What is glomerulonephritis
Glomerulonephritis is a general term for a group of disorders in which there is bilateral, symmetrical inflammation of the tiny filters in your kidneys (glomeruli). Most often, glomerulonephritis is caused by an autoimmune disease (your immune system attacking healthy kidney tissue), but it can also result from infection.
A renal glomerulus consists of a capillary plexus invaginating the blind end of the proximal renal tubule. There are about one million glomeruli in each kidney. The glomerular capillaries are lined by a glomerular basement membrane. Glomeruli remove excess fluid, electrolytes and waste from your bloodstream and pass them into your urine.
Glomerulonephritis doesn’t usually cause any noticeable symptoms. It’s more likely to be diagnosed when blood or urine tests are carried out for another reason.
Glomerulonephritis can come on suddenly (acute) or gradually (chronic). Glomerulonephritis occurs on its own or as part of another disease, such as lupus or diabetes. Severe or prolonged inflammation associated with glomerulonephritis can damage your kidneys. Although mild cases of glomerulonephritis can be treated effectively, for some people the condition can lead to long-term kidney problems.
Treatment for glomerulonephritis depends on the cause and severity of your condition. Mild cases may not need any treatment.
Treatment can be as simple as making changes to your diet, such as eating less salt to reduce the strain on your kidneys.
Medication to lower blood pressure, such as angiotensin-converting enzyme (ACE) inhibitors, is commonly prescribed because they help protect the kidneys.
If the condition is caused by a problem with your immune system, medication called immunosuppressants may be used.
Table 1. Classification of Primary Glomerular Disease Based on Clinical Syndrome
| Nephrotic Syndrome |
| Minimal change disease |
| Membranous glomerular nephropathy |
| Focal segmental glomerulosclerosis |
| Membranoproliferative glomerulonephritis* |
| C1q nephropathy† |
| Fibrillary glomerulonephritis† |
| Acute Glomerulonephritis |
| Membranoproliferative glomerulonephritis |
| IgA nephropathy |
| Rapidly Progressive Glomerulonephritis |
| Antiglomerular basement membrane disease |
| Immune complex crescentic glomerulonephritis |
| Pauci-immune crescentic glomerulonephritis |
| Membranoproliferative glomerulonephritis |
| IgA nephropathy |
| Membranous glomerular nephropathy (rare) |
| Asymptomatic Hematuria and/or Proteinuria |
| IgA nephropathy |
| Membranoproliferative glomerulonephritis |
Footnote:
* Usually with active sediment; e.g., red blood cell casts, dysmorphic red blood cells), unlike other causes of nephrotic syndrome.
† Extremely rare disorders.
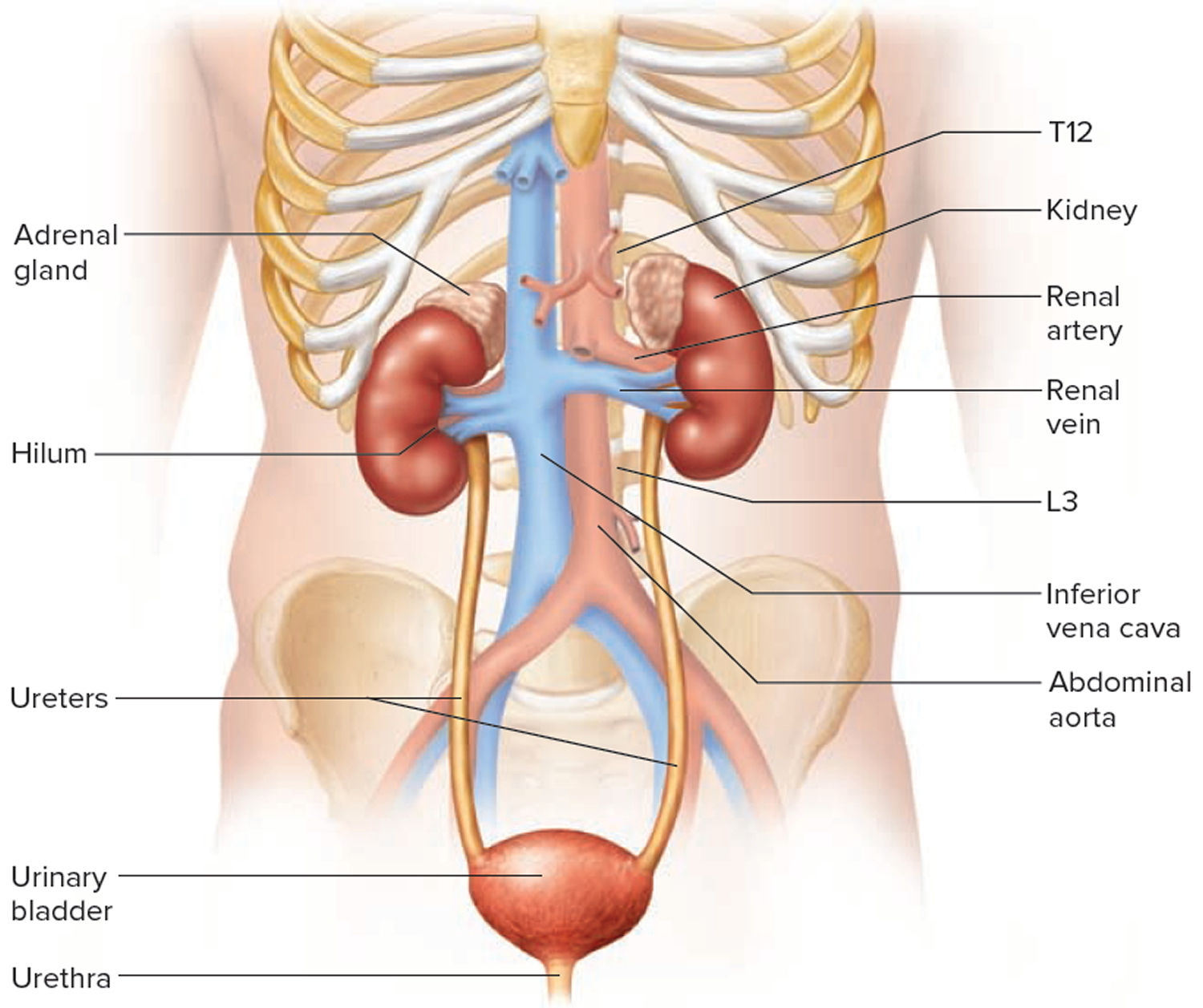
[Source 1]Kidney Anatomy
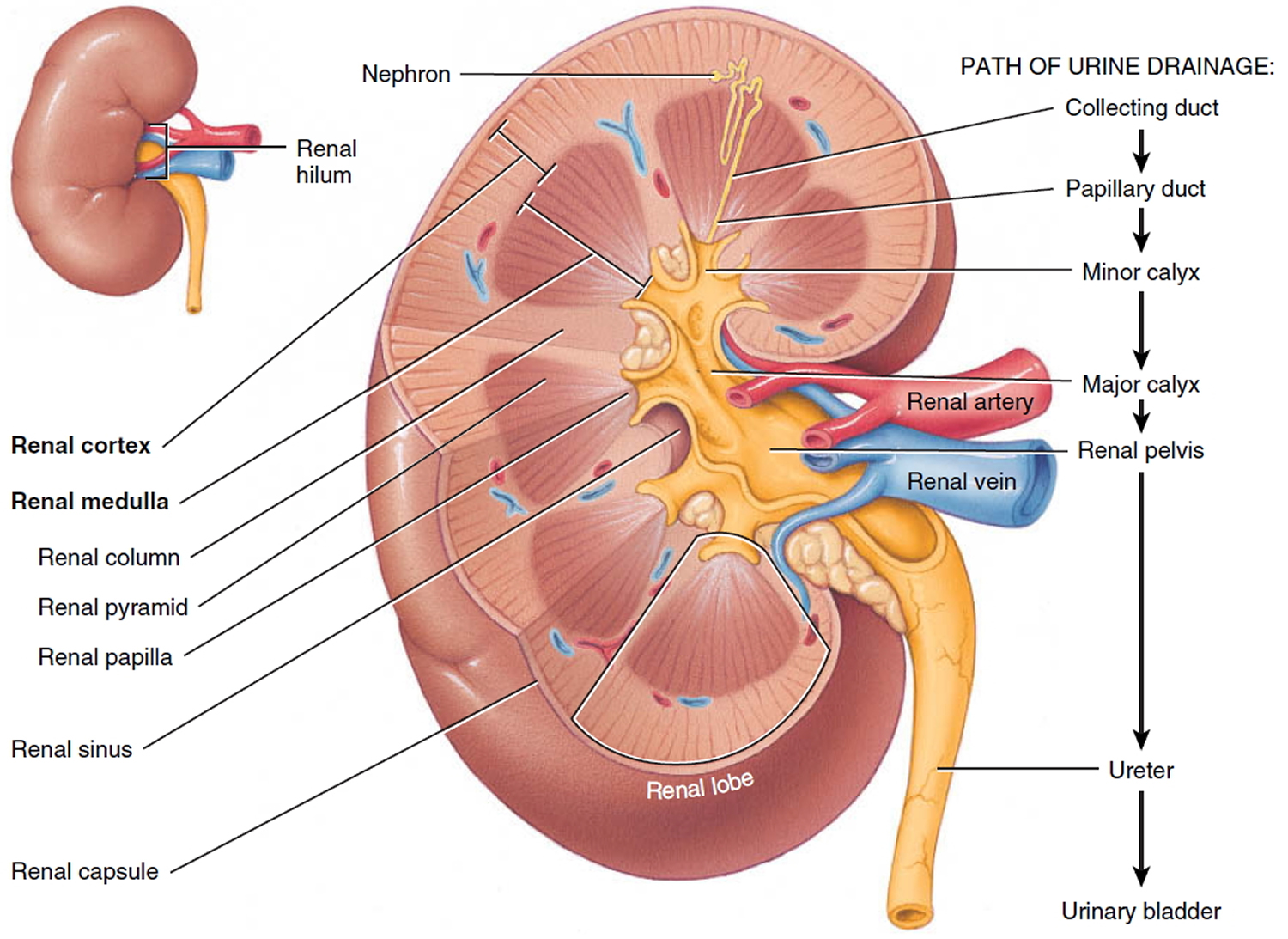
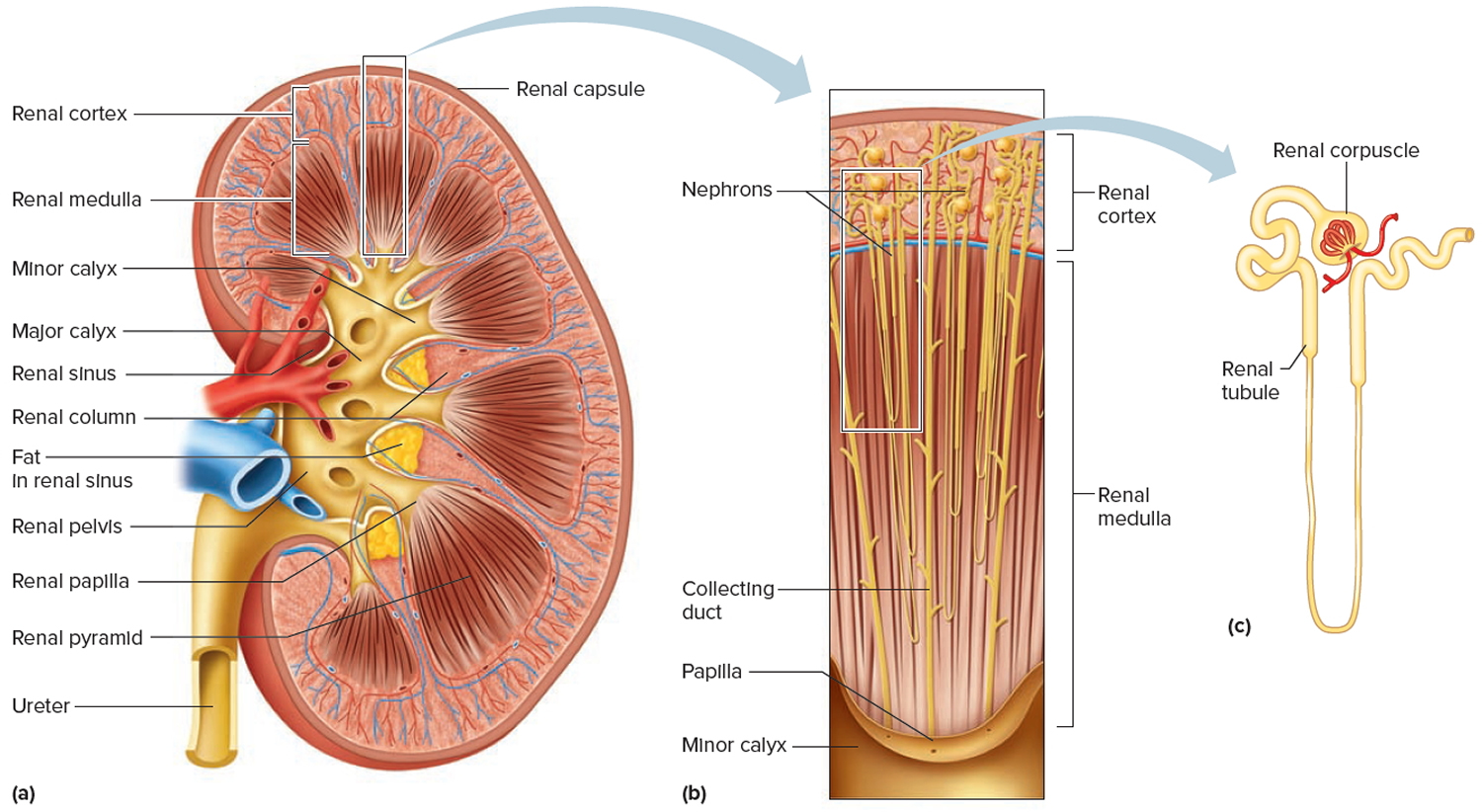
A frontal section through the kidney reveals two distinct regions: a superficial, light red region called the renal cortex and a deep, darker reddish-brown inner region called the renal medulla (medulla = inner portion) (Figures 2 and 3). The renal medulla consists of several cone-shaped renal pyramids. The base (wider end) of each pyramid faces the renal cortex, and its apex (narrower end), called a renal papilla, points toward the renal hilum. The renal cortex is the smooth-textured area extending from the renal capsule to the bases of the renal pyramids and into the spaces between them. It is divided into an outer cortical zone and an inner juxtamedullary zone. Those portions of the renal cortex that extend between renal pyramids are called renal columns.
Together, the renal cortex and renal pyramids of the renal medulla constitute the parenchyma or functional portion of the kidney. Within the parenchyma are the functional units of the kidney—about 1 million microscopic structures called nephrons. Filtrate (filtered fluid) formed by the nephrons drains into large papillary ducts, which extend through the renal papillae of the pyramids. The papillary ducts drain into cuplike structures called minor and major calyces. Each kidney has 8 to 18 minor calyces and 2 or 3 major calyces. A minor calyx receives filtrate from the papillary ducts of one renal papilla and delivers it to a major calyx. Once the filtrate enters the calyces it becomes urine because no further reabsorption can occur. The reason for this is that the simple epithelium of the nephron and ducts becomes transitional epithelium in the calyces. From the major calyces, urine drains into a single large cavity called the renal pelvis and then out through the ureter to the urinary bladder.
Figure 1. Kidney location
Figure 2. Kidney anatomy
Figure 3. Kidney structure
Figure 4. Microcirculation of the kidney
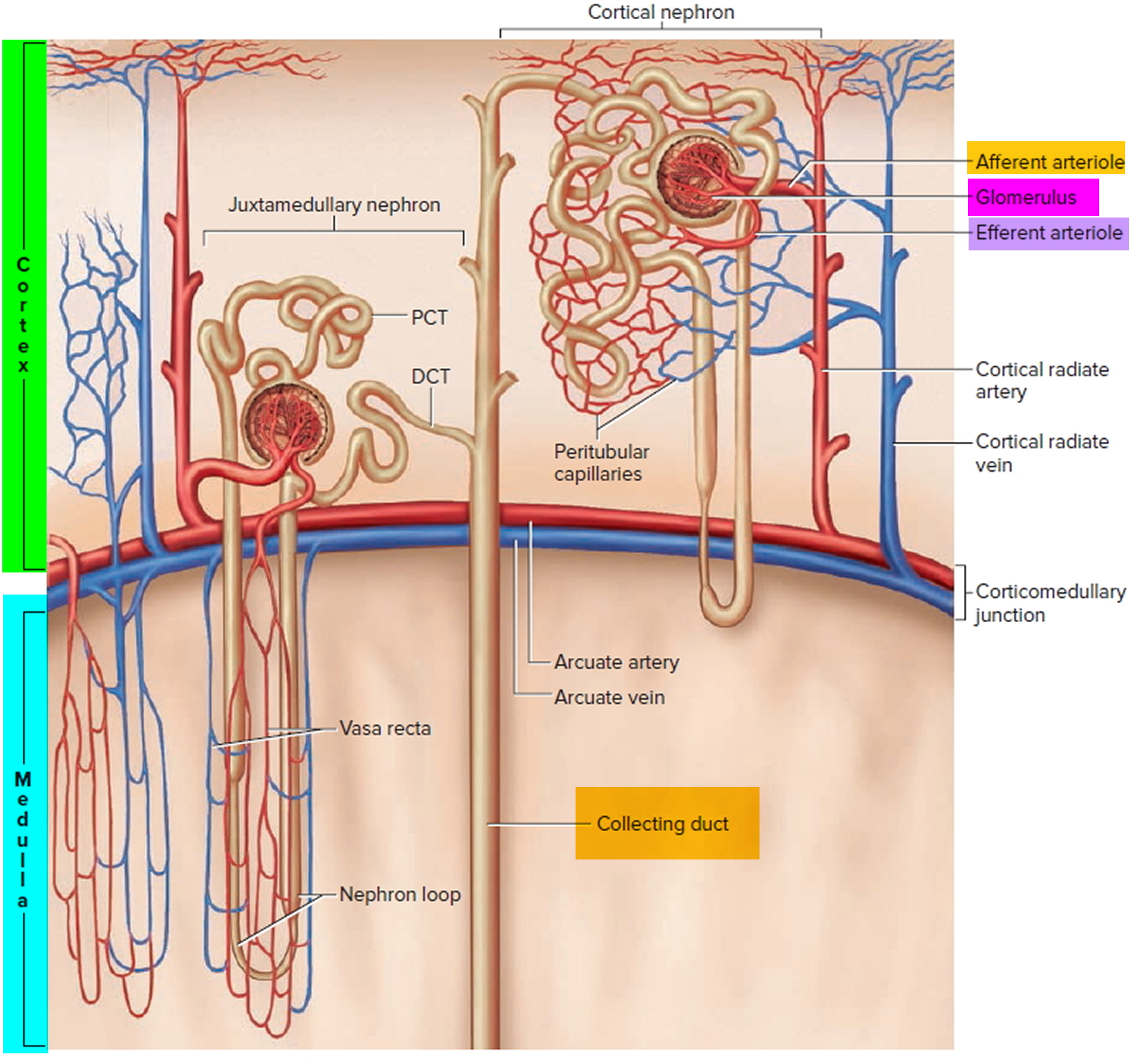 Note: DCT = distal convoluted tubule; PCT = proximal convoluted tubule
Note: DCT = distal convoluted tubule; PCT = proximal convoluted tubule
Glomerulonephritis types
There are two types of glomerulonephritis—acute and chronic glomerulonephritis.
Acute glomerulonephritis
The acute glomerulonephritis develops suddenly. You may get it after an infection in your throat or on your skin. Sometimes, you may get better on your own. Other times, your kidneys may stop working unless the right treatment is started quickly. The early symptoms of the acute glomerulonephritis are:
- puffiness of your face in the morning
- blood in your urine (or brown urine)
- urinating less than usual.
You may be short of breath and cough because of extra fluid in your lungs. You may also have high blood pressure. If you have one or all of these symptoms, be sure to see your doctor right away.
Acute glomerulonephritis causes
The acute disease may be caused by infections such as strep throat. It may also be caused by other illnesses, including lupus, Goodpasture’s syndrome, Wegener’s disease, and polyarteritis nodosa. Early diagnosis and prompt treatment are important to prevent kidney failure.
Acute glomerulonephritis treatment
The acute glomerulonephritis may go away by itself. Sometimes you may need medication or even temporary treatment with an artificial kidney machine to remove extra fluid and control high blood pressure and kidney failure. Antibiotics are not used for acute glomerulonephritis, but they are important in treating other forms of disease related to bacterial infection. If your illness is getting worse rapidly, you may be put on high doses of medicine that affect your immune system. Sometimes, your doctor may order plasmapheresis, a special blood filtering process to remove harmful proteins from your blood.
Chronic glomerulonephritis
The chronic glomerulonephritis may develop silently (without symptoms) over several years. Chronic glomerulonephritis often leads to complete kidney failure. Early signs and symptoms of the chronic glomerulonephritis may include:
- Blood or protein in the urine (hematuria, proteinuria)
- High blood pressure
- Swelling of your ankles or face (edema)
- Frequent nighttime urination
- Very bubbly or foamy urine
Symptoms of kidney failure include:
- Lack of appetite
- Nausea and vomiting
- Tiredness
- Difficulty sleeping
- Dry and itchy skin
- Nighttime muscle cramps
Chronic glomerulonephritis causes
Sometimes, chronic glomerulonephritis runs in the family. This kind often shows up in young men who may also have hearing loss and vision loss. Some chronic glomerulonephritis are caused by changes in the immune system. However, in many cases, the cause is not known. Sometimes, you will have one acute attack of glomerulonephritis and develop the chronic glomerulonephritis years later.
Chronic glomerulonephritis treatment
There is no specific treatment for the chronic form of the illness. You doctor may tell you to:
- Eat less protein, salt and potassium
- Control your blood pressure
- Take diuretics (water pills) to treat puffiness and swelling
- Take calcium supplements
Membranoproliferative glomerulonephritis
Membranoproliferative glomerulonephritis is a form of glomerulonephritis caused by an abnormal immune response. Deposits of antibodies build up in a part of the kidneys called the glomerular basement membrane. This membrane helps filter wastes and extra fluids from the blood.
Biopsy specimens from patients with membranoproliferative glomerulonephritis are characterized by global capillary wall thickening and glomerular hypercellularity. The increased cellular content occurs because of proliferation of resident glomerular cells, as well as infiltrating mononuclear cells and neutrophils. Often seen, but not necessarily specific to membranoproliferative glomerulonephritis, is double contouring or splitting of the glomerular capillary basement membranes. A subset of patients with membranoproliferative glomerulonephritis may exhibit cellular crescents within Bowman’s space. Immunofluorescence studies demonstrate diffuse granular or bandlike intense staining of capillary loops and mesangium with C3, and to a lesser extent IgG and IgM. Membranoproliferative glomerulonephritis pathognomonic changes on electron microscopy are subendothelial and mesangial electron-dense deposits; the former are found in an expanded subendothelial region of the glomerular basement membrane formed by projections of mesangial cytoplasm. Some subepithelial deposits may also been seen, but they are not as prominent as in cases of membranous glomerulonephritis (discussed later).
The 2 forms of this disease are membranoproliferative glomerulonephritis I and membranoproliferative glomerulonephritis II.
Most people with the disease have type I. Membranoproliferative glomerulonephritis II is much less common. It also tends to get worse faster than membranoproliferative glomerulonephritis I.
A subset of membranoproliferative glomerulonephritis cases (type II membranoproliferative glomerulonephritis) have a different hallmark electron microscopic finding than the discrete subendothelial deposits (type I membranoproliferative glomerulonephritis). In the former, a bandlike, almost continuous, ribbon of the electron-dense material is found in the subendothelial space.
Damage to this membrane affects the kidney’s ability to create urine normally. It may allow blood and protein to leak into the urine. If enough protein leaks into the urine, fluid may leak out of the blood vessels into body tissues, leading to swelling (edema). Nitrogen waste products may also build up in the blood (azotemia).
Primary membranoproliferative glomerulonephritis is a disease mostly found in children, with more than 75% of cases diagnosed between ages 8 and 16 years 2. It accounts for approximately 10% of biopsy specimens of primary glomerular disorders.
Patients with membranoproliferative glomerulonephritis follow the rule of thirds. That is, approximately one third will have a spontaneous remission, one third will have persistent manifestations that intermittently wax and wane, and one third will have a progressive decline to end stage kidney disease. Factors that may predict the latter include heavier degrees of proteinuria or the nephrotic syndrome, or both, hypertension, advanced azotemia at baseline, and a nephritic presentation, especially with crescents on biopsy. After excluding important secondary causes of membranoproliferative glomerulonephritis, most notably hepatitis C infection, immunosuppressive therapy should be tried for these patients, in addition to conservative management. Most data on treatment have come from pediatric studies 3, but a potential adult regimen includes prednisone, 2 mg/kg every other day for 3 to 12 months, depending on the rate of response. If a significant response is seen, with a decline in proteinuria, stabilization of serum creatinine level, and improvement in activity of the urine sediment, the steroids may be tapered to 20 mg every other day and maintained for another few years. Other therapies, in addition to steroids, such as antiplatelet agents (e.g., aspirin, dipyridamole), with or without cytotoxic agents, have not convincingly proven to be of benefit.
Membranoproliferative glomerulonephritis causes
In membranoproliferative glomerulonephritis, your immune system starts to attack the healthy cells in your kidneys which damage the glomeruli. Your immune system makes proteins called antibodies to attack substances in your body that they see as harmful. The harmful substances are called antigens. Antigens combine with antibodies to make immune complexes. These immune complexes get stuck in your kidneys and cause damage.
Membranoproliferative glomerulonephritis is classified as an immune complex disease and the presumptive pathophysiologic mechanism is the inappropriate production of antibodies recognizing a nephritogenic antigen. Membranoproliferative glomerulonephritis is believed to occur as a result of deposition of circulating antigen-antibody complexes. These traverse the large pores found between glomerular endothelial cells and deposit between them and the glomerular basement membrane. Complement activation results from the deposition of these antigen-antibody complexes and results in a cascade of proinflammatory signals that stimulate local cell proliferation and recruitment of circulating immune cells, which augments the inflammatory reaction. This ongoing inflammation is believed to be the major reason for the ensuing renal damage.
Causes of membranoproliferative glomerulonephritis may include:
- Autoimmune diseases (systemic lupus erythematosus, scleroderma, Sjögren syndrome, sarcoidosis)
- Cancer (leukemia, lymphoma)
- Infections (hepatitis B, hepatitis C, endocarditis, malaria)
Membranoproliferative glomerulonephritis prognosis
The disorder often slowly gets worse and eventually results in chronic kidney failure.
Half of people with this condition develop chronic kidney failure within 10 years. This is more likely in those who have higher levels of protein in their urine.
Membranoproliferative glomerulonephritis possible complications
Complications that may result from this disease include:
- Acute nephritic syndrome
- Acute renal failure
- Chronic kidney disease
Membranoproliferative glomerulonephritis symptoms
Symptoms may include any of the following:
- Blood in the urine (hematuria): Glomerular disease can cause your glomeruli to leak blood into your urine. Your urine may look pink or light brown from blood.
- Protein in the urine (proteinuria): Glomerular disease can cause your glomeruli to leak protein into your urine. Your urine may be foamy because of the protein.
- Changes in mental status such as decreased alertness or decreased concentration
- Cloudy urine
- Dark urine (smoke, cola, or tea colored)
- Decrease in urine volume
- Swelling of any part of the body (edema). Glomerular disease can cause fluid to build in your body. The extra fluid can cause swelling in body parts like your hands, ankles, or around your eyes.
- Nephrotic Syndrome: A set of symptoms that happen together and affect your kidneys. These include:
- Swelling in body parts like your legs, ankles, or around your eyes (edema)
- Large amounts of protein in your urine (proteinuria)
- Loss of protein in your blood
- High levels of fat lipids in your blood (high cholesterol)
- High blood pressure
Membranoproliferative glomerulonephritis diagnosis
The health care provider will examine you and ask about your symptoms. The provider may find that you have signs of too much fluid in the body, such as:
- Swelling, often in the legs
- Abnormal sounds when listening to your heart and lungs with a stethoscope
- You may have high blood pressure
The following tests help confirm the diagnosis:
- Urine test: A urine test will help find protein and blood in your urine.
- Blood test: A blood test will help find levels of protein, cholesterol, and wastes in your blood.
- Glomerular filtration rate (GFR): A blood test will be done to know how well your kidneys are filtering the wastes from your body.
- Kidney biopsy (to confirm membranoproliferative glomerulonephritis type I or II): In this test, a tiny piece of your kidney is removed with a special needle, and looked at under a microscope. Because membranoproliferative glomerulonephritis is so rare, and because knowing the class of your disease can help your healthcare provider decide on the best treatment, it is very important that the person looking at your biopsy is an expert in glomerular diseases. You or your doctor may need to contact a large research center to find such an expert.
- Genetic Testing: A test may be done to see if the cause of your membranoproliferative glomerulonephritis comes from genes you inherited from your family.
Membranoproliferative glomerulonephritis treatment
Treatment depends on the symptoms. The goals of treatment are to reduce symptoms, prevent complications, and slow the progression of the disorder.
Before a treatment plan is made, the doctor will try to find the cause of your membranoproliferative glomerulonephritis. If membranoproliferative glomerulonephritis is not caused by another disease, such as hepatitis C, your treatment plan will be different. Treatment with many medications can slow the progress of the disease and help you manage your symptoms like high blood pressure, proteinuria, and edema.
You may need a change in diet. This may include limiting sodium, fluids, or protein to help control high blood pressure, swelling, and the buildup of waste products in the blood.
Medicines that may be prescribed include:
- Blood pressure medicines such as Angiotensin-converting enzyme (ACE) inhibitors and Angiotensin 2 receptor blockers (ARBs)
- Dipyridamole, with or without aspirin
- Diuretics
- Medicines to suppress the immune system (immunosuppressive drugs), such as cyclophosphamide
- Corticosteroids (often called “steroids”)
- Diet change
Corticosteroids and immunosuppressive drugs: These medications are used to calm your immune system (your body’s defense system) and stop it from attacking your glomeruli.
Angiotensin-converting enzyme (ACE) inhibitors and angiotensin 2 receptor blockers (ARBs): These are blood pressure medications used to reduce protein loss and control blood pressure.
Diet change: Some diet changes may be needed, such as reducing salt (sodium) and protein in your food choices to lighten the load of wastes on the kidneys.
For both adults and children, the general treatment plan will be the same. The goal of your treatment is to stop your immune system from causing harm to your kidneys by giving you certain types of medications. There’s no cure for the disease. Treatment focuses on controlling your symptoms and slowing the progression of the disease.
Treatment is more effective in children than in adults. Dialysis or kidney transplant may eventually be needed to manage kidney failure.
Crescentic glomerulonephritis
Crescentic glomerulonephritis is defined as any glomerular disease characterized by extensive crescents involving more than 50% of the glomeruli with a rapid loss of renal function (at least 50% decline in the glomerular filtration rate {GFR} within 3 months) 4.
Crescentic glomerulonephritis is classified into 4 types according to immunofluorescence findings:
- Type I was defined as linear IgG staining/deposition of immunoglobulins along the glomerular basement membrane [anti-GBM crescentic glomerulonephritis]. Approximately one-half of patients with anti-GBM glomerulonephritis have pulmonary capillaritis (Goodpasture’s syndrome). Patients with anti-GBM disease can have anti-GBM glomerulonephritis alone or in combination with anti-GBM, antibody-mediated pulmonary hemorrhage (Goodpasture’s syndrome). Approximately 40% to 60% of patients with anti-GBM disease have pulmonary hemorrhage 5. Other factors such as pulmonary alveolar capillary damage by cigarette smoke or other hydrocarbon exposure might predispose patients to lung involvement 6. Cigarette smoke likely predisposes to lung involvement via oxidant-induced neutralization of alveolar alpha 1-antiproteinase and resultant greater susceptibility to capillary injury by unopposed proteinases released by activated leukocytes 7.
- Type II, as glomerular deposition of immune complex or immune complex mediated crescentic glomerulonephritis (lupus nephritis and immunoglobulin A [IgA] nephropathy) [granular glomerular staining on immunofluorescence].
- Type III, as pauci-immune deposition (little or no staining for immunoglobulins or complement). Pauci-immune crescentic glomerulonephritis is one of the most common causes of rapidly progressive glomerulonephritis. The characteristic feature of pauci-immune crescentic glomerulonephritis is focal necrotizing and crescentic glomerulonephritis with little or no glomerular staining for Ig by immunofluorescence microscopy examination. The majority of patients with pauci-immune crescentic glomerulonephritis have glomerular diseases as a part of a systemic small vessel vasculitis, including Wegener’s granulomatosis, microscopic polyangiitis, and Churg-Strauss syndrome, or as a part of renal-limited vasculitis 8. In approximately 80% of patients, pauci-immune crescentic glomerulonephritis is associated with ANCA and thus can be called ANCA-associated crescentic glomerulonephritis 9. Approximately three-fourths of patients with pauci-immune or ANCA-associated crescentic glomerulonephritis have systemic small-vessel vasculitis 9. The pauci-immune glomerulonephritis in patients with no evidence for systemic vasculitis sometimes is called “renal-limited vasculitis” because it is pathologically identical to the glomerulonephritis in patients with concurrent vasculitis elsewhere. The three clinicopathologic categories of ANCA-associated, systemic, small-vessel vasculitis are microscopic polyangiitis, Wegener’s granulomatosis, and Churg-Strauss syndrome 10. Drugs known to be associated with the development of pauci-immune crescentic glomerulonephritis include propylthiouracil, benzylthiouracil, methimazole, d-penicillamine, minocycline, ciprofloxacin, and hydralazine 11. While most of the reported cases of drug-induced pauci-immune crescentic glomerulonephritis have a circulating ANCA, antibody positivity has not been observed for minocycline and d-penicillamine associated crescentic glomerulonephritis 12.
- Type IV combination of anti-GBM (type 1) & pauci-immune (type III) 13.
Crescentic glomerulonephritis is one of the leading causes for acute or rapidly progressive renal failure. The incidence of crescentic glomerulonephritis varies with geographic location and policies of kidney biopsies from 2-10% in different studies 14. There is regional and temporal variation in aetiology, prevalence and prognosis of diffuse crescentic glomerulonephritis across the world 15.
The prognosis in crescentic glomerulonephritis is dependent on the age, aetiology, extent of the renal failure and the histological subtype 16. A strong predictor of outcome for all types of crescentic glomerulonephritis is the severity of renal insufficiency at the time of presentation 16. The other unfavorable predictors are elderly patients, presence of oliguria, requirement of haemodialysis, very late presentation, >75% circumferential crescents, Fibrous crescents and interstitial fibrosis tubular atrophy in histopathology 17.
Crescentic glomerulonephritis must be diagnosed promptly and precisely so that appropriate treatment can be initiated as quickly as possible. The best predictor of outcome for all types of crescentic glomerulonephritis is the severity of renal failure at the time therapy begins 16. Even several days’ delay in diagnosis and treatment can have a major negative impact on outcome because of the rapidly progressing loss of renal function that typically accompanies crescentic glomerulonephritis.
In a patient with rapidly progressive glomerulonephritis, statistically the most likely diagnosis is ANCA-associated pauci-immune crescentic glomerulonephritis unless the patient is a child 16. In children, immune-complex crescentic glomerulonephritis is most common because of the combined effect of less-frequent ANCA disease and a higher frequency of most types of immune-complex glomerulonephritis, including acute post-streptococcal glomerulonephritis, Henoch-Schönlein purpura nephritis, IgA nephropathy, membranoproliferative glomerulonephritis, and lupus nephritis. ANCA glomerulonephritis is by far the most common cause of rapidly progressive glomerulonephritis in adults, especially older adults. Approximately 80% of crescentic glomerulonephritis in patients over 60 years of age is pauci-immune disease, which is associated with ANCA approximately 80% of the time. Anti-GBM disease is uncommon at any age.
Anti-GBM glomerulonephritis is the most aggressive form of glomerulonephritis, with the highest frequency of renal insufficiency and the highest frequency of crescent formation at the time of diagnosis. More than 95% of patients with anti-GBM glomerulonephritis have crescents at the time of biopsy, and approximately 85% have 50% or more of glomeruli with crescents. ANCA glomerulonephritis is a close second; approximately 90% of patients have crescents, and approximately 50% have 50% or more of glomeruli with crescents. In contrast, all types of immune-complex glomerulonephritis have a much lower frequency of crescent formation and, when crescents are present, they rarely affect 50% or more of glomeruli.
The best laboratory predictors of pauci-immune crescentic glomerulonephritis and anti-GBM crescentic glomerulonephritis are serologic detection of ANCA or anti-GBM antibodies, respectively 9. The best laboratory predictors of immune-complex crescentic glomerulonephritis are various serologic markers for different types of immune-complex disease, for example, hypocomplementemia, antinuclear antibodies, cryoglobulins, or antibodies indicative of a potentially nephritogenic infection.
The standard treatment for anti-GBM glomerulonephritis, ANCA glomerulonephritis, and severe crescentic immune complex glomerulonephritis (for example, crescentic lupus nephritis) is high-dose corticosteroids and cytotoxic immunosuppressive drugs 18. Plasmapheresis is added for anti-GBM glomerulonephritis and for ANCA glomerulonephritis that is accompanied by pulmonary hemorrhage. Levy et al 19 found that the 1-year patient and renal survival rates for anti-GBM glomerulonephritis are 100% and 95%, respectively, if immunosuppression and plasma exchange are begun when the serum creatinine is less than 5.7 mg/dL. If the serum creatinine is 5.7 mg/dL or higher, the 1-year patient and renal survival rates are 83% and 82%, respectively, if dialysis is not necessary initially, but only 65% and 8%, respectively, if dialysis is required.
Optimal treatment for pauci-immune ANCA-associated crescentic glomerulonephritis is different than that for anti-GBM disease. In this case, plasmapheresis has not shown to add any advantage to a combination of cytotoxic and steroid therapies unless the patient also has hemoptysis or anti-GBM antibody present. Initial steroid dosing should be more aggressive in the form of pulse intravenous high doses, such as methylprednisolone, 1000 mg daily for 3 consecutive days, followed by oral prednisone at a dosage of 1 mg/kg daily. Cytotoxic therapy should accompany this steroid therapy, typically either 2 mg/kg of oral cyclophosphamide daily, or monthly intravenous pulse cyclophosphamide. Typical duration of therapy is 6 to 12 months, depending on how quickly the patient has entered remission. Patients who need dialysis should still be treated unless contraindicated, because the chance for renal recovery is higher than with anti-GBM disease, although adjusting down the dose of cyclophosphamide is necessary.
Post streptococcal glomerulonephritis
The epidemiology of acute post-streptococcal glomerulonephritis has changed substantially over the past 50 years. Before the 1980s acute post-streptococcal glomerulonephritis was relatively common worldwide with multiple large and recurrent epidemics reported, especially in the Native Americans in the United States and in Central and South America 20. Many of these epidemics were thought to be related to streptococcal skin rather than throat infection, often associated with preceding scabies 21. Over the past 20 years there has been a substantial decline in the reported incidence of acute post-streptococcal glomerulonephritis in many industrialized countries 22.
Despite this declining incidence of acute post-streptococcal glomerulonephritis in many developed countries, there is still a significant global burden of disease. It has been estimated that there are more than 470,000 cases of acute post-streptococcal glomerulonephritis worldwide annually with ~5,000 deaths, with 97% occurring in less developed countries 23. It is likely that acute post-streptococcal glomerulonephritis is underreported in many developing countries and these figures are likely to be an underestimate of the true burden of this condition.
The majority of these cases are related to pyoderma caused by infection with Streptococcus pyogenes (Group A Streptococcus [GAS]), often with underlying scabies 24. It has long been recognized that certain Group A Streptococcus M protein types, as now determined by the emm genotype (emm sequence type), are associated with nephritis and these are mostly different from the emm types that cause acute rheumatic fever 25. Although acute post-streptococcal glomerulonephritis has classically been associated with infection with Group A Streptococcus, it has occasionally been reported to occur after infection with other streptococcal species 26. Lancefield group C and G streptococci (GCS/GGS) have been associated with acute post-streptococcal glomerulonephritis, in particular Streptococcus zooepidemicus, which has been responsible for a number of acute post-streptococcal glomerulonephritis outbreaks associated with unpasteurized milk 27.
The short term prognosis for children with acute post-streptococcal glomerulonephritis is generally good with a mortality of < 0.5% and fewer than 2% progressing to end-stage renal failure 28. The long-term implications of acute post-streptococcal glomerulonephritis are less clear with studies reporting mixed outcomes 29. Although many studies have reported favorable outcomes, some are less reassuring, especially in the Indigenous Australian population. A recent study has found significantly higher rates of albuminuria in Indigenous Australians with previous acute post-streptococcal glomerulonephritis compared with controls 30. Given albuminuria is a marker of early chronic kidney disease, this suggests that acute post-streptococcal glomerulonephritis may be contributing to the extremely high rates of chronic renal failure seen in Indigenous Australian adults 31.
Post streptococcal glomerulonephritis causes
Poststreptococcal glomerulonephritis is a form of glomerulonephritis. It is caused by an infection with a type of streptococcus bacteria. The infection does not occur in the kidneys, but in a different part of the body, such as the skin or throat.
The strep bacterial infection causes the tiny blood vessels in the filtering units of the kidneys (glomeruli) to become inflamed. This makes the kidneys less able to filter the urine.
Poststreptococcal glomerulonephritis is uncommon today because infections that can lead to the disorder are commonly treated with antibiotics. The disorder may develop 1 to 2 weeks after an untreated throat infection, or 3 to 4 weeks after a skin infection.
It may occur in people of any age, but it most often occurs in children ages 6 through 10. Although skin and throat infections are common in children, poststreptococcal glomerulonephritis is a rare complication of these infections.
Risk factors include:
- Strep throat
- Streptococcal skin infections (such as impetigo)
Post streptococcal glomerulonephritis possible complications
Health problems that may result from this disorder include:
- Acute renal failure (rapid loss of kidneys’ ability to remove waste and help balance fluids and electrolytes in the body)
- Chronic glomerulonephritis
- Chronic kidney disease
- Heart failure or pulmonary edema (fluid buildup in the lungs)
- End-stage renal disease
- Hyperkalemia (abnormally high potassium level in the blood)
- High blood pressure (hypertension)
- Nephrotic syndrome (group of symptoms that include protein in the urine, low blood protein levels in the blood, high cholesterol levels, high triglyceride levels, and swelling)
Post streptococcal glomerulonephritis symptoms
Symptoms may include any of the following:
- Decreased urine output
- Rust-colored urine
- Swelling (edema), general swelling, swelling of the abdomen, swelling of the face or eyes, swelling of the feet, ankles, hands
- Visible blood in the urine
- Joint pain
- Joint stiffness or swelling
Post streptococcal glomerulonephritis diagnosis
A physical examination shows swelling (edema), especially in the face. Abnormal sounds may be heard when listening to the heart and lungs with a stethoscope. Blood pressure is often high.
Other tests that may be done include:
- Anti-DNase B
- Serum ASO (and streptolysin O)
- Serum complement levels
- Urinalysis
- Kidney biopsy (usually not needed)
Post streptococcal glomerulonephritis treatment
There is no specific treatment for this disorder. Treatment is focused on relieving symptoms.
- Antibiotics, such as penicillin, will likely be used to destroy any streptococcal bacteria that remain in the body.
- Blood pressure medicines and diuretic drugs may be needed to control swelling and high blood pressure.
- Corticosteroids and other anti-inflammatory medicines are generally not effective.
You may need to limit salt in the diet to control swelling and high blood pressure.
Patients with acute post-streptococcal glomerulonephritis should be treated as though they have active streptococcal infection. The reason for this recommendation is that positive cultures may sometimes be obtained from patients in whom upper respiratory or skin infections are not clinically evident. Treatment of a carrier state may prevent spread to other household members; in addition, at least one report suggested that patients who receive post-streptococcal glomerulonephritis antibiotic treatment have a milder clinical course 32.
Prophylactic penicillin treatment should be used in epidemics in closed communities and prescribed to household contacts of index cases in areas where post-streptococcal glomerulonephritis is very common or when clusters of cases are reported. This recommendation is based on the finding that cross-infection among family members of index cases in communities where post-streptococcal glomerulonephritis is prevalent is very high.
Membranous glomerulonephritis
Membranous nephropathy occurs when the small blood vessels in the kidney (glomeruli), which filter wastes from the blood, become damaged and thickened. As a result, proteins leak from the damaged blood vessels into the urine (proteinuria). For many, loss of these proteins eventually causes signs and symptoms known as nephrotic syndrome. Membranous glomerulonephritis is a slowly progressive disease of the kidney affecting mostly patients between ages of 30 and 50 years, usually Caucasian men in older than 40. It is the second most common cause of nephrotic syndrome in adults (33% of cases), with focal segmental glomerulosclerosis being the most common 33.
Membranous glomerulonephritis is a kidney disorder defined by characteristic microscopic and immunofluorescence findings. On light microscopy, there is diffuse thickening of glomerular capillary walls without associated hypercellularity. On immunofluorescence, there is diffuse granular staining of the glomerular capillary loops: typically, for IgG more than IgA or IgM, as well as C3. On electron microscopy, the pathologic hallmark confirming membranous glomerulonephritis is electron-dense deposits in the subepithelial region of the glomerular basement membrane. These deposits correspond to the immunoglobulins seen on immunofluorescence. Occasionally, these deposits are large enough that they can be seen with special stains on light microscopy directly, or may induce adjacent changes of glomerular basement membrane material, leading to a spike appearance on either side of the deposit.
In mild cases, membranous nephropathy may get better on its own, without any treatment. As protein leakage increases, so does the risk of long-term kidney damage. In many, the disease ultimately leads to kidney failure. There’s no absolute cure for membranous nephropathy, but successful treatment can lead to remission of proteinuria and a good long-term outlook.
Membranous nephropathy causes
Often, membranous nephropathy results from some type of autoimmune activity. Your body’s immune system mistakes healthy tissue as foreign and attacks it with substances called autoantibodies. These autoantibodies target certain proteins located in the kidney’s filtering systems (glomeruli). This is known as primary membranous nephropathy.
The cause of immunoglobulin deposition in the subepithelial location of the glomerular basement membranes in membranous glomerulonephritis and its subsequent damage and altered structure, function, or both, are not completely known.
Sometimes membranous nephropathy is brought on by other causes. When this happens, it’s called secondary membranous nephropathy. Causes may include:
- Autoimmune disease, such as lupus erythematosus (SLE)
- Infection with hepatitis B, hepatitis C or syphilis
- Certain medications, such as gold salts and nonsteroidal anti-inflammatory drugs
- Solid cancerous tumors or blood cancers
Membranous nephropathy may also occur along with other kidney diseases, such as diabetic nephropathy and rapidly progressive (crescentic) glomerulonephritis.
Risk factors for membranous nephropathy
Factors that can increase your risk of membranous nephropathy include:
- Having a medical condition that can damage your kidneys. Certain diseases and conditions increase your risk of developing membranous nephropathy, such as lupus and other autoimmune diseases.
- Use of certain medications. Examples of medications that can cause membranous nephropathy include nonsteroidal anti-inflammatory drugs and gold salts.
- Exposure to certain infections. Examples of infections that increase the risk of membranous nephropathy include hepatitis B, hepatitis C and syphilis.
- Genetic background. Certain genetic factors make it more likely that you’ll develop membranous nephropathy.
Membranous nephropathy complications
Complications associated with membranous nephropathy include:
- High cholesterol. Levels of cholesterol and triglycerides are often high in people with membranous nephropathy, which greatly increases the risk of heart disease.
- Blood clots. With proteinuria, you may lose proteins that help prevent clotting from your blood into your urine. This makes you more prone to having blood clots develop in deep veins or blood clots that travel to your lungs.
- High blood pressure. Waste buildup in your blood (uremia) and salt retention can raise blood pressure.
- Infections. You’re more susceptible to infections when proteinuria causes you to lose immune system proteins (antibodies) that protect you from infection.
- Nephrotic syndrome. High protein levels in the urine, low protein levels in the blood, high blood cholesterol, and swelling (edema) of the eyelids, feet and abdomen occur with this syndrome.
- Acute kidney failure. In cases of severe damage to the kidneys’ filtering units (glomeruli), waste products may build up quickly in your blood. You may need emergency dialysis to remove extra fluids and waste from your blood.
- Chronic kidney disease. Your kidneys may gradually lose function over time to the point where you need dialysis or a kidney transplant.
Membranous nephropathy prognosis
The prognosis of membranous glomerulonephritis is diverse and varied, based on pertinent clinical factors at presentation and the occurrence of remission, whether it is spontaneous or induced by specific immunotherapy. In general, those patients free of remission typically have a slow progressive loss of renal function, leading to end stage kidney disease. A pertinent caveat of membranous glomerulonephritis is the higher degree of hypercoagulability with the nephrotic syndrome compared with other primary glomerular disorders. Although any venous thrombosis event appears to be more likely in patients with membranous glomerulonephritis compared with other primary glomerular diseases, a significant consideration that may significantly affect renal and patient survival is the development of renal vein thrombosis, which may occur in approximately 15% of cases.
Membranous nephropathy symptoms
Membranous nephropathy may develop gradually, so you may not suspect that anything is wrong. As you lose protein from your blood, swelling in your legs and ankles and weight gain from excess fluid can occur. Many people have lots of swelling from the very beginning of the disease, but others may not have any severe symptoms until they have advanced kidney disease.
Signs and symptoms of membranous nephropathy include:
- Swelling in the legs and ankles
- Weight gain
- Fatigue
- Poor appetite
- Urine that looks foamy
- High cholesterol
- Increased protein in the urine (proteinuria)
- Decreased protein in the blood, particularly albumin
Membranous nephropathy diagnosis
Membranous nephropathy may not cause any signs or symptoms. Sometimes, it’s diagnosed when a routine urine test — performed for another health reason — shows that you have high levels of protein in your urine (proteinuria).
If you do have signs or symptoms of protein in the urine, your doctor will ask questions about your medical history and perform a complete physical exam. Your blood pressure will be checked.
Blood, urine and imaging tests can tell your doctor how well your kidneys are working and diagnose membranous nephropathy. They can also help rule out other possible causes of your symptoms.
Tests that may be done include:
- A urine test (urinalysis). You may be asked to provide a urine sample so your doctor can measure how much protein is in your urine.
- Blood tests. A blood sample allows your doctor to check for high cholesterol, high triglycerides, high blood sugar and other factors that can affect the kidneys. A creatinine blood test gives information about your kidney function. Other blood tests can be done to check for autoimmune diseases or viral infections that can cause kidney damage, such as hepatitis B or C.
- Glomerular filtration rate (GFR) test. The GFR test estimates your level of kidney function and can help your doctor determine your stage of kidney disease.
- Antinuclear antibody (ANA) test. This blood tests looks for antinuclear antibodies, substances that attack your body’s own tissues. High levels of antinuclear antibodies are a sign of an autoimmune disease.
- Kidney ultrasound or computed tomography (CT). Imaging scans allow your doctor to see the structure of your kidneys and urinary tract.
- Kidney biopsy. A doctor removes a small piece of your kidney to be examined under a microscope. A kidney biopsy is usually needed to confirm the diagnosis. It can tell your doctor the type of kidney disease you have, the amount of kidney damage and what treatments may work best.
- Anti-PLA2R antibody test. This new blood test looks for certain immune substances related to membranous nephropathy. It may help confirm or rule out the disease when a biopsy cannot be done. High levels of these antibodies are a sign of active disease. They’ve been linked to an increased risk of worsening kidney function.
Membranous nephropathy treatment
Treatment of membranous nephropathy focuses on addressing the cause of your disease and relieving your symptoms. There is no certain cure.
However, up to three out of 10 people with membranous nephropathy have their symptoms completely disappear (remission) after five years without any treatment. About 25 to 40 percent have a partial remission.
In cases where membranous nephropathy is caused by a medication or another disease — such as cancer — stopping the medication or controlling the other disease usually improves the condition.
Low risk of advanced kidney disease
With membranous nephropathy, you’re considered at low risk of developing advanced kidney disease in the next five years if:
- Your urine protein level remains less than 4 grams a day for six months
- Your blood creatinine level remains in the normal range for six months
If you’re at low risk of advanced kidney disease, treatment of membranous nephropathy usually begins by taking the following steps:
- Take blood pressure medication. Doctors typically prescribe an angiotensin-converting enzyme (ACE) inhibitor or an angiotensin II receptor blocker (ARB) to keep your blood pressure under control.
- Decrease swelling (edema). Water pills (diuretics) help remove sodium and water from your blood.
- Control cholesterol. Medications called statins are used to keep your cholesterol in check.
- Lower your risk for blood clots. People with membranous nephropathy are more likely to have deep vein thrombosis or pulmonary embolism. Doctors may prescribe blood-thinners, or anticoagulants, to prevent these dangerous events.
- Cut back on salt. Salt can increase urine protein levels. It also makes your body retain fluid. Check the salt content in foods, drinks and condiments.
Doctors generally prefer to avoid using strong drugs (which can cause significant side effects) early in the course of the disease, when there’s a chance that the disease will improve on its own.
Moderate to high risk of advanced kidney disease
Your doctor may recommend more-intensive treatment as the amount of protein in your urine increases. The more protein you have in your urine (proteinuria), the greater the risk to your kidneys and well-being.
In the past, doctors have assessed risk based on the amount of protein in the urine over time:
- Moderate risk. Urine protein level stays between 4 and 8 grams a day and blood creatinine level is at normal or near normal for six months of observation. About half the people with these signs develop serious kidney disease over five years.
- High risk. Urine protein level is persistently greater than 8 grams a day for three months or kidney function is below normal or falls below normal during the observation period. About 3 out of 4 people with these signs are highly likely to develop serious kidney disease over 10 years.
A new approach for assessing risk allows doctors to evaluate antibody levels in the blood along with how much protein is in the urine. This approach also helps doctors determine how you’ll respond to therapy.
If you have a moderate to high risk of advanced kidney disease, your doctor may talk to you about these treatments for membranous nephropathy:
- Steroids plus a chemotherapy drug. If your urine protein level keeps rising, your doctor may prescribe a corticosteroid medication with a chemotherapy drug to suppress your immune system. This can lower your urine protein levels and stop the progress toward kidney failure. However, immune suppressing medications don’t help everyone. They can also have significant side effects. Some of the side effects of chemotherapy drugs — such as risk of cancer or infertility — may occur many years after taking the drug.
- Cyclosporine. If you don’t want to take a chemotherapy drug or cannot tolerate it, cyclosporine (a calcineurin inhibitor drug) is an option.
- Rituximab (Rituxan). Rituximab has helped some people who have not improved with immunosuppressive therapy. Studies suggest it works at least as well as steroid therapy. The medication kills B cells in the immune system — the cells that produce substances, called antibodies, that damage the glomeruli. However, it’s expensive and not generally covered by insurance.
Sometimes, the disease comes back after treatment ends. This has happened to people taking any kind of immune suppressants. In some cases, if the first round of treatment doesn’t work or you have a relapse, you may benefit from a second round. Talk to your doctor about the best treatment plan for you.
Home remedies
Talk to your doctor about how to reduce your chances of developing kidney disease. Your doctor may suggest that you:
- Have regular checkups
- Follow your prescribed treatment for diabetes or high blood pressure
- Lose excess weight by following a healthy diet and regular exercise program
- Stop smoking, if you are a smoker
- Limit use of over-the-counter pain medications
- Make changes in your diet, such as eating less salt and less protein
- Limit your intake of alcohol.
Glomerulonephritis complications
Although treatment for glomerulonephritis is effective in many cases, further problems can sometimes develop.
These include:
- High blood pressure. Damage to your kidneys and the resulting buildup of wastes in the bloodstream can raise your blood pressure.
- High cholesterol
- Blood clots – including deep vein thrombosis (DVT) or a pulmonary embolism
- Damage to other organs
- Acute kidney failure. Loss of function in the filtering part of the nephron can result in rapid accumulation of waste products. You might need emergency dialysis — an artificial means of removing extra fluids and waste from your blood — typically by an artificial kidney machine.
- Chronic kidney disease. Your kidneys gradually lose their filtering ability. Kidney function that deteriorates to less than 10 percent of normal capacity results in end-stage kidney disease, which requires dialysis or a kidney transplant to sustain life.
- Nephrotic syndrome. With this syndrome, too much protein in your urine results in too little protein in your blood. Nephrotic syndrome can be associated with high blood cholesterol and swelling (edema) of the eyelids, feet and abdomen.
If you’re diagnosed with glomerulonephritis, your doctor may prescribe medication to help lower your blood pressure, lower your cholesterol or protect against blood clots.
Glomerulonephritis causes
Many conditions can cause glomerulonephritis. Sometimes the disease runs in families and sometimes the cause is unknown. Conditions that can lead to inflammation of the kidneys’ glomeruli include:
Infections
- Post-streptococcal glomerulonephritis. Glomerulonephritis may develop a week or two after recovery from a strep throat infection or, rarely, a skin infection (impetigo). To fight the infection, your body produces extra antibodies that can eventually settle in the glomeruli, causing inflammation. Children are more likely to develop post-streptococcal glomerulonephritis than are adults, and they’re also more likely to recover quickly.
- Bacterial endocarditis. Bacteria occasionally can spread through your bloodstream and lodge in your heart, causing an infection of one or more of your heart valves. You’re at greater risk of this condition if you have a heart defect, such as a damaged or artificial heart valve. Bacterial endocarditis is associated with glomerular disease, but the connection between the two is unclear.
- Viral infections. Viral infections, such as the human immunodeficiency virus (HIV), hepatitis B and hepatitis C, can trigger glomerulonephritis.
Immune diseases
- Systemic lupus erythematosus (SLE). A chronic inflammatory disease, lupus can affect many parts of your body, including your skin, joints, kidneys, blood cells, heart and lungs.
- Goodpasture’s syndrome. A rare immunological lung disorder that can mimic pneumonia, Goodpasture’s syndrome causes bleeding in your lungs as well as glomerulonephritis.
- IgA nephropathy. Characterized by recurrent episodes of blood in the urine, this primary glomerular disease results from deposits of immunoglobulin A (IgA) in the glomeruli. IgA nephropathy can progress for years with no noticeable symptoms.
- Minimal change glomerulopathy
In some cases, the immune system abnormalities are triggered by an infection, such as:
- HIV
- Hepatitis B and hepatitis C – viral infections of the liver
- Infection of the heart valves (endocarditis)
Vasculitis
- Polyarteritis. This form of vasculitis affects small and medium blood vessels in many parts of your body, such as your heart, kidneys and intestines.
- Granulomatosis with polyangiitis. This form of vasculitis, formerly known as Wegener’s granulomatosis, affects small and medium blood vessels in your lungs, upper airways and kidneys.
In most cases, glomerulonephritis doesn’t run in families. If you’re diagnosed with an inherited type of glomerulonephritis, your doctor can advise you about the chances of someone else in your family being affected. They may recommend screening, which can identify people who may be at increased risk of developing the condition.
Conditions likely to cause scarring of the glomeruli
- High blood pressure. This can damage your kidneys and impair their ability to function normally. Glomerulonephritis can also lead to high blood pressure because it reduces kidney function and can influence how your kidneys handle sodium.
- Diabetic kidney disease (diabetic nephropathy). This can affect anyone with diabetes, usually taking years to develop. Good control of blood sugar levels and blood pressure might prevent or slow kidney damage.
- Focal segmental glomerulosclerosis. Characterized by scattered scarring of some of the glomeruli, this condition can result from another disease or occur for no known reason.
Infrequently, chronic glomerulonephritis runs in families. One inherited form, Alport syndrome, also might impair hearing or vision.
In addition to the causes listed above, glomerulonephritis is associated with certain cancers, such as multiple myeloma, lung cancer and chronic lymphocytic leukemia.
Glomerulonephritis prevention
There may be no way to prevent most forms of glomerulonephritis. However, here are some steps that might be beneficial:
- Seek prompt treatment of a strep infection with a sore throat or impetigo.
- To prevent infections that can lead to some forms of glomerulonephritis, such as HIV and hepatitis, follow safe-sex guidelines and avoid intravenous drug use.
- Control high blood pressure, which lessens the likelihood of damage to your kidneys from hypertension.
- Control your blood sugar to help prevent diabetic nephropathy.
If you have the chronic type of glomerulonephritis, it is very important to control your blood pressure since this may slow down kidney damage. Your doctor may tell you to eat less protein. A dietitian trained to work with kidney patients (a renal dietitian) can be very helpful in planning your diet.
Glomerulonephritis symptoms
Signs and symptoms of glomerulonephritis depend on whether you have the acute or chronic form and the cause. Your first indication that something is wrong might come from symptoms or from the results of a routine urinalysis.
In severe cases of glomerulonephritis, you may see blood in your urine. However, this is usually noticed when a urine sample is tested.
Your urine may be frothy if it contains a large amount of protein.
If a lot of protein leaks into your urine, swelling of the legs or other parts of the body (edema) can also develop. This is known as nephrotic syndrome.
Depending on your type of glomerulonephritis, other parts of your body can be affected and cause symptoms such as:
- rashes
- joint pain
- breathing problems
- tiredness
Many people with glomerulonephritis also have high blood pressure.
Glomerulonephritis diagnosis
Glomerulonephritis often comes to light when a routine urinalysis is abnormal.
If your doctor suspects glomerulonephritis, they’ll usually arrange:
- Blood test – This test can provide information about kidney damage and impairment of the glomeruli by measuring levels of waste products, such as creatinine and blood urea nitrogen. Blood test to measure your creatinine level; if your kidneys aren’t working normally, the creatinine level in your blood rises and estimated glomerular filtration rate (eGDR) falls
- Urine test – to check for blood or protein in your urine, either by dipping special strips into a sample of your urine or sending the sample to a laboratory for further testing. A urinalysis might show red blood cells and red cell casts in your urine, an indicator of possible damage to the glomeruli. Urinalysis results might also show white blood cells, a common indicator of infection or inflammation, and increased protein, which can indicate nephron damage. Other indicators, such as increased blood levels of creatinine or urea, are red flags.
If glomerulonephritis is confirmed, further blood tests may be needed to help determine the cause.
If your kidney problem needs to be investigated further, it may be recommended that you have:
- an ultrasound scan – this is to check the size of your kidneys, make sure there are no blockages, and look for any other problems
- a biopsy – this is to remove a small sample of kidney tissue, carried out using local anesthetic to numb the area; an ultrasound machine locates your kidneys and a small needle is used to take a sample. A kidney biopsy is almost always necessary to confirm a diagnosis of glomerulonephritis.
Glomerulonephritis treatment
Treatment of glomerulonephritis and your outcome depend on:
- Whether you have an acute or chronic form of the disease
- The underlying cause
- The type and severity of your signs and symptoms
In mild cases, treatment isn’t always necessary. If treatment is needed, it’s usually carried out by a kidney specialist.
Some cases of acute glomerulonephritis, especially those that follow a Strep infection, might improve on their own and require no treatment. If there’s an underlying cause, such as high blood pressure, an infection or an autoimmune disease, treatment will be directed to the underlying cause.
In general, the goal of treatment is to protect your kidneys from further damage.
Dietary and lifestyle changes
Simple lifestyle changes can often help reduce high blood pressure (hypertension), although some people may need to take medication as well.
In mild cases, your doctor or dietitian will give you relevant advice about diet.
You may be advised to REDUCE your intake of:
- foods that contain a high amount of salt
- cutting your salt intake to less than 1.5 g (1500 mg) a day (that’s about half a teaspoon of salt)
- foods or drinks that contain a high amount of potassium
- eating a low-fat, balanced diet – including plenty of fresh fruit and vegetables
- being active – getting more exercise
- fluid
- cutting down on alcohol
- losing weight – if you’re overweight
- drinking less caffeine – found in coffee, tea and cola
- stopping smoking
- getting at least six hours of sleep a night if you can
This should help control your blood pressure and ensure the amount of fluid in your body is regulated.
You should have a regular review to ensure your blood contains the right levels of potassium, sodium chloride and other salts.
Coping and support
Living with a chronic illness can tax your emotional resources. If you have chronic glomerulonephritis or chronic kidney failure, you might benefit from joining a support group. A support group can provide both sympathetic listening and useful information.
To find a support group, ask your doctor for a recommendation or contact the National Kidney Foundation (https://www.kidney.org/) to find the chapter nearest you.
Stopping smoking
Smoking may make kidney disease caused by glomerulonephritis worse more quickly.
It also increases the risk of complications like heart disease and stroke, which are already more common in people with glomerulonephritis.
Immunosuppressants
Severe cases of glomerulonephritis, caused by problems with the immune system, are sometimes treated with types of medicine known as immunosuppressants. These medicines suppress your immune system.
Suppressing your immune system can be effective, but it also increases your risk of infections and can cause other side effects.
If you’re offered treatment with immunosuppressant medicines, they’ll be adjusted to the level needed to treat your condition and will be carefully monitored.
Corticosteroids
You may be put on a course of medicines containing steroids (corticosteroids), such as Prednisolone.
Corticosteroids are used to reduce swelling and suppress your immune system.
Once your kidneys have started to recover, your dose of corticosteroid medicine will usually be lowered. You may continue to take a small dose, or this treatment may be stopped altogether.
Cyclophosphamide
Cyclophosphamide is an immunosuppressant used in very high doses to treat some cancers. It’s also an established treatment, in much lower doses, for glomerulonephritis.
Other immunosuppressants
Other medicines to help control your immune system include:
- mycophenolate mofetil
- azathioprine
- rituximab
- ciclosporin
- tacrolimus
Other medicines
If your condition is thought to be linked to a viral infection, it may be treated with antiviral medication.
Individual symptoms can sometimes be treated. For example, swelling caused by a build-up of fluid may be treated with a type of medication called a diuretic.
Treating high blood pressure
Glomerulonephritis often leads to high blood pressure, which can cause further kidney damage and other health problems.
Your blood pressure will be carefully monitored by the healthcare professionals treating you.
You may need to take medicines that lower blood pressure and help reduce the amount of protein that leaks into your urine, such as:
- Angiotensin-converting enzyme (ACE) inhibitors. Angiotensin-converting enzyme (ACE) inhibitors reduce blood pressure by relaxing your blood vessels. Common examples are enalapril, lisinopril, perindopril and ramipril. The most common side effect is a persistent dry cough. Other possible side effects include headaches, dizziness and a rash.
- Angiotensin 2 receptor blockers (ARBs). Angiotensin 2 receptor blockers (ARBs) work in a similar way to ACE inhibitors. They’re often recommended if ACE inhibitors cause troublesome side effects. Common examples are candesartan, irbesartan, losartan, valsartan and olmesartan. Possible side effects include dizziness, headaches, and cold or flu-like symptoms.
- Calcium channel blockers. Calcium channel blockers reduce blood pressure by widening your blood vessels. Common examples are amlodipine, felodipine and nifedipine. Other medicines such as diltiazem and verapamil are also available. Possible side effects include headaches, swollen ankles and constipation. Drinking grapefruit juice while taking some calcium channel blockers can increase your risk of side effects.
- Diuretics. Sometimes known as water pills, diuretics work by flushing excess water and salt from the body through urine. They’re often used if calcium channel blockers cause troublesome side effects. Common examples are indapamide and bendroflumethiazide. Possible side effects include dizziness when standing up, increased thirst, needing to go to the toilet frequently, and a rash. Low potassium level (hypokalaemia) and low sodium level (hyponatraemia) may also be seen after long-term use.
- Beta-blockers. Beta-blockers can reduce blood pressure by making your heart beat more slowly and with less force. They used to be a popular treatment for high blood pressure, but now only tend to be used when other treatments haven’t worked. This is because beta-blockers are considered less effective than other blood pressure medications. Common examples are atenolol and bisoprolol. Possible side effects include dizziness, headaches, tiredness, and cold hands and feet.
The medication recommended for you at first will depend on your age and ethnicity:
- if you’re under 55 years of age – you’ll usually be offered an ACE inhibitor or an angiotensin-2 receptor blocker (ARB)
- if you’re aged 55 or older, or you’re any age and of African or Caribbean origin – you’ll usually be offered a calcium channel blocker
Often, people who have high blood pressure and kidney disease need to take several medicines to control their blood pressure.
These medications are commonly prescribed, even if your blood pressure is not particularly high, as they can help protect the kidneys.
Treating high cholesterol
High cholesterol levels are common in people with glomerulonephritis.
Your doctor may recommend treatment with medication to reduce cholesterol and help protect you against complications such as heart and vascular disease.
There are several different types of cholesterol-lowering medication that work in different ways.
The most commonly prescribed medications are:
Statins
Statins block the enzyme (a type of chemical) in your liver that helps to make cholesterol. This leads to a reduction in your blood cholesterol level.
You’ll usually be started on a medication called atorvastatin. Other statins include simvastatin and rosuvastatin.
When someone has side effects from using a statin, it’s described as having an “intolerance” to it. Side effects of statins include headaches, muscle pain and stomach problems, such as indigestion, diarrhoea or constipation.
Statins will only be prescribed to people who continue to be at high risk of heart disease, because they need to be taken for life. Cholesterol levels start to rise again once you stop taking them.
Aspirin
In some cases, a low daily dose of aspirin may be prescribed, depending on your age (usually over 40 years old) and other risk factors.
Low-dose aspirin can help to prevent blood clots forming, particularly for someone who’s had a heart attack, has established vascular disease, or a high risk of developing cardiovascular disease (CVD).
You may also be advised to have periodic blood tests to ensure your liver is functioning well.
Ezetimibe
Ezetimibe is a medication that blocks the absorption of cholesterol from food and bile juices in your intestines into your blood. It’s generally not as effective as statins, but is less likely to cause side effects.
You can take ezetimibe at the same time as your usual statin if your cholesterol levels aren’t low enough with the statin alone. The side effects of this combination are generally the same as those of the statin on its own (muscle pain and stomach problems).
You can take ezetimibe by itself if you’re unable to take a statin. This may be because you have another medical condition, you take medication that interferes with how the statin works, or because you experience side effects from statins. Ezetimibe taken on its own rarely causes side effects.
Plasma exchange
Plasma is a fluid that is part of the blood. It contains proteins, such as antibodies that can cause your kidneys to become inflamed.
Plasma exchange involves removing some of the plasma from your blood.
During the procedure, you’re connected to a machine that gradually removes some of your blood.
The plasma is separated from the blood cells and removed. A plasma substitute is then added to the blood before it’s put back into your body.
Plasma exchange may be used in certain circumstances if your condition is particularly severe – usually if you have a type of glomerulonephritis called ANCA vasculitis or anti-glomerular basement membrane disease.
Therapies for associated kidney failure
For acute glomerulonephritis and acute kidney failure, dialysis can help remove excess fluid and control high blood pressure. The only long-term therapies for end-stage kidney disease are kidney dialysis and kidney transplant. When a transplant isn’t possible, often because of poor general health, dialysis is the only option.
Vaccinations
People with glomerulonephritis can be more prone to infections, particularly if:
- you have nephrotic syndrome
- you develop chronic kidney disease
It’s usually a good idea to help protect yourself against infection by having a seasonal flu jab and a pneumonia immunization.
References- http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/nephrology/primary-glomerular-diseases/
- West CD: Childhood membranoproliferative glomerulonephritis: An approach to management. Kidney Int 1986;29:1077–1093.
- Tarshish P, Bernstein J, Tobin JN, et al: Treatment of mesangiocapillary glomerulonephritis with alternate-day prednisone: A report of the International Study of Kidney Disease in Children. Pediatr Nephrol 1992;6:123–130.
- Nagaraju SP, Laxminarayana SLK, Kosuru S, et al. Clinicopathological Characteristics and Outcomes of Diffuse Crescentic Glomerulonephritis – A Single Center Experience from Southern India. Journal of Clinical and Diagnostic Research : JCDR. 2017;11(9):OC21-OC24. doi:10.7860/JCDR/2017/28307.10621. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5713776/
- Savage, C.O., Pusey, C.D., Bowman, C. et al. Antiglomerular basement membrane antibody mediated disease in the British Isles 1980–4. Br Med J (Clinical Res Ed). 1986; 292: 301–304
- Bonzel, K.E., Muller-Wiefel, D.E., Ruder, H. et al. Anti-glomerular basement membrane antibody-mediated glomerulonephritis due to glue sniffing. Eur J Pediatr. 1987; 146: 296–300
- Evans, M.D. and Pryor, W.A. Cigarette smoking, emphysema, and damage to alpha 1-proteinase inhibitor. Am J Physiol. 1994; 266: L593–L611
- Falk RJ, Jennette JC: ANCA small-vessel vasculitis. J Am Soc Nephrol 8 : 314 –322, 1997
- Savage, C.O.S. ANCA-associated renal vasculitis. Kidney Int. 2001; 60: 1614–1627
- Jennette, J.C. and Falk, R.J. Small vessel vasculitis. N Engl J Med. 1997; 337: 1512–1523
- Drug-induced glomerular disease: immune-mediated injury. Hogan JJ, Markowitz GS, Radhakrishnan J. Clin J Am Soc Nephrol. 2015 Jul 7; 10(7):1300-10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4491282/
- Evaluation of antineutrophil cytoplasmic antibody seroconversion induced by minocycline, sulfasalazine, or penicillamine. Choi HK, Slot MC, Pan G, Weissbach CA, Niles JL, Merkel PA. Arthritis Rheum. 2000 Nov; 43(11):2488-92. https://www.ncbi.nlm.nih.gov/pubmed/11083272/
- Jennette JC. Rapidly progressive crescentic glomerulonephritis. Kidney Int. 2003;63:1164–77. https://www.ncbi.nlm.nih.gov/pubmed/12631105
- Chen S, Tang Z, Xiang H, Li X, Chen H, Zhang H, et al. Aetiology and outcome of crescentic glomerulonephritis from a single center in China: A 10-year review. American Journal of Kidney Diseases. 2016;67(3):376–83 https://www.ncbi.nlm.nih.gov/pubmed/26388283
- Chen S, Tang Z, Xiang H, Li X, Chen H, Zhang H, et al. Aetiology and outcome of crescentic glomerulonephritis from a single center in China: A 10-year review. American Journal of Kidney Diseases. 2016;67(3):376–83. https://www.ncbi.nlm.nih.gov/pubmed/26388283
- Jennette JC. Rapidly progressive crescentic glomerulonephritis. Kidney Int. 2003;63:1164–77. http://www.kidney-international.theisn.org/article/S0085-2538(15)48992-6/fulltext
- Oudah N, Al Duhailib Z, Alsaad K, Qurashi S, Ghamdi G, Flaiw A, et al. Glomerulonephritis with crescents among adult Saudi patients outcome and its predictors. Clin Exp Med. 2012;12:121–25. https://www.ncbi.nlm.nih.gov/pubmed/21706346
- Couser, W.G. Rapidly progressive glomerulonephritis: classification, pathogenetic mechanisms, and therapy. Am J Kidney Dis. 1988; 11: 449–464
- Levy, J.B., Turner, A.N., Rees, A.J., and Pusey, C.D. Long-term outcome of anti-glomerular basement membrane antibody disease treated with plasma exchange and immunosuppression. Ann Intern Med. 2001; 134: 1033–1042
- Rodriguez-Iturbe B, Musser JM. The current state of poststreptococcal glomerulonephritis. J Am Soc Nephrol. 2008;19:1855–1864
- Berrios X, Lagomarsino E, Solar E, Sandoval G, Guzman B, Riedel I. Post-streptococcal acute glomerulonephritis in Chile–20 years of experience. Pediatr Nephrol. 2004;19:306–312 https://www.ncbi.nlm.nih.gov/pubmed/14689289
- Coppo R, Gianoglio B, Porcellini MG, Maringhini S. Frequency of renal diseases and clinical indications for renal biopsy in children (report of the Italian National Registry of Renal Biopsies in Children). Group of Renal Immunopathology of the Italian Society of Pediatric Nephrology and Group of Renal Immunopathology of the Italian Society of Nephrology. Nephrol Dial Transplant. 1998;13:293–297.
- Carapetis JR, Steer AC, Mulholland EK, Weber M. The global burden of group A streptococcal diseases. Lancet Infect Dis. 2005;5:685–694 https://www.ncbi.nlm.nih.gov/pubmed/16253886
- Kearns T, Evans C, Krause V. Outbreak of acute post streptococcal glomerulonephritis in the Northern Territory—2000. NT Dis Control Bulletin. 2001;8:6–14.
- Rammelkamp CH, Jr, Weaver RS. Acute glomerulonephritis, the significance of the variations in the incidence of the disease. J Clin Invest. 1953;32:345–358 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC438348/pdf/jcinvest00605-0073.pdf
- Rodriguez-Iturbe B, Musser JM. The current state of poststreptococcal glomerulonephritis. J Am Soc Nephrol. 2008;19:1855–1864 http://jasn.asnjournals.org/content/19/10/1855.long
- Balter S, Benin A, Pinto SW, Teixeira LM, Alvim GG, Luna E, Jackson D, LaClaire L, Elliott J, Facklam R, Schuchat A. Epidemic nephritis in Nova Serrana, Brazil. Lancet. 2000;355:1776–1780. https://www.ncbi.nlm.nih.gov/pubmed/10832828
- Holm SE, Nordstrand A, Stevens DL, Norgren M. In: Streptococcal Infections: Clinical Aspects, Microbiology and Molecular Patheogenesis. Stevens DL, Kaplan EL, editors. New York: Oxford University Press; 2000. pp. 152–162. (Acute postreptococcal glomerulonephritis).
- Eison TM, Ault BH, Jones DP, Chesney RW, Wyatt RJ. Post-streptococcal acute glomerulonephritis in children: clinical features and pathogenesis. Pediatr Nephrol. 2011;26:165–180.
- White AV, Hoy WE, McCred DA. Childhood post-streptococcal glomerulonephritis as a risk factor for chronic renal disease in later life. MJA. 2001;174:492–496.
- Hoy WE, Mathews JD, McCredie DA, Pugsley DJ, Hayhurst BG, Rees M, Kile E, Walker KA, Wang Z. The multidimensional nature of renal disease: rates and associations of albuminuria in an Australian Aboriginal community. Kidney Int. 1998;54:1296–1304
- Zoch-Zwierz W, Wasilewska A, Biernacka A, Tomaszewska B, Winiecka W, Wiercinski R, Porowski T: The course of post-streptococcal glomerulonephritis depending on methods of treatment of the preceding respiratory tract infection.
- Haas M, Meehan SM, Karrison TG, et al: Changing etiologies of unexplained adult nephrotic syndrome: A comparison of renal biopsy findings from 1976–1979 and 1995–1997. Am J Kidney Dis 1997;30:621–631.