What is Healthy Eating
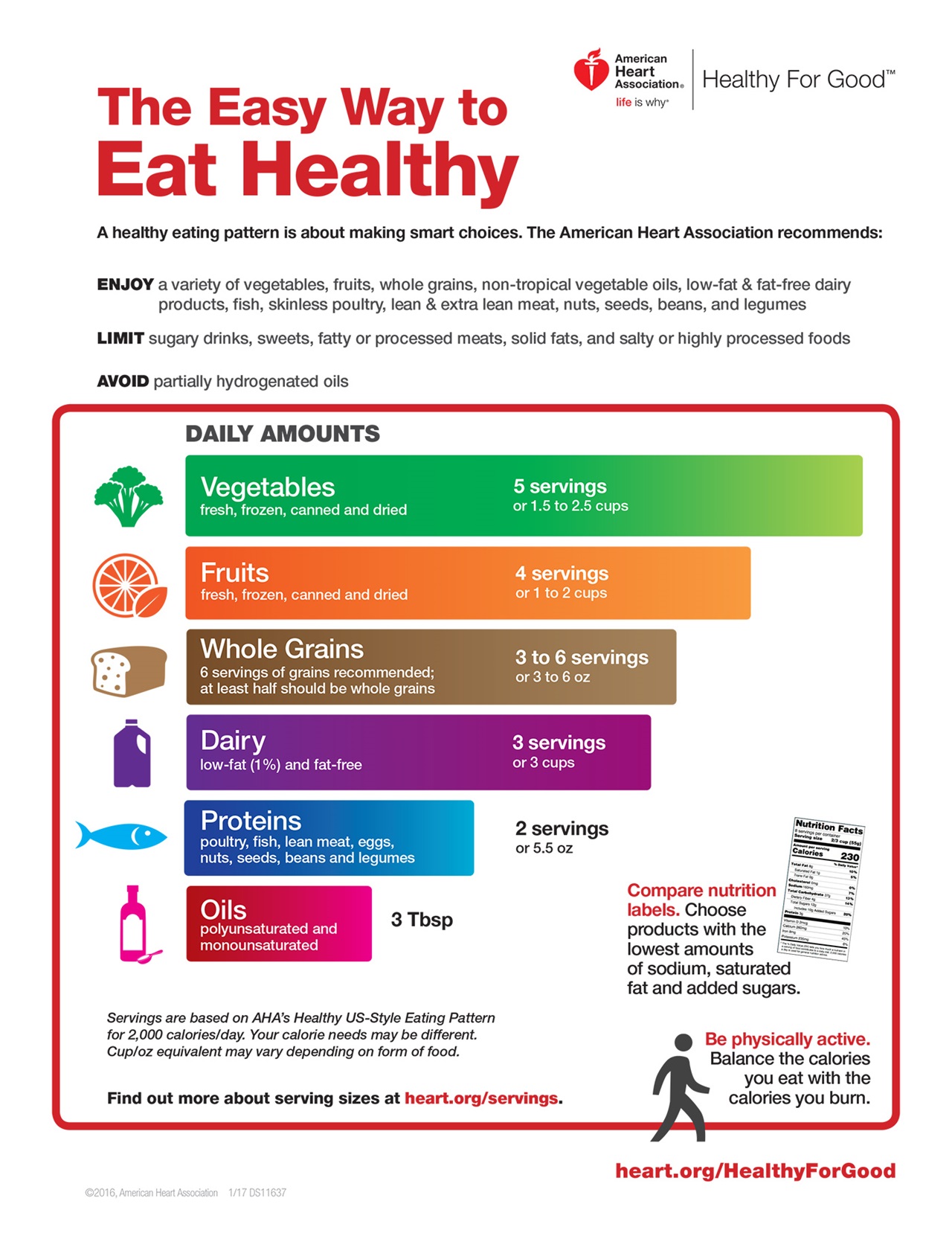
Eating healthy doesn’t have to mean dieting or giving up all the foods you love. An overall healthy eating pattern is tailored to your personal and cultural food preferences. This eating pattern can include a variety of vegetables, fruits, whole grains, beans, legumes, fish, skinless poultry, nuts, and fat-free/low-fat dairy products, and should limit sugary drinks, sweets, fatty or processed meats, solid fats, and salty or highly processed foods. It’s all about making smart choices. Learn how to ditch the junk, give your body the nutrient-dense fuel it needs, and love every minute of it! (Source 1).
Because how much calories you eat and what food groups you need are highly dependent on your age, sex, and your level of physical activity. For the most accurate way calculate how much food and calories you need to eat per day from each food group >>> Go to the United States Department of Agriculture’s MyPlate Daily Checklist 2 >>> https://www.myplate.gov
Simply enter your age, sex, height, weight, and physical activity level to get a plan that’s right for you. The MyPlate Daily Checklist shows your food group targets – what and how much to eat within your calorie allowance.
Health is defined as the state of being free from illness or injury. Health describes a person’s physical or mental condition. It’s synonymous with well-being, vigor, wellness, good-shape, good condition.
Nutrition is characteristic of foods and beverages that are nutrient dense, that provide vitamins, minerals, and other substances that contribute to adequate nutrient intakes or may have positive health effects, with little or no solid fats and added sugars, refined starches, and sodium. Ideally, these foods and beverages also are in forms that retain naturally occurring components, such as dietary fiber. All vegetables, fruits, whole grains, seafood, eggs, beans and peas, unsalted nuts and seeds, fat-free and low-fat dairy products, and lean meats and poultry—when prepared with little or no added solid fats, sugars, refined starches, and sodium—are nutrient dense foods. These foods contribute to meeting food group recommendations within calorie and sodium limits. The term “nutrient dense” indicates the nutrients and other beneficial substances in a food have not been “diluted” by the addition of calories from added solid fats, sugars, or refined starches, or by the solid fats naturally present in the food.
Malnutrition refers to deficiencies, excesses, or imbalances in a person’s intake of energy and/or nutrients. The term malnutrition addresses 3 broad groups of conditions:
- Undernutrition, which includes wasting (low weight-for-height), stunting (low height-for-age) and underweight (low weight-for-age);
- Micronutrient-related malnutrition, which includes micronutrient deficiencies (a lack of important vitamins and minerals) or micronutrient excess; and
- Overweight, obesity and diet-related noncommunicable diseases (such as heart disease, stroke, diabetes and some cancers). Which is the main topic of discussion of this entire site. In adults, overweight is defined as a Body Mass Index (BMI) of 25 or more, whereas obesity is a BMI of 30 or more. Overweight and obesity result from an imbalance between energy consumed (too much) and energy expended (too little). Worldwide, people are consuming foods and drinks that are more energy-dense (high in sugars and fats), and engaging in less physical activity.
Diet is an important determinant of chronic disease risk, particularly heart disease. This Cochrane review3 assessed the effects of providing dietary advice to healthy adults in order to produce sustained improvements in their diets. Whether dietary improvement would reduce the risk factors associated with heart disease was also examined. They found 44 trials in which healthy adults were randomly assigned to receive dietary advice or no dietary advice. The dietary improvements recommended to the people in the intervention groups centered largely on the reduction of salt and fat intake and an increase in the intake of fruit, vegetables and fiber. Advice was delivered in a variety of ways, including one-to-one contact, group sessions and written materials. There were variations in intensity of the intervention, ranging from one contact per study participant to 50 hours of counseling over four years. The duration of the trials ranged from three months to four years, with a median follow-up period of 12 months. There was some evidence of greater effectiveness in people told that they were at risk of heart disease or cancer. Modest improvements were shown in cardiovascular risk factors, such as blood pressure and total and LDL-cholesterol levels. In the trials that separated effects by gender, women tended to make larger reductions in fat intake but there was insufficient evidence to show whether this translated to a larger reduction in total cholesterol levels. Two trials followed people up 10 to 15 years after the end of the trials and showed that the beneficial changes in cardiovascular risk factors may have resulted in a reduced incidence of heart disease, stroke or heart attack, although more evidence is needed to confirm this.
A healthy diet can help protect your heart, improve your blood pressure and cholesterol, and reduce your risk of type 2 diabetes. A healthy eating plan includes:
- Vegetables and fruits
- Beans or other legumes
- Lean meats and fish
- Low-fat or fat-free dairy foods
- Whole grains
- Healthy fats, such as olive oil
The following foods are the foundation of a healthy eating plan:
- Vegetables such as leafy greens (spinach, collard greens, kale, cabbage), broccoli, and carrots
- Fruits such as apples, bananas, oranges, pears, grapes, and prunes
- Whole grains such as plain oatmeal, brown rice, and whole-grain bread or tortillas
- Fat-free or low-fat dairy foods such as milk, cheese, or yogurt
- Protein-rich foods:
- Fish high in omega-3 fatty acids (salmon, tuna, and trout)
- Lean meats such as 95% lean ground beef or pork tenderloin or skinless chicken or turkey
- Eggs
- Nuts, seeds, and soy products (tofu)
- Legumes such as kidney beans, lentils, chickpeas, black-eyed peas, and lima beans
- Oils and foods high in monounsaturated and polyunsaturated fats:
- Canola, corn, olive, safflower, sesame, sunflower, and soybean oils (not coconut or palm oil)
- Nuts such as walnuts, almonds, and pine nuts
- Nut and seed butters
- Salmon and trout
- Seeds (sesame, sunflower, pumpkin, or flax)
- Avocados
- Tofu
Research shows that the best foods that protect your heart and blood vessels, include the following:
- Fruits and Vegetables. Current World Health Organization (WHO) recommendations for fruit intake combined with vegetable intake are a minimum 400 g/day 4. A recent meta-analysis indicated that the intake of 800 g/day of fruit was associated with a 27% reductions in relative risk of cardiovascular disease 5.
- Fatty fish (Omega-3 fatty acids). Omega-3 fatty acid is a polyunsaturated fatty acid that must be obtained through dietary intake from fish as well as other types of seafood as it is not produced naturally in the human body 6. Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are essential fatty acids present in omega-3 7. Fatty fish such as salmon, sardines and mackerel are abundant sources of omega-3 fatty acids, healthy unsaturated fats that have been linked to lower blood levels of beta-amyloid—the protein that forms damaging clumps in the brains of people with Alzheimer’s disease. Omega-3 fatty acids are thought to help keep your blood vessels healthy and to help to reduce blood pressure. Research into this style of eating has shown a reduced risk of developing problems such as type 2 diabetes, high blood pressure and raised cholesterol, which are all risk factors for heart disease 8. The American Heart Association recommends eating 2 servings of fish (particularly fatty fish) per week. A serving is 3.5 ounce cooked, or about ¾ cup of flaked fish. Fatty fish like salmon, mackerel, herring, lake trout, sardines and albacore tuna are high in omega-3 fatty acids 9. Eating oily fish is a nutritious choice which can form part of the Mediterranean diet (more bread, fruit, vegetables, fish and less meat, and replacing butter with unsaturated fat spreads). Researchers have also found that people who closely follow a traditional Mediterranean style diet are more likely to live a longer life and also are less likely to become obese. Try to eat fish at least twice a week, but choose varieties that are low in mercury, such as salmon, cod, canned light tuna, and pollack. If you’re not a fan of fish, ask your doctor about taking an omega-3 supplement, or choose terrestrial omega-3 sources such as flaxseeds, avocados, and walnuts. Plant sources of omega-3 fatty acids include flaxseed, oils (olive, canola, flaxseed, soybean), nuts and other seeds (walnuts, butternut squash and sunflower). Replacements for vegans/vegetarians exist that are not supplements, but the evidence is not as robust for plant sources of omega-3 fatty acids.
- Berries. Researchers credit the high levels of flavonoids in berries with the benefit 10. Flavonoids, the natural plant pigments that give berries their brilliant hues, also help improve memory, research shows. Berries contain a particularly high amount of flavonoids called anthocyanidins that are capable of crossing the blood brain barrier and localizing themselves in the hippocampus, an area of the brain known for memory and learning. Epidemiological evidence has established strong inverse associations between flavonoid-rich fruit (e.g. strawberries, grapefruit) and coronary heart disease mortality in cardiovascular disease-free postmenopausal women after multivariate adjustment 11. In a 20-year study of over 16,000 older adult women (aged ≥70 years), those who ate the most blueberries and strawberries had the slowest rates of cognitive decline by up to two-and-a-half years 10.
- Walnuts. Nuts are excellent sources of protein, fat-soluble vitamin E and healthy fats, and one type of nut in particular might also improve memory. A 2015 study from UCLA linked higher walnut consumption to improved cognitive test scores. Walnuts are high in a type of omega-3 fatty acid called alpha-linolenic acid (ALA). Diets rich in alpha-linolenic acid and other omega-3 fatty acids have been linked to lower blood pressure and cleaner arteries. That’s good for both the heart and brain.
- Meat-free meals. Heart-healthy eating encourages consuming meat sparingly. Beans, lentils and soybeans, which pack protein and fiber, make a worthy substitute. They’ll keep you full and are rich in B vitamins, which are important for brain health. In one study analyzing the diets of older adults, those who had the lowest intakes of legumes had greater cognitive decline than those who ate more.
The American Heart Association suggests these daily amounts:
- Vegetables – canned, dried, fresh and frozen vegetables; 5 servings
- Fruits – canned, dried, fresh and frozen fruits; 4 servings
- Whole grains – barley, brown rice, millet, oatmeal, popcorn and whole wheat bread, crackers and pasta; 3-6 servings
- Dairy – low fat (1%) and fat-free dairy products; 3 servings
- Proteins – eggs, fish, lean meat, legumes, nuts, poultry and seeds; 1-2 servings. Eat a variety of fish at least twice a week, especially fish containing omega-3 fatty acids (for example, salmon, trout and herring).
- Oils – polyunsaturated and monounsaturated canola, olive, peanut, safflower and sesame oil; 3 tablespoons
- Limit – sugary drinks, sweets, fatty meats, and salty or highly processed foods
- Choose foods with less salt (sodium) and prepare foods with little or no salt. To lower blood pressure, aim to eat no more than 2,300 milligrams of sodium per day. Reducing daily intake to 1,500 mg is desirable because it can lower blood pressure even further.
- Limit saturated fat and trans fat and replace them with the better fats, monounsaturated and polyunsaturated. If you need to lower your blood cholesterol, reduce saturated fat to no more than 5 to 6 percent of total calories. For someone eating 2,000 calories a day, that’s about 13 grams of saturated fat.
- Avoid – partially hydrogenated oils, tropical oils, and excessive calories
- Replace – highly processed foods with homemade or less-processed options
- If you drink alcohol, drink in moderation. That means no more than one drink per day if you’re a woman and no more than two drinks per day if you’re a man.
Nutrition with Healthy Eating Patterns & Health Are Closely Related
There are very few studies to date examining provision of, or advice to increase the consumption of, fruit and vegetables in the absence of additional dietary interventions or other lifestyle interventions for the primary prevention of cardiovascular disease (e.g. high blood pressure, heart attacks, stroke). The limited evidence suggests advice to increase fruit and vegetables as a single intervention has favourable effects on cardiovascular disease risk factors but more trials are needed to confirm this.
Evidence shows that healthy eating patterns, are associated with positive health outcomes. The evidence base for associations between eating patterns and specific health outcomes continues to grow. Strong evidence shows that healthy eating patterns are associated with a reduced risk of cardiovascular disease (CVD). Moderate evidence indicates that healthy eating patterns also are associated with a reduced risk of type 2 diabetes, certain types of cancers (such as colorectal and postmenopausal breast cancers), overweight, and obesity. Emerging evidence also suggests that relationships may exist between eating patterns and some neurocognitive disorders and congenital anomalies.
Within this body of evidence, higher intakes of vegetables and fruits consistently have been identified as characteristics of healthy eating patterns; whole grains have been identified as well, although with slightly less consistency. Other characteristics of healthy eating patterns have been identified with less consistency and include fat-free or low-fat dairy, seafood, legumes, and nuts. Lower intakes of meats, including processed meats; processed poultry; sugar-sweetened foods, particularly beverages; and refined grains have often been identified as characteristics of healthy eating patterns.
Additional information about how food groups and dietary components fit within healthy eating patterns is discussed throughout this site. For example, research has shown that vegetables and fruits are associated with a reduced risk of many chronic diseases, including cardiovascular disease and may be protective against certain types of cancers. Additionally, some evidence indicates that whole grain intake may reduce risk for cardiovascular disease and is associated with lower body weight. Research also has linked dairy intake to improved bone health, especially in children and adolescents.
A healthy eating pattern limits:
- Saturated fats and trans fats, added sugars, and sodium. Limit calories from added sugars and saturated fats and reduce sodium intake.
- Consume an eating pattern low in added sugars, saturated fats, and sodium. Cut back on foods and beverages higher in these components to amounts that fit within healthy eating patterns.
- Replace typical food and beverages choices with more nutrient-dense options. Choose nutrient-dense foods and beverages across and within all food groups in place of less healthy choices. Consider cultural and personal preferences to make these shifts easier to accomplish and maintain.

Reduced dietary Salt (sodium) for the prevention of cardiovascular disease
- Fact #1: Science strongly supports the link between less sodium intake and healthier lives – even in children and teens 12. For example, kids who eat high sodium diets are about 35% more likely to have elevated blood pressure than kids who eat lower sodium diets 13. And the rate of high blood pressure is increasing in American children. In addition to heart health, sodium impacts bone, brain, stomach, and kidney health 14.
- Fact #2: There has been a lot of noise about some sodium studies, leading to confusion and helping efforts to undermine nutrition standards for school meals. A large body of scientific research indicates that lowering sodium intake lowers blood pressure in adults and children 15.
- Fact #3: Actually, more than 99 percent of schools are successfully meeting the updated meal standards 16. Some schools are already meeting the USDA’s 2017 targets. Many companies already offer foods that meet the target limits set by the USDA 17. A variety of methods exist that can help reduce sodium in foods 18, and modelling suggests that some newly developed ingredients could make a big impact. 19.
- Fact #4: Replacing nutrient-poor, high-sodium foods with healthier foods could improve overall consumption of other beneficial nutrients. Gradually lowering the sodium content in foods can decrease kids’ (and adults’) taste for salty food over time. 20.
Cardiovascular disease includes heart attacks and strokes and is a major cause of premature death and disability. In the most updated clinical and scientific review first published in 2014 21. The review of a total of eight trials with 7284 participants found dietary advice and salt substitution did reduce the amount of salt eaten, which led to a small reduction in blood pressure by six months. There was weak evidence of benefit for cardiovascular events, but these findings were inconclusive and were driven by a single trial among retirement home residents, which reduced salt intake in the kitchens of the homes.
The findings of the review do not mean that advising people to reduce salt should be stopped. However, additional measures – reducing the amount of hidden salt in processed foods, for example – will make it much easier for people to achieve a lower salt diet. Overall many of the trials failed to report sufficient detail to assess their potential risk of bias. Further evidence of the effects of different ways of reducing dietary salt on clinical events is needed from experimental and observational studies to underpin public health policies.
The review concluded that despite collating more event data than previous systematic reviews of randomized controlled trials, there is insufficient power to confirm clinically important effects of dietary advice and salt substitution on cardiovascular mortality in normal blood pressure or high blood pressure populations. Their estimates of the clinical benefits from advice to reduce dietary salt are imprecise, but are larger than would be predicted from the small blood pressure reductions achieved. Further well-powered studies would be needed to obtain more precise estimates. Their findings do not support individual dietary advice as a means of restricting salt intake. It is possible that alternative strategies that do not require individual behavior change may be effective and merit further trials.
The specified limits can help you achieve healthy eating patterns within calorie limits:
- Consume less than 10 percent of calories per day from added sugars.
- Consume less than 10 percent of calories per day from saturated fats.
- Consume less than 2,300 milligrams (mg) per day of sodium.
- If alcohol is consumed, it should be consumed in moderation—up to one drink per day for women and up to two drinks per day for men—and only by adults of legal drinking age.
A healthy eating pattern is not a rigid prescription, but rather, an adaptable framework in which individuals can enjoy foods that meet their personal, cultural, and traditional preferences and fit within their budget.
Healthy Eating means consuming the right quantities of foods from all food groups in order to lead a healthy life. Healthy eating means eating a variety of foods that give you the nutrients you need to maintain your health, feel good, and have energy. These nutrients include protein, carbohydrates, fat, water, vitamins, and minerals. Several examples of healthy eating patterns that translate and integrate the recommendations in overall healthy ways to eat are provided.
What Does “Healthy Eating” Mean?
According to the Dietary Guidelines for Americans, a healthy diet:
- Emphasizes vegetables, fruits, whole grains, and fat-free or low-fat milk products.
- Includes lean meats, poultry, fish, beans, eggs, and nuts.
- Is low in saturated fats, trans fats, cholesterol, salt, and added sugars. Limit calories from added sugars and saturated fats and reduce sodium intake. Consume an eating pattern low in added sugars, saturated fats, and sodium. Cut back on foods and beverages higher in these components to amounts that fit within healthy eating patterns.
- Balances the calories you take in from food and beverages with the calories burned through physical activity to maintain a healthy weight.
Here are some tips to help you meet the guidelines:
- Eating fruits and vegetables of different colors gives your body a wide range of valuable nutrients. A variety of vegetables from all of the subgroups—dark green, red and orange, legumes (beans and peas), starchy.
- Include foods that contain fiber such as fruits, vegetables, beans, and whole-grains.
- Eat lean cuts of meat and poultry. Trim away excess fat and remove skin from poultry before cooking.
- Pay attention to portion sizes, especially at restaurants. Smaller portions equal fewer calories.
- Season your food with lemon juice, herbs, and spices, rather than using butter and salt.
- Choose foods that are baked, broiled, braised, grilled, steamed, sautéed, or boiled, rather than fried.
- When eating out, select a dish from the menu, rather than getting your money’s worth at the all-you-can-eat buffet.

Nutrition is important for everyone. When combined with being physically active and maintaining a healthy weight, eating well is an excellent way to help your body stay strong and healthy. What you eat can affect your immune system, your mood, and your energy level.
Diet is often referred to as some dietary regimen for losing weight. However, diet simply means what food we eat in the course of a 24-hour, one week, or one month, etc.
Healthy US Style Eating Pattern is based on the types and proportions of foods Americans typically consume, but in nutrient-dense forms and appropriate amounts. It is designed to meet nutrient needs while not exceeding calorie requirements and while staying within limits for over-consumed dietary components.
- Vegetables and fruits, 1 cup-equivalent is: 1 cup raw or cooked vegetable or fruit, 1 cup vegetable or fruit juice, 2 cups leafy salad greens, ½ cup dried fruit or vegetable.
- Grains, 1 ounce-equivalent is: ½ cup cooked rice, pasta, or cereal; 1 ounce dry pasta or rice; 1 medium (1 ounce) slice bread; 1 ounce of ready-to-eat cereal (about 1 cup of flaked cereal).
- Dairy, 1 cup-equivalent is: 1 cup milk, yogurt, or fortified soymilk; 1½ ounces natural cheese such as cheddar cheese or 2 ounces of processed cheese.
- Protein Foods, 1 ounce-equivalent is: 1 ounce lean meat, poultry, or seafood; 1 egg; ¼ cup cooked beans or tofu; 1 Tbsp peanut butter; ½ ounce nuts or seeds.
Carbohydrate
Carbohydrate (starch) is the body’s main energy (fuel) source. Starch is broken down to produce glucose which is used by your body for energy.
Starchy foods are an important part of the healthy diet. They should make up about a third of all the food that you eat. You don’t have to avoid or restrict them because they are ‘fattening’. Instead, be aware of the total amount of starch that you eat. Cutting out one food group, such as carbohydrate can cause dietary imbalance. Starchy foods include bread, potatoes, rice and pasta. Wholegrain options are healthier choices.
Fiber rich foods help your gut to function properly and have many other health benefits. Studies have shown that people who are overweight or obese tend to lose weight if they include plenty of high fiber, starchy carbohydrate in their diets.
Sugar
Sugar is a type of carbohydrate. Like starch, it breaks down into glucose, to provide energy for your body. ‘Free’ sugars are often added to foods during manufacture and include refined sugars such as sucrose (table sugar). This kind of sugar is also found naturally, in unsweetened fruit juices, and in syrups and honey.
Excess consumption of free sugars is linked to the risk of obesity, type 2 diabetes and tooth decay. Many of the free sugars that you consume, are in sugary drinks. A regular can of cola for instance, can contain the equivalent of seven teaspoons of sugar (35g). The guidance about free sugar consumption suggests a daily limit of 30g. This is equivalent to six teaspoons.
The natural sugars found in milk and in whole fruits and vegetables are not free sugars and do not need to be restricted in the same way.
Fruit and vegetables
Fruit and vegetables contain high levels of ‘micronutrients’. These include vitamins, minerals and antioxidants. Micronutrients are essential to the body’s many biochemical processes.
Fruit and vegetables are often high in fiber. They are generally low in calorie and they taste good. The current Dietary Guidelines for Americans recommends at least five portions of different fruit and vegetable per day 22. Like carbohydrate, fruit and vegetable should account for about one third of what you eat, per day. Dried, frozen, tinned, as well as fresh, fruit and veg are all included. One portion of pulses (baked beans, lentils, dried peas) can also count towards your five a day.
Dietary fiber
Fiber comes from plant-based foods, including fruits, vegetables and wholegrains. Dietary fiber is the part of plants that you eat but which doesn’t get digested in your small intestine. Instead, it is completely or partially broken down (fermented) by bacteria in your large intestine. Once broken down in your large intestine, it has been suggested that dietary fibers increase the beneficial bacteria in your gut. This improves your immune system. Fiber includes carbohydrates called polysaccharides and resistant oligosaccharides. Recent research suggests that fiber should be categorized by its physical characteristics; how well it dissolves (solubility), how thick it is (viscosity) and how well it breaks down (fermentability). Some commonly known terms are described below:
- Soluble fiber including pectins and beta glucans is found in foods like fruit and oats.
- Insoluble fiber including cellulose is found in wheat bran and nuts.
- Resistant starch is a soluble fiber that is highly fermentable in the gut. It gets broken down by good bacteria to produce short chain fatty acids (SCFAs). Resistant starch is naturally present in some foods such as bananas, potatoes, grains and pulses.
- Prebiotics are types of carbohydrate that only our gut bacteria can feed upon. Some examples are onions, garlic, asparagus and banana
Fiber is essential for your gut to work normally. It increases good bacteria which supports your immunity against inflammatory disorders and allergies. A high fiber diet seems to reduce the risk of chronic diseases such as heart disease, type 2 diabetes and bowel cancer.
Eating a range of dietary fiber can:
- Improve the diversity of your microbiota
- Improve constipation and lactose intolerance
- Enhance immunity
- Reduce inflammation in your gut
For example, high quality randomized controlled trials have shown that eating oat bran leads to lower blood pressure and lower total cholesterol.
Benefits of a high-fiber diet:
- Normalizes bowel movements. Dietary fiber increases the weight and size of your stool and softens it. A bulky stool is easier to pass, decreasing your chance of constipation. If you have loose, watery stools, fiber may help to solidify the stool because it absorbs water and adds bulk to stool.
- Helps maintain bowel health. A high-fiber diet may lower your risk of developing hemorrhoids and small pouches in your colon (diverticular disease). Studies have also found that a high-fiber diet likely lowers the risk of colorectal cancer. Some fiber is fermented in the colon. Researchers are looking at how this may play a role in preventing diseases of the colon.
- Lowers cholesterol levels. Soluble fiber found in beans, oats, flaxseed and oat bran may help lower total blood cholesterol levels by lowering low-density lipoprotein, or “bad,” cholesterol levels. Studies also have shown that high-fiber foods may have other heart-health benefits, such as reducing blood pressure and inflammation.
- Helps control blood sugar levels. In people with diabetes, fiber — particularly soluble fiber — can slow the absorption of sugar and help improve blood sugar levels. A healthy diet that includes insoluble fiber may also reduce the risk of developing type 2 diabetes.
- Aids in achieving healthy weight. High-fiber foods tend to be more filling than low-fiber foods, so you’re likely to eat less and stay satisfied longer. And high-fiber foods tend to take longer to eat and to be less “energy dense,” which means they have fewer calories for the same volume of food.
- Helps you live longer. Studies suggest that increasing your dietary fiber intake — especially cereal fiber — is associated with a reduced risk of dying from cardiovascular disease and all cancers.
Good sources of dietary fiber include:
- Pulses (like lentils and peas) and beans and legumes (think navy beans, small white beans, split peas, chickpeas, lentils, pinto beans)
- Fruits and vegetables, vegetables such as carrots, broccoli, green peas, and collard greens; fruits especially those with edible skin (like pears and apples with the skin on) and those with edible seeds (like berries)
- Nuts—try different kinds (pumpkin seeds, almonds, sunflower seeds, pistachios and peanuts are a good source of fiber and healthy fats, but be mindful of portion sizes, because they also contain a lot of calories in a small amount!)
- Whole grains such as:
- Quinoa, barley, bulgur, oats, brown rice and farro
- Whole wheat pasta
- Whole grain cereals, including those made from whole wheat, wheat bran and oats
Choose fiber rich foods from a variety of sources including wholegrains, fruit and vegetable, nuts and seeds, beans and pulses. When you read food labels check for the grams of fiber per serving or per 100g. Foods that are naturally high in fiber and contain at least 3 grams per 100 gram are often labeled as a “good source,” and foods labeled as “excellent source” contain more than 5 grams of fiber per serving.
Depending on your age and sex, adults should get 25 to 31 grams of fiber a day 23. Older adults sometimes don’t get enough fiber because they may lose interest in food.
- Men over the age of 50 should get at least 38 grams of fiber per day.
- Women over the age of 50 should get 25 grams per day.
- Children ages 1 to 3 should get 19 grams of fiber per day.
- Children between 4 and 8 years old should get 25 grams per day.
- Girls between 9 and 18 should get 26 grams of fiber each day. Boys of the same age range should get between 31 and 38 grams of fiber per day.
You may wish to see a dietitian if you:
- are unsure about how much and/or what types of fiber you currently have in your diet
- suffer with constipation or diarrhea (e.g. irritable bowel syndrome [IBS])
- have a condition which can restrict your fiber intake (e.g. inflammatory bowel disease)
Keep in mind that if you haven’t been eating a lot of foods high in fiber on a daily basis, it’s important to increase your intake slowly to allow your body to adjust. A sudden increase in eating foods high in fiber (especially foods with added fiber or when using supplements) can cause gas, bloating or constipation. Be sure you are drinking enough water too, because fiber needs water to move through your body.
Protein
Protein is vital. It is your body’s main building block. Proteins help build and maintain muscle, bone, skin, connective tissue, internal organs, and blood. They help fight disease and heal wounds. Protein is found in foods from plants and animals. Animal products such as meat, fish, eggs and dairy are good sources of dietary protein. Meat and fish also provide your body with a form of iron (heme), which is easy to absorb. Fish also contains essential fatty acids (e.g, Omega-3).
Protein also comes from foods of plant origin. Pulses, nuts, and seeds are all high in protein. Pulses are a very good meat alternative, whether or not you are vegetarian or vegan. Most people eat both types of protein. Talk to your dietitian about how to choose the right combination of protein foods for you.
Cutting back on consumption of red meat (beef, lamb, goat, pork) especially, is better for your health and for the environment: current advice is to have no more than 300g of red meat per week. Try to avoid processed meats such as bacon, salami, hot dogs, ham. Consumption of these cured meat products has been linked to a much higher risk of certain gut cancers.
All protein isn’t alike. Protein is built from building blocks called amino acids. Your body makes amino acids in two different ways: Either from scratch, or by modifying others. A few amino acids (known as the essential amino acids) must come from food.
Food protein containing all 9 amino acids in adequate amounts is called complete or high-quality protein.
- ANIMAL FOODS with complete protein include liver (chicken, pork, beef), goose, duck, turkey, chicken, lamb, pork, most fish, rabbit, eggs, milk, cheese (cottage, gjetost, cream, swiss, ricotta, limburger, gruyere, gouda, fontina, edam) and certain beef cuts. Animal foods with incomplete protein include certain yogurts and beef cuts.
- PLANT FOODS with complete protein include spinach, beans (black, cranberry, french, pink, white, winged, yellow), soy, split peas, chickpeas, chestnuts, pistachios, pumpkin seeds, avocado, potatoes, quinoa, a seaweed spirulina, tofu and hummus. Common plant foods with incomplete protein: rice (white and brown), white bread (including whole-wheat), pasta, beans (adzuki, baked, kidney, lima, pinto, snap), peas, lentils, nuts (walnuts, peanuts, hazelnuts, almonds, coconut), sunflower seeds, kamut.
In determining the effectiveness of a protein is accomplished by determining its quality and digestibility. Quality refers to the availability of amino acids that it supplies, and digestibility considers how the protein is best utilized. Typically, all dietary animal protein sources are considered to be complete proteins. That is, a protein that contains all of the essential amino acids 24. Proteins from vegetable sources are incomplete in that they are generally lacking one or two essential amino acids. Thus, someone who desires to get their protein from vegetable sources (i.e. vegetarian, vegan) will need to consume a variety of vegetables, fruits, grains, and legumes to ensure consumption of all essential amino acids. As such, individuals are able to achieve necessary protein requirements without consuming beef, poultry, or dairy 24. Protein digestibility ratings usually involve measuring how the body can efficiently utilize dietary sources of protein. Typically, vegetable protein sources do not score as high in ratings of biological value, net protein utilization, protein digestibility corrected amino acid score and protein efficiency ratio as animal proteins.
Vegetarians need to be aware of this. People who don’t eat meat, fish, poultry, eggs, or dairy products need to eat a variety of protein-containing foods each day in order to get all the amino acids needed to make new protein.
- Animal Protein Foods : Animal sources of protein tend to deliver all the amino acids we need. Meat, such as pork, beef, chicken, turkey, duck / Eggs / Dairy products, such as milk, yogurt, cheese / Fish
- Plant (Vegetable) Protein Foods : Other protein sources, such as fruits, vegetables, grains, nuts and seeds, lack one or more essential amino acids.
- High Protein Plant Foods: Beans, peas, lentils / Soy foods, such as soy milk, tofu / Nuts and nut spreads, such as almond butter, pea
/ nut butter, soy nut butter /Sunflower seeds 25 - Low Protein Plant Foods: Bread, tortillas / Oatmeal, grits, cereals / Pasta, noodles, rice / Rice milk (not enriched).
Finding balance, choosing the right kind and amount of protein.
- When choosing protein, opt for low-fat options, such as lean meats, skim milk or other foods with high levels of protein. Legumes, for example, can pack about 16 grams of protein per cup and are a low-fat and inexpensive alternative to meat.
Choose main dishes that combine meat and vegetables together, such as low-fat soups, or a stir-fry that emphasizes veggies.
- Some high-protein foods are healthier than others because of what comes along with the protein: healthy fats or harmful ones, beneficial fiber or hidden salt. It’s this protein package that’s likely to make a difference for health. For example, a 6-ounce broiled porterhouse steak is a great source of protein—about 40 grams worth. But it also delivers about 12 grams of saturated fat 26. For someone who eats a 2,000 calorie per day diet, that’s more than 60 percent of the recommended daily intake for saturated fat.
- Watch portion size. Aim for 2- to 3-ounce servings.
- If you’re having an appetizer, try a plate of raw veggies instead of a cheese plate. Cheese adds protein, but also fat.
- A 6-ounce ham steak has only about 2.5 grams of saturated fat, but it’s loaded with sodium—2,000 milligrams worth, or about 500 milligrams more than the daily sodium max.
6-ounces of wild salmon has about 34 grams of protein and is naturally low in sodium, and contains only 1.7 grams of saturated fat 26. Salmon and other fatty fish are also excellent sources of omega-3 fats, a type of fat that’s especially good for the heart. Alternatively, a cup of cooked lentils provides about 18 grams of protein and 15 grams of fiber, and it has virtually no saturated fat or sodium 26.
The Vegetarian Society’s Vegetarian sources of protein include 27:
- Nuts, beans and pulses, such as quinoa – these have very high levels of protein
- Cheese
- Eggs – have the perfect balance of amino acids
- Soya is very versatile and found in soya milk, tofu, miso and ready made products such as burgers and sausages
- Quorn is a form of myco-protein and sold in a range of forms
- Rice, grains, pasta, bread and potatoes, although not generally known for their protein, play an important part in your protein intake
Vegetarian food of animal origin such as cheese, milk and eggs have a good balance of essential amino acids. However, food groups such as cereals, rice and legumes (peas, lentils and beans) have an imbalance of 2 of the essential amino acids. To provide a ‘complete’ protein, containing a balance of all 8 essential amino acids, it is recommended to consume a combination of cereals and legumes in your diet e.g. beans on toast.
Dairy
Dairy products and calcium-fortified alternatives are your body’s main source of calcium, which is necessary for the growth, development and maintenance of healthy bones and teeth. Dairy products and alternatives are also a source of protein. Milk, cheese, cream and milk-based sauces and yogurts can have a high saturated fat content. Fat reduced options are recommended, and small quantities.
Fats
Fats also known as lipids, is an essential nutrient (a primary storage form of energy, a kilojoule-dense nutrient) your body need for energy and to help your gut absorb vitamins A, D, E and K from foods. Fat has twice as many calories as proteins or carbohydrates. There are nine calories (37kJ) in every gram of fat, regardless of what type of fat it is. Fats are more energy-dense than carbohydrates and proteins, which provide four calories (17kJ) per gram. Dietary fat also plays a major role in your cholesterol levels. You need some fat in your diet but not too much. There are different types of fats, some are “good” and some are “bad”, however, you should try to avoid “bad” fats. When it comes to dietary fat, what matters most is the type of fat you eat. Contrary to past dietary advice promoting low-fat diets, newer research shows that healthy fats are necessary and beneficial for health.
Healthy fats are unsaturated. They keep cholesterol levels within a healthy range, reduce your risk of heart problems and may be good for the skin, eyes and brain. Unsaturated fats are the best choice for a healthy diet.
Unhealthy fats are saturated and trans fats, which can raise levels of ‘bad’ cholesterol and increase the risk of heart disease. Multiple studies have linked high levels of saturated fat with cognitive decline. A diet that is higher in unsaturated fats and lower in saturated fats is linked to better cognition.
- Saturated fats such as butter, solid shortening, and lard. Eating foods that contain saturated fats raises the level of cholesterol in your blood. High levels of LDL cholesterol (low-density lipoprotein or “bad” cholesterol) in your blood increase your risk of heart disease and stroke. The American Heart Association recommends aiming for a dietary pattern that achieves 5% to 6% of calories from saturated fat. For example, if you need about 2,000 calories a day, no more than 120 of them should come from saturated fat. That’s about 13 grams of saturated fat per day 28.
- Trans fats also known as trans fatty acids or “partially hydrogenated oils”. These are found in vegetable shortenings, some margarines, crackers, cookies, snack foods, and other foods made with or fried in partially hydrogenated oils. By 2018, most U.S. companies will not be allowed to add partially hydrogenated oils to food.
“Bad” fats, such as artificial trans fats and saturated fats, are guilty of the unhealthy things all fats have been blamed for—weight gain, clogged arteries, an increased risk of certain diseases, and so forth. Large studies have found that replacing saturated fats in your diet with unsaturated fats and omega-3 fatty acids can reduce your risk of heart disease by about the same amount as cholesterol-lowering drugs. Since fat is an important part of a healthy diet, rather than adopting a low-fat diet, it’s more important to focus on eating more beneficial “good” fats and limiting harmful “bad” fats. For good health, the majority of the fats that you eat should be monounsaturated or polyunsaturated. Eat foods containing monounsaturated fats and/or polyunsaturated fats such as canola oil, olive oil, safflower oil, sesame oil or sunflower oil instead of foods that contain saturated fats and/or trans fats.
For years you’ve been told that eating fat will add inches to your waistline, raise cholesterol, and cause a myriad of health problems. When food manufacturers reduce fat, they often replace it with carbohydrates from sugar, refined grains, or other starches. Your body digests these refined carbohydrates and starches very quickly, affecting your blood sugar and insulin levels and possibly resulting in weight gain and disease 29. But now scientists know that not all fat is the same. Research has shown that unsaturated fats are good for you. Healthy fats play a huge role in helping you manage your moods, stay on top of your mental game, fight fatigue, and even control your weight. These fats come mostly from plant sources. Cooking oils that are liquid at room temperature, such as canola, peanut, safflower, soybean, and olive oil, contain mostly unsaturated fat. Nuts, seeds, and avocados are also good sources. Fatty fish—such as salmon, sardines, and herring—are rich in unsaturated fats, too. You should actively make unsaturated fats a part of your diet. Of course, eating too much fat will put on the pounds too. Note also that by swapping animal fats for refined carbohydrates—such as replacing your breakfast bacon with a bagel or pastry—won’t have the same benefits. In fact eating refined carbohydrates or sugary foods can have a similar negative effect on your cholesterol levels, your risk for heart disease, and your weight. Limiting your intake of saturated fat can still help improve your health—as long as you take care to replace it with good fat rather than refined carbs. In other words, don’t go no fat, go good fat.
Healthy-eating tips:
- Use olive oil in cooking.
- Replace saturated fats with unsaturated fats; for example, use avocado, tahini, nut or seed butter instead of dairy butter.
- Eat fish, especially oily fish, twice a week.
- Consume legume- or bean-based meals twice a week.
- Snack on nuts or add them to your cooking.
- Throw avocado in salads.
- Choose lean meats and trim any fat you can see (including chicken skin).
- Use table spreads that have less than 0.1g of trans fats per 100g.
Saturated fats
Saturated fats are fat molecules that are “saturated” with hydrogen molecules. Saturated fats are normally solid at room temperature. Saturated fats occur naturally in many foods — primarily meat and dairy foods (butter, cream, full-fat milk and cheese). Beef, lamb, pork on poultry (with the skin on) contain saturated fats, as do butter, cream and cheese made from whole or 2% milk. Plant-based foods that contain saturated fats include coconut, coconut oil, coconut milk and coconut cream, cooking margarine, and cocoa butter, as well as palm oil and palm kernel oil (often called tropical oils). Saturated fats are also found in snacks like chips, cakes, biscuits and pastries, and takeaway foods. Consuming more than the recommended amount of saturated fat is linked to heart disease and high cholesterol.
The American Dietary Guidelines recommend that:
- men should not eat more than 30g of saturated fat a day
- women should not eat more than 20g of saturated fat a day
- children should have less
For people who need to lower their cholesterol, the American Heart Association recommends reducing saturated fat to less than 6% of total daily calories. For someone eating 2,000 calories a day, that’s about 11 to 13 grams of saturated fat 28.
Examples of foods with saturated fat are:
- fatty beef,
- lamb,
- pork,
- poultry with skin,
- beef fat (tallow),
- meat products including sausages and pies,
- lard and cream,
- butter and ghee,
- cheese especially hard cheese like cheddar,
- other dairy products made from whole or reduced-fat (2 percent) milk,
- cream, soured cream and ice cream,
- some savory snacks, like cheese crackers and some popcorns,
- chocolate confectionery,
- biscuits, cakes, and pastries
In addition, many baked goods and fried foods can contain high levels of saturated fats. Some plant-based oils, such as palm oil, palm kernel oil, coconut oil and coconut cream, also contain primarily saturated fats, but do not contain cholesterol.
Unsaturated Fats
If you want to reduce your risk of heart disease, it’s best to reduce your overall fat intake and swap saturated fats for unsaturated fats. Unsaturated fats are in fish, such as salmon, trout and herring, and plant-based foods such as avocados, olives and walnuts. Liquid vegetable oils, such as soybean, corn, safflower, canola, olive and sunflower, also contain unsaturated fats.
There are 2 types of unsaturated fats: monounsaturated and polyunsaturated. Unsaturated fats help reduce your risk of heart disease and lower your cholesterol levels.
- Polyunsaturated fats such as omega-3 and omega-6 fats are found in fish, nuts, and safflower and soybean oil.
- Monounsaturated fats are found in olive and canola oil, avocado, cashews and almonds.
Monounsaturated fats have one (“mono”) unsaturated carbon bond in the molecule. Polyunsaturated fats have more than one (“poly,” for many) unsaturated carbon bonds. Both of these unsaturated fats are typically liquid at room temperature.
Eaten in moderation, both kinds of unsaturated fats may help improve your blood cholesterol when used in place of saturated and trans fats.
Polyunsaturated fats
Polyunsaturated fats are simply fat molecules that have more than one unsaturated carbon bond in the molecule, this is also called a double bond. Oils that contain polyunsaturated fats are typically liquid at room temperature but start to turn solid when chilled. Olive oil is an example of a type of oil that contains polyunsaturated fats.
There are 2 main types of polyunsaturated fats: omega-3 and omega-6. Oils rich in polyunsaturated fats also provide essential fats that your body needs but can’t produce itself – such as omega-6 and omega-3 fatty acids. You must get essential fats through food. Omega-6 and omega-3 fatty acids are important for many functions in the body. A deficiency of essential fatty acids—either omega-3s or omega-6s—can cause rough, scaly skin and dermatitis 30.
Polyunsaturated fats can help reduce bad cholesterol levels in your blood which can lower your risk of heart disease and stroke. Polyunsaturated fats also provide nutrients to help develop and maintain your body’s cells. Oils rich in polyunsaturated fats also contribute vitamin E to the diet, an antioxidant vitamin most Americans need more of.
Foods high in polyunsaturated fat include a number of plant-based oils, including:
- soybean oil
- corn oil
- sunflower oil
Other sources include some nuts and seeds such as walnuts and sunflower seeds, tofu and soybeans.
Omega-6 fats are found in vegetable oils, such as:
- rapeseed
- corn
- sunflower
- some nuts
Omega-3 fats are found in oily fish, such as:
- kippers
- herring
- trout
- sardines
- salmon
- mackerel
The American Heart Association also recommends eating tofu and other forms of soybeans, canola, walnut and flaxseed, and their oils. These foods contain alpha-linolenic acid (ALA), another omega-3 fatty acid.
Polyunsaturated fats (PUFAs) are frequently designated by their number of carbon atoms and double bonds. Alpha-linolenic acid (ALA), for example, is known as C18:3n-3 because it has 18 carbons and 3 double bonds and is an omega-3 fatty acid. Similarly, eicosapentaenoic acid (EPA) is known as C20:5n-3 and docosahexaenoic acid (DHA) as C22:6n-3. Omega-6 fatty acids (omega-6s) have a carbon–carbon double bond that is six carbons away from the methyl end of the fatty acid chain. Linoleic acid (LA) known as C18:2n-6 and arachidonic acid (AA) known as C20:4n-6 are two of the major omega-6s.
The human body can only form carbon–carbon double bonds after the 9th carbon from the methyl end of a fatty acid 31. Therefore, alpha-linolenic acid (ALA) and linoleic acid (LA) are considered essential fatty acids, meaning that they must be obtained from the diet 32. Alpha-linolenic acid (ALA) can be converted into eicosapentaenoic acid (EPA) and then to docosahexaenoic acid (DHA), but the conversion (which occurs primarily in the liver) is very limited, with reported rates of less than 15% 33. Therefore, consuming EPA and DHA directly from foods and/or dietary supplements is the only practical way to increase levels of these fatty acids in the body.
Alpha-linolenic acid (ALA) is present in plant oils, such as flaxseed, soybean, and canola oils 33. Docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) are present in fish, fish oils, and krill oils, but they are originally synthesized by microalgae, not by the fish. When fish consume phytoplankton that consumed microalgae, they accumulate the omega-3s in their tissues 33.
Some researchers propose that the relative intakes of omega-6s and omega-3s—the omega-6/omega-3 ratio—may have important implications for the pathogenesis of many chronic diseases, such as cardiovascular disease and cancer 34, but the optimal ratio—if any—has not been defined 35. Others have concluded that such ratios are too non-specific and are insensitive to individual fatty acid levels 36. Most agree that raising eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) blood levels is far more important than lowering linoleic acid (LA) or arachidonic acid levels.
Currently, most clinicians do not assess omega-3 status, but it can be done by measuring individual omega-3s in plasma or serum phospholipids and expressing them as the percentage of total phospholipid fatty acids by weight 37. Experts have not established normal ranges, but mean values for serum or plasma phospholipid eicosapentaenoic acid (EPA) plus docosahexaenoic acid (DHA) among U.S. adults not taking omega-3 supplements are about 3%–4% 37. Plasma and serum fatty acid values, however, can vary substantially based on an individual’s most recent meal, so they do not reflect long-term dietary consumption 38.
It is also possible to assess omega-3 status via analysis of erythrocyte fatty acids, a measurement that reflects longer-term intakes over approximately the previous 120 days 39. The “omega-3 index” proposed by Harris and von Schacky reflects the content of eicosapentaenoic acid (EPA) plus docosahexaenoic acid (DHA) in erythrocyte membranes expressed as a percentage of total erythrocyte fatty acids 40. This index can be used as a surrogate for assessing tissue levels of eicosapentaenoic acid (EPA) plus docosahexaenoic acid (DHA) 41. Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) typically comprise about 3%–5% of erythrocyte fatty acids in Western populations with low fish intakes. In Japan, where fish consumption is high, erythrocyte eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) levels are about twice those of Western populations 33.
Table 1. Alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) content of selected foods
| Food | Grams per serving | ||
| ALA | DHA | EPA | |
| Flaxseed oil, 1 tbsp | 7.26 | ||
| Chia seeds, 1 ounce | 5.06 | ||
| English walnuts, 1 ounce | 2.57 | ||
| Flaxseed, whole, 1 tbsp | 2.35 | ||
| Salmon, Atlantic, farmed cooked, 3 ounces | 1.24 | 0.59 | |
| Salmon, Atlantic, wild, cooked, 3 ounces | 1.22 | 0.35 | |
| Herring, Atlantic, cooked, 3 ounces* | 0.94 | 0.77 | |
| Canola oil, 1 tbsp | 1.28 | ||
| Sardines, canned in tomato sauce, drained, 3 ounces* | 0.74 | 0.45 | |
| Mackerel, Atlantic, cooked, 3 ounces* | 0.59 | 0.43 | |
| Salmon, pink, canned, drained, 3 ounces* | 0.04 | 0.63 | 0.28 |
| Soybean oil, 1 tbsp | 0.92 | ||
| Trout, rainbow, wild, cooked, 3 ounces | 0.44 | 0.4 | |
| Black walnuts, 1 ounce | 0.76 | ||
| Mayonnaise, 1 tbsp | 0.74 | ||
| Oysters, eastern, wild, cooked, 3 ounces | 0.14 | 0.23 | 0.3 |
| Sea bass, cooked, 3 ounces* | 0.47 | 0.18 | |
| Edamame, frozen, prepared, ½ cup | 0.28 | ||
| Shrimp, cooked, 3 ounces* | 0.12 | 0.12 | |
| Refried beans, canned, vegetarian, ½ cup | 0.21 | ||
| Lobster, cooked, 3 ounces* | 0.04 | 0.07 | 0.1 |
| Tuna, light, canned in water, drained, 3 ounces* | 0.17 | 0.02 | |
| Tilapia, cooked, 3 ounces* | 0.04 | 0.11 | |
| Scallops, cooked, 3 ounces* | 0.09 | 0.06 | |
| Cod, Pacific, cooked, 3 ounces* | 0.1 | 0.04 | |
| Tuna, yellowfin, cooked 3 ounces* | 0.09 | 0.01 | |
| Kidney beans, canned ½ cup | 0.1 | ||
| Baked beans, canned, vegetarian, ½ cup | 0.07 | ||
| Ground beef, 85% lean, cooked, 3 ounces** | 0.04 | ||
| Bread, whole wheat, 1 slice | 0.04 | ||
| Egg, cooked, 1 egg | 0.03 | ||
| Chicken, breast, roasted, 3 ounces | 0.02 | 0.01 | |
| Milk, low-fat (1%), 1 cup | 0.01 | ||
Footnotes: *Except as noted, the U.S. Department of Agriculture (USDA) database does not specify whether fish are farmed or wild caught. **The USDA database does not specify whether beef is grass fed or grain fed.
Essential Fatty Acids
Essential Fatty Acids such as omega-3 oils are ‘essential’ because your body can’t make them and you have to obtain them from your food. Essential Fatty Acids are found in the skin of white fish but also in the flesh of oily fish such as fresh and tinned salmon, mackerel, sardines and fresh tuna. Advice for fish eaters is to have one portion of oily fish, and one portion of white fish per week.
Essential Fatty Acids can also be found in some plant oils such as flaxseed, rapeseed and soya but there is not as much in these oils as there is in fish and seafood.
Omega-3 fatty acids
Omega-3 fatty acids (omega-3s) are a type of polyunsaturated fat and have a carbon–carbon double bond located three carbons from the methyl end of the chain (see Figure 6). Omega-3 fatty acids, sometimes referred to as “n-3s,” are present in certain foods such as flaxseed and fish, as well as dietary supplements such as fish oil. Omega-3 fatty acids are especially beneficial to your health. Omega-3s play important roles in the body as components of the phospholipids that form the structures of cell membranes 30. There are different types of omega-3s: eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are found in fish and algae and have the most health benefits, while alpha-linolenic acid (ALA) comes from plants and is a less potent form of omega-3, although the body does convert ALA to EPA and DHA at low rates. Alpha-linolenic acid (ALA) contains 18 carbon atoms, whereas eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA) are considered “long-chain” omega-3s because EPA contains 20 carbons and DHA contains 22 41.
Docosahexaenoic acid (DHA), in particular, is especially high in the retina, brain, and sperm 33. In addition to their structural role in cell membranes, omega-3s (along with omega-6s) provide energy for the body and are used to form eicosanoids. Eicosanoids are signaling molecules that have similar chemical structures to the fatty acids from which they are derived; they have wide-ranging functions in the body’s cardiovascular, pulmonary, immune, and endocrine systems 31. Higher concentrations of EPA and DHA than arachidonic acid tip the eicosanoid balance toward less inflammatory activity 42.
Research has shown that a diet rich in omega-3 fatty acids may help to:
- Prevent and reduce symptoms of depression, ADHD, and bipolar disorder.
- Protect against memory loss and dementia.
- Reduce the risk of heart disease, stroke, and cancer.
- Ease arthritis, joint pain, and inflammatory skin conditions.
- Support a healthy pregnancy.
- Battle fatigue, sharpen your memory, and balance your mood.
Fish the best source of omega-3 (high in EPA and DHA):
- Anchovies
- Herring
- Salmon
- Mackerel
- Sardines
- Trout
- Tuna
- Mussels
- Oysters
- Halibut
Vegetarian sources of omega-3s (high in ALA):
- Algae such as seaweed (high in EPA and DHA)
- Eggs (small amounts of DHA)
- Flaxseeds and flaxseed oil
- Chia seeds
- Canola and soybean oil
- Walnuts
- Mayonnaise
- Edamame
- Beans (refried, kidney, etc.)
- Brussels sprouts
- Kale
- Spinach
Fish is a good source of protein and omega-3 fatty acids, which are good for your heart. Research has shown that omega-3 fatty acids can reduce your risk of heart disease and stroke. A 2020 Cochrane review 43 of 86 randomized controlled trials published between 1968 and 2019 found that 0.5 g/day to more than 5 g/day omega-3 fatty acids for 12 to 88 months in a total of 162,796 participants reduced serum triglyceride levels by about 15% and slightly decreased rates of cardiovascular mortality and coronary heart disease events. However, the omega-3 fatty acids supplements did not affect all-cause mortality, cardiovascular events, stroke, or arrhythmia. The authors of several earlier meta-analyses and systematic reviews, as well as a 2016 report from the Agency for Healthcare Research and Quality, concluded that omega-3 fatty acids supplements do not appear to significantly reduce the risk of most cardiovascular events 44. Many of these analyses 45, however, but not all 46, did find that omega-3s reduce the risk of cardiac death.
The American Heart Association recommends eating 2 servings of fish (particularly fatty fish) per week. A serving is 3.5 ounce (100 g) cooked, or about ¾ cup of flaked fish. Fatty fish like salmon, mackerel, herring, lake trout, sardines and albacore tuna are high in omega-3 fatty acids. For people with existing coronary heart disease, such as a recent heart attack (myocardial infarction), the American Heart Association recommends approximately 1 gram/day EPA plus DHA, preferably from oily fish; however, supplements could also be considered under the direction of a physician 47. The American Heart Association does not recommend omega-3 supplements for people who do not have a high cardiovascular disease risk.
While omega-3s are best obtained through food, there are many omega-3 and fish oil supplements available. A typical fish oil supplement provides about 1,000 mg fish oil, containing 180 mg EPA and 120 mg DHA, but doses vary widely 48. If you need to substantially lower your triglycerides, your doctor may recommend prescription fish oil, which has been concentrated to contain about 900 mg of EPA plus DHA per capsule. Cod liver oil supplements provide vitamin A and vitamin D in addition to omega-3s. For strict vegetarians or vegans, as well as obtaining ALA from food sources, look for capsules containing DHA and EPA extracted from algae, the original source of omega-3s for fish. Although seafood contains varying levels of methyl mercury (a toxic heavy metal) 49, omega-3 supplements have not been found to contain this contaminant because it is removed during processing and purification 50.
Some types of fish may contain high levels of mercury, PCBs (polychlorinated biphenyls), dioxins and other environmental contaminants. Levels of these substances are generally highest in older, larger, predatory fish and marine mammals.
The benefits and risks of eating fish vary depending on a person’s stage of life.
Children and pregnant women are advised by the U.S. Food and Drug Administration (FDA) to:
- Avoid eating those fish with the potential for the highest level of mercury contamination (such as shark, swordfish, king mackerel or tilefish).
- Eat a variety of fish and shellfish that are lower in mercury (such as canned light tuna, salmon, pollock, catfish).
- Check local advisories about the safety of fish caught by family and friends in local lakes, rivers and coastal areas.
For middle-aged and older men and postmenopausal women, the benefits far outweigh the potential risks when the amount of fish eaten is within the recommendations established by the FDA and Environmental Protection Agency.
Eating a variety of fish will help minimize any potentially adverse effects due to environmental pollutants. Five of the most commonly eaten fish or shellfish that are low in mercury are shrimp, canned light tuna, salmon, pollock, and catfish. Avoid eating shark, swordfish, king Mackerel, or tilefish because they contain high levels of mercury.
Cholesterol
Dietary fat plays a major role in your cholesterol levels. Cholesterol is a type of fat, a wax-like substance that your body needs to function properly that comes from foods such as eggs and is also found in your blood mostly made by your body in your liver. In and of itself, cholesterol isn’t bad. But when you get too much of it, it can have a negative impact on your health. The 2 main types of cholesterol are:
- “Good” cholesterol or HDL (high-density lipoprotein) cholesterol. “Good” HDL cholesterol has a positive effect by taking cholesterol from parts of the body where there’s too much of it to the liver, where it’s disposed of.
- “Bad” cholesterol or LDL (low-density lipoprotein) cholesterol.
High levels of LDL cholesterol (low-density lipoprotein or “bad” cholesterol) can increase your risk of heart disease. The key is to keep your LDL levels low and HDL high, which may protect against heart disease and stroke. High levels of LDL cholesterol (low-density lipoprotein or “bad” cholesterol) can clog arteries and low HDL (high-density lipoprotein or “good” cholesterol) can be a marker for increased cardiovascular risk. However, eating foods that contain any type of cholesterol won’t actually raise your body’s cholesterol levels. Rather than the amount of cholesterol you eat, the biggest influence on your cholesterol levels is the type of fats you consume. Eating saturated or trans fats is far more likely to give you high cholesterol. So instead of counting cholesterol, it’s important to focus on replacing bad fats with good fats.
LDL (bad) cholesterol
LDL (low-density lipoprotein) cholesterol is considered the “bad” cholesterol, because it contributes to fatty buildups in arteries (atherosclerosis). This narrows the arteries and increases the risk for heart attack, stroke and peripheral artery disease. Your body naturally produces all the LDL cholesterol you need. Eating foods containing saturated fats and trans fats causes your body to produce even more LDL — raising the level of “bad” cholesterol in your blood.
HDL (good) cholesterol
HDL (high-density lipoprotein) cholesterol can be thought of as the “good” cholesterol because a healthy level may protect against heart attack and stroke. HDL carries LDL (bad) cholesterol away from the arteries and back to the liver, where the LDL is broken down and passed from the body. But HDL cholesterol doesn’t completely eliminate LDL cholesterol. Only one-third to one-fourth of blood cholesterol is carried by HDL.
Trans fats
Avoid trans fat. Trans fats also known as trans fatty acids or “partially hydrogenated oils”, are created in an industrial process that adds hydrogen to liquid vegetable oils to make them more solid, so they ‘behave’ like a saturated fat. There are two broad types of trans fats found in foods: naturally-occurring and artificial trans fats. Naturally-occurring trans fats are produced in the gut of some animals and foods made from these animals (e.g., milk and meat products) may contain small quantities of these fats. Artificial trans fats (or trans fatty acids) are created in an industrial process that adds hydrogen to liquid vegetable oils to make them more solid.
Trans fats increase the levels of ‘bad’ LDL cholesterol and decreases the levels of ‘good’ HDL cholesterol in your body, which increases your risk of developing heart disease and stroke. Trans fats is also associated with a higher risk of developing type 2 diabetes. Trans fats can be found in many foods such as in butter, margarine (in small amounts), deep-fried and processed foods like doughnuts, cakes and pastries. Baked goods, such as pastries, pizza dough, frozen pizza, pie crust, cookies, biscuits, and crackers also can contain trans fats.
Since 2006, the FDA has required trans fat content to be listed on the Nutrition Facts panel of packaged foods. In recent years, many major national fast-food chains and casual-dining restaurant chains have announced they will no longer use trans fats to fry or deep-fry foods.
The American Heart Association recommends that adults who would benefit from lowering LDL cholesterol eliminate trans fat from their diet.
To find the amount of trans fats in a particular packaged food, look at the Nutrition Facts panel. Companies must list any measurable amount of trans fat (0.5 grams or more per serving) in a separate line in the “Total Fat” section of the panel, directly beneath the line for “Saturated Fat.” This means if a food package states 0 grams of trans fats, it might still have some trans fats if the amount per serving is less than 0.5 g. You can also spot trans fats by reading ingredient lists and looking for the ingredients referred to as “partially hydrogenated oils.”
Salt
Salt or sodium is a mineral that’s essential for life. Table salt is a combination of two minerals — about 40% sodium and 60% chloride. Salt or sodium is regulated by your kidneys, and it helps control your body’s fluid balance. It also helps send nerve impulses and affects muscle function. High levels of salt in your diet can increase blood pressure. High blood pressure is known as the “silent killer” because its symptoms are not always obvious. It’s one of the major risk factors for heart disease, the No. 1 killer worldwide. Ninety percent of American adults are expected to develop high blood pressure over their lifetimes. Because high blood pressure is an important risk factor for stroke, and strokes are detrimental to cognitive health, excessive salt intake is harmful for your brain health. There is a well-established relationship between consuming high levels of sodium and risk of stroke. In Japan, a public health education intervention in the 1960s showed the effectiveness of dietary interventions to reduce sodium intake. A 50% reduction in salt in the diet was associated with an 85% reduction in mortality caused by stroke.
Most of the salt that you eat is added to processed foods. More than 70% of the sodium you consume comes from packaged, prepared and restaurant foods. The rest of the sodium in the diet occurs naturally in food (about 15 percent) or is added when we’re cooking food or sitting down to eat (about 11 percent). Current recommendations from the Dietary Guidelines for Americans are to limit sodium intake to 2,300 milligrams (mg) a day, which amounts to about one teaspoon of salt. The American Heart Association recommends an ideal limit of no more than 1,500 mg per day for most adults. On average, Americans eat more than 3,400 milligrams of sodium each day — much more than the American Heart Association and other health organizations recommend. Because the average American eats so much excess sodium, even cutting back by 1,000 milligrams a day can significantly improve blood pressure and heart health. One estimate suggested that if the U.S. population dropped its sodium intake to 1,500 mg/day (1/2 teaspoon salt), overall blood pressure could decrease by 25.6%, with an estimated $26.2 billion in health care savings. Another estimate projected that achieving this goal would reduce cardiovascular disease deaths by anywhere from 500,000 to nearly 1.2 million over the next decade.
Here are the approximate amounts of sodium in a given amount of salt:
- 1/4 teaspoon salt = 575 mg sodium
- 1/2 teaspoon salt = 1,150 mg sodium
- 3/4 teaspoon salt = 1,725 mg sodium
- 1 teaspoon salt = 2,300 mg sodium
The body needs only a small amount of sodium (less than 500 milligrams per day) to function properly. That’s a mere smidgen — the amount in less than ¼ teaspoon. Very few people come close to eating less than that amount. Plus, healthy kidneys are great at retaining the sodium that your body needs.
What and How much Should you Eat?
For an average adult male who requires 2000 Calories (8368 kilojoules)
Note: 1 Calorie (kilocalories) = 4.184 kilojoules (kJ)
Because how much calories you eat and what food groups you need are highly dependent on your age, sex, and your level of physical activity. For the most accurate way calculate how much food and calories you need to eat per day from each food group >>> Go to the United States Department of Agriculture’s MyPlate Daily Checklist 2 >>> https://www.choosemyplate.gov/myplate-daily-checklist-input
Simply enter your age, sex, height, weight, and physical activity level to get a plan that’s right for you. The MyPlate Daily Checklist shows your food group targets – what and how much to eat within your calorie allowance.
An important part of maintaining a healthy weight and healthy lifestyle is to maintain energy balance is the amount of ENERGY OUT (physical activity) that you do. People who are more physically active burn more calories than those who are not as physically active.
The same amount of ENERGY IN (calories consumed) and ENERGY OUT (calories burned) over time = weight stays the same
- More IN than OUT over time = weight gain
- More OUT than IN over time = weight loss
- To lose weight, most people need to reduce the number of calories they get from food and beverages (energy IN) and increase their physical activity (energy OUT).
- For a weight loss of 1–1 ½ pounds per week, daily intake should be reduced by 500 to 750 calories 51. In general:
- Eating plans that contain 1,200–1,500 calories each day will help most women lose weight safely.
- Eating plans that contain 1,500–1,800 calories each day are suitable for men and for women who weigh more or who exercise regularly.
Table 2. Estimated Calorie Requirements (in kilocalories) for Each Gender and Age Group at Three Levels of Physical Activity.
| Gender | Age (years) | Activity Level | ||
| Sedentary | Moderately Active | Active | ||
| Child | 02/03/21 | 1000 | 1,000 – 1,400 | 1,000 – 1,400 |
| Female | 4 – 8 | 1200 | 1,400 – 1,600 | 1,400 – 1,800 |
| Female | 01/09/13 | 1600 | 1,600 – 2,000 | 1,800 – 2,000 |
| Female | 14-18 | 1800 | 2000 | 2400 |
| Female | 19-30 | 2000 | 2,000 – 2,200 | 2400 |
| Female | 31-50 | 1800 | 2000 | 2200 |
| Female | 51 | 1600 | 1800 | 2,000 – 2,200 |
| Male | 04/08/21 | 1400 | 1,400 – 1,600 | 1,600 – 2,000 |
| Male | 01/09/13 | 1800 | 1,800 – 2,200 | 2,000 – 2,600 |
| Male | 14-18 | 2200 | 2,400 – 2,800 | 2,800 – 3,200 |
| Male | 19-30 | 2400 | 2,600 – 2,800 | 3000 |
| Male | 31-50 | 2200 | 2,400 – 2,600 | 2,800 – 3,000 |
| Male | 51 | 2000 | 2,200 – 2,400 | 2,400 – 2,800 |
Footnotes:
- These levels are based on Estimated Energy Requirements from the IOM Dietary Reference Intakes macronutrients report, 2002, calculated by gender, age, and activity level for reference-sized individuals. “Reference size,” as determined by IOM, is based on median height and weight for ages up to age 18 years of age and median height and weight for that height to give a BMI of 21.5 for adult females and 22.5 for adult males.
- Sedentary means a lifestyle that includes only the light physical activity associated with typical day-to-day life.
- Moderately active means a lifestyle that includes physical activity equivalent to walking about 1.5 to 3 miles per day at 3 to 4 miles per hour, in addition to the light physical activity associated with typical day-to-day life.
- Active means a lifestyle that includes physical activity equivalent to walking more than 3 miles per day at 3 to 4 miles per hour, in addition to the light physical activity associated with typical day-to-day life.
- The calorie ranges shown are to accommodate needs of different ages within the group. For children and adolescents, more calories are needed at older ages. For adults, fewer calories are needed at older ages.
- Note: 1 Calorie (kilocalories) = 4.184 kilojoules (kJ)
- For an average adult male who requires 2000 Calories = 8368 kilojoules
Healthy Eating Plan
A healthy eating plan gives your body the nutrients it needs every day while staying within your daily calorie goal for weight loss. A healthy eating plan also will lower your risk for heart disease and other health conditions.
A healthy eating plan 51:
- Emphasizes vegetables, fruits, whole grains, and fat-free or low-fat dairy products
- Includes lean meats, poultry, fish, beans, eggs, and nuts
- Limits saturated and trans fats, sodium, and added sugars
- Controls portion sizes
How to Eat Healthy
Follow these steps to help you eat healthy:
- Eat the right types of food by following Healthy Food Guide. Choose a variety of foods from each of the four food groups.
- Eat the recommended amount of food for your age, sex, and activity level.
- Read food labels to compare and choose healthier foods when shopping. The Nutrition Facts table and the Percent Daily Value can help you make better choices.
- Limit foods and drinks that are high in calories, fat, sugar, and sodium.
A healthy eating pattern limits:
- Saturated fats and trans fats, added sugars, and sodium
- Consume less than 10 percent of calories per day from added sugars
- Consume less than 10 percent of calories per day from saturated fats
- Consume less than 2,300 milligrams (mg) per day of sodium
- If alcohol is consumed, it should be consumed in moderation—up to one drink per day for women and up to two drinks per day for men—and only by adults of legal drinking age.
Key Recommendations that are quantitative are provided for several components of the diet that should be limited. These components are of particular public health concern in the United States, and the specified limits can help individuals achieve healthy eating patterns within calorie limits.
- Vegetables
- Dark-green vegetables: All fresh, frozen, and canned dark-green leafy vegetables and broccoli, cooked or raw: for example, broccoli; spinach; romaine; kale; collard, turnip, and mustard greens.
- Red and orange vegetables: All fresh, frozen, and canned red and orange vegetables or juice, cooked or raw: for example, tomatoes, tomato juice, red peppers, carrots, sweet potatoes, winter squash, and pumpkin.
- Legumes (beans and peas): All cooked from dry or canned beans and peas: for example, kidney beans, white beans, black beans, lentils, chickpeas, pinto beans, split peas, and edamame (green soybeans). Does not include green beans or green peas.
- Starchy vegetables: All fresh, frozen, and canned starchy vegetables: for example, white potatoes, corn, green peas, green lima beans, plantains, and cassava.
- Other vegetables: All other fresh, frozen, and canned vegetables, cooked or raw: for example, iceberg lettuce, green beans, onions, cucumbers, cabbage, celery, zucchini, mushrooms, and green peppers.
- Fruits
- All fresh, frozen, canned, and dried fruits and fruit juices: for example, oranges and orange juice, apples and apple juice, bananas, grapes, melons, berries, and raisins.
- Grains
- Whole grains: All whole-grain products and whole grains used as ingredients: for example, whole-wheat bread, whole-grain cereals and crackers, oatmeal, quinoa, popcorn, and brown rice.
- Refined grains: All refined-grain products and refined grains used as ingredients: for example, white breads, refined grain cereals and crackers, pasta, and white rice. Refined grain choices should be enriched.
- Dairy
- All milk, including lactose-free and lactose-reduced products and fortified soy beverages (soymilk), yogurt, frozen yogurt, dairy desserts, and cheeses. Most choices should be fat-free or low-fat. Cream, sour cream, and cream cheese are not included due to their low calcium content.
- Protein Foods
- All seafood, meats, poultry, eggs, soy products, nuts, and seeds. Meats and poultry should be lean or low-fat and nuts should be unsalted. Legumes (beans and peas) can be considered part of this group as well as the vegetable group, but should be counted in one group only.
Evidence shows that healthy eating patterns are associated with positive health outcomes. And the evidence base for associations between eating patterns and specific health outcomes continues to grow. Strong evidence shows that healthy eating patterns are associated with a reduced risk of cardiovascular disease. Moderate evidence indicates that healthy eating patterns also are associated with a reduced risk of type 2 diabetes, certain types of cancers (such as colorectal and postmenopausal breast cancers), overweight, and obesity. Emerging evidence also suggests that relationships may exist between eating patterns and some neuro-cognitive disorders and congenital anomalies.
Within this body of evidence, higher intakes of vegetables and fruits consistently have been identified as characteristics of healthy eating patterns; whole grains have been identified as well, although with slightly less consistency. Other characteristics of healthy eating patterns have been identified with less consistency and include fat-free or low-fat dairy, seafood, legumes, and nuts.
Lower intakes of meats, including processed meats; processed poultry; sugar-sweetened foods, particularly beverages; and refined grains have often been identified as characteristics of healthy eating patterns.
A) Vegetables
Healthy intake: Healthy eating patterns include a variety of vegetables from all of the five vegetable subgroups—dark green, red and orange, legumes (beans and peas), starchy, and other. These include all fresh, frozen, canned, and dried options in cooked or raw forms, including vegetable juices. The recommended amount of vegetables in the Healthy U.S.-Style Eating Pattern at the 2,000-calorie level is 2½ cup-equivalents of vegetables per day. In addition, weekly amounts from each vegetable subgroup are recommended to ensure variety and meet nutrient needs.
Key nutrient contributions: Vegetables are important sources of many nutrients, including dietary fiber, potassium, vitamin A, vitamin C, vitamin K, copper, magnesium, vitamin E, vitamin B6, folate, iron, manganese, thiamin, niacin, and choline. Each of the vegetable subgroups contributes different combinations of nutrients, making it important for individuals to consume vegetables from all the subgroups. For example, dark-green vegetables provide the most vitamin K, red and orange vegetables the most vitamin A, legumes the most dietary fiber, and starchy vegetables the most potassium. Vegetables in the “other” vegetable subgroup provide a wide range of nutrients in varying amounts.
Considerations: To provide all of the nutrients and potential health benefits that vary across different types of vegetables, the Healthy U.S.-Style Eating Pattern includes weekly recommendations for each subgroup. Vegetable choices over time should vary and include many different vegetables. Vegetables should be consumed in a nutrient-dense form, with limited additions such as salt, butter, or creamy sauces. When selecting frozen or canned vegetables, choose those lower in sodium.
B) Fruits
Healthy intake: Healthy eating patterns include fruits, especially whole fruits. The fruits food group includes whole fruits and 100% fruit juice. Whole fruits include fresh, canned, frozen, and dried forms. The recommended amount of fruits in the Healthy U.S.-Style Eating Pattern at the 2,000-calorie level is 2 cup-equivalents per day. One cup of 100% fruit juice counts as 1 cup of fruit. Although fruit juice can be part of healthy eating patterns, it is lower than whole fruit in dietary fiber and when consumed in excess can contribute extra calories. Therefore, at least half of the recommended amount of fruits should come from whole fruits. When juices are consumed, they should be 100% juice, without added sugars. Also, when selecting canned fruit, choose options that are lowest in added sugars. One-half cup of dried fruit counts as one cup-equivalent of fruit. Similar to juice, when consumed in excess, dried fruits can contribute extra calories.
Key nutrient contributions: Among the many nutrients fruits provide are dietary fiber, potassium, and vitamin C.
Considerations: Juices may be partially fruit juice, and only the proportion that is 100% fruit juice counts (e.g., 1 cup of juice that is 50% juice counts as ½ cup of fruit juice). The remainder of the product may contain added sugars. Sweetened juice products with minimal juice content, such as juice drinks, are considered to be sugar-sweetened beverages rather than fruit juice because they are primarily composed of water with added sugars (see the Added Sugars section). The percent of juice in a beverage may be found on the package label, such as “contains 25% juice” or “100% fruit juice.” The amounts of fruit juice allowed in the US Department of Agriculture (USDA) Food Patterns for young children align with the recommendation from the American Academy of Pediatrics that young children consume no more than 4 to 6 fluid ounces of 100% fruit juice per day. Fruits with small amounts of added sugars can be accommodated in the diet as long as calories from added sugars do not exceed 10 percent per day and total calorie intake remains within limits.
C) Grains
Healthy Intake: Healthy eating patterns include whole grains and limit the intake of refined grains and products made with refined grains, especially those high in saturated fats, added sugars, and/or sodium, such as cookies, cakes, and some snack foods. The grains food group includes grains as single foods (e.g., rice, oatmeal, and popcorn), as well as products that include grains as an ingredient (e.g., breads, cereals, crackers, and pasta). Grains are either whole or refined. Whole grains (e.g., brown rice, quinoa, and oats) contain the entire kernel, including the endosperm, bran, and germ. Refined grains differ from whole grains in that the grains have been processed to remove the bran and germ, which removes dietary fiber, iron, and other nutrients. The recommended amount of grains in the Healthy U.S.-Style Eating Pattern at the 2,000-calorie level is 6 ounce-equivalents per day. At least half of this amount should be whole grains.
Key nutrient contributions: Whole grains are a source of nutrients, such as dietary fiber, iron, zinc, manganese, folate, magnesium, copper, thiamin, niacin, vitamin B6, phosphorus, selenium, riboflavin, and vitamin A. Whole grains vary in their dietary fiber content. Most refined grains are enriched, a process that adds back iron and four B vitamins (thiamin, riboflavin, niacin, and folic acid). Because of this process, the term “enriched grains” is often used to describe these refined grains.
Considerations: Individuals who eat refined grains should choose enriched grains. Those who consume all of their grains as whole grains should include some grains, such as some whole-grain ready-to-eat breakfast cereals, that have been fortified with folic acid. This is particularly important for women who are or are capable of becoming pregnant, as folic acid fortification in the United States has been successful in reducing the incidence of neural tube defects during fetal development. Although grain products that are high in added sugars and saturated fats, such as cookies, cakes, and some snack foods, should be limited, as discussed in the Added Sugars and Saturated Fats sections below, grains with some added sugars and saturated fats can fit within healthy eating patterns.
D) Dairy
Healthy intake: Healthy eating patterns include fat-free and low-fat (1%) dairy, including milk, yogurt, cheese, or fortified soy beverages (commonly known as “soymilk”). Soy beverages fortified with calcium, vitamin A, and vitamin D, are included as part of the dairy group because they are similar to milk based on nutrient composition and in their use in meals. Other products sold as “milks” but made from plants (e.g., almond, rice, coconut, and hemp “milks”) may contain calcium and be consumed as a source of calcium, but they are not included as part of the dairy group because their overall nutritional content is not similar to dairy milk and fortified soy beverages (soymilk). The recommended amounts of dairy in the Healthy U.S.-Style Pattern are based on age rather than calorie level and are 2 cup-equivalents per day for children ages 2 to 3 years, 2½ cup-equivalents per day for children ages 4 to 8 years, and 3 cup-equivalents per day for adolescents ages 9 to 18 years and for adults.
Key nutrient contributions: The dairy group contributes many nutrients, including calcium, phosphorus, vitamin A, vitamin D (in products fortified with vitamin D), riboflavin, vitamin B12, protein, potassium, zinc, choline, magnesium, and selenium.
Considerations: Fat-free and low-fat (1%) dairy products provide the same nutrients but less fat (and thus, fewer calories) than higher fat options, such as 2% and whole milk and regular cheese. Fat-free or low-fat milk and yogurt, in comparison to cheese, contain less saturated fats and sodium and more potassium, vitamin A, and vitamin D. Thus, increasing the proportion of dairy intake that is fat-free or low-fat milk or yogurt and decreasing the proportion that is cheese would decrease saturated fats and sodium and increase potassium, vitamin A, and vitamin D provided from the dairy group. Individuals who are lactose intolerant can choose low-lactose and lactose-free dairy products. Those who are unable or choose not to consume dairy products should consume foods that provide the range of nutrients generally obtained from dairy, including protein, calcium, potassium, magnesium, vitamin D, and vitamin A (e.g., fortified soy beverages [soymilk]). Additional sources of potassium, calcium, and vitamin D.
E) Protein Foods
Healthy intake: Healthy eating patterns include a variety of protein foods in nutrient-dense forms. The protein foods group comprises a broad group of foods from both animal and plant sources and includes several subgroups: seafood; meats, poultry, and eggs; and nuts, seeds, and soy products. Legumes (beans and peas) may also be considered part of the protein foods group as well as the vegetables group. Protein also is found in some foods from other food groups (e.g., dairy). The recommendation for protein foods in the Healthy U.S.-Style Eating Pattern at the 2,000-calorie level is 5½ ounce-equivalents of protein foods per day.
Key nutrient contributions: Protein foods are important sources of nutrients in addition to protein, including B vitamins (e.g., niacin, vitamin B12, vitamin B6, and riboflavin), selenium, choline, phosphorus, zinc, copper, vitamin D, and vitamin E). Nutrients provided by various types of protein foods differ. For example, meats provide the most zinc, while poultry provides the most niacin. Meats, poultry, and seafood provide heme iron, which is more bioavailable than the non-heme iron found in plant sources. Heme iron is especially important for young children and women who are capable of becoming pregnant or who are pregnant. Seafood provides the most vitamin B12 and vitamin D, in addition to almost all of the polyunsaturated omega-3 fatty acids, eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA), in the Patterns. Eggs provide the most choline, and nuts and seeds provide the most vitamin E. Soy products are a source of copper, manganese, and iron, as are legumes.
Considerations: For balance and flexibility within the food group, the Healthy U.S.-Style Eating Pattern includes weekly recommendations for the subgroups: seafood; meats, poultry, and eggs; and nuts, seeds, and soy products. A specific recommendation for at least 8 ounce-equivalents of seafood per week also is included for the 2,000-calorie level. One-half ounce of nuts or seeds counts as 1 ounce-equivalent of protein foods, and because they are high in calories, they should be eaten in small portions and used to replace other protein foods rather than being added to the diet. When selecting protein foods, nuts and seeds should be unsalted, and meats and poultry should be consumed in lean forms. Processed meats and processed poultry are sources of sodium and saturated fats, and intake of these products can be accommodated as long as sodium, saturated fats, added sugars, and total calories are within limits in the resulting eating pattern. The inclusion of protein foods from plants allows vegetarian options to be accommodated.
F) Oils
Healthy intake: Oils are fats that contain a high percentage of monounsaturated and polyunsaturated fats and are liquid at room temperature. Although they are not a food group, oils are emphasized as part of healthy eating patterns because they are the major source of essential fatty acids and vitamin E. Commonly consumed oils extracted from plants include canola, corn, olive, peanut, safflower, soybean, and sunflower oils. Oils also are naturally present in nuts, seeds, seafood, olives, and avocados. The fat in some tropical plants, such as coconut oil, palm kernel oil, and palm oil, are not included in the oils category because they do not resemble other oils in their composition. Specifically, they contain a higher percentage of saturated fats than other oils. The recommendation for oils in the Healthy U.S.-Style Eating Pattern at the 2,000-calorie level is 27 g (about 5 teaspoons) per day.
Key nutrient contributions: Oils provide essential fatty acids and vitamin E.
Considerations: Oils are part of healthy eating patterns, but because they are a concentrated source of calories, the amount consumed should be within the AMDR for total fats without exceeding calorie limits. Oils should replace solid fats rather than being added to the diet. More information on types of fats is provided in the Dietary Fats and information on the relationship between dietary fats and health is discussed in the Saturated Fats, Trans Fats, and Cholesterol section, below.
G) Saturated Fats
Healthy intake: Intake of saturated fats should be limited to less than 10 percent of calories per day by replacing them with unsaturated fats and while keeping total dietary fats within the age-appropriate AMDR. The human body uses some saturated fats for physiological and structural functions, but it makes more than enough to meet those needs. Individuals 2 years and older therefore have no dietary requirement for saturated fats.
Strong and consistent evidence shows that replacing saturated fats with unsaturated fats, especially polyunsaturated fats, is associated with reduced blood levels of total cholesterol and of low-density lipoprotein-cholesterol (LDL-cholesterol). Additionally, strong and consistent evidence shows that replacing saturated fats with polyunsaturated fats is associated with a reduced risk of CVD events (heart attacks) and CVD-related deaths.
Some evidence has shown that replacing saturated fats with plant sources of monounsaturated fats, such as olive oil and nuts, may be associated with a reduced risk of CVD. However, the evidence base for monounsaturated fats is not as strong as the evidence base for replacement with polyunsaturated fats. Evidence has also shown that replacing saturated fats with carbohydrates reduces blood levels of total and LDL-cholesterol, but increases blood levels of triglycerides and reduces high-density lipoprotein-cholesterol (HDL-cholesterol). Replacing total fat or saturated fats with carbohydrates is not associated with reduced risk of CVD. Additional research is needed to determine whether this relationship is consistent across categories of carbohydrates (e.g., whole versus refined grains; intrinsic versus added sugars), as they may have different associations with various health outcomes. Therefore, saturated fats in the diet should be replaced with polyunsaturated and monounsaturated fats.
Considerations: The main sources of saturated fats in the U.S. diet include mixed dishes containing cheese, meat, or both, such as burgers, sandwiches, and tacos; pizza; rice, pasta, and grain dishes; and meat, poultry, and seafood dishes. Although some saturated fats are inherent in foods, others are added. Healthy eating patterns can accommodate nutrient-dense foods with small amounts of saturated fats, as long as calories from saturated fats do not exceed 10 percent per day, intake of total fats remains within the AMDR, and total calorie intake remains within limits. When possible, foods high in saturated fats should be replaced with foods high in unsaturated fats, and other choices to reduce solid fats should be made.
H) Trans Fats
Individuals should limit intake of trans fats to as low as possible by limiting foods that contain synthetic sources of trans fats, such as partially hydrogenated oils in margarines, and by limiting other solid fats. A number of studies have observed an association between increased intake of trans fats and increased risk of CVD. This increased risk is due, in part, to its LDL-cholesterol-raising effect.
Trans fats occur naturally in some foods and also are produced in a process called hydrogenation. Hydrogenation is used by food manufacturers to make products containing unsaturated fatty acids solid at room temperature (i.e., more saturated) and therefore more resistant to becoming spoiled or rancid. Partial hydrogenation means that some, but not all, unsaturated fatty acids are converted to saturated fatty acids; some of the unsaturated fatty acids are changed from a cis to trans configuration. Trans fatty acids produced this way are referred to as “artificial” or “industrially produced” trans fatty acids. Artificial trans fatty acids are found in the partially hydrogenated oils used in some margarines, snack foods, and prepared desserts as a replacement for saturated fatty acids. Although food manufacturers and restaurants have reduced the amounts of artificial trans fats in many foods in recent years, these fats can still be found in some processed foods, such as some desserts, microwave popcorn, frozen pizza, margarines, and coffee creamers.
Naturally occurring trans fats, known as “natural” or “ruminant” trans fats, are produced by ruminant animals. Natural trans fats are present in small quantities in dairy products and meats, and consuming fat-free or low-fat dairy products and lean meats and poultry will reduce the intake of natural trans fats from these foods. Because natural trans fats are present in dairy products and meats in only small quantities and these foods can be important sources of nutrients, these foods do not need to be eliminated from the diet.
I) Dietary Cholesterol
The body uses cholesterol for physiological and structural functions but makes more than enough for these purposes. Therefore, people do not need to obtain cholesterol through foods.
The Key Recommendation from the 2010 Dietary Guidelines to limit consumption of dietary cholesterol to 300 mg per day is not included in the 2015 edition, but this change does not suggest that dietary cholesterol is no longer important to consider when building healthy eating patterns. As recommended by the IOM, individuals should eat as little dietary cholesterol as possible while consuming a healthy eating pattern. In general, foods that are higher in dietary cholesterol, such as fatty meats and high-fat dairy products, are also higher in saturated fats. The USDA Food Patterns are limited in saturated fats, and because of the commonality of food sources of saturated fats and dietary cholesterol, the Patterns are also low in dietary cholesterol. For example, the Healthy U.S.-Style Eating Pattern contains approximately 100 to 300 mg of cholesterol across the 12 calorie levels. Current average intake of dietary cholesterol among those 1 year and older in the United States is approximately 270 mg per day.
Strong evidence from mostly prospective cohort studies but also randomized controlled trials has shown that eating patterns that include lower intake of dietary cholesterol are associated with reduced risk of CVD, and moderate evidence indicates that these eating patterns are associated with reduced risk of obesity. As described earlier, eating patterns consist of multiple, interacting food components and the relationships to health exist for the overall eating pattern, not necessarily to an isolated aspect of the diet. More research is needed regarding the dose-response relationship between dietary cholesterol and blood cholesterol levels. Adequate evidence is not available for a quantitative limit for dietary cholesterol specific to the Dietary Guidelines.
Dietary cholesterol is found only in animal foods such as egg yolk, dairy products, shellfish, meats, and poultry. A few foods, notably egg yolks and some shellfish, are higher in dietary cholesterol but not saturated fats. Eggs and shellfish can be consumed along with a variety of other choices within and across the subgroup recommendations of the protein foods group.
J) Sodium
Healthy intake: The scientific consensus from expert bodies, such as the IOM, the American Heart Association, and Dietary Guidelines Advisory Committees, is that average sodium intake, which is currently 3,440 mg per day, is too high and should be reduced. Healthy eating patterns limit sodium to less than 2,300 mg per day for adults and children ages 14 years and older and to the age- and sex-appropriate Tolerable Upper Intake Levels (UL) of sodium for children younger than 14 years. Sodium is an essential nutrient and is needed by the body in relatively small quantities, provided that substantial sweating does not occur. Sodium is primarily consumed as salt (sodium chloride).
The limits for sodium are the age- and sex-appropriate ULs. The UL is the highest daily nutrient intake level that is likely to pose no risk of adverse health effects to almost all individuals in the general population. The recommendation for adults and children ages 14 years and older to limit sodium intake to less than 2,300 mg per day is based on evidence showing a linear dose-response relationship between increased sodium intake and increased blood pressure in adults. In addition, moderate evidence suggests an association between increased sodium intake and increased risk of CVD in adults. However, this evidence is not as consistent as the evidence on blood pressure, a surrogate indicator of CVD risk.
Calorie intake is highly associated with sodium intake (i.e., the more foods and beverages people consume, the more sodium they tend to consume). Because children have lower calorie needs than adults, the IOM established lower ULs for children younger than 14 years of age based on median intake of calories. Similar to adults, moderate evidence also indicates that the linear dose-response relationship between sodium intake and blood pressure is found in children as well.
Adults with prehypertension and hypertension would particularly benefit from blood pressure lowering. For these individuals, further reduction to 1,500 mg per day can result in even greater blood pressure reduction. Because of the linear dose-response relationship between sodium intake and blood pressure, every incremental decrease in sodium intake that moves toward recommended limits is encouraged. Even without reaching the limits for sodium intake, strong evidence indicates that reductions in sodium intake can lower blood pressure among people with prehypertension and hypertension. Further, strong evidence has demonstrated that adults who would benefit from blood pressure lowering should combine the Dietary Approaches to Stop Hypertension (DASH) dietary pattern with lower sodium intake.
The DASH Eating Plan is high in vegetables, fruits, low-fat dairy products, whole grains, poultry, fish, beans, and nuts and is low in sweets, sugar-sweetened beverages, and red meats. It is low in saturated fats and rich in potassium, calcium, and magnesium, as well as dietary fiber and protein. It also is lower in sodium than the typical American diet, and includes menus with two levels of sodium, 2,300 and 1,500 mg per day.
Considerations: As a food ingredient, sodium has multiple uses, such as in curing meat, baking, thickening, enhancing flavor (including the flavor of other ingredients), as a preservative, and in retaining moisture. For example, some fresh meats have sodium solutions added to help retain moisture in cooking. Sodium is found in foods across the food supply, including mixed dishes such as burgers, sandwiches, and tacos; rice, pasta, and grain dishes; pizza; meat, poultry, and seafood dishes; and soups. Multiple strategies should be implemented to reduce sodium intake to the recommended limits.
Healthy Eating on a Budget
- PLAN
+ Know how much money you have to spend on food.
+ Before you head to the grocery store, plan your meals for the week. Include meals like stews, casseroles, or stir-fries, which “stretch” expensive items into more portions. Check to see what foods you already have and make a list for what you need to buy.
+ Plan meals and snacks for the week according to an established budget.
+ Find quick and easy recipes online.
+ Include meals that will “stretch” expensive food items (stews, casseroles, stir‐fried dishes).
+ Make a grocery list.
+ Get the best price. Check the local newspaper, online, and at the store for sales and coupons. Ask about a loyalty card for extra savings at stores where you shop. Look for specials or sales on meat and seafood — often the most expensive items on your list.
+ Check for sales and coupons in the local paper or online and consider discount stores.
+ Read the sales flyer. Sales flyers are usually released mid-week and can be found at the store’s entrance, in the newspaper, or on their website.
+ Ask about a loyalty card at your grocery store.
+ Eat before you shop. Grocery shopping hungry can lead to impulse buying and unhealthy food choices.
- PURCHASE
+ Eat before you shop. Grocery shopping hungry can lead to impulse buying and unhealthy food choices.
+ Buy groceries when you are not hungry and when you are not too rushed.
+ Use coupons – but only for items that you know you’ll use.
+ Stick to the grocery list and stay out of the aisles that don’t contain items on your list.
+ Buy store brands if cheaper.
+ Stores often stock the priciest items at eye level. You can save big by looking at the upper and lower shelves too.
+ Buy in bulk. It is almost always cheaper to buy foods in bulk. Smart choices are family packs of chicken, steak, or fish and larger bags of potatoes and frozen vegetables. Before you shop, remember to check if you have enough freezer space.
+ Buy only the amounts of fresh foods you can use before it spoils.
+ Find and compare unit prices listed on shelves to get the best price.
+ Choose fresh fruits and vegetables in season; buy canned vegetables with less salt.
+ Convenience foods like frozen dinners, pre-cut vegetables, and instant rice, oatmeal, or grits will cost you more than if you were to make them from scratch. Take the time to prepare your own — and save!
+ Certain foods are typically low-cost options all year round. Try beans for a less expensive protein food. For vegetables, buy carrots, greens, or potatoes. As for fruits, apples and bananas are good choices.
+ Cook once… eat all week! Prepare a large batch of favorite recipes on your day off (double or triple the recipe). Freeze in individual containers. Use them throughout the week and you won’t have to spend money on take-out meals.
+ Spice up your leftovers — use them in new ways. For example, try leftover chicken in a stir-fry or over a garden salad, or to make chicken chili. Remember, throwing away food is throwing away your money!
+ Eating out. Restaurants can be expensive. Save money by getting the early bird special, going out for lunch instead of dinner, or looking for “2 for 1” deals. Stick to water instead of ordering other beverages, which add to the bill.
- American Heart Association – Suggested Servings from Each Food Group – https://healthyforgood.heart.org/eat-smart/articles/suggested-servings-from-each-food-group
- https://www.choosemyplate.gov/myplate-daily-checklist-input
- Cochrane Review 4 June 2013 – Increased fruit and vegetable intake to prevent cardiovascular disease – http://www.cochrane.org/CD009874/VASC_increased-fruit-and-vegetable-intake-to-prevent-cardiovascular-disease
- WHO. Diet, nutrition and the prevention of chronic diseases. Report of a Joint FAO, WHO Expert Consultation. WHO Technical Report Series. Geneva: World Helath Organization; 2003.
- Aune D, Giovannucci E, Boffetta P, Fadnes LT, Keum N, Norat T, Greenwood DC, Riboli E, Vatten LJ, Tonstad S. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality—a systematic review and dose-response meta-analysis of prospective studies. Int J Epidemiol. 2017;46(3):1029–1056. doi: 10.1093/ije/dyw319
- Davis B.A., Prall B.C. The challenges of incorporation of omega-3 fatty acids into ration components and their prevalence in garrison feeding. Military medicine. 2014;179:162–167. doi: 10.7205/MILMED-D-14-00172
- Bailes J.E., Patel V. The potential for DHA to mitigate mild traumatic brain injury. Mil. Med. 2014;179:112–116. doi: 10.7205/MILMED-D-14-00139
- Michael I McBurney, Nathan L Tintle, Ramachandran S Vasan, Aleix Sala-Vila, William S Harris, Using an erythrocyte fatty acid fingerprint to predict risk of all-cause mortality: the Framingham Offspring Cohort, The American Journal of Clinical Nutrition, 2021;, nqab195, https://doi.org/10.1093/ajcn/nqab195
- Fish and Omega-3 Fatty Acids. https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/fats/fish-and-omega-3-fatty-acids
- Devore, E. E., Kang, J. H., Breteler, M. M., & Grodstein, F. (2012). Dietary intakes of berries and flavonoids in relation to cognitive decline. Annals of neurology, 72(1), 135–143. https://doi.org/10.1002/ana.23594
- Mink PJ, Scrafford CG, Barraj LM, Harnack L, Hong CP, Nettleton JA, Jacobs DR., Jr Flavonoid intake and cardiovascular disease mortality: a prospective study in postmenopausal women. Am J Clin Nutr. 2007;85(3):895–909. doi: 10.1093/ajcn/85.3.895
- Appel et al. Reducing Sodium Intake in Children: A Public Health Investment. Journal of Clinical Hypertension. 2015:1–6.
- Rosner et al. Childhood blood pressure trends and risk factors for high blood pressure: The NHANES experience 1998-2008. Hypertension. 2013;62:247-254.
- Appel et al. The importance of population-wide sodium reduction as a means to prevent cardiovascular disease and stroke: A call to action from the American Heart Association. Circulation. 2011, 15;123(10):1138-43.
- Whelton et al. Sodium, blood pressure, and cardiovascular disease: Further evidence supporting the American Heart Association sodium reduction recommendations. Circulation. 2012;126:2880-2889 4/14/2015
- Statement from Secretary Vilsack on New Data Showing the Vast Majority of Schools Now Meet the Updated Meals Standards. USDA. May 6, 2015. Accessed online at http://www.fns.usda.gov/school-meals/school-meal-certification-data
- National Alliance for Nutrition and Activity. Mission: Possible Companies Can Meet USDA’s New Sodium Limits for School Meals. Accessed online 8/14/2014: http://cspinet.org/new/pdf/NANA%20 Sodium%20products%20that%20meet%20new%20guidelines%20oct%2014.pdf
- Antman et al. Stakeholder discussion to reduce population-wide sodium intake and decrease sodium in the food supply: A conference report from the American Heart Association sodium conference 2013 planning group. Circulation. 2014.
- Agarwal et al. Sodium Intake Status in United States and Potential Reduction Modeling: an NHANES 2007-2010 analysis. Food Science and Nutrition. 2015. DOI: 10.1002/ fsn3.248
- IOM. 2010. Strategies to Reduce Sodium Intake in the United States. Washington, DC: The National Academies Press
- Cochrane Review 18 December 2014 – Reduced dietary salt for the prevention of cardiovascular disease – http://www.cochrane.org/CD009217/VASC_reduced-dietary-salt-for-the-prevention-of-cardiovascular-disease
- https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2015-2020. https://health.gov/sites/default/files/2019-09/2015-2020_Dietary_Guidelines.pdf
- J Sports Sci Med. 2004 Sep; 3(3): 118–130. International Society of Sports Nutrition Symposium, June 18-19, 2005, Las Vegas NV, USA – Symposium – Macronutrient Utilization During Exercise: Implications For Performance And Supplementation. Protein – Which is Best ? https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3905294
- The National Kidney Disease Education Program. Protein – tips for people with chronic kidney disease. https://www.niddk.nih.gov/health-information/health-communication-programs/nkdep/a-z/nutrition-protein/Documents/nutrition-protein-508.pdf
- Agriculture, U.D.o., USDA Nutrient Database for Standard Reference, Release 14. 2005.
- The Vegetarian Society. Protein. https://www.vegsoc.org/facts/protein
- The Skinny on Fats. https://www.heart.org/en/health-topics/cholesterol/prevention-and-treatment-of-high-cholesterol-hyperlipidemia/the-skinny-on-fats
- Jakobsen, M.U., et al., Intake of carbohydrates compared with intake of saturated fatty acids and risk of myocardial infarction: importance of the glycemic index. Am J Clin Nutr, 2010. 91(6): p. 1764-8.
- Institute of Medicine, Food and Nutrition Board. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids (macronutrients). Washington, DC: National Academy Press; 2005.
- Jones PJH, Rideout T. Lipids, sterols, and their metabolites. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, eds. Modern Nutrition in Health and Disease. 11th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2014.
- Jones PJH, Papamandjaris AA. Lipids: cellular metabolism. In: Erdman JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. 10th ed. Washington, DC: Wiley-Blackwell; 2012:132-48.
- Harris WS. Omega-3 fatty acids. In: Coates PM, Betz JM, Blackman MR, et al., eds. Encyclopedia of Dietary Supplements. 2nd ed. London and New York: Informa Healthcare; 2010:577-86.
- Simopoulos AP. The importance of the omega-6/omega-3 fatty acid ratio in cardiovascular disease and other chronic diseases. Exp Biol Med (Maywood). 2008 Jun;233(6):674-88. doi: 10.3181/0711-MR-311
- Wang C, Chung M, Lichtenstein A, Balk E, Kupelnick B, DeVine D, et al. Effects of omega-3 fatty acids on cardiovascular disease. Summary, evidence report/technology assessment no. 94. (Prepared by the Tufts New England Medical Center Evidence-based Practice Center, Boston, MA.) AHRQ Publication No. 04-E009-1. Agency for Healthcare Research and Quality, 2004. https://archive.ahrq.gov/downloads/pub/evidence/pdf/o3cardio/o3cardio.pdf
- Harris WS, Davidson MH. RE: Plasma phospholipid fatty acids and prostate cancer risk in the SELECT trial. J Natl Cancer Inst. 2014 Apr;106(4):dju019. doi: 10.1093/jnci/dju019
- Brasky TM, Darke AK, Song X, Tangen CM, Goodman PJ, Thompson IM, Meyskens FL Jr, Goodman GE, Minasian LM, Parnes HL, Klein EA, Kristal AR. Plasma phospholipid fatty acids and prostate cancer risk in the SELECT trial. J Natl Cancer Inst. 2013 Aug 7;105(15):1132-41. doi: 10.1093/jnci/djt174
- Harris WS. Are n-3 fatty acids still cardioprotective? Curr Opin Clin Nutr Metab Care. 2013 Mar;16(2):141-9. doi: 10.1097/MCO.0b013e32835bf380
- Agency for Healthcare Research and Quality. Omega-3 fatty acids and cardiovascular disease – 2015. https://effectivehealthcare.ahrq.gov/products/fatty-acids-cardiovascular-disease/research-protocol
- Harris WS. The omega-3 index as a risk factor for coronary heart disease. Am J Clin Nutr. 2008 Jun;87(6):1997S-2002S. doi: 10.1093/ajcn/87.6.1997S
- Metcalf RG, Cleland LG, Gibson RA, Roberts-Thomson KC, Edwards JR, Sanders P, Stuklis R, James MJ, Young GD. Relation between blood and atrial fatty acids in patients undergoing cardiac bypass surgery. Am J Clin Nutr. 2010 Mar;91(3):528-34. doi: 10.3945/ajcn.2009.28302
- James M, Proudman S, Cleland L. Fish oil and rheumatoid arthritis: past, present and future. Proc Nutr Soc. 2010 Aug;69(3):316-23. doi: 10.1017/S0029665110001564
- Abdelhamid AS, Brown TJ, Brainard JS, Biswas P, Thorpe GC, Moore HJ, Deane KH, Summerbell CD, Worthington HV, Song F, Hooper L. Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2020 Feb 29;3(2):CD003177. doi: 10.1002/14651858.CD003177.pub5
- Weylandt KH, Serini S, Chen YQ, Su HM, Lim K, Cittadini A, Calviello G. Omega-3 Polyunsaturated Fatty Acids: The Way Forward in Times of Mixed Evidence. Biomed Res Int. 2015;2015:143109. doi: 10.1155/2015/143109
- Casula M, Soranna D, Catapano AL, Corrao G. Long-term effect of high dose omega-3 fatty acid supplementation for secondary prevention of cardiovascular outcomes: A meta-analysis of randomized, placebo controlled trials [corrected]. Atheroscler Suppl. 2013 Aug;14(2):243-51. doi: 10.1016/S1567-5688(13)70005-9. Erratum in: Atheroscler Suppl. 2014 Mar;233(1):122.
- Agency for Healthcare Research and Quality. Omega-3 fatty acids and cardiovascular disease: an updated systematic review. 2016. https://effectivehealthcare.ahrq.gov/products/fatty-acids-cardiovascular-disease/research
- Siscovick DS, Barringer TA, Fretts AM, Wu JH, Lichtenstein AH, Costello RB, Kris-Etherton PM, Jacobson TA, Engler MB, Alger HM, Appel LJ, Mozaffarian D; American Heart Association Nutrition Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Epidemiology and Prevention; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; and Council on Clinical Cardiology. Omega-3 Polyunsaturated Fatty Acid (Fish Oil) Supplementation and the Prevention of Clinical Cardiovascular Disease: A Science Advisory From the American Heart Association. Circulation. 2017 Apr 11;135(15):e867-e884. doi: 10.1161/CIR.0000000000000482
- National Institutes of Health. Dietary Supplement Label Database. 2015.
- U.S. Food and Drug Administration. Fish: what pregnant women and parents should know. 2014. https://www.fda.gov/food/consumers/advice-about-eating-fish
- ConsumerLab.com. Product review: fish oil and omega-3 fatty acid supplements review (including krill, algae, calamari, green-lipped mussel oil). 2021. https://www.consumerlab.com/reviews/fish-oil-supplements-review/omega3
- National Institutes of Health, Department of Health and Human Services – Healthy Eating Plan – https://www.nhlbi.nih.gov/health/educational/lose_wt/eat/calories.htm
- https://www.nhlbi.nih.gov/health/educational/wecan/healthy-weight-basics/balance.htm