Jaccoud arthropathy
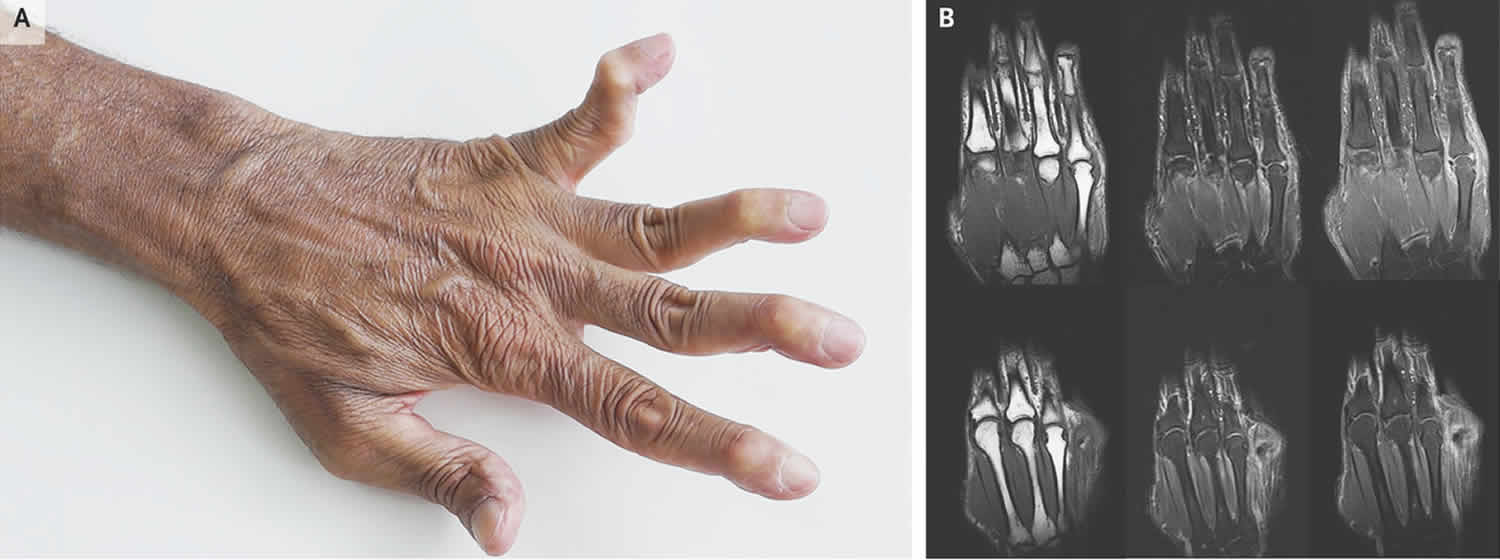
Jaccoud’s arthropathy is a chronic and non-erosive deforming arthropathy, usually affecting the hands characterized by ulnar deviation of the second to fifth fingers and subluxation of the metacarpophalangeal joints 1. Joint subluxations are voluntarily correctable by the patients. Toes may also be affected. Jaccoud’s arthropathy may be seen in association with several rheumatic and non-rheumatic disorders, such as systemic lupus erythematosus (SLE) 2, recurrent rheumatic fever 3, other connective tissue diseases 4, psoriatic arthritis 5, inflammatory bowel disease arthritis 6 and malignancy 7. It has been reported that about 5% of patients with systemic lupus erythematosus (SLE) have Jaccoud’s arthropathy 8.
Jaccoud’s arthropathy is characterized by the presence of joint deformities such as “swan neck,” ulnar deviation and “Z-thumb” resembling rheumatoid arthritis (RA) but that are passively correctable and without bone erosion on plain radiographs 9.
On imaging, ulnar deviation of the second to fifth fingers and subluxation of the metacarpophalangeal joints is seen.
Definite criteria for the diagnosis of Jaccoud’s arthropathy have not yet been established, and the pathogenesis is understood incompletely 10. However, an inflammatory process localized in the periarticular soft tissues (including the tendons and joint capsules) has been indicated as the primary cause 2.
Figure 1. Jaccoud’s arthritis
Jaccoud arthropathy causes
Jaccoud’s arthropathy was initially described as a complication of recurrent rheumatic fever 3. Jaccoud’s arthropathy may be seen in association with several rheumatic and non-rheumatic disorders, such as systemic lupus erythematosus (SLE), recurrent rheumatic fever, other connective tissue diseases 4, psoriatic arthritis 5, inflammatory bowel disease arthritis 6 and malignancy 7. It has been reported that about 5% of patients with systemic lupus erythematosus (SLE) have Jaccoud’s arthropathy 8. Jaccoud’s arthropathy has also been reported in patients without active arthritis 11. Jaccoud arthropathy is thought to be related to ligamentous laxity 12.
Jaccoud’s arthropathy pathophysiology is poorly known but involves periarticular structures such as tendons and the joint capsule.
Jaccoud arthropathy symptoms
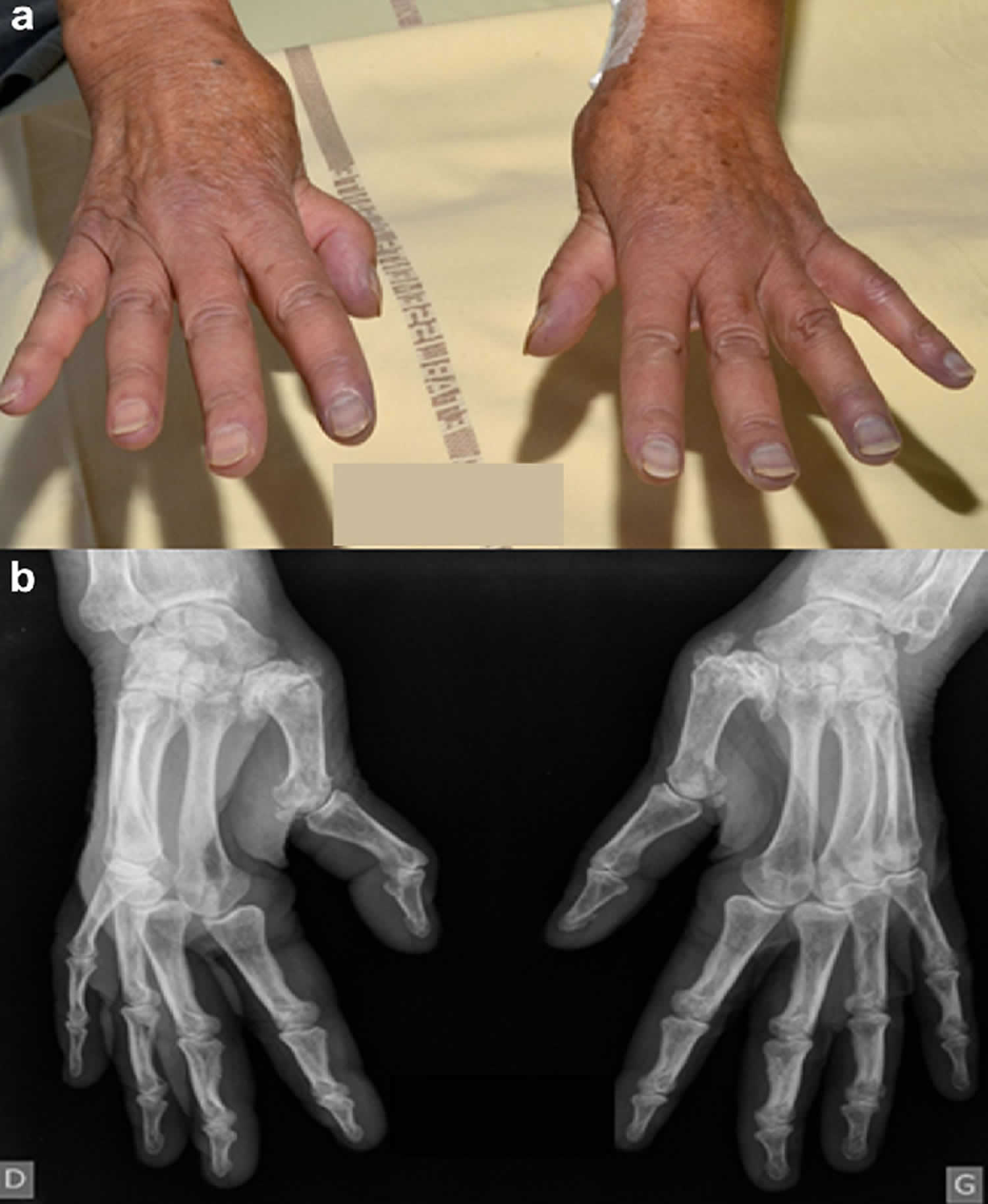
Common presentation of Jaccoud’s arthropathy is involvement of the wrist, metacarpophalangeal joints, and joints of the feet. Jaccoud arthropathy is characterized by marked ulnar subluxation and deviation at the metacarpophalangeal joints that is correctable or reducible with physical manipulation 12. Typical features include characteristic joint deviation with metacarpophalangeal subluxation, ulnar deviation, swan neck deformity of the fingers, Z deformity of both thumbs and hook formation, and alignment disorders without noticeable erosions on radiographs 13. Deformity of the long bones is generally rare.
In contrast to rheumatoid arthritis, the gradual development of deformity of the hands or feet occurs without symptoms, with little evidence of active synovitis, and with the maintenance of functional capacity 14.
Jaccoud arthropathy diagnosis
Jaccoud’s arthropathy has been described as severe joint deformity with no or minimal osseous destruction 15. Although it has been reported that bone erosions do not occur in Jaccoud’s arthropathy, recent findings from ultrasound and magnetic resonance imaging have shown otherwise 16.
Radiologically, the earliest bone change is erosion of the metacarpal head on the palmar and radial part of their circumference in an anteroposterior projection producing a hook like erosion 17. “Hook” erosions may occur on the radial palmar aspect of the metacarpal heads and can be differentiated from the marginal erosions of rheumatoid arthritis 18. Jaccoud’s arthropathy is not associated with swelling, obliteration of joint spaces, or destruction of articular surfaces 11. Erythrocyte sedimentation rate (ESR) and rheumatoid factor tests are generally negative in patients with Jaccoud’s arthropathy. Although the hands are the most common site of involvement, this condition has also been reported to involve the feet 11.
One important differential diagnosis that should be considered is Madelung’s deformity. Madelung’s deformity is characterized by ulnar and dorsal curvature of the distal radius due to deficient growth of the volar and ulnar aspect of the distal radial physis, increased inclination of the distal radial joint surface, triangulation of the corpus with proximal and volar migration, and prominent dorsal subluxation of the ulnar head 19. Madelung’s deformity usually presents in late childhood or adolescence, is more common in females, and is usually bilateral 20. A number of anatomical changes occur in Madelung deformity, which result in biomechanical alterations leading to a decreased range of movement, decreased grip strength, and often pain 20. In most patients, there is a hereditary component. In either case, presentation of
Jaccoud’s arthropathy is expected to be similar.
Jaccoud arthropathy treatment
Jaccoud’s arthropathy optimal therapeutic approach remains to be established. Presently, the therapy for Jaccoud’s arthropathy is conservative and based on the use of non-hormonal anti-inflammatory drugs, low doses of corticosteroids, methotrexate and antimalarials 21. The role of surgery through either the realignment of soft tissue around the joint–or more aggressive procedures such as arthrodesis, silastic implant and arthroplasty–needs to be proven 21. No benefit from either prednisone or a combination of prednisone and methotrexate was obtained 22.
References- [Three cases of Jaccoud’s arthropathy during systemic sclerosis]. Rev Med Interne. 2016 Oct;37(10):708-713. doi: 10.1016/j.revmed.2016.01.007. Epub 2016 Feb 8. https://doi.org/10.1016/j.revmed.2016.01.007
- van Vugt RM, Derksen RHWM, Kater J, Bijlsma JWJ. Deforming arthropathy or lupus and rhupus hands in systemic lupus erythematosus. Ann Rheum Dis 1998;57:540–4.
- Jaccoud FS. Sur une forme de rhumatisme chronique. Leçons de clinique médicale faites à l’Hôpital de la Charité. Paris: Delahaye, 1869:598–616.
- Bradley JD. Jaccoud’s arthropathy in adult dermatomyositis. Clin Exp Rheumatol 1986;3:273–6.
- Tishler M, Yaron M. Jaccoud’s arthropathy and psoriatic arthritis. Clin Exp Rheumatol 1993;11:663–4.
- Maher JM, Strosberg JM, Rowley RF, Farber M. Jaccoud’s arthropathy and inflammatory bowel disease. J Rheumatol 1992; 19:1637–9.
- Johnson JJ, Leonard‐Segal A, Nashel DJ. Jaccoud’s‐type arthropathy: an association with malignancy. J Rheumatol 1989; 16:1278–80.
- Alarcón-Segovia D, Abud-Mendoza C, Diaz-Jouanen E, Iglesias A, De los Reyes V,Hernández-Ortiz J. Deforming arthropathy of the hands in systemic lupus erythemato-sus. J Rheumatol 1988; 15:65-9.
- Severe Jaccoud’s arthropathy in systemic lupus erythematosus. Rheumatol Int. 2015 Oct;35(10):1773-7. doi: 10.1007/s00296-015-3351-9. Epub 2015 Aug 27. DOI:10.1007/s00296-015-3351-9
- Spronk PE, ter Borg EJ, Kallemberg CGM. Patients with systemic lupus erythematosus and Jaccoud’s arthropathy: a clinical subset with an increased C reactive protein response? Ann Rheum Dis 1992;51:358–61.
- Thakur R, Gupta LC, Misra M, Saran RK, Hasan M. Jaccoud’s arthropathy – diagnostic and therapeutic im-plications. Postgraduate Medical Journal Journal 1988; 64:809-811.
- Mittermayer S, Viviane M. Jaccoud’s Arthropathy. (2015) The New England journal of medicine. 373 (1): e1. doi:10.1056/NEJMicm1410743
- van Vugt RM, Derksen RHWM, Kater L, Bijlsma JW. Deforming arthropathy or lupus and rhupus hands in systemic lupus erythematosus. Ann Rheum Dis 1998; 57:540–544.
- Meyers OL, Chalmers IM. Jaccoud’s arthropathy: report of seven cases. S Afr Med J 1977; 51:753-7.
- American Journal of Roentgenology. 1973;118: 300-307. 10.2214/ajr.118.2.300 https://www.ajronline.org/doi/pdf/10.2214/ajr.118.2.300
- Ribeiro DS, Galvão V, Fernandes JL, Neto CA, D’Almeida F, Santiago M. Magnetic resonance imaging of Jaccoud’s arthropathy in systemic lupus erythematosus. Joint Bone Spine 2010; 77:241-245.
- Bywaters FGL. Relation between heart and joint disease including “rheumatoid heart disease” and chronic post-rheumatic arthritis (type Jaccoud). Brit Heart J 1950; 12:101-131.
- Shostak NA. Jaccoud’s arthropathy (abstract). Ter Arkh 1995; 67:80-83.
- Kumar A, Rai GK, Akhtar J, Phillip R, Gutch M, Arya TVS. All Madelung deformities are not endocrine. Indian J Endocrinol Metab 2013; 17:231-233.
- dos Reis FB, Katchburian MV, Faloppa F, Albertoni WM, Filho JL J. Osteotomy of the radius and ulna for the Madelung deformity. J Bone Joint Surg [Br] 1998; 80:817-24.
- Miscellaneous non-inflammatory musculoskeletal conditions. Jaccoud’s arthropathy. Best Pract Res Clin Rheumatol. 2011 Oct;25(5):715-25. doi: 10.1016/j.berh.2011.10.018. https://doi.org/10.1016/j.berh.2011.10.018
- Najm, A.A., Goff, B.L., Achille, A., Espitia, O., Durant, C., Perrin, F., & Agard, C. (2016). [Three cases of Jaccoud’s arthropathy during systemic sclerosis]. La Revue de medecine interne, 37 10, 708-713.