What is gestational age
Gestational age is the age of a fetus or baby that starts on the first day of the mother’s last menstrual period (LMP). Gestational age is the common term used during pregnancy to describe how far along the pregnancy is. Gestational age is measured in weeks, from the first day of the woman’s last menstrual cycle to the current date. A normal pregnancy can range from 38 to 42 weeks. A pregnancy is now considered “full term” at 39 weeks.
Infants born before 37 weeks are considered premature. Infants born after 42 weeks are considered postmature.
Gestation is the period of time between conception and birth. During this time, the baby grows and develops inside the mother’s womb.
Exact gestational age is important because premature babies won’t be as developed and will probably need more medical support for their lungs, hearts, tummy and bowels, temperature control and feeding. For example, most babies who are born at less than 32 weeks of pregnancy will need help with breathing. This means they’ll be cared for in a neonatal intensive care unit (NICU). If they’re more developed, they might be cared for in a special care nursery (SCN).
An examination called the Dubowitz/Ballard Examination for Gestational Age is often used. A baby’s gestational age often can be closely estimated using this examination. The Dubowitz/Ballard Examination evaluates a baby’s appearance, skin texture, motor function, and reflexes. The physical maturity part of the examination is done in the first 2 hours of birth. The neuromuscular maturity examination is completed within 24 hours after delivery.
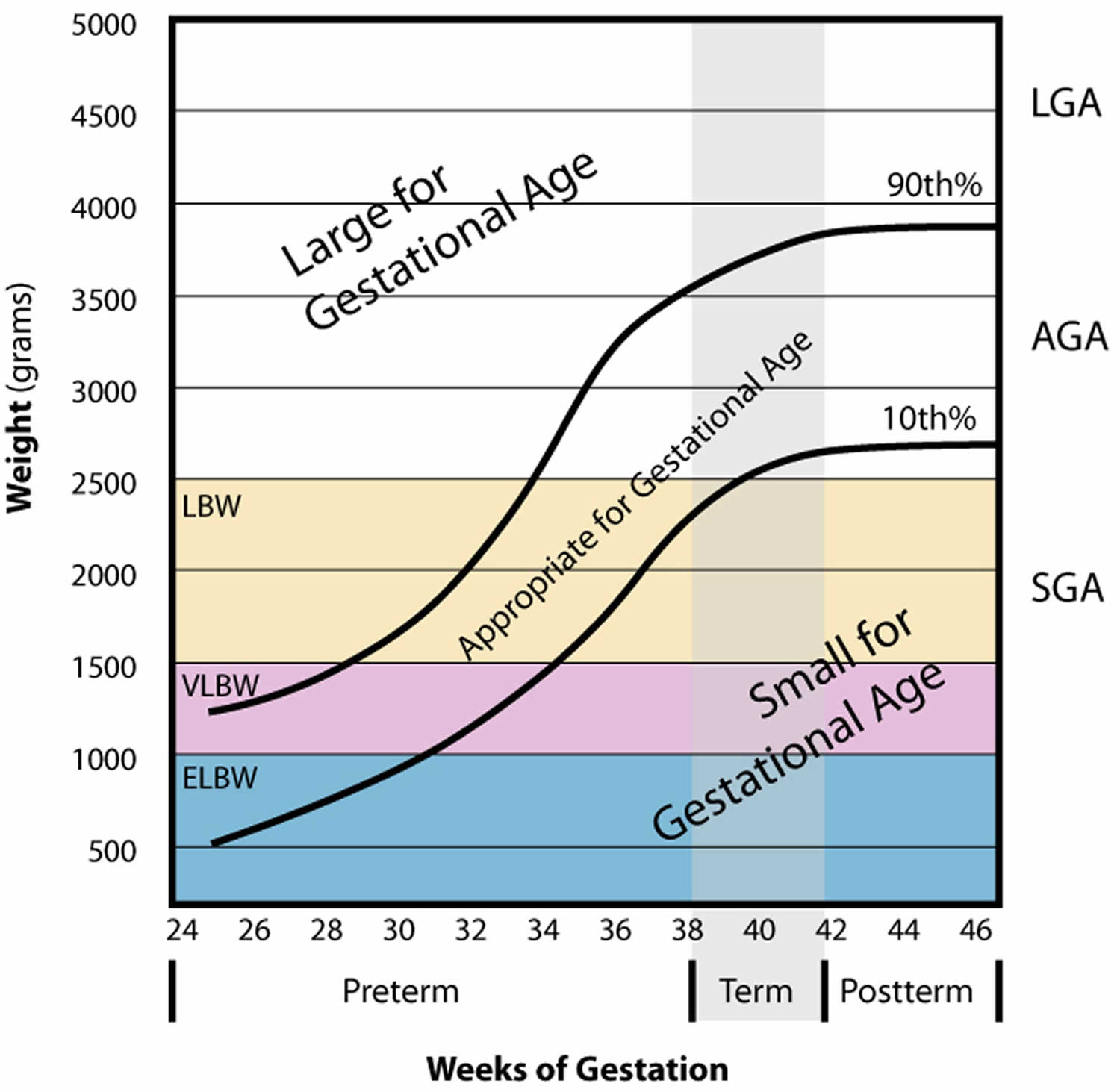
Figure 1. Gestational age chart
Abbreviations: AGA =appropriate for gestational age ; LGA = large for gestational age ; SGA = small for gestational age
How to calculate gestational age
Gestational age can be calculated before or after birth.
- Before birth, your health care provider will use ultrasound to measure the size of the baby’s head, abdomen, and thigh bone. This provides a view on how well the baby is growing in the womb.
- After birth, gestational age can be measured by looking at the baby’s weight, length, head circumference, vital signs, reflexes, muscle tone, posture, and the condition of the skin and hair.
If the baby’s gestational age findings after birth match the calendar age, the baby is said to be appropriate for gestational age (AGA). Appropriate for gestational age babies have lower rates of problems and death than babies that are small or large for their gestational age.
The weight for full-term infants that are born appropriate for gestational age will most often be between 2,500 grams (about 5.5 lbs or 2.5 kg) and 4,000 grams (about 8.75 lbs or 4 kg).
- Infants weighing less are considered small for gestational age (SGA). A low birth weight is less than 5.5 pounds.
- Infants weighing more are considered large for gestational age (LGA). A high birth weight is more than 8.8 pounds.
Prenatal Techniques
Non-Sonographic Methods for Determining Gestational Age
Naegele’s Rule: Establish the date of the last menstrual period by obtaining a history from the patient. From this date, add 1 year and 7 days, then subtract 3 months. This will approximate the estimated delivery date. The date of the last known menstrual period will give the approximate start date for age of the fetus 1. Naegele’s rule assumes a standardized 28-day menstrual cycle with fertilization occurring on day 14. However, many women have irregular cycles with variability in the length of the follicular phase affecting ovulation. History of last menstrual period may be confounded by early pregnancy bleeding, hormonal contraceptive use, or incorrect recall of last menstrual period date 2.
Uterine Size: The uterus has been described as a soft and globular pelvic organ. In pregnancy, the uterus increases in size to accommodate the developing fetus. At approximately 12 weeks gestation the uterus becomes large enough to be palpable just above the pubic symphysis. At 16 weeks gestation, the fundus of the uterus can be palpated at the midpoint between the umbilicus and the pubic symphysis. At 20 weeks gestation, the fundus can be palpable at the level of the umbilicus. After 20 weeks of gestation, the pubic symphysis to fundal height in centimeters should correlate with the week of gestation.
Uterine size finding primarily relies on the provider’s physical examination. This may be confounded by maternal factors including but not limited to obesity, multiple gestation, leiomyoma, and fibroids. The mother may also have a retroverted uterus which will alter normal progressive landmarks. Individual practitioner skill and experience make findings less reliable and reproducible.
Sonographic Methods for Determining Gestational Age
- First Trimester Dating: Sonographic assessment within the first 13 weeks and 6 days will provide the most accurate estimate of gestational age. Both transvaginal and transabdominal approaches may be used. However, the transvaginal approach may provide a more clear and accurate view of early embryonic structures. Although the gestational sac and yolk sac are the first measurable markers visible on ultrasound, these poorly correlate with gestational age.
- The crown-rump length (CRL) is the most accurate measurement correlating with gestational age. Using the mean of three measurements, crown-rump length can be determined by using the calipers on the ultrasound machine, measuring a straight line from the outer margin of the cephalic pole to the rump of the embryo. This measurement can be plugged into numerous validated tables and formulas that correlate well with gestational age 3. Crown-rump length (CRL) parameter becomes less accurate for predicting gestational age and delivery date with the advancement of gestation due to normal embryonic development and variability in anatomic positioning. Once the crown-rump length exceeds 84 mm, the Biparietal Diameter (BPD) serves as a better indicator for gestational age 3.
- Second Trimester Dating: If gestational age is not determined within the first trimester, alternate sonographic techniques may be used to estimate gestational age. These techniques are generally not recommended as first-line options for dating but are more helpful in determining if fetal size is within normal range. These measurements should not change the gestational age or delivery date if a previous crown-rump length has been calculated within the first trimester.
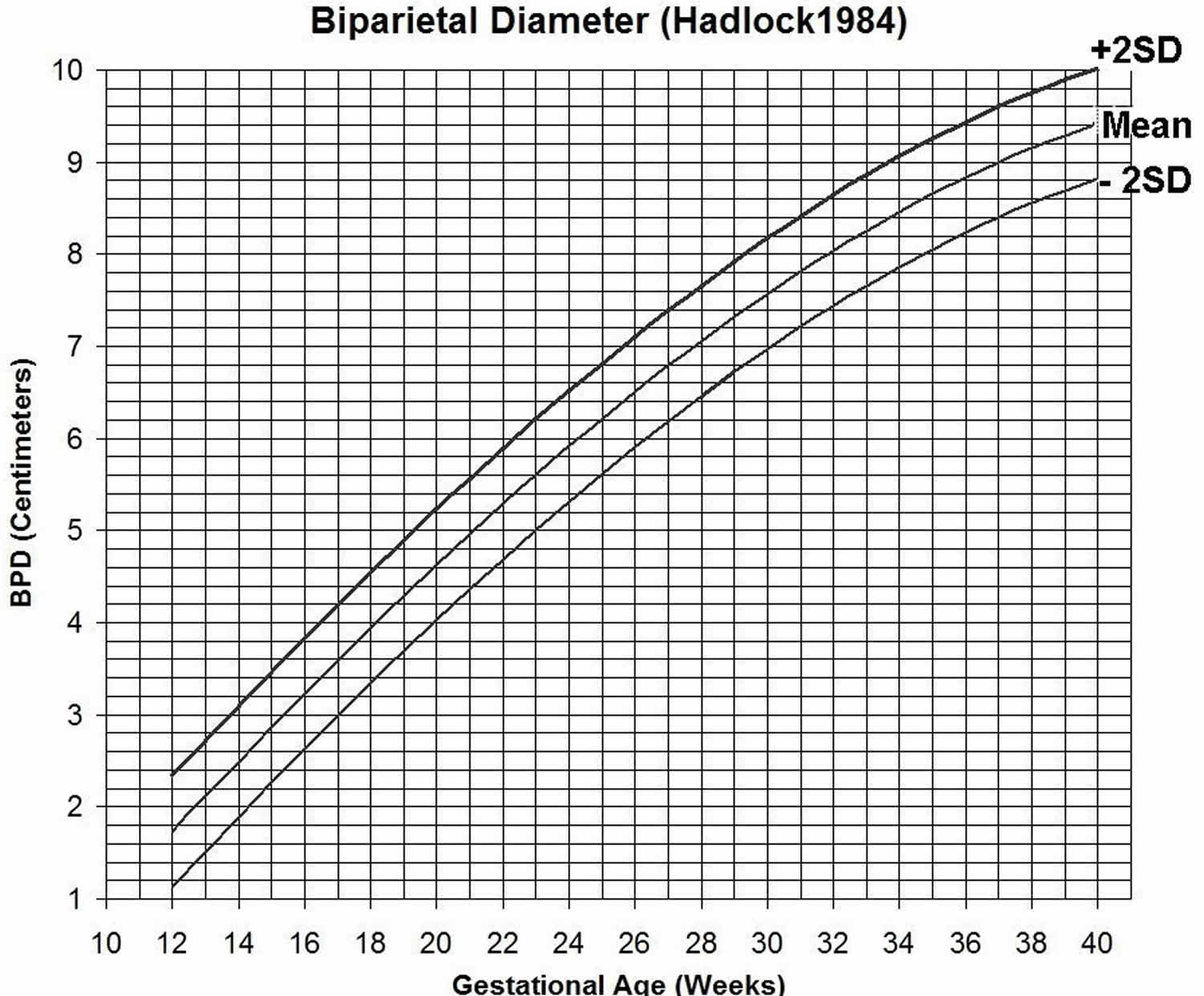
- Biparietal Diameter (BPD): This biometric parameter is recommended as a strong modality for dating because it has been extensively studied and is well reproduced. The technique involves a transabdominal approach by positioning the phased array or curvilinear transducer perpendicular to the fetal parietal bones. The calvarium should appear as a hyperechoic (bright white) structure that is smooth and symmetric. The Biparietal Diameter (BPD) is measured along a plane that intersects the third ventricle and the thalami. Using the caliper function, cursors are placed on the outer edge of the proximal skull and the inner edge of the distal skull. This value will give the biparietal diameter 4. Biparietal Diameter (BPD) parameter becomes limited after 22 weeks gestation due to normal biologic development with variations in fetal size and shape. If there is a physiologic or pathologic cause for the skull size and shape to be altered, the Biparietal Diameter (BPD) may produce false measurements 4.
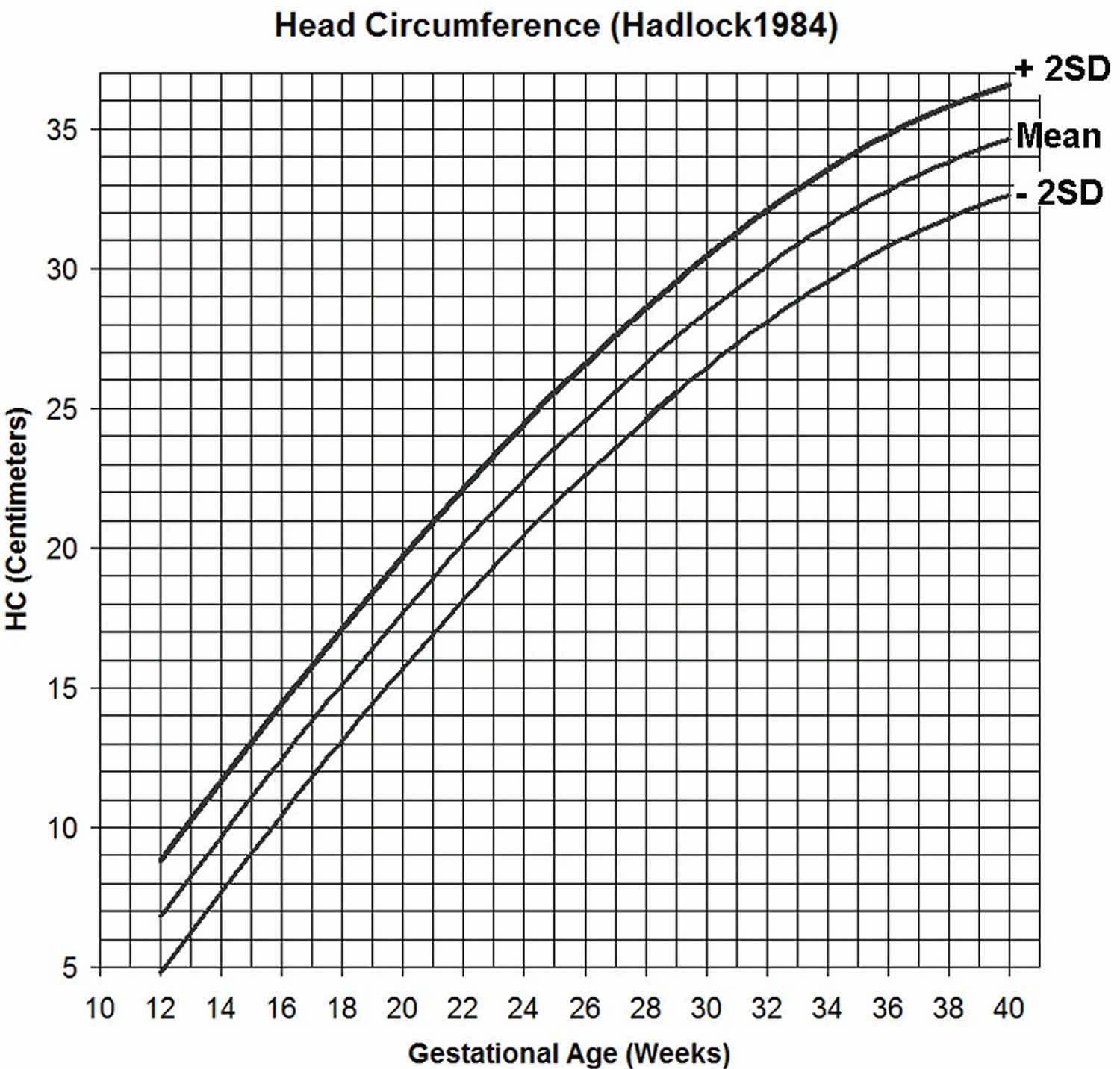
- Head Circumference (HC): This biometric parameter has been regarded as a good estimator of gestational age with some studies suggesting superiority to the biparietal diameter. This parameter may also be useful clinically in assessing for growth disorders. A similar sonographic approach as the Biparietal Diameter (BPD) is used here. A phased array or curvilinear transducer is used to visualize a plane that intersects the third ventricle and thalami. However, to achieve the greatest anterior-posterior diameter, the cavum septum pellucidum must be visualized anteriorly, and the tentorial hiatus must be visualized posteriorly. The cerebellum and lateral ventricles should not be visualized in a standard Head Circumference view. Using the calipers, mark the cursors on the outer margins of the calvarium bilaterally. The ultrasound should have an elliptical measuring tool that will generate a measurement of the perimeter of the calvarium 5. Head Circumference parameter is useful for obtaining gestation age, but multiple landmarks need to be identified before taking measurements. After 22 weeks, there is significant variation due to normal development affecting size and shape 5.
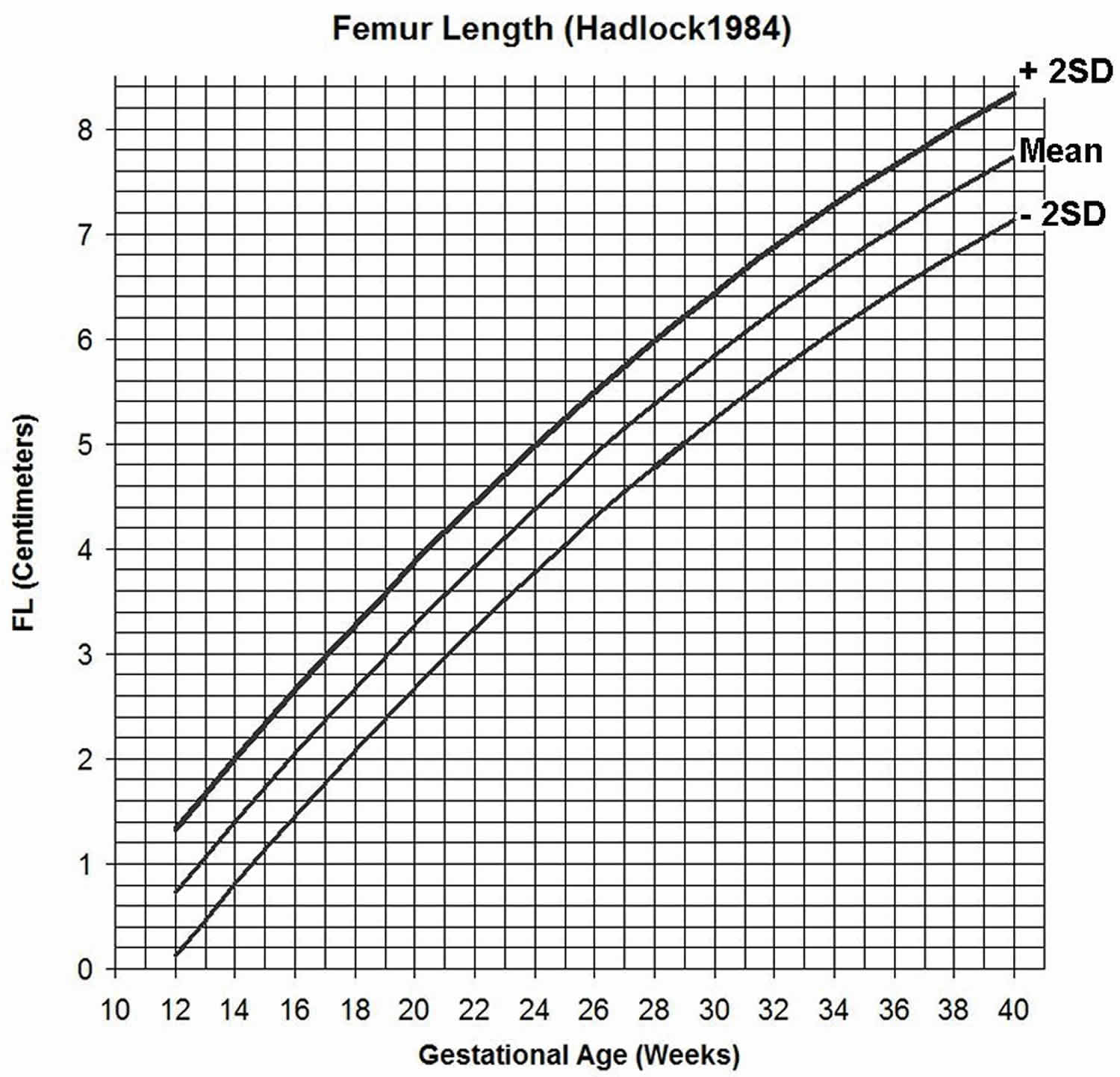
- Femur Length (FL): The femur can be visualized as early as 10 weeks gestation due to its size and density on ultrasound. Using a phased array or curvilinear transducer, align along the long axis of the closest femur. Proximally, visualize either the femoral head or greater trochanter and distally, visualize the femoral condyle. Using the calipers, measure the length of the diaphysis, at the junction of bone and cartilage, taking care not to include the femoral head, greater trochanter, or femoral condyle 5. In Femur Length (FC), multiple errors may occur when obtaining this parameter including but not limited to, non-ossified portions of the femur and not visualizing the full femur. This can lead to incorrect gestational age calculations. Average femur lengths may differ among certain ethnic groups or can be indicative of pathology. Again, this parameter does have variability after 22 weeks due to normal biologic development 5.
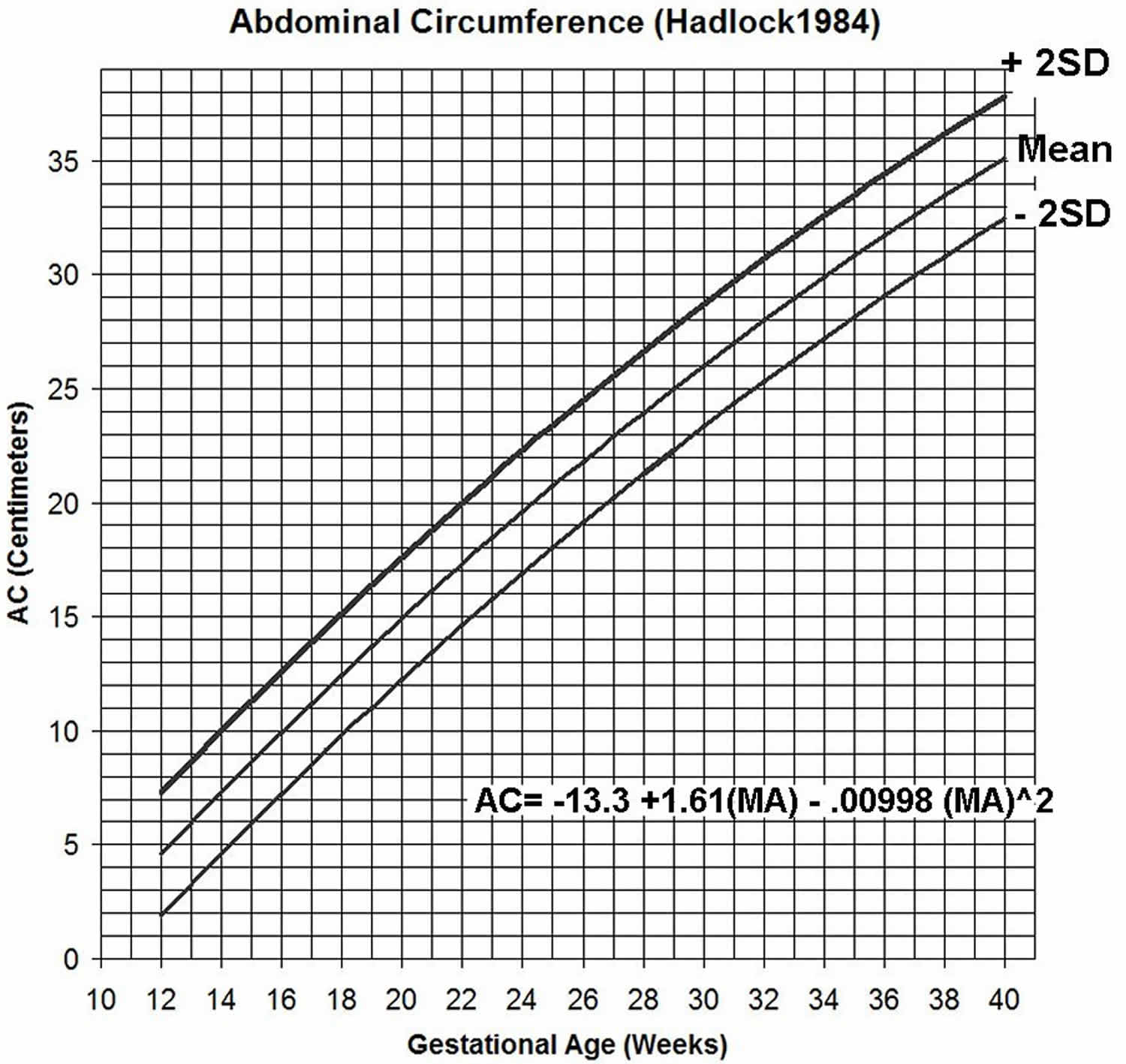
- Abdominal Circumference (AC): The biometric parameter is more difficult to measure and is less able to predict gestational age than the other described techniques accurately. However, it may be useful in fetuses with cranial or limb abnormalities and to estimate a fetal weight and note interval growth. Using the phased array or curvilinear transducer, position the transducer perpendicular to the fetal abdominal wall and visualize the symmetric appearance of the lower ribs. This view should be at the largest diameter of the fetal liver. Note, the fetal stomach is often visualized at this level. The umbilical portion of the left portal vein in its shortest view is another hallmark of appropriate positioning. Using the calipers, obtain four calibration points around the abdomen on the skin edge making sure not to include the rib cage. The elliptical tool may also be used to calculate circumference 5. Abdominal Circumference (AC) parameter has a wide margin of error for determining gestational age due to multiple factors including asymmetry of the abdomen, changes with respiration and movement, and user skills. Like the other parameters, significant variability is seen after 22 weeks 5.
- Third Trimester Dating: If gestational age has not been determined by the third trimester multiple parameters are correlated with estimated age and fetal maturity. For example, femoral epiphyseal ossification centers are often noted at 32 weeks. Proximal tibial ossification centers are visualized at 35 weeks. The proximal humeral ossification centers appear in the late trimester and have been correlated with fetal lung maturity 6.
Figure 2. Biparietal Diameter gestational age chart
[Source 5 ]Figure 3. Head Circumference gestational age chart
[Source 5 ]Figure 4. Femur Length gestational age chart
[Source 5 ]Figure 5. Abdominal Circumference gestational age chart
[Source 5 ]Postnatal Techniques
- Dubowitz Method: This was the historically standard method of determining postnatal gestational age based on 34 physical and neurologic assessments. These assessments are divided into 6 categories: tone, tone patterns, reflexes, movements, abnormal signs, and behaviors. Scores are assigned based on a detailed illustration sheet. Higher scores correlate with greater maturity. The total score can be plotted on a graph that also correlates with gestational age 7. Due to a large number of criteria needed to perform the exam, this method may be more difficult to perform on sick and preterm infants. Also, it can take up to 20 minutes to perform this exam. Studies have shown that this method tends to overestimate the gestational age 7.
- New Ballard Score: This improved scoring system is used to determine postnatal gestational age in infants as preterm as 20 weeks. The system is divided into 6 physical maturity components and six neuromuscular components. The physical maturity components include skin, lanugo, plantar creases, breast, ear/eye, and genitals. The neuromuscular components include posture, square window/wrist, arm recoil, popliteal angle, scarf sign, and heel to ear. Detailed illustrations have been created to assist the examiner in determining appropriate scores which correlate with gestational age. This exam is quicker to perform and may be more tolerable for sicker infants 8. Although this exam is quicker to perform, studies have shown that this system can overestimate gestational age in preterm infants 8.
Corrected gestational age
When a baby is born before their due date, they will have two ages: their corrected age and their chronological age. Your baby also had a gestational age, which was the age of your baby from conception to birth, calculated in weeks.
When following your baby’s growth and development, it can be helpful to know the difference between the ages:
- Corrected age: The age your baby would be if they had been born on their due date. For example, a baby who was born three months early (who now has a chronological age of seven months) has a corrected age of four months. Corrected age is useful while following your baby’s growth and development.
- Chronological age: The age of your baby since birth. Your child’s birthdays are celebrations of his or her chronological age.
To calculate your baby’s corrected age, start with your baby’s age in weeks (the number of weeks since birth) and subtract the number of weeks your baby was premature.
If your baby was born early, you have 2 important days to mark on the calendar:
- the day your baby was born and
- your estimated due date.
When you measure your baby’s development—that is, when you look at what is “normal” for your baby’s age—consider both of those dates. By looking at the difference between them, you can adjust your baby’s calendar age to account for prematurity and calculate his or her corrected age.
During the first 2 years, using your baby’s corrected age will give you a better idea when he or she should reach common developmental goals.
Calculating corrected age isn’t difficult.
Here’s how to calculate your baby’s corrected age:
Begin with your baby’s actual age in weeks (number of weeks since the date of birth) and then subtract the number of weeks your baby was preterm. This is your baby’s corrected age. (A pregnancy is now considered “full term” at 39 weeks.)
To determine the number of weeks’ preterm your baby was at birth, subtract gestational age at birth from 40.
The formula for calculating corrected age is:
- Actual Age in weeks minus Weeks preterm = Corrected Age
For example, Eli was born at 25 weeks gestation (15 weeks early) and 27 weeks have passed since his birth. His corrected age is 27 weeks – 15 weeks = 12 weeks or three months corrected.
For most pre-term babies, you will only need to correct their age until they are two or three years, as by this time most children have caught up developmentally to their peers.
Here’s an example:
If your baby was born at 32 weeks’ gestation, she was 8 weeks (2 months) preterm. If she is now 4 months old (16 weeks since birth), her corrected age is 2 months. In this case, even if your baby is 4 months old, you should expect her to have the developmental skills of a 2-month-old term baby. It would be unrealistic to expect your baby to be ready to roll from her stomach to her back—a skill that often develops in term babies around the age of 4 months.
Your baby may just be beginning to hold her head up and smile, which is developmentally normal for a term baby of 2 months and, therefore, for a preterm baby whose corrected age is 2 months.
Parents are often frustrated by well-meaning family and friends who express concerns about their baby’s development. People may think your baby is delayed for a 4-month-old, for example, when, in fact, she is on target for a baby with a corrected age of 2 months.
Small for gestational age
Small for gestational age also called low birth weight, is a term used to describe a baby or an infant who is smaller or less developed than normal for the baby’s gender and gestational age. Gestational age is the age of a fetus or baby that starts on the first day of the mother’s last menstrual period. Small for gestational age babies usually have birthweights below the 10th percentile for babies of the same gestational age. This means that they are smaller than many other babies of the same gestational age.
Ultrasound is used to find out if a fetus is smaller than normal for their age. This condition is called intrauterine growth restriction (IUGR). The most common definition of small for gestational age is a birth weight that is below the 10th percentile.
Small for gestational age babies may appear physically and neurologically mature but are smaller than other babies of the same gestational age. small for gestational age babies may be proportionately small (equally small all over) or they may be of normal length and size but have lower weight and body mass. small for gestational age babies may be premature (born before 37 weeks of pregnancy), full term (37 to 41 weeks), or post term (after 42 weeks of pregnancy).
Small for gestational age causes
Although some babies are small because of genetics (their parents are small), most small for gestational age babies are small because of fetal growth problems that occur during pregnancy. Many babies with small for gestational age have a condition called intrauterine growth restriction (IUGR). IUGR occurs when the fetus does not receive the necessary nutrients and oxygen needed for proper growth and development of organs and tissues. Intrauterine growth restriction can begin at any time in pregnancy. Early-onset intrauterine growth restriction is often due to chromosomal abnormalities, maternal disease, or severe problems with the placenta. Late-onset growth restriction (after 32 weeks) is usually related to other problems.
Some factors that may contribute to small for gestational age and/or intrauterine growth restriction include the following:
Maternal factors:
- High blood pressure
- Chronic kidney disease
- Advanced diabetes
- Heart or respiratory disease
- Malnutrition, anemia
- Infection
- Substance use (alcohol, drugs)
- Cigarette smoking
Factors involving the uterus and placenta:
- Decreased blood flow in the uterus and placenta
- Placental abruption (placenta detaches from the uterus)
- Placenta previa (placenta attaches low in the uterus)
- Infection in the tissues around the fetus
Factors related to the developing baby (fetus):
- Multiple gestation (for example, twins or triplets)
- Infection
- Birth defects
- Chromosomal abnormality
- Genetic diseases
- Inherited metabolic diseases
Small for gestational age prevention
Prenatal care is important in all pregnancies, and especially to identify problems with fetal growth. Stopping smoking and use of substances such as drugs and alcohol are essential to a healthy pregnancy and can reduce the risk for sudden infant death syndrome (SIDS) and other sleep-related infant deaths. Eating a healthy diet in pregnancy may also help.
Why is small for gestational age a concern?
When the fetus does not receive enough oxygen or nutrients during pregnancy, overall body and organ growth is limited, and tissue and organ cells may not grow as large or as numerous. Some of the conditions that cause small for gestational age and intrauterine growth restriction (IUGR) restrict blood flow through the placenta. This can cause the fetus to receive less oxygen than normal, increasing the risks for the baby during pregnancy, delivery, and afterwards.
Babies with small for gestational age and/or intrauterine growth restriction (IUGR) may have problems at birth including the following:
- Decreased oxygen levels
- Low body temperature
- Low Apgar scores (an assessment that helps identify babies with difficulty adapting after delivery)
- Meconium aspiration (inhalation of the first stools passed in utero) which can lead to difficulty breathing
- Hypoglycemia (low blood sugar)
- Difficulty maintaining normal body temperature
- Polycythemia (too many red blood cells)
Small for gestational age diagnosis
The baby with small for gestational age is often identified before birth. During pregnancy, a baby’s size can be estimated in different ways. The height of the fundus (the top of a mother’s uterus) can be measured from the pubic bone. This measurement in centimeters usually corresponds with the number of weeks of pregnancy after the 20th week. If the measurement is low for the number of weeks, the baby may be smaller than expected.
Although many small for gestational age babies have low birthweight, they are not all premature and may not experience the problems of premature babies. Other small for gestational age babies, especially those with IUGR, appear thin, pale, and with loose, dry skin. The umbilical cord is often thin, and dull-looking rather than shiny and fat.
Other diagnostic procedures may include the following:
Ultrasound. Ultrasound (a test using sound waves to create a picture of internal structures) is a more accurate method of estimating fetal size. Measurements can be taken of the fetus’ head and abdomen and compared with a growth chart to estimate fetal weight. The fetal abdominal circumference is a helpful indicator of fetal nutrition.
Doppler flow. Another way to interpret and diagnose IUGR during pregnancy is Doppler flow, which uses sound waves to measure blood flow. The sound of moving blood produces wave-forms that reflect the speed and amount of the blood as it moves through a blood vessel. Blood flow through blood vessels in both the fetal brain and the umbilical cord can be checked with Doppler flow studies.
Mother’s weight gain. A mother’s weight gain can also indicate a baby’s size. Small maternal weight gains in pregnancy may correspond with a small baby
Gestational assessment. Babies are weighed within the first few hours after birth. The weight is compared with the baby’s gestational age and recorded in the medical record. The birthweight must be compared to the gestational age. Some doctors use a formula for calculating a baby’s body mass to diagnose small for gestational age.
Treatment of babies who are small for gestational age
Specific treatment for small for gestational age will be determined by your baby’s doctor based on:
- Your baby’s gestational age, overall health, and medical history
- Extent of the condition
- Your baby’s tolerance for specific medications, procedures, or therapies
- Expectations for the course of the condition
- Your opinion or preference
Babies with small for gestational age may be physically more mature than their small size indicates. But they may be weak and less able to tolerate large feedings or to stay warm. Treatment of the small for gestational age baby may include:
- Temperature controlled beds or incubators
- Tube feedings (if the baby does not have a strong suck)
- Checking for hypoglycemia (low blood sugar) through blood tests
- Monitoring of oxygen levels
Babies who are small for gestational age and are also premature may have additional needs including oxygen and mechanical help to breathe.
Large for gestational age
Large for gestational age is a term used to describe babies who are born weighing more than the usual amount for the number of weeks of pregnancy. Large for gestational age babies have birthweights greater than the 90th percentile for their gestational age, meaning that they weigh more than 90 percent of all babies of the same gestational age. The average baby weighs about 7 pounds at birth. About 9 percent of all babies weigh more than 4,000 grams (8 pounds, 13 ounces). Rarely do babies weigh over 10 pounds.
Large for gestational age means that a fetus or infant is larger or more developed than normal for the baby’s gestational age.
The large for gestational age measurement is based on the estimated gestational age of the fetus or infant. Their actual measurements are compared with normal height, weight, head size, and development of a fetus or infant of the same age and gender.
Although most large for gestational age babies are born at term (37 to 41 weeks of pregnancy), a few premature babies may be large for gestational age.
Large for gestational age causes
Some babies are large because their parents are large; genetics does play a part. Birthweight may also be related to the amount of weight a mother gains during pregnancy. Excessive weight gain can translate to increased fetal weight.
By far, maternal diabetes is the most common cause of large for gestational age babies. Diabetes during pregnancy causes the mother’s increased blood glucose (sugar) to circulate to the baby. In response, the baby’s body makes insulin. All the extra sugar and the extra insulin production can lead to excessive growth and deposits of fat, thus, a larger baby.
Common causes of large for gestational age are:
- Gestational diabetes
- Obese pregnant mother
- Excessive weight gain during pregnancy
A baby that is large for gestational age has a higher risk of birth injury. There is also a risk of complications of low blood sugar after delivery if the mother has diabetes.
Large for gestational age prevention
Prenatal care is important in all pregnancies, especially to monitor fetal growth when a baby seems to be too small or too large. Examinations during pregnancy that show a large baby can help identify a mother who may have undetected diabetes, or other problems. Careful management of diabetes and proper weight gain, according to your doctor’s recommendations, can help lower some of the risks to the baby.
Why is large for gestational age a concern?
Because large for gestational age babies are so large, delivery can be difficult. Delivery problems may include the following:
- Prolonged vaginal delivery time
- Difficult birth
- Birth injury
- Increased risk of cesarean delivery
Because many large babies are born to diabetic mothers, many problems of large for gestational age babies are related to problems with glucose regulation. These may include the following:
- Hypoglycemia (low blood sugar) of baby after delivery
- Increased incidence of birth defects
- Respiratory distress (difficulty breathing)
Many babies with large for gestational age also have hyperbilirubinemia (jaundice or yellowing of the skin, eyes, and mucous membranes).
How is large for gestational age diagnosed?
During pregnancy, a baby’s birthweight can be estimated in different ways. The height of the fundus (the top of a mother’s uterus) can be measured from the pubic bone. This measurement, in centimeters, usually corresponds with the number of weeks of pregnancy. If the measurement is high for the number of weeks, the baby may be larger than expected. Other diagnostic procedures may include the following:
- Ultrasound (a test using sound waves to create a picture of internal structures) is a more accurate method of estimating fetal size. Measurements can be taken of the fetus’ head, abdomen, and femur to estimate fetal weight.
- A mother’s weight gain can also influence a baby’s size. Excessive maternal weight gain in pregnancy may correspond with a big baby.
Babies are weighed within the first few hours after birth. The weight is compared with the baby’s gestational age and recorded in the medical record.
Large for gestational age treatment
Specific treatment for large for gestational age will be determined by your baby’s doctor based on:
- Your baby’s gestational age, overall health, and medical history
- Extent of the condition
- Your baby’s tolerance for specific medications, procedures, or therapies
- Expectations for the course of the condition
- Your opinion or preference
If ultrasound examinations during pregnancy show a fetus is quite large, some doctors may recommend early delivery. A planned cesarean delivery may also be recommended depending on the ultrasound estimate of the baby’s weight.
After delivery, a large for gestational age baby will be carefully examined for any birth injuries. Blood glucose testing is also performed to check for hypoglycemia.
Gestational age vs Fetal age
Fetal age is the actual age of the growing baby. Gestational age is the age of the pregnancy from the last normal menstrual period (LMP). Most references to pregnancy are usually in gestational age rather than fetal age development.
Pregnancy is also divided into trimesters which last about 12 – 14 weeks each. Similar to development, these can be calculated from different dates so not all trimester calculations will equal the same. The following information divides the three trimesters into a little over 3 completed months each.
The first trimester is week 1 through the end of week 13 and consists of the 1st, 2nd and 3rd months. The second trimester usually ends around the 26th week and consists of the 4th, 5th and 6th completed months. The third trimester can end anywhere between the 38th – 42nd week and is the 7th, 8th and 9th completed months of pregnancy.
How is physical maturity assessed?
The physical assessment part of the Dubowitz/Ballard Examination examines physical characteristics that look different at various stages of a baby’s gestational maturity. Babies who are physically mature usually have higher scores than premature babies.
Points are given for each area of assessment, with a low of minus one or minus two for extreme immaturity to as high as plus 4 or plus 5 for postmaturity. Areas of assessment include the following:
- Skin textures (for example, sticky, smooth, peeling)
- Lanugo. This is the soft downy hair on a baby’s body. It is absent in immature babies, then appears with maturity, and then disappears again with postmaturity.
- Plantar creases. These creases on the soles of the feet range from absent to covering the entire foot, depending on the maturity.
- Breast. The thickness and size of breast tissue and areola (the darkened ring around each nipple) are assessed.
- Eyes and ears. Whether or not eyes are fused or open, and the amount of cartilage and stiffness of the ear tissue are noted.
- Genitals, male. The presence of testes and appearance of scrotum, from smooth to wrinkled, are assessed.
- Genitals, female. The appearance and size of the clitoris and the labia are assessed.
How is neuromuscular maturity assessed?
Six evaluations of the baby’s neuromuscular system are performed. These include:
- Posture. How the baby holds his or her arms and legs.
- Square window. How far the baby’s hands can be flexed toward the wrist.
- Arm recoil. How far the baby’s arms “spring back” to a flexed position.
- Popliteal angle. How far the baby’s knees extend.
- Scarf sign. How far the elbows can be moved across the baby’s chest.
- Heel to ear. How close the baby’s feet can be moved to the ears.
A score is assigned to each assessment area. Typically, the more neurologically mature the baby, the higher the score.
When the physical assessment score and the neuromuscular score are added together, the gestational age can be estimated. Scores range from very low for immature babies (less than 26 to 28 weeks) to very high scores for mature and postmature babies. However, the score might not be accurate in very low birth weight preterm infants (birth weight less than 1500 grams).
All of these examinations are important ways to learn about your baby’s well-being at birth. By identifying any problems, your baby’s doctor can plan the best possible care.
References- Loytved CA, Fleming V. Naegele’s rule revisited. Sex Reprod Healthc. 2016 Jun;8:100-1.
- Loytved CA, Fleming V. Naegele’s rule revisited. Sex Reprod Healthc. 2016 Jun;8:100-1
- Robinson HP, Fleming JE. A critical evaluation of sonar “crown-rump length” measurements. Br J Obstet Gynaecol. 1975 Sep;82(9):702-10.
- Hohler CW, Quetel TA. Comparison of ultrasound femur length and biparietal diameter in late pregnancy. Am. J. Obstet. Gynecol. 1981 Dec 01;141(7):759-62
- Hadlock FP, Deter RL, Harrist RB, Park SK. Estimating fetal age: computer-assisted analysis of multiple fetal growth parameters. Radiology. 1984 Aug;152(2):497-501
- Benson CB, Doubilet PM. Sonographic prediction of gestational age: accuracy of second- and third-trimester fetal measurements. AJR Am J Roentgenol. 1991 Dec;157(6):1275-7
- Dubowitz L, Ricciw D, Mercuri E. The Dubowitz neurological examination of the full-term newborn. Ment Retard Dev Disabil Res Rev. 2005;11(1):52-60
- Ballard JL, Khoury JC, Wedig K, Wang L, Eilers-Walsman BL, Lipp R. New Ballard Score, expanded to include extremely premature infants. J. Pediatr. 1991 Sep;119(3):417-23.