What is Iodine
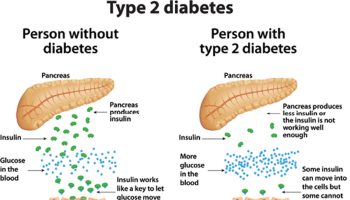
Iodine is a trace element that is naturally present in some foods, added to others, and available as a dietary supplement. Iodine is an essential component of the thyroid hormones thyroxine (T4) and triiodothyronine (T3) 1. Thyroid hormones regulate many important biochemical reactions, including protein synthesis and enzymatic activity, and are critical determinants of metabolic activity 2, 3. They are also required for proper skeletal and central nervous system development in fetuses and infants 2.
Thyroid function is primarily regulated by thyroid-stimulating hormone, also known as thyrotropin. It is secreted by the pituitary gland to control thyroid hormone production and secretion, thereby protecting the body from hypothyroidism and hyperthyroidism 2. Thyroid-stimulating hormone secretion increases thyroidal uptake of iodine and stimulates the synthesis and release of T3 and T4. In the absence of sufficient iodine, thyroid-stimulating hormone levels remain elevated, leading to goiter, an enlargement of the thyroid gland that reflects the body’s attempt to trap more iodine from the circulation and produce thyroid hormones.
Iodine may have other physiological functions in the body as well. For example, it appears to play a role in immune response and might have a beneficial effect on mammary dysplasia and fibrocystic breast disease 3.
The earth’s soils contain varying amounts of iodine, which in turn affects the iodine content of crops. In some regions of the world, iodine-deficient soils are common, increasing the risk of iodine deficiency among people who consume foods primarily from those areas. Salt iodization programs, which many countries have implemented, have dramatically reduced the prevalence of iodine deficiency worldwide 3, 4.
Iodine in food and iodized salt is present in several chemical forms including sodium and potassium salts, inorganic iodine (I2), iodate, and iodide, the reduced form of iodine 5. Iodine rarely occurs as the element, but rather as a salt; for this reason, it is referred to as iodide and not iodine. Iodide is quickly and almost completely absorbed in the stomach and duodenum. Iodate is reduced in the gastrointestinal tract and absorbed as iodide 3, 6. When iodide enters the circulation, the thyroid gland concentrates it in appropriate amounts for thyroid hormone synthesis and most of the remaining amount is excreted in the urine 3. The iodine-replete healthy adult has about 15–20 mg of iodine, 70%–80% of which is contained in the thyroid 7.

How much Iodine do you need?
The body needs iodine to make thyroid hormones. These hormones control the body’s metabolism and many other important functions. The body also needs thyroid hormones for proper bone and brain development during pregnancy and infancy. Getting enough iodine is important for everyone, especially infants and women who are pregnant.
The amount of iodine you need each day depends on your age. Average daily recommended amounts are listed below in micrograms (mcg).
Intake recommendations for iodine and other nutrients are provided in the Dietary Reference Intakes (DRIs) developed by the Food and Nutrition Board (FNB) at the Institute of Medicine of the National Academies (formerly National Academy of Sciences) 3. Dietary Reference Intakes is the general term for a set of reference values used for planning and assessing nutrient intakes of healthy people. These values, which vary by age and gender 3, include:
- Recommended Dietary Allowance (RDA): average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy individuals.
- Adequate Intake (AI): established when evidence is insufficient to develop an RDA and is set at a level assumed to ensure nutritional adequacy.
- Estimated Average Requirement (EAR): average daily level of intake estimated to meet the requirements of 50% of healthy individuals. It is usually used to assess the adequacy of nutrient intakes in populations but not individuals.
- Tolerable Upper Intake Level (UL): maximum daily intake unlikely to cause adverse health effects 3.
Table 1 lists the current Recommended Dietary Allowances (RDA – the average daily level of intake sufficient to meet the nutrient requirements of nearly all [97%–98%] healthy individuals; often used to plan nutritionally adequate diets for individuals) for iodine 8. For infants from birth to 12 months, the Food and Nutrition Board at the Institute of Medicine of the National Academies established an Adequate Intake (AI) for iodine that is equivalent to the mean intake of iodine in healthy, breastfed infants in the United States.
The World Health Organization (WHO), United Nations Children’s Fund (UNICEF), and the International Council for the Control of Iodine Deficiency Disorders (ICCIDD) recommend a slightly higher iodine intake for pregnant women of 250 mcg per day 9, 10.
Table 1. Recommended Dietary Allowances (RDAs) for Iodine
| Age | Male | Female | Pregnancy | Lactation |
| Birth to 6 months | 110 mcg* | 110 mcg* | ||
| 7–12 months | 130 mcg* | 130 mcg* | ||
| 1–3 years | 90 mcg | 90 mcg | ||
| 4–8 years | 90 mcg | 90 mcg | ||
| 9–13 years | 120 mcg | 120 mcg | ||
| 14–18 years | 150 mcg | 150 mcg | 220 mcg | 290 mcg |
| 19+ years | 150 mcg | 150 mcg | 220 mcg | 290 mcg |
Footnote: * Adequate Intake (AI)
What foods provide iodine?
Seaweed (such as kelp, nori, kombu, and wakame) is one of the best food sources of iodine, but it is highly variable in its content (Table 2). Other good sources include seafood, dairy products (partly due to the use of iodine feed supplements and iodophor sanitizing agents in the dairy industry 11, grain products, and eggs. Dairy products, especially milk, and grain products are the major contributors of iodine to the American diet 12. Iodine is also present in human breast milk 3, 6 and infant formulas.
Fruits and vegetables contain iodine, but the amount varies depending on the iodine content of the soil, fertilizer use and irrigation practices 3. Iodine concentrations in plant foods can range from as little as 10 mcg/kg to 1 mg/kg dry weight 6. This variability in turn affects the iodine content of meat and animal products because it affects the iodine content of foods that the animals consume 13. The iodine content of different seaweed species also varies greatly 14. For these reasons, the values in Table 2 are approximate.
Iodine is found naturally in some foods and is also added to salt that is labeled as “iodized”. You can get recommended amounts of iodine by eating a variety of foods, including the following:
- Fish (such as cod and tuna), seaweed, shrimp, and other seafood, which are generally rich in iodine.
- Dairy products (such as milk, yogurt, and cheese) and products made from grains (like breads and cereals), which are the major sources of iodine in American diets.
- Fruits and vegetables, which contain iodine, although the amount depends on the iodine in the soil where they grew and in any fertilizer that was used.
- Iodized salt, more than 70 countries, including the United States and Canada, have salt iodization programs. As a result, approximately 70% of households worldwide use iodized salt, ranging from almost 90% of households in North and South America to less than 50% in Europe and the Eastern Mediterranean regions 4. Processed foods, however, such as canned soups, almost never contain iodized salt.
Table 2: Selected Food Sources of Iodine
| Food | Micrograms (mcg) per serving | Percent DV* |
| Seaweed, nori, dried, 10 g | 232 | 155 |
| Bread, whole-wheat, made with iodate dough conditioner, 1 slice | 198 | 132 |
| Bread, white, enriched, made with iodate dough conditioner, 1 slice | 185 | 123 |
| Cod, baked, 3 ounces | 158 | 106 |
| Yogurt, Greek, plain, nonfat, 1 cup | 116 | 77 |
| Oysters, cooked, 3 ounces | 93 | 62 |
| Milk, nonfat, 1 cup | 85 | 57 |
| Iodized table salt, 1.5 g (approx. ¼ teaspoon) | 76 | 51 |
| Fish sticks, cooked, 3 ounces | 58 | 39 |
| Pasta, enriched, boiled in water with iodized salt, 1 cup | 36 | 24 |
| Egg, hard boiled, 1 large | 26 | 17 |
| Ice cream, chocolate, ½ cup | 21 | 14 |
| Liver, beef, cooked, 3 ounces | 14 | 9 |
| Cheese, cheddar, 1 ounce | 14 | 9 |
| Shrimp, cooked, 3 ounces | 13 | 9 |
| Tuna, canned in water, drained, 3 ounces | 7 | 5 |
| Soy beverage, 1 cup | 7 | 5 |
| Fruit cocktail in light syrup, canned, ½ cup | 6 | 4 |
| Beef, chuck, roasted, 3 ounces | 3 | 2 |
| Chicken breast, roasted, 3 ounces | 2 | 1 |
| Almond beverage, 1 cup | 2 | 1 |
| Apple juice, 1 cup | 1 | 1 |
| Bread, whole-wheat, made without iodate dough conditioner, 1 slice | 1 | 1 |
| Bread, white, enriched, made without iodate dough conditioner, 1 slice | 1 | 1 |
| Raisin bran cereal, 1 cup | 1 | 1 |
| Rice, brown, cooked, ½ cup | 1 | 1 |
| Corn, canned, ½ cup | 1 | 1 |
| Sea salt, non-iodized, 1.5 g (approx. ¼ teaspoon) | <1 | <1 |
| Broccoli, boiled, ½ cup | 0 | 0 |
| Banana, 1 medium | 0 | 0 |
| Lima beans, mature, boiled, ½ cup | 0 | 0 |
| Green peas, frozen, boiled, ½ cup | 0 | 0 |
| Pasta, enriched, boiled in water without iodized salt, 1 cup | 0 | 0 |
Footnotes: *DV = Daily Value. DVs were developed by the U.S. Food and Drug Administration (FDA) to help consumers compare the nutrient contents of products within the context of a total diet. The DV for iodine is 150 mcg for adults and children aged 4 and older. However, the FDA does not require food labels to list iodine content unless a food has been fortified with this nutrient. Foods providing 20% or more of the DV are considered to be high sources of a nutrient.
[Source 15, 14, 16 ]What kinds of iodine dietary supplements are available?
Iodine is available in dietary supplements, usually in the form of potassium iodide or sodium iodide. Dietary supplements of iodine-containing kelp (a seaweed) are also available.
Many multivitamin/mineral supplements contain iodine in the forms of potassium iodide or sodium iodide. A small study found that potassium iodide is almost completely (96.4%) absorbed in humans 17.
Iodine supplements have the potential to interact with several types of medications. A few examples are provided below. Individuals taking these medications on a regular basis should discuss their iodine intakes with their healthcare providers.
- Anti-thyroid medications. Anti-thyroid medications, such as methimazole (Tapazole®), are used to treat hyperthyroidism. Taking high doses of iodine with anti-thyroid medications can have an additive effect and could cause hypothyroidism 18.
- Angiotensin-converting enzyme (ACE) inhibitors. ACE inhibitors, such as benazepril (Lotensin®), lisinopril (Prinivil® and Zestril®), and fosinopril (Monopril®), are used primarily to treat high blood pressure. Taking potassium iodide with ACE inhibitors can increase the risk of hyperkalemia (elevated blood levels of potassium) 18.
- Potassium-sparing diuretics. Taking potassium iodide with potassium-sparing diuretics, such as spironolactone (Aldactone®) and amiloride (Midamor®), can increase the risk of hyperkalemia 18.
Are you getting enough iodine?
Most people in the United States get enough iodine from foods and beverages. However, certain groups of people are more likely than others to have trouble getting enough iodine:
- People who do not use iodized salt. Adding iodine to salt is the most widely used strategy to control iodine deficiency. Currently, about 70% of households worldwide use iodized salt.
- Pregnant women. Women who are pregnant need about 50% more iodine than other women to provide enough iodine for their baby. Surveys show that many pregnant women in the United States may not get quite enough iodine, although experts do not know whether this affects their babies.
- People living in regions with iodine-deficient soils who eat mostly local foods. These soils produce crops that have low iodine levels. Among the regions with the most iodine-poor soil are mountainous areas, such as the Himalayas, the Alps, and the Andes regions, as well as river valleys in South and Southeast Asia.
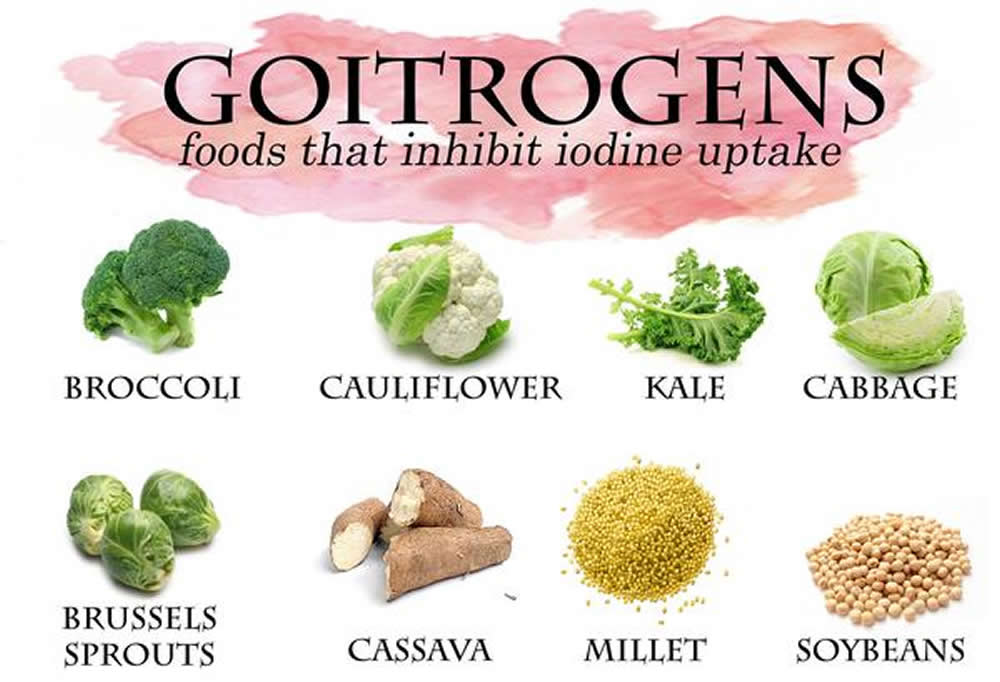
- People who get marginal amounts of iodine and who also eat foods containing goitrogens. Goitrogens are substances that interfere with the way the body uses iodine. They are present in some plant foods including soy, and cruciferous vegetables such as cabbage, broccoli, cauliflower and Brussels sprouts. For most people in the United States who get adequate amounts of iodine, eating reasonable amounts of foods containing goitrogens is not a concern.
What happens if you don’t get enough iodine?
Iodine deficiency is uncommon in the United States and Canada. People who don’t get enough iodine cannot make sufficient amounts of thyroid hormone. This can cause many problems. In pregnant women, severe iodine deficiency can permanently harm the fetus by causing stunted growth, mental retardation, and delayed sexual development. Less severe iodine deficiency can cause lower-than-average IQ in infants and children and decrease adults’ ability to work and think clearly. Goiter, an enlarged thyroid gland, is often the first visible sign of iodine deficiency.
Groups at risk of Iodine Inadequacy
Historically, iodine deficiency was endemic in mountainous regions of the United States and Mexico, and in the so called “goiter belt” around the Great Lakes. Thanks to a more national food supply, iodized salt and other factors, iodine deficiency is now uncommon in North America. Worldwide however, iodine deficiency remains a public health problem in 47 countries 7 and about 2.2 billion people (38% of the world’s population) live in areas with iodine deficiency 19. International efforts since the early 1990s have dramatically reduced the incidence of iodine deficiency, but some groups of people are still at risk of inadequate iodine intake.
People living in regions with iodine-deficient soils
Iodine-deficient soils produce crops that have low iodine levels. Mountainous areas, such as the Himalayas, Alps, and Andes regions, and river valleys prone to flooding, especially in South and Southeast Asia, are among the most iodine-deficient regions in the world 6. Populations in these areas are at risk of iodine deficiency unless they have access to iodized salt or foods produced outside the iodine-deficient area.
People with marginal iodine status who eat foods containing goitrogens
Consumption of foods that contain goitrogens, substances that interfere with the uptake of iodine in the thyroid, can exacerbate iodine deficiency 3. Foods high in goitrogens include soy and cassava, cabbage, broccoli, cauliflower, and other cruciferous vegetables. Deficiencies of iron and/or vitamin A may also be goitrogenic 20. These issues are of concern primarily for people living in areas prone to iodine deficiency 7. For most people, including most of the U.S. population, who have adequate iodine intakes and eat a variety of foods, the consumption of foods containing goitrogens in reasonable amounts is not a concern.
People who do not use iodized salt
The use of iodized salt is the most widely used strategy to control iodine deficiency. Currently, about 70% of households worldwide use iodized salt, but iodine insufficiency is still prevalent in certain regions. In the European region included in WHO reports, 52% of the population has insufficient iodine intake and, according to UNICEF, only about 49% of households in Europe (outside of the Western European subregion) have access to iodized salt. Iodine insufficiency is also prevalent in Africa, Southeast Asia, and the Eastern Mediterranean WHO regions where rates of iodized salt use range from approximately 47% to 67% [3,36]. Worldwide, it is estimated that about 31% of school-age children do not have access to iodized salt 21.
Pregnant women
During pregnancy, the RDA for iodine increases from 150 to 220 mcg/day 3. Surveys indicate that many pregnant women in the United States, while not showing signs of overt iodine deficiency, may obtain insufficient amounts of iodine 22. The impact of this, if any, on fetal development is not known at this time.
What are some effects of iodine on health?
Due to its important role in fetal and infant development and thyroid hormone production, iodine is a critical nutrient for proper health at all life stages. This section focuses on four areas of biomedical research examining iodine’s role in health and disease: 1) fetal and infant development, 2) cognitive function during childhood, 3) fibrocystic breast disease, and 4) radiation-induced thyroid cancer.
Fetal and infant development
Iodine sufficiency during pregnancy is extremely important for proper fetal development. During early pregnancy, when fetal thyroid gland development is incomplete, the fetus depends entirely on maternal thyroxine (T4) and therefore, on maternal iodine intake 23. Production of T4 increases by approximately 50% during pregnancy 24, requiring a concomitant increase in maternal iodine intake. Sufficient iodine intake after birth is also important for proper physical and neurological growth and maturation.
Research suggests that infants are more sensitive to the effects of iodine deficiency than other age groups, as indicated by changes in their thyroid stimulating hormone (TSH) and T4 levels in response to even mild iodine deficiency 25. To accommodate increased iodine needs during pregnancy and lactation, the iodine RDA is 220 mcg/day for pregnant women and 290 mcg/day for lactating women 3. Similarly, the WHO recommends 250 mcg/day during pregnancy and lactation 26.
Although severe iodine deficiency disorders are uncommon in the United States, mild-to-moderate iodine insufficiency during pregnancy may subtly affect fetal development 27, 28, 29. In a 2009 study, researchers measured the neuropsychological status of Spanish infants whose mothers received daily supplements of 300 mcg iodine (as potassium iodide) during pregnancy and lactation 30. The mothers were moderately, but not severely, iodine deficient. Iodine supplementation resulted in significant improvements in some but not all aspects of neurodevelopment (as measured by Bayley Psychomotor Development scores) at 3–18 months of age compared with infants whose mothers did not receive iodine supplements.
Breast milk contains iodine, although concentrations vary based on maternal iodine levels. Infants who are exclusively breastfed depend on maternal iodine sufficiency for optimal development. In a study of 57 healthy lactating women from the Boston area, median breast milk iodine content was 155 mcg/L 31. Based on reported infant iodine needs and the typical volume of breast milk consumed, the authors calculated that 47% of the women may have been providing their infants breast milk containing insufficient amounts of iodine. During the weaning period, infants not receiving iodine-containing complementary foods may also be at risk of iodine deficiency, even in countries with iodized salt programs 32.
To ensure that adequate amounts of iodine are available for proper fetal and infant development, several national and international groups recommend iodine supplementation during pregnancy, lactation, and early childhood. For women living in countries with weak, sporadic, or uneven iodized salt distribution, the WHO recommends iodine supplementation for all women of childbearing age to achieve a total iodine intake of 150 mcg/day. For pregnant and lactating women in these countries, iodine intakes of 250 mcg/day from both supplements and dietary sources are recommended 4, 33. WHO recommendations for these countries also include breastfeeding through 24 months of age, combined with complementary foods fortified with iodine for children between the ages of 7–24 months 33.
In the United States and Canada, the American Thyroid Association recommends iodine supplementation (150 mcg/day) as part of a prenatal vitamin/mineral supplement for pregnant and lactating women 34. A National Research Council committee also recommends adding iodide to prenatal vitamins 2. Currently, it is estimated that only 51% of the types of prenatal multivitamins marketed in the United States contain iodine 35 and according to 2001–2006 NHANES data, 15% of lactating women and 20% of non-pregnant and pregnant women in the United States take a supplement containing iodine 36.
Results from a 2010 study however, raise some questions as to the safety of widespread iodine supplementation in areas of relative iodine sufficiency. In this cross-sectional study, pregnant women living in Spain had a significantly increased risk of hyperthyrotropinemia (TSH >3 microU/mL) if they consumed iodine supplements in doses ≥200 mcg/day compared with those who consumed doses <100 mcg/day 37. These findings suggest that taking higher doses of supplemental iodine during pregnancy could induce thyroid dysfunction in some women and underscore the need for additional research into the effects on maternal thyroid function of iodine supplementation during pregnancy.
Taken as a whole, these findings indicate that increased public awareness of iodine’s importance during pregnancy and lactation is warranted and that further research into the effects of iodine supplementation during pregnancy is needed. Many researchers, as well as the American Thyroid Association, stress the importance of continued iodine status monitoring among women of reproductive age.
Cognitive function during childhood
The effects of severe iodine deficiency on neurological development are well documented. Results from several studies suggest, for example, that chronic, moderate-to-severe iodine deficiency, particularly in children, reduces IQ by about 12–13.5 points 24. A 2004 Cochrane review concluded that iodine supplementation in children living in areas of iodine deficiency appears to both positively affect physical and mental development and decrease mortality with only minor and transient adverse effects 38.
The effects of mild iodine deficiency during childhood are more difficult to quantify. Some research suggests that mild iodine deficiency is associated with subtle neuro-developmental deficits and that iodine supplementation might improve cognitive function in mildly iodine-deficient children 23.
In a 2009 randomized, placebo-controlled study, 184 children aged 10–13 years in New Zealand with a median urinary iodine concentration of 63 mcg/L received iodine supplements (150 mcg/day) or placebo for 28 weeks 39. Iodine supplementation improved iodine status (median urinary iodine concentration after supplementation was 145 mcg/L) and significantly improved measures of perceptual reasoning and overall cognitive score compared with children taking a placebo. These findings suggest that correcting mild iodine deficiency in children could improve certain components of cognition. Additional research is required to fully understand the effects of mild iodine deficiency and iodine supplementation on cognitive function.
Fibrocystic breast disease
Fibrocystic breast disease is a benign condition characterized by lumpy, painful breasts and palpable fibrosis. It commonly affects women of reproductive age, but it can also occur during menopause, especially in women taking estrogens 40. Breast tissue has a high concentration of iodine, especially during pregnancy and lactation) 27, 41. Some research suggests that iodine supplementation might be helpful for fibrocystic breast disease, although a specific mechanism of action has not been established 42 and data are limited.
In a double-blind study, researchers randomly assigned 56 women with fibrocystic breast disease to receive daily supplements of iodine (70 to 90 mcg I2/kg body weight) or placebo for 6 months 40. At treatment completion, 65% of the women receiving iodine reported decreased pain compared with 33% of women in the placebo group. A more recent randomized, double-blind, placebo-controlled clinical trial had similar findings. In this study, researchers randomly assigned 111 women (18–50 years of age) with fibrosis and a history of breast pain to receive tablets containing 0 mcg, 1,500 mcg, 3,000 mcg, or 6,000 mcg of iodine per day 42. After 5 months of treatment, women receiving doses of 3,000 or 6,000 mcg iodine had a significant decrease in breast pain, tenderness, and nodularity compared with those receiving placebo or 1,500 mcg iodine. The researchers also reported a dose-dependent reduction in self-assessed pain. None of the doses was associated with major adverse events or changes in thyroid function test results.
Although the results of these studies are promising, more research is needed to clarify iodine’s role in fibrocystic breast disease. Moreover, the doses used in these studies (approximately 1,500–6,000 mcg per day) are several times higher than the iodine UL of 1,100 mcg for adults. Doses of this magnitude should only be used under the guidance of a physician 3.
Radiation-induced thyroid cancer
Nuclear accidents can release radioactive iodine into the environment, increasing the risk of thyroid cancer in exposed individuals, especially children 43, 44. Thyroidal uptake of radioactive iodine is higher in people with iodine deficiency than in people with iodine sufficiency. For this reason, iodine-deficient individuals have a particularly high risk of developing radiation-induced thyroid cancer when exposed to radioactive iodine.
The FDA has approved potassium iodide as a thyroid-blocking agent to reduce the risk of thyroid cancer in radiation emergencies involving the release of radioactive iodine 43. The FDA recommends that exposed people take a daily pharmacological dose (16–130 mg potassium iodide, depending on age) until the risk of significant radiation exposure ends 43, 44. Potassium iodide was widely used in Poland following the 1986 Chernobyl accident and childhood thyroid cancer rates did not increase substantially in subsequent years 45. In areas where iodide prophylaxis was not used, such as Belarus and Ukraine, where many children were mildly iodine-deficient, the incidence of thyroid cancer sharply increased among children and adolescents 43.
Can Too Much Iodine be Harmful?
Yes, if you get too much. Getting high levels of iodine can cause some of the same symptoms as iodine deficiency, including goiter (an enlarged thyroid gland). High iodine intakes can also cause thyroid gland inflammation and thyroid cancer. Getting a very large dose of iodine (several grams, for example) can cause burning of the mouth, throat, and stomach; fever; stomach pain; nausea; vomiting; diarrhea; weak pulse; and coma.
Health Risks from Excessive Iodine
High intakes of iodine can cause some of the same symptoms as iodine deficiency—including goiter, elevated TSH levels, and hypothyroidism—because excess iodine in susceptible individuals inhibits thyroid hormone synthesis and thereby increases TSH stimulation, which can produce goiter 3, 46. Iodine-induced hyperthyroidism can also result from high iodine intakes, usually when iodine is administered to treat iodine deficiency. Studies have also shown that excessive iodine intakes cause thyroiditis and thyroid papillary cancer 3, 46. Cases of acute iodine poisoning are rare and are usually caused by doses of many grams. Acute poisoning symptoms include burning of the mouth, throat, and stomach; fever; abdominal pain; nausea; vomiting; diarrhea; weak pulse; and coma 3.
Responses to excess iodine and the doses required to cause adverse effects vary 46. Some people, such as those with autoimmune thyroid disease and iodine deficiency, may experience adverse effects with iodine intakes considered safe for the general population 3, 6.
The the Food and Nutrition Board at the Institute of Medicine of the National Academies has established iodine Tolerable Upper Intake Levels (ULs – the maximum daily intake unlikely to cause adverse health effects) for food and supplement intakes (Table 3). In most people, iodine intakes from foods and supplements are unlikely to exceed the UL [2]. Long-term intakes above the UL increase the risk of adverse health effects. The Tolerable Upper Intake Levels (ULs) do not apply to individuals receiving iodine for medical treatment, but such individuals should be under the care of a physician 3.
Table 3. Tolerable Upper Intake Levels (ULs) for Iodine
| Age | Male | Female | Pregnancy | Lactation |
| Birth to 6 months | Not possible to establish* | Not possible to establish* | ||
| 7–12 months | Not possible to establish* | Not possible to establish* | ||
| 1–3 years | 200 mcg | 200 mcg | ||
| 4–8 years | 300 mcg | 300 mcg | ||
| 9–13 years | 600 mcg | 600 mcg | ||
| 14–18 years | 900 mcg | 900 mcg | 900 mcg | 900 mcg |
| 19+ years | 1,100 mcg | 1,100 mcg | 1,100 mcg | 1,100 mcg |
Footnote: * Formula and food should be the only sources of iodine for infants.
References- National Institute of Health. Iodine. https://ods.od.nih.gov/factsheets/Iodine-HealthProfessional/
- National Research Council, Committee to Assess the Health Implications of Perchlorate Ingestion. Health Implications of Perchlorate Ingestion. Washington, DC: The National Academies Press, 2005.
- Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington, DC: National Academy Press, 2001.
- World Health Organization. United Nations Children’s Fund & International Council for the Control of Iodine Deficiency Disorders. Assessment of iodine deficiency disorders and monitoring their elimination. 3rd ed. Geneva, Switzerland: WHO, 2007.
- Patrick L. Iodine: deficiency and therapeutic considerations. Altern Med Rev. 2008 Jun;13(2):116-127.
- Zimmermann MB. Iodine deficiency. Endocr Rev. 2009 Jun;30(4):376-408. https://www.ncbi.nlm.nih.gov/pubmed/19460960?dopt=Abstract
- Zimmermann MB, Jooste PL, Pandav CS. Iodine-deficiency disorders. Lancet. 2008 Oct 4;372(9645):1251-1262. https://www.ncbi.nlm.nih.gov/pubmed/18676011?dopt=Abstract
- Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington, DC: National Academy Press, 2001. https://www.nap.edu/read/10026/chapter/2
- World Health Organization. United Nations Children’s Fund & International Council for the Control of Iodine Deficiency Disorders. Assessment of iodine deficiency disorders and monitoring their elimination. 3rd ed. Geneva, Switzerland: WHO, 2007. http://apps.who.int/iris/bitstream/handle/10665/43781/9789241595827_eng.pdf;jsessionid=2E9F56538AEFD33C83934FB34BD4E8C4
- WHO Secretariat, Andersson M, de Benoist B, Delange F, Zupan J. Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the Technical Consultation. Public Health Nutr. 2007 Dec;10(12A):1606-11. doi: 10.1017/S1368980007361004. Erratum in: Public Health Nutr. 2008 Mar;11(3):327.
- Pennington JA, Young B. Iron, zinc, copper, manganese, selenium, and iodine in foods from the United States Total Diet Study. J Food Compost Anal. 1990 June;3(2):166-184.
- Murray CW, Egan SK, Kim H, Beru N, Bolger PM. US Food and Drug Administration’s Total Diet Study: dietary intake of perchlorate and iodine. J Expo Sci Environ Epidemiol. 2008 Nov;18(6):571-580. https://www.ncbi.nlm.nih.gov/pubmed/18167505?dopt=Abstract
- Pennington JAT, Schoen SA, Salmon GD, Young B, Johnson RD, Marts RW. Composition of Core Foods of the U.S. Food Supply, 1982-1991. III. Copper, Manganese, Selenium, and Iodineexternal link disclaimer. J Food Comp Anal. 1995;8(2):171-217.
- Teas J, Pino S, Critchley A, Braverman LE. Variability of iodine content in common commercially available edible seaweeds. Thyroid. 2004 Oct;14(10):836-841. https://www.ncbi.nlm.nih.gov/pubmed/15588380?dopt=Abstract
- Pennington JAT, Schoen SA, Salmon GD, Young B, Johnson RD, Marts RW. Composition of Core Foods of the U.S. Food Supply, 1982-1991. III. Copper, Manganese, Selenium, and Iodine. J Food Comp Anal. 1995;8(2):171-217.
- Dasgupta PK, Liu Y, Dyke JV. Iodine nutrition: iodine content of iodized salt in the United States. Environ Sci Technol. 2008 Feb 15;42(4):1315-1323. https://www.ncbi.nlm.nih.gov/pubmed/18351111?dopt=Abstract
- Aquaron R, Delange F, Marchal P, Lognoné V, Ninane L. Bioavailability of seaweed iodine in human beings. Cell Mol Biol (Noisy-le-grand). 2002 Jul;48(5):563-569. https://www.ncbi.nlm.nih.gov/pubmed/12146713
- Iodine. https://ods.od.nih.gov/factsheets/Iodine-HealthProfessional
- International Council for the Control of Iodine Deficiency Disorders. http://www.ign.org/
- Hess SY. The impact of common micronutrient deficiencies on iodine and thyroid metabolism: the evidence from human studies. Best Pract Res Clin Endocrinol Metab. 2010 Feb;24(1):117-132. https://www.ncbi.nlm.nih.gov/pubmed/20172476?dopt=Abstract
- Andersson M, de Benoist B, Rogers L. Epidemiology of iodine deficiency: Salt iodisation and iodine status. Best Pract Res Clin Endocrinol Metab. 2010 Feb;24(1):1-11. https://www.ncbi.nlm.nih.gov/pubmed/20172466?dopt=Abstract
- Caldwell KL, Makhmudov A, Ely E, Jones RL, Wang RY. Iodine Status of the U.S.Population, National Health and Nutrition Examination Survey, 2005-2006 and 2007-2008. Thyroid. 2011 Feb 16. https://www.ncbi.nlm.nih.gov/pubmed/21323596?dopt=Abstract
- Melse-Boonstra A, Jaiswal N. Iodine deficiency in pregnancy, infancy and childhood and its consequences for brain development. Best Pract Res Clin Endocrinol Metab. 2010 Feb;24(1):29-38. https://www.ncbi.nlm.nih.gov/pubmed/20172468?dopt=Abstract
- Zimmermann MB. Iodine deficiency in pregnancy and the effects of maternal iodine supplementation on the offspring: a review. Am J Clin Nutr. 2009 Feb;89(2):668S-672S. https://www.ncbi.nlm.nih.gov/pubmed/19088150?dopt=Abstract
- Delange F. Iodine requirements during pregnancy, lactation and the neonatal period and indicators of optimal iodine nutrition. Public Health Nutr. 2007 Dec;10(12A):1571-1580. https://www.ncbi.nlm.nih.gov/pubmed/18053281?dopt=Abstract
- World Health Organization. United Nations Children’s Fund & International Council for the Control of Iodine Deficiency Disorders. Assessment of iodine deficiency disorders and monitoring their elimination. 3rd ed. Geneva, Switzerland: WHO, 2007
- Patrick L. Iodine: deficiency and therapeutic considerations. Altern Med Rev. 2008 Jun;13(2):116-127. https://www.ncbi.nlm.nih.gov/pubmed/18590348?dopt=Abstract
- Pearce EN, Bazrafshan HR, He X, Pino S, Braverman LE. Dietary iodine in pregnant women from the Boston, Massachusetts area. Thyroid. 2004 Apr;14(4):327-328. https://www.ncbi.nlm.nih.gov/pubmed/15142369?dopt=Abstract
- Hollowell JG, Haddow JE. The prevalence of iodine deficiency in women of reproductive age in the United States of America. Public Health Nutr. 2007 Dec;10(12A):1532-1539; discussion 1540-1541. https://www.ncbi.nlm.nih.gov/pubmed/18053275?dopt=Abstract
- Velasco I, Carreira M, Santiago P, Muela JA, García-Fuentes E, Sánchez-Muñoz B, Garriga MJ, González-Fernández MC, Rodríguez A, Caballero FF, Machado A, González-Romero S, Anarte MT, Soriguer F. Effect of iodine prophylaxis during pregnancy on neurocognitive development of children during the first two years of life. J Clin Endocrinol Metab. 2009 Sep;94(9):3234-3241. https://www.ncbi.nlm.nih.gov/pubmed/19567536?dopt=Abstract
- Pearce EN, Leung AM, Blount BC, Bazrafshan HR, He X, Pino S, Valentin-Blasini L, Braverman LE. Breast milk iodine and perchlorate concentrations in lactating Boston-area women. J Clin Endocrinol Metab. 2007 May;92(5):1673-1677. https://www.ncbi.nlm.nih.gov/pubmed/17311853?dopt=Abstract
- Andersson M, Aeberli I, Wüst N, Piacenza AM, Bucher T, Henschen I, Haldimann M, Zimmermann MB. The Swiss Iodized Salt Program Provides Adequate Iodine for School Children and Pregnant Women, but Weaning Infants Not Receiving Iodine-Containing Complementary Foods as well as Their Mothers Are Iodine Deficient. J Clin Endocrinol Metab. 2010 Sep 1. https://www.ncbi.nlm.nih.gov/pubmed/20810570?dopt=Abstract
- WHO Secretariat, Andersson M, de Benoist B, Delange F, Zupan J. Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the Technical Consultation. Public Health Nutr. 2007 Dec;10(12A):1606-1611. https://www.ncbi.nlm.nih.gov/pubmed/18053287?dopt=Abstract
- Public Health Committee of the American Thyroid Association, Becker DV, Braverman LE, Delange F, Dunn JT, Franklyn JA, Hollowell JG, Lamm SH, Mitchell ML, Pearce E, Robbins J, Rovet JF. Iodine supplementation for pregnancy and lactation-United States and Canada: recommendations of the American Thyroid Association. Thyroid. 2006 Oct;16(10):949-951. https://www.ncbi.nlm.nih.gov/pubmed/17042677?dopt=Abstract
- Leung AM, Pearce EN, Braverman LE. Iodine content of prenatal multivitamins in the United States. N Engl J Med. 2009 Feb 26;360(9):939-940. https://www.ncbi.nlm.nih.gov/pubmed/19246372?dopt=Abstract
- Gregory CO, Serdula MK, Sullivan KM. Use of supplements with and without iodine in women of childbearing age in the United States. Thyroid. 2009 Sep;19(9):1019-1020. https://www.ncbi.nlm.nih.gov/pubmed/19678748?dopt=Abstract
- Rebagliato M, Murcia M, Espada M, Alvarez-Pedrerol M, Bolúmar F, Vioque J, Basterrechea M, Blarduni E, Ramón R, Guxens M, Foradada CM, Ballester F, Ibarluzea J, Sunyer J. Iodine intake and maternal thyroid function during pregnancy. Epidemiology. 2010 Jan;21(1):62-69. https://www.ncbi.nlm.nih.gov/pubmed/19940773?dopt=Abstract
- Angermayr L, Clar C. Iodine supplementation for preventing iodine deficiency disorders in children. Cochrane Database Syst Rev. 2004;(2):CD003819. https://www.ncbi.nlm.nih.gov/pubmed/15106221?dopt=Abstract
- Gordon RC, Rose MC, Skeaff SA, Gray AR, Morgan KM, Ruffman T. Iodine supplementation improves cognition in mildly iodine-deficient children. Am J Clin Nutr. 2009 Nov;90(5):1264-1271. https://www.ncbi.nlm.nih.gov/pubmed/19726593?dopt=Abstract
- Ghent WR, Eskin BA, Low DA, Hill LP. Iodine replacement in fibrocystic disease of the breast. Can J Surg. 1993 Oct;36(5):453-460. https://www.ncbi.nlm.nih.gov/pubmed/8221402?dopt=Abstract
- Azizi F, Smyth P. Breastfeeding and maternal and infant iodine nutrition. Clin Endocrinol (Oxf). 2009 May;70(5):803-809. https://www.ncbi.nlm.nih.gov/pubmed/19178515?dopt=Abstract
- Kessler JH. The effect of supraphysiologic levels of iodine on patients with cyclic mastalgia. Breast J. 2004 Jul-Aug;10(4):328-336. https://www.ncbi.nlm.nih.gov/pubmed/15239792?dopt=Abstract
- Center for Drug Evaluation and Research, Food and Drug Administration. Guidance. Potassium iodide as a thyroid blocking agent in radiation emergencies. December 2001.
- World Health Organization. Guidelines for Iodine Prophylaxis following Nuclear Accidents. 1999.
- Nauman J, Wolff J. Iodide prophylaxis in Poland after the Chernobyl reactor accident: benefits and risks. Am J Med 1993;94:524-532. https://www.ncbi.nlm.nih.gov/pubmed/8498398?dopt=Abstract
- Pennington JA. A review of iodine toxicity reports. J Am Diet Assoc. 1990 Nov;90(11):1571-1581. https://www.ncbi.nlm.nih.gov/pubmed/2229854?dopt=Abstract