What is a Holter monitor
A Holter monitor is also called a continuous electrocardiogram (ECG), continuous ECG or ambulatory electrocardiography (ambulatory ECG) that can record your heart rate and rhythm when you feel chest pain or symptoms of an irregular heartbeat (called arrhythmia). A Holter monitor is a small, portable electrocardiogram (ECG) device that monitors your heart’s electrical activity for 24 hours or longer. The Holter heart monitor is worn for 24 to 48 hours during your normal activity. Holter monitoring gives your doctor a constant reading of your heart rate and rhythm over a 24-hour period (or longer). Your doctor can then look at the time when you noticed your symptoms. Reviewing the Holter monitor record will give your doctor an idea about the nature of your heart problem.
How does Holter monitor work?
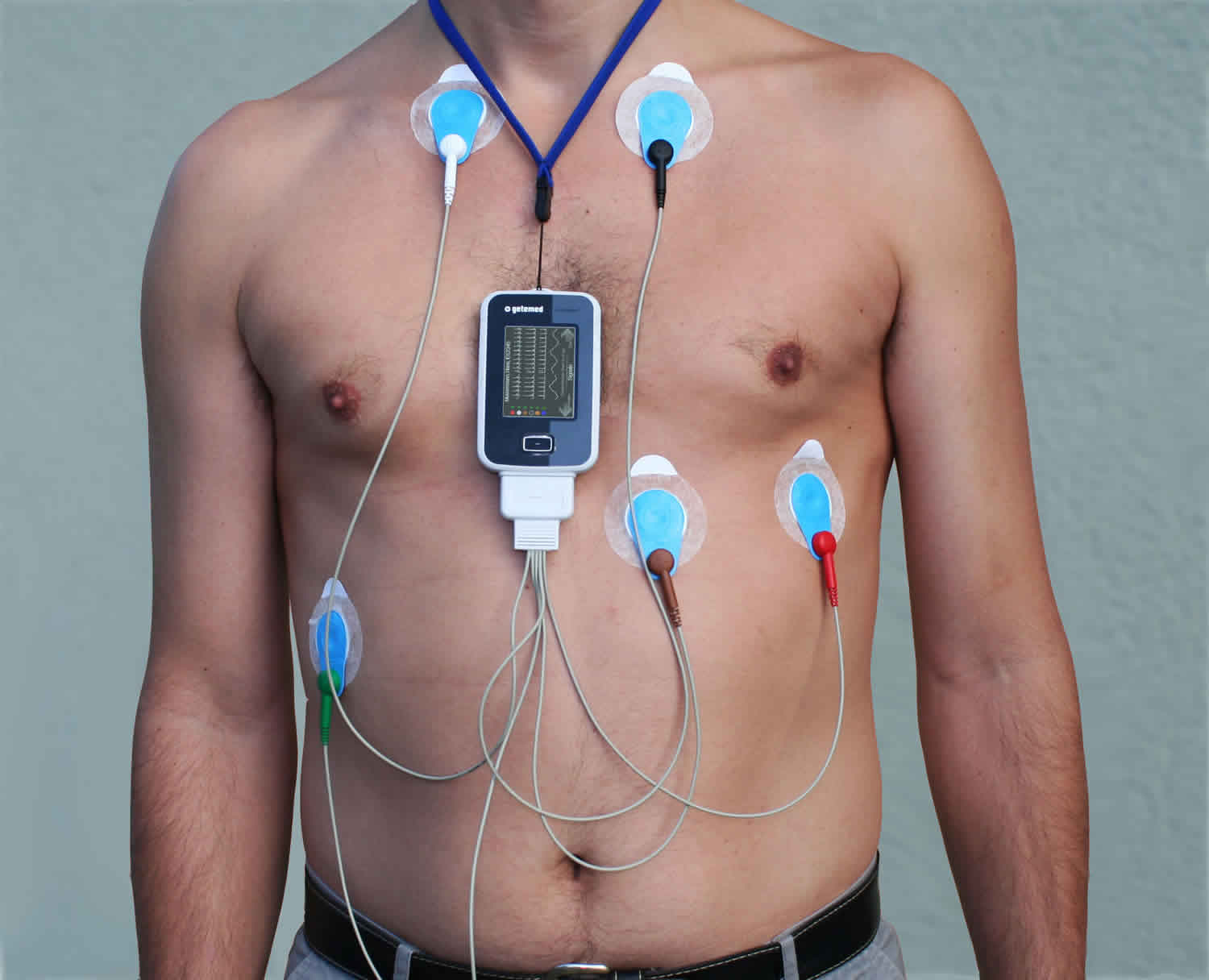
The Holter monitor ambulatory electrocardiography (ambulatory ECG), an ECG recording device. The Holter monitor runs on batteries and can be placed in a pocket or pouch worn around your neck or waist. Holter monitor has 5 to 7 wires called leads. The leads attach to metal disks called electrodes (small conducting patches), which are stuck onto your chest. The electrodes must be firmly attached to your chest so the Holter monitor gets an accurate recording of your heart’s activity. Tell your doctor if you are allergic to any tape or other adhesives. These electrodes are very sensitive, and they can pick up the electrical impulses of the heart. The impulses are recorded by the Holter monitor and give your doctor a 24-hour record of your heart’s electrical activity.
Holter monitoring is a painless test. You will need to go into your doctor’s office to be fitted for the Holter monitor. It is a good idea that you shower or bathe before you go to the doctor’s office, because once you are wearing the Holter monitor, you cannot get it wet in the shower or bathtub.
You must keep the Holter monitor close to your body. This may make it hard for you to sleep.
Occasionally there may be an uncomfortable skin reaction to the sticky electrodes. You should call your doctor’s office where it was placed to tell them about it.
While you wear the Holter monitor, it records your heart’s electrical activity.
- Keep a diary of what activities you do while wearing the Holter monitor, and how you feel.
- After 24 to 48 hours, you will return the Holter monitor to your health care provider’s office. At your doctor’s office you’ll have the electrodes removed. This may cause some discomfort, similar to having a bandage pulled off.
- Your doctor will look at the Holter monitor records and see if there have been any abnormal heart rhythms.
It is very important that you accurately record your symptoms and activities so the provider can match them with your Holter monitor findings.
While wearing the Holter monitor, AVOID:
- Electric blankets
- High-voltage areas
- Magnets
- Metal detectors
- Water
Continue your normal activities while wearing the Holter monitor. You may be asked to exercise while being monitored if your symptoms have occurred in the past while you were exercising.
Why is the Holter monitor test is done?
Your doctor may also order a Holter monitor if you have a heart condition that increases your risk of an abnormal heart rhythm, most commonly to evaluate medication changes, heart palpitations or irregular heart rhythms, and symptoms such as fainting, dizziness, or shortness of breath which may be experienced on a daily basis. Your doctor may suggest you wear a Holter monitor for a day or two, even if you haven’t had any symptoms of an abnormal heartbeat.
If you have signs or symptoms of a heart problem, such as an irregular heartbeat (arrhythmia) or unexplained fainting, your doctor may order a test called an electrocardiogram (ECG) first. An electrocardiogram is a brief, noninvasive test that uses electrodes taped to your chest to check your heart’s rhythm. However, sometimes an electrocardiogram (ECG) doesn’t detect any irregularities in your heart rhythm because you’re hooked up to the machine for only a short time. If your signs and symptoms suggest that an occasionally irregular heart rhythm may be causing your condition, your doctor may recommend that you wear a Holter monitor for a day or so.
Over that time, the Holter monitor may be able to detect irregularities in your heart rhythm that an electrocardiogram couldn’t detect.
Holter monitoring is used to determine how your heart responds to normal activity. The Holter monitor may also be used:
- After a heart attack
- To diagnose heart rhythm problems that may be causing symptoms such as palpitations or syncope (passing out/fainting)
- When starting a new heart medicine
Heart rhythms which may be recorded include:
- Atrial fibrillation or atrial flutter
- Multifocal atrial tachycardia
- Paroxysmal supraventricular tachycardia
- Slow heart rate (bradycardia)
- Ventricular tachycardia (≥3 beats)—sustained (≥30 s) or non-sustained (<30 s)
- Sinus tachycardia
- Pauses
- Junction rhythms or ectopy
- Atrioventricular block (second-degree heart block type 1 (Mobitz 1), second-degree heart block type 2 (Mobitz 2), 2:1, high-grade)
- Complete heart block (third-degree heart block)
- Atrial ectopy
- Supraventricular ectopy or tachycardia
- Wide complex tachycardia
- Ventricular ectopy (single, couplet, triplet, bigeminy, trigeminy)
Holter monitor lead placement
A nurse will clean the areas with alcohol and then place the electrodes on your chest. For men, the nurse may have to shave some small areas of your chest. The electrodes stick to the skin with a gel. Sometimes, an electrode and lead wire will be taped to your chest to prevent them from moving around.
The most important element in Holter monitoring is recording a clean long-term ECG signal. Because a clean signal is directly dependent on the hookup procedure, great care should be taken when attaching the electrodes on the patient. Poor attachment causes poor signal quality and artifact. To ensure proper hookup, follow these steps:
- Using either the 5-Lead (3-channel) or 7-Lead (3-channel) hook-ups shown below, identify sites for the electrodes.
- Prepare the patient’s skin. If the patient has hair in any of the electrode areas, shave it with a safety razor. Use an alcohol pad and rub the sites briskly until the skin reddens. Let the skin air dry before proceeding.
- Attach the patient cable to the recorder. Next, snap a lead wire from the patient cable to each of the electrodes.
- Attach an electrode at each of the patient’s prepared sites. As you attach electrodes, be careful to not let any unattached electrode come in contact with other conductive objects, including ground. Be sure to refer to the diagrams below for correct placement of each colored lead. The electrodes should be placed over bone at each of the sites. Press the center of each electrode against the patient’s skin, then rub the outer circle of each electrode to secure it.
- If you use lead lock or clip lock electrodes, be sure to use the lock or clip to relieve stress on each lead wire. Otherwise, tape each lead wire into a stress loop to help prevent movement of the electrode (Figure 3).
Figure 1. Holter monitor lead placement (5-Lead placement)
Figure 2. Holter monitor lead placement (7-Lead placement)
Abnormal holter monitor results
The Holter monitor can record heart rate and rhythm when you feel chest pain or symptoms of an irregular heartbeat (called arrhythmia). The Holter monitor records every heartbeat over the 24 – 48 hour period that the monitor is worn (approximately 100,000 – 120,000 heart beats). Abnormal results may include various arrhythmias such as those listed below. Some changes may mean that the heart is not getting enough oxygen.
Heart rhythms which may be recorded include:
- Atrial fibrillation or atrial flutter
- Multifocal atrial tachycardia
- Paroxysmal supraventricular tachycardia
- Slow heart rate (bradycardia)
- Ventricular tachycardia (≥3 beats)—sustained (≥30 s) or non-sustained (<30 s)
- Sinus tachycardia
- Pauses
- Junction rhythms or ectopy
- Atrioventricular block (second-degree heart block type 1 (Mobitz 1), second-degree heart block type 2 (Mobitz 2), 2:1, high-grade)
- Complete heart block (third-degree heart block)
- Atrial ectopy
- Supraventricular ectopy or tachycardia
- Wide complex tachycardia
- Ventricular ectopy (single, couplet, triplet, bigeminy, trigeminy)
Figure 4. Atrial fibrillation
Figure 5. Atrial flutter
Figure 6. Multifocal atrial tachycardia
Figure 7. Supraventricular tachycardia
Figure 8. Sinus tachycardia
Figure 9. Junction rhythm
Figure 10. Second-degree heart block type 1 (Mobitz 1)
Figure 11. Second-degree heart block type 2
Figure 12. Third-degree heart block
Figure 13. Ventricular bigeminy
Figure 14. Ventricular trigeminy
After your doctor has looked at the results of your Holter monitor recorder and what you’ve written in your activity diary, he or she will talk to you about your results. The information from the Holter monitor may reveal that you have a heart condition, or your doctor may need more tests to find out what may be causing your symptoms.
In some cases, your doctor may not be able to diagnose your condition based on the results of the Holter monitor test, especially if you didn’t have any irregular heart rhythms while you wore the Holter monitor.
Your doctor may then recommend a wireless Holter monitor or an event recorder, both of which can be worn longer than a standard Holter monitor. Event recorders are similar to Holter monitors and generally require you to push a button when you feel symptoms. There are several different types of event recorders.