What is a hysteroscopy
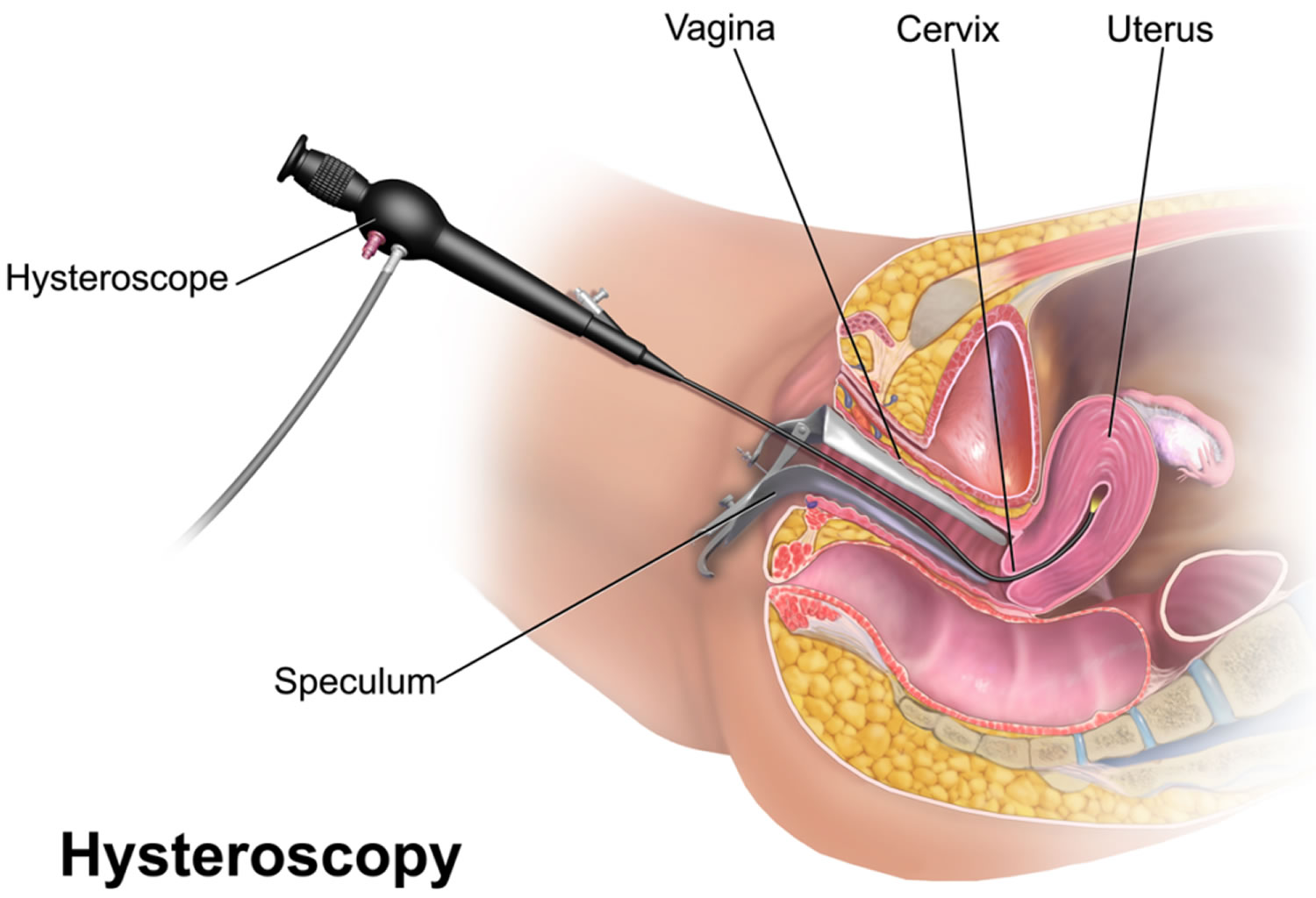
A hysteroscopy is a medical procedure (minor surgery) that is used to diagnose or treat problems on the inside of the uterus (womb). A hysteroscopy is carried out using a narrow telescope, called the hysteroscope, which is a thin, lighted telescope-like device that is inserted through your vagina into the cervix (opening of the womb) and then into the uterus. The hysteroscope is connected to a light and camera, which sends images to a monitor so that your gynecologist is able to see inside the uterus. As the hysteroscope is passed into your uterus through the vagina and cervix, no cut needs to be made in your skin.
The hysteroscopy procedure can be performed under local or general anesthetic, or without any anesthetic, and usually takes less than five to ten minutes if it’s just being done to diagnose a condition or investigate symptoms, but can last up to 30 minutes in total and is usually carried out as a day case procedure, meaning that you need not stay in hospital overnight.
Some hospitals offer an outpatient hysteroscopy service where the procedure is performed in a clinic setting without the need to have a general anesthetic. You will usually be advised to take some pain killers an hour before the procedure. Sometimes a local anesthetic or light sedation may be given.
A hysteroscopy can be used to:
- investigate symptoms or problems – such as heavy periods, unusual vaginal bleeding, postmenopausal bleeding, pelvic pain, repeated miscarriages or difficulty getting pregnant
- diagnose conditions – such as fibroids and polyps (non-cancerous growths in the womb)
- treat conditions and problems – such as removing uterine fibroids, polyps, displaced intrauterine devices (IUDs) and intrauterine adhesions (scar tissue that causes absent periods and reduced fertility)
A procedure called dilatation and curettage (D&C) used to be common to examine the womb and remove abnormal growths, but now hysteroscopies are carried out instead.
During a hysteroscopy procedure, your cervix is widened (dilated) and a telescope (hysteroscope) is passed through your vagina, across your cervix and into your womb to look at the inside of the uterus (see Figure 1). Your gynecologist will inflate your womb using gas (carbon dioxide) or a fluid (saline solution), so they can have a clear view. Your gynecologist can use instruments to perform a biopsy or remove polyps and small fibroids. A sample of the lining is often taken (biopsy) to be examined more closely. It is also possible to remove a polyp or a fibroid with a hysteroscope. This procedure does not involve any cuts or stitches to the abdomen. It takes approximately ten minutes but you can expect to be in theater and recovery for a number of hours.
Before you go home, your doctor will talk to you about the results of the hysteroscopy procedure and whether further treatment is needed. If you need to phone the hospital for your results, you will be given the necessary contact details before you leave. Information about your hysteroscopy procedure will be sent by post to your doctor.
Recovering from a hysteroscopy
Most women feel able to return to their normal activities the following day, although some women return to work the same day.
You may wish to have a few days off to rest if general anesthetic was used.
Your doctor or surgeon can advise you about any activities you need to avoid while you recover, but generally speaking:
- you can eat and drink as normal straight away – if you feel a bit sick after a general anesthetic, try eating small, light meals at first
- you can have a shower the same day or the next day
- you may experience cramping that’s similar to period pain and some spotting or bleeding for a few days – this is normal and nothing to worry about unless it’s heavy
- you should avoid having sex for a week, or until any bleeding has stopped, to reduce the risk of infection
Your doctor or nurse will discuss the findings of the procedure with you before you leave hospital.
If a small sample of tissue (biopsy) was removed from the womb, it can take several weeks to get your results. These may be sent through the post to your home address or to your doctor’s surgery.
Make sure you know how you’ll receive your results before leaving the hospital.
When to get medical advice
Contact your doctor or the hospital clinic if you experience:
- severe pain that isn’t relieved by regular painkillers
- heavy bleeding that means you have to change sanitary pads frequently
- passing bright red blood or large clots
- foul-smelling vaginal discharge
- a fever of over 38 °C (100.4 °F)
These symptoms could be a sign of a problem, such as an infection.
Is a hysteroscopy painful?
This seems to vary considerably between women. Some women feel no or only mild pain during a hysteroscopy, but for others the pain can be severe.
If you find it too uncomfortable, tell the doctor or nurse. They can stop the procedure at any time.
If you’re worried, speak to the doctor or nurse before having the procedure about what to expect and ask them about pain relief options.
Alternatives to hysteroscopy
This depends on the nature of your problem. An ultrasound scan may be performed to look at the uterus, but it does not provide as detailed an examination as hysteroscopy.
Your womb could also be examined by using a:
- pelvic ultrasound – where a small probe is inserted in the vagina and uses sound waves to produce an image of the inside of your womb
- endometrial biopsy – when a narrow tube is passed through your cervix into your womb, with suction used to remove a sample of your womb’s lining
These alternatives may be performed alongside a hysteroscopy, but do not provide as much information and can’t be used to treat problems in the same way as a hysteroscopy.
What can go wrong during a hysteroscopy procedure?
Hysteroscopy is usually a very safe procedure. You should be aware that every surgical procedure has some risk although the risks associated with hysteroscopy are low. Most women have bleeding after hysteroscopy, similar to a menstrual period, for 2 to 7 days. There might be some discomfort, similar to period pain or cramps. If you have fever, severe pain, unusual vaginal discharge or heavy bleeding, you should see a doctor.
There are some specific risks to be aware of in relation to hysteroscopy surgery:
- The hysteroscopy procedure may not be able to be completed, due to narrowing of the interior of the cervix. Further surgery may then be necessary.
- It is possible to make a small hole in the uterus (uterine perforation). In most circumstances this is of no consequence; however, this may require a laparoscopy and/or laparotomy, and/or longer stay in hospital than expected. In the event of uterine perforation, there is a risk of damage to adjacent organs, such as bowel or bladder, which may require further corrective surgery.
- Infection could be introduced into the uterus or tubes or abdominal cavity. This would require treatment with antibiotics.
- The uterus may bleed excessively. This may require blood transfusion and further surgery.
If you were to undergo a general anesthetic there are some further general risks (inherent to all operations):
- Small areas of the lungs may collapse (atelectasis), increasing your risk of chest infection. This may need antibiotics and physiotherapy.
- Clots in the legs with pain and swelling. Rarely part of this clot may break off and go to the lungs which can be fatal.
- You may suffer a heart attack or stroke because of strain on the heart. Death is an extremely rare possibility for anyone undergoing an operation
Some women are at an increased risk of complications:
- Women who are very overweight have an increased risk of wound infection, chest infection, heart and lung complications and blood clots.
- Smokers have an increased risk of wound and chest infections, heart and lung complications and blood clots.
Figure 1. Hysteroscopy
Figure 2. Uterus location
Why is a hysteroscopy performed?
One of the most common uses for hysteroscopy is to find the cause of abnormal uterine bleeding. Abnormal bleeding can mean that a woman’s menstrual periods are heavier or longer than usual or occur less often or more often than normal. Bleeding between menstrual periods also is abnormal, so is post-menopausal bleeding.
Common reasons for having a hysteroscopy include abnormal bleeding, uterine fibroids, polyps or difficulty getting pregnant. You should have a clear understanding why you are having this surgery, if not, please ask your doctor.
Hysteroscopy also is used in the following situations:
- Remove adhesions that may occur because of infection or from past surgery
- Diagnose the cause of repeated miscarriage when a woman has more than two miscarriages in a row
- Locate an intrauterine device (IUD)
- Remove an intrauterine device (IUD)
- Perform sterilization, in which the hysteroscope is used to place small implants into a woman’s fallopian tubes as a permanent form of birth control (“Essure” method)
- Remove scar tissue from the womb
- Take a tissue sample (biopsy) from the cervix or womb
- Remove scar tissue from the womb
Hysteroscopy procedure may also have other uses not listed here.
Hysteroscopic tubal ligation: This procedure is called the “Essure” method and is done in an operating or office setting using local anesthesia (numbing medicine) about 7-10 days after a woman’s period. While the women is awake, the doctor inserts a thin instrument with a camera at the end, into the vagina, which is then passed through the cervix, uterus and finally to the fallopian tube where a tiny coil is placed. Scar tissue then grows which seals the tube shut. Since this takes time to happen, another form of birth control must be used for the first 3 months.
A follow-up test called the Essure Confirmation Test is done within 3 months after the procedure. This is similar to an x-ray which allows your doctor to see that your tubes are closed off. If the tubes are tightly sealed at this point, your health care provider will likely tell you that you can stop other forms of birth control. However, you should always use condoms to prevent sexually transmitted infections (STIs). Essure can usually be done anytime except immediately after a woman gives birth.
Diagnostic Hysteroscopy
Hysteroscopy is a useful procedure to evaluate women with infertility, recurrent miscarriage, or abnormal uterine bleeding. Diagnostic hysteroscopy is used to examine the uterine cavity and is helpful in diagnosing abnormal uterine conditions such as fibroids protruding into the uterine cavity, scarring, polyps, and congenital malformations. A hysterosalpingogram (an x-ray using dye to outline the uterus and fallopian tubes), pelvic ultrasound or sonohysterogram (ultrasound with introduction of saline into the uterine cavity), or an endometrial biopsy may be performed to evaluate the uterus prior to hysteroscopy.
Diagnostic hysteroscopy is an outpatient procedure that is performed in a physician’s office or operating room. It is often performed soon after menstruation has ended because the uterine cavity is more easily evaluated. Hysteroscopy will be scheduled when you are not having your menstrual period.
Before the procedure, you may be given a medication to help you relax, or general anesthesia or local anesthesia may be used to block the pain. If you have general anesthesia, you will not be awake during the procedure.
The first step of diagnostic hysteroscopy often involves slightly stretching the canal of the cervix with a series of dilators to temporarily increase the size of the opening. You may be given medication that is inserted into the cervix, or special dilators may be used. A speculum is first inserted into the vagina. The hysteroscope (a long, thin, lighted, telescopelike instrument) is then inserted and gently moved through the cervix into your uterus. Skin incisions are not required for hysteroscopy. Carbon dioxide gas or a fluid, such as saline (salt water), will be put through the hysteroscope into your uterus to expand it. The gas or fluid helps your health care provider see the lining more clearly. The amount of fluid used is carefully checked throughout the procedure. Your health care provider can view the lining of your uterus and the openings of the fallopian tubes by looking through the hysteroscope. If a biopsy or other procedure is done, small instruments will be passed through the hysteroscope.
What should I expect during recovery?
You should be able to go home shortly after the procedure. If you had general anesthesia, you may need to wait until its effects have worn off.
It is normal to have some mild cramping or a little bloody discharge for a few days after the procedure. You may be given medication to help ease the pain. If you have a fever, chills, or heavy bleeding, call your health care provider right away.
Operative Hysteroscopy
Operative hysteroscopy can treat many of the abnormalities found during diagnostic hysteroscopy or on other imaging studies. Operative hysteroscopy is similar to diagnostic hysteroscopy except that narrow instruments are placed into the uterine cavity through a channel in the operative hysteroscope (see Figures 2). Uterine fibroids, scar tissue, and polyps can be removed from inside the uterus. Some structural abnormalities, such as a uterine septum, may be corrected through the hysteroscope.
Your physician may want you to take medications to prepare the uterus for surgery. At the conclusion of surgery, your physician may insert a balloon catheter or other device inside the uterus. Antibiotics and/or estrogen may be prescribed after some types of uterine surgery to prevent infection and stimulate healing of the endometrium. Endometrial ablation, a procedure in which the lining of the uterus is destroyed, can be used to treat some cases of excessive uterine bleeding. Ablation of the uterine lining is not performed in women who wish to become pregnant.
Figure 3. Operative Hysteroscope
How to prepare for hysteroscopy
You should ask questions, both before agreeing to have the surgery and before the surgery itself.
Before a hysteroscopy, you may be advised to:
- have tests such as blood tests to make sure that there are no health issues that might prevent you from proceeding with the procedure. This is usually done in the week before the hysteroscopy
- have a vaginal swab taken to make sure there is no likelihood of infection
- use contraception as a hysteroscopy cannot be performed if you are pregnant. You may have a pregnancy test on the day you arrive for the procedure
- stop smoking – this will reduce the risks of complications from the anesthetic
If you’re going to have fibroids removed, you may be given medicine to help shrink them beforehand.
It is important that you have all the tests, which your doctor has ordered, prior to coming to hospital.
If you are taking any blood thinning or arthritis medications they may need to be stopped prior to surgery. Please check with your preadmission nurse or pharmacist.
Before the hysteroscopy procedure
Your provider may prescribe medicine to open your cervix. This makes it easier to insert the scope. You need to take this medicine about 8 to 12 hours before your procedure.
Before any surgery tell your provider:
- About all the medicines you take. This includes vitamins, herbs, and supplements.
- If you have diabetes, heart disease, kidney disease, or other health problems.
- If you are or could be pregnant.
- If you smoke, try to stop. Ask your provider for help. Smoking can slow wound healing.
In the 2 weeks before your procedure:
- You may need to stop taking drugs that make it hard for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), naproxen (Naprosyn, Aleve), clopidogrel (Plavix), and warfarin (Coumadin). Your provider will tell you what you should or should not take.
- Ask your provider which medicines you can take on the day of your procedure.
- Tell your provider if you have a cold, flu, fever, herpes outbreak, or other sickness.
- You will be told when to arrive at the hospital. Ask if you need to arrange for someone to drive you home.
On the day of the hysteroscopy procedure
If you’re having a general anesthetic, you should fast (not have anything to eat or drink) for at least six hours before your procedure. Your doctor will be able to advise you if you should have your regular medications or not on the day of your procedure. Your appointment letter will mention whether this applies to you.
- You may be asked not to drink or eat anything 6 to 12 hours before your procedure.
- Take any approved drugs with a small sip of water.
If you’re having no anesthetic or just a local anesthetic, you can eat and drink as normal.
It’s a good idea to wear loose, comfortable clothes when you arrive for your appointment, as you’ll be asked to remove any clothes from below your waist and change into a hospital gown for the procedure.
You can bring a friend or relative with you for support, although they may not be allowed in the room during your hysteroscopy.
What happens during hysteroscopy
Although hysteroscopy is usually carried out under general anesthetic, modern hysteroscopes are very thin and allow for the procedure to be performed in an outpatient setting with a local anesthetic to numb your cervix, as it’s a relatively quick procedure and does not involve making cuts (incisions) in your skin. Taking painkillers such as ibuprofen or paracetamol about an hour beforehand can help reduce discomfort after the procedure.
- You will usually be asked to lie down and put your legs into stirrups.
- An instrument called a speculum may be inserted into your vagina to hold it open (the same instrument used for a cervical screening test), although this is not always needed
- The vagina and cervix are cleaned with an antiseptic solution
- A thin tube (hysteroscope) with a camera on the end is put into your vagina and passed through the cervix into the uterus.
- Fluid is gently pumped into the womb to make it easier for your doctor to see inside
- The camera sends pictures to a monitor so your doctor or specialist nurse can spot any abnormalities
- In some cases, a small tissue sample from the lining of the uterus may be taken for further testing. This is known as an endometrial biopsy.
- If you’re having a hysteroscopy to treat a condition such as fibroids or polyps, fine surgical instruments can be passed along the hysteroscope. These are used to cut or burn away the abnormal tissue.
If at any point you are finding the procedure too uncomfortable, tell the doctor or nurse. They can stop at any time.
Your doctor will discuss with you which type of hysteroscopy procedure will be suitable for you. Hysteroscopy is usually a quick procedure, lasting 10 to 30 minutes and does not involve any cut.
If general anesthesia is used, you will be asleep throughout the procedure and will not feel anything. If it is performed as an outpatient procedure, most women do not feel much pain but may feel some discomfort, similar to period pain.
Taking painkillers such as ibuprofen (Motrin) or paracetamol (Tylenol) about an hour beforehand can help reduce this. Occasionally, local anesthetic may be used to numb your cervix during the procedure.
Every patient is different and the anesthetist will make changes as required to suit your needs.
Hysteroscopy recovery
After a hysteroscopy, you will be monitored while any anesthetic wears off. You might need some pain relief. You can usually go home the same day, although someone should drive you home. Rarely, you may need to stay overnight.
Most women having a general anesthetic are able to go home after two to four hours, although some may stay longer. You must have a responsible adult to take you home afterwards and stay with you for 24 hours. If you are having an outpatient procedure, you will have a short stay in the department and be allowed home if you feel well. Arrange for a relative or friend to drive you home. You should be able to return to normal activities later that day or the next day. You might feel some mild, period-like pain or cramps. Some discomfort is to be expected after the procedure and you can take painkillers (such as paracetamol or ibuprofen) as instructed. If you find that the pain is hard to control, please contact your doctor or your gynecologist, or attend the Emergency Department of your local hospital if outside working hours.
For 24 hours after hysteroscopy, you should not:
- drive or operate heavy machinery
- do any heavy work or exercise.
You should use sanitary pads rather than tampons for any bleeding after the procedure. Avoid sexual intercourse until 48 hours after any bleeding has stopped.
Recovering at home
You may eat and drink as normal straight away. You may have a shower as normal but avoid baths, spas and swimming because there is a small risk of infection.
You can return to normal daily activities within 1 to 2 days.
DO NOT have sex until your provider says it is OK. It is not advisable to have sexual intercourse for at least seven days after the hysteroscopy procedure to help prevent an infection in the uterus or vagina.
You may experience:
- cramping that is similar to period pain – this should settle down in a few days and taking regular paracetamol or ibuprofen will help relieve the pain
- vaginal spotting or bleeding – this can last up to a week. This bleeding might be heavier than a normal period and can stop and start – these variations are normal. Use sanitary pads rather than tampons until your next period to reduce the risk of infection
- a watery discharge for up to several weeks.
When can I return to work?
This will depend on the type of anesthetic you had, and your occupation. Please ask your doctor or nurse before you go home. Every patient reacts differently to the anesthetic and there is no definite rule as to when you can return to work. Most women feel that they can return to normal activities, including work, the day after having a hysteroscopy. Some women return to work later the same day if they had an outpatient hysteroscopy. You may wish to have a few days off to rest, particularly if you had treatment such as fibroid removal or endometrial ablation.
When can I have sexual intercourse?
It is not advisable to have sexual intercourse for at least seven days after the hysteroscopy procedure to help prevent an infection in the uterus or vagina.
When can I use tampons again?
Do not use tampons during your next period. This will help to prevent an infection. After your next period, you can start to use tampons again.
Hysteroscopy side effects
A hysteroscopy is generally safe, but like any procedure, there is a small risk of complications, and the risk is higher if the procedure is used for carrying out a surgical treatment rather than simply to make an examination (diagnostic hysteroscopy).
Your doctor will explain the risks to you when you sign the consent for the procedure.
The uterus or cervix can be punctured by the hysteroscope, bleeding may occur, or excess fluid may build up in your system. In rare cases, hysteroscopy can cause life-threatening problems.
Some of the main risks associated with hysteroscopy include:
- Accidental damage to the uterus where a perforation (hole) is made in the wall. This is not common, but may require treatment with antibiotics in hospital, or in rare cases, another operation such as laparoscopy (keyhole surgery) or laparotomy (open surgery) to repair the uterus or organs closeby such as the bowel
- Accidental damage to the cervix – this is rare and can be easily repaired
- Infection – this can cause a vaginal discharge, fever and heavy bleeding. It is usually treated with a short course of antibiotics from your doctor
- Excessive bleeding during or after hysteroscopy surgery – this can be treated with medication or another procedure; very rarely it may be necessary to remove the womb (hysterectomy)
- Feeling faint – this affects 1 in every 200 women who have a hysteroscopy carried out without an anesthetic or just a local anesthetic
- Scarring of the lining of the womb
- Unusual fluid absorption during the procedure leading to low sodium levels
Complications of hysteroscopy occur in about 2 out of every 100 procedures. Although still uncommon, perforation of the uterus (a small hole in the uterus) is the most common complication. Although perforations usually close spontaneously, they may cause bleeding or rarely result in damage to nearby organs, which may require further surgery. Uterine cavity adhesions or infections may develop after hysteroscopy. Serious complications related to the fluids used to distend the uterus include fluid in the lungs, blood clotting, fluid overload, electrolyte imbalance, and severe allergic reactions. Severe or life-threatening complications, however, are very uncommon. Some of the complications above may prevent completion of the surgery.
Risks of any pelvic surgery may include:
- Damage to nearby organs or tissues
- Blood clots, which could travel to the lungs and be deadly (rare)
Risks of anesthesia include:
- Nausea and vomiting
- Dizziness
- Headache
- Breathing problems
- Lung infection
Risks of any surgery include:
- Infection
- Bleeding
Hysteroscopy ablation
Endometrial ablation using hysteroscopy is a surgery or procedure done to destroy (ablates) the lining of the uterus (endometrium) in order to minimize heavy or prolonged menstrual flow. The goal of endometrial ablation is to reduce menstrual flow. In some women, menstrual flow may stop completely.
No incisions are needed for endometrial ablation. Your doctor inserts slender tools through the hysteroscope into your uterus (womb).
The tools vary, depending on the method used to ablate the endometrium. They might include extreme cold, heated fluids, microwave energy or high-energy radiofrequencies.
Some types of endometrial ablation can be done in your doctor’s office. Others must be performed in an operating room. Factors such as the size and condition of your uterus will help determine which endometrial ablation method is most appropriate.
It might take a few months to see the final results, but endometrial ablation usually reduces the amount of blood lost during menstruation. Most women will have lighter periods, and some will stop having periods entirely.
Endometrial ablation isn’t a sterilization procedure, so you should continue to use contraception. Pregnancy might still be possible, but it will likely be hazardous and end in miscarriage.
Why is endometrial ablation done?
Endometrial ablation is a treatment for excessive menstrual blood loss. Your doctor might recommend endometrial ablation if you have:
- Unusually heavy periods, sometimes defined as soaking a pad or tampon every two hours or less
- Bleeding that lasts longer than eight days
- Anemia from excessive blood loss
To reduce menstrual bleeding, doctors generally start by prescribing medications or an intrauterine device (IUD). Endometrial ablation might be an option if these other treatments don’t help or if you’re not able to have other therapies.
Endometrial ablation generally isn’t recommended for postmenopausal women or women who have:
- Certain abnormalities of the uterus
- Cancer of the uterus, or an increased risk of uterine cancer
- An active pelvic infection
Endometrial ablation risks
Complications of endometrial ablation are rare and can include:
- Pain, bleeding or infection
- Heat or cold damage to nearby organs
- A puncture injury of the uterine wall from surgical instruments
Future fertility
Pregnancy can occur after endometrial ablation. However, these pregnancies might be higher risk to mother and baby. The pregnancy might end in miscarriage because the lining of the uterus has been damaged, or the pregnancy might occur in the fallopian tubes or cervix instead of the uterus (ectopic pregnancy).
Some types of sterilization procedures can be done at the time of endometrial ablation. If you are having endometrial ablation, long-lasting contraception or sterilization is recommended to prevent pregnancy.
How you prepare for endometrial ablation
In the weeks before the procedure, your doctor might:
- Perform a pregnancy check. Endometrial ablation can’t be done if you’re pregnant.
- Check for cancer. A thin tube (catheter) is inserted through your cervix to obtain a small sample of your endometrium to be tested for cancer.
- Remove an IUD. Endometrial ablation isn’t performed with an IUD in place.
- Thin your endometrium. Some types of endometrial ablation are more successful when the uterine lining is thin. Your doctor might prescribe medications or perform a dilation and curettage (D&C), a procedure in which the doctor scrapes out the extra tissue.
- Discuss anesthesia options. Some methods of endometrial ablation require general anesthesia, so you’re asleep during the procedure. Other types of endometrial ablation might be performed with conscious sedation or with numbing shots into your cervix and uterus.
During the endometrial ablation procedure
Endometrial ablation can be performed in your doctor’s office. But some types of endometrial ablation are performed in a hospital, especially if you will need general anesthesia.
The opening in your cervix needs to be widened (dilated) to allow for the passage of the instruments used in endometrial ablation. Dilation of your cervix can happen with medication or the insertion of a series of rods that gradually increase in diameter.
Endometrial ablation procedures vary by the method used to remove your endometrium. Options include:
- Electrosurgery. A slender scope is used to see inside the uterus. An instrument passed through the scope, such as a wire loop, is heated and used to carve furrows into the endometrium. Electrosurgery requires general anesthesia.
- Cryoablation. Extreme cold is used to create two or three ice balls that freeze and destroy the endometrium. Real-time ultrasound allows the doctor to track the progress of the ice balls. Each freeze cycle takes up to six minutes, and the number of cycles needed depends on the size and shape of your uterus.
- Free-flowing hot fluid. Heated saline fluid is circulated within the uterus for about 10 minutes. An advantage of this method is that it can be performed in women who have an irregular-shaped uterus from abnormal tissue growth — such as intracavity lesions or uterine fibroids — that distorts the uterus.
- Heated balloon. A balloon device is inserted through your cervix and then inflated with heated fluid. Depending on the type of balloon device, the procedure can take from two to 10 minutes.
- Microwave. A slender wand is inserted through the cervix. The wand emits microwaves, which heat the endometrial tissue. Treatment usually lasts three to five minutes.
- Radiofrequency. A special instrument unfurls a flexible ablation device inside the uterus. The device transmits radiofrequency energy that vaporizes the endometrial tissue in one to two minutes. The device is then removed from the uterus.
After the endometrial ablation procedure
After endometrial ablation, you might experience:
- Cramps. You may have menstrual-like cramps for a few days. Over-the-counter medications such as ibuprofen or acetaminophen can help relieve cramping.
- Vaginal discharge. A watery discharge, mixed with blood, may occur for a few weeks. The discharge is typically heaviest for the first few days after the procedure.
- Frequent urination. You may need to pass urine more often during the first 24 hours after endometrial ablation.
Hysteroscopy dilation and curettage
D & C is short for dilation and curettage, is a procedure to remove tissue from inside your uterus. Doctors perform dilation and curettage to diagnose and treat certain uterine conditions — such as heavy bleeding — or to clear the uterine lining after a miscarriage or abortion.
In a dilation and curettage — sometimes spelled “dilatation” and curettage — your doctor uses small instruments or a medication to open (dilate) your cervix — the lower, narrow part of your uterus. Your doctor then uses a surgical instrument called a curette to remove uterine tissue. Curettes used in a D&C can be sharp or use suction.
Your doctor may perform the D&C along with hysteroscopy procedure. During a hysteroscopy, your doctor inserts a slim instrument with a light and camera on the end into your vagina, through your cervix and up into your uterus.
Your doctor then views the lining of your uterus on a screen, noting any areas that look abnormal, making sure there aren’t any polyps and taking tissue samples as needed. During a hysteroscopy, your doctor can also remove uterine polyps and fibroid tumors.
Why is D & C done?
Dilation and curettage can diagnose or treat a uterine condition.
To diagnose a condition
Your doctor might recommend a type of D&C called endometrial sampling to diagnose a condition if:
- You have abnormal uterine bleeding
- You experience bleeding after menopause
- Your doctor discovers abnormal endometrial cells during a routine test for cervical cancer
To perform the test, your doctor collects a tissue sample from the lining of your uterus (endometrium) and sends the sample to a lab for testing.
The test can check for:
- Endometrial hyperplasia — a precancerous condition in which the uterine lining becomes too thick
- Uterine polyps
- Uterine cancer
To treat a condition
When performing a therapeutic D&C, your doctor removes the contents from inside your uterus, not just a small tissue sample. Your doctor may do this to:
- Clear out tissues that remain in the uterus after a miscarriage or abortion to prevent infection or heavy bleeding
- Remove a molar pregnancy, in which a tumor forms instead of a normal pregnancy
- Treat excessive bleeding after delivery by clearing out any placenta that remains in the uterus
- Remove cervical or uterine polyps, which are usually noncancerous (benign)
D & C risks
Dilation and curettage is usually very safe, and complications are rare. However, there are risks. These include:
- Perforation of the uterus. Perforation of the uterus occurs when a surgical instrument pokes a hole in the uterus. This happens more often in women who were recently pregnant and in women who have gone through menopause. Most perforations heal on their own. However, if a blood vessel or other organ is damaged, a second procedure may be necessary to repair it.
- Damage to the cervix. If the cervix is torn during the D&C, your doctor can apply pressure or medicine to stop the bleeding, or can close the wound with stitches (sutures).
- Scar tissue on the uterine wall. Rarely, a D&C results in development of scar tissue in the uterus, a condition known as Asherman’s syndrome. Asherman’s syndrome happens most often when the D&C is done after a miscarriage or delivery. This can lead to abnormal, absent or painful menstrual cycles, future miscarriages and infertility.
- Infection. Infection after a D&C is possible, but rare.
Contact your doctor if you experience any of the following after a D&C:
- Bleeding that’s heavy enough that you need to change pads every hour
- Fever
- Cramps lasting more than 48 hours
- Pain that gets worse instead of better
- Foul-smelling discharge from the vagina
How you prepare for a D & C
Dilation and curettage may be performed in a hospital, clinic or your doctor’s office, and it’s usually done as an outpatient procedure.
Before the D & C procedure
- Follow your doctor’s instructions on limiting food and drink.
- Arrange for someone to help you get home because you may be drowsy after the anesthesia wears off.
- Clear your schedule to allow enough time for the procedure and recovery afterward. You’ll likely spend a few hours in recovery after the procedure.
In some cases, your doctor may start the process of dilating your cervix a few hours or even a day before the procedure. This helps your cervix open gradually and is usually done when your cervix needs to be dilated more than in a standard D&C, such as during pregnancy terminations or with certain types of hysteroscopy.
To promote dilation, your doctor uses a medication called misoprostol (Cytotec) — given orally or vaginally — to soften the cervix or inserts a slender rod made of laminaria into your cervix. The laminaria gradually expands by absorbing the fluid in your cervix, causing your cervix to open.
During the D & C procedure
For dilation and curettage, you’ll receive anesthesia. The choice of anesthesia depends on the reason for the D&C and your medical history.
General anesthesia makes you unconscious and unable to feel pain. Other forms of anesthesia provide light sedation or use injections to numb only a small area (local anesthesia) or a larger region (regional anesthesia) of your body.
During the D & C procedure:
- You lie on your back on an exam table while your heels rest in supports called stirrups.
- Your doctor inserts an instrument called a speculum into your vagina, as during a Pap test, in order to see your cervix.
- Your doctor inserts a series of thicker and thicker rods into your cervix to slowly dilate your cervix until it’s adequately opened.
- Your doctor removes the dilation rods and inserts a spoon-shaped instrument with a sharp edge or a suction device and removes uterine tissue.
Because you’re either unconscious or sedated during a D&C, you shouldn’t feel any discomfort.
After the D & C procedure
You may spend a few hours in a recovery room after the D&C so that your doctor can monitor you for heavy bleeding or other complications. This also gives you time to recover from the effects of anesthesia.
If you had general anesthesia, you may become nauseated or vomit, or you might have a sore throat if a tube was placed in your windpipe to help you breathe. With general anesthesia or light sedation, you may also feel drowsy for several hours.
Normal side effects of a D&C may last a few days and include:
- Mild cramping
- Spotting or light bleeding
For discomfort from cramping, your doctor may suggest taking ibuprofen (Advil, Motrin IB, others) or another medication.
You should be able to resume your normal activities within a day or two.
Wait to put anything in your vagina until your cervix returns to normal to prevent bacteria from entering your uterus, possibly causing an infection. Ask your doctor when you can use tampons and resume sexual activity.
Your uterus must build a new lining after a D&C, so your next period may not come on time. If you had a D&C because of a miscarriage, and you want to become pregnant, talk with your doctor about when it’s safe to start trying again.