Hemoperitoneum
Hemoperitoneum (plural: haemoperitoneums) is the presence of blood within the peritoneal cavity. The blood accumulates in the space between the inner lining of the abdominal wall and the internal abdominal organs. Hemoperitoneum is generally classified as a surgical emergency; in most cases, urgent laparotomy is needed to identify and control the source of the bleeding. In selected cases, careful observation may be permissible. The abdominal cavity is highly distensible and may easily hold greater than five liters of blood, or more than the entire circulating blood volume for an average-sized individual. Therefore, large-scale or rapid blood loss into the abdomen will reliably induce hemorrhagic shock and may, untreated, rapidly lead to death. CT is the imaging modality of choice because of its ability to help distinguish blood from other fluids 1. The crucial initial steps for the radiologist are to use the various CT signs to detect the presence of intraperitoneal blood, locate the source of hemorrhage, and determine whether emergent intervention is indicated. After these steps are completed, a differential diagnosis may be generated on the basis of the clinical history and radiologic findings.
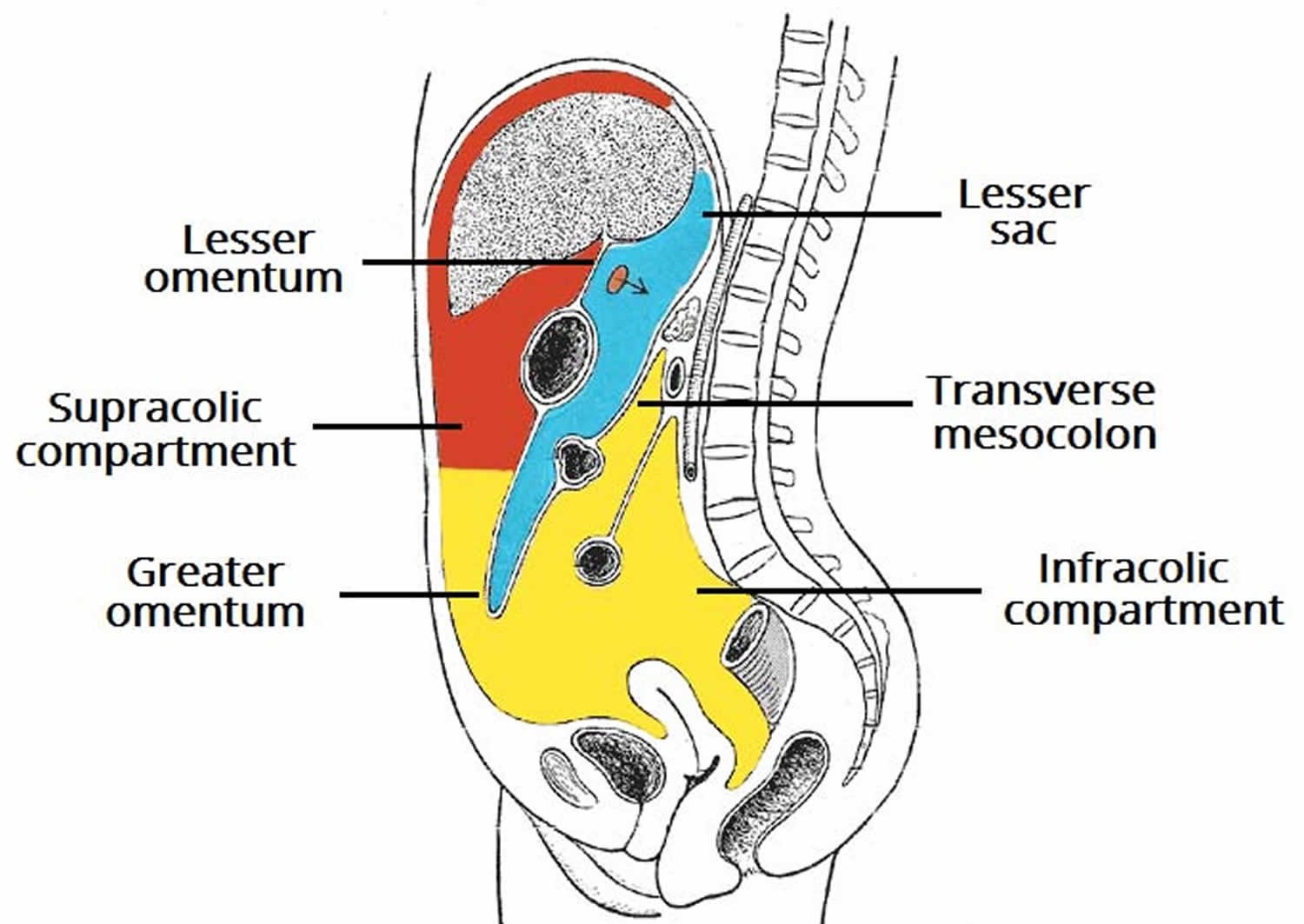
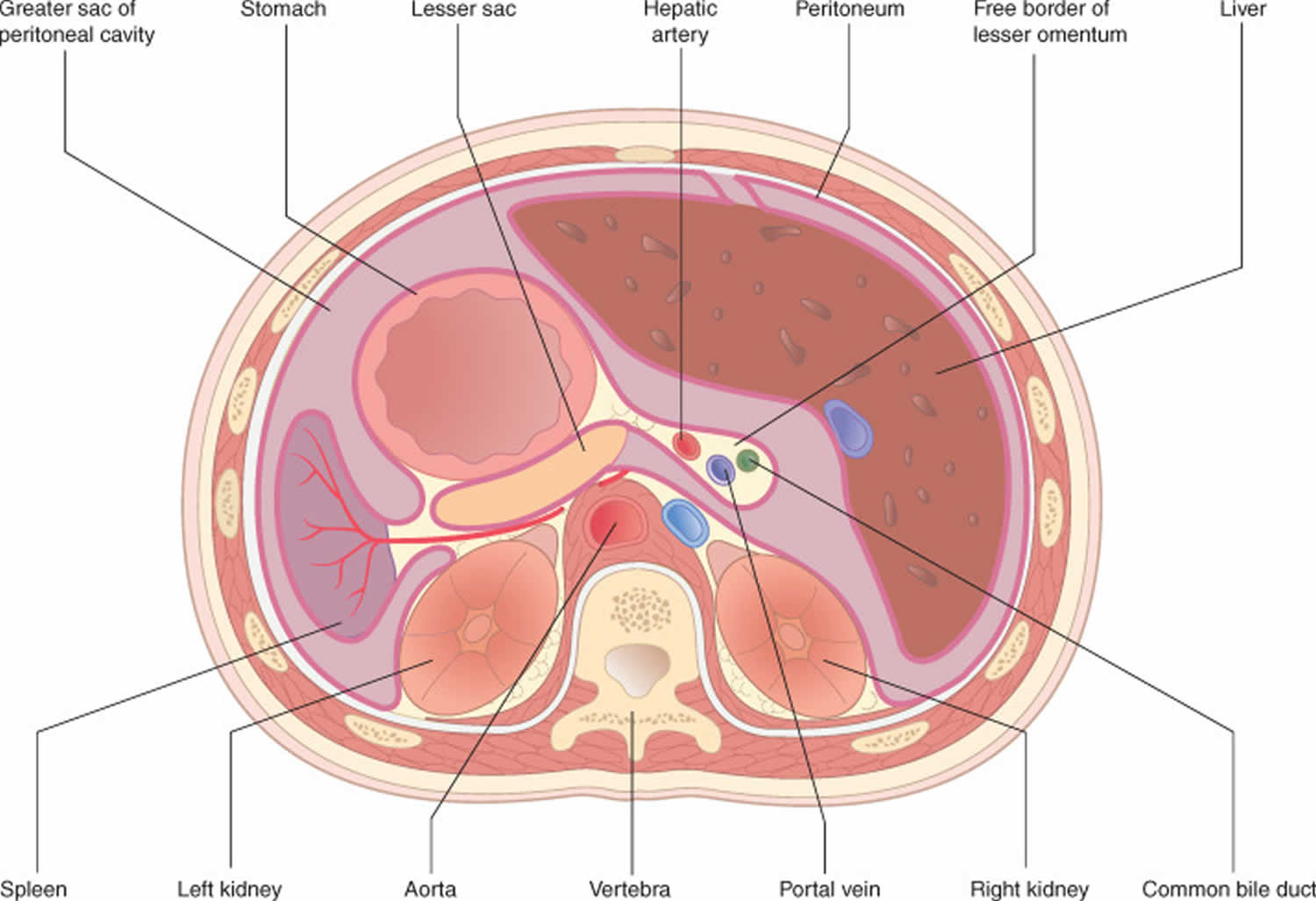
In the abdomen, there is a thin membrane that surrounds the outer abdominal wall called the parietal peritoneum. Additionally, there is a separate thin membrane that surrounds all the organs in the abdomen, enclosing all the organs in a bag-like membrane. This membrane is called the visceral peritoneum. The space between the parietal peritoneum and the visceral peritoneum is a space called the peritoneal cavity.
The peritoneal cavity contains the liver, spleen, bowel, stomach, and mesentery. In the supine position, the most dependent portion of the abdomen is the hepatorenal fossa (Morison pouch), and the most dependent portion of the pelvis is the pelvic cul-de-sac (pouch of Douglas). Hemoperitoneum starts near the site of injury and flows along expected anatomic pathways. Hemorrhage from the liver typically flows in a caudal direction from the perihepatic spaces and hepatorenal fossa, along the right paracolic gutter, and into the cul-de-sac, which is the rectouterine space in women and rectovesical space in men (Figure 2). Similarly, hemorrhage from the spleen typically flows in a caudal direction from the perisplenic spaces, along the left paracolic gutter, and into the pelvis 2. A large volume of blood may collect in the pelvis without an obvious hematoma surrounding the source organ. Thus, the appearance of the cul-de-sac is crucial to the diagnosis of hemoperitoneum. Small amounts of fluid or blood in this region may be the only sign of an intraperitoneal injury and should prompt a careful inspection of images of the viscera 3.
There are many situations that can cause blood to accumulate in the peritoneal cavity, ultimately leading to hemoperitoneum. These situations include the following:
- Blunt force trauma to the abdomen (such as the bat hitting Jack in the stomach)
- Penetrating trauma to the abdomen
- Injuries to an organ such as the spleen, liver, or pancreas
Less commonly, hemoperitoneum may have a nontraumatic origin. Iatrogenic hemoperitoneum may occur as a complication of surgery or other interventional procedures in the abdominal cavity or as a result of anticoagulation therapy. Hemoperitoneum also may be seen in the setting of blood dyscrasias such as hemophilia and polycythemia vera. Tumor-associated hemorrhage, which most often occurs in hepatocellular carcinoma, hepatic adenoma, or vascular metastatic disease, also may produce hemoperitoneum. Other potential causes of nontraumatic hemoperitoneum are gynecologic conditions such as hemorrhage or rupture of an ovarian cyst and rupture of the gestational sac in ectopic pregnancy, and hepatic hematoma in syndromic hemolysis with elevated liver enzymes and low platelet count (HELLP syndrome). Vascular lesions (visceral artery aneurysms and pseudoaneurysms) that occur in systemic vascular diseases such as Ehlers-Danlos syndrome or in pancreatitis are another less common source of hemoperitoneum.
It is important to bear in mind that, in trauma cases, significant abdominal injuries may be present without apparent hemoperitoneum. For example, intraparenchymal lacerations or contusions may be present without penetration of the organ capsule. Knowledge of the relationship of abdominal organs to the surrounding peritoneal spaces is crucial. For example, because the bare area of the liver is contiguous with the retroperitoneum, retroperitoneal fluid rarely may be the only sign of hepatic injury, although intraperitoneal fluid is more commonly seen in cases of solid organ injury. In a patient with abdominal trauma, a CT finding of free intraperitoneal fluid without solid organ injury should arouse suspicion about the possible presence of a bowel laceration or perforation 4.
Most cases of hemoperitoneum are benign 5. Uncommonly, hemoperitoneum is a sign of underlying intraperitoneal pathology. In these patients, bleeding often persists beyond 36 hours. Fewer than 25% of cases have major hemorrhage and need transfusion or surgical intervention. An initial assessment includes a good history, including details of menstruation, recent trauma, and use of anticoagulant or antiplatelet drugs. The patient should undergo assessment of the hemodynamic status, and be evaluated for signs of an abdominal catastrophe. Subsequent evaluation is often dictated by this initial assessment.
The management of hemoperitoneum is directed at the underlying cause.
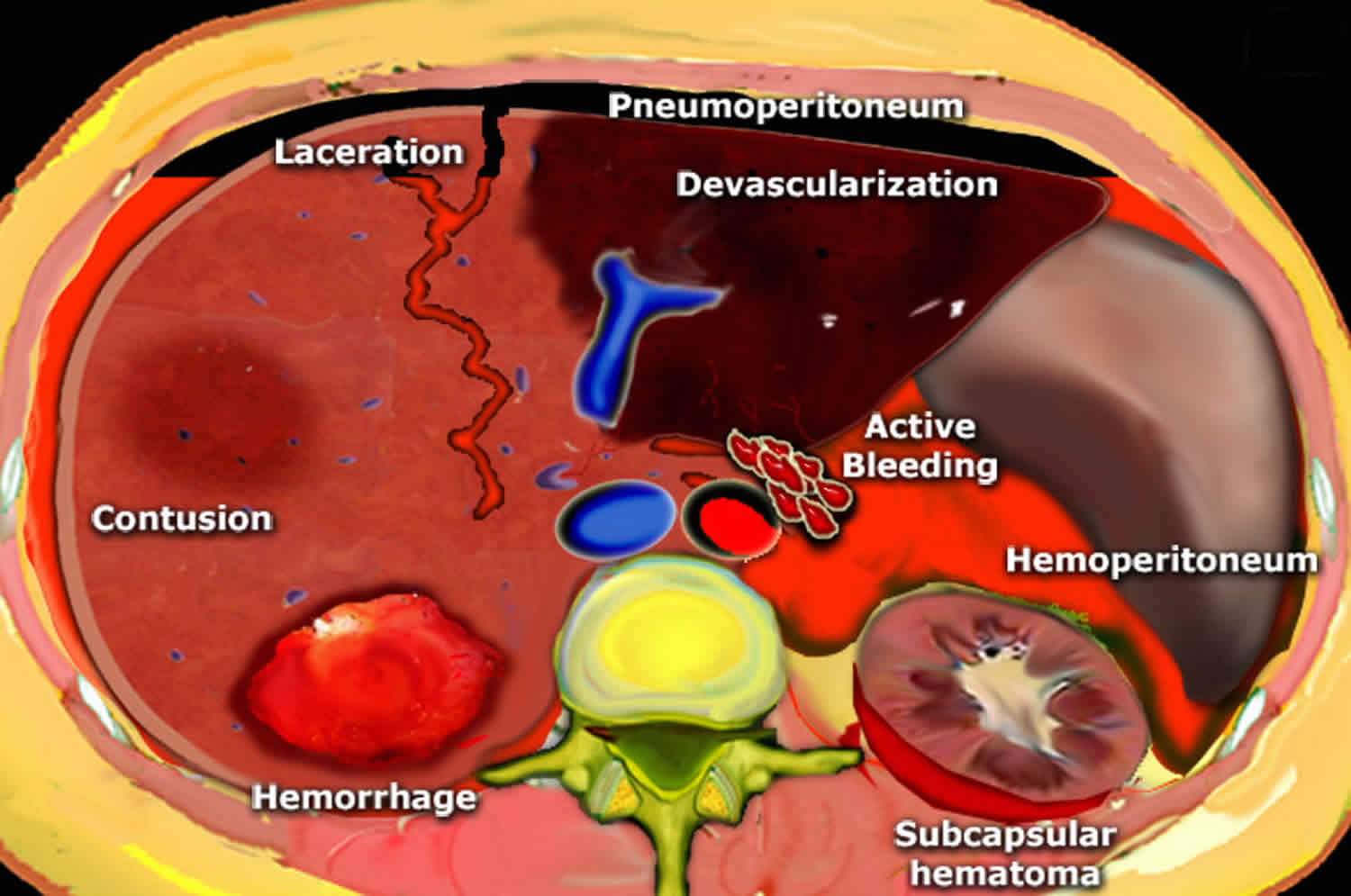
Figure 1. Peritoneal cavity
Figure 2. Massive hemoperitoneum
Footnote: Typical flow pattern of hemorrhage from a liver laceration. (a) Contrast material–enhanced CT image shows high-attenuation fluid (arrows) in perihepatic and perisplenic regions, the hepatorenal fossa, and the lesser sac. (b) Contrast-enhanced CT image at a lower level than a shows blood tracking laterally along the paracolic gutters (arrows).
Hemoperitoneum causes
There are numerous causes of hemoperitoneum in both traumatic and nontraumatic settings.
Hemoperitoneum causes include:
- Penetrating abdominal trauma (often with associated organ injury) 6
- Blunt trauma, most commonly injuries to solid organs such as the liver and spleen.
- Gynecologic disorders
- Ruptured ectopic pregnancy
- Uterine rupture
- Ruptured corpus luteum or ruptured ovarian cyst in some cases.
- Aneurysm or pseudoaneurysm rupture e.g., rupture of an abdominal aortic aneurysm, iliac aneurysm, or splenic aneurysm.
- Bleeding due to rupture of an intra-abdominal neoplasm, (e.g., repatoblastoma, renal tumor)
- Acute hemorrhagic pancreatitis
- Acute cholecystitis
- Splenic rupture or infarction
- Iatrogenic e.g., postcolonoscopy
- Idiopathic
- Spontaneous bleeding, especially patients with coagulopathy or on anticoagulant therapy (uncommon) e.g., disseminated intravascular coagulation (DIC) 6
- Perforation of the colon
- Peritonitis
- Peritoneal membrane abnormalities
- Sclerosing peritonitis
- Peritoneal carcinomatosis
- Peritoneal calcification
- Radiation injury
- Rupture of hepatic or renal cysts
- IgA nephropathy
- Hepatic hematoma in syndromic hemolysis with elevated liver enzymes and low platelet count (HELLP syndrome)
- Less commonly, bleeding due to a perforated gastric ulcer.
Traumatic hemoperitoneum
Solid organ injury
The spleen is the most frequently injured organ in blunt abdominal trauma; splenic injuries account for 40% of abdominal organ injuries 7. Injuries to the liver account for 20% of solid organ injuries related to blunt abdominal trauma 8. However, the liver is the single most commonly injured organ when blunt and penetrating trauma are combined. There are numerous systems for classifying visceral injuries, all of which include the following categories, in some form: intraparenchymal contusion or hematoma, subcapsular hematoma, laceration, fracture, and vascular pedicle injury 9. In the trauma setting, CT can help accurately diagnose the type and extent of the primary injury, determine the presence and amount of hemoperitoneum, and detect associated injuries 10.
Traumatic injury to the right hepatic lobe, especially the posterior segment, is much more common than is left lobe trauma, whereas injury to the caudate lobe is rare. The presence of small amounts of contrast material in the liver or spleen with adjacent hemoperitoneum may be indicative of arterial injury or pseudoaneurysm formation and should prompt surgical or angiographic intervention. Poletti et al 11 reported that major vascular injury is more likely in the presence of high-grade liver lacerations that involve branches of the hepatic or portal veins or from which there is active bleeding, and these findings should prompt angiography. There is also a high likelihood of venous disruption and biliary injury in the presence of lacerations that extend into the region of the inferior vena cava or the major hepatic veins 12. Fang et al 13 showed a significant correlation between the need for surgical intervention and the presence of hepatic and intraperitoneal bleeding or parenchymal contrast material extravasation in association with hemoperitoneum.
Bowel and mesenteric injuries
Bowel and mesenteric injuries are found in approximately 5% of patients who undergo surgery for blunt abdominal trauma 14. Bowel and mesenteric injuries usually occur together but also may occur separately, with purely mesenteric avulsions sometimes seen in the setting of seat-belt-related injuries. Bowel injuries can be difficult to detect clinically; abdominal rigidity, pain, and decreased bowel sounds are found during the physical examination of only one-third of patients at initial presentation 15. Undiagnosed bowel injuries are associated with significant morbidity and mortality from peritonitis, sepsis, and hemorrhage 3.
CT has high accuracy for the detection of bowel and mesenteric injuries 16. Various investigators in previous studies reported sensitivity of 84%–94% and accuracy of 84%–99% for the diagnosis of bowel injury at CT 17. The presence of free air is a less common sign of bowel perforation than is the presence of free fluid, especially in cases of small-bowel injury; the intraluminal contents of the small bowel consist mostly of fluid rather than gas. More reliable signs of bowel or mesenteric injury are interloop fluid, mesenteric hematoma or infiltration, wall thickening with associated enhancement, and bowel wall discontinuity 18. Oral contrast material extravasation, though rare, is the most specific sign of bowel rupture. Active extravasation of intravenous contrast material can be seen in the setting of mesenteric vessel injury.
The intraperitoneal bowel segments that are most commonly affected by trauma are the portion of the jejunum near the ligament of Treitz and the portion of the ileum near the ileocecal valve, presumably because these segments are more fixed than the rest of the small bowel. Injury occurs more commonly on the antimesenteric side than on the mesenteric side.
Nontraumatic hemoperitoneum
Nontraumatic hemoperitoneum may occur spontaneously or may be iatrogenic. Spontaneous hemoperitoneum is an uncommon and often unsuspected condition that may be catastrophic if it is not promptly diagnosed and treated. It may be associated with severe abdominal pain and distention, a decreased hematocrit level, or, more rarely, hypovolemic shock 19. However, these signs may not be present or may be equivocal, and the hematocrit level in a serum sample obtained at initial presentation may not reflect the extent of a hemorrhage 20. In such cases, the diagnosis frequently is made on the basis of radiologic findings 21. Nontraumatic hemoperitoneum has various possible causes, including hemorrhage from a highly vascular neoplasm (tumor-associated hemorrhage), hemorrhage or rupture of an ovarian cyst, rupture of the gestational sac or other affected anatomic part in an ectopic pregnancy, and bleeding from a vascular lesion such as an arterial aneurysm. Nontraumatic hemoperitoneum also may result from anticoagulation therapy, surgery, or an invasive procedure.
In nontraumatic hemoperitoneum, as in traumatic hemoperitoneum, it is critical to identify any active bleeding. A finding of active bleeding should lead to the abandonment of a conservative management strategy in favor of surgical or endovascular intervention. After active bleeding has been excluded, a careful search should be undertaken for the source of hemoperitoneum (,35).
Iatrogenic causes
Any surgical procedure performed within the peritoneal cavity may be complicated by hemoperitoneum. Even minimally invasive percutaneous or endovascular procedures occasionally lead to intraperitoneal hemorrhage.
Bleeding diatheses are common in patients who are undergoing anticoagulation therapy with heparin or coumadin. In most cases, the risk of bleeding is directly related to the intensity of the anticoagulant effect 22. Anticoagulation therapy most commonly causes hemorrhage into the psoas or rectus muscles, but it also occasionally results in hemoperitoneum. Hemoperitoneum due to rupture of the gallbladder or spleen has been reported in patients undergoing anticoagulation therapy 23. The use of CT to evaluate such patients for abdominal hemorrhage had a direct effect on clinical management for about one-half of the patients in one study, and positive and negative findings at CT were equally likely to affect management 24.
Like anticoagulation therapy, blood dyscrasias may alter coagulation status and lead to hemoperitoneum.
Tumor-associated hemorrhage
Spontaneous hemoperitoneum rarely occurs in the absence of trauma, a surgical or interventional procedure, or anticoagulation therapy 25. In such cases, the possibility of the rupture of an un-identified neoplasm must be excluded. Although the occurrence is uncommon, any primary or metastatic tumor can rupture and bleed into the peritoneal cavity.
The most common cause of nontraumatic hepatic hemorrhage is a hypervascular neoplasm such as hepatocellular carcinoma or hepatocellular adenoma 26. Hepatocellular carcinoma is commonly seen in the setting of cirrhosis or chronic hepatic inflammation and is the most common primary malignancy of a solid organ in the global population 27. Rupture has been reported to occur in 6.9%–14% of cases of hepatocellular carcinoma in Asia and Africa, where the prevalence of this type of cancer is high, and it is the most common cause of nontraumatic hemoperitoneum in male patients of all ages; however, ruptured hepatocellular carcinoma is less common in Europe and the United States 28. Patients with large or peripherally located tumors devoid of normal overlying tissue are at a higher risk for rupture 29. There also seems to be a higher likelihood of rupture in patients with both cirrhosis and hepatocellular carcinoma 30. In these cases, a wide spectrum of imaging findings can be seen, ranging from minor intrahepatic bleeding to subcapsular hemorrhage and rupture through the hepatic capsule into the peritoneum. Blood-tinged ascites is present in almost all cases 31. Necrosis and hemorrhage also may occur in less common hypervascular hepatic tumors, such as hepatic angiosarcoma 32. Hemangiomas, though common, are not associated with nontraumatic hemoperitoneum. A lesion that resembles a hemangioma on CT images obtained in a patient with nontraumatic hemoperitoneum may actually be an atypical angiomatous hepatic lesion such as an angiosarcoma.
The spontaneous rupture of a metastatic lesion in a solid organ is rare but usually results in massive hemoperitoneum 31. Lung carcinoma, renal cell carcinoma, and melanoma are the meta-static lesions that most often cause hemoperitoneum 25.
Hemoperitoneum associated with a benign neoplasm most often occurs with hepatic adenoma. These tumors are strongly associated with oral contraceptive use and estrogen steroid therapy; they most often are found in women of childbearing age who have a history of prolonged oral contraceptive use 33. The identification of a hepatic adenoma is essential, given the associated risk of life-threatening hemorrhage 34. Focal nodular hyperplasia, in contrast, is not usually accompanied by spontaneous hemorrhage. Large adenomas are prone to bleed 35, and because the tumor capsule is incomplete, a hemorrhage may spread into the liver or the abdominal cavity 36. For these reasons, although a very low rate of malignant degeneration has been reported, hepatic adenomas are surgically resected 37.
Pathologic splenic rupture may occur as a complication of a viral infection, including infection by cytomegalovirus, malaria, or Epstein-Barr virus 38; a congenital disease; a metabolic abnormality such as Gaucher disease or amyloidosis 39; and, rarely, a neoplastic process such as hemangiomatosis, angiosarcoma, leukemia, or lymphoma 40. The prevalence of bleeding has been correlated directly with increased splenic weight 40. At times, even seemingly minor trauma, such as that caused by lying prone, can induce hemorrhage in patients with splenomegaly.
Bleeding due to gynecologic conditions
The primary imaging modality used for the assessment of gynecologic conditions is US. However, CT is often requested if the clinical findings are nonspecific. The reproductive tract is the most common source of spontaneous hemoperitoneum in women of childbearing age. The most common gynecologic sources of bleeding are ectopic pregnancy and ruptured ovarian cyst 41. Hemoperitoneum also has been seen in the setting of endometriosis and uterine rupture, but such occurrences are uncommon 42.
A hemorrhagic ovarian cyst (usually, a corpus luteal or follicular cyst) is a frequent cause of acute pelvic pain in women of childbearing age 41. Accurate diagnosis of a hemorrhagic ovarian cyst is important because, although it rarely causes a clinically significant blood loss, the clinical manifestations may be confused with those of conditions that require immediate surgery, such as appendicitis 43. Hemorrhage into an ovarian cyst is a relatively common occurrence, but few hemorrhagic ovarian cysts rupture and cause hemoperitoneum 44. Fluid with internal echogenicity or high attenuation can be seen surrounding the uterus and adnexa in the presence of recent bleeding, and an associated mixed-attenuation adnexal mass with a high-attenuation component and at times a fluid-fluid level may be present 41.
Ectopic pregnancy can cause life-threatening bleeding and therefore must be considered in every woman of childbearing age who presents with abdominal or pelvic pain. Ectopic pregnancy accounts for up to 1% of pregnancies, with 97% of occurrences located in either the ampullary (most common) or the isthmic portion of the fallopian tube 45. Risk factors include previous ectopic pregnancy, pelvic inflammatory disease, in vitro fertilization, use of an intrauterine device, and tubal surgery 46. In the context of a positive human chorionic gonadotropin level of more than 2000 IU/L and no intrauterine pregnancy, the finding of an extraovarian mass is highly suggestive of an ectopic pregnancy 47. Hemoperitoneum in a patient with an ectopic pregnancy is not necessarily indicative of tubal rupture; however, the larger the amount of fluid, the higher the likelihood of tubal rupture 48.
HELLP syndrome is a peripartum condition that comprises the clinical triad of hemolysis, elevated liver enzymes, and low platelet count 49. Disseminated intravascular coagulation occurs in 20%–40% of patients with HELLP syndrome, and other complications, including hepatic infarction, hematoma, hepatic rupture, and placental abruption, may occur 50. CT may be the modality of choice for the demonstration of subcapsular hematoma, hepatic rupture, and hemoperitoneum 51. Hepatic infarction appears on CT images as a wedge-shaped peripheral area with low attenuation and without a mass effect 51.
Vascular sources
Intraperitoneal bleeding from vascular lesions (eg, ruptured abdominal aortic aneurysms) is less common than retroperitoneal hemorrhage from such lesions. However, abdominal aortic aneurysms with very large leaks occasionally result in bleeding that extends into the peritoneal cavity 52.
Splenic artery aneurysms account for 60% of visceral artery aneurysms 53. Splenic artery aneurysms are four times as common in women as they are in men, and the rate of rupture is particularly increased during pregnancy 54. Spontaneous rupture occurs in 3%–10% of splenic artery aneurysms and produces a high mortality rate, estimated to be approximately 36% 55. Hepatic artery aneurysms are the second most common type (20%) of visceral artery aneurysms 56. In young patients, splanchnic artery aneurysms should precipitate a thorough search for systemic vascular disease, most notably type IV Ehlers-Danlos syndrome. These patients may present with a spontaneous aneurysm rupture, and angiography may be contraindicated because of the risk of aneurysm formation at the site of puncture. Pseudoaneurysms of the hepatic, splenic, and gastroduodenal arteries are complications that must be excluded during an imaging evaluation for pancreatitis 57.
Hemoperitoneum signs and symptoms
Hemoperitoneum signs and symptoms depends on the underlying cause.
The history and physical exam serve to eliminate some diagnoses and suggest others. The immediate onset of pain suggests a vascular event such as mesenteric ischemia. Syncope hints at blood loss as from a ruptured ectopic or leaking abdominal aortic aneurysm (AAA). Various causes of hemoperitoneum have classic presentations.
Ruptured ectopic pregnancy signs and symptoms may include:
- Fainting or feeling faint
- Intense pressure in the rectum
- Low blood pressure
- Pain in the shoulder area
- Severe, sharp, and sudden pain in the lower abdomen
A ruptured fallopian tube can cause life-threatening internal bleeding. If you have sudden, severe pain; shoulder pain; or weakness, you should go to an emergency room.
Hemoperitoneum diagnosis
There are several different ways to diagnose hemoperitoneum. The following chart describes the various methods of diagnosing this condition.
- Ultrasound: An ultrasound is a procedure in which sound waves are used to produce images of the inside of the body (just like an ultrasound of a pregnant woman’s stomach is used to see the fetus). Ultrasounds can help to detect the presence of fluid/blood in the peritoneal cavity. For example, Focused Assessment with Sonography for Trauma (FAST).
- CT Scan: A CT scan (also known as a CAT scan) stands for ‘computerized axial tomography.’ This procedure produces cross-sectional x-rays of the inside of the body and can help detect the presence of fluid/blood in the peritoneal cavity.
- MRI: An MRI stands for ‘magnetic resonance imaging’ and involves the use of magnetic and radio waves to produce images of the inside of the body, which can help diagnose hemoperitoneum.
- Paracentesis or diagnostic peritoneal lavage: Diagnostic peritoneal lavage or diagnostic peritoneal aspiration is a surgical diagnostic procedure to determine if there is free floating fluid in the abdominal cavity.
- Diagnostic laparoscopy or exploratory laparotomy:
- Laparoscopy is an operation performed in the abdomen or pelvis using small incisions with the aid of a camera. The laparoscope aids diagnosis or therapeutic interventions with a few small cuts in the abdomen.
- Exploratory laparotomy is a surgical operation where the abdomen is opened and the abdominal organs examined for injury or disease. It is the standard of care in various blunt and penetrating trauma situations in which there may be multiple life-threatening injuries, and in many diagnostic situations in which the operation is undertaken in search of a unifying cause for multiple signs and symptoms of disease.
Hemoperitoneum treatment
Goals of therapy for patients with hemoperitoneum include maintenance and restoration of effective circulating volume, maintenance and restoration of oxygen‐carrying capacity, and arrest of hemorrhage. These goals can be achieved via fluid resuscitation, administration of blood products or hemoglobin‐based oxygen carriers, as well as application of abdominal counterpressure, and surgical intervention. Surgery usually is required for bleeding intra‐abdominal neoplasms. Emergency surgery is recommended for hemorrhaging patients with penetrating trauma, gastric dilatation and volvulus, bleeding cysts, liver lobe torsion, splenic torsion, and any other condition resulting in organ ischemia.
Initial management of massive hemoperitoneum consists of immediate blood transfusion if the patient is in hemorrhagic shock. Treatment for hemoperitoneum involves both the removal of the blood inside the peritoneal cavity and the stopping of the bleeding. Classically, hemoperitoneum was an indication for emergency surgery to locate the source of bleeding and also to recover spilled blood from the peritoneal cavity and to use it for auto-transfusion if it has not been contaminated by ruptured bowel contents. The method of control depends on the source of blood loss. Vascular bleeding, i.e. from a blood vessel, would be treated by clamping and ligation of the offending vessel, or repair of the vessel in the case of major arteries such as the aorta or mesenteric arteries. Bleeding from the spleen most often requires splenectomy, or removal of the spleen, usually but not always in the form of a total splenectomy. Bleeding from the liver might be controlled by application of hemostatic sponges, thrombin, or more recently, argon beam cauterization.
With modern diagnostic aids such as computed tomography (CT) scans, certain injuries such as low-grade lacerations of the spleen may be diagnosed early and observed, with surgical options deferred unless clinical deterioration obligates them. In rare occasions, rupture of an abdominal aortic aneurysm may be repaired via an endovascular technique, though this is generally not performed in the setting of acute rupture.
Hemoperitoneum method of treatment
- Paracentesis: Paracentesis involves inserting a large syringe into the peritoneal cavity. The plunger is then pulled back in order to draw the fluid from inside the peritoneal cavity into the syringe.
- Ligation: Ligation involves clamping or tying off a blood vessel that is ruptured and causing bleeding.
- Cauterization: Cauterization involves the burning of tissue in order to close the tissue off to stop the bleeding process.
- Medications: Coagulant medications (drugs that help to clot the blood) can be used to slow or stop bleeding.
- Laparotomy: Laparotomy involves making an incision into the abdomen to drain fluids that have accumulated in the abdomen. This procedure can also be used to diagnose hemoperitoneum.
Hemoperitoneum prognosis
Prognosis in patients with hemoperitoneum may depend on the underlying cause and concurrent injuries.
References- Blood in the Belly: CT Findings of Hemoperitoneum. Meghan Lubner, Christine Menias, Creed Rucker, Sanjeev Bhalla, Christine M. Peterson, Lisa Wang, and Brett Gratz. RadioGraphics 2007 27:1, 109-125 https://pubs.rsna.org/doi/pdf/10.1148/rg.271065042
- Shuman WP. CT of blunt abdominal trauma in adults. Radiology 1997;205:297–306.
- Shanmuganathan K. Multi-detector row CT imaging of blunt abdominal trauma. Semin Ultrasound CT MR 2004;25:180–204.
- Harris HW, Morabito DJ, Mackersie RC, et al. Leukocytosis and free fluid are important indicators of isolated intestinal injury after blunt trauma. J Trauma 1999;46:656–659.
- Handbook of Dialysis Therapy 4th edition 2008. ISBN 978-1-4160-4197-9 https://doi.org/10.1016/B978-1-4160-4197-9.X5001-7
- Lubner M, Menias C, Rucker C et-al. Blood in the belly: CT findings of hemoperitoneum. Radiographics. 27 (1): 109-25. doi:10.1148/rg.271065042
- Novelline RA, Rhea JT, Bell T. Helical CT of abdominal trauma. Radiol Clin North Am 1999;37: 591–612.
- Shanmuganathan K, Mirvis SE. CT evaluation of the liver with acute blunt trauma. Crit Rev Diagn Imaging 1995;36:73–113.
- Weishaupt D, Grozaj AM, Willman JK, et al. Traumatic injuries: imaging of abdominal and pelvic injuries. Eur Radiol 2002;12:1295–1311.
- Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR. Organ injury scaling: spleen and liver (1994 revision). J Trauma 1995;38:323–324.
- Poletti PA, Mirvis SE, Shanmuganathan K, et al. CT criteria for management of blunt liver trauma: correlation with angiographic and surgical findings. Radiology 2000;216:418–427.
- Savolaine ER, Grecos GP, Howard J, White P. Evolution of CT findings in hepatic hematoma. J Comput Assist Tomogr 1985;9:1090–1096.
- Fang JF, Chen RJ, Wong YC, et al. Classification and treatment of pooling of contrast material on computed tomographic scan of blunt hepatic trauma. J Trauma 2000;49:1083–1088.
- Rizzo MJ, Federle MP, Griffiths BG. Bowel and mesenteric injury following blunt abdominal trauma: evaluation with CT. Radiology 1989;173: 143–148.
- Donohue JH, Crass RA, Trunkey DD. Management of duodenal and small intestinal injury. World J Surg 1985;9:904–913.
- Nghiem HV, Jeffrey RB Jr, Mindelzun RE. CT of blunt trauma to the bowel and mesentery. AJR Am J Roentgenol 1993;160:53–58.
- Killeen KL, Shanmuganathan K, Poletti PA, et al. Helical computed tomography of bowel and mesenteric injuries. J Trauma 2001;51:26–36.
- Breen DJ, Janzen DL, Swirewich CV, Nagy AG. Blunt bowel and mesenteric injury: diagnostic performance of CT signs. J Comput Assist Tomogr 1997;21:706–712.
- McCort JJ. Intraperitoneal and retroperitoneal hemorrhage. Radiol Clin North Am 1976;14:391–405.
- Scott WW, Fishman EK, Siegelmann SS. Anticoagulants and abdominal pain: the role of computed tomography. JAMA 1984;252:2053–2056.
- Lucey BC, Varghese JC, Soto JA. Spontaneous hemoperitoneum: causes and significance. Curr Probl Diagn Radiol 2005;34:182–195.
- Coon WW, Wills PW 3rd. Hemorrhagic complications of anticoagulant therapy. Arch Intern Med 1974;133:386–392.
- Ghobrial MW, Karim M, Mannam S. Spontaneous splenic rupture following the administration of intravenous heparin: case report and retrospective case review. Am J Hematol 2002;71:314–317.
- Nazarian LN, Lev-Toaff AS, Spettell CM, Wechsler RJ. CT assessment of abdominal hemorrhage in coagulopathic patients: impact on clinical management. Abdom Imaging 1999;24:246–249.
- Casillas VJ, Amendola MA, Caascue A, Pinnar N, Levi JU, Perez JM. Imaging of nontraumatic hemorrhagic hepatic lesions. RadioGraphics 2000;20:367–388.
- Mortele KJ, Cantisani V, Brown DL, Ros PR. Spontaneous intraperitoneal hemorrhage: imaging features. Radiol Clin North Am 2003;41:1183–1201.
- Levy AD. Malignant liver tumors. Clin Liver Dis 2002;6:147–164.
- Fernandez MP, Redvanly RD. Primary hepatic malignant neoplasms. Radiol Clin North Am 1998;36:333–348.
- Kanematsu M, Imaeda T, Yamawaki Y, et al. Rupture of hepatocellular carcinoma: predictive value of CT findings. AJR Am J Roentgenol 1992; 158:1247–1250.
- Hirai K, Kawazoe Y, Yamashita K, et al. Transcatheter arterial embolization for spontaneous rupture of hepatocellular carcinoma. Am J Gastroenterol 1986;81:275–279.
- Miyamoto M, Sudo T, Kuyama T. Spontaneous rupture of hepatocellular carcinoma: a review of 172 Japanese cases. Am J Gastroenterol 1991;86:67–71.
- Molina E, Hernandez A. Clinical manifestations of primary hepatic angiosarcoma. Dig Dis Sci 2003;48:677–682.
- Rabe T, Feldmann K, Grunwald K, Runnebaum B. Liver tumours in women on oral contraceptives. Lancet 1994;344:1568–1569.
- Meissner K. Hemorrhage caused by ruptured liver cell adenoma following long term oral contraceptives: a case report. Hepatogastroenterology 1998; 45:224–225.
- Leese T, Farges O, Bismuth H. Liver cell adenomas: a 12-year surgical experience from a specialist hepato-biliary unit. Ann Surg 1988;208:558–564.
- Molina EG, Schiff ER. Benign solid lesions of the liver. In: Schiff ER, Sorrell MF, Maddrey WC, eds. Schiff’s diseases of the liver. 8th ed. Philadelphia, Pa: Lippincott-Raven, 1999; 1245–1267.
- Flowers BF, McBurney RP, Vero SR. Ruptured hepatic adenoma: a spectrum of presentation and treatment. Am Surg 1990;56:380–384.
- Bellaiche G, Habib E, Baledent F, et al. Hemoperitoneum due to spontaneous splenic rupture: a rare complication of primary cytomegalovirus infection. Gastroenterol Clin Biol 1998;22:107–108.
- Khan AZ, Escofet X, Roberts KM, et al. Spontaneous splenic rupture—a rare complication of amyloidosis. Swiss Surg 2003;9:92–94.
- Giagounidis AA, Burk M, Meckenstock G, Koch AJ, Schneider W. Pathologic rupture of the spleen in hematologic malignancies: two additional cases. Ann Hematol 1996;73:297–302.
- Hertzberg BS, Kliewer MA, Paulson EK. Ovarian cyst rupture causing hemoperitoneum: imaging features and potential for misdiagnosis. Abdom Imaging 1999;24:304–308.
- Dibbs KI, Ball RH, Huetner PC. Spontaneous uterine rupture and hemoperitoneum in the first trimester. Am J Perinatol 1995;12:439–441.
- Yoffe N, Bronshtein M, Brandes J, et al. Hemorrhagic ovarian cyst detection by transvaginal sonography: the great imitator. Gynecol Endocrinol 1991;5:123–129.
- Hallatt JG, Steele CH, Snyder M. Ruptured corpus luteum with hemoperitoneum: a study of 173 surgical cases. Am J Obstet Gynecol 1984;149: 5–9.
- Della-Giustina D, Denny M. Ectopic pregnancy. Emerg Med Clin North Am 2003;21:565–584.
- Lozeau AM, Potter B. Diagnosis and management of ectopic pregnancy. Am Fam Physician 2005;72: 1707–1714.
- Hertzberg BS, Kliewer MA, Bowie JD. Adnexal ring sign and hemoperitoneum caused by hemorrhagic ovarian cyst: pitfall in the sonographic diagnosis of ectopic pregnancy. AJR Am J Roentgenol 1999;173:1301–1302.
- Mortele KJ, Cantisani V, Brown DL, Ros PR. Spontaneous intraperitoneal hemorrhage: imaging features. Radiol Clin North Am 2003;41:1183– 1201.
- Weinstein L. Syndrome of hemolysis, elevated liver enzymes, low platelet count: a severe consequence of hypertension in pregnancy. Am J Obstet Gynecol 1982;142:159–165.
- Byrd DE, Riely CA. Liver disease in preeclampsia. Gastroenterologist 1996;4:65–69.
- Nunes JO, Turner MA, Fulcher AS. Abdominal imaging feature of HELLP syndrome: a 10-year retrospective review. AJR Am J Roentgenol 2005; 185:1205–1210.
- Golledge J, Abrokwah J, Shenoy KN, Armour RH. Morphology of ruptured abdominal aortic aneurysms. Eur J Vasc Endovasc Surg 1999;18:96–104.
- Borioni R, Garofalo M, Innocenti P, et al. Hemoperitoneum due to spontaneous rupture of an aneurysm of the left gastroepiploic artery. J Cardiovasc Surg (Torino) 1999;40:63–64.
- Stanley JC, Thompson NW, Fry WJ. Splanchnic artery aneurysms. In: Rutherford RB, ed. Vascular surgery. 4th ed. Philadelphia, Pa: Saunders, 1995; 1124–1139.
- Shanley CJ, Shah NL, Messina LM. Common splanchnic artery aneurysms: splenic, hepatic and celiac. Ann Vasc Surg 1996;10:315–322.
- Berceli SA. Hepatic and splenic artery aneurysms. Semin Vasc Surg 2005;18:196–201.
- Gadacz TR, Trunkey D, Kieffer RF Jr. Visceral vessel erosion associated with pancreatitis. Arch Surg 1978;113:1438–1440.