume, fatigue and dyspnea levels, which will vary according to the clinical status.
- The forced expiration technique (huffing followed by breathing control) is repeated 1 to 3 times depending on the clinical status of the patient, either through or outside of the device
- The total number of cycles may range from 6 to 10. This will depend on individuals’ symptoms and sputum volume, which will vary according to the clinical status.
Depending on the daily secretion production, Acapella flutter device therapy may be applied daily or twice daily in a stable clinical state. During an acute infection, the frequency, the number of breaths per cycle and the number of cycles may alter.
Evidence for clinical application of the Acapella flutter device
In patients with non-cystic fibrosis bronchiectasis, a three month trial of regular Acapella flutter device was associated with improvement in sputum volume and patient reported outcomes of cough and health-related quality of life and exercise capacity compared to no treatment 1. In this same patient group, it offers comparable benefit compared to Active Cycle of Breathing Technique (ACBT) or other airway clearance techniques in those in a stable disease state 2 and when acutely unwell 3. Sputum expectoration was greater with the Acapella flutter device compared to a threshold inspiratory muscle training applied as an airway clearance technique, suggesting that the oscillatory effect of the Acapella flutter device and enhanced expiratory flow are of significant benefit 4. In children, a study has shown that the resistor set at 4 is an optimal setting for secretion mobilization as it has a similar beat frequency to the cilia 5.
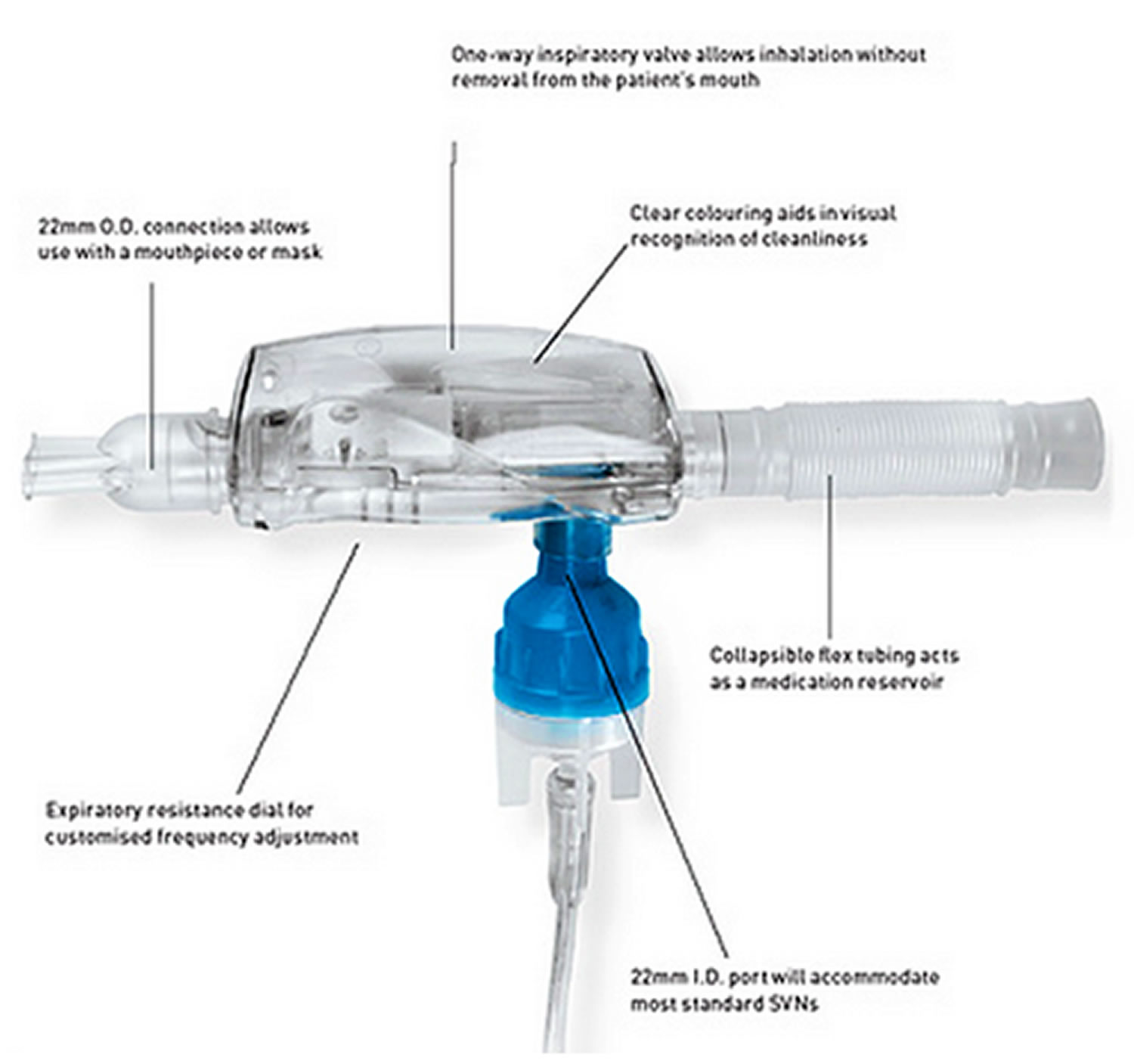
Oscillating PEP using the Aerobika flutter valve
The Aerobika Oscillating Positive Expiratory Pressure Therapy System (Figure 2) is designed to aid in the loosening and removal of excess secretions. With the correct attachment it can also be used with the Aeroeclipse breath actuated nebulizer (Figure 3).
How to use Aerobika flutter device:
- Carefully inspect the device and ensure the Resistance Indicator is on the prescribed setting.
- In a comfortably seated position, close your lips tightly around the mouthpiece.
- Inhale through the device taking a deeper breath than normal, but do not totally fill your lungs.
- Hold your breath for about 3 seconds.
- Breathe out actively, but not forcefully, through the device for at least three times longer than it took you to breathe in. During exhalation, keep your cheeks flat and firm. Active exhalation can best be described as the type of effort required to starting blowing up a balloon, but is not as forceful as blowing out candles. The Aerobika Oscillating PEP device will offer resistance to your exhaled breath meaning that you will need to exhale with more energy than you would normally.
- Continue taking deep breaths and long exhalations for 10-20 breaths and then perform 2-3 ‘huff coughs’ to clear your airways. A ‘huff cough’ will help move mucus up and out of your lungs. Just like when you use your breath to create fog on a mirror, you would take a short, shallow breath and exhale forcefully with your mouth in an ‘O’ shape. Your healthcare professional will help you with the proper ‘huff cough’ technique.
- Continue this cycle for 10-20 minutes or as prescribed by your healthcare professional.
Each 10-20 minute treatment should be performed at least twice a day. The goal is to produce little to no mucus on a daily basis which means your lungs are clear. If you are bringing up a lot of mucus, you need to use your Aerobika Oscillating PEP more often.
Figure 2. Aerobika flutter valve
Figure 3. Aerobika nebulizer
Oscillating PEP using Bottle PEP
Bottle PEP is prescribed for single patient use only. Bottle PEP is a simple and inexpensive method of administering low pressure PEP. In the pediatric setting, it is frequently called Bubble PEP as the creation of bubbles (by the addition of liquid detergent and food coloring to the water) is enticing for young children.
Bottle PEP therapy is generally used in the following circumstances:
- To ascertain if oscillating PEP therapy is effective for the patient
- The patient cannot afford any other device
- PEP therapy is only required for an in-patient exacerbation
- Other equipment is not available
Bottle PEP therapy is not appropriate and or necessary when:
- The patient doesn’t have the cognitive ability to use the device without inhaling the water
- They are not able to sit to do their airway clearance
- It is likely that the device will not be cleaned
- They obtain effective airway clearance without using a device – e.g., Active Cycle of Breathing Technique (ACBT)
The resistance with this apparatus is created by a water seal. Tubing of > or = 10 mm inner diameter (such as suction tubing), is placed in the bottle with the bottom of the tubing resting on the base of the bottle. With tubing > or = 10 mm inner diameter there are no significant PEP-pressure differences with any of the tubing lengths or flow rates, which indicates a threshold-resistor system. An escape orifice of less than 8mm inner diameter significantly increases the PEP pressure 6.
Depending on the desired effect of the technique and the flow rate of the patient, the column of water is generally 10 – 13 cm in depth in a bottle of at least one liter. The level of PEP generated with this device is generally between 10 and 20 cm H2O. Increasing the water depth will increase the pressure and decrease oscillations during expiration. Conversely, decreasing the water depth will increase oscillations and decrease the pressure during expiration. For this Bottle PEP set up, the oscillation frequency is 13 to 17 Hz and approximate pressure between 10 to 12 cm H20 is generated 7. To check the expiratory pressure, and as a teaching tool, it is advisable to attach a manometer to the circuit.
Sitting with the bottle resting on a table, the patient is instructed to breathe in through their nose. If this isn’t possible, they are instructed to take their lips off the tubing and breathe in through their mouth (see bottle PEP video).
Breathing
The breath in should be a little more than tidal volume and, with the lips sealed around the tubing, expiration needs to be active with longer than normal expiratory flow.
The airflow and pressure generates bubbles within the water. As the water may flow out of the top of the bottle during expiration, it is important to stress to patients that they must not seal off the top of the bottle as this will increase the pressure which may be a contraindication for some patients. A towel can be placed under the bottle to catch any excess water.
Forced Expiration Technique
Cycles of breaths are followed by the forced expiration technique (FET), then coughing to further mobilize secretions.
It is imperative that the water in the bottle is emptied and that the bottle and tubing are thoroughly cleaned after each use with warm soapy water. To assist with drying the tubing, it can be hung up.
Prescription
- The number of breaths may vary from 6 to 10. This will depend on the individual’s sputum volume, fatigue and dyspnea levels, which will vary according to the clinical status.
- Approximately 2-3 forced expiratory technique (huffing) is generally performed after breathing.
- The total number of cycles may range from 6 to 10. This, and the frequency of treatment will depend on individuals’ symptoms and sputum volume, which will vary according to the clinical status.
Evidence for the clinical application of Bottle PEP
When applied in adults with stable bronchiectasis, Bottle PEP improved sputum expectoration compared to no treatment and led to greater sputum expectoration at 60 minutes post treatment conclusion 7.
A recent study has evaluated that the height of the water in the bottle should be 5 cm for optimal mucus mobilization 7.
An alternative option is a Therabubble
The Therabubble has recently been updated to enable two set up options:
- Original set up (not threshold PEP). The pressures generated are listed in the instruction booklet and are similar to Flutter and Acapella. When tested, these range between 8 and 13 cm H20 with 10cm water, even with a flow rate of only 5L/min 8. This suggests they are suitable for people with an impaired ability to generate expiratory flow.
- Threshold PEP – the water level equals the pressure generated. Therabubble recommend the prescribing therapist to do a full risk assessment before using this option as the valve is removed during use. The instruction booklet that comes with each device describes how to do the risk assessment.
Oscillating PEP using the PARI O PEP, Flutter, TurboForte and PEPE
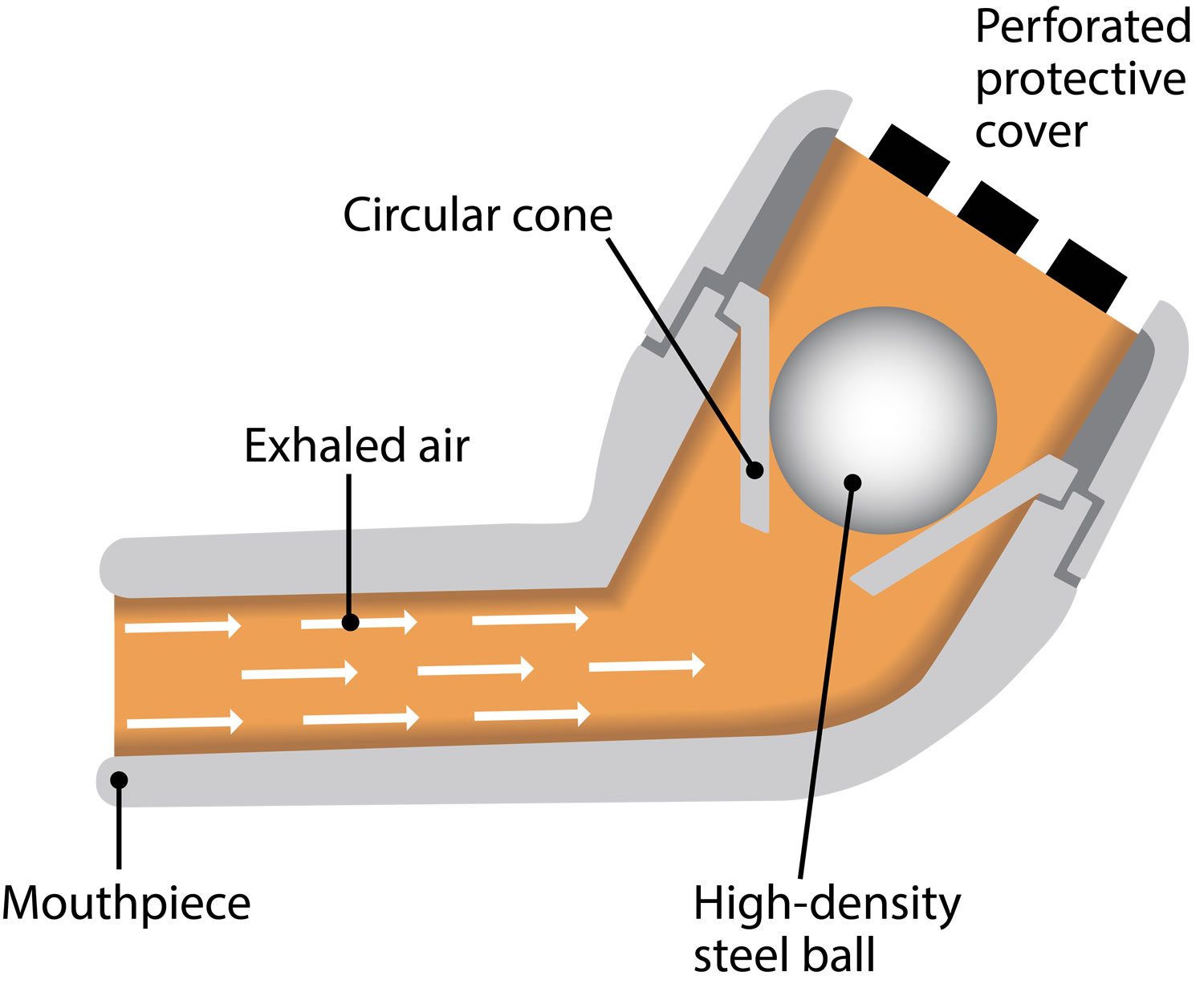
This small pipe-shaped hand-held device has a mouthpiece and a perforated cover which encases a stainless steel ball resting in a circular cone (Figure 4).
Application of Oscillating Positive Expiratory Pressure Therapy using PARI O-PEP (Flutter) device has 2 components:
- Breathing (inhalation and slightly forced exhalation)
- Huffing/coughing
Breathing
The individual is instructed to inspire slowly to a volume slightly greater than tidal volume and perform an end inspiratory breath hold for 2 to 3 seconds. Inhalation occurs through the nose or through the mouth by breathing around the mouthpiece. Inspiration should be slow, with the inspiratory hold encouraging homogenous ventilation.
Following the breath hold, the individual is instructed to breathe out through the device, with enough flow velocity, against a slight expiratory resistance, using their abdominal muscles at a slightly faster rate than normal.
Individuals may stabilize their cheeks (buccal muscles) with their other hand during expiration, if necessary, to ensure better airflow reaches the lungs. This is repeated consecutively for the prescribed number of breaths.
- When the device is tilted a little more down there is a lower pressure and frequency to mobilize phlegm from the distal airways
- When the device is tilted a little more up there is a higher pressure and frequency to mobilize the phlegm form the proximal airways
During expiration, the stainless steel ball rolls up and down the cone, creating interruptions in expiratory flow and generating a positive expiration pressure (PEP) within the range of 18 to 35 cm H20. An oscillatory vibration of the air within the airways is also generated which shear secretions from the airways and reduces their viscoelasticity. The mid-range frequency of oscillations mimic cilial beat frequency and are determined by the angle at which the device is held.
Optimal oscillation frequency and flow are those which give reinforcement of airway resonance/vibration in the lower chest and upper abdominal region. Individuals are generally taught to recognize this tactile feedback and use this to adapt their technique.
Forced Expiration Technique
Cycles of breaths are followed by the forced expiration technique (FET), then coughing to further mobilize secretions.
Prescription
This form of oscillating positive expiratory pressure (PEP) therapy using a mouthpiece oscillating positive expiratory pressure (PEP) device is generally performed in an upright seated position. It can be applied in other positions, provided that effective oscillation is still achieved.
A typical cycle of Oscillating Positive Expiratory Pressure Therapy using PARI O-PEP (Flutter) therapy consists of:
- The number of breaths through the device may vary from 6 to 10 (one cycle). This will depend on the individual’s sputum volume, fatigue and dyspnoea levels
- The forced expiration technique (huffing followed by breathing control) is repeated 1 to 3 times depending on the clinical status of the patient, either through or outside of the device
- Each treatment session should consist of 6 to 10 cycles
Depending on the daily secretion production, this type of oscillating positive expiratory pressure (PEP) therapy may be applied daily, or twice daily in a stable clinical state. During an acute infection, the frequency, the number of breaths per cycle and the number of cycles may alter. In pediatric patients, it may also depend on other factors as discussed in conjunction with the therapist and family.
Clinical application and evidence for this device
In bronchiectasis, the Pari flutter valve device improved secretion transport and reduced viscosity more than mask PEP therapy 9. Compared to no treatment, it enhanced sputum expectoration and improved quality of life in people with stable bronchiectasis 10. It was also found to reduce hyperinflation more effectively than postural drainage and slow expiration 11. When compared to Active Cycle of Breathing Technique (ACBT), with or without postural drainage or autogenic drainage in people with bronchiectasis in a stable clinical state or during an acute exacerbation, the Flutter valve device was as well tolerated and offered similar benefits in sputum expectoration as the other techniques 12 and was preferred by patients 13.
In children with cystic fibrosis (CF), a longer term study by Orlik et al 14 comparing ACBT, postural drainage with percussion +/- vibration and the Flutter found that both the ACBT and Flutter valve device improved FEV1 and FVC values. Another study over a one year period, carried out with a group of children with cystic fibrosis (CF) compared the Flutter with PEP 15. The PEP group maintained or improved their pulmonary function whereas the Flutter group showed a significant decline and were also shown to have increased antibiotic use and hospitalizations.
Figure 4. PARI O PEP flutter valve device
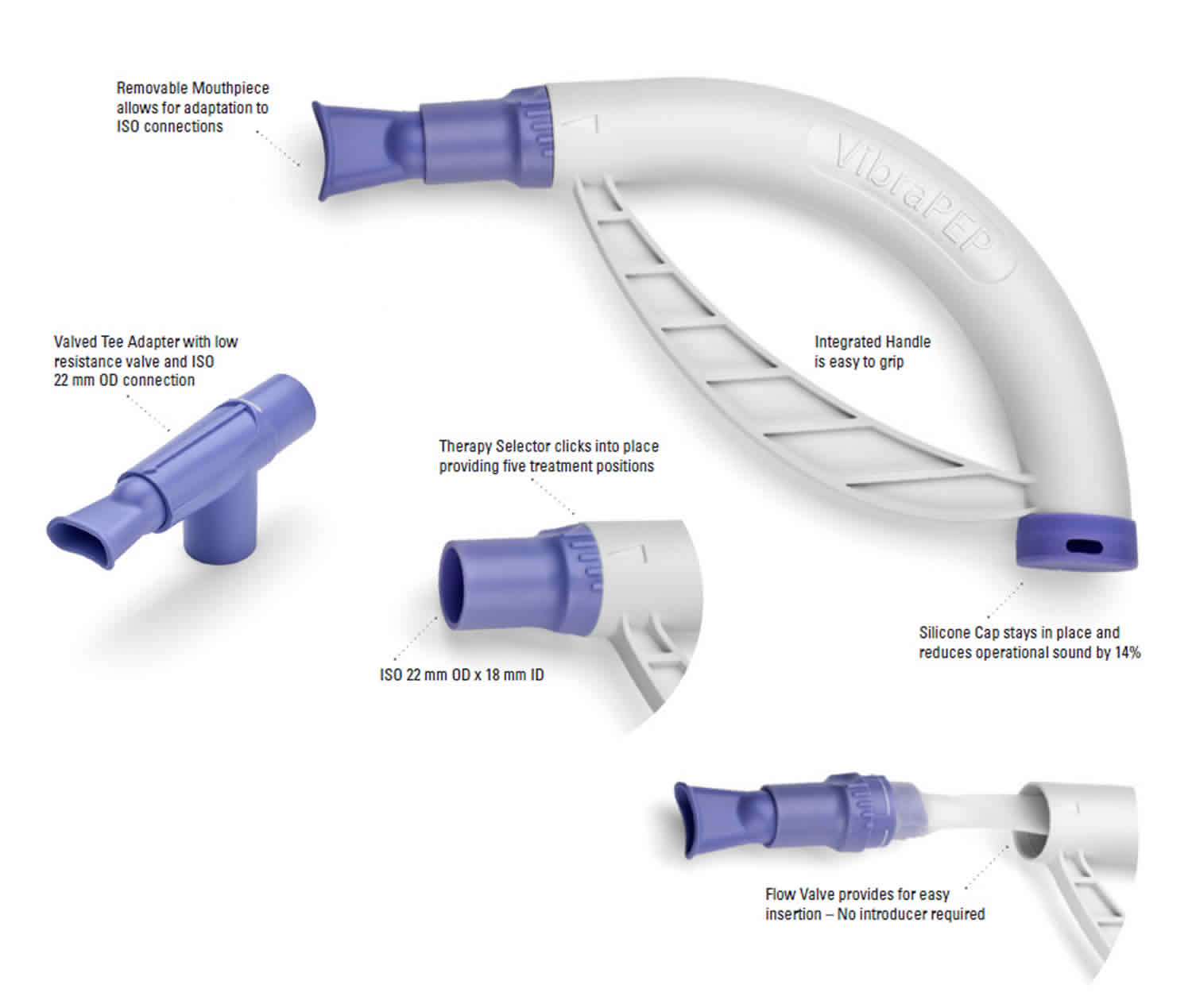
Cornet flutter device
The Cornet flutter device (Figure 5) uses low frequency acoustic wave technology to facilitate secretion clearance. Cornet flutter device consists of a mouthpiece, a curved tube, a valve hose and a sound damper.
Expiration through the tube creates an increasing pressure within the hose until it is sufficient to cause the hose end to open, allowing air to flow through the device, creating a positive expiratory pressure and oscillatory vibrations within the airways.
The pressure and flow rate can be adjusted by rotating the mouthpiece in the tube.
It has the advantage of being able to be used in any position with the flow, pressure and frequency of oscillations adjusted to the patients’ needs.
The disadvantage is that it is not easy to effectively clean.
Figure 5. Cornet flutter device
References- Murray MP, Pentland JL, Hill AT (2009). A randomised crossover trial of chest physiotherapy in non-cystic fibrosis bronchiectasis. Eur Respir J Nov;34(5):1086-92.
- Patterson JE, Bradley JM, Hewitt O, Bradbury I, Elborn S (2005). Airway clearance in bronchiectasis: a randomized crossover trial of Active Cycle of Breathing Techniques versus Acapella. Respiration 72(3):239-242.
- Patterson JE, Hewitt O, Kent L, Bradbury I, Elborn JS, Bradley JM (2007). Acapella versus ‘usual airway clearance’ during acute exacerbation in bronchiectasis: a randomized crossover trial. Chronic respiratory Disease 4(2):67-74.
- Naraparaju S, Vaishali K, Venkatesan P, Acharya V (2012). A comparison of the Acapella and a threshold inspiratory muscle trainer for sputum clearance in bronchiectasis – A pilot study. Physiotherapy Theory & Practice 2696:353-7.
- Osadnik CR; McDonald CF; Miller BR; Hill CJ; Tarrant B; Steward R; Chao C; Stodden N; Oliveira CC; Gagliardi N; Holland AE (2014). The effect of positive expiratory pressure (PEP) therapy on symptoms, quality of life and incidence of re-exacerbation in patients with acute exacerbations of chronic obstructive pulmonary disease: a multicentre, randomised controlled trial. Thorax 69(2):137-43.
- Mestriner RG, Fernandes RO, Steffen LC, Donadio MV (2009). Optimum design parameters for a therapist-constructed positive-expiratory-pressure therapy bottle device. Respir Care Apr;54(4):504-8.
- Santos M, Milroos M, McKenzie D, Alison J.(2017a) Bubble-positive expiratory pressure improve sputum clearance in people with bronchiectasis: a randomized crossover trial. Eur Respir J ; 50: PA2546
- Santos M, Milross M, Eisenhuth J, Alison J.(2017b) Pressure and oscillation frequencies generated by bubble-positive expiratory pressure devices. Respiratory Care 62(4), 444-450
- Tambascio J, de Sousa LT, Lisboa RM, Passarelli RdeC, de Souza HC, Gastaldi AC (2011). The influence of Flutter VRP1 components on mucus transport of patients with bronchiectasis. Respiratory Medicine 105(9):1316-21.
- Annemarie L Lee, Hannah C Williamson, Sarah Lorensin and Lissa M Spencer (2015). The effects of oscillating positive expiratory pressure therapy in adults with stable non-cystic fibrosis bronchiectasis: A systematic review. Chronic Respiratory Diseases 12(1):36-46.
- Guimaraes FS, Moco VJ, Menezes SL, Dias CM, Salles RE, Lopes AJ (2012). Effects of ELTGOL and Flutter VRP1 on the dynamic and static pulmonary volumes and on the secretion clearance of patients with bronchiectasis. Revista Brasileira de Fisioterapia 16(2):108-13.
- Cortina-Herrero B, Vilaro J, Marti D, Torres A, San Miguel-Pagola M, Alcaraz V, Polverino E (2016). Short term effects of slow expiratory airway clearance techniques in patients with bronchiectasis. A randomised crossover trial. Physiotherapy; 102(4): 357-364.
- Eaton T, Young P, Zeng I, Kolbe J (2007). A randomized evaluation of the acute efficacy, acceptability and tolerability of flutter and active cycle of breathing with and without postural drainage in noncystic fibrosis bronchiectasis. Chron Respir Dis 4(1):23-30.
- Orlik T, Sands D. Long‐term study of efficiencies of select physiotherapy methods used in the treatment of cystic fibrosis [abstract]. Proceedings of the 24th European Cystic Fibrosis Conference; 2001 June 6‐9; Vienna, Austria. 2001:P113.
- McIlwaine PM, Wong LT, Peacock D, Davidson AG (2001). Long-term comparative trial of positive expiratory pressure versus oscillating positive expiratory pressure (flutter) physiotherapy in the treatment of cystic fibrosis. J Pediatr Jun; 138(6): 845-50.