Ganglioneuroma
Ganglioneuroma is a very rare, benign (non-cancerous), neuroblastic tumor of neural crest origin made up of mature ganglion and nerve sheath cells and arise wherever sympathetic nerves or sympathetic nervous tissue exist 1. Ganglioneuroma tumor usually appears in areas with large vessels in the course of the trunk of the sympathetic system 2. Ganglioneuromas are the most benign and well differentiated of neuroblastic tumors (such as neuroblastoma and ganglioneuroblastoma) and composed entirely of mature sympathetic ganglion cells, Schwannian stroma, fibrous tissue, and nerve fibers 3. By definition, ganglioneuromas do not contain immature elements, such as neuroblasts, mitotic figures, or intermediate cells 4, thus predicting a favorable prognosis. Ganglioneuromas can arise de novo or arise from maturing ganglioneuroblastomas or neuroblastomas, especially when treated with chemotherapy 5. Ganglioneuroma is predominatingly detected in children older than the age of 7 6.
The sympathetic nervous system is part of the autonomic nervous system. It includes:
- Nerve fibers that run along either side the spinal cord.
- Clusters of nerve cells called ganglia (plural of ganglion) at certain points along the path of the nerve fibers.
- Nerve-like cells found in the medulla (center) of the adrenal glands. The adrenals are small glands that sit on top of each kidney. These glands make hormones (such as adrenaline [epinephrine]) that help control heart rate, blood pressure, blood sugar, and how the body reacts to stress.
The origin of ganglioneuroma tumor is usually from the great sympathetic chain, which extends from the base of the skull, neck, in the chest posterior mediastinum to the retroperitoneum along with the adrenal gland 7. Ganglioneuromas can be found in the neck, heart, bones, adrenal medulla, intestine, and spermatic cord 7. Ganglioneuroma commonly occurs in the retroperitoneum (in 32% to 52% of cases) and posterior mediastinum (in 39% to 43% of cases) 8. Only 20–30% ganglioneuroma tumor occurs in the adrenal medulla 9, while other locations include the neck, spermatic cord, heart, bone, and intestine 10, with fewer cases reported in head 11. Intracranial ganglioneuroma is extremely rare and only 4 cases of ganglioneuroma originating from the trigeminal nerve have been reported 12. Chest and extraperitoneal ganglioneuroma is most commonly recognised in older children, while the adrenal location is characteristic of patients between 30 and 50 years of age 13.
Ganglioneuroma tumor is very rare and mostly found during the third and fourth decades of life 7. A recent review reported that retroperitoneal ganglioneuromas actually appear in patients younger than 18 years in only one-third of the cases 14. Several series showed mean age at diagnosis to fall within the 3rd and the 4th decade of life 15. Ganglioneuroma is mostly found in women, with a female:male ratio of 3:2 16.
Ganglioneuroma was first described more than 150 years ago 17. A variety of case reports on ganglioneuroma have been published 18, ranging from patients with symptoms due to huge tumor masses 19 to speculations about malignant transformation and dedifferentiation into neuroblastoma 20.
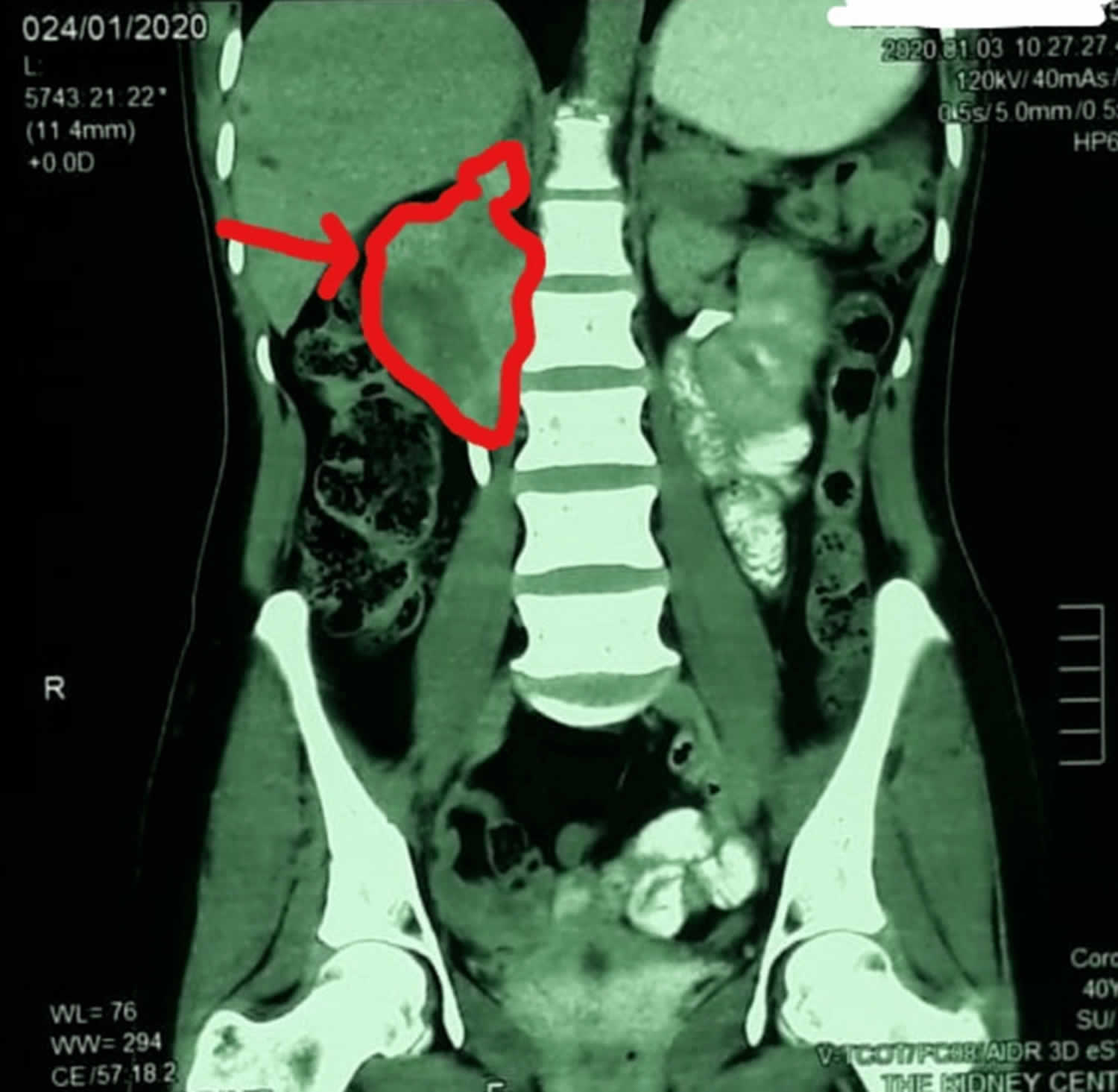
Usually, ganglioneuroma tumors are discovered incidentally in adolescents or adults during thoracic or abdominal examinations 21. Although the imaging studies, including CT, are available to detect ganglioneuromas, the definitive diagnosis can only be made by histological examination. Ganglioneuroma contains mature sympathetic ganglion cells, Schwann cells, stroma, and nerve fibers along with fibrous tissue 1. Pathologic diagnosis is essential in order to identify lymph node metastases.
Ganglioneuroma is generally considered a benign tumor that is treated by surgery alone. After surgery, ganglioneuroma tumor may relapse 22. Ganglioneuromas are usually removed by surgery and looked at carefully with a microscope to be sure they don’t have areas of malignant cells (which would make the tumor a ganglioneuroblastoma). If the final diagnosis is ganglioneuroma, no other treatment is needed. If it’s found to be a ganglioneuroblastoma, it’s treated the same as a neuroblastoma. Ganglioneuroblastoma is a tumor that has both malignant and benign parts. It contains neuroblasts (immature nerve cells) that can grow and spread abnormally, similar to neuroblastoma, as well as areas of more mature tissue that are similar to ganglioneuroma.
Ganglioneuroma causes
There are no known risk factors for ganglioneuromas. However, the tumors may be associated with some genetic problems, such as neurofibromatosis type 1 23. According to Shimada 24, ganglioneuroma develops as a result of maturation of neuroblastoma. There is no evidence that all ganglioneuromas are formed this way, but more research seems to confirm this way of its development 22.
Ganglioneuroma symptoms
A ganglioneuroma usually causes no symptoms. The tumor is only discovered when a person is examined or treated for another condition. Ganglioneuroma tumors are usually an incidental finding during routine radiographic examination, as most patients remain asymptomatic, given that most of these tumors are hormone silent 25. Ganglioneuroma tumor may cause pressure symptoms due to its large size 26. Furthermore, retroperitoneal ganglioneuromas tend to produce less symptoms than intraperitoneal ganglioneuromas and they can reach huge dimensions, up to 25 cm 27, before being diagnosed. Ganglioneuromas, however, have been associated with a variety of hormonal secretions, such as catecholamines, vasoactive intestinal polypeptides or testosterone 28, which manifest with symptoms like hypertension, diarrhea, and virilization 29. It has been shown that catecholamine production is found most frequently 30. Differential diagnosis with pheochromocytoma is necessary, bearing in mind the eventuality of a composite pheochromocytoma-ganglioneuroma, a mixed neuroendocrine-neural tumor that is composed of pheochromocytoma and other neural crest derivatives 31.
Symptoms depend on the location of the ganglioneuroma tumor and the type of hormones it releases.
If the ganglioneuroma tumor is in the chest area (mediastinum), symptoms may include:
- Breathing difficulty
- Chest pain
- Compression of the windpipe (trachea)
If the ganglioneuroma tumor is lower down in the abdomen in the area called the retroperitoneal space, symptoms may include:
- Abdominal pain
- Bloating
If the ganglioneuroma tumor is near the spinal cord, it may cause:
- Compression of the spinal cord, which leads to pain and loss of strength or feeling in the legs, arms, or both
- Spine deformity
Ganglioneuroma tumors may produce certain hormones, which can cause the following symptoms:
- Diarrhea
- Enlarged clitoris (women)
- High blood pressure
- Increased body hair
- Sweating.
Ganglioneuroma complications
If ganglioneuroma tumor has been present for a long time and has pressed on the spinal cord or caused other symptoms, surgery to remove the tumor may not reverse the damage. Compression of the spinal cord may result in loss of movement (paralysis), especially if the cause is not detected promptly.
Surgery to remove the tumor may also lead to complications in some cases. In rare cases, problems due to compression may occur even after the tumor is removed.
Ganglioneuroma diagnosis
The best tests to identify a ganglioneuroma are:
- CT scan of the chest, abdomen, and pelvis
- MRI scan of the chest and abdomen
- Ultrasound of the abdomen or pelvis
Blood and urine tests may be done to determine if the tumor is producing hormones or other chemicals.
A biopsy or complete removal of the tumor may be needed to confirm the diagnosis.
Ganglioneuroma tumors are usually an incidental finding during routine radiographic examination. Imaging characteristics of ganglioneuromas are not discriminating. Ultrasound usually reveals a homogeneous, hypoecoic mass with well-defined borders 32. On CT, ganglioneuromas appear as hypodense and homogeneous, demonstrating slight to moderate contrast enhancement 33. At magnetic resonance imaging, ganglioneuromas show low signal intensity on T1-weighted images and heterogeneous high signal intensity on T2-weighted images 32. None of these exams, however, allow differentiation among ganglioneuromas and the other neuroblastic tumors or adrenal incidentalomas.
Preoperative diagnosis of a ganglioneuroma is often difficult 34 and is usually confirmed by histopathological findings after surgical excision of the neoplasia. Ganglioneuroma definitive diagnosis can only be made by histological examination. Ganglioneuroma contains mature sympathetic ganglion cells, Schwann cells, stroma, and nerve fibers along with fibrous tissue 1. Pathologic diagnosis is essential in order to identify lymph node metastases.
Fine-needle biopsies are not recommended as a standard diagnostic procedure in patients with adrenal masses 35. Furthermore, in a case where the location of the ganglioneuroma tumor adjacent to the aorta and the pancreatic tail, the option of a biopsy was discarded because the procedure being too risky.
Ganglioneuroma treatment
The method of choice in the treatment of ganglioneuroma is a surgery with total or subtotal resection of the tumor, having a similar prognosis to the incomplete resection with less than 2 cm residual disease 36, although there is still no absolute consensus about the indications of surgery for adrenal masses. Adjuvant chemotherapy does not affect the progression-free survival or overall survival in any way. The benefits of chemotherapy occur only in cases that include immature cells and only within the tumors that have not been resected completely 22. If the prognosis shows that the excision would not cause any clinical improvement and the surgery is more risky than the disease’s progression, the observation appears to be the only right solution 13. According to a 2004 National Institutes of Health State-of-the-Science statement 37, the generally accepted recommendation regarding nonfunctional adrenal masses is to excise asymptomatic lesions >6 cm, while close follow-up is indicated for asymptomatic lesions <4 cm. For lesions between 4 and 6 cm, both surgery and follow-up can represent reasonable approaches.
Ganglioneuroma prognosis
Ganglioneuroma prognosis seems to be excellent after surgical resection without further therapies, even in the few documented cases of metastatic disease 3. A Japanese study indicated a good prognosis postoperatively 34. Although benign, ganglioneuromas can exceptionally metastasize to distant sites; there are a few reports of metastases to regional lymph nodes 38, liver, spleen 39 and soft tissues 30. These cases of metastatic ganglioneuromas are believed to be the results of the spreading of neuroblastomas or ganglioneuroblastomas that subsequently matured to ganglioneuromas. A neoadjuvant therapy was described to reduce the size of the ganglioneuroma tumor, but was ineffective 40. Local recurrences have been reported, so long-term follow-up is recommended after surgery 33.
References- Hussain MH, Iqbal Z, Mithani MS, Khan MN. Retroperitoneal Ganglioneuroma in a Patient Presenting With Vague Abdominal Pain. Cureus. 2020;12(7):e9133. Published 2020 Jul 11. doi:10.7759/cureus.9133 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7417092
- Cerullo G, Marrelli D, Rampone B, Miracco C, Caruso S, Marianna DM. Presacral ganglioneuroma: a case report and review of literature. World J Gastroenterol. 2007;13:2129–2131.
- Oderda M, Cattaneo E, Soria F, et al. Adrenal ganglioneuroma with multifocal retroperitoneal extension: a challenging diagnosis. ScientificWorldJournal. 2011;11:1548-1553. doi:10.1100/tsw.2011.144 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3201631/pdf/758352.pdf
- Geoerger, B., Hero, B., Harms, D., Grebe, J., Scheidhauer, K., and Berthold, F. (2001) Metabolic activity and clinical features of primary ganglioneuromas. Cancer 91, 1905–1913.
- Ambros, I.M., Zellner, A., Roald, B., et al. (1996) Role of ploidy, chromosome 1p, and Schwann cells in the maturation of neuroblastoma. N. Engl. J. Med. 334,1505–1511.
- Grosfeld JL, Skinner MA, Rescorla FJ, West KW, Scherer LR. Mediastinal tumors in children: experience with 196 cases. Ann Surg Oncol. 1994;1:121–127.
- Adrenal ganglioneuroma with multifocal retroperitoneal extension: a challenging diagnosis. Oderda M, Cattaneo E, Soria F, et al. Sci World J. 2011;11:1548–1553.
- Deng X, Fang J, Luo Q, Tong H, Zhang W. Advanced MRI manifestations of trigeminal ganglioneuroma: a case report and literature review. BMC Cancer. 2016;16(1):694. Published 2016 Aug 30. doi:10.1186/s12885-016-2729-8 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5006494
- Lonergan, G.F., Schwab, C.M., Suarez, E.S., and Carlson, C.L. (2002) Neuroblastoma, ganglioneuroblastoma and ganglioneuroma: radiologic-pathologic correlation. Radiographics 22,911–934.
- Jain, M., Shubba, B.S., Sethi, S., Banga, V., and Bagga, D. (1999) Retroperitoneal ganglioneuroma: a report of a case diagnosed by fine-needle aspiration cytology, with review of the literature. Diagn. Cytopathol. 21,194–196.
- Lonergan GJ, Schwab CM, Suarez ES, Carlson CL. Neuroblastoma, ganglioneuroblastoma, and ganglioneuroma: radiologic-pathologic correlation. Radiographics. 2002;22:911–34. doi: 10.1148/radiographics.22.4.g02jl15911
- Kim SK, Jeong MY, Kang HK, Yoon W. Diffusion-weighted magnetic resonance imaging findings in a patient with trigeminal ganglioneuroma. Korean J Radiol. 2013;14:118–21. doi: 10.3348/kjr.2013.14.1.118
- Kołodziejek A, Pronobis K, Derlatka P, Grabowska-Derlatka K, Grabowska-Derlatka L. Presacral ganglioneuroma in an adult with 6-year follow-up without surgical treatment. Radiol Case Rep. 2020;15(10):1983-1987. Published 2020 Aug 21. doi:10.1016/j.radcr.2020.06.028 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7452074
- Papavramidis, T.S., Michalopoulos, N., Karayannopoulou, G., Kesisoglou, I., Tzioufa, V., Raptou, G., and Papavramidis, S.T. (2009) Retroperitoneal ganglioneuroma in an adult patient: a case report and literature review of the last decade. South. Med. J.102(10),1065–1067.
- Rondeau, G., Nolet, S., Latour, M., Braschi, S., Gaboury, L., Lacroix, A., Panzini, B., Arjane, P., Cohade, C., and Bourdeau, I. (2010) Clinical and biochemical features of seven adult adrenal ganglioneuromas. J. Clin. Endocrinol. Metab. 95(7),3118–3125.
- Thoracolumbar paravertebral giant ganglioneuroma and scoliosis: a case report and literature review. Yang Y, Ren M, Yuan Z, et al. World J Surg Oncol. 2016;14:65.
- McFarland J, Sappington SW. A Ganglioneuroma in the neck of a child. Am J Pathol. 1935;11(3):429–48.
- Decarolis B, Simon T, Krug B, et al. Treatment and outcome of Ganglioneuroma and Ganglioneuroblastoma intermixed. BMC Cancer. 2016;16:542. Published 2016 Jul 27. doi:10.1186/s12885-016-2513-9 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4964292
- Cronin EM, Coffey JC, Herlihy D, Romics L, Aftab F, Keohane C, et al. Massive retroperitoneal ganglioneuroma presenting with small bowel obstruction 18 years following initial diagnosis. Ir J Med Sci. 2005;174(2):63–6. doi: 10.1007/BF03169133
- Kulkarni AV, Bilbao JM, Cusimano MD, Muller PJ. Malignant transformation of ganglioneuroma into spinal neuroblastoma in an adult. Case report. J Neurosurg. 1998;88(2):324–7. doi: 10.3171/jns.1998.88.2.0324
- Shawa H, Elsayes KM, Javadi S, Morani A, Williams MD, Lee JE, et al. Adrenal ganglioneuroma: features and outcomes of 27 cases at a referral cancer centre. Clin Endocrinol (Oxf) 2014;80:342–7. doi: 10.1111/cen.12320
- Qing Y, Bin X, Jian W, Li G, Linhui W, Bing L. Adrenal ganglioneuromas: a 10-year experience in a Chinese population. Surgery. 2010;147:854–860.
- Ganglioneuroma. https://medlineplus.gov/ency/article/001437.htm
- Shimada H., Ambros IM, Dehner LP, Hata J, Joshi VV, Roald B. Terminology and morphologic criteria of neuroblastic tumors. Recommendations by the International Neuroblastoma Pathology Committee. Cancer. 1999;86:349–396.
- Ganglioneuroma presenting as an adrenal incidentaloma: a case report. Adas M, Koc B, Adas G, Ozulker F, Aydin T. J Med Case Rep. 2014;8:131.
- Retroperitoneal ganglioneuroma combined with scoliosis: a case report and literature review. Wang X, Yang L, Shi M, Liu X, Liu Y, Wang J. Medicine. 2018;97:0.
- Lai, M.C., Wang, C.C., Lin, W.C., Liu, K.L., and Huang, K.H. (2011) Huge adrenal ganglioneuroma. Urology 78(1),58–59.
- Rondeau, G., Nolet, S., Latour, M., Braschi, S., Gaboury, L., Lacroix, A., Panzini, B., Arjane, P., Cohade, C., and Bourdeau, I. (2010) Clinical and biochemical features of seven adult adrenal ganglioneuromas. J. Clin. Endocrinol. Metab. 95(7),3118–3125.
- Adrenal and extra-adrenal retroperitoneal ganglioneuroma: imaging findings in 13 adults. Radin R, David CL, Goldfarb H, Francis IR. Radiology. 1997;202:703–707.
- Geoerger, B., Hero, B., Harms, D., Grebe, J., Scheidhauer, K., and Berthold, F. (2001) Metabolic activity and clinical features of primary ganglioneuromas. Cancer 91,1905–1913.
- Mahajan, H., Lee, D., Sharma, R., Chin, P., Watt, W.H., McBride, G., and Bilous, M. (2010) Composite phaeochromocytoma-ganglioneuroma, an uncommon entity: reportof two cases. Pathology 42 (3),295–298.
- Erem, C., Ucuncu, O., Nuhoglu, I., Cinel, A., Cobanoglu, U., Demirel, A., Koc, E., Kocak, M., and Guvendi, G.F. (2009) Adrenal ganglioneuroma: report of a new case. Endocrine 35,293–296.
- Lonergan, G.F., Schwab, C.M., Suarez, E.S., and Carlson, C.L. (2002) Neuroblastoma, ganglioneuroblastoma and ganglioneuroma: radiologic-pathologic correlation. Radiographics 22,911–934.
- Retroperitoneal ganglioneuroma: a case report and review of the Japanese literature. Moriwaki Y, Miyake M, Yamamoto T, et al. Intern Med. 1992;31:82–85.
- Mansmann, G., Lau, J., Balk, E., Rothberg, M., Miyachi, Y., and Bornstein, S.R. (2004) The clinically inapparent adrenal mass: update in diagnosis and management. Endocr. Rev. 25(2),309–340.
- Li L, Shao J, Gu J, Wang X, Qu L. Adrenal ganglioneuromas: experience from a retrospective study in a Chinese population. Urol J. 2014;11:1485–1490.
- Mansmann, G., Lau, J., Balk, E., Rothberg, M., Miyachi, Y., and Bornstein, S.R. (2004) The clinically inapparent adrenal mass: update in diagnosis and management. Endocr. Rev. 25(2),309–340.
- Srinivasan, R., Koliyadan, K.S., Krishand, G., and Bhat, S.S. (2007) Retroperitoneal ganglioneuroma with lymphnode metastasis: a case report. Indian J. Pathol. Microbiol. 50 (1),32–35.
- Chen, G.H. and He, J.N. (1986) Malignant ganglioneuroma of adrenals with metastasis to liver and spleen. Chin. Med. J. 99(3),261–263.
- Qureshi, S.S. and Medhi, S.S. (2008) Large adrenal ganglioneuromawith left inferior vena cava: implications for surgery. Pediatr. Surg. Int. 24,455–457.