What is Job syndrome
Job syndrome is now called autosomal dominant hyperimmunoglobulin E (hyper-IgE) syndrome, is the name given to a very rare inherited immune deficiency characterized by severe infections of the skin and other organs. Job syndrome is characterized by abnormally high levels of an immune system protein called immunoglobulin E (IgE) in the blood. Job syndrome signs and symptoms may include recurrent infections (e.g., pneumonia, skin infections), eczema (inflammatory skin disorder ) and occasionally bone and tooth abnormalities. Affected individuals tend to have frequent bouts of pneumonia, which are caused by certain kinds of bacteria that infect the lungs and cause inflammation. These infections often result in the formation of air-filled cysts (pneumatoceles) in the lungs. People with Job syndrome also have long-term, severe skin infections. The eczema and skin infections may cause rashes, blisters, collections of pus (abscesses), open sores, and scaling of the skin. Some cases of Job syndrome are caused by mutations in the STAT3 gene. In other cases, the cause is unknown 1. The symptoms are most often present in childhood, but because Job syndrome (autosomal dominant hyperimmunoglobulin E) is so rare, it often takes years before a correct diagnosis is made. In a recent chart review, the average age of diagnosis was 11.5 years. However, the diagnosis can be made in infancy or adulthood.
Job syndrome is characterized by abnormally high levels of an immune system protein called immunoglobulin E (IgE) in the blood. IgE normally triggers an immune response against foreign invaders in the body, particularly parasitic worms, and plays a role in allergies. It is unclear why people with Job syndrome have such high levels of IgE.
Job syndrome also affects other parts of the body, including the bones and teeth. Many people with Job syndrome have skeletal abnormalities such as an unusually large range of joint movement (hyperextensibility), an abnormal curvature of the spine (scoliosis), reduced bone density (osteopenia), and a tendency for bones to fracture easily. Dental abnormalities are also common in this condition. The primary (baby) teeth do not fall out at the usual time during childhood but are retained as the adult teeth grow in. Other signs and symptoms of Job syndrome can include abnormalities of the arteries that supply blood to the heart muscle (coronary arteries), distinctive facial features, and structural abnormalities of the brain, which do not affect a person’s intelligence.
Job syndrome is rare, affecting fewer than 1 per million people.
There is no known cure for Job syndrome. Antibiotics are used to control bacterial infections, often requiring a longer course of treatment than is usually necessary. Several doctors from different specialties may need to help care for affected children.
What is the cause of Job syndrome?
The cause of Job syndrome is unknown but recent research suggests that Job syndrome is often caused by a genetic change (mutation) that takes place in the STAT3 gene on chromosome 17. How this gene abnormality causes the symptoms of the disease is not well understood. However, people with Job syndrome (autosomal dominant hyperimmunoglobulin E) have a higher-than-normal level of an antibody called IgE. IgE normally triggers an immune response against foreign invaders in the body, particularly parasitic worms, and plays a role in allergies. It is unclear why people with Job syndrome have such high levels of IgE.
Mutations in the STAT3 gene cause most cases of Job syndrome. This gene provides instructions for making a protein that plays an important role in several body systems. To carry out its roles, the STAT3 protein attaches to DNA and helps control the activity of particular genes. In the immune system, the STAT3 protein regulates genes that are involved in the maturation of immune system cells, especially T cells. These cells help control the body’s response to foreign invaders such as bacteria and fungi.
Changes in the STAT3 gene alter the structure and function of the STAT3 protein, impairing its ability to control the activity of other genes. A shortage of functional STAT3 blocks the maturation of T cells (specifically a subset known as Th17 cells) and other immune cells. The resulting immune system abnormalities make people with Job syndrome highly susceptible to infections, particularly bacterial and fungal infections of the lungs and skin. The STAT3 protein is also involved in the formation of cells that build and break down bone tissue, which could help explain why STAT3 gene mutations lead to the skeletal and dental abnormalities characteristic of this condition. It is unclear how STAT3 gene mutations lead to increased IgE levels.
When Job syndrome is not caused by STAT3 gene mutations, the genetic cause of the condition is unknown.
Job syndrome inheritance pattern
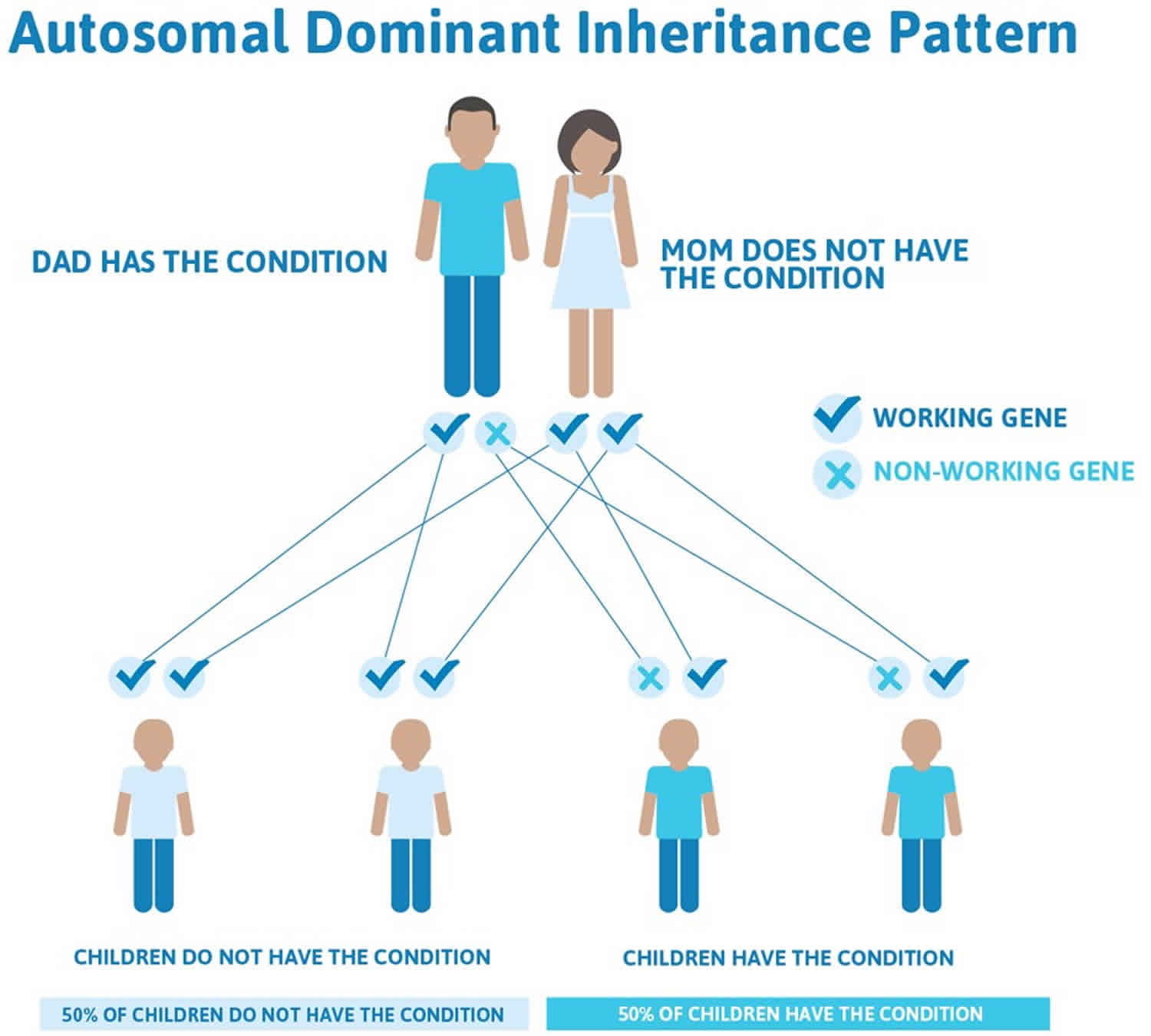
Job syndrome has an autosomal dominant pattern of inheritance, which means one copy of an altered gene in each cell is sufficient to cause the disorder. In about half of all cases caused by STAT3 gene mutations, an affected person inherits the genetic change from an affected parent. Other cases result from new mutations in this gene. These cases occur in people with no history of the disorder in their family.
In cases where the autosomal dominant condition does run in the family, the chance for an affected person to have a child with the same condition is 50% regardless of whether it is a boy or a girl. These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
- When one parent has the abnormal gene, they will pass on either their normal gene or their abnormal gene to their child. Each of their children therefore has a 50% (1 in 2) chance of inheriting the changed gene and being affected by the condition.
- There is also a 50% (1 in 2) chance that a child will inherit the normal copy of the gene. If this happens the child will not be affected by the disorder and cannot pass it on to any of his or her children.
Figure 1. Job syndrome autosomal dominant inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Job syndrome symptoms
Symptoms of Job syndrome include:
- Variable severity in affected family members
- Bone and tooth defects, including fractures and losing the baby teeth late
- Skin abscesses and infection
- Repeated sinus infections
- Repeated lung infections
- Rash similar to atopic dermatitis (eczema)
- The rash is often present at birth or within the first few weeks, unlike atopic dermatitis (which appears after 3 months of age)
- Secondary infection with Staphylococcus aureus resulting in crusted dermatitis, folliculitis and abscesses
- Episodes of bronchitis and pneumonia
- Other sites may also become infected including sinuses, ears, teeth and gums
- Mucocutaneous candidiasis
- Pitted scarring of the face
- Bony abnormalites including fractures and scoliosis (twisted spine)
- Dental abnormalities such as double rows of teeth
- Unusual facial appearance
- Very high levels of the ‘allergy’ immunoglobulin IgE in the blood
- High levels of eosinophils in the blood
Individuals with Job syndrome typically manifest in the newborn period with a rash, often diagnosed as eosinophilic pustulosis. The rash evolves into an eczematoid dermatitis that is often driven by staphylococcal infection 2.
Recurrent staphylococcal boils usually manifest in the first few years of life, and may be “cold,” lacking the cardinal features of inflammation, warmth, redness, and pain.
Recurrent pneumonias begin as well in the first few years, with the most common bacterial isolates being Staphylococcus aureus, Streptococcus pneumoniae, and Haemophilus influenzae. Abnormal healing of these pneumonias, pneumatocoeles, and bronchiectasis are common complications.
Staphylococcal infections outside of the lung and skin, such as osteomyelitis or liver abscess, occur much less frequently.
Mucocutaneous candidiasis affecting the oropharynx, vagina, fingernails, and toenails is common.
Opportunistic infections may occur, including Pneumocystis jiroveci pneumonia, disseminated histoplasmosis and Cryptococcus, and secondary infection of the pneumatocoeles with molds such as Aspergillus fumigatus or Scedosporium species.
Decreased central memory T-cell formation may lead to increased incidence of varicella zoster virus (VZV) reactivation and modestly increased levels of circulating Epstein-Barr virus (EBV) 3.
Non-immunologic characteristics
Individuals with Job syndrome have several connective tissue, skeletal, and vascular abnormalities.
A characteristic facial appearance typically emerges by adolescence characterized by facial asymmetry, deep-set eyes, a broad nose, and prominent skin pores 4. A high arched palate is common, as are oral mucosal variants including palatal ridges [Domingo et al 2008]. Failure of primary teeth exfoliation is common; secondary tooth development is normal if the primary teeth are removed.
Skeletal abnormalities include osteopenia, minimal trauma fractures, and scoliosis. Scoliosis typically develops through childhood and adolescence, and may require surgical correction. Joint hyperextensibilty is common, and adults may have degenerative joint disease. Varying degrees of craniosynostosis can be seen, although surgical correction is rarely required. Skull radiographs often have a beaten copper appearance.
Brain imaging reveals Chiari 1 malformations in approximately 20% of individuals and focal hyperintensities prominent on T2-weighted images in approximately 70% of individuals. The focal hyperintensities are usually localized to the white matter and tend to increase in number with age. Both the Chiari 1 malformations and the hyperintensities are usually asymptomatic 5.
Vascular abnormalities including middle-sized arterial tortuosity and aneurysms have been described 6. The coronary arteries have been the most completely studied. The combination of tortuosity and dilation is found in approximately 50% of affected individuals; either abnormality is present in approximately 70%. Clinical sequelae have been rare but include myocardial infarction. Cerebral artery aneurysm has also been described and infrequently associated with subarachnoid hemorrhage.
Symptoms of esophageal dysmotility are present in more than 50% of individuals and manifest as gastrointestinal reflux disease and dysphagia. Upper endoscopy frequently shows eosinophilic esophagitis. Diverticuli can occur at a relatively young age and may be associated with bowel perforation 7. Isolated colonic perforations have also been described.
Job syndrome possible complications
Job syndrome complications may include:
- Repeated infections
- Sepsis
Job syndrome diagnosis
The diagnosis of Job syndrome (autosomal dominant hyper IgE syndrome) is most often made based on a combination of clinical and laboratory findings. Diagnostic guidelines have been developed that include both immunologic /infectious manifestations and skeletal/connective tissue abnormalities. Molecular genetic testing of the STAT3 gene confirms the diagnosis 8.
A physical exam may show:
- Curving of the spine (kyphoscoliosis)
- Osteomyelitis
- Repeat sinus infections
Tests used to confirm the diagnosis include:
- Absolute eosinophil count
- Complete blood count (CBC) with blood differential
- Serum globulin electrophoresis to look for high blood IgE level
An eye exam may reveal signs of dry eye syndrome.
A chest x-ray may reveal lung abscesses.
Other tests that may be done:
- CT scan of the chest
- Cultures of the infected site
- Special blood tests to check parts of the immune system
- X-ray of the bones
- CT scan of the sinuses
A scoring system that combines the different problems of Hyper IgE syndrome is used to help make the diagnosis.
A scoring system that weighted both the immunologic and somatic features of Job syndrome was designed to aid in the clinical diagnosis of these patients.
Table 1. Scoring system for Job Syndrome
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 10 | |
| Clinical Findings | ||||||||||
| Highest IgE (IU/mL) | < 200 | 200-500 | 501-1000 | 1001-2000 | >2000 | |||||
| Total # skin abscesses/boils | None | 1-2 | 3-4 | >4 | ||||||
| Total # pneumonias | None | 1 | 2 | 3 | >3 | |||||
| Parenchymal lung abnormalities | None | Bronchiectasis | Pneumatocele | |||||||
| Other serious infection | None | Present | ||||||||
| Fatal infection | None | Present | ||||||||
| Highest eosinophils/uL | < 700 | 701-800 | >800 | |||||||
| Newborn rash | None | Present | ||||||||
| Eczema (worst stage) | None | Mild | Moderate | Severe | ||||||
| Sinusitis/otitis (# in worst year) | 1-2 | 3 | 4-6 | >6 | ||||||
| Candidiasis | None | Oral, vaginal | Fingernail | Systemic | ||||||
| Retained primary teeth | None | 1 | 2 | 3 | >3 | |||||
| Scoliosis (max. curvature) | < 10 | 10-14 | 15-20 | >20 | ||||||
| Minimal trauma fractures | None | 1-2 | >2 | |||||||
| Hyperextensibility | None | Present | ||||||||
| Characteristic face | None | Mild | Present | |||||||
| Increased interalar distance | < 1 SD | 1-2 SD | >2 SD | |||||||
| High palate | None | Present | ||||||||
| Congenital anomaly | None | Present | ||||||||
| Lymphoma | None | Present |
Job syndrome treatment
There is no known cure for Job syndrome. The goal of treatment is to control the infections. Medicines include:
- Antibiotics
- Antifungal and antiviral medicines (when appropriate)
Good general hygiene is helpful in preventing skin infections. Some doctors may recommend preventive antibiotics (prophylactic antimicrobials) for people who develop many infections, especially with Staphylococcus aureus. This treatment does not change the condition, but it can lessen its complications.
Preventive antibiotics, such as trimethoprim/sulfamethoxazole, are highly effective. With the increasing prevalence of antibiotic-resistant S aureus and other pathogens, it is important that microbial culture sensitivities be actively obtained to direct antimicrobial therapies. As patients often have minimal signs of systemic toxicity, the threshold for considering active infection requiring aggressive treatment should be low.
The control of dermatitis is essential to decrease the frequency of skin infections and improve the quality of life, particularly for pediatric patients with more severe dermatitis. Exposure to low concentrations of bleach, such as achieved from frequent swimming in a chlorinated pool or taking bleach baths (1/2 cup of bleach to a tub of water for 15 minutes, 3 times a week) are highly effective for controlling staphylococcal skin infections.
Mucocutaneous candidiasis and onychomycosis are treated as needed with antifungals therapy, most commonly fluconazole. Broadening antifungal coverage to include Aspergillus species (itraconazole, voriconazole, posaconazole) should be considered for individuals with pneumatoceles. Annual flu vaccine is recommended.
Intravenous immunoglobulin (IVIG) therapy has been used anecdotally in selected patients with improvement in severe infections.
Currently, no clear recommendations exist for routine medical therapy of the vascular, musculoskeletal, and connective tissue abnormalities associated with the disorder. Immune reconstitution would theoretically be of benefit for Job syndrome, but the benefit to repairing the immune dysfunction while leaving the somatic abnormalities intact in these patients is unknown. Bone marrow or stem cell transplant has been used in too few cases to be sure of its safety or value in Job syndrome.
Sometimes, surgery is needed to drain abscesses. The most common surgical procedure needed is incision and drainage of skin boils, which can often be performed in the office with local anesthesia. Extraction of primary teeth because of delayed deciduation is also common. Some patients with severe scoliosis require bracing and surgical treatment depending upon the degree of curvature. Rarely, patients require lobectomy or pneumonectomy because of pneumatoceles with recurrent infection. However, surgical resection of pneumatoceles should be undertaken only with expert advice, as patients may experience difficulty with residual lung expansion to fill the intrathoracic space with attendant medical complications.
Further outpatient care
Most patients continue as outpatients to monitor for changes in skin disease, pulmonary status, and musculoskeletal complaints. Frequent monitoring is recommended for patients with pneumatoceles or bronchiectasis, as these patients are at increased risk for secondary lung infections. Patients need to be aware that systemic signs of infection are often absent and to seek care if any infection is suspected.
Patients may benefit from referral to tertiary care centers well versed in the evaluation, monitoring and treatment of patients with this rare disorder.
Job syndrome prognosis
Job syndrome (hyper IgE syndrome) is a lifelong chronic condition. Each new infection requires treatment.
Job syndrome life expectancy
Survival is typically into adulthood, but a shortened life span is typical, with deaths occurring predominantly in adulthood due to the consequences of chronic infections 8. Most deaths of individuals with Job syndrome are associated with Gram-negative (Pseudomonas) or filamentous fungal pneumonias (most commonly Aspergillus) infecting damaged lung parenchyma (i.e., pneumatocoeles, bronchiectasis) in the setting of pneumatoceles or bronchiectasis or both 9. Fungi such as Aspergillus and Scedosporium species, may invade the pulmonary blood vessels leading to massive hemoptysis, or may disseminate to multiple organs. These infections are secondary opportunists in regions of destroyed lung caused by the inappropriate healing of previous infections 10. In a recent review of a large cohort of patients, the average living patient age was 27 years, but ages ranged from 3-58 years. Infection-related deaths occurred at an average age of 29 years.
Complications of arterial aneurysms have included myocardial infarction related to coronary artery aneurysm and subarachnoid hemorrhage related to intracranial aneurysm 11.
Job syndrome patients are at increased risk for Hodgkin and non-Hodgkin lymphoma (relative risk 259), although the number of cases reported is small 12. Lymphomas treatment has been successful with standard chemotherapy. Other malignancies have been reported 13.
References- Autosomal dominant hyper-IgE syndrome. https://ghr.nlm.nih.gov/condition/autosomal-dominant-hyper-ige-syndrome
- Eberting CL, Davis J, Puck JM, Holland SM, Turner ML. Dermatitis and the newborn rash of hyper-IgE syndrome. Arch Dermatol. 2004;140:1119–25
- Siegel AM, Heimall J, Freeman AF, Hsu AP, Brittain E, Brenchley JM, Douek DC, Fahle GH, Cohen JI, Holland SM, Milner JD. A critical role for STAT3 transcription factor signaling in the development and maintenance of human T cell memory. Immunity. 2011;35:806–18
- Grimbacher B, Holland SM, Gallin JI, Greenberg F, Hill SC, Malech HL, Miller JA, O’Connell AC, Puck JM. Hyper-IgE syndrome with recurrent infections–an autosomal dominant multisystem disorder. N Engl J Med. 1999a;340:692–702.
- Freeman AF, Collura-Burke CJ, Patronas NJ, Ilcus LS, Darnell D, Davis J, Puck JM, Holland SM. Brain abnormalities in patients with hyperimmunoglobulin E syndrome. Pediatrics. 2007a;119:e1121–5.
- Chandesris MO, Azarine A, Ong KT, Taleb S, Boutouyrie P, Mousseaux E, Romain M, Bozec E, Laurent S, Boddaert N, Thumerelle C, Tillie-Leblond I, Hoarau C, Lebranchu Y, Aladjidi N, Tron F, Barlogis V, Body G, Munzer M, Jaussaud R, Suarez F, Clément O, Hermine O, Tedgui A, Lortholary O, Picard C, Mallat Z, Fischer A. Frequent and widespread vascular abnormalities in human signal transducer and activator of transcription 3 deficiency. Circ Cardiovasc Genet. 2012;2012;5:25–34.
- Stover DG, Freeman AF, Wright PW, Hummell DS, Ness RM. Diverticulitis in a young man with hyper-IgE syndrome. South Med J. 2010;103:1261–3.
- Hsu AP, Davis J, Puck JM, et al. Autosomal Dominant Hyper IgE Syndrome. 2010 Feb 23 [Updated 2012 Jun 7]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK25507
- Freeman AF, Kleiner DE, Nadiminti H, Davis J, Quezado M, Anderson V, Puck JM, Holland SM. Causes of death in hyper-IgE syndrome. J Allergy Clin Immunol. 2007b;119:1234–40.
- Freeman AF, Kleiner DE, Nadiminti H, Davis J, Quezado M, Anderson V. Causes of death in hyper-IgE syndrome. J Allergy Clin Immunol. 2007 May. 119(5):1234-40.
- Fathi AR, Vortmeyer A, Holland SM, Pluta RM. Intracranial aneurysms associated with hyperimmunoglobulinaemia E (Job) syndrome: report of two cases. J Neurol Neurosurg Psychiatry. 2011;82:704–6.
- Leonard GD, Posadas E, Herrmann PC, Anderson VL, Jaffe ES, Holland SM. Non-Hodgkin’s lymphoma in Job’s syndrome: a case report and literature review. Leuk Lymphoma. 2004 Dec. 45(12):2521-5.
- Leonard GD, Posadas E, Herrmann PC, Anderson VL, Jaffe ES, Holland SM, Wilson WH. Non-Hodgkin’s lymphoma in Job’s syndrome: a case report and literature review. Leuk Lymphoma. 2004;45:2521–5.