Hip dislocation
Hip dislocation occurs when the head of the thighbone (femur) slips out of its socket (acetabulum) in the hip bone (pelvis). A traumatic hip dislocation typically takes a major force to dislocate the hip. Car collisions and falls from significant heights are common causes and, as a result, other injuries like broken bones often occur with hip dislocation. A traumatic hip dislocation is a serious medical emergency. Immediate treatment is necessary.
Some children are born with dislocated hips in a disorder called Developmental Dysplasia of the Hip or congenital hip dislocation.
When there is a hip dislocation, the femoral head is pushed either backward out of the socket, or forward.
- Posterior hip dislocation. In approximately 90% of hip dislocation patients, the thighbone is pushed out of the socket in a backwards direction. This is called a posterior dislocation. A posterior dislocation leaves the lower leg in a fixed position, with the knee and foot rotated in toward the middle of the body.
- Anterior hip dislocation. When the thighbone slips out of its socket in a forward direction, the hip will be bent only slightly, and the leg will rotate out and away from the middle of the body.
When the hip dislocates, the ligaments, labrum, muscles, and other soft tissues holding the bones in place are often damaged, as well. The nerves around the hip may also be injured.
A traumatic hip dislocation is a medical emergency. Call for help immediately. Do not try to move the injured person, but keep him or her warm with blankets.
In cases in which hip dislocation is the only injury, an orthopaedic surgeon can often diagnose it simply by looking at the position of the leg. Because hip dislocations often occur with additional injuries, your doctor will complete a thorough physical evaluation.
Your doctor may order imaging tests, such as x-rays, to show the exact position of the dislocated bones, as well as any additional fractures in the hip or thighbone.
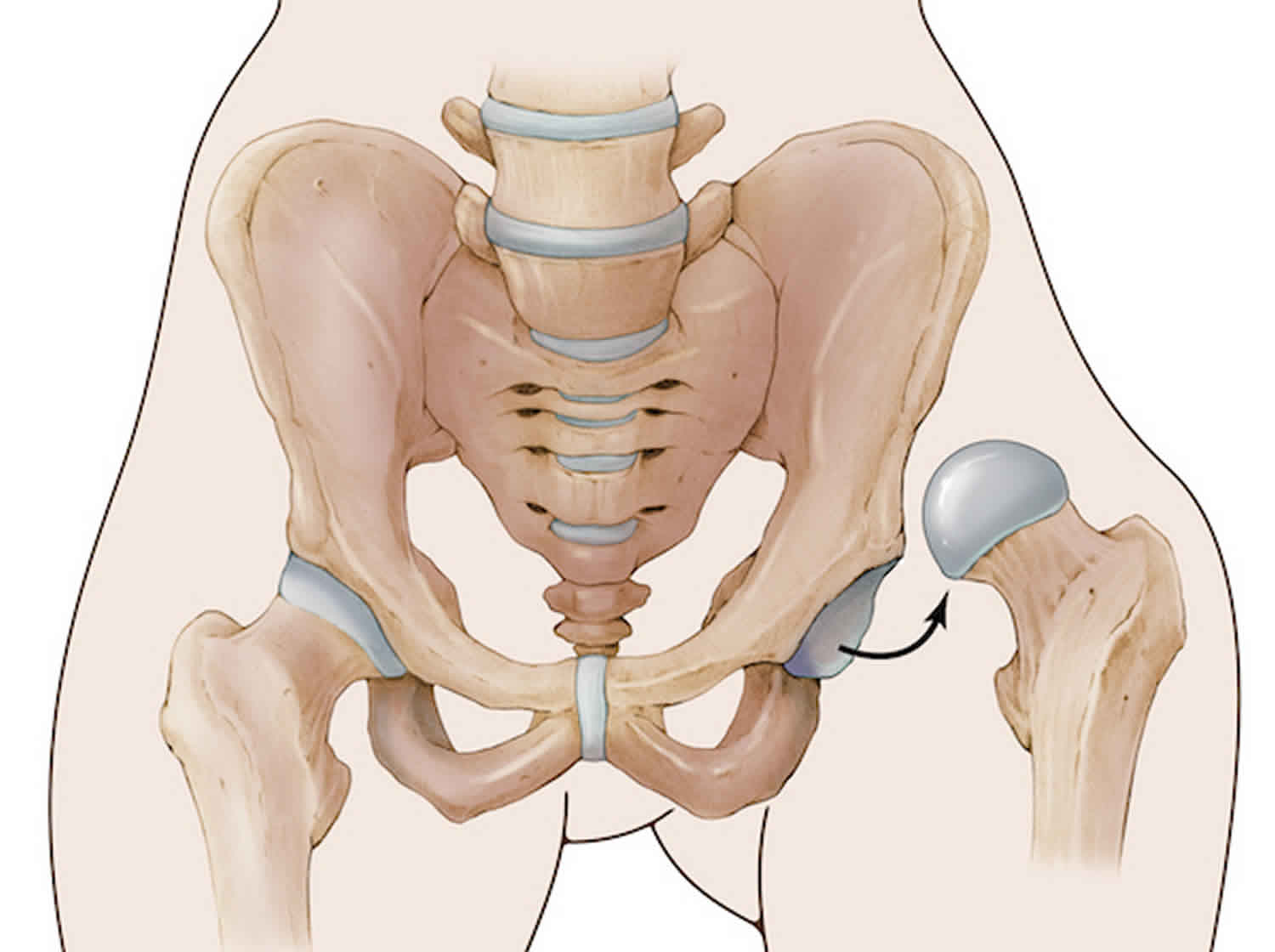
Hip anatomy
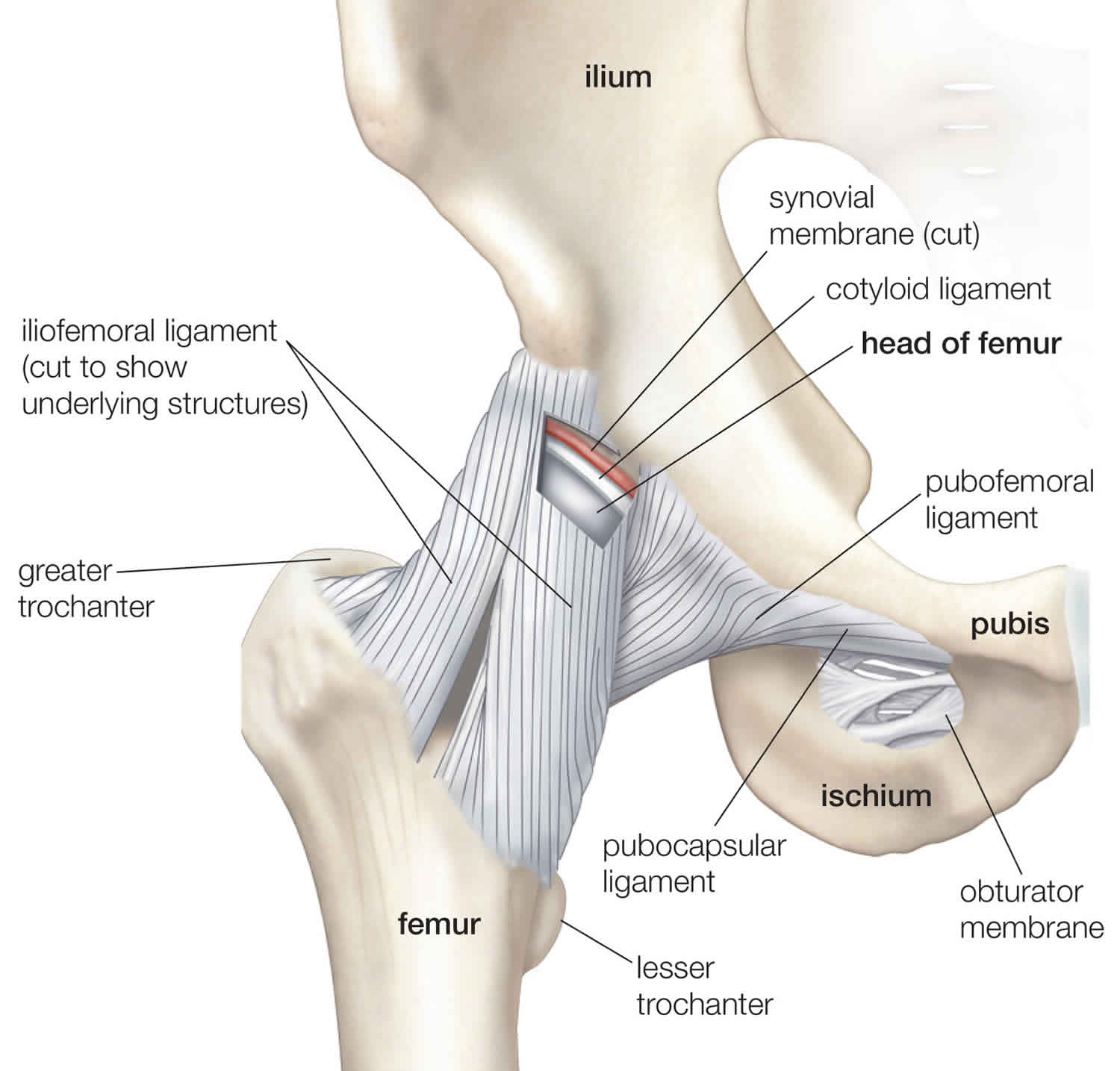
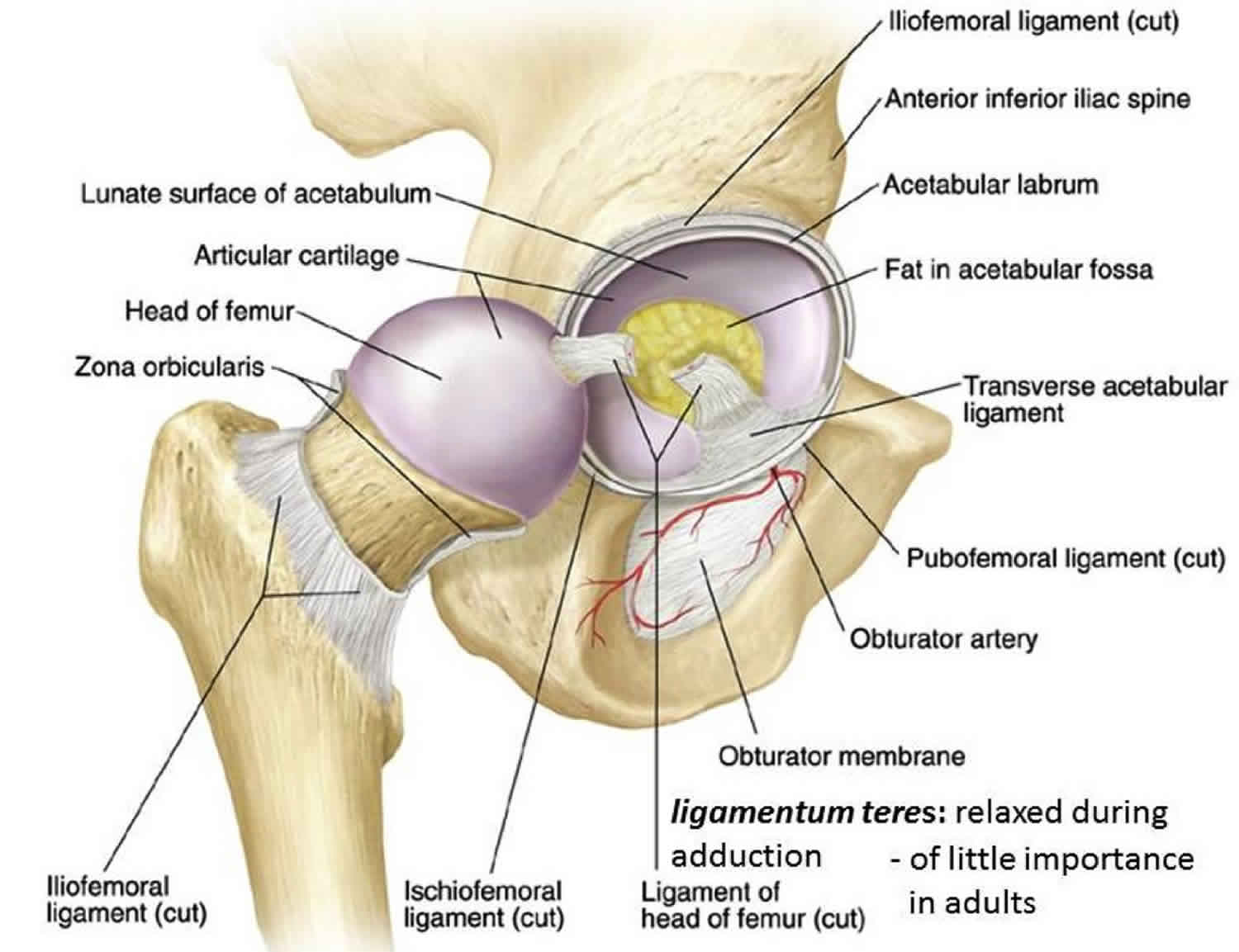
The hip is a ball-and-socket joint. The socket is formed by the acetabulum, which is part of the large pelvis bone. The ball is the femoral head, which is the upper end of the femur (thighbone).
A smooth tissue called articular cartilage covers the surface of the ball and the socket. It creates a low friction surface that helps the bones glide easily across each other.
The acetabulum is ringed by strong fibrocartilage called the labrum. The labrum forms a gasket around the socket, creating a tight seal and helping to provide stability to the joint.
Figure 1. Hip joint anatomy (in a healthy hip, the head of the femur stays firmly within the acetabulum)
Hip dislocation causes
High speed impacts where a large force is transmitted through the hip joint is the most common cause of hip dislocations that do not involve a joint replacement. Examples of this type of injury include:
- Motor vehicle accidents: Motor vehicle collisions are the most common cause of traumatic hip dislocations. As many as 70% of hip dislocations have been reported to have been caused by car accidents. The hip is most vulnerable to dislocation when it is bent (flexed) as in the sitting position. During a car accident, the knee may strike the dashboard leading to a force being transmitted through to the hip joint. This force drives the thigh backwards, which drives the ball head of the femur out of the hip socket. This usually leads to a posterior (to the back) dislocation. Wearing a seatbelt can greatly reduce your risk of hip dislocation during a collision.
- High impact sport: Sports such as rugby, AFL, and American football may be a cause of hip dislocation. Most commonly, an athlete is running and jumping, striking the ground while the hip is flexed (bent), adducted (tilted in), and internally rotated (twisted inwards). This is uncommon and is a rare sporting injury.
- Alpine skiing: Posterior dislocations may occur when the knee strikes a solid object after the skier has fallen whilst travelling at high speeds. This is a similar type of injury to that caused by a car accident.
- Falls: A fall from a significant height (such as from a ladder) or an industrial accident can lead to hip dislocation. This may be as a result of an occupational accident.
Another cause of hip dislocation is an unstable hip joint. This is usually due to a past total hip replacement. In this situation, a significant force is not required in order to create a hip dislocation. Incidental movements, usually with the hip in a bent position, can lead to a hip dislocation.
With hip dislocations, there are often other related injuries, such as fractures in the pelvis and legs, and back, abdominal, knee, and head injuries. Perhaps the most common fracture occurs when the head of the femur hits and breaks off the back part of the hip socket during the injury. This is called a posterior wall acetabular fracture-dislocation.
Risk factors for hip dislocation
The following risk factors make hip dislocation more likely:
- Previous hip dislocation
- High impact sports
- Total hip replacement
- Arthritis of the hip – especially rheumatoid and gout
- Poor muscle conditioning
Hip dislocation prevention
Hip dislocations are usually caused by high impact injuries in a normal hip. In order to prevent hip dislocations, avoiding activities that may lead to such an injury is the best method of preventing a hip dislocation.
Hip dislocations also commonly occur in people who have had a hip replacement. In this case, a high impact injury is not necessary in order to dislocate the hip. In the early stages following a hip replacement, to avoid dislocation, you should avoid:
- crossing your legs whilst seated
- bending at the hips past 90 degrees
- turning your affected foot inward or internally rotating your hip
Once rehabilitation of the hip replacement is complete, extreme hip movements should be avoided in order to minimize hip dislocation.
Congenital hip dislocation
Developmental dysplasia of the hip or congenital hip dislocation is an abnormal development of the hip joint leading to a joint that is dislocated or prone to dislocation. Congenital hip dislocation is found in babies or young children and affects 1-3% of newborns.
Congenital hip dislocation is where the two bones that make up the joint are not lined up properly. The hip joint is made up of a ball at the top of the thighbone (called the femoral head) which sits inside the socket (called the acetabulum) of the pelvis. In developmental dysplasia of the hip the femoral head slips and does not properly join the hip socket or acetabulum.
In hips affected by developmental dysplasia of the hip, the ball is not stable within the socket because the socket is abnormally shallow. The ligaments around the hip joint that normally help hold the hip joint in place, are also abnormal, allowing the ball to slip out of the socket.
Developmental dysplasia of the hip can vary from mild forms where there is slightly less stability in the joint to severe where the joint easily dislocates. It may be present on one side only or it may affect both hips.
Congenital hip dislocation causes
The precise cause of congenital hip dislocation (developmental dysplasia of the hip) is unknown, but genetic and environmental factors may both play a role.
There is an increased risk of developing developmental dysplasia of the hip if someone in the family has previously had this condition. This suggests that developmental dysplasia of the hip may be caused partly by genetic factors. Currently there is not a clear understanding of how this occurs.
As well as genetic factors that may play a role, there are ‘environmental’ factors that may affect the hip such as the position of the hip within the womb or in the first few months of life. How the baby is born may also impact on the hip, particularly if the baby is delivered in the breech position (feet first). It is thought that pressure on the infants hips either in the womb or whilst being born, may stretch the ligaments of the hips and lead to the joint becoming unstable. Once the baby is born, certain swaddling techniques may place the hip in a position that stretches the ligaments and leads to instability.
Risk factors for congenital hip dislocation
The risk factors for congenital hip dislocation (developmental dysplasia of the hip) are as follows:
- Family history: If other family members have been diagnosed with developmental dysplasia of the hip then this is risk factor for developing the condition
- Breech position at birth: This means the baby is born feet first. If the baby is in the breech position and a Caesarian section is performed, there is still a slightly increased risk of developmental dysplasia of the hip but not as high as if the birth is a vaginal delivery.
- High birth weight (>5kg): A large baby will have less room to move in the womb. It is thought that due to the size of the baby there is more pressure on the hips which stretches the ligaments and makes them more susceptible to developmental dysplasia of the hip
- Prematurity: If a baby is born before 38 weeks of the pregnancy, this holds a slightly increased risk of developmental dysplasia of the hip
- Low amount of fluid in the womb: The medical term for this condition is oligohydramnios. This may cause developmental dysplasia of the hip in the same way that a high birth weight affects the hips (see above).
- Positioning or swaddling: Overly tight swaddling may lead to pressure on the hips and lead to instability
- Female gender: girls suffer developmental dysplasia of the hip more commonly than boys
It is important to note that infants and children with developmental dysplasia of the hip may have none of these risk factors and all babies should be screened for this condition at birth. Of note is the fact that the left hip is more commonly affected than the right.
Congenital hip dislocation symptoms
Because congenital hip dislocation affects newborns and young infants, the diagnosis of developmental dysplasia of the hip (congenital hip dislocation) is highly dependent on screening tests and clinical observations. However the following signs and symptoms may indicate that developmental dysplasia of the hip may be present:
Newborn
- Asymmetry of the legs: this may be noticed by an asymmetry of thigh or buttock creases, a shortened leg on the affected side
- Clicking: this is an unreliable indicator of developmental dysplasia of the hip. Many normal hips will click when moved but this can occur in developmental dysplasia of the hip as well.
3 Months – 1 year
- Restricted leg movements: Moving the leg to the side is the movement that is usually limited in developmental dysplasia of the hip. This may cause difficulty when putting on nappies or difficulty in sitting astride an adults knee.
- Difficulty in crawling: rather than crawling evenly, one leg may be dragging to the side when crawling
Early childhood
- Limping: usually a limp caused by developmental dysplasia of the hip will not be painful.
- The child may walk on their toes on the affected side
- Despite these problems, walking is not usually delayed
Late childhood and adulthood
If developmental dysplasia of the hip is not picked up in early stages of life, the hip will become worn out and cause symptoms similar to osteoarthritis of the hip. These can include:
- Walking with a limp which may become painful
- Restriction of leg movements to the side (abduction of the hip)
- Pain in the groin or buttock area on hip movements
Congenital hip dislocation complications
Early diagnosis and treatment for developmental dysplasia of the hip is essential to avoid progression of hip problems relating to this condition. If the hip is unstable or dislocated due to developmental dysplasia of the hip, the muscles of the hip will shorten as the infant grows leading to the hip being stuck in the dislocated position. This will lead to the socket of the hip joint not forming properly. If the socket is more shallow than it should be then the ball (femoral head) may change shape, becoming more flattened. This process is termed ‘dysplasia’ of the hip and means abnormal development. If dysplasia of the hip is left untreated, the following complications can occur:
- a persistent limp on the affected side
- premature osteoarthritis of the hip which may eventually require a total hip replacement
- lower back or hip pain
If developmental dysplasia of the hip is treated early, the problem usually resolves with no further complications. If however, the condition is treated late, when some degree of dysplasia or abnormal development has occurred, then there are complications associated with this treatment. These include:
- Recurrent dislocations: If a hip is dislocated due to developmental dysplasia of the hip and is put back into place late in early childhood then it may be prone to future dislocations due to a shallow hip socket.
- Avascular necrosis: This means that the blood supply to the hip joint is disrupted and the bone dies. This can occur when the hip is put back in place after it has been sitting out of the socket for a prolonged period of time. To learn more about this condition follow the link to osteonecrosis of the hip.
Congenital hip dislocation diagnosis
When a dislocated hip joint is put back in place, the developmental dysplasia of the hip often normalizes within the first months of life. If the hip remains dislocated, muscles will shorten, locking the hip in the wrong place and surgery is likely to be required. For this reason early diagnosis is very important
Newborn investigations
All babies should be examined for congenital hip dislocation within 24 hours of birth before leaving the hospital; at 6 weeks; between 6-9 months; and at walking age.
These examinations are called screening tests as all infants receive them. If the initial examination reveals a suspicion of an unstable or loose hip, further examination may be required.
Clinical examination
All infants are assessed in the hospital by a doctor when they are born in order to test the stability of their hip joints. The doctor will perform two maneuvers that test whether the hip is sitting in the socket or if the hip moves more than it should. These maneuvers are called Ortolani and Barlow tests named after the doctors that developed them. If these test indicate that the hip is dislocated or unstable, further investigation is required.
Observation of additional signs, such as a discrepancy in leg length or asymmetrical thigh and buttock skin folds, may also be present and re-enforce the need for further investigations
Further investigation – ultrasound
Ultrasound scans of the hip are the best investigation from birth until the age of 4-5 months, while the hips are mainly cartilage instead of bone. The ultrasound will be able to show the shape of the hip socket and also whether the ball of the hip is sitting in the socket.
Infant and child investigations
Clinical examination
Ortolani and Barlow tests may still be used in infants under 1 year of age but increasingly these tests become less valuable as the child ages. The most reliable indicator of developmental dysplasia of the hip in a young child is the inability to move the hip away from the midline (to abduct the hip). If the child is crawling with one leg swinging to the side, walking with a limp or has an observable leg length discrepancy, then this may also indicate developmental dysplasia of the hip. If following a clinical examination, the doctor suspects that developmental dysplasia of the hip may be present, then further investigations are required to confirm this.
Further investigations – X-ray
Ultrasound imaging is only effective in diagnosing developmental dysplasia of the hip in infants under 4 months of age. As the infant ages, the hip joint progresses from being largely made of cartilage to being made of bone. X-rays are the most effective tool of imaging a hip joint that has made the progression to bone. In children over 4 months of age, an X-ray is used to diagnose developmental dysplasia of the hip.
Congenital hip dislocation treatment
Early treatment – birth to 6 months
The primary aim of treatment is to achieve a stable hip that does not dislocate and moves freely. If diagnosed and treated early, the outcomes for developmental dysplasia of the hip are very good.
The early treatment consists of the use of a soft brace that is called the Pavlik Harness. This brace is a device that allows the baby to move their legs in all directions that do not cause dislocation of the hips. It restricts movements that the baby may perform which can lead to dislocation.
The harness may need to be worn for several months and it is important that the full course recommended by your doctor is completed. Whilst the child is wearing the harness they will have regular check ups to readjust the fitting of the harness and also to assess how the hips are responding. Over a period of weeks to months the ligaments and muscles around the hips will tighten and strengthen leading to a stable hip joint.
Following completion of this period, most children require no further treatment.
Later treatment – after 6 months of age
If congenital hip dislocation is not diagnosed early, more invasive treatment may be required. If a splint has been tried but the hips remain unstable or if the diagnosis is made after 6 months of age, relocation of the hip under anesthesia or surgery is often required.
The first step is to relocate the hip whilst the child is either sedated or under anesthetic. If this is unsuccesful, an operation may be required. The operation involves surgically putting the hip back into the socket and often also involves releasing tight muscles that are holding the hip out of place.
For children aged 18-24 months, the operation may include reshaping either the pelvic bone or the thigh bone to create a stable hip joint. This type of operation is called a femoral or pelvic osteotomy. Generally, the older the child at the time of diagnosis, the more invasive the surgery becomes in order to correct the problem. This is why early diagnosis is so important in developmental dysplasia of the hip. These operations are followed by a period where a more rigid cast must be worn to ensure the hips stay in the right place.
Adult treatment
If developmental dysplasia of the hip is left untreated in childhood, the hip will become abnormally developed (dysplastic). This can lead to premature osteoarthritis. Treatment in this situation is often to perform a total hip replacement.
Dislocated hip symptoms
A traumatic hip dislocation is very painful. A pop or tearing sensation may be felt at the time of injury. Patients are unable to move the leg and, if there is nerve damage, may not have any feeling in the foot or ankle area.
- Pain: Dislocation of the hip is very painful. This pain is felt in the hip region, upper thigh and groin. Pain may also be felt in the knee, lower leg or lower back due to the dislocation.
- Loss of hip movement: Once dislocated, hip motion will be very difficult. Usually people with a dislocated hip are unable to walk or move their leg at all.
- Numbness: There may be numbness and tingling in the leg due to damage to blood vessels and nerves that run past the hip joint.
- Deformity: The leg of the dislocated hip may appear shorter or longer than the unaffected side depending on which direction the head of the femur has moved during the dislocation. It may also be turned inwards if it is a posterior (to the back) dislocation or turned outward if it is an anterior (to the front) dislocation.
- Swelling and bruising: The hip may swell up quite quickly following the injury, bruising may take several hours to appear.
Hip dislocation complications
The hip is normally a very stable joint due to the shape of the joint and the strong ligaments and muscles that surround it. Due to this, a dislocation of the hip may cause damage to these surrounding structures. Complications to the surrounding area include:
- Blood vessel damage: The blood supply to the bones that make up the hip joint, particularly the head of the femur may be affected by a dislocation. This can lead to bone death which is a condition that is known as avascular necrosis or osteonecrosis. Osteonecrosis is a serious condition and is a painful condition that can ultimately lead to the destruction of the hip joint and arthritis. Osteonecrosis may require surgery to maintain the hip joint.
- Nerve damage: Two large nerves – the femoral and sciatic nerve run either side (front and back) of the hip joint. Depending on the direction of the dislocation, these nerves may be damaged. Usually this is only temporary damage leading to pain, numbness or tingling. Permanent injury is uncommon but may occur. The sciatic nerve, which extends from the lower back down the back of the legs, is the nerve most commonly affected. Injury to the sciatic nerve may cause weakness in the lower leg and affect the ability to move the knee, ankle and foot normally. Sciatic nerve injury occurs in approximately 10% of hip dislocation patients. The majority of these patients will experience some nerve recovery.
- Fracture: Along with dislocation, there may be a fracture of either the femur (thigh bone) or acetabulum (hip socket).
- Cartilage damage: The hip socket is lined by a ring of cartilage known as the acetabulum. This increases the depth of the socket and contributes to the stability of the hip. This cartilage may be torn during a dislocation.
When the hip joint has been dislocated, there are future complications that may occur months or years following the initial event. These include:
- Recurrent dislocations: Due to damage to the surrounding tissues of the hip, a dislocation makes the hip less stable and increases the risk of further dislocations.
- Osteoarthritis: During a dislocation, the surrounding cartilage may be damaged. This combined with the chance of the hip not tracking as well as it should following a dislocation, increase the risk of developing osteoarthritis. Osteoarthritis can eventually lead to the need for other procedures, like a total hip replacement.
Hip dislocation diagnosis
Diagnosis of a hip dislocation needs to be made promptly in order to minimize the risk of complications and long term damage. The injured person should not try to use the affected leg. On arrival to a hospital, the doctors will:
- Take a history of the injury, finding out exactly how the injury occurred and whether there are any other relevant conditions that might affect the management of the dislocated hip
- Perform an examination of the affected area by feeling the hip joint and assessing the available movement. They will also check the nerves and blood vessels associated with the hip
- Order an X-ray of the hip which can confirm the diagnosis of hip dislocation
Hip dislocation treatment
Initial treatment
Hip dislocations are a serious injury and before the hip is treated, a person’s general health needs to be assessed and stabilized. Once this has been carried out by the doctors, they will attempt to put the hip back into place which is known as ‘reduction of the dislocation’.
- Because the hip is surrounded by very strong muscles, it is difficult to put the hip back into place and requires sedation in the form of an anesthetic as well as medication to relax the muscles and reduce the pain. Once the person with the dislocation is relatively comfortable and sedated, the hip will be manipulated using traction back into place.
- If the dislocation is too difficult to put back into place, or complicated by a fracture, then an operation may be required to effectively return the hip to a normal position.
- Once the hip is back in place, rehabilitation may be required to ensure the muscles around the hip remain strong.
Reduction procedures
If there are no other injuries, the doctor will administer an anesthetic or a sedative and manipulate the bones back into their proper position. This is called a reduction.
In some cases, the reduction must be done in the operating room with anesthesia. In rare cases, torn soft tissues or small bony fragments block the bone from going back into the socket. When this occurs, surgery is required to remove the loose tissues and correctly position the bones.
Following reduction, the surgeon will request another set of x-rays and possibly a computed tomography (CT) scan to make sure that the bones are in the proper position.
Hip dislocation rehabilitation
Proper rehabilitation must be performed to return to a normal level of activity. Rehabilitation takes the following path:
- Weight bearing with the help of crutches should begin immediately after the patient is able to stand
- Full weight bearing can begin as the pain further reduces
- Range of motion and strengthening exercises should be carried out under the guidance of a physiotherapist for the six weeks following the injury
- Gradual return to normal activities and sports can occur as pain resolves and movement returns during the following months
Dislocated hip recovery
A hip dislocation is a major injury. It takes time—sometimes 2 to 3 months—for the hip to heal after a dislocation. The rehabilitation time may be longer if there are additional fractures. The doctor may recommend limiting hip motion for several weeks to protect the hip from dislocating again. Physical therapy is often recommended during recovery.
Patients often begin walking with crutches within a short time. Walking aids, such as walkers, crutches and, eventually, canes, help patients get mobilized.