Healthy foods for diabetics
Nutrition and physical activity are important parts of a healthy lifestyle when you have diabetes. However, there is no specific diet for diabetes. A panel of scientists, doctors, endocrinologists, diabetes educators and dietitians reviewed over 600 research articles over the course of five years to see what diets—or eating patterns—work well for people with diabetes. The results were published in our Nutrition Consensus Report 1. The main finding is that everyone’s body responds differently to different types of foods and diets, so there is no single “magic” diet for diabetes. There are many different eating patterns can help you manage your diabetes—from Mediterranean to low-carbohydrate to vegetarian 1. Whatever you choose, be sure to include lots of non-starchy vegetables, minimize added sugars and refined grains, and choose whole, minimally processed foods.
While there is growing evidence to show that low-carbohydrate eating patterns can benefit people with diabetes and prediabetes, there is no one definition for “low carb.” For some, following an eating pattern lower in carbs (26–45% of total calories from carbohydrate) showed better blood sugars and a reduction in diabetes medications, among other benefits. Work closely with your doctor and registered dietitian nutritionist if you choose a lower carb approach to minimize risks (such as hypoglycemia) and maximize success.
The key to healthy eating with diabetes is to eat a variety of healthy foods from all food groups every day.
The food groups are:
- Vegetables
- nonstarchy: includes broccoli, carrots, greens, peppers, and tomatoes
- starchy: includes potatoes, corn, and green peas
- Fruits—includes oranges, melon, berries, apples, bananas, and grapes
- Grains—at least half of your grains for the day should be whole grains
- includes wheat, rice, oats, cornmeal, barley, and quinoa
- examples: bread, pasta, cereal, and tortillas
- Protein
- lean meat
- chicken or turkey without the skin
- fish
- eggs
- nuts and peanuts
- dried beans and certain peas, such as chickpeas and split peas
- meat substitutes, such as tofu
- Dairy—nonfat or low fat
- milk or lactose-free milk if you have lactose intolerance
- yogurt
- cheese
Eat foods with heart-healthy fats, which mainly come from these foods:
- oils that are liquid at room temperature, such as canola and olive oil
- nuts and seeds
- heart-healthy fish such as salmon, tuna, and mackerel
- avocado
Use oils when cooking food instead of butter, cream, shortening, lard, or stick margarine.
Foods and drinks to limit or avoid include:
- fried foods and other foods high in saturated fat and trans fat
- foods high in salt, also called sodium
- sweets, such as baked goods, candy, and ice cream
- beverages with added sugars, such as juice, regular soda, and regular sports or energy drinks
Drink water instead of sweetened beverages. Consider using a sugar substitute in your coffee or tea.
If you drink alcohol, drink moderately—no more than one drink a day if you’re a woman or two drinks a day if you’re a man. If you use insulin or diabetes medicines that increase the amount of insulin your body makes, alcohol can make your blood glucose level drop too low. This is especially true if you haven’t eaten in a while. It’s best to eat some food when you drink alcohol.
Losing modest amounts of weight (start with 5%) can improve your blood sugars and other diabetes outcomes in both type 1 and type 2 diabetes 2. There are lots of ways to lose weight, from changing your diet to getting more exercise, taking medications or even surgery. A focus on lifestyle changes is the preferred starting point, but it’s important to be familiar with all valid options.
Tweaking your food choices can help reduce risk factors for complications. Food swaps are easy ways for people with diabetes to reduce their risk for cardiovascular disease and kidney disease. For example, consider replacing foods high in saturated fat, such as butter and fatty beef, with foods rich in unsaturated fats, like olive oil and fish.
Healthy diet for diabetics
Eating the right amount of food will also help you manage your blood glucose level and your weight. Your health care team can help you figure out how much food and how many calories you should eat each day.
Two common ways to help you plan how much to eat if you have diabetes are the plate method and carbohydrate counting, also called carb counting. Check with your health care team about the method that’s best for you.
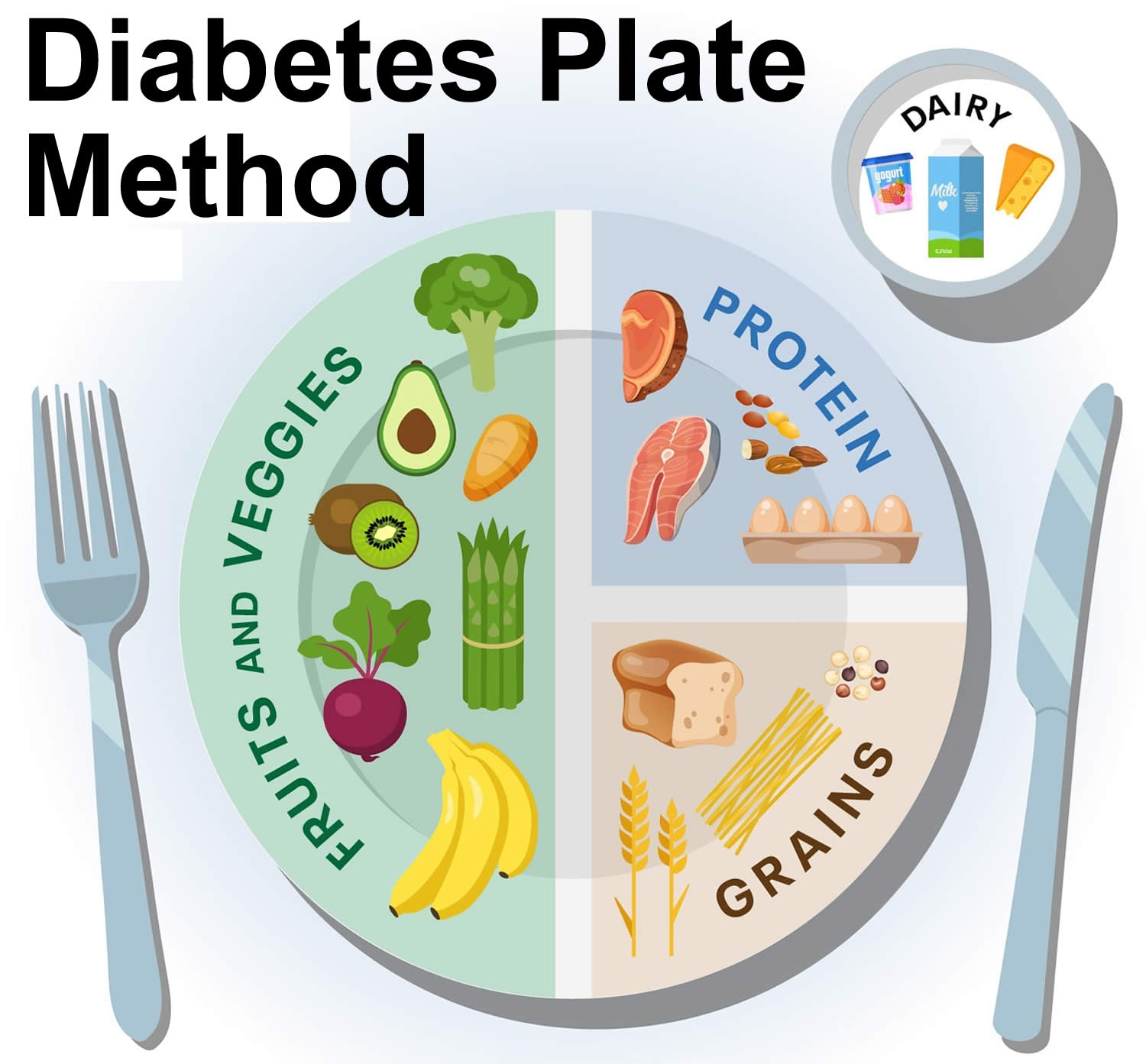
Plate method
It’s easy to eat more food than you need without realizing it. The plate method is a simple, visual way to make sure you get enough nonstarchy vegetables and lean protein while limiting the amount of higher-carb foods you eat that have the highest impact on your blood sugar. The plate method helps you control your portion sizes. You don’t need to count calories. The plate method works best for lunch and dinner.
Start with a 9-inch dinner plate (about the length of a business envelope):
- Fill half with nonstarchy vegetables, such as salad, green beans, broccoli, cauliflower, cabbage, and carrots. These vegetables keep you feeling full for longer and provide you with the great-tasting nutrients your body needs without as many calories and carbs. The following is a list of common non-starchy vegetables:
- Amaranth or Chinese spinach
- Artichoke
- Artichoke hearts
- Asparagus
- Baby corn
- Bamboo shoots
- Beans (green, wax, Italian)
- Bean sprouts
- Beets
- Brussels sprouts
- Broccoli
- Cabbage (green, bok choy, Chinese)
- Carrots
- Cauliflower
- Celery
- Chayote
- Cucumber
- Daikon
- Eggplant
- Greens (collard, kale, mustard, turnip)
- Hearts of palm
- Jicama
- Kohlrabi
- Leeks
- Mushrooms
- Okra
- Onions
- Pea pods
- Peppers
- Radishes
- Rutabaga
- Salad greens (chicory, endive, escarole, lettuce, romaine, spinach, arugula, radicchio, watercress)
- Sprouts
- Squash (cushaw, summer, crookneck, spaghetti, zucchini)
- Sugar snap peas
- Swiss chard
- Tomato
- Turnips
- Water chestnuts
- Yard-long beans
- Fill one quarter with a lean protein, such as chicken, fish, turkey, beans, tofu, or eggs. Try to include fish at least two times per week. Fish high in omega-3 fatty acids like Albacore tuna, herring, mackerel, rainbow trout, sardines and salmon.
- There are plenty of protein-rich plant-based options, such as beans, hummus, lentils and others. Plant-based protein foods provide quality protein, healthy fats and fiber. They vary in how much fat and carbohydrate they contain, so make sure to read labels.
- Beans such as black, kidney and pinto
- Bean products like baked beans and refried beans
- Hummus and falafel
- Lentils such as brown, green or yellow
- Peas such as black-eyed or split peas
- Edamame
- Soy nuts
- Nuts and spreads like almond butter, cashew butter or peanut butter
- Tempeh, tofu
- Products like meatless “chicken” nuggets, “beef” crumbles, “burgers”, “bacon”, “sausage” and “hot dogs”
- There are plenty of protein-rich plant-based options, such as beans, hummus, lentils and others. Plant-based protein foods provide quality protein, healthy fats and fiber. They vary in how much fat and carbohydrate they contain, so make sure to read labels.
- Fill one quarter with carb foods. Foods that are higher in carbs include grains, starchy vegetables (such as potatoes and peas), rice, pasta, beans, fruit, and yogurt. A cup of milk also counts as a carb food.
Then choose water or a low-calorie drink such as unsweetened iced tea to go with your meal. You also may eat a small bowl of fruit or a piece of fruit in your meal plan.
Portion size
Portion size and serving size aren’t always the same. A portion is roughly what fits in the palm of your hand. A portion is the amount of food you choose to eat at one time, while a serving is a specific amount of food, such as one slice of bread or 8 ounces (1 cup) of milk.
Portion sizes:
- You can use everyday objects or your hand to judge the size of a portion.
- 1 serving of meat or poultry is the palm of your hand or a deck of cards
- 1 3-ounce serving of fish is a checkbook
- 1 serving of cheese is six dice
- 1/2 cup of cooked rice or pasta is a rounded handful or a tennis ball
- 1 serving of a pancake or waffle is a DVD
- 2 tablespoons of peanut butter is a ping-pong ball
These days, portions at restaurants are quite a bit larger than they were several years ago. One entrée can equal 3 or 4 servings! Studies show that people tend to eat more when they’re served more food, so getting portions under control is really important for managing weight and blood sugar.
If you’re eating out, have half of your meal wrapped up to go so you can enjoy it later. At home, measure out snacks; don’t eat straight from the bag or box. At dinnertime, reduce the temptation to go back for seconds by keeping the serving bowls out of reach.
Carbohydrate counting
Counting carbohydrates or counting carbs is a way of keeping track of the carbs in all your meals, snacks, and drinks—can help you match your activity level and medicines to the food you eat.
There are 3 types of carbs:
- Sugars, such as the natural sugar in fruit and milk or the added sugar in soda and many other packaged foods.
- Starches, including wheat, oats, and other grains; starchy vegetables such as corn and potatoes; and dried beans, lentils, and peas.
- Fiber, the part of plant foods that isn’t digested but helps you stay healthy.
Sugars and starches raise your blood sugar, but fiber doesn’t.
Carbs are measured in grams. To count carbohydrate grams in what you eat, you’ll need to:
- learn which foods have carbohydrates
- read the Nutrition Facts food label, or learn to estimate the number of grams of carbohydrate in the foods you eat
- add the grams of carbohydrate from each food you eat to get your total for each meal and for the day
Most carbohydrates come from starches, fruits, milk, and sweets. Try to limit carbohydrates with added sugars or those with refined grains, such as white bread and white rice. Instead, eat carbohydrates from fruit, vegetables, whole grains, beans, and low-fat or nonfat milk.
Talk with your dietitian about the right amount of carbs for you or you can also use a carb-counting app to find grams of carbs in foods and drinks.
For diabetes meal planning, 1 carb serving is about 15 grams of carbs. This isn’t always the same as what you think of as a serving of food. For example, most people would count a small baked potato as 1 serving. However, at about 30 grams of carbs, it counts as 2 carb servings.
Many people with diabetes count carbs to make managing blood sugar easier, which can also help them:
- Stay healthy longer.
- Feel better and improve their quality of life.
- Prevent or delay diabetes complications such as kidney disease, eye disease, heart disease, and stroke.
If you take mealtime insulin, you’ll count carbs to match your insulin dose to the amount of carbs in your foods and drinks. You may also take additional insulin if your blood sugar is higher than your target when eating.
Work with your doctor or a registered dietitian to find out how many carbs you can eat each day and at each meal.
How many carbs should I eat?
There’s no “one size fits all” answer—everyone is different because everyone’s body is different. The amount you can eat and stay in your target blood sugar range depends on your age, weight, activity level, and other factors.
On average, people with diabetes should aim to get about half of their calories from carbs. That means if you normally eat about 1,800 calories a day to maintain a healthy weight, about 800 to 900 calories can come from carbs. At 4 calories per gram, that’s 200–225 carb grams a day. Try to eat about the same amount of carbs at each meal to keep your blood sugar levels steady throughout the day (not necessary if you use an insulin pump or give yourself multiple daily injections—you’ll take a fast-acting or short-acting insulin at mealtimes to match the amount of carbs you eat).
This sample menu has about 1,800 calories and 200 grams of carbs:
- Breakfast
- ½ cup rolled oats (28g)
- 1 cup low-fat milk (13g)
- 2/3 medium banana (20g)
- ¼ cup chopped walnuts (4g)
- Total carbs: 65 grams
- Lunch
- 2 slices whole wheat bread (24g)
- 4 oz. low-sodium turkey meat (1g)
- 1 slice low-fat Swiss cheese (1g)
- ½ large tomato (3g)
- 1 TBS yellow mustard (1g)
- ¼ cup shredded lettuce (0g)
- 8 baby carrots (7g)
- 6 oz. plain fat-free Greek yogurt (7g)
- ¾ cup blueberries (15g)
- Total carbs: 59 grams
- Snack
- 1 low-fat string cheese stick (1g)
- 2 tangerines (18g)
- Total carbs: 19 grams
- Dinner
- 6 ounces baked chicken breast (0g)
- 1 cup brown rice (45g)
- 1 cup steamed broccoli (12g)
- 2 tbs margarine (0g)
- Total carbs: 57 grams
Superfoods that are good for diabetes
“Superfood” is a term used by many food and beverage companies as a way to promote a food thought to have health benefits; however, there is no official definition of the word by the Food and Drug Administration (FDA). The FDA regulates the health claims allowed on food labels to ensure there is scientific research to support the claims. The list of foods below are rich in vitamins, minerals, antioxidants and fiber that are good for overall health and may also help prevent disease.
Beans
Kidney, pinto, navy or black beans are packed with vitamins and minerals such as magnesium and potassium. They are very high in fiber too.
Beans do contain carbohydrates, but ½ cup also provides as much protein as an ounce of meat without the saturated fat. To save time you can use canned beans, but be sure to drain and rinse them to get rid of as much added salt as possible.
Dark green leafy vegetables
Spinach, collards and kale are dark green leafy vegetables packed with vitamins and minerals such as vitamins A, C, E and K, iron, calcium and potassium. These powerhouse foods are low in calories and carbohydrates too. Try adding dark leafy vegetables to salads, soups and stews.
Citrus fruit
Grapefruits, oranges, lemons and limes or pick your favorites to get part of your daily dose of fiber, vitamin C, folate and potassium.
Sweet potatoes
A starchy vegetable packed full of vitamin A and fiber. They are also a good source of vitamin C and potassium.
Try a sweet potato in place of a regular potato and sprinkle cinnamon on top.
Berries
Which are your favorites: blueberries, strawberries or another variety? Regardless, they are all packed with antioxidants, vitamins and fiber. Berries can be a great option to satisfy your sweet tooth and they provide an added benefit of vitamin C, vitamin K, manganese, potassium and fiber.
Tomatoes
The good news is that no matter how you like your tomatoes, pureed, raw, or in a sauce, you’re eating vital nutrients like vitamin C, vitamin E and potassium.
Fish high in omega-3 fatty acids
Omega-3 fats may help to reduce the risk of heart disease and inflammation. Fish high in these healthy fats are sometimes referred to as “fatty fish.” Salmon is well known in this group. Other fish high in omega-3 are herring, sardines, mackerel, trout and albacore tuna. Choose fish that is broiled, baked or grilled to avoid the carbohydrate and extra calories that would be in fish that is breaded and fried. The American Diabetes Association Standards of Medical Care in Diabetes recommends eating fish (mainly fatty fish) twice per week for people with diabetes.
Nuts
An ounce of nuts can go a long way in getting key healthy fats along with helping to manage hunger. In addition, they offer magnesium and fiber. Some nuts and seeds, such as walnuts and flax seeds, are a good source of omega-3 fatty acids.
Whole grains
It’s the whole grain you’re after. The first ingredient on the label should have the word “whole” in it. Whole grains are rich in vitamins and minerals like magnesium, B vitamins, chromium, iron and folate. They are a great source of fiber too. Some examples of whole grains are whole oats, quinoa, whole grain barley and farro.
Milk and yogurt
You may have heard that milk and yogurt can help build strong bones and teeth. In addition to calcium, many milk and yogurt products are fortified to make them a good source of vitamin D. More research is emerging on the connection between vitamin D and good health. Milk and yogurt do contain carbohydrate that will be a factor in meal planning when you have diabetes. Look for yogurt products that are lower in fat and added sugar.
Gestational diabetes
Gestational diabetes also known as GDM, is diabetes diagnosed for the first time during pregnancy (gestation). Like other types of diabetes, gestational diabetes affects how your cells use sugar (glucose). Gestational diabetes causes higher than normal blood sugar levels that can affect your pregnancy and your baby’s health. If the diabetes isn’t treated, both you and your baby may be more likely to have problems at birth. For example, your baby may have a low blood sugar level or jaundice. Or your baby may weigh much more than normal. If your baby is very large, you may have a more difficult delivery. You may even need a Cesarean section. Gestational diabetes also increases your risk of developing preeclampsia. Preeclampsia is a condition that can be serious if left untreated.
Gestational diabetes (GDM) affects approximately 6% of pregnancies in the United States 3 and it is increasing in prevalence, with a range from 1% to 25% depending on the population and diagnostic criteria used 4.
Gestational diabetes usually develops in the second trimester (usually occurs around the 24th to 28th week of pregnancy, but sometimes as early as the 20th week of pregnancy). Typically, women with gestational diabetes have no symptoms. Most women are diagnosed after routine tests during pregnancy. All pregnant women should be tested for gestational diabetes at 24-28 weeks of pregnancy (except those women who already have diabetes). Women who have risk factors for gestational diabetes should be tested earlier in their pregnancy. Most often, gestational diabetes goes away after the baby is born.
Women at increased risk of developing gestational diabetes include those who 5:
- Gestational diabetes mellitus in previous pregnancy
- Have prediabetes, meaning your blood glucose levels are higher than normal yet not high enough for a diagnosis of diabetes
- Body mass index (BMI) > 25 kg/m²
- Ethnicity
- Asian
- Native American
- Pacific Islander
- Black
- Hispanic
- Have a family history of type 2 diabetes or a first-degree relative (mother or sister) who has had gestational diabetes
- Weight gain of more than 11 lb (5 kg) since 18 years of age
- Maternal age older than 35 years
- Gestational weight gain in excess of Institute of Medicine guidelines
- Have Polycystic Ovary Syndrome (also known as PCOS)
- Have previously given birth to a large baby also known as macrosomia (weighing more than 4.5kg)
- Are currently taking some types of anti-psychotic or steroid medications.
- Gestational diabetes may also occur in women with no known risk factors.
Being overweight or obese is linked to gestational diabetes. Women who are overweight or obese may already have insulin resistance when they become pregnant. Gaining too much weight during pregnancy may also be a factor. Having a family history of diabetes makes it more likely that a woman will develop gestational diabetes, which suggests that genes play a role.
In pregnancy, your placenta produces hormones that help your baby grow and develop. These hormones also block the action of the insulin hormone made in your pancreas that helps your body use glucose (sugar) for energy and helps control your blood glucose levels. This is called insulin resistance 6. Because of this insulin resistance, the need for insulin in pregnancy is 2 to 3 times higher than normal. If you already have insulin resistance, then your body may not be able to cope with the extra demand for insulin production and the blood glucose levels will be higher resulting in gestational diabetes being diagnosed.
All pregnant women have some insulin resistance during late pregnancy. Most pregnant women can produce enough insulin to overcome insulin resistance, but some cannot. These women develop gestational diabetes.
When your pregnancy is over and your blood glucose levels usually return to normal and the gestational diabetes disappears, however this insulin resistance increases your risk of developing type 2 diabetes in later life. Your child may also be more likely to become obese and develop type 2 diabetes later in life.
Gestational diabetes is diagnosed using an oral glucose tolerance test (OGTT). This is done at a pathology lab. You will need to fast overnight before having this test. Blood will be taken to check your fasting blood glucose level. After this, you will be given a sugary drink and have your blood tested one and two hours later. You will be asked to sit and wait between tests. If your blood glucose level is above the normal range at your fasting, one or two hour test, you have gestational diabetes.
In women with gestational diabetes, blood sugar usually returns to normal soon after delivery. But if you’ve had gestational diabetes, you have a higher risk of getting type 2 diabetes. You’ll need to be tested for changes in blood sugar more often.
While any pregnancy complication is concerning, there’s good news. Expectant mothers can help control gestational diabetes by eating healthy foods, exercising and, if necessary, taking medication. Controlling blood sugar can keep you and your baby healthy and prevent a difficult delivery.
Gestational diabetes is managed by monitoring your blood glucose levels, adopting a healthy eating plan and performing regular physical activity. Effective management of gestational diabetes will reduce the risk of complications during pregnancy and the birth of your baby.
Your healthcare team including your doctor, specialist, dietician and diabetes educator, can help you with blood glucose monitoring, healthy eating and physical activity.
There are three basic components in effectively managing gestational diabetes:
- Monitoring blood glucose levels. If you’re testing your blood glucose, the American Diabetes Association suggests the following targets for women who develop gestational diabetes during pregnancy. More or less stringent blood sugar goals may be appropriate for each individual (ask your doctor what targets are right for you) 7:
- Before meals, at bedtime, and overnight: 95 mg/dL (5.3 mmol/L) or less
- 1 hour after eating: 140 mg/dL (7.8 mmol/L) or less
- 2 hours after eating: 120 mg/dL (6.7 mmol/L) or less
- Adopting a healthy eating pattern
- Physical activity.
Gestational diabetes can often initially be managed with healthy eating and regular physical activity. However, for some women with gestational diabetes, insulin injections will be necessary for the rest of the pregnancy. Approximately 10 – 20% of women will need insulin; however, once the baby is born insulin is no longer needed. This is safe for both you and your baby.
After the baby is born, gestational diabetes usually disappears. A special blood glucose test (Oral Glucose Tolerance Test) (OGTT) is performed six weeks after delivery to ensure that blood glucose levels have returned to normal. However, women who have had gestational diabetes have an increased risk of developing type 2 diabetes later in life and should be tested for diabetes at least every 2 – 3 years.
How can gestational diabetes affect my baby?
High blood glucose levels during pregnancy can cause problems for your baby, such as:
- being born too early
- weighing too much, which can make delivery difficult and injure your baby
- having low blood glucose, also called hypoglycemia, right after birth
- having breathing problems
High blood glucose also can increase the chance that you will have a miscarriage or a stillborn baby 8. Stillborn means the baby dies in the womb during the second half of pregnancy.
Your baby also will be more likely to become overweight and develop type 2 diabetes as he or she gets older.
How can gestational diabetes affect me?
If you have gestational diabetes, you are more likely to develop preeclampsia, which is when you develop high blood pressure and too much protein in your urine during the second half of pregnancy.
Preeclampsia can cause serious or life-threatening problems for you and your baby. The only cure for preeclampsia is to give birth. If you have preeclampsia and have reached 37 weeks of pregnancy, your doctor may want to deliver your baby early. Before 37 weeks, you and your doctor may consider other options to help your baby develop as much as possible before he or she is born.
Gestational diabetes may increase your chance of having a Cesarean section, also called a C-section, because your baby may be large. A C-section is major surgery.
If you have gestational diabetes, you are more likely to develop type 2 diabetes later in life. Over time, having too much glucose in your blood can cause health problems such as diabetic retinopathy, heart disease, kidney disease, and nerve damage. You can take steps to help prevent or delay type 2 diabetes.
How can I manage my gestational diabetes?
Many women with gestational diabetes can manage their blood glucose levels by following a healthy eating plan and being physically active. However, for some women with gestational diabetes, insulin injections will be necessary for the rest of the pregnancy. Approximately 10 – 20% of women will need insulin; however, once the baby is born insulin is no longer needed. Insulin is safe for both you and your baby and is usually the first choice of diabetes medicine for gestational diabetes.
Researchers are studying the safety of the diabetes pills metformin and glyburide during pregnancy, but more long-term studies are needed. Talk with your health care professional about what treatment is right for you.
After the baby is born, gestational diabetes usually disappears. A special blood glucose test (Oral Glucose Tolerance Test) (OGTT) is performed six weeks after delivery to ensure that blood glucose levels have returned to normal. However, women who have had gestational diabetes have an increased risk of developing type 2 diabetes later in life and should be tested for diabetes at least every 2 – 3 years.
How can I lower my chance of developing gestational diabetes?
If you are thinking about becoming pregnant and are overweight, you can lower your chance of developing gestational diabetes by losing extra weight and increasing physical activity before you become pregnant. Taking these steps can improve how your body uses insulin and help your blood glucose levels stay normal.
Once you are pregnant, don’t try to lose weight. You need to gain some weight for your baby to be healthy. However, gaining too much weight too quickly may increase your chance of developing gestational diabetes. Ask your doctor how much weight gain and physical activity during pregnancy are right for you.
After I have my baby, how can I find out whether I have diabetes?
You should get tested for diabetes no later than 12 weeks after your baby is born. If your blood glucose is still high, you may have type 2 diabetes. Even if your blood glucose is normal, you still have a greater chance of developing type 2 diabetes in the future. Therefore, you should be tested for diabetes every 3 years.
Here are steps you should take for yourself and your child if you had gestational diabetes:
- Get tested for diabetes 6 to 12 weeks after your baby is born. If your blood glucose is still high, you may have type 2 diabetes. If your blood glucose is normal, you should get tested every 3 years to see if you have developed type 2 diabetes.
- Be more active and make healthy food choices to get back to a healthy weight.
- Breastfeed your baby. Breastfeeding gives your baby the right balance of nutrients and helps you burn calories.
How can I prevent or delay type 2 diabetes later in life?
Research such as the Diabetes Prevention Program (https://dppos.bsc.gwu.edu) shows that you can do a lot to reduce your chances of developing type 2 diabetes. Here are some things you can change to lower your risk if you had gestational diabetes:
- Be more active and make healthy food choices to get back to a healthy weight. Get at least 30 minutes of physical activity 5 days a week. If you have not been active, talk with your health care professional about which activities are best. Start slowly to build up to your goal.
- Breastfeed your baby. Breastfeeding External link gives your baby the right balance of nutrients and helps you burn calories.
- Lose weight and keep it off. You may be able to prevent or delay diabetes by losing 5 to 7 percent of your starting weight 9. For instance, if you weigh 200 pounds, your goal would be to lose about 10 to 14 pounds.
- If your test results show that you could get diabetes and you are overweight, ask your doctor about what changes you can make to lose weight and for help in making them. Your doctor may recommend that you take medicine such as metformin to help prevent type 2 diabetes 9.
Most often, your best chance for preventing type 2 diabetes is to make lifestyle changes that work for you long term.
Gestational diabetes healthy diet
An important part of managing gestational diabetes relates to your diet and eating healthily. Healthy diet during pregnancy will help you keep your blood sugar levels in the safe range so you’re more likely to enjoy a healthy pregnancy and give birth to a healthy baby. It is advisable to see a registered dietitian nutritionist to work out a meal plan that is appropriate for you and your growing baby. If this has not happened ask your maternity care team to refer you. Making healthy choices helps the whole family and may protect your child from becoming obese or developing diabetes.
To help you get started, here are some options to try for breakfast, lunch, snacks and dinner. It’s important to be physically active every day as well, to help you manage your sugar levels.
These healthy eating tips for women with gestational diabetes are general. Your maternity care team should talk to you about making changes to your diet and refer you to a dietitian for individual advice that’s right for you.
Choose healthier carbohydrates (carbs)
All carbs affect your blood sugar levels, so you need to know which foods contain carbs. All the carbohydrates you eat and drink are broken down into glucose. The type and amount of carbs you eat or drink can make a difference to your blood glucose levels and diabetes management. The amount makes the biggest difference. And your dietitian may talk to you about reducing your carb portion sizes. It’s important too, to choose healthier carbs.
Quality of carbs has been assessed using glycemic index (GI), glycemic load, fiber content and wholegrain among others. Generally, lower GI (glycemic index) foods can be useful for managing blood glucose levels. More importantly for overall health, choosing foods that are high in fiber and wholegrains instead of refined carbs, such as white bread, is better for your heart health and reducing your risk of certain types of cancers. Scientists also know that some specific carb-containing foods, such as fruits and vegetables, are associated with good health.
Easy swaps for healthier carbs:
- Swap white bread for multigrain, wholegrain, wholemeal, rye, linseed or pumpernickel.
- Swap chapatti and roti made with white flour to those made with wholemeal flour.
- Swap white pittas for brown pittas.
- Swap chips and mash for wholemeal pasta, baked plantain or sweet potato.
- Swap white rice for brown rice.
- Swap cereals like Cornflakes and Rice Krispies for Weetabix, Branflakes, Shredded Wheat (or supermarket brand ones) or porridge
Other healthier carbs:
- Fruit. Have fruit whole, rather than as a juice. Eating an apple with the skin on, for example, will provide more fiber than drinking a glass of apple juice.
- Vegetables
- Pulses such as chickpeas, beans and lentils
- Try seeds and nuts as lower carb sources of fiber
- Choose unsweetened milk and yogurts. If you are using a non-dairy milk, check they are unsweetened and fortified with vitamins and minerals.
You can check food labels when you’re looking for foods high in fiber if you’re unsure.
Cut down on sugar
Cutting down sugar can be really hard at the beginning, so small practical swaps are a good starting point.
Easy ways to cut down on excess sugar:
- Swap sugary drinks, energy drinks and fruit juices with water, plain skimmed or semi-skimmed milk, or decaffeinated tea and coffee.
- Try low or zero-calorie sweeteners, also known as artificial sweeteners, instead of using sugar.
- Have fewer foods like cakes, chocolates, ice cream and biscuits.
- Know the other names for sugar on the food label. These are sucrose, glucose, dextrose, fructose, lactose, maltose, honey, invert sugar, syrup, corn sweetener and molasses.
Getting your portion sizes right
A portion is roughly what fits in the palm of your hand. Using everyday items and household utensils to get your portion sizes right can be really useful. It’s an easy way to visualize what a portion should look like. Use smaller plates and bowls to help make your portion sizes look bigger.
Remember, everybody’s needs are different so the number of portion sizes you need is individual and your weight, gender, body composition and activity levels all make a difference. Your dietitian will be able to advise you on the amount of portions that are right for you.
Starchy foods are your main source of carbohydrate and have an important role in a healthy diet. As well as starch, they contain fiber, calcium, iron and B vitamins. Starchy food includes rice, pasta, potatoes, bread, cereals and chapattis for energy. Where you can, choose wholegrain varieties, and eat potatoes with their skin on for more fiber. One portion is:
- Cooked rice = 2 heaped tablespoons
- Half a jacket potato = 1 computer mouse
- Breakfast cereal = 3 tablespoons
- Boiled pasta or cooked noodles = 3 heaped tablespoons
Dairy food includes milk, cheese and yogurt for calcium, which is essential for strong bones and teeth. One portion is:
- Semi or skimmed milk = one medium glass (200ml or 1/3 pint)
- Hard cheese = small matchbox (30g)
- Reduced or low-fat cream cheese = two small matchboxes (60g)
- Low-sugar, low-fat fromage frais/yoghurt = 125g pot
Meat, fish, eggs, pulses, beans and nuts are high in protein, essential to build and replace muscle. One portion is:
- Cooked lean meat (eg chicken, beef or pork) = deck of playing cards (60–90g)
- Beans and pulses (eg red kidney beans, butter beans, chickpeas or lentils) = 4 tablespoons
- Nuts or peanut butter (unsalted) = golf ball (2 level tablespoons)
- Quorn, tofu or soya = snooker ball (120g)
Fruits provide you with important vitamins, minerals and fiber that help protect you against stroke, high blood pressure, heart disease and certain cancers. One portion is:
- One handful of grapes
- One small glass (150ml) of fruit juice (limit to one portion a day)
- Two small satsumas, clementines or tangerines
- Two medium plums
- Two tinned pineapple rings or 12 chunks in natural juice
- One heaped tbsp raisins, sultanas, currants or dried cranberries
- Seven strawberries
Vegetables are important sources of fiber, minerals and vitamins, and an important part of any five-a-day plan. One portion is:
- Three heaped tablespoons cooked veg (eg carrots, peas, sweetcorn, mixed veg)
- One medium onion
- One large sweet potato
- Two broccoli spears
- One heaped tablespoon tomato purée
- One piece of cucumber (5cm)
- Four large mushrooms or 14 button mushrooms
- Three heaped tablespoons beans or pulses (eg kidney beans, chickpeas or lentils)
Foods high in fat and sugar
You can enjoy foods from this group as an occasional treat, but they will add extra calories so it’s best to keep them to a minimum, especially if you are trying to lose weight. One portion is:
- Butter/margarine = one dice (5g)
- Low fat spread = two dice (10g)
- Unsaturated oil (eg sunflower, rapeseed, olive oil) = 1 teaspoon
- Chocolate = one fun size bar
Choose healthy snacks
Select foods that satisfy your hunger, supply your body with energy and provide important nutrients for you and your baby. If you do need to snack when you have gestational diabetes, swap cake, biscuits, crisps and chocolate for:
- plain or low sugar yogurt
- unsalted nuts
- seeds, fruit and veg
But watch your portion sizes still – it’ll help you keep an eye on your weight.
Here are several suggestions for snacks that are 100 calories or less:
- 1 cup sliced bananas and fresh raspberries (or any fruit)
- 2 cups baby carrots
- 2 cups air-popped popcorn
- 5 pieces Melba toast, rye or pumpernickel
- 2 tablespoons peanuts
- 2 domino-sized slices low-fat colby or cheddar cheese
Fruits and veggies. Generous portions of fruits or vegetables can easily help fill you up while staying below 100 calories. All of the following servings have fewer than 100 calories:
- Medium apple: 95 calories
- Small banana: 90 calories
- Two kiwis: 84 calories
- 20 medium baby carrots: 70 calories
- 20 grapes: 68 calories
- Medium orange: 65 calories
- 20 cherry tomatoes: 61 calories
- Medium peach: 58 calories
- Medium red pepper: 37 calories
- 20 pea pods: 28 calories
For comparison, one reduced-fat cheese stick has about 60 calories, which is well below the 100-calorie goal, but it also has 4.5 grams of fat. While the protein and fat may help curb your appetite, a single cheese stick may not be as satisfying as, say, 20 baby carrots, which add up to nearly 10 times the weight of the cheese stick, have 70 calories and less than 1 gram of fat.
Other snacks that are healthy and low in calories include the following:
- Popcorn. Two cups of air-popped popcorn has 62 calories and is a good source of nutrients, such as magnesium and potassium.
- Whole-grain crispbreads. Toasted whole-grain bread crackers, such as rye Melba toast, are good sources of fiber and complex carbohydrates. Five pieces of Melba toast have about 97 calories.
- Hummus. Hummus is made primarily from chickpeas, a small amount of ground sesame seeds and olive oil. It’s a good source of protein. Although it contains fats, they are mostly healthy polyunsaturated and monounsaturated fats. Two tablespoons of hummus — a good dip for a low-calorie vegetable snack — has 50 calories and 2.8 grams of fat.
- Nuts. While nuts may have a bad reputation, research studies have shown that they don’t generally contribute to increased calorie intake or weight gain when eaten in moderation, in part because you feel satisfied after eating them. Nuts also have been associated with a decreased risk of heart disease and overall mortality. Thirteen almonds provide a 100-calorie snack with 7.8 grams of healthy fats.
Healthy snacking requires planning. Here are some tips to snack sensibly:
- Keep your house stocked with fresh fruits and vegetables. Buy a variety so that you don’t get bored with your selection.
- Keep a supply of frozen or canned fruits at home and work for backup.
- Don’t keep conventional snacks, such as candy or chips, in the house.
- Have a small amount of mixed nuts when hungry, which will go a long way toward decreasing hunger sensations.
- Experiment with herbs or spices to make fruits and vegetables more interesting.
- Prepare snacks in the evening for the next day. For example, before bedtime slice up a red pepper, wash an apple or count out a snack-size serving of grapes.
Avoid diabetic foods
The law has changed and manufacturers are no longer allowed to label food as diabetic or suitable for diabetics. They don’t have any special health benefits, they’re expensive, could still affect your blood sugar and may cause an upset stomach.
What is dietary fiber?
Fiber is the name given to a range of substances found in the cell walls of vegetables, fruits, pulses and cereal grains. Fiber that cannot be digested helps other food and waste products to move through the gut. Potato skins, wholegrain bread and breakfast cereals, brown rice, and wholewheat pasta are all good sources of this kind of fiber.
Fiber can help keep your bowels healthy and can help you feel full, which means you’re less likely to eat too much.
This makes wholegrain starchy foods and potatoes eaten with their skin on a particularly good choice if you’re trying to lose weight.
Some types of fiber found in fruits and vegetables – such as apples, carrots, potatoes – and in oats and pulses can be partly digested and may help reduce the amount of cholesterol in your blood.
Understand the glycemic index
The glycemic index (GI) tells you whether a food raises blood glucose levels quickly, moderately or slowly. This means glycemic index (GI) can be useful to help you manage your diabetes. Different carbohydrates are digested and absorbed at different rates, and glycemic index (GI) is a ranking of how quickly each carbohydrate-based food and drink makes blood glucose levels rise after eating them. Eating to manage your gestational diabetes isn’t just about GI ratings. Think of the bigger picture and choose foods high in fiber and wholegrains, as well as low in saturated fat, salt and sugar, as part of a long-term healthy diet.
The glycemic index (GI) index runs from 0 to 100 and usually uses pure glucose, which has a glycemic index (GI) of around 100, as the reference. Slowly absorbed carbohydrates have a low glycemic index (GI) rating (55 or below), and include most fruits and vegetables, unsweetened milk, nuts, pulses, some wholegrain cereals and bread. Research has shown that choosing low-GI foods can particularly help manage long-term blood glucose (HbA1c) levels in people with Type 2 diabetes. There is less evidence to support this in people with Type 1 diabetes, but scientists know that on a day-to-day basis choosing low GI foods can help keep blood glucose levels steady after eating.
The glycemic index (GI) numbers are to be used as a guide only as individual foods do not have the same response in all people with diabetes.
- Low GI foods are foods with a GI less than 55.
- Intermediate GI foods are foods with a GI between 55 and 70.
- High GI foods are foods with a GI greater than 70.
Below are examples of foods based on their GI.
Low GI Foods (55 or less)
- 100% stone-ground whole wheat or pumpernickel bread
- Oatmeal (rolled or steel-cut), oat bran, muesli
- Pasta, converted rice, barley, bulgar
- Sweet potato, corn, yam, lima/butter beans, peas, legumes and lentils
- Most fruits, non-starchy vegetables and carrots
Not all low-GI foods are healthy choices – chocolate, for example, has a low-GI because of its fat content, which slows down the absorption of carbohydrate.
Medium GI (56-69)
- Whole wheat, rye and pita bread
- Quick oats
- Brown, wild or basmati rice, couscous
High GI (70 or more)
- White bread or bagel
- Corn flakes, puffed rice, bran flakes, instant oatmeal
- Shortgrain white rice, rice pasta, macaroni and cheese from mix
- Russet potato, pumpkin
- Pretzels, rice cakes, popcorn, saltine crackers
- melons and pineapple
Not all low-GI foods are healthy choices – most chocolates, for example, have a low-GI because of their fat content, which slows down the absorption of carbohydrate. Combining foods with different GIs alters the overall GI of a meal. You can maximize the benefit of GI by switching to a low GI option with each meal or snack. Go easy on lower GI foods like chocolate, which is high in calories, especially if you are trying to lose weight. Save them for occasional treats.
It’s easy to include low-GI carbs in everyday meals:
- Choose basmati or easy cook rice, pasta or noodles. Or, try plantain, quinoa or bulgur wheat for a change.
- Eat wholemeal roti and include dhal in your meals.
- Use new potatoes instead of old potatoes – try sweet potatoes for a change.
- Instead of white and wholemeal bread, choose granary, pumpernickel or rye bread.
- Swap frozen chips for pasta or noodles.
- Try porridge, natural muesli or wholegrain breakfast cereals.
Table 1. 100 common foods glycemic index and glycemic load, per serving
| FOOD | Glycemic index (glucose = 100) | Serving size (grams) | Glycemic load per serving |
| BAKERY PRODUCTS AND BREADS | |||
| Banana cake, made with sugar | 47 | 60 | 14 |
| Banana cake, made without sugar | 55 | 60 | 12 |
| Sponge cake, plain | 46 | 63 | 17 |
| Vanilla cake made from packet mix with vanilla frosting (Betty Crocker) | 42 | 111 | 24 |
| Apple muffin, made with rolled oats and sugar | 44 | 60 | 13 |
| Apple muffin, made with rolled oats and without sugar | 48 | 60 | 9 |
| Waffles, Aunt Jemima® | 76 | 35 | 10 |
| Bagel, white, frozen | 72 | 70 | 25 |
| Baguette, white, plain | 95 | 30 | 14 |
| Coarse barley bread, 80% kernels | 34 | 30 | 7 |
| Hamburger bun | 61 | 30 | 9 |
| Kaiser roll | 73 | 30 | 12 |
| Pumpernickel bread | 56 | 30 | 7 |
| 50% cracked wheat kernel bread | 58 | 30 | 12 |
| White wheat flour bread, average | 75 | 30 | 11 |
| Wonder® bread, average | 73 | 30 | 10 |
| Whole wheat bread, average | 69 | 30 | 9 |
| 100% Whole Grain® bread (Natural Ovens) | 51 | 30 | 7 |
| Pita bread, white | 68 | 30 | 10 |
| Corn tortilla | 52 | 50 | 12 |
| Wheat tortilla | 30 | 50 | 8 |
| BEVERAGES | |||
| Coca Cola® (US formula) | 63 | 250 mL | 16 |
| Fanta®, orange soft drink | 68 | 250 mL | 23 |
| Lucozade®, original (sparkling glucose drink) | 95 | 250 mL | 40 |
| Apple juice, unsweetened | 41 | 250 mL | 12 |
| Cranberry juice cocktail (Ocean Spray®) | 68 | 250 mL | 24 |
| Gatorade, orange flavor (US formula) | 89 | 250 mL | 13 |
| Orange juice, unsweetened, average | 50 | 250 mL | 12 |
| Tomato juice, canned, no sugar added | 38 | 250 mL | 4 |
| BREAKFAST CEREALS AND RELATED PRODUCTS | |||
| All-Bran®, average | 44 | 30 | 9 |
| Coco Pops®, average | 77 | 30 | 20 |
| Cornflakes®, average | 81 | 30 | 20 |
| Cream of Wheat® | 66 | 250 | 17 |
| Cream of Wheat®, Instant | 74 | 250 | 22 |
| Grape-Nuts® | 75 | 30 | 16 |
| Muesli, average | 56 | 30 | 10 |
| Oatmeal, average | 55 | 250 | 13 |
| Instant oatmeal, average | 79 | 250 | 21 |
| Puffed wheat cereal | 80 | 30 | 17 |
| Raisin Bran® | 61 | 30 | 12 |
| Special K® (US formula) | 69 | 30 | 14 |
| GRAINS | |||
| Pearled barley, average | 25 | 150 | 11 |
| Sweet corn on the cob | 48 | 60 | 14 |
| Couscous | 65 | 150 | 9 |
| Quinoa | 53 | 150 | 13 |
| White rice, boiled, type non-specified | 72 | 150 | 29 |
| Quick cooking white basmati | 63 | 150 | 26 |
| Brown rice, steamed | 50 | 150 | 16 |
| Parboiled Converted white rice (Uncle Ben’s®) | 38 | 150 | 14 |
| Whole wheat kernels, average | 45 | 50 | 15 |
| Bulgur, average | 47 | 150 | 12 |
| COOKIES AND CRACKERS | |||
| Graham crackers | 74 | 25 | 13 |
| Vanilla wafers | 77 | 25 | 14 |
| Shortbread | 64 | 25 | 10 |
| Rice cakes, average | 82 | 25 | 17 |
| Rye crisps, average | 64 | 25 | 11 |
| Soda crackers | 74 | 25 | 12 |
| DAIRY PRODUCTS AND ALTERNATIVES | |||
| Ice cream, regular, average | 62 | 50 | 8 |
| Ice cream, premium (Sara Lee®) | 38 | 50 | 3 |
| Milk, full-fat, average | 31 | 250 mL | 4 |
| Milk, skim, average | 31 | 250 mL | 4 |
| Reduced-fat yogurt with fruit, average | 33 | 200 | 11 |
| FRUITS | |||
| Apple, average | 36 | 120 | 5 |
| Banana, raw, average | 48 | 120 | 11 |
| Dates, dried, average | 42 | 60 | 18 |
| Grapefruit | 25 | 120 | 3 |
| Grapes, black | 59 | 120 | 11 |
| Oranges, raw, average | 45 | 120 | 5 |
| Peach, average | 42 | 120 | 5 |
| Peach, canned in light syrup | 52 | 120 | 9 |
| Pear, raw, average | 38 | 120 | 4 |
| Pear, canned in pear juice | 44 | 120 | 5 |
| Prunes, pitted | 29 | 60 | 10 |
| Raisins | 64 | 60 | 28 |
| Watermelon | 72 | 120 | 4 |
| BEANS AND NUTS | |||
| Baked beans | 40 | 150 | 6 |
| Black-eyed peas | 50 | 150 | 15 |
| Black beans | 30 | 150 | 7 |
| Chickpeas | 10 | 150 | 3 |
| Chickpeas, canned in brine | 42 | 150 | 9 |
| Navy beans, average | 39 | 150 | 12 |
| Kidney beans, average | 34 | 150 | 9 |
| Lentils | 28 | 150 | 5 |
| Soy beans, average | 15 | 150 | 1 |
| Cashews, salted | 22 | 50 | 3 |
| Peanuts | 13 | 50 | 1 |
| PASTA and NOODLES | |||
| Fettucini | 32 | 180 | 15 |
| Macaroni, average | 50 | 180 | 24 |
| Macaroni and Cheese (Kraft®) | 64 | 180 | 33 |
| Spaghetti, white, boiled, average | 46 | 180 | 22 |
| Spaghetti, white, boiled 20 min | 58 | 180 | 26 |
| Spaghetti, whole-grain, boiled | 42 | 180 | 17 |
| SNACK FOODS | |||
| Corn chips, plain, salted | 42 | 50 | 11 |
| Fruit Roll-Ups® | 99 | 30 | 24 |
| M & M’s®, peanut | 33 | 30 | 6 |
| Microwave popcorn, plain, average | 65 | 20 | 7 |
| Potato chips, average | 56 | 50 | 12 |
| Pretzels, oven-baked | 83 | 30 | 16 |
| Snickers Bar®, average | 51 | 60 | 18 |
| VEGETABLES | |||
| Green peas | 54 | 80 | 4 |
| Carrots, average | 39 | 80 | 2 |
| Parsnips | 52 | 80 | 4 |
| Baked russet potato | 111 | 150 | 33 |
| Boiled white potato, average | 82 | 150 | 21 |
| Instant mashed potato, average | 87 | 150 | 17 |
| Sweet potato, average | 70 | 150 | 22 |
| Yam, average | 54 | 150 | 20 |
| MISCELLANEOUS | |||
| Hummus (chickpea salad dip) | 6 | 30 | 0 |
| Chicken nuggets, frozen, reheated in microwave oven 5 min | 46 | 100 | 7 |
| Pizza, plain baked dough, served with parmesan cheese and tomato sauce | 80 | 100 | 22 |
| Pizza, Super Supreme (Pizza Hut®) | 36 | 100 | 9 |
| Honey, average | 61 | 25 | 12 |
Footnotes: This kind of list does have its limitations. The GI value relates to the food eaten on its own and in practice you usually eat foods in combination as meals. Bread, for example is usually eaten with butter or vegetable-oil based spread, and potatoes could be eaten with meat and vegetables. An additional problem is that GI compares the glycemic effect of an amount of food containing 50g of carbohydrate but in real life you eat different amounts of food containing different amounts of carbohydrate. The amount of carbohydrate you eat has a bigger effect on blood glucose levels than GI alone.
Eat more fish
Try to eat fish regularly, as it’s good for you and the development of your baby. Fish are part of a healthy eating pattern and provide 10:
- Protein
- Healthy omega-3 fats (called DHA and EPA)
- More vitamin B12 and vitamin D than any other type of food
- Iron which is important for infants, young children, and women who are pregnant or who could become pregnant
- Other minerals like selenium, zinc, and iodine.
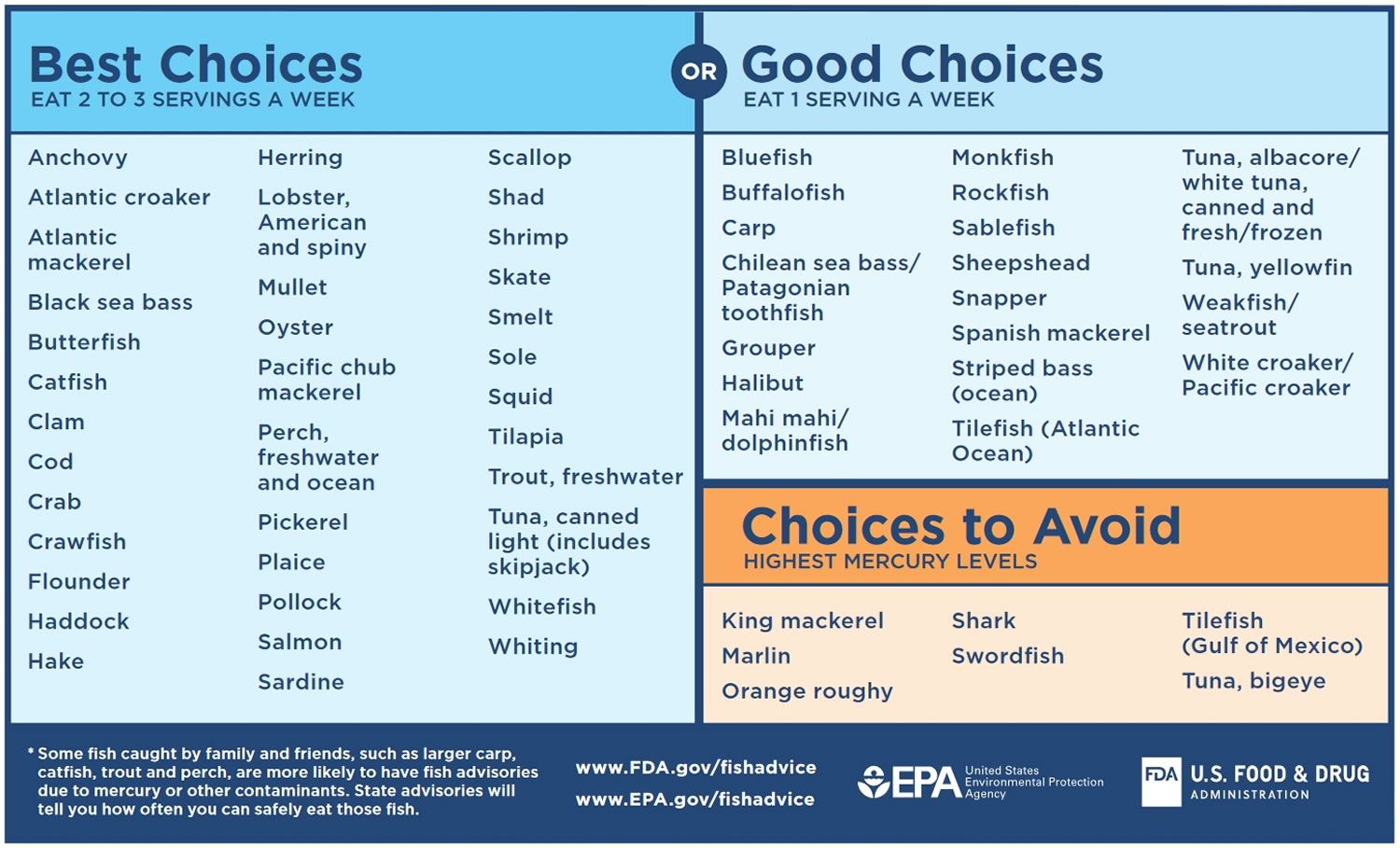
The advice is to eat at least 2 to 3 servings (between 8 and 12 ounces) of fish a week from the “Best Choices” list OR 1 serving (4 ounces) from the “Good Choices” list on the chart in Figure 1 below, including at least one portion of oily fish – like mackerel, sardines, salmon, herrings, trout or pilchards. Oily fish is really good for heart health, but don’t have more than two portions a week because it contains low levels of pollutants (toxins). A portion is about 140g.
Avoid fish which tend to have higher levels of mercury, like swordfish, shark and marlin. And, don’t have more than four medium-sized cans of tuna, or two tuna steaks a week, as it can have relatively high amounts of mercury compared to other fish.
There are some foods you should avoid when you’re pregnant, including raw shellfish.
Figure 1. Eating fish for Women Who Are or Might Become Pregnant, Breastfeeding Mothers, and Young Children
[Source 10 ]Protein in pregnancy
Foods containing protein help your baby grow. Sources of protein include meat (but avoid liver), fish (however, avoid fish that is high in mercury such as shark/flake, marlin or broadbill/ swordfish), poultry, eggs, beans, legumes/beans and nuts. Eat some protein every day. Choose lean meat, remove the skin from poultry, and cook it using only a little fat.
Make sure eggs, poultry, pork, burgers and sausages are cooked all the way through. Check that there is no pink meat, and that juices have no pink or red in them. Try to eat 2 portions of fish a week, one of which should be oily fish such as sardines or mackerel. There are some types of fish you should avoid when you’re pregnant or planning to get pregnant, including shark, swordfish and marlin.
Eat some protein-rich foods every day. Sources of protein include:
- beans
- pulses
- fish
- eggs
- meat (but avoid liver)
- poultry
- nuts
Choose lean meat, remove the skin from poultry, and try not to add extra fat or oil when cooking meat.
You should avoid eating some raw or partially cooked eggs, as there is a risk of salmonella.
Foods to avoid in pregnancy
Most foods and drinks are safe to have during pregnancy. But there are some things you should be careful with or avoid.
Cheese, milk and other dairy
Unpasteurized dairy products may contain listeria. This bacteria can causes an infection called listeriosis. There’s a small chance listeriosis can lead to miscarriage, stillbirth, or make your newborn baby very unwell.
Soft cheeses with a white coating on the outside have more moisture. This can make it easier for bacteria to grow.
What to avoid
- mold-ripened soft cheeses with a white coating on the outside, such as brie, camembert and chèvre (unless cooked until steaming hot)
- soft blue cheeses such as danish blue, gorgonzola and roquefort (unless cooked until steaming hot)
- any unpasteurized cows’ milk, goats’ milk or sheep’s milk
- any foods made from unpasteurized milk, such as soft goats’ cheese
Meat and poultry
There’s a small risk of getting toxoplasmosis if you eat raw and undercooked meat, which can cause miscarriage.
Cured meats are not cooked, so they may have parasites in them that cause toxoplasmosis.
Liver and liver products have lots of vitamin A in them. This can be harmful to an unborn baby.
Game meats may contain lead shot.
What to be careful with:
- cold cured meats, such as salami, pepperoni, chorizo and prosciutto (unless cooked thoroughly)
What to avoid:
- raw or undercooked meat
- liver and liver products
- all types of pâté, including vegetarian pâté
- game meats such as goose, partridge or pheasant
Eggs
What to avoid:
- raw or partially cooked eggs that are not British Lion
- duck, goose or quail eggs, unless cooked thoroughly until the whites and yolks are solid
Salmonella is unlikely to harm your unborn baby, but you could get food poisoning.
Caffeine
You can have caffeine, but no more than 200mg per day.
There is:
- 100mg in a mug of instant coffee
- 140mg in a mug of filter coffee
- 75mg in a mug of tea (green tea can have the same amount of caffeine as regular tea)
- 40mg in a can of cola
- 80mg in a 250ml can of energy drink
- less than 25mg in a 50g bar of plain dark chocolate
- less than 10mg in a 50g bar of plain milk chocolate
Alcohol
Drinking alcohol in pregnancy can lead to long-term harm to your baby.
If you’re pregnant or planning to get pregnant, the safest approach is to not drink alcohol at all.
This keeps risks to your baby to a minimum.
Keeping active
For women with gestational diabetes, moderate intensity physical activity can help to manage blood glucose levels. ‘Moderate’ means a slight but noticeable increase in breathing and heart rate. If there are no specific obstetric or medical conditions, you should be able to safely exercise during pregnancy. However, it is best to discuss this with your obstetrician or midwife prior to commencing any exercise regime in pregnancy.
It’s never too late to start moving, and there are many ways that you can keep active as a part of your everyday routine. Basically, anything that gets you moving is generally good for your diabetes and will also improve your overall feeling of wellbeing. For example, walking is a great way to move.
Benefits of keeping active
- Physical activity helps to reduce insulin resistance. Regular exercise, like walking, helps to increase fitness and prepares you for the birth of your baby. Physical activity also helps manage blood glucose levels. Remember, before starting or continuing any form of physical activity, always check with your obstetrician or midwife.
Below are some tips on how you can incorporate more walking into your life. It is important never to exert yourself.
- Walking to the local shops instead of driving.
- Start a ‘walking group’ with family or friends – perhaps meet at a regular time and day. This will help make sure you’re committed and help you stay in touch with your loved ones.
- Take the stairs instead of the elevator.
- Stand and move while on the phone.
- Garden.
- Buy a ‘pedometer’ (or a ‘step counter’), a small device you can clip to yourself that counts your daily steps. This will help you measure just how much walking you’re doing.
Manage your weight
If you gain too much weight in pregnancy it can affect your health and increase your blood pressure. However, evidence suggests that pregnancy isn’t the time to be on a really strict diet and you shouldn’t aim to lose weight. But it’s important that your weight is monitored by your care team and you don’t gain too much weight, which could cause problems for you and your baby.
Making changes to your diet and physical activity levels can help you avoid gaining too much weight. It’ll also help you to keep your blood sugar within a safe range.
It’s important to keep going with your healthier lifestyle after you’ve had your baby and keep to a healthy weight. This will reduce your risk of developing gestational diabetes in future pregnancies. And, it will also help to reduce your future risk of developing type 2 diabetes too.
Gestational diabetes diet plan
To manage your blood glucose, you need to balance what you eat and drink with physical activity. What you choose to eat, how much you eat, and when you eat are all important in keeping your blood glucose level in the range that your health care team recommends. Try to include protein foods with each of your main meals, to help fill you up and help manage your sugar levels.
Eating well and being physically active most days of the week can help you:
- keep your blood glucose level, blood pressure, and cholesterol in your target ranges
- lose weight if you’re overweight or stay at a healthy weight
- prevent or delay diabetes problems
- feel good and have more energy
Breakfast
- A bowl of wholegrain cereal, such as porridge, with semi-skimmed milk
- 2 slices of wholegrain toast with unsaturated low-fat spread
- Low-fat and low-sugar yogurt and fruit.
Or you could try making:
- Apple and cinnamon fruity porridge
- Wholemeal spinach and cheddar pancakes
- Mushroom and spring onion omelette.
Lunch
- An egg, cheese, fish or chicken salad sandwich, made with wholegrain bread or chapatti/roti made with wholemeal flour
- A small pasta salad, with plenty of veggies
- Soup – containing lots of veggies and pulses – with a wholegrain roll. Some soup contains lots of added salt and sugar so check the label.
Or you could try making:
- Cauliflower pizza
- Chicken and soya bean salad
- Cauliflower pilaf
- Chickpea and tuna salad
- Tuna niçoise salad
- Greek style chicken pittas
Dinner
- Thai chicken stir fry
- Butternut and borlotti bean stew
- Mixed bean chilli
- Chicken, squash and coriander pilaf
- Aubergine stuffed with tofu, mushrooms and borlotti beans
- Aubergine and parmesan bake
- Italian style braised lamb steaks
- Channa dahl
- Chicken balti
Try serving dinners with cauliflower pilaf instead of rice.
Gestational diabetes meal plan
A meal plan is your guide for when, what, and how much to eat to get the nutrition you need while keeping your blood sugar levels in your target range. Following a meal plan will help you manage your blood glucose, blood pressure, and cholesterol. A good meal plan will consider your goals, tastes, and lifestyle, as well as any medicines you’re taking. There are many factors to think about before starting any meal plan. It is best to ask your diabetes health care team to help you make a diabetes meal plan. This is especially important if you treat your condition with insulin and diabetes medications that increase the risk of hypos (low blood sugar levels). Reducing your carbohydrate intake and changes to your body weight may mean your insulin and diabetes medication needs to be adjusted.
A good meal plan will include:
- More nonstarchy vegetables, such as broccoli, spinach, and green beans.
- Focusing on whole foods instead of highly processed foods as much as possible.
- Choosing foods that are lower in calories, saturated fat, trans fat, sugar, and salt.
- Choosing fruits and vegetables, beans, whole grains, chicken or turkey without the skin, fish, lean meats, and nonfat or low-fat milk and cheese.
- Drinking water instead of sugar-sweetened beverages.
- Fewer added sugars and refined grains, such as white bread, rice, and pasta with less than 2 grams of fiber per serving.
Carbohydrates in the food you eat raise your blood sugar levels. How fast carbs raise your blood sugar depends on what the food is and what you eat with it. For example, drinking fruit juice raises blood sugar faster than eating whole fruit. Eating carbs with foods that have protein, fat, or fiber slows down how quickly your blood sugar rises.
Monday
- Breakfast: Baked eggs with two slices of rye bread
- Lunch: Chilli bean soup with avocado salsa
- Dinner: Mackerel tomatoes served with leeks and broccoli
- Pudding: Apple strudel
- Snacks: Greek yogurt, two satsumas, plain almonds, one apple
- Milk: 225ml semi-skimmed milk. Any dairy alternative should be unsweetened and fortified with calcium.
Tuesday
- Breakfast: Porridge made with 30g porridge oats, 200ml almond milk, 40g blueberries and 10g pumpkin seeds
- Lunch: Bang bang chicken salad
- Dinner: Minced beef and vegetable filo pie
- Pudding: 80g strawberries
- Snacks: Avocado, brazil nuts, celery and peanut butter
- Milk: 225ml semi-skimmed milk. Any dairy alternative should be unsweetened and fortified with calcium.
Wednesday
- Breakfast: Mushroom and spring onion omelette
- Lunch: Butterbean paté with carrots, tomatoes and mini wholemeal pitta bread
- Dinner: Aubergine and courgette parmesan bake with rocket, tomato and tinned kidney beans
- Pudding: 80g melon
- Snacks: One apple and peanut butter, one pear with almonds, natural yogurt and pumpkin seeds
- Milk: 225ml semi-skimmed milk. Any dairy alternative should be unsweetened and fortified with calcium.
Thursday
- Breakfast: Summerberry smoothie
- Lunch: Chickpea and tuna salad
- Dinner: Chicken tikka masala and cauliflower pilaf
- Pudding: Summer berry posset
- Snacks: Greek yogurt, two satsumas, one orange, almonds, two oatcakes topped with smooth peanut butter
- Milk: 225ml semi-skimmed milk. Any dairy alternative should be unsweetened and fortified with calcium.
Friday
- Breakfast: Baked eggs with two slices of rye bread
- Lunch: Two slices of medium wholemeal bread with grated cheddar, vegetable oil-based spread, tomato and cucumber
- Dinner: Grilled salmon steak with baked sweet potato, broccoli and cabbage
- Pudding: Sugar-free jelly
- Snacks: raspberries, melon, avocado, plain almonds
- Milk: 225ml semi-skimmed milk. Any dairy alternative should be unsweetened and fortified with calcium.
Saturday
- Breakfast: Welsh leek rarebit
- Lunch: Cauliflower and leek soup with 25g cheddar
- Dinner: Butternut squash and borlotti bean stew
- Pudding: Tinned peaches in juice
- Snacks: One apple, 30g almonds, Greek yogurt, small pear and almonds, 60g pistachios with shells
- Milk: 225ml semi-skimmed milk. Any dairy alternative should be unsweetened and fortified with calcium.
Sunday
- Breakfast: Omelette made with two eggs and milk along with 80g spinach, 80g mushrooms, 1tsp of vegetable oil, 25g grated cheddar. Pair with a slice of rye bread with 1tsp of unsaturated margarine
- Lunch: Smoked mackerel on granary toast with 1sp of veg spread, rocket, tomato and cucumber.
- Dinner: Greek homestyle chicken with broccoli and leeks
- Pudding: 80g raspberries and 80g melon
- Snacks: Low-fat Greek yogurt with almonds and pumpkin seeds, spicy roasted chickpeas, one small pear
- Milk: 225ml semi-skimmed milk. Any dairy alternative should be unsweetened and fortified with calcium.
- Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Alison B. Evert, Michelle Dennison, Christopher D. Gardner, W. Timothy Garvey, Ka Hei Karen Lau, Janice MacLeod, Joanna Mitri, Raquel F. Pereira, Kelly Rawlings, Shamera Robinson, Laura Saslow, Sacha Uelmen, Patricia B. Urbanski, William S. Yancy. Diabetes Care May 2019, 42 (5) 731-754; DOI: 10.2337/dci19-0014
- Food for Thought. Key Takeaways from ADA’s Nutrition Consensus Report. https://www.diabetes.org/sites/default/files/2019-10/ADV_2019_Consumer_Nutrition_One%20Pager.pdf
- Wier LM, Witt E, Burgess J, Elixhauser A. Hospitalizations related to diabetes in pregnancy, 2008. HCUP Statistical Brief #102. December 2010. Rockville, Md.: Agency for Healthcare Research and Quality. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb102.pdf
- Hartling L, Dryden DM, Guthrie A, et al. Screening and Diagnosing Gestational Diabetes Mellitus. Rockville (MD): Agency for Healthcare Research and Quality (US); 2012 Oct. (Evidence Reports/Technology Assessments, No. 210.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK114844
- Screening, Diagnosis, and Management of Gestational Diabetes Mellitus. Am Fam Physician. 2015 Apr 1;91(7):460-467. https://www.aafp.org/afp/2015/0401/p460.html
- Butte NF. Carbohydrate and lipid metabolism in pregnancy: normal compared with gestational diabetes mellitus. Am J Clin Nutr. 2000;71(5 suppl):1256S–1261S.
- American Diabetes Association. Management of diabetes in pregnancy. Section 12 in Standards of Medical Care in Diabetes—2016. Diabetes Care. 2016;39(1)(suppl 1):S94–S98.QC
- ACOG Committee on Practice Bulletins. ACOG practice bulletin. Clinical management guidelines for obstetrician-gynecologists. Number 60, March 2005. Pregestational diabetes mellitus. Obstetrics and Gynecology. 2005;105(3):675–685.
- Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the Diabetes Prevention Program Outcomes Study. The Lancet Diabetes & Endocrinology. 2015;3(11):866‒875.
- ADVICE ABOUT EATING FISH. For Women Who Are or Might Become Pregnant, Breastfeeding Mothers, and Young Children. https://www.fda.gov/media/102331/download