What is HPV
HPV is short for human papillomavirus 1. HPVs are a group of more than 200 related viruses. Each HPV virus is given a number, which is called an HPV type. HPVs are called papillomaviruses because some HPV types cause papillomas (warts), which are non-cancerous tumors. About 40 of those HPV types affect the genitals. They are spread through sexual contact with an infected partner. Some of those can put you at risk or known to cause cancer, including cancers of the cervix (the base of the womb at the top of the vagina), vagina, vulva (the area around the outside of the vagina), penis, anus, and parts of the mouth and throat.
HPV infections are the most common sexually transmitted infections in the United States. About 14 million new genital HPV infections occur each year 2. In fact, the Centers for Disease Control and Prevention (CDC) estimates that more than 90% and 80%, respectively, of sexually active men and women will be infected with at least one type of HPV at some point in their lives 3. Around one-half of these infections are with a high-risk HPV type 4.
Most high-risk HPV infections occur without any symptoms, go away within 1 to 2 years, and do not cause cancer. Some HPV infections, however, can persist for many years. Persistent infections with high-risk HPV types can lead to cell changes that, if untreated, may progress to cancer.
HPVs are attracted to and can live only in certain cells called squamous epithelial cells. These cells are found on the surface of the skin and on moist surfaces (called mucosal surfaces) like:
- The vagina, cervix, vulva (area around the outside of the vagina), and anus
- The inner foreskin and urethra of the penis
- The inner lining of the nose, mouth, and throat
- The trachea (windpipe) and bronchi (smaller breathing tubes branching off the trachea)
- The inner eyelids
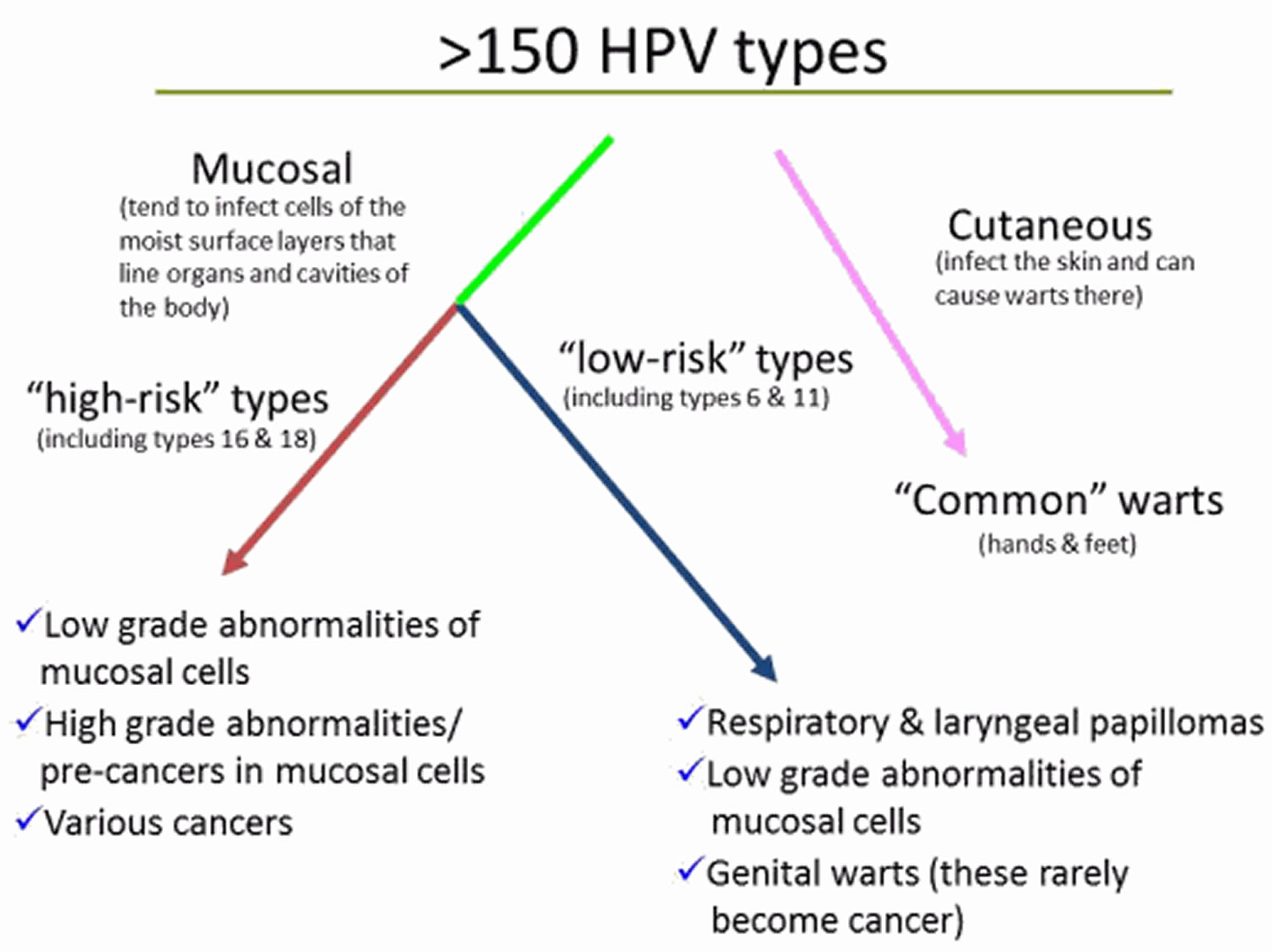
Cutaneous (skin) HPV types
Most HPV types are called cutaneous because they cause warts on the skin, such as on the arms, chest, hands, and feet. These are common warts, not genital warts.
Mucosal (genital) HPV types
The other HPV types are considered mucosal types because they invade and live in cells on mucosal surfaces. The mucosal HPV types are also called genital (or anogenital) HPV types because they often affect the anal and genital area. These types can also infect the lining of the mouth and throat. Mucosal HPV types generally don’t grow in the skin or parts of the body other than the mucosal surfaces.
Low-risk genital HPV types
Low-risk genital HPV types tend to cause warts and not cancer are called low-risk types. Low-risk genital HPV infection can cause cauliflower-shaped warts on or around the genitals and anus of both men and women – technically known as condylomata acuminata on or around the genitals and anus.
For example, HPV types 6 and 11 cause 90% of all genital warts. HPV types 6 and 11 also cause recurrent respiratory papillomatosis, a less common disease in which benign tumors grow in the air passages leading from the nose and mouth into the lungs.
In women, warts may appear in areas that aren’t always noticed, such as the cervix and vagina.
High-risk genital HPV types
High-risk genital HPV types can cause cancer are called high-risk types. About a dozen high-risk HPV types have been identified. Two of these, HPV types 16 and 18, are responsible for most HPV-caused cancers 5. These types have been linked to certain cancers in both men and women. Doctors worry about the cell changes and pre-cancers these types cause because they are more likely to grow into cancers over time.
This diagram shows the different groups of HPV types and the problems each group can cause.
Which cancers are caused by HPV ?
High-risk HPVs cause several types of cancer.
- Cervical cancer: Virtually all cases of cervical cancer are caused by HPV, and just two HPV types, 16 and 18, are responsible for about 70% of all cases 6, 7.
- Anal cancer: About 95% of anal cancers are caused by HPV. Most of these are caused by HPV type 16.
- Oropharyngeal cancers (cancers of the middle part of the throat, including the soft palate, the base of the tongue, and the tonsils): About 70% of oropharyngeal cancers are caused by HPV. In the United States, more than half of cancers diagnosed in the oropharynx are linked to HPV type 16 8.
- Rarer cancers: HPV causes about 65% of vaginal cancers, 50% of vulvar cancers, and 35% of penile cancers 9. Most of these are caused by HPV type 16.
High-risk HPV types cause approximately 5% of all cancers worldwide 10. In the United States, high-risk HPV types cause approximately 3% of all cancer cases among women and 2% of all cancer cases among men 11.
How does high-risk HPV cause cancer ?
HPV infects epithelial cells. These cells, which are organized in layers, cover the inside and outside surfaces of the body, including the skin, the throat, the genital tract, and the anus.
Once HPV enters an epithelial cell, the virus begins to make the proteins it encodes. Two of the proteins made by high-risk HPVs (E6 and E7) interfere with cell functions that normally prevent excessive growth, helping the cell to grow in an uncontrolled manner and to avoid cell death.
Many times these infected cells are recognized by the immune system and eliminated. Sometimes, however, these infected cells are not destroyed, and a persistent infection results. As the persistently infected cells continue to grow, they may develop mutations in cellular genes that promote even more abnormal cell growth, leading to the formation of an area of precancerous cells and, ultimately, a cancerous tumor.
Other factors may increase the risk that an infection with a high-risk HPV type will persist and possibly develop into cancer.
These include 12:
- Smoking or chewing tobacco (for increased risk of oropharyngeal cancer)
- Having a weakened immune system
- Having many children (for increased risk of cervical cancer)
- Long-term oral contraceptive use (for increased risk of cervical cancer)
- Poor oral hygiene (for increased risk of oropharyngeal cancer)
- Chronic inflammation
Researchers believe that it can take between 10 and 30 years from the time of an initial HPV infection until a tumor forms. However, even when severely abnormal cells are seen on the cervix (a condition called cervical intraepithelial neoplasia 3, or CIN3), these do not always lead to cancer. The percentage of CIN3 lesions that progress to invasive cervical cancer has been estimated to be 50% or less 13.
How do you get HPV ?
Mucosal HPV is spread mainly by direct skin-to-skin contact during vaginal, oral, or anal sexual activity. It’s not spread through blood or body fluids. It can be spread even when an infected person has no visible signs or symptoms.
Anyone who has had sexual contact can get HPV, even if it was only with only one person, but infections are more likely in people who have had many sex partners.
The virus can also be spread by genital contact without sex, but this is not common. Oral-genital and hand-genital spread of some genital HPV types have been reported. And there may be other ways to become infected with HPV that aren’t yet clear.
You DO NOT get HPV from:
- Toilet seats
- Hugging or holding hands
- Swimming in pools or hot tubs
- Sharing food or utensils
- Being unclean
Transmission from mother to newborn during birth is rare, but it can happen, too. When it does, it can cause warts (papillomas) in the infant’s breathing tubes (trachea and bronchi) and lungs, which is called respiratory papillomatosis. These papillomas can also grow in the voice box, which is called laryngeal papillomatosis. Both of these infections can cause life-long problems.
How common is HPV ? Who gets it ?
HPV is a very common virus. Some doctors think it’s almost as common as the cold virus. The Centers for Disease Control (CDC) estimates that about 79 million people are currently infected with HPV in the United States, and about 14 million people in the US get a new HPV infection every year.
HPV is so common that most sexually-active men and women will get at least one type of HPV at some point in their lives. Because the infection is so common, most people get HPV infections shortly after becoming sexually active for the first time 14.
Most men and women who have ever had sexual contact get at least one type of genital HPV at some time in their lives. Even people who have only had sex with one person in their lifetime can get HPV.
In most people, the body clears the infection on its own. But sometimes, the infection doesn’t go away. Chronic, or long-lasting infection, especially when it’s caused by certain high-risk HPV types, can cause cancer over time.
Health problems caused by HPV
Health problems related to HPV include genital warts and cervical cancer.
Genital warts: Before HPV vaccines were introduced, roughly 340,000 to 360,000 women and men were affected by genital warts caused by HPV every year.* Also, about one in 100 sexually active adults in the U.S. has genital warts at any given time.
Cervical cancer: More than 11,000 women in the United States get cervical cancer each year.
There are other conditions and cancers caused by HPV that occur in people living in the United States. Every year, approximately 17,600 women and 9,300 men are affected by cancers caused by HPV.
*These figures only look at the number of people who sought care for genital warts. This could be an underestimate of the actual number of people who get genital warts.
Can HPV be prevented ?
HPV is very common, so the only way to keep from becoming infected may be to completely avoid any contact of the areas of your body that can become infected (like the mouth, anus, and genitals) with those of another person. This means not having vaginal, oral, or anal sex, but it also means not allowing those areas to come in contact with someone else’s skin.
HPV vaccines can prevent infection with the types of HPV most likely to cause cancer and genital warts, although the vaccines are most effective when given at a younger age (in older children and teens). The Food and Drug Administration (FDA) has approved three vaccines to prevent HPV infection: Gardasil®, Gardasil® 9, and Cervarix®. These vaccines provide strong protection against new HPV infections, but they are not effective at treating established HPV infections or disease caused by HPV 15.
If you are sexually active, limiting the number of sex partners and avoiding sexual activity with people who have had many other sex partners can help lower your risk of exposure to genital HPV. But again, HPV is very common, so having sexual contact with even one other person can put you at risk.
Condoms can offer some protection from HPV infection, but HPV might be on skin that’s not covered by the condom. And condoms must be used every time, from start to finish. The virus can spread during direct skin-to-skin contact before the condom is put on, and male condoms don’t protect the entire genital area, especially for women. The female condom covers more of the vulva in women, but hasn’t been studied as carefully for its ability to protect against HPV. Condoms are very helpful, though, in protecting against other infections that can be spread through sexual activity.
It’s usually not possible to know who has a mucosal HPV infection, and HPV is so common that even using these measures doesn’t guarantee that a person won’t get infected, but they can help lower the risk.
Can HPV infections be detected ?
HPV infections can be detected by testing a sample of cells to see if they contain viral DNA or RNA.
Several HPV tests are currently approved by the FDA for three cervical screening indications: for follow-up testing of women who seem to have abnormal Pap test results, for cervical cancer screening in combination with a Pap test among women over age 30, and for use alone as a first-line primary cervical cancer screening test for women ages 25 and older.
The most common HPV test detects DNA from several high-risk HPV types in a group, but it cannot identify the specific type(s) that are present. Other tests do tell in addition whether there is DNA or RNA from HPV types 16 and 18, the two types that cause most HPV-associated cancers. These tests can detect HPV infections before abnormal cell changes are evident, and before any treatment for cell changes is needed.
There are no FDA-approved tests to detect HPV infections in men. There are also no currently recommended screening methods similar to a Pap test for detecting cell changes caused by HPV infection in anal, vulvar, vaginal, penile, or oropharyngeal tissues. However, this is an area of ongoing research.
What are treatment options for HPV-infected individuals ?
There is currently no medical treatment for persistent HPV infections that are not associated with abnormal cell changes. However, the genital warts, benign respiratory tract tumors, precancerous changes at the cervix, and cancers resulting from HPV infections can be treated.
Methods commonly used to treat precancerous cervical changes include cryosurgery (freezing that destroys tissue), LEEP (loop electrosurgical excision procedure, or the removal of cervical tissue using a hot wire loop), surgical conization (surgery with a scalpel, a laser, or both to remove a cone-shaped piece of tissue from the cervix and cervical canal), and laser vaporization conization (use of a laser to destroy cervical tissue).
Treatments for other types of benign respiratory tract tumors and precancerous changes caused by HPV (vaginal, vulvar, penile, and anal lesions) and genital warts include topical chemicals or drugs, excisional surgery, cryosurgery, electrosurgery, and laser surgery. Treatment approaches are being tested in clinical trials, including a randomized controlled trial that will determine whether treating anal precancerous lesions will reduce the risk of anal cancer in people who are infected with HIV.
HPV-infected individuals who develop cancer generally receive the same treatment as patients whose tumors do not harbor HPV infections, according to the type and stage of their tumors. However, people who are diagnosed with HPV-positive oropharyngeal cancer may be treated differently than people with oropharyngeal cancers that are HPV-negative. Recent research has shown that patients with HPV-positive oropharyngeal tumors have a better prognosis and may do just as well on less intense treatment. Ongoing clinical trials are investigating this question 16.
HPV in Men
How do men get HPV ?
You can get HPV by having sex with someone who is infected with HPV. This disease is spread easily during anal or vaginal sex, and it can also be spread through oral sex or other close skin-to-skin touching during sex. HPV can be spread even when an infected person has no visible signs or symptoms.
Will HPV in Men cause health problems ?
Most of the time HPV infections completely go away and don’t cause any health problems. However, if an infection does not go away on its own, it is possible to develop HPV symptoms months or years after getting infected. This makes it hard to know exactly when you became infected. Lasting HPV infection can cause genital warts or certain kinds of cancer. It is not known why some people develop health problems from HPV and others do not.
What are the symptoms of HPV in Men ?
Most men who get HPV never develop symptoms and the infection usually goes away completely by itself. However, if HPV does not go away, it can cause genital warts or certain kinds of cancer.
See your healthcare provider if you have questions about anything new or unusual such as warts, or unusual growths, lumps, or sores on your penis, scrotum, anus, mouth, or throat.
What are the symptoms of genital warts in men ?
Genital warts usually appear as a small bump or group of bumps in the genital area around the penis or the anus. These warts might be small or large, raised or flat, or shaped like a cauliflower. The warts may go away, or stay the same, or grow in size or number. Usually, a healthcare provider can diagnose genital warts simply by looking at them. Genital warts can come back, even after treatment. The types of HPV that cause warts do not cause cancer.
Can HPV in men cause cancer ?
Yes. HPV infection isn’t cancer but can cause changes in the body that lead to cancer. HPV infections usually go away by themselves but having an HPV infection can cause certain kinds of cancer to develop. These include cervical cancer in women, penile cancer in men, and anal cancer in both women and men. HPV can also cause cancer in the back of the throat, including the base of the tongue and tonsils (called oropharyngeal cancer). All of these cancers are caused by HPV infections that did not go away. Cancer develops very slowly and may not be diagnosed until years, or even decades, after a person initially gets infected with HPV. Currently, there is no way to know who will have only a temporary HPV infection, and who will develop cancer after getting HPV.
Although HPV is the most common sexually transmitted infection, HPV-related cancers are not common in men.
Certain men are more likely to develop HPV-related cancers:
- Men with weak immune systems (including those with HIV) who get infected with HPV are more likely to develop HPV-related health problems.
- Men who receive anal sex are more likely to get anal HPV and develop anal cancer.
Can men get tested for HPV ?
No, there is currently no approved test for HPV in men.
Routine testing (also called ‘screening’) to check for HPV or HPV-related disease before there are signs or symptom, is not recommended by the CDC for anal, penile, or throat cancers in men in the United States. However, some healthcare providers do offer anal Pap tests to men who may be at increased risk for anal cancer, including men with HIV or men who receive anal sex. If you have symptoms and are concerned about cancer, please see a healthcare provider.
Can men get treatment for HPV or health problems caused by HPV ?
There is no specific treatment for HPV, but there are treatments for health problems caused by HPV. Genital warts can be treated by your healthcare provider, or with prescription medication. HPV-related cancers are more treatable when diagnosed and treated promptly.
How can men lower my chance of getting HPV ?
There are two steps you can take to lower your chances of getting HPV and HPV-related diseases:
- Get vaccinated. The HPV vaccine is safe and effective. It can protect men against warts and certain cancers caused by HPV. Ideally, you should get vaccinated before ever having sex (see below for the recommended age groups). CDC recommends 11 to 12 year olds get two doses of HPV vaccine to protect against cancers caused by HPV. For more information on the recommendations, please see: 17
- Use condoms the correct way every time you have sex. This can lower your chances of getting all STIs, including HPV. However, HPV can infect areas that are not covered by a condom, so condoms may not give full protection against getting HPV.
Can men get the HPV vaccine ?
In the United States, The HPV vaccine is recommended for the following men:
- All boys at age 11 or 12 years (or as young as 9 years)
- Older boys through age 21 years, if they did not get vaccinated when they were younger
- Gay, bisexual, and other men who have sex with men through age 26 years, if they did not get vaccinated when they were younger
- Men with HIV or weakened immune systems through age 26 years, if they did not get vaccinated when they were younger
What does having HPV mean for me or my sex partner’s health ?
See a healthcare provider if you have questions about anything new or unusual (such as warts, growths, lumps, or sores) on your own or your partner’s penis, scrotum, anus, mouth or throat. Even if you are healthy, you and your sex partner(s) may also want to get checked by a healthcare provider for other STIs.
If you or your partner have genital warts, you should avoid having sex until the warts are gone or removed. However, it is not known how long a person is able to spread HPV after warts are gone.
What does HPV mean for my relationship ?
HPV infections are usually temporary. A person may have had HPV for many years before it causes health problems. If you or your partner are diagnosed with an HPV-related disease, there is no way to know how long you have had HPV, whether your partner gave you HPV, or whether you gave HPV to your partner. HPV is not necessarily a sign that one of you is having sex outside of your relationship. It is important that sex partners discuss their sexual health, and risk for all STIs, with each other.
HPV in Women
What are the symptoms of HPV in Women ?
Mucosal HPV infection usually has no symptoms, unless it’s an HPV type that causes genital warts. Genital warts may appear within weeks or months after contact with a partner who has HPV. The warts may also show up years after exposure, but this is rare. The warts usually look like small bumps or groups of bumps in the genital area. They can be small or large, raised or flat, or shaped like a cauliflower. If they’re not treated, genital warts might go away, stay and not change, or increase in size or number. But warts rarely turn into cancer.
Most people will never know they have HPV because they have no symptoms. In most people, their immune system attacks the virus and clears the HPV infection, typically within 2 years. This is true of both high-risk and low-risk HPV types. But sometimes HPV infections are not cleared. This can lead to cell changes that over many years may develop into cancer.
I’m pregnant. Will having HPV affect my pregnancy ?
If you are pregnant and have HPV, you can get genital warts or develop abnormal cell changes on your cervix. Abnormal cell changes can be found with routine cervical cancer screening. You should get routine cervical cancer screening even when you are pregnant.
Will HPV affect my pregnancy or my baby ?
HPV infection does not directly affect the chances of getting pregnant.
If HPV infection leads to cervical changes that need to be treated, the treatment should not affect your chances of getting pregnant. But if you have many treatments and biopsies, which can happen with more frequent screening, the risk of pre-term labor and low birth weight babies can go up.
HPV is rarely passed from a mother to her baby. The rare cases where this has happened do not involve the types of HPV that can cause cancer.
Can women be treated for HPV or health problems caused by HPV ?
There’s no treatment for the virus itself. But most genital HPV infections go away with the help of a person’s immune system.
However, there are treatments for the health problems that HPV can cause:
- Genital warts can be treated by your healthcare provider or with prescription medication. If left untreated, genital warts may go away, stay the same, or grow in size or number.
- Cervical precancer can be treated. Women who get routine Pap tests and follow up as needed can identify problems before cancer develops. Prevention is always better than treatment.
- Other HPV-related cancers are also more treatable when diagnosed and treated early.
Testing for HPV in Women
What’s the difference between a Pap test and an HPV test ?
A Pap test is used to find cell changes or abnormal cells in the cervix. (These abnormal cells may be pre-cancer or cancer, but they may also be other things, too.) Cells are lightly scraped or brushed off the cervix. They are sent to a lab and looked at under a microscope to see if the cells are normal or if changes can be seen. The Pap test is a very good test for finding cancer cells and cells that might become cancer.
HPV is a virus that can cause cervix cell changes. The HPV test checks for the virus, not cell changes. The test can be done at the same time as the Pap test, with the same swab or a second swab. You won’t notice a difference in your exam if you have both tests. A Pap test plus an HPV test (called co-testing) is the preferred way to find early cervical cancers or pre-cancers in women 30 and older.
Should women be tested for HPV ?
If you are a woman under age 30
The American Cancer Society recommends that women between ages 21 and 29 should have a Pap test every 3 years (at ages 21, 24, and 27) to test for cervical cancer and pre-cancers. These women should not get the HPV test with the Pap test (co-testing) because HPV is so common in women these ages that it’s not helpful to test for it. But HPV testing may be used in this age group after an abnormal Pap test result.
The most common abnormal Pap test result seen is called ASC-US (your health care provider may say this as “ask us”). ASC-US cells usually are not pre-cancer, but they aren’t quite normal either. If there are ASC-US cells in your Pap test result, an HPV test may be done to see if HPV is causing the cell changes. If HPV is found, you’ll need more tests.
In cases like this, the HPV test is used to help decide if more testing is needed. This is not the same as using the HPV test with the Pap test as part of your normal health visit.
Women who are HIV positive or who have been diagnosed or treated for a cervical cancer or pre-cancer should talk to their health care providers about how often they should be tested for cervical cancer and what tests should be used.
If you are a woman aged 30 to 65
The American Cancer Society recommends that women aged 30 to 65 have an HPV test with their Pap test (co-testing) every 5 years to test for cervical cancer. Talk to your health care provider about co- testing. It’s also OK to continue just to have Pap tests every 3 years.
Women who are HIV positive or who have been diagnosed or treated for a cervical cancer or pre-cancer should talk to their health care providers about how often they should be tested for cervical cancer and what tests should be used.
Why should women over age 30 with normal test results change to co-testing every 5 years and start doing HPV testing ? Is that safe ?
Cell changes in the cervix happen very slowly. It usually takes more than 10 years for cell changes to become cancer. Pap tests have been done yearly in the past, but now we know that Pap tests are not needed every year – every 3 years is enough. In fact, doing Pap tests every year can lead to unneeded treatment of cell changes that would never go on to cause cancer.
One of the benefits of adding testing for HPV is that women can get cervical cancer testing even less often. Getting the Pap test and HPV test (co-testing) every 5 years means fewer tests, follow-up visits, and treatments may be needed. Women with normal Pap and HPV test results have almost no chance of getting cervical cancer within at least 5 years.
Co-testing is preferred, but it’s also OK to continue to have the Pap test alone every 3 years.
What about testing other sites on the body, or testing men ?
There’s no FDA-approved HPV test for men at this time, nor is there an FDA-approved HPV test to find the virus anywhere besides the cervix, including the mouth or throat.
The FDA has only approved tests to find HPV in a woman’s cervix, where positive results can be managed with extra testing and prompt treatment if the infection causes abnormal cell growth. Although HPV tests might be used in research studies to look for HPV in other sites, there’s no proven way to manage positive findings. Also, the accuracy of the test itself may be affected by the site it’s taken from and the way the sample is taken.
Finally, there’s no useful test to find out a person’s “HPV status,” because an HPV test result can change over a period of months or years as the body fights the virus.
If I have a positive HPV test, what does it mean ?
If you have cervical HPV infection and an abnormal Pap test result, your health care provider will explain what other tests you might need.
If you have cervical HPV infection and a normal Pap test result, it means that you have genital HPV, but no cell changes were seen on your Pap test.
There are 2 options:
- You’ll most likely be tested with an HPV test and a Pap test again in 12 months.
- In most cases, re-testing in 12 months shows no sign of the virus.
- If the virus does go away and your Pap test is normal you can go back to normal screening.
- If the virus is still there or changes are seen on the Pap test, you’ll need more testing.
- As another option, the provider may suggest testing specifically for HPV-16 or both -16 and -18 (the 2 types that are most likely to cause cervical cancer).
- If testing shows that you have HPV-16 and/or -18, more testing will be needed.
- If the test doesn’t show infection with HPV-16 and/or -18, you should be retested in 12 months with both an HPV test and a Pap test.
If HPV goes away, can you get it again ?
There are many types of HPV. You may have one type that goes away, but you can get another different type. It’s possible to get the same type again, but the risk of this is low.
HPV vaccine
Over 30,000 people in the United States each year are affected by a cancer caused by HPV infection. While there is screening available for cervical cancer for women, there is no screening for the other cancers caused by HPV infection, like cancers of the mouth/throat, anus/rectum, penis, vagina, or vulva.
HPV vaccination provides safe, effective, and lasting protection against the HPV infections that most commonly cause cancer.
Are HPV vaccines safe ?
All of the HPV vaccines were tested in thousands of people around the world before they were approved. So far, all studies show no serious side effects caused by the vaccines, and no deaths have been linked to any HPV vaccine. Common, mild side effects include pain and redness where the shot was given, fever, dizziness, and nausea.
People may faint after getting any vaccine, including HPV vaccines. Fainting after getting a shot is more common in teens than in young children or adults. To keep people from getting hurt from fainting, a 15-minute waiting period for people of all ages is recommended after any vaccination.
Monitoring for possible side effects
Like all vaccines, even “old” vaccines approved many years ago, the HPV vaccines are continuously monitored for side effects. The US Centers for Disease Control and Prevention (CDC) and the US Food and Drug Administration (FDA) review all serious side effects reported to the Vaccine Adverse Event Reporting System (VAERS) to watch for potential safety concerns that may need further study.
What Types of HPV Vaccines Are There ?
Two HPV vaccines have been licensed by the U.S. Food and Drug Administration (FDA).
- Gardasil (Merck) is a quadrivalent HPV vaccine (4vHPV) that protects against HPV types 6, 11, 16, and 18.
- Gardasil-9 (Merck) is a nine-valent HPV vaccine (9vHPV) that protects against HPV types 6, 11, 16, 18, 31, 45, 52, and 58.
All two HPV vaccines protect against the two HPV types, 16 and 18, that cause most HPV cancers.
Who Should Get This Vaccine
Either Gardasil or Gardasil-9 is recommended for boys and girls 11 or 12 years old, or starting at 9 years old. The vaccine can be given to people up to 26 years old.
Gardasil is given as a 3-dose series:
First dose: now
Second dose: 1 to 2 months after the first dose
Third dose: 6 months after the first dose
Gardasil-9 is given as a 2-dose series to boys and girls 9 through 14 years old:
First dose: now
Second dose: 6 to 12 months after the first dose
If vaccine is given at 15 years or older, 3 doses are recommended
Pregnant women should not receive this vaccine. However, there have been no problems found in women who received the vaccine during pregnancy, before they knew they were pregnant.
Why is the HPV vaccine important ?
Genital HPV is a common virus that is passed from one person to another through direct skin-to-skin contact during sexual activity. Most sexually active people will get HPV at some time in their lives, though most will never even know it. HPV infection is most common in people in their late teens and early 20s. There are about 40 types of HPV that can infect the genital areas of men and women. Most HPV types cause no symptoms and go away on their own. But some types can cause cervical cancer in women and other less common cancers — like cancers of the anus, penis, vagina, and vulva and oropharynx. Other types of HPV can cause warts in the genital areas of men and women, called genital warts. Genital warts are not life-threatening. But they can cause emotional stress and their treatment can be very uncomfortable. Every year, about 12,000 women are diagnosed with cervical cancer and 4,000 women die from this disease in the U.S. About 1% of sexually active adults in the U.S. have visible genital warts at any point in time.
- These vaccines do not treat cervical cancer.
Can a vaccine help prevent HPV ?
Yes. Vaccines are available to help prevent infection by certain types of HPV and some of the cancers linked to those types. Gardasil®, Gardasil 9®, and Cervarix® are the brand names of the vaccines used today.
All of these vaccines help prevent infection by HPV-16 and HPV-18. These 2 types cause about 70% of all cervical cancers and pre-cancers, as well as many cancers of the anus, penis, vulva, vagina, and throat.
Gardasil also helps prevent infection by the 2 types of HPV (HPV-6 and HPV-11) that cause most genital warts.
Gardasil 9 helps prevent infection with the same 4 types of HPV as Gardasil, plus 5 other high risk types: 31, 33, 45, 52 and 58. Together these types cause about 90% of cervical cancers.
How Well Do These HPV Vaccines Work ?
HPV vaccination works extremely well. Clinical trials showed the vaccines provided close to 100% protection against pre-cancers and, for Gardasil and Gardasil 9, genital warts.
- Since the vaccine was first recommended in 2006, there has been a significant reduction in HPV infections.
- Research has also shown that fewer teens and young adults are getting genital warts.
- In other countries such as Australia where there is higher HPV vaccination coverage, HPV vaccine has also reduced the number of cases of precancers of the cervix in young women in that country.
- Also, genital warts have decreased dramatically in young adults in Australia since the HPV vaccine was introduced.
HPV vaccine offers long-lasting protection against HPV infection and HPV disease:
- 10 years of data show that HPV vaccination provides long-lasting protection.
- There is no evidence to suggest that HPV vaccine loses the ability to provide protection over time.
Who should be vaccinated against HPV and when ?
HPV vaccine produces the strongest immune response in preteens. To work best, the HPV vaccines should be given at age 11 or 12. The vaccines are given in a series of shots.
The American Cancer Society’s recommendations for HPV vaccine use
- Routine HPV vaccination for girls and boys should be started at age 11 or 12. The vaccination series can be started as early as age 9.
- HPV vaccination is also recommended for females 13 to 26 years old and for males 13 to 21 years old who have not started the vaccines, or who have started but not completed the series. Males 22 to 26 years old may also be vaccinated.*
- HPV vaccination is also recommended through age 26 for men who have sex with men and for people with weakened immune systems (including people with HIV infection), if they have not previously been vaccinated.
- Transgender individuals should also get HPV vaccine until they are 27.
*For people 22 to 26 years old who have not started the vaccines, or who have started but not completed the series, it’s important to know that vaccination at older ages is less effective in lowering cancer risk.
The Centers for Disease Prevention and Control (CDC) recommends that 11- to 12-year-olds receive two doses of HPV vaccine at least six months apart to protect against cancers caused by human papillomavirus (HPV) infections 18.
- The first dose is routinely recommended at 11-12 years old.
- The second dose of the vaccine should be administered 6 to 12 months after the first dose.
- Vaccination with the two-dose series can be started at age 9 and through age 14.
Teens and young adults who start the series later, at ages 15 through 26 years, need three doses of HPV vaccine to protect against cancer-causing HPV infection.
- Adolescents aged 9 through 14 years who have already received two doses of HPV vaccine less than 5 months apart, will require a third dose.
- Three doses are recommended for people with weakened immune systems aged 9-26 years.
Why should the vaccines be given to pre-teens ?
The vaccines work best at this age. Research shows that younger people have a better immune response to the vaccine than those in their late teens and early 20s. And, the vaccines will prevent the covered types of HPV only if they are given before exposure to the virus.
This is also an age when other vaccinations are given, and when children are likely to still be getting regular medical check-ups.
What about men and women older than 26 ? Should they get one of the vaccines ?
HPV vaccines are not approved nor recommended after age 26. While the vaccines are safe, they will not provide much, if any, benefit.
Who should not get one of the HPV vaccines or who should wait ?
Pregnant women should not get any HPV vaccine at this time, even though they appear to be safe for both mother and the unborn baby. If a woman who is pregnant does get an HPV vaccine, it’s not a reason to consider ending the pregnancy. Women who started a vaccine series before they learned they were pregnant should complete the series after the pregnancy.
Make sure the health care provider knows about any severe allergies.
The following should not get an HPV vaccine:
- Anyone with a severe allergy to latex should not get the Cervarix vaccine.
- Those with a severe allergy to yeast should not receive Gardasil or Gardasil 9.
- Anyone who has ever had a life-threatening allergic reaction to anything else contained in the vaccines
- Anyone who has had a serious reaction to an earlier dose of HPV vaccine
Is HPV testing needed before getting the vaccine ?
No. In fact, testing is not recommended because it cannot show if the HPV vaccine will be effective or not. A positive HPV test result doesn’t always tell you which types of HPV you have. And even if you are infected with one type of HPV, the vaccine could still prevent other types of HPV infection. A negative test result cannot tell you if you’ve had HPV in the past.
How long will the vaccines prevent HPV infection ?
How long a vaccine will protect people is never known when the vaccine is first introduced. Current research shows that the vaccines are effective, and there’s no sign that the protection decreases with time. Research will continue to look at how long protection against HPV lasts, and if booster shots will be needed.
Do women who have been vaccinated against HPV still need Pap tests ?
Yes. Women who have been vaccinated will still need regular testing for cervical cancer because the vaccines do not prevent all of the types of HPV that can cause cervical cancer.
HPV vaccine side effects
Vaccines, like any medicine, can have side effects. Many people who get HPV vaccine have no side effects at all. Some people report having very mild side effects, like a sore arm from the shot.
The most common side effects of HPV vaccine are usually mild, and include:
- Pain, redness, or swelling in the arm where the shot was given
- Fever
- Headache or feeling tired
- Nausea
- Muscle or joint pain
Brief fainting spells and related symptoms (such as jerking movements) can happen after any medical procedure, including vaccination. Sitting or lying down when getting a shot and staying in that position for about 15 minutes after a vaccination can help prevent fainting and injuries caused by falls.
On very rare occasions, severe (anaphylactic) allergic reactions may occur after vaccination. People with severe allergies to any component of a vaccine should not receive that vaccine.
References- HPV and HPV Testing. https://www.cancer.org/cancer/cancer-causes/infectious-agents/hpv/hpv-and-hpv-testing.html
- Satterwhite CL, Torrone E, Meites E, et al. Sexually transmitted infections among US women and men: Prevalence and incidence estimates, 2008. Sexually Transmitted Diseases 2013; 40(3):187-193. https://www.ncbi.nlm.nih.gov/pubmed/23403598
- Chesson HW, Dunne EF, Hariri S, Markowitz LE. The estimated lifetime probability of acquiring human papillomavirus in the United States. Sexually Transmitted Diseases 2014; 41(11):660-664. https://www.ncbi.nlm.nih.gov/pubmed/25299412
- Hariri S, Unger ER, Sternberg M, et al. Prevalence of genital human papillomavirus among females in the United States, the National Health and Nutrition Examination Survey, 2003–2006. Journal of Infectious Diseases 2011; 204(4):566–573. https://www.ncbi.nlm.nih.gov/pubmed/21791659
- Lowy DR, Schiller JT. Reducing HPV-associated cancer globally. Cancer Prevention Research (Philadelphia) 2012;5(1):18-23. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3285475/
- Division of STD Prevention (1999). Prevention of genital HPV infection and sequelae: report of an external consultants’ meeting. Atlanta, GA: Centers for Disease Control and Prevention. https://www.cdc.gov/std/hpv/HPVSupplement99.pdf
- Winer RL, Hughes JP, Feng Q, et al. Condom use and the risk of genital human papillomavirus infection in young women. New England Journal of Medicine 2006; 354(25):2645–2654. http://www.nejm.org/doi/full/10.1056/NEJMoa053284
- Chaturvedi AK, Engels EA, Pfeiffer RM, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. Journal of Clinical Oncology 2011; 29(32):4294–4301. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3221528/
- Gillison ML, Chaturvedi AK, Lowy DR. HPV prophylactic vaccines and the potential prevention of noncervical cancers in both men and women. Cancer 2008; 113(10 Suppl):3036-3046. https://www.ncbi.nlm.nih.gov/pubmed/18980286
- de Martel C, Ferlay J, Franceschi S, et al. Global burden of cancers attributable to infections in 2008: A review and synthetic analysis. Lancet Oncology 2012; 13(6):607-615. https://www.ncbi.nlm.nih.gov/pubmed/22575588
- Jemal A, Simard EP, Dorell C, et al. Annual Report to the Nation on the Status of Cancer, 1975-2009, featuring the burden and trends in human papillomavirus (HPV)-associated cancers and HPV vaccination coverage levels. Journal of the National Cancer Institute 2013; 105(3):175-201. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3565628/
- Shi R, Devarakonda S, Liu L, Taylor H, Mills G. Factors associated with genital human papillomavirus infection among adult females in the United States, NHANES 2007-2010. Biomed Central Research Notes 2014; 7:544. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4141114/
- McCredie MR, Sharples KJ, Paul C, et al. Natural history of cervical neoplasia and risk of invasive cancer in women with cervical intraepithelial neoplasia 3: A retrospective cohort study. Lancet Oncology 2008; 9(5):425-434. https://www.ncbi.nlm.nih.gov/pubmed/18407790
- Winer RL, Feng Q, Hughes JP, et al. Risk of female human papillomavirus acquisition associated with first male sex partner. Journal of Infectious Diseases 2008; 197(2):279-282. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2875685/
- Schiller JT, Castellsague X, Garland SM. A review of clinical trials of human papillomavirus prophylactic vaccines. Vaccine 2012; 30 Suppl 5:F123-138. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4636904/
- Mirghani H, Amen F, Blanchard P, et al. Treatment de-escalation in HPV-positive oropharyngeal carcinoma: Ongoing trials, critical issues and perspectives. International Journal of Cancer 2015;136(7):1494-503. https://www.ncbi.nlm.nih.gov/pubmed/24622970
- https://www.cdc.gov/hpv/parents/questions-answers.html
- Human Papillomavirus (HPV) Vaccination: What Everyone Should Know. https://www.cdc.gov/vaccines/vpd/hpv/public/index.html