What is intracranial pressure
The intracranial pressure (ICP) represents the pressure exerted by the essentially incompressible components (brain tissue and interstitial fluids, blood and cerebrospinal fluid [CSF]) contained within the rigid confines of the skull 1. The pressure in the cranial vault is measured in millimeters of mercury (mm Hg) and normally, the intracranial pressure ranges from 1 to 20 mm Hg 2. Under a dynamic equilibrium, the normal range of cerebrospinal fluid (CSF) pressure is between 5 and 15 mmHg (7.5-20 cm H2O) 3. In children, however, there are different upper tolerated limits, defined for age groups – in general the normal interval is considered to be 3 to 7 mmHg for young children and 1.5 to 6 mmHg for term infants 3. High intracranial pressure means that both nervous system and blood vessel tissues are under pressure. If not treated, this can lead to permanent damage. In some cases, it can be life threatening.
Intracranial pressure has a normal pulsatile variation derived from the transient changes in blood volume associated with the cardiac and respiratory cycles 4. Cerebrospinal fluid (CSF) is a clear fluid found in the subarachnoid spaces and ventricles that cushions the brain and spinal cord. The cerebrospinal fluid (CSF) is secreted by the choroid plexus in the lateral ventricles, travels to the third ventricle via the foramen of Monroe (see Firgure 3). From the third ventricle, CSF reaches the fourth ventricle through the aqueduct of Sylvius. From here, it flows into the subarachnoid space via the foramina of Magendie and Luschka and is eventually reabsorbed into the dural venous sinuses by arachnoid granulation.
The Monro-Kellie hypothesis explains the pressure-volume relationship that aims to keep a dynamic equilibrium among the essential non-compressible components inside the rigid compartment of the skull 5. According to the Monro-Kellie hypothesis 6, the cranial volume is fixed, however the brain tissue, blood and cerebrospinal fluid (CSF) that are contained in it are in an equilibrium. The average intracranial volume in the adult is around 1700 mL, composed of brain tissue (~1400 mL), cerebrospinal fluid (CSF) (~150 mL), and blood (~150 mL) 5. The volume of these three components remains nearly constant in a state of dynamic equilibrium (Figure 1). Thus, a decrease in one component should be compensated by the increase in other and vice-a-versa (Figure 2). The clinical implication of the change in volume of the component is a decrease in cerebral blood flow or herniation of the brain.
It is important to note that most of the blood in the cranial cavity is contained in the low-pressure venous system, so venous compression serves as a means of displacing blood volume 7.
There are many classic brain imaging findings that the theoretical Monro-Kellie hypothesis can explain:
- venous distention in intracranial hypotension
- sulcal effacement in brain edema or expansive lesion
- brain shift with intracranial hypertension
- hydrocephalus in idiopathic intracranial hypertension
Figure 1. Monro-Kellie hypothesis on intracranial pressure
[Source 7 ]Figure 2. Monro-Kellie hypothesis on intracranial pressure
Footnote: The figures in this diagram illustrate some situations related to Monro-Kellie hypothesis. The proportions are not equivalent to real for teaching purposes.Monro-Kellie doctrine holds that total intracranial volume remains constant.
A, Physiological state with normal intracranial pressure (ICP). The major intracranial components are brain (80%), arterial and venous blood (10%), and cerebrospinal fluid (CSF) (10%). The cranium is a rigid container, the intracranial volume is constant, and the normal intracranial contents are shown with ICP within physiological range (1 to 20 mm Hg).
B, Intracranial mass with compensation (normal ICP). This patient has an intracranial mass (space-occupying lesion) of moderate size. Because intracranial volume is constant, the increasing volume caused by the mass is compensated by a decrease in the intracranial content. Venous volume decreases through egress of venous blood from the intracranial cavity into the jugular veins. CSF volume decreases because of egress of CSF through the foramen magnum into the spinal canal. The brain itself is nearly incompressible, and thus no significant change in its volume occurs; neither is there change in arterial volume. Intracranial volume is constant and there is no net rise in ICP (pressure buffering).
C, Intracranial mass with decompensation and elevated ICP. The intracranial mass is much larger, beyond the pressure-buffering capacity of venous blood and CSF; there is a net rise in ICP.
[Source 7 ]Figure 3. Cerebrospinal fluid formation, absorption and circulation around and within the brain
Figure 4. Ventricles of the brain
Changes in intracranial pressure have been shown to depend on four variables:
- CSF production rate
- intracranial compliance
- outflow resistance
- intradural sinus pressure
Physiological elevations of intracranial pressure can occur briefly (e.g. due to coughing, head-down tilt, and neck veins compression). As they are equally distributed throughout the spinal axis and last for a short period of time, they do not cause neurological damage 4.
The causes of increased intracranial pressure (ICP) can be divided based on the intracerebral components causing elevated pressures:
Increase in brain volume
Generalized swelling of the brain or cerebral edema from a variety of causes such as trauma, ischemia, hyperammonemia, uremic encephalopathy, and hyponatremia
Mass effect
- Hematoma
- Tumor
- Abscess
- Blood clots
Increase in cerebrospinal fluid
- Increased production of CSF
- Choroid plexus tumor
Decreased re-absorption of CSF
- Obstructive hydrocephalus
- Meningeal inflammation or granulomas
Increase in blood volume
- Increased cerebral blood flow during hypercarbia, aneurysms
- Venous stasis from
- Venous sinus thromboses,
- Elevated central venous pressures, e.g., heart failure
Other causes
- Idiopathic intracranial hypertension (IIH) or pseudotumor cerebri
- Skull deformities such as craniosynostosis
- Hypervitaminosis A, tetracycline use
Intracranial pressure monitoring
Intracranial pressure monitoring is performed by inserting a catheter placed inside the head with a sensing device to monitor the pressure around the brain. The monitor senses the pressure inside the skull and sends measurements to a recording device. An increase in intracranial pressure can cause a decrease in blood flow to the brain causing brain damage. High intracranial pressure can be treated by draining CSF through the catheter. It can also be treated by changing the ventilator settings for people who are on a respirator, or by giving certain medicines through a vein (intravenously).
In certain clinical situations, monitoring of intracranial pressure (ICP) is indicated. Unrecognized increased intracranial pressure leads to decreased cerebral perfusion pressure, brain ischemia, herniation and death. Elevations of intracranial pressure may precede clinical deterioration and therefore intracranial pressure monitoring may allow earlier interventions to prevent clinical deterioration.
Indications for intracranial pressure monitoring
Intracranial pressure monitoring is most often done to measure intracranial pressure. Intracranial pressure monitoring may be done when there is a severe head injury or brain/nervous system disease. Intracranial pressure monitoring also may be done after surgery to remove a tumor or fix damage to a blood vessel if the surgeon is worried about brain swelling.
- Head injury (indications: Glasgow Coma Score (GCS) <8 with an abnormal head CT (e.g., hematoma, contusion, edema) or Glasgow Coma Score (GCS) <8 and a normal CT scan but with 2or more of the following: hypotension on admission; age > 40; motor posturing)
- Postoperative Craniotomy
- Reye’s Syndrome
- Brain swelling of unknown origin
Note: intracranial pressure monitoring is NOT useful for hypoxia (i.e., ischemic stroke, drowning, strangulation or post-cardiac arrest) 8.
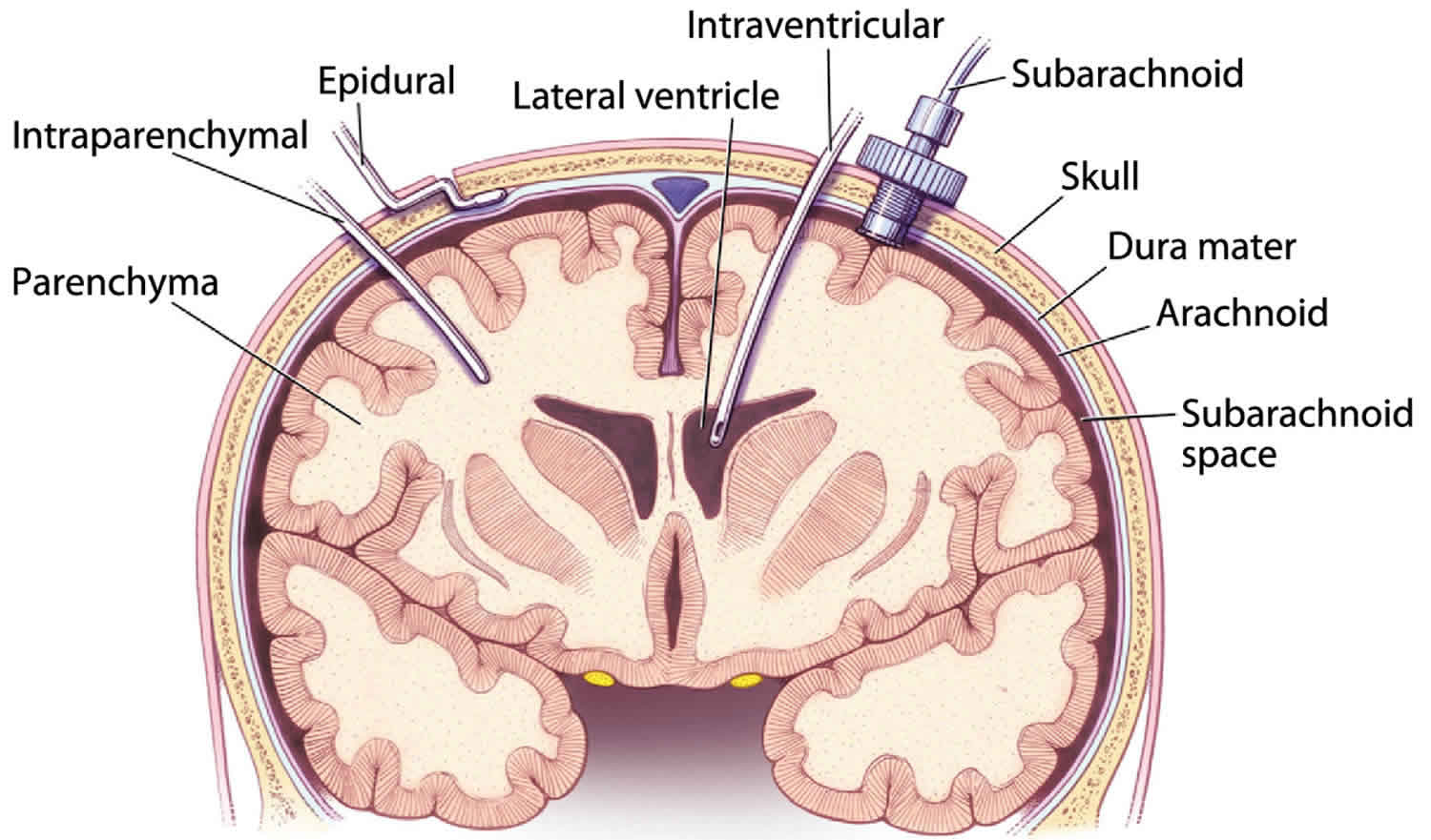
Intracranial pressure monitoring sites
- Epidural (disadvantage: imperfect correlation with the intradural pressure)
- Subdural (disadvantages: infections are serious, tubes may clog)
- Intraparenchymal (typically a fiberotic catheter; advantages: ease of insertion and replacement, true brain pressure)
- Intraventricular (advantages: very accurate intracranial pressure, can withdraw fluid to lower the pressure; disadvantages: may be difficult to insert if ventricles small or displaced)
Figure 5. Intracranial pressure monitoring
Intracranial pressure monitoring risks
Risks from the intracranial pressure monitoring procedure may include:
- Bleeding
- Brain herniation or injury from the increased pressure
- Damage to the brain tissue
- Inability to find the ventricle and place catheter
- Infection
- Risks of general anesthesia
How the intracranial pressure monitoring is done
There are 3 main ways to monitor intracranial pressure (pressure in the skull). Most of the time, this procedure is done when a person is in the hospital intensive care unit (ICU). If you are awake and aware, your health care provider will explain the procedure and the risks. You will have to sign a consent form.
Intraventricular catheter
The intraventricular catheter is the most accurate monitoring method.
To insert an intraventricular catheter, a hole is drilled through the skull. The catheter is inserted through the brain into the lateral ventricle. This area of the brain contains liquid (cerebrospinal fluid or CSF) that protects the brain and spinal cord.
The intraventricular catheter can also be used to drain fluid out through the catheter.
The catheter may be hard to get into place when the intracranial pressure is high.
Subdural screw (bolt)
This method is used if monitoring needs to be done right away. A hollow screw is inserted through a hole drilled in the skull. It is placed through the membrane that protects the brain and spinal cord (dura mater). This allows the sensor to record from inside the subdural space.
Epidural sensor
An epidural sensor is inserted between the skull and dural tissue. The epidural sensor is placed through a hole drilled in the skull. This procedure is less invasive than other methods, but it cannot remove excess CSF.
Lidocaine or another local anesthetic will be injected at the site where the cut will be made. You will most likely get a sedative to help you relax.
- First the area is shaved and cleansed with antiseptic.
- After the area is dry, a surgical cut is made. The skin is pulled back until the skull is seen.
- A drill is then used to cut through the bone.
How the intracranial pressure monitoring will feel
If the procedure is done using general anesthesia, you will be asleep and pain-free. When you wake up, you will feel the normal side effects of anesthesia. You will also have some discomfort from the cut made in your skull.
If the procedure is done under local anesthesia, you will be awake. Numbing medicine will be injected to the place where the cut is to be made. This will feel like a prick on your scalp, like a bee sting. You may feel a tugging sensation as the skin is cut and pulled back. You will hear a drill sound as it cuts through the skull. The amount of time this takes will depend on the type of drill that is used. You will also feel a tugging as the surgeon sutures the skin back together after the procedure.
Your provider may give you mild pain medicines to ease your discomfort. You will not get strong pain medicines, because your provider will want to check for signs of brain function.
What is increased intracranial pressure
Increased intracranial pressure also called intracranial hypertension, is a pathological increase in the intracranial pressure (pressure inside the skull) that can result from or cause brain injury and is a medical emergency. Increased intracranial pressure is almost always indicative of severe medical problems. Increased intracranial pressure itself can be responsible for further damage to the central nervous system by decreasing blood flow to the brain or by causing the brain to herniate (push through) the opening in the back of the skull where the spinal cord is attached. Causes of increased intracranial presure may include bleeding into the subdural space (subdural hematoma).
The harmful effects of increased intracranial pressure are primarily due to brain injury caused by cerebral ischemia. Cerebral ischemia is the result of decreased brain perfusion secondary to increased intracranial pressure. Cerebral perfusion pressure (CPP) is the pressure gradient between mean arterial pressure (MAP) and intracranial pressure (Cerebral perfusion pressure (CPP) = mean arterial pressure (MAP) – intracranial pressure). Cerebral perfusion pressure (CPP) = mean arterial pressure (MAP) – central venous pressure (CVP) if central venous pressure is higher than intracranial pressure. Cerebral perfusion pressure (CPP) targets for adults following severe traumatic brain injury is recommended at greater than 60 to 70 mm Hg, and a minimum cerebral perfusion pressure greater than 40 mm Hg is recommended for infants, with very limited data on normal cerebral perfusion pressure targets for children in between 2.
Cerebral autoregulation is the process by which cerebral blood flow varies to maintain adequate cerebral perfusion. When the mean arterial pressure (MAP) is elevated, vasoconstriction occurs to limit blood flow and maintain cerebral perfusion. However, if a patient is hypotensive, cerebral vasculature can dilate to increase blood flow and maintain cerebral perfusion pressure.
Clinical suspicion for increased intracranial pressure should be raised if a patient presents with the following signs and symptoms:
- headaches,
- vomiting, and
- altered mental status varying from drowsiness to coma.
Visual changes can range from blurred vision, double vision from cranial nerve defects, photophobia to optic disc edema and eventually optic atrophy. Infants in whom the anterior fontanelle is still open may have a bulge overlying the area.
Cushing triad is a clinical syndrome consisting of hypertension, bradycardia and irregular respiration and is a sign of impending brain herniation 2. This occurs when the intracranial pressure is too high the elevation of blood pressure is a reflex mechanism to maintain cerebral perfusion pressure. High blood pressure causes reflex bradycardia and brain stem compromise affecting respiration. Ultimately the contents of the cranium are displaced downwards due to the high intracranial pressure, causing a phenomenon known as herniation which can be potentially fatal.
The true incidence of increased intracranial pressure is unknown. The Centers for Disease Control and Prevention (CDC) estimates that in 2010, 2.5 million people sustained a traumatic brain injury (TBI) 2. Traumatic brain injury is associated with increased intracranial pressure. Intracranial pressure monitoring is recommended for all patients with severe traumatic brain injury. Studies of American-based populations have estimated that the incidence of idiopathic increased intracranial pressure (IIH) ranges from 0.9 to 1.0 per 100,000 in the general population, increasing in women that are overweight 2.
- All patients with severe traumatic brain injury (TBI) (Glasgow coma scale of 3 to 8 on initial presentation) should follow the latest guidelines on the management of severe traumatic brain injury that includes monitoring of intracranial pressure, maintenance of cerebral perfusion pressure (CPP) greater than 60 to 70 mm Hg for adults and treatment of intracranial pressure greater than 22 mm Hg.
Increased intracranial pressure can be either acute or chronic. In chronic increased intracranial pressure, the increased CSF pressure can cause swelling and damage to the optic nerve—a condition called papilledema.
Chronic increased intracranial pressure can be caused by many conditions including certain drugs such as tetracycline, a blood clot in the brain, excessive intake of vitamin A, or brain tumor. It can also occur without a detectable cause. This is idiopathic increased intracranial hypertension (IIH).
Because the symptoms of increased intracranial hypertension (IIH) can resemble those of a brain tumor, it is sometimes known by the older name pseudotumor cerebri, which means “false brain tumor.”
What causes increased intracranial pressure
Increased intracranial pressure can be due to a rise in pressure of the cerebrospinal fluid (CSF). This is the fluid that surrounds the brain and spinal cord. Increase in intracranial pressure can also be due to a rise in pressure within the brain itself. This can be caused by a mass (such as a tumor), bleeding into the brain or fluid around the brain, or swelling within the brain itself.
An increase in intracranial pressure is a serious medical problem. The pressure can damage the brain or spinal cord by pressing on important structures and by restricting blood flow into the brain.
Causes of increased intracranial pressure:
- Congenital
- Iatrogenic
- neurosurgery
- therapeutic agents
- Idiopathic intracranial hypertension (IIH) or pseudotumor cerebri
- Infection
- meningitis
- encephalitis
- abscess
- empyema (epidural/subdural)
- Trauma
- Cancer
- primary
- metastases
- cerebrovascular
- dural sinus thrombosis
- aneurysm
- arteriovenous malformation (AVM)
- intracranial hemorrhage
- extradural
- subdural
- subarachnoid
- intracerebral
- intraventricular
Common causes of increased intracranial pressure include:
- Aneurysm rupture and subarachnoid hemorrhage
- Brain tumor
- Encephalitis irritation and swelling, or inflammation, of the brain)
- Head injury
- Hydrocephalus (increased fluid around the brain)
- Hypertensive brain hemorrhage (bleeding in the brain from high blood pressure)
- Intraventricular hemorrhage (bleeding into the fluid-filled areas, or ventricles, inside the brain)
- Meningitis (infection of the membranes covering the brain and spinal cord)
- Subdural hematoma (bleeding between the covering of the brain and the surface of the brain)
- Epidural hematoma (bleeding between the inside of the skull and the outer covering of the brain)
- Seizure
- Stroke
Increased intracranial pressure prevention
Increased intracranial pressure usually cannot be prevented. If you have a persistent headache, blurred vision, changes in your level of alertness, nervous system problems, or seizures, seek medical help right away.
Increased intracranial pressure signs and symptoms
The most common symptoms of increased intracranial pressure are headaches and visual loss, including blind spots, poor peripheral (side) vision, double vision, and short temporary episodes of blindness. Many patients experience permanent vision loss. Other common symptoms include pulsatile tinnitus (ringing in the ears) and neck and shoulder pain.
The symptoms and signs of raised intracranial pressure are often non-specific and insidious in onset:
- headache
- drowsiness
- anorexia
- visual disturbances
- blurred vision: often the first manifestation noted by patients
- visual field loss: early finding
- visual acuity is usually preserved
- double vision
- “greying out of vision” or transient visual obscurations
- commonly occur with changes in posture
- papilloedema
- neck/back pain
- nausea and/or vomiting
- convulsions
- pulsatile tinnitus
- blackouts
- decreased Glasgow Coma Score (GCS)/coma
Infants symptoms and signs of raised intracranial pressure:
- Drowsiness
- Separated sutures on the skull
- Bulging of the soft spot on top of the head (bulging fontanelle)
- Vomiting
Older children and adults symptoms and signs of raised intracranial pressure:
- Behavior changes
- Decreased alertness
- Headache
- Lethargy
- Nervous system symptoms, including weakness, numbness, eye movement problems, and double vision
- Seizures
- Vomiting
Increased intracranial pressure complications
- permanent loss of vision
- permanent loss of neurological functions
- death
Increased intracranial pressure diagnosis
A health care provider will usually make the diagnosis at the patient’s bedside in an emergency room or hospital. Primary care doctors may sometimes spot early symptoms of increased intracranial pressure such as headache, seizures, or other nervous system problems. A funduscopic exam can reveal papilledema which is a tell-tale sign of raised intracranial pressure as the cerebrospinal fluid (CSF) is in continuity with the fluid around the optic nerve.
An MRI or CT scan of the head can usually determine the cause of increased intracranial pressure and confirm the diagnosis.
Intracranial pressure may be measured during a spinal tap (lumbar puncture). It can also be measured directly by using a device that is drilled through the skull or a tube (catheter) that is inserted into a hollow area in the brain called the ventricle.
Measurement of opening pressure with a lumbar puncture
In this procedure, a needle is introduced in the subarachnoid space. This can be connected to a manometer to give the pressure of the CSF prior to drainage. A measurement greater than 20 mm Hg is suggestive of raised intracranial pressure. Brain imaging should precede an lumbar puncture because lumbar puncture can cause a sudden and rapid decrease in intracranial pressure and the sudden change in volume can lead to herniation.
Radiographic features
It follows from the Monro-Kellie doctrine that as the CSF pressure inside the skull increases, the brain and blood volume have to accommodate this, resulting in the phenomenon of mass-effect, explaining the findings of raised intracranial pressure on cross-sectional brain imaging:
- effacement of the ventricles, basal cisterns and other CSF spaces
- brain herniation
- loss of grey-white matter differentiation
Increased intracranial pressure treatment
Sudden increased intracranial pressure is an emergency. The person will be treated in the intensive care unit of the hospital. The health care team will measure and monitor the person’s neurological and vital signs, including temperature, pulse, breathing rate, and blood pressure.
Management principles should be targeted toward:
- Maintenance of cerebral perfusion pressure by raising mean arterial pressure (MAP)
- Treatment of the underlying cause.
- Lowering of intracranial pressure
Treatment may include:
- Breathing support
- Draining of cerebrospinal fluid to lower pressure in the brain
- Medicines to decrease swelling
- Removal of part of the skull, especially in the first 2 days of a stroke that involves brain swelling
If a tumor, hemorrhage, or other problem has caused the increase in intracranial pressure, these problems will be treated.
Measures to lower intracranial pressure include:
- Elevate of the head of the bed to greater than 30 degrees.
- Keep the neck midline to facilitate venous drainage from the head.
- Hypercarbia (raising blood CO2) lowers serum pH and can increase cerebral blood flow contributing to rising intracranial pressure, hence hyperventilation to lower pCO2 to around 30 mm Hg can be transiently used.
- Osmotic agents can be used to create an osmotic gradient across blood thereby drawing fluid intravascularly and decreasing cerebral edema. Mannitol was the primary agent used at doses of 0.25 to 1 g/kg body weight and is thought to exert its greatest benefit by decreasing blood viscosity and to a lesser extent by decreasing blood volume. Side effects of mannitol use are eventual osmotic diuresis and dehydration as well as renal injury if serum osmolality exceeds 320 mOsm.
- Three percent hypertonic saline is also commonly used to decrease cerebral edema and can be administered as a 5 ml/kg bolus or a continuous infusion, monitoring serum sodium levels closely. It is considered relatively safe while serum sodium is < than 160mEq/dl or serum osmolality is less than 340 mOsm.
- Drugs of the carbonic anhydrase inhibitor class, such as acetazolamide, can be used to decrease the production of CSF and is used to treat idiopathic intracranial hypertension.
- Lumbar punctures, besides being diagnostic, can be used to drain CSF thus reducing the intracranial pressure. The limitation to this is raised intracranial pressure secondary to mass effect with a possible risk of herniation if the CSF pressure drops too low.
- Similar to a lumbar puncture, an External Ventricular Drain (EVD) can also be used to not only monitor intracranial pressure but also to drain CSF. An external ventricular drain (EVD) is placed directly into the lateral ventricles can be connected to a manometer to give a reading for the pressure in the ventricles.
- Optic nerve fenestrations can be performed for patients with chronic idiopathic hypertension at risk of blindness. Neurosurgical shunts such as ventriculoperitoneal or lumbar-peritoneal shunts can divert CSF to another part of the body from where it can be reabsorbed.
- A decompressive craniectomy is a neurosurgical procedure wherein a part of the skull is removed, and dura lifted, allowing the brain to sell without causing compression. It is usually considered as a last resort when all other intracranial pressure lowering measures have failed.
Increased intracranial pressure prognosis
Prognosis depends on the underlying cause and severity of presentation. Sudden increased intracranial pressure is a serious and often life-threatening condition. Prompt treatment results in better outlook.
If the increased pressure pushes on important brain structures and blood vessels, it can lead to serious, permanent problems or even death.
Benign intracranial hypertension does not increase the risk of death rate by itself; rather, the death rate is increased by morbid obesity which is a common association with benign intracranial hypertension. Visual loss is a significant morbidity in idiopathic intracranial hypertension (IIH) or pseudotumor cerebri.
References- Rohkamm R. Color Atlas of Neurology. Thieme. (2011) ISBN:1604061405.
- Pinto VL, Adeyinka A. Increased Intracranial Pressure. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482119
- Rangel-Castilla L, Rangel-Castillo L, Gopinath S et-al. Management of intracranial hypertension. Neurol Clin. 2008;26 (2): 521-41, x. doi:10.1016/j.ncl.2008.02.003
- Yasargil MG. CNS Tumors. Thieme. (1994) ISBN:0865772606.
- Hickey JV. Clinical Practice of Neurological and Neurosurgical Nursing. Lippincott Williams & Wilkins. (2011) ISBN:1451161018.
- The Monro–Kellie hypothesis. Bahram Mokri. Neurology Jun 2001, 56 (12) 1746-1748; DOI: 10.1212/WNL.56.12.1746 http://n.neurology.org/content/56/12/1746.full
- Monro-Kellie hypothesis. https://radiopaedia.org/cases/monro-kellie-hypothesis
- IMPORTANCE AND INDICATIONS FOR INTRACRANIAL PRESSURE MONITORING. http://casemed.case.edu/clerkships/neurology/NeurLrngObjectives/ICP%20monitoring.htm