Hypertriglyceridemia
Hypertriglyceridemia also called elevated plasma triglyceride concentration, refers to a fasting plasma triglyceride above 150 to 199 mg/dL (1.7-2.2 mmol/L) in adults, typically above the 95th percentile for age and sex, although additional quantitative or qualitative lipoprotein abnormalities can also be present 1. Hypertriglyceridemia can result from a variety of causes. Mild to moderate hypertriglyceridemia occurs commonly as part of the metabolic syndrome, can be the result of multiple genetic mutations in an individual or family and can be secondary to several diseases and drugs 2.
Your doctor will usually check for high triglycerides as part of a cholesterol test, which is sometimes called a lipid panel or lipid profile. You’ll have to fast before blood can be drawn for an accurate triglyceride measurement.
For adults, triglyceride levels results are categorized as follows:
- Normal: Less than 150 mg/dL (1.7 mmol/L)
- Mild high: 150 to 199 mg/dL (1.7-2.2 mmol/L)
- Moderate high: 200 to 999 mg/dL (2.3-11.3 mmol/L)
- Severe high: 1,000 to 1,999 mg/dL (11.3-22.6 mmol/L)
- Very severe: Greater than 2,000 mg/dL (22.6 mmol/L)
Note: For improved metabolic health and protection to the heart and blood vessels, the American Heart Association now recommends an optimum fasting triglyceride level of 100 mg/dL (1.12 mmol/L). This puts an even stronger emphasis on lifestyle change which has been the recommended therapy for mildly elevated triglycerides. However, the American Heart Association does not recommend people use drug therapy to achieve this optimal level because there has not been adequate study to show that drug therapy to lower triglycerides to this level is helpful. Many people will be able to reduce their triglycerides as well as other metabolic risk factors such as elevated blood sugar and elevated blood pressure with diet, weight loss and increased physical activity.
For children, teens and young adults:
- From newborn to age 9
- Acceptable: Less than 75 mg/dL (0.85 mmol/L)
- Borderline high: 75-99 mg/dL (0.85-1.12 mmol/L)
- High: Greater than 100 mg/dL (1.13 mmol/L)
- For ages 10-19 years
- Acceptable: Less than 90 mg/dL (1.02 mmol/L)
- Borderline high: 90-129 mg/dL (1.02-1.46 mmol/L)
- High: Greater than 130 mg/dL (1.47 mmol/L)
- For young adults older than 19
- Acceptable: Less than 115 mg/dL (1.30 mmol/L)
- Borderline high: 115-149 mg/dL (1.30-1.68 mmol/L)
- High: Greater than 150 mg/dL (1.7 mmol/L)
When triglycerides are very high (greater than 1000 mg/dL (11.30 mmol/L)), there is a risk of developing pancreatitis in children and adults. Treatment to lower triglycerides should be started as soon as possible.
Note: These values are based on fasting triglyceride levels.
Serum triglycerides are higher in men than in women 3. Serum triglycerides increase with age in both genders. In youth and adolescents, with increasing obesity rates, the prevalence of hypertriglyceridemia is increasing as well. In the National Health and Nutrition Examination Survey 1999 through 2004, about a third of participants had serum triglycerides above 150 mg/dL 3. In subjects aged 60 years or older, prevalence was 42%. Two percent of subjects with hypertriglyceridemia had triglycerides of more than 500 mg/dL. The incidence of hypertriglyceridemia also varies by race, with a higher incidence in Hispanic-Americans and Asian-Indians, and lower incidence in African-Americans who generally have lower triglyceride levels.
The serum triglyceride level reflects the concentration of the triglyceride-rich lipoproteins (VLDL and chylomicrons). VLDL (very-low-density lipoprotein) and chylomicrons become relatively cholesterol-enriched once the triglyceride core is hydrolyzed at peripheral tissues. It appears that remnant triglyceride-rich lipoproteins, as opposed to very large triglyceride-rich lipoproteins, may be atherogenic. Although triglyceride itself is not found in atherosclerotic plaques, it is thought that the cholesterol content of triglyceride-rich lipoproteins may contribute to plaque development. Also, the lipolysis of triglyceride-rich lipoproteins produces free fatty acids, lysolecithin, and other reactive lipids that may have pro-inflammatory and pro-coagulant effects.
The plasma level of triglyceride is a well-established independent biomarker of cardiovascular disease risk 4 and triglyceride-rich lipoproteins have atherogenic properties. Triglyceride predicts cardiovascular disease in a wide range of circumstances. Its association with cardiovascular disease risk is partly attenuated by adjustment for HDL cholesterol, with which it is moderately correlated 5.
Genetic variation associated with lifelong low triglyceride levels is associated with a lower incidence of cardiovascular disease 6. Triglyceride is carried primarily within large lipoproteins, chylomicrons, and VLDL (very low density lipoprotein), which are also rich in cholesterol and like LDL can enter the arterial wall and stimulate atherosclerosis. These triglyceride-rich lipoproteins carry various atherogenic proteins such as apolipoprotein C-III, itself associated with atherosclerosis and cardiovascular disease 7.
Replacing 1% of daily energy intake from saturated fat with polyunsaturated or monounsaturated fat lowers triglyceride by 0.9 or 0.4 mg/dL 8 perhaps more in those with hypertriglyceridemia 9.
Replacing the 1% saturated fat with 1% carbohydrates raises serum triglycerides by ≈1 mg/dL. Dietary carbohydrates raise plasma triglyceride levels by increasing the production by the liver of triglycerides and subsequent incorporation into VLDL (very low density lipoprotein) 9. The magnitude that dietary carbohydrates increase plasma triglyceride is similar whether the carbohydrate has a high or low glycemic index 10.
Most often, having high triglycerides has no warning signs or symptoms. Levels above 150mg/dl (1.7 mmol/L) may raise your risk for heart disease. A triglyceride level of 150 mg/dL (1.7 mmol/L) or higher is also a risk factor for metabolic syndrome. Above 2,000 mg/dL (22.58 mmol/L) poses a high risk for pancreatitis [inflammation of the pancreas]. Triglycerides are the most common type of fat in your body and triglycerides store excess energy (calories) from your diet, thus triglycerides is a major source of energy for your body. Triglycerides is stored in your body’s fat (adipose) cells and is also found in foods such as dairy products, meat and cooking oils. Some triglycerides circulate in your blood to provide fuel for muscles to work. After a person eats, an increased level of triglycerides is found in the blood as the body converts the excess calories (energy you don’t need right away) into fat. Triglycerides move via the blood from the gut to adipose (fat) tissue for storage. In between meals, triglycerides are released from fat tissue to be used as an energy source for your body. Most triglycerides are carried in the blood by lipoproteins called very low-density lipoproteins (VLDL).
If you are diabetic and your blood sugar (glucose) is out of control, your triglycerides may be very high.
Certain drugs such as corticosteroids, protease inhibitors for HIV, beta blockers, and estrogens can increase blood triglyceride levels.
Triglycerides change dramatically in response to meals, increasing as much as 5 to 10 times higher than fasting levels just a few hours after eating. Even fasting levels vary considerably day to day. Therefore, modest changes in fasting triglycerides measured on different days are not considered to be abnormal.
Normal triglyceride levels vary by age and sex. Triglycerides normally increase with age.
Also, many people with high triglycerides have other lipid problems or other risk factors for heart disease. A high triglyceride level is one part of the metabolic syndrome, a cluster of risk factors that increase the risk for heart disease and diabetes. People with high triglycerides often have a high total cholesterol level, including a high LDL (bad) cholesterol level and a low HDL (good) cholesterol level. Many people with heart disease or diabetes also have high triglyceride levels.
The management of hypertriglyceridemia is by a multidisciplinary team that includes an endocrinologist, gastroenterologist, internist, primary care provider, nurse practitioner and a cardiologist. Appropriate management of the patient with hypertriglyceridemia requires knowledge of the likely cause of the hypertriglyceridemia, in order to prevent its complications. Although current guidelines agree that a triglyceride level of less than 150 mg/dL is desirable, the number varies in definitions of hypertriglyceridemia and recommendations concerning management. Besides pharmacological therapy the key is lifestyle changes. This includes dietary changes, for example, the reducing your carbohydrate intake, avoidance of sugar-sweetened beverages and processed carbohydrates, along with exercise and weight loss, is the foundation in managing hypertriglyceridemia. Weight loss of 5% to 10% can reduce triglycerides by about 20%, and regular aerobic exercise can reduce triglycerides by 10% to 20%. Even with all the controversy surrounding dietary fat, a mono-unsaturated fatty acid rich Mediterranean-type diet has been shown in many studies to reduce postprandial (after meal) lipemia (high blood fat). In the setting of triglyceride levels above 500 mg/dL, dietary fat restriction becomes important to avoid post prandial rise in chylomicrons to levels that increase risk of pancreatitis. Addressing the underlying cause and secondary contributors is important. Quitting alcohol, and improving glycemic control in patients with diabetes, is effective in improving secondary components of hypertriglyceridemia. In patients with triglycerides of more than 500 mg/dL, the primary goal is to reduce triglycerides levels to triglycerides the risk of pancreatitis. In patients with mild to moderate elevations in triglycerides (200 mg/dL to 500 mg/dL), the focus should be on preventing cardiovascular disease. For cardiovascular risk reduction, the goal should be to reduce non-HDL cholesterol level down to 30 mg/dL above LDL goal. Those who remain compliant with lifestyle changes and medications have a good outcome with fewer complications 11.
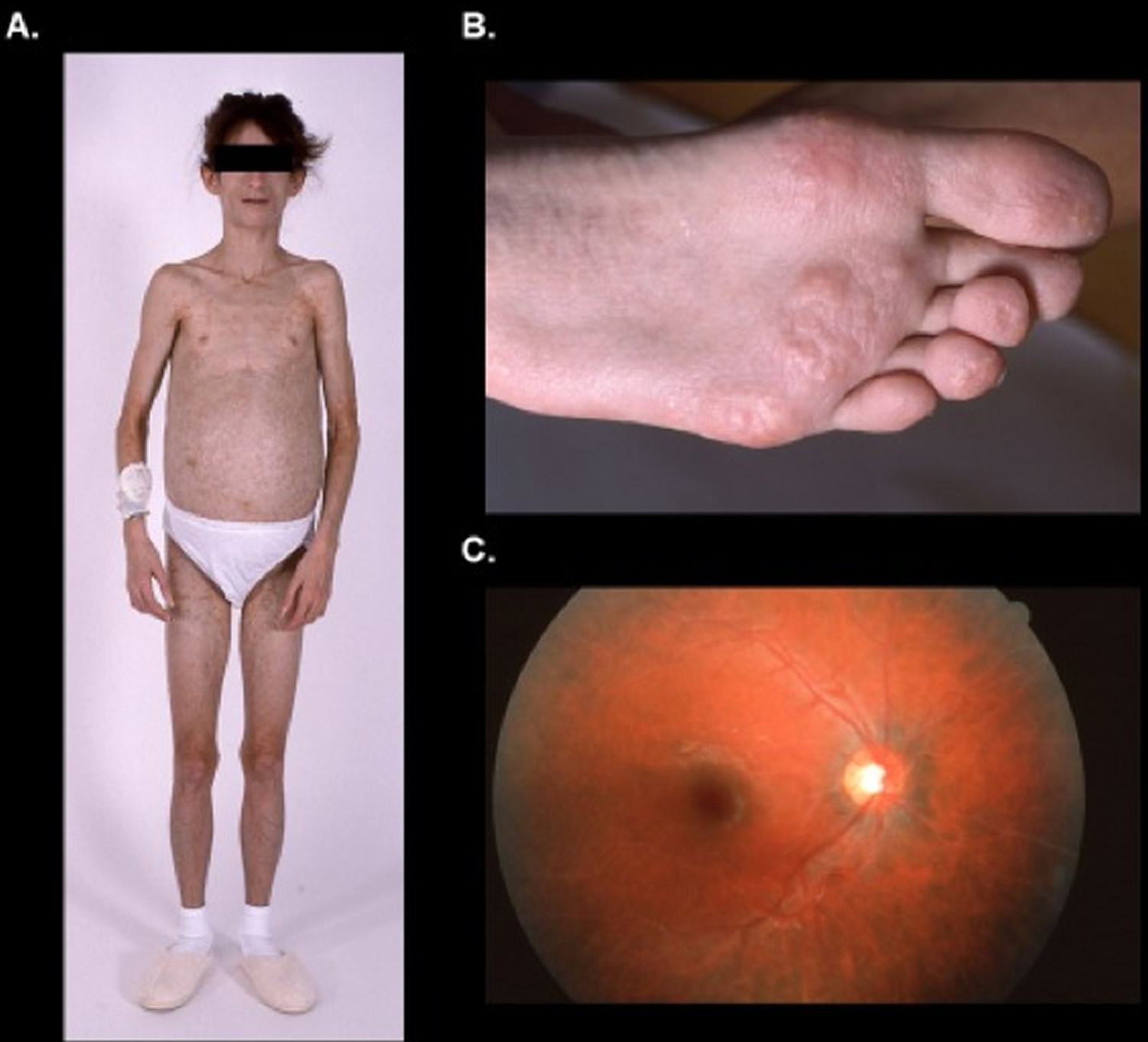
Figure 1. Hypertriglyceridemia
Footnote: Generalized lack of subcutaneous fat (6A), eruptive xanthomata (6B), and lipemia retinalis (6C) secondary to severe hypertriglyceridemia in a patient with heterozygous LMNA p.T10I pathogenic variant.
[Source 12 ]Figure 2. Triglyceride
Hypertriglyceridemia causes
Elevated triglycerides can be caused by several factors. Hypertriglyceridemia in many cases is multifactorial, resulting from the combination of genetic factors and other causes of increased production and or impaired clearance of triglyceride-rich lipoproteins 13.
Several factors can contribute to high triglyceride level, including:
- Being overweight, or obesity
- Physical inactivity
- Cigarette smoking
- Excess alcohol consumption
- A diet very high in carbohydrates (more than 60 percent of total calories)
- Sometimes underlying diseases or genetic disorders can also cause high triglyceride levels.
These factors can be addressed with lifestyle changes.
Genetic causes
The primary disorders predominantly causing high triglyceride are 14:
- Familial hypertriglyceridemia. Familial hypertriglyceridemia is a common autosomal dominant inherited disorder characterized by increased plasma concentration of very-low-density lipoprotein (VLDL) (type 4 lipoprotein pattern), typically with low LDL (low-density lipoprotein) and HDL (high-density lipoprotein) 14. Usually asymptomatic but in the setting of secondary contributors to hypertriglyceridemia, can present with chylomicronemia syndrome and pancreatitis. Moderate elevations of triglycerides usually occur during early adulthood, and a triad of obesity, hyperglycemia, and hyperinsulinemia can be seen in affected individuals. In individuals with moderate elevation in plasma triglycerides associated with a normal cholesterol level, the possibility of familial hypertriglyceridemia should be suspected 14. Although patients with familial hypertriglyceridemia usually have moderate elevation of plasma triglycerides, whenever conditions known to elevate triglyceride, such as diabetes mellitus or alcohol or oral contraceptive consumption, concurrently occur, they may develop a profound hypertriglyceridemia and a mixed hyperlipidemia (type 5 lipoprotein pattern). An increased incidence of atherosclerosis has been reported. Hypertension and hyperuricemia have also been frequently observed. Familial hypertriglyceridemia is not associated with premature cardiovascular disease.
- Familial combined hyperlipidemia. Elevated VLDL (very-low-density lipoprotein) and or LDL (low-density lipoprotein), the phenotype can vary from isolated hypertriglyceridemia to isolated hypercholesterolemia. Regardless of phenotype, increased apo-B concentration is seen and is used to distinguish from familial hypertriglyceridemia. Associated with premature cardiovascular disease.
- Congenital deficiency of lipoprotein lipase. Congenital lipoprotein lipase deficiency is a rare autosomal recessive disorder secondary to absence or severe diminution in the activity of lipoprotein lipase. Affected individuals are homozygous for a mutation that prevents normal expression of lipoprotein lipase activity. The parents, although clinically normal, are obligate heterozygotes. This enzymatic disorder is reflected in a massive accumulation of chylomicrons in the plasma without elevation of very-low-density lipoprotein (VLDL) (type 1 lipoprotein pattern). Triglycerides may reach levels of 2000 to 10,000 mg/dl. This disorder usually appears in childhood with recurrent bouts of abdominal pain secondary to pancreatitis. Another characteristic feature of the disorder is the occurrence of eruptive xanthomas, predominantly in the buttocks and other pressure-sensitive areas of the body, attributed to the deposition of chylomicron triglycerides in histiocytes. The elevation in chylomicrons may also cause a lipemic serum, a picture of lipemia retinalis, and hepatosplenomegaly. The diagnosis is suspected by the presence of a lipemic plasma in a young patient who has fasted for 12 hours. Overnight incubation of a test tube of such plasma in a refrigeration at 4°C demonstrates a visible white layer at the top of the tube. Failure of lipoprotein lipase levels to increase after an infusion of heparin confirms the diagnosis. The occurrence of accelerated atherosclerosis is not reported in this condition.
- Apoprotein CII deficiency. Apoprotein CII deficiency is a rare autosomal recessive disorder caused by absence of apoprotein CII, a required co-factor for the activity of lipoprotein lipase. The ensuing functional deficiency in this enzyme leads to a clinical picture similar to that described above for congenital lipoprotein lipase deficiency. However, in contrast to what occurs in the latter disorder, affected individuals are diagnosed at later age and rarely present eruptive xanthomas. The usual presentation is also with recurrent abdominal pains secondary to acute pancreatitis. At times the diagnosis is made by chance discovery of a milky serum. Due to the inherent defect in this condition, in which lipoprotein lipase is not activated, both chylomicrons and very-low-density lipoprotein (VLDL) are elevated in the blood causing a type 1 or type 5 lipoprotein pattern.
- Familial dysbetalipoproteinemias (type III hyperlipoproteinemia). Familial dysbetalipoproteinemia, also called familial type 3 hyperlipoproteinemia, is a condition inherited through a single gene mechanism whose clinical presentation requires the presence of other genetic or environmental factors. Elevation of both plasma cholesterol and triglycerides occurs because of accumulation of remnant very-low-density lipoprotein (VLDL) particles in the plasma. The metabolic defect in most patients occurs in apolipoprotein E. This has three common alleles, designated E2, E3, and E4. Patients with this disorder have only apolipoprotein E2 in very-low-density lipoprotein (VLDL), which is less effective in facilitating clearance of remnants than E3 or E4. The condition occurs only in individuals who are homozygous for E2, that is, those with an E2/E2 genotype. Clinical evidence of hyperlipoproteinemia usually appears after the second decade. The characteristic clinical findings are xanthoma striata palmaris and tuberous and tuberoeruptive xanthomas over the elbows and knees. The disorder is associated with severe atherosclerosis of the coronary arteries, abdominal aorta, and peripheral arteries. The diagnosis is facilitated by encountering a broad beta band on lipoprotein electrophoresis. Confirmation can be obtained in specialized laboratories either by measuring the chemical composition of the VLDL fraction after ultracentrifugation of the plasma or by determining for the E2 allele after isoelectric focusing of remnant proteins.
Severe hypertriglyceridemia with plasma triglyceride levels >1000-1500 mg/dL can result from 3 groups of conditions 2:
- Rare mutations in the lipoprotein lipase (LPL) complex, where it is termed the familial chylomicronemia syndrome,
- The co-existence of genetic and secondary forms of hypertriglyceridemia, termed the multifactorial chylomicronemia syndrome, which is a much more common cause of severe hypertriglyceridemia, and
- Familial partial lipodystrophy.
Other causes
- Obesity and associated insulin-resistant states
- Diabetes mellitus, more frequently in type 2 diabetes mellitus
- Excessive alcohol intake
- Endocrine conditions: Hypothyroidism: predominant dyslipidemia is increase in LDL, but hypertriglyceridemia can also occur, Cushings syndrome,
- Acromegaly
- Drug-induced: thiazides, beta blockers, oral estrogens, tamoxifen, oral contraceptives (birth control pills), corticosteroids, atypical antipsychotics, isotretinoin, bile acid binding resins, anti-retroviral protease inhibitors, immunosuppressive agents: sirolimus (mTOR inhibitors)
- Pregnancy: triglyceride levels in the third trimester can increase by 200% or more from pre-pregnancy levels. In the setting of underlying primary or secondary disorders of hypertriglyceridemia, this can result in pancreatitis.
- HIV
- Renal disease: nephrotic syndrome, chronic kidney disease
- Critical illness: sepsis
- Autoimmune conditions: Juvenile dermatomyositis, systemic lupus erythematosus (SLE)
- Inherited and congenital lipodystrophies
Hypertriglyceridemia symptoms
Usually, most people with hypertriglyceridemia or high triglyceride levels, have no symptoms and the only means of discovering a high triglyceride level is with blood tests. However, in rare cases, a person may have an extremely high level of triglycerides (well above 1000 mg/dL) sustained over time and the individual may experience repeated bouts of acute pancreatitis. Some of the signs and symptoms include pain in the upper half of the stomach area that develops suddenly and then gradually gets worse, fever, nausea, vomiting, and sometimes jaundice. A person with severely high levels may also develop lesions on the skin called xanthomas. These typically appear as several small, round, solid, yellow bumps mostly on the back, chest, buttocks, shoulders and thighs.
The mechanisms leading to pancreatitis are not clear. It is suspected to be related to release of excess free fatty acids and lysolecithin from chylomicrons exceeding the binding capacity of albumin in pancreatic capillaries. The unbound free fatty acids are thought to form micellar structures with detergent properties, causing injury and ischemia leading to pancreatitis. Risk of pancreatitis markedly increases with triglycerides levels above 200 mg/dL and in most cases can be prevented by keeping triglycerides levels below 250 mg/dL to 500 mg/dL.
Mild to moderate hypertriglyceridemia is associated with an increased risk of premature cardiovascular disease (CVD), while severe hypertriglyceridemia can lead to pancreatitis and other features of the chylomicronemia syndrome, as well as an increased risk of premature cardiovascular disease. Severe hypertriglyceridemia is the third leading cause of pancreatitis in the United States. Patients can fluctuate between hypertriglyceridemic states: given an appropriate metabolic stress, mild or moderate hypertriglyceridemia can deteriorate into severe hypertriglyceridemia 15.
Hypertriglyceridemia diagnosis
The diagnosis of hypertriglyceridemia should be made based on a fasting lipid panel with recommended length of the fast of 12 hours. An important point in the setting of triglycerides higher than 400 mg/dL, the Friedewald equation which is commonly used to calculate LDL-cholesterol (bad choletserol) levels, underestimates LDL-cholesterol (bad choletserol) levels. In this setting, it is best to rely on calculation of non-HDL-cholesterol levels (total cholesterol minus HDL “good” cholesterol) or obtain direct LDL-cholesterol (bad choletserol) levels when available.
Regarding utility of advanced lipoprotein testing, measurement of LDL size or density is not recommended for prevention of cardiovascular events. Apo B and Lp(a) may have utility for assessment of cardiovascular risk in the setting of hypertriglyceridemia. Although effective therapies exist for Apo B lowering, there is no evidence-based therapy for Lp(a) lowering in the prevention of atherosclerotic cardiovascular disease events, although niacin and estrogen have been shown to lower levels of Lp(a). Lp(a) has strong familial inheritance and association with premature cardiovascular disease, thus aggressive LDL lowering is recommended when Lp(a) is high.
Hepatic steatosis, commonly associated with insulin resistance states and hypertriglyceridemia, can be associated with elevation of aminotransferases on hepatic function panel (commonly alanine aminotransferase (ALT) elevation) and should be evaluated radiologically with ultrasound as an initial step.
Hypertriglyceridemia treatment
The goal of treatment is to lower your triglycerides. Patients with very severe high triglycerides should try to lower their triglycerides below 1,000 mg/dL (11.3 mmol/L), to reduce their risk for pancreatitis.
For many people, high triglycerides are caused by another disorder, such as diabetes, obesity, renal failure, or alcoholism. With these conditions, the strategy is to treat the primary cause. When high triglycerides are not caused by another disorder, they are often seen together with high cholesterol and treatment is directed toward lowering both cholesterol and triglycerides. Lifestyle changes, such as a healthy diet and increased exercise, are usually the primary strategy for lowering levels. If these fail, lipid-lowering medications such as statins are generally recommended.
First-line therapy for acute hypertriglyceridemia pancreatitis includes intravenous (IV) fluids and fasting. Pancreatitis can be a life-threatening condition and may require admission to an intensive care unit. Identifying and treating the underlying cause is important. Also, low-dose IV insulin infusion (as low as 1 unit/hour) is effective through suppression of lipolysis and decreased hepatic triglyceride assembly. With IV insulin infusion, concomitant glucose infusion may be needed in the absence of hyperglycemia to prevent hypoglycemia. Heparin causes a release of LpL from the capillary endothelial surface and may reduce triglyceride levels rapidly, but is short-acting and so not commonly used. Plasmapheresis is an option, when available, for extremely high triglyceride levels but the cost is limiting, the risk of infection is a concern, and the effect is also short-lived. On discharge from the hospital, to decrease recurrence of pancreatitis, lifestyle change, treatment of the underlying cause, use of fibrate therapy to keep triglyceride levels below 500 mg/dL and ideally less than 150 mg/dL, has benefit 16.
Lifestyle changes
If you have mild to moderate hypertriglyceridemia, focus on cutting calories. Extra calories are converted to triglycerides and stored as fat. Reducing your calories will reduce triglycerides.
Lose weight
The first step for lowering triglycerides is to lose weight if you are overweight, exercise often, and eat a healthy diet low in saturated (bad) fat and sugar. Also, limit the amount of refined, processed grains you eat, such as white bread, rice, and pasta. Follow your doctor’s advice about limiting intake of alcohol, which
raises triglycerides in some people.
Exercise
Be active for at least 30 minutes a day. A good starting goal is at least 150 minutes a week, but if you don’t want to sweat the numbers, just move more!
Regular physical activity strengthens your heart and reduces your ‘bad’ cholesterol. Being active helps increase your ‘good’ HDL cholesterol while helping your body move the ‘bad’ non-HDL cholesterol to your liver where it will be disposed of.
You don’t have to join a gym or take up a sport, just look for chances to move more every day. Staying active is great way to keep your heart healthy.
Stop smoking
Quitting smoking can help to lower your cholesterol and improve your heart health. Smoking stops ‘good’ cholesterol doing its job of getting rid of your ‘bad’ cholesterol. Speak to your doctor about how to stop smoking as soon as you can. Not smoking will really help you avoid heart disease.
Limit how much alcohol you drink
Alcohol is high in calories and sugar and has a particularly potent effect on triglycerides. If you have severe hypertriglyceridemia, avoid drinking any alcohol.
Hypertriglyceridemia diet
Eat a healthy balanced diet
Eating more fruit, vegetables and wholegrain is better than eating foods high in saturated fat and sugar. Eating a healthy, balanced diet low in saturated fats can also reduce your level of LDL “bad” cholesterol.
Avoid or cut down on the following foods, which are high in saturated fat:
- fatty cuts of meat and meat products, such as sausages and pies
- butter, ghee and lard
- cream, soured cream, crème fraîche and ice cream
- cheese, particularly hard cheese
- cakes and biscuits
- milk chocolate
- coconut oil, coconut cream and palm oil
Choose healthier healthy monounsaturated and polyunsaturated fats such as:
- olive, rapeseed or sunflower oils and spreads
- vegetable oil spreads
- nuts
- seeds
- oily fish.
Choose more wholegrains and foods that are high in soluble fiber as this can help lower cholesterol such as:
- oats
- beans
- pulses
- lentils
- nuts
- fruits and vegetables.
Omega-3 fatty acids
Omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) lower triglycerides. However, too much omega-3 fatty acids can contribute to obesity.
These polyunsaturated (good) fats are found in oily fish such as salmon, mackerel and tuna. Omega-3 fatty acids is also found in avocados. In high doses, omega-3 fatty acids (EPA and DHA) can treat high triglycerides. For people with a high triglyceride level, at least 2 portions of oily fish a week is thought to be beneficial.
You can get high doses of omega-3 fatty acids in a fish oil supplement or by prescription. However, there’s no evidence that taking omega-3 fatty acid supplements has the same benefit.
Triglycerides-lowering medication
Besides lifestyle changes, you may also need drug treatment. There are several different types of cholesterol-lowering medication that work in different ways. Your doctor can advise you about the most suitable type of treatment, and may also prescribe medication to lower high blood pressure (hypertension) if it affects you.
For mildly or moderately high triglycerides, your doctor may prescribe one of these types of drugs:
Note: It is unclear if fibrates and niacin prevent heart attacks and strokes.
If your triglycerides are above 1,000 mg/dL, though, the first choice of medicine is a fibrate. You may need a statin, too, but experts advise against treatment with statins alone if your high triglycerides are severe or very severe. Fibrates are better than statins at lowering triglycerides. However, people with liver disease or gallbladder disease should not take fibrates.
Talk to your doctor about the risks and benefits of all these drugs. Medications do not cure the problem of high triglycerides, so you will need to take them long term. However, weight loss and other lifestyle changes can lower high trigylcerides enough to eliminate the need for medication.
Fibrates
Fibrates, which greatly lower triglycerides and sometimes raise HDL (good) cholesterol. In the U.S., these prescription drugs include gemfibrozil and fenofibrate.
Fibrates help to slow or halt the build-up of cholesterol in the arteries to reduce the risk of heart problems. They are given to people who have high cholesterol levels because they have a raised level of triglycerides in their blood.
Fibrates are first-line medications for triglyceride lowering with a decrease of 30% to 50% with concomitant increase in HDL-C. Fibrates decrease VLDL production, increase catabolism of TGRL through increased fatty acid oxidation, increased LpL synthesis, and reduced apoC-III. The effect on LDL-C can be variable in that with high triglyceride levels, LDL-C can increase but can decrease with mildly elevated hypertriglyceridemia. Dose adjustment is required with renal insufficiency, and pre-existing liver and gallbladder disease are contraindications. In the setting of concomitant statin use, fenofibrate is the preferred fibrate as gemfibrozil is associated with a higher risk of myositis. Due to protein binding, fenofibrate has an interaction with warfarin and requires close monitoring. Treatment triglyceride goal of less than 500 mg/dL is recommended to decrease the risk of recurrent pancreatitis. Concerning cardiovascular disease reduction, secondary analysis and meta-analysis of cardiovascular disease trials have shown the consistent reduction in cardiovascular disease in subgroups with baseline triglycerides below 200 and low HDL. Other potential benefits include the reduction in retinopathy and albuminuria in patients with diabetes.
Niacin (vitamin B3)
Niacin (vitamin B3) at doses of 1,000 to 3,000 mg per day, lowers triglycerides and LDL cholesterol and raises HDL cholesterol. These doses apply to immediate-release (released into the body right away) niacin, available by prescription or as a supplement.
The dose of sustained-release (released into the body over time) niacin, which is only available as a supplement, shouldn’t exceed 2,000 mg per day because of the risk of liver damage.
Niacin reduces triglyceride by about 15% to 40%, decreasing triglyceride synthesis through inhibition of liver DGAT 2, and decreasing lipolysis by inhibiting hormone-sensitive lipase. With recent clinical trials not showing any cardiovascular disease benefit when used with statins, the use of niacin has declined. Flushing is a common side effect that can be reduced by concomitant aspirin use and starting with a low dose at bedtime and slow-dose titration. Complications include hepatotoxicity, impaired glucose tolerance, and hyperuricemia. Niacin is contraindicated in patients with active peptic ulcer disease.
Omega-3 fatty acids
Omega-3 fatty acids, which are FDA-indicated for treatment of severe and very severe hypertriglyceridemia (greater than 1000 mg/dL), reduce triglycerides by 20% to 50% at 3 g to 4 g/day of eicosapentaenoic acid (EPA) plus docosahexaenoic acid (DHA). Higher baseline triglycerides are associated with greater triglyceride lowering. As triglyceride lowering is dose-related, and over the counter dietary fish oil supplements contain variable amounts of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), it is important to look at the nutrition label and instruct patients to ingest 3 gm to 4 gm per day of omega-3 fatty acids. Fishy taste and gastrointestinal discomfort can occur with such high doses of over-the-counter omega-3 fatty acid, and change to available FDA-approved prescription omega-3 fatty acid may be beneficial. Increased conversion of VLDL to LDL can lead to a rise in levels of low-density lipoprotein cholesterol (LDL-C) but has not been shown with the eicosapentaenoic acid (EPA)-only prescription product. No studies have shown cardiovascular disease benefit in patients with hypertriglyceridemia on high dose omega-3 fatty acid. Recent trials have failed to demonstrate that lowering triglyceride with omega-3 fatty acid in statin-treated patients with hypertriglyceridemia can reduce cardiovascular risk. A diet rich in omega-3 fatty acids is associated with cardiovascular health benefits.
Statins
Your doctor may add a statin to your other drug treatment. Though statins mainly lower LDL cholesterol, they also can decrease triglycerides. Some studies show that statins reduce the risk of heart attacks and strokes.
Statins block the enzyme (a type of chemical) in your liver that helps to make cholesterol. This leads to a reduction in your blood cholesterol level.
You’ll usually be started on a medication called atorvastatin. Other statins include simvastatin and rosuvastatin.
When someone has side effects from using a statin, it’s described as having an “intolerance” to it. Side effects of statins include headaches, muscle pain and stomach problems, such as indigestion, diarrhea or constipation.
Statins will only be prescribed to people who continue to be at high risk of heart disease, because they need to be taken for life. Cholesterol levels start to rise again once you stop taking them.
Statins lower triglyceride by about 10% to 30% in a dose-dependent manner and can be used as monotherapy in triglyceride levels of more than 500 m/dL when indicated to decrease cardiovascular risk.
Aspirin
In some cases, a low daily dose of aspirin may be prescribed, depending on your age (usually over 40 years old) and other risk factors.
Low-dose aspirin can help to prevent blood clots forming, particularly for someone who’s had a heart attack, has established vascular disease, or a high risk of developing cardiovascular disease.
You may also be advised to have periodic blood tests to ensure your liver is functioning well.
Hypertriglyceridemia prognosis
Patients with hyperlipidemia are at extremely high risk of developing premature coronary artery disease (coronary heart disease) (30%) 17. If the disease is inadequately managed, the prognosis is poor, especially if other cardiovascular risk factors are present. If the patient complies with lipid-lowering therapy, dietary modification, and lifestyle modification and if therapy is successful, outcome is improved significantly.
Cardiovascular disease
Hypertriglyceridemia is correlated with an increased risk of cardiovascular disease (CVD), particularly in the setting of low high-density lipoprotein (HDL) cholesterol levels and/or elevated low-density lipoprotein (LDL) cholesterol levels. When low HDL cholesterol levels are controlled for, some studies demonstrate that elevated triglycerides do not correlate with risk of cardiovascular disease. Others suggest that high triglyceride levels are an independent risk factor.
Because metabolism of the triglyceride-rich lipoproteins (chylomicrons, very low-density lipoprotein [VLDL]) and metabolism of HDL are interdependent and because triglycerides are very labile, the independent impact of hypertriglyceridemia on cardiovascular disease risk is difficult to confirm. However, randomized clinical trials using triglyceride-lowering medications have demonstrated decreased coronary events in both the primary and secondary coronary prevention populations.
An understanding of lipoprotein catabolism provides an explanation for the absence of increased risk of cardiovascular disease in patients with the most severe form of hypertriglyceridemia, type I hyperlipoproteinemia. The atherogenicity correlated with elevated triglyceride levels is thought to be secondary to increased levels of chylomicron and VLDL remnants. Remnants are smaller, richer in cholesterol, and more readily taken up by macrophages, which are converted to plaque-forming foam cells. The chylomicrons in patients with type I disease cannot be converted to remnants and, therefore, should not be atherogenic.
Using data from the National Health and Nutrition Examination Survey (2007-2014), Fan et al 18 estimated that in adult statin users with triglyceride levels in the range between greater than 150 and 500 mg/dL, the mean 10-year risk of atherosclerotic cardiovascular disease is 11.3-19.1%, while in non–statin users falling within the same parameters, the mean 10-year risk is 6.0-15.6%.
Pancreatitis
Extreme elevations of triglycerides, usually well above 1000 mg/dL, may cause acute pancreatitis and all the sequelae of that condition. A study by Pedersen et al 19 indicated that even nonfasting mild to moderate hypertriglyceridemia (177 mg/dL or above) raises the risk for acute pancreatitis; the investigators found, for example, the multivariable adjusted hazard ratio for acute pancreatitis to be 2.3 for persons with triglyceride levels of 177-265 mg/dL. However, many patients tolerate triglycerides of 4000 mg/dL or higher without developing symptoms 20.
The National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III) guidelines 21 indicate that triglycerides are so labile that a level between 500 and 1000 mg/dL may in certain settings increase dramatically and should be a target of treatment even before ensuring that the LDL goal is reached. Thus, these guidelines stipulate that if triglycerides are 500 mg/dL or greater, the initial management should be to lower the triglycerides to prevent pancreatitis. Only when the triglyceride level is below 500 should LDL-lowering be addressed.
The risk of recurrent pancreatitis secondary to hypertriglyceridemia can be avoided entirely by ensuring that levels are maintained well below 700 mg/dL. Because triglyceride levels are so labile, simply moderating levels to less than 1000 mg/dL does not decrease risk substantially, because the slightest metabolic imbalance or dietary indiscretion may push levels several hundred points higher.
Chylomicronemia syndrome
The chylomicronemia syndrome 22 is an often unrecognized and less severe condition than pancreatitis that is usually caused by triglyceride levels greater than 1000 mg/dL. Recurrent episodes of ill-defined abdominal pain that may be accompanied by nausea and vomiting are the most common presenting symptom, but chest pain and dyspnea may sometimes occur. A papular rash may be present on the trunk, thighs, and buttocks, which resolves with treatment. Amylase and lipase are minimally, if at all, elevated. Symptoms resolve when triglyceride levels decrease well below 1000 mg/dL.
References- Monogenic dyslipidemias: window on determinants of plasma lipoprotein metabolism. Hegele RA. Am J Hum Genet. 2001 Dec; 69(6):1161-77.
- Chait A, Subramanian S. Hypertriglyceridemia: Pathophysiology, Role of Genetics, Consequences, and Treatment. 2019 Apr 23. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK326743
- Karanchi H, Wyne K. Hypertriglyceridemia. [Updated 2019 Feb 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459368
- Miller M, Stone NJ, Ballantyne C, Bittner V, Criqui MH, Ginsberg HN, et. al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011;123:2292–2333. doi: 10.1161/CIR.0b013e3182160726.
- Sarwar N, Danesh J, Eiriksdottir G, Sigurdsson G, Wareham N, Bingham S, Boekholdt SM, Khaw KT, Gudnason V. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation. 2007;115:450–458. doi: 10.1161/CIRCULATIONAHA.106.637793.
- TG and HDL Working Group of the Exome Sequencing Project, National Heart, Lung, and Blood Institute. Loss-of-function mutations in APOC3, triglycerides, and coronary disease. N Engl J Med.2014;371:22–31.
- Wyler von Ballmoos MC, Haring B, Sacks FM. The risk of cardiovascular events with increased apolipoprotein CIII: a systematic review and meta-analysis. J Clin Lipidol. 2015;9:498–510. doi: 10.1016/j.jacl.2015.05.002.
- Mensink RP. Effects of Saturated Fatty Acids on Serum Lipids and Lipoproteins: A Systematic Review and Regression Analysis. Geneva, Switzerland: World Health Organization; 2016.
- Miller M, Stone NJ, Ballantyne C, Bittner V, Criqui MH, Ginsberg HN, Goldberg AC, Howard WJ, Jacobson MS, Kris-Etherton PM, Lennie TA, Levi M, Mazzone T, Pennathur S; on behalf of the American Heart Association Clinical Lipidology, Thrombosis, and Prevention Committee of the Council on Nutrition, Physical Activity, and Metabolism; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Nursing; Council on the Kidney in Cardiovascular Disease. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011;123:2292–2333. doi: 10.1161/CIR.0b013e3182160726.
- Sacks FM, Carey VJ, Anderson CA, Miller ER 3rd, Copeland T, Charleston J, Harshfield BJ, Laranjo N, McCarron P, Swain J, White K, Yee K, Appel LJ. Effects of high vs low glycemic index ofdietary carbohydrate on cardiovascular disease risk factors andinsulin sensitivity: the OmniCarb randomized clinical trial. JAMA.2014;312:2531–2541. doi: 10.1001/jama.2014.16658.
- Generoso G, Janovsky CCPS, Bittencourt MS. Triglycerides and triglyceride-rich lipoproteins in the development and progression of atherosclerosis. Curr Opin Endocrinol Diabetes Obes. 2019 Apr;26(2):109-116.
- Akinci B, Sahinoz M, Oral E. Lipodystrophy Syndromes: Presentation and Treatment. [Updated 2018 Apr 24]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Figure 6, [Generalized lack of subcutaneous fat…]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513130/figure/lipodystrophy_f_lipodystrophy_etx-obesity-new-ch15-fig6
- Schaefer EJ, Geller AS, Endress G. The biochemical and genetic diagnosis of lipid disorders. Curr. Opin. Lipidol. 2019 Apr;30(2):56-62.
- Cox RA, García-Palmieri MR. Cholesterol, Triglycerides, and Associated Lipoproteins. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 31. Available from: https://www.ncbi.nlm.nih.gov/books/NBK351
- Yuan G, Al-Shali KZ, Hegele RA. Hypertriglyceridemia: its etiology, effects and treatment. CMAJ. 2007;176(8):1113–1120. doi:10.1503/cmaj.060963 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1839776
- Lv YB, Mao C, Gao X, Yin ZX, Kraus VB, Yuan JQ, Zhang J, Luo JS, Zeng Y, Shi XM. Triglycerides Paradox Among the Oldest Old: “The Lower the Better?”. J Am Geriatr Soc. 2019 Jan 10
- Stamler J, Wentworth D, Neaton JD. Is relationship between serum cholesterol and risk of premature death from coronary heart disease continuous and graded? Findings in 356,222 primary screenees of the Multiple Risk Factor Intervention Trial (MRFIT). JAMA. 1986 Nov 28. 256(20):2823-8.
- Fan W, Philip S, Granowitz C, Toth PP, Wong ND. Hypertriglyceridemia in statin-treated US adults: the National Health and Nutrition Examination Survey. J Clin Lipidol. 2019 Jan – Feb. 13 (1):100-8.
- Pedersen SB, Langsted A, Nordestgaard BG. Nonfasting Mild-to-Moderate Hypertriglyceridemia and Risk of Acute Pancreatitis. JAMA Intern Med. 2016 Dec 1. 176 (12):1834-42.
- Athyros VG, Giouleme OI, Nikolaidis NL, Vasiliadis TV, Bouloukos VI, Kontopoulos AG, et al. Long-term follow-up of patients with acute hypertriglyceridemia-induced pancreatitis. J Clin Gastroenterol. 2002 Apr. 34(4):472-5.
- Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001 May 16. 285(19):2486-97.
- Chait A, Brunzell JD. Chylomicronemia syndrome. Adv Intern Med. 1992. 37:249-73.